Abstract
Purpose
This study tested whether participation in organized physical activity (active vs. inactive) or weight status (normal weight vs. overweight or obese) independently relate to hildren’s cognition, using a matched-pairs design.
Design and Methods
Normal weight, active children (8–11 yrs, 5th–75th percentile BMI) were recruited from extracurricular physical activity programs while normal weight inactive (5th–75th percentile BMI) and overweight inactive children (BMI ≥85th percentile) were recruited from local Augusta, Georgia area schools. Measures included the Cognitive Assessment System, anthropometrics, and parent- and self-report of physical activity. Paired t-tests compared cognition scores between matched groups of normal weight active vs. normal weight inactive (N=24 pairs), normal weight inactive vs. overweight inactive (N=21 pairs), and normal weight active vs. overweight inactive children (N=16 pairs). Children in each comparison were matched for race, gender, age, and socioeconomic status.
Results
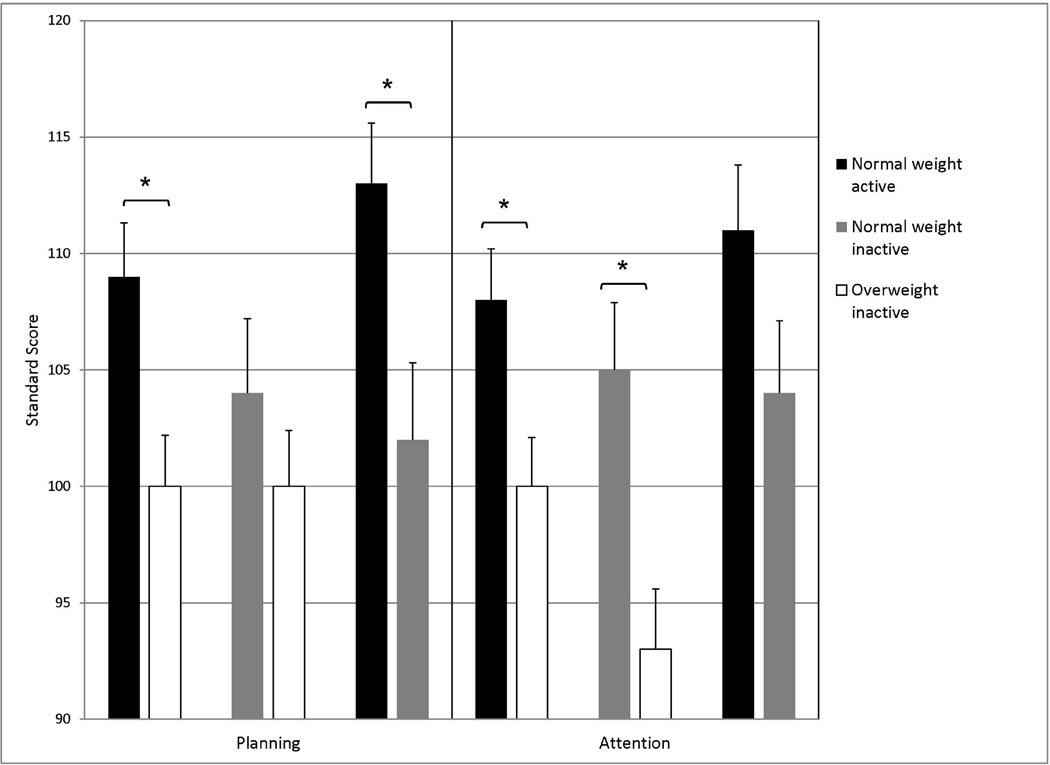
Normal weight active children had higher Planning (M±SD=109±11 vs. 100±11, p=.011) and Attention scores (108±11 vs. 100±11, p=013) than overweight inactive children. Normal weight inactive children had higher Attention scores than overweight inactive children (105±13 vs. 93±12, p=008). When compared to normal weight inactive children, normal weight active children had higher Planning (113±10 vs. 102±13, p=008) and marginally higher Attention scores (111±11 vs. 104±12, p=06).
Conclusion
Findings suggest independent associations of children’s weight status with selective attention, and physical activity with higher-order processes of executive function.
Keywords: childhood obesity, overweight, physical activity, executive function, cognition
Introduction
The increase in childhood overweight and obesity over the past several decades has fueled concern about the relationship between children’s physical and mental health (65). There is widespread concern that the entrenched environmental changes underlying the obesity epidemic are impairing not only the physical health of our youth, but also their cognition and academic achievement (35). Despite many recent studies on this topic, it remains unclear whether weight status and physical activity are independently related to children’s cognition.
Fitness and children’s executive function and academic achievement
Numerous studies, including one in overweight children (17), have linked better fitness with better cognition (6, 11, 23, 24, 68). Executive function appears to be the type of cognition most closely linked with fitness and physical activity (12). Executive function is a broad construct encompassing the higher order cognitive functions necessary for reasoning, problem solving, planning, organization, and behavioral execution (66). Executive function is crucial for academic achievement, relies on prefrontal cortex circuitry, and includes the more specific but overlapping core elements of cognitive control, namely inhibition (e.g., selective attention), working memory, and cognitive flexibility (20). Physically fit children have also been shown to have better academic achievement than their less-fit peers (72). The pediatric literature supports a cross-sectional link of one component of executive function (i.e. selective attention, also referred to as resistance to distraction) with aerobic fitness, and this is often thought to be the mechanism conferring brain benefits from physical activity (33).
Physical activity and cognition
The cross-sectional literature associating objectively measured physical activity with children’s cognition is scant. To our knowledge, only two groups have examined the association of accelerometry-measured physical activity with cognition in children (41, 67, 69, 70). A study in 224 children linked greater physical activity with improved reaction time, but not other aspects of cognition (i.e., memory, executive function, sustained attention) (67). In a small study by van der Niet and colleagues (N = 80), physical activity volume, particularly that spent in moderate to vigorous physical activity, was associated with better performance on higher-order executive functions (Tower of London), while no association with a task thought to tap cognitive flexibility and/or working memory (Trail Making Test) was detected (60, 70). A structural equation model by the same group in a larger sample of children (N = 263) supported executive function as a mediator between fitness and academic achievement (69).
Trials of physical activity with cognitive outcomes
The case for physical activity improving children’s cognition is more robust, though trials vary with regard to acute bouts or training programs, weight status and fitness level of enrolled children, and cognitive outcomes (19, 34, 64, 71). Acute, single bouts of physical activity have been shown in several randomized trials to benefit selective attention (71). Two groups have conducted trials showing that aerobic exercise programs result in improvements in executive function, compared to no intervention (19, 34). The first of these trials randomized 222 inactive, overweight or obese 7–11 year olds, characterized by poor aerobic fitness, to either a control condition or a low dose (20 min) or high dose (40 min) daily vigorous activity program (19). Psychometric outcome measures demonstrated linear dose-response effects of greater time in vigorous activity benefiting higher-order executive function and math achievement. The other trial, in a similar number of children (7–9 years old) with a healthy average fitness level, utilized laboratory tasks of core executive function, which showed a benefit of the physical activity program on cognitive flexibility (34).
Physical activity is distinct from fitness
Habitual physical activity and physical fitness should not be conflated. Physical activity is behavior (movement of skeletal muscle that results in energy expenditure). In contrast, physical fitness is an adaptive state of the human body in response to physical activity (7), which also increases with growth in children (50). Physical activity has only small associations with children’s physical fitness (1, 40). Despite this distinction, fitness is often used as a proxy for physical activity, and interpreted as demonstrating effects of physical activity (e.g., 36). However, cross-sectional associations with fitness do not necessarily correspond to effects of increased physical activity in an experiment (17). Independent of physical activity, constitutional or other factors may explain the association of fitness with cognitive ability. Baseline aerobic fitness and improved fitness with training are each highly variable and substantially genetically influenced (2, 3). In children, growth is a major influence on physical capacity (50). Improved fitness is a candidate mechanism for the benefit of physical activity on cognition. However, among experimental studies that demonstrate benefits of physical activity on brain and cognitive function in children (10, 19, 34, 43, 44, 62), none showed a direct link between improved fitness and better cognition. A meta-analysis found no support for aerobic fitness mediating the effect of physical activity on cognition (23) and a study that tested this link in children did not confirm it (14).
Weight status and cognition
Childhood overweight and high adiposity have been associated with poorer cognitive function and poor academic achievement, compared to children with lower adiposity or BMI (17, 37–39, 49). The largest of these studies (N = 2,519) found greater risk of poor performance on a single psychometric subtest of visuospatial organization (block design) among overweight (odds ratio = 2.0) or obese (odds ratio = 2.8) children and adolescents, compared to normal weight peers, after adjusting for a wide variety of confounders; the differences in working memory (digit span) and academic achievement did not survive adjustment (49). Most other studies have focused on executive function (e.g., NoGo and flanker tasks, and more complex psychometric tests) (17, 37–39). Weight status has been described as an easily measurable marker of physical activity (16), and fatness is strongly related to physical activity (1, 54). Thus, the associations of overweight status and adiposity with poorer cognition and academic achievement may instead reflect the benefits of physical activity. One study matched obese and normal weight children on gender and fitness, and found worse performance by the obese children on a flanker task (39). However, some studies have obtained null results (31) or attributed such associations to confounders such as physical activity, fitness or social factors (13, 16). Thus, it is unclear whether physical activity and weight status are associated with cognition independently from one another.
This study utilized a matched-pairs design to investigate the independent relationships of weight status and physical activity with children’s cognition. It was hypothesized that normal weight active children would demonstrate superior executive function relative to normal weight inactive and overweight or obese inactive children. Because the evidence is stronger for fitness and physical activity than weight status or adiposity as determinants of cognition, normal weight inactive children were expected to show similar performance to overweight inactive children.
Methods
Participants
Forty-five normal weight children (24 active, 21 inactive) ranging from 7 to 11 years of age (M = 9.5 years, SD = 1.1; 56% female, 27% Black) were recruited via flyers distributed to community sites. Children were eligible if they were normal weight (5th – 75th percentile body mass index, BMI, for age and sex (55)), did not have a medical condition that would affect study results or limit physical activity, and were not taking medication that would affect study results (e.g. antipsychotics, stimulants). Normal weight children were classified as active if they were recruited from local extracurricular physical activity programs, including swimming, boxing, tennis, gymnastics, soccer, and dance programs, that met for >1 hour per week (n = 21), with parent corroboration of their participation, or if they were recruited by word of mouth, with parent report of being enrolled in an athletic program for >1 hour per week (n = 3). Normal weight children recruited from other community sites (e.g. schools, churches), whose parent reported that they took part in <1 hr/wk of organized physical activity, were assigned to the inactive condition (Table 1).
Table 1.
Participant characteristics by matched group comparisons [N or Mean (SD)]
| Normal weight | Overweight | Normal weight | Overweight | Normal weight | Normal weight | |
|---|---|---|---|---|---|---|
| active vs. inactive | active vs. inactive | active vs. inactive | ||||
| (N = 24 pairs) | (N = 21 pairs) | (N = 16 pairs) | ||||
| White | 18 | 18 | 15 | 15 | 12 | 12 |
| Black | 6 | 6 | 6 | 6 | 4 | 4 |
| Male | 14 | 14 | 6 | 6 | 6 | 6 |
| Female | 10 | 10 | 15 | 15 | 10 | 10 |
| Parent marital status and education | ||||||
| Married | 19 | 19 | 18 | 18 | 14 | 15 |
| Not married | 5 | 5 | 3 | 3 | 2 | 1 |
| High school or less | 3 | 6 | 2 | 2 | 2 | 2 |
| At least some college | 21 | 18 | 19 | 19 | 14 | 14 |
| Age (years) | 9.7 (0.9) | 9.7 (0.9) | 9.3 (1.2) | 9.2 (1.0) | 9.9 (0.8) | 9.4 (1.3) † |
| BMI percentile | 39 (20) | 97 (0)*** | 36 (19) | 97 (0)*** | 32 (18) | 37 (17) |
| BMI z-score | −0.3 (0.6) | 2.0 (0.5)*** | −0.4 (0.6) | 2.0 (0.4)*** | −0.5 (0.5) | −0.4 (0.5) |
| Body fat (%) | 18 (4) | 40 (6)*** | 21 (4) | 41 (6)*** | 19 (5) | 21 (4)† |
| Resting heart rate (bpm) | 75 (3) | 81 (10)* | 84 (12) | 87 (12) | 74 (6) | 83 (10)*** |
| Physical activity (PA) | ||||||
| Vigorous PA(days/wk) | 4.3 (1.8) | 2.5 (2.1)*** | 3.4 (2.6) | 3.6 (2.6) | 4.8 (1.7) | 3.9 (2.6) |
| Moderate to vigorous | 6.3 (3.0) | 4.3 (2.6)* | 5.6 (4.1) | 5.4 (3.4) | 6.9 (2.8) | 6.7 (3.9) |
| PA (days/week) | ||||||
| PA programs (hrs/wk) | 2.4 (3.0) | 0.3 (0.4)** | 0.1 (0.2) | 0.6 (0.9)* | 2.7 (3.7) | 0.1 (0.3)* |
| Cognitive Assessment System | ||||||
| Planning | 109 (11) | 100 (11)* | 104 (15) | 100 (11) | 113 (10) | 102 (13)** |
| Attention | 108 (11) | 100 (11)* | 105 (13) | 93 (12)** | 111 (11) | 104 (12)† |
| Simultaneous | 108 (13) | 107 (9) | 110 (14) | 106 (15) | 109 (11) | 108 (15) |
| Successive | 98 (15) | 101 (9) | 103 (11) | 99 (10) | 98 (13) | 101 (10) |
| Full Scale | 107 (12) | 102 (10) | 107 (14) | 99 (13) † | 110 (10) | 104 (12) |
p < .10
p < .05
p < .01
p < .001 for paired t-tests
Forty-five overweight, inactive children (aged 7–11; mean age = 9.5; SD= 1.0; 56% female, 27% Black) were also included in the study. These children were selected from a prior study based on characteristics (i.e., race, sex, age, parental education, parental marital status) to match the 45 normal weight children (17). In that study, Black or White children were eligible if they were 8–11 yrs old, overweight (≥85th percentile BMI), were not currently participating in any organized physical activity program for more than one hour per week, had no medical condition that would affect study results or limit physical activity (e.g. orthopedic conditions), and attended a school that was included in the study.
Methods and Procedures
Children and parents completed written informed assent and consent. The study was reviewed and approved by the Medical College of Georgia’s Institutional Review Board. Children were offered a $20 gift card as an incentive for completing evaluations. Parents reported their education level (high school or less, or at least some college) and marital status (married or not), their child’s demographic information and health history, and the level of their child’s participation in organized physical activity programs. All child measures were obtained in our laboratories by trained research staff. Characteristics of the sample are presented in Table 1.
Anthropometrics
Anthropometrics were measured at least twice until consistent measures were obtained. Body weight (in light clothing) and height (without shoes) were measured with an electronic scale (Detecto, Web City, MO) and stadiometer (Tanita, Arlington Heights, IL) and converted to a BMI z-score for analysis (55). BMI percentiles are presented in Table 1 for interpretability. Because weight status was an inclusion criterion for the study, this was evaluated prior to enrollment.
Body composition and fitness
Whole-body dual energy x-ray absorptiometry (QDR 4500W, Hologic Inc., Bedford, MA) assessed percent body fat, which adjusts for body mass. Resting heart rate was a proxy for aerobic fitness (56). Children rested for 10 minutes, and then 5 measurements were taken with a Dinamap machine at 1 minute intervals, with the last 3 averaged.
Physical activity
Physical activity program leaders in the community were contacted to recruit participating children. In addition, parents reported “all physical activity programs this child is involved in,” including each type of activity, days per week, minutes per day, and duration of participation. Hours per week were calculated and averaged across seasons. For example, a child who participated in football for 10 hours per week during Fall, and no other program during the rest of the year, was assigned a value of 2.5 hours per week.
To supplement their adult-verified participation in organized physical activity programs, children reported the number of days over the past week they participated in bouts of moderate (i.e., “On how many of the past 7 days did you participate in physical activity for at least 30 minutes that did not make you sweat or breathe hard, such as fast walking, slow bicycling, skating, pushing a lawn mower, or mopping floors?”) and vigorous physical activity (i.e., “On how many of the past 7 days did you exercise or participate in physical activity for at least 20 minutes that made you sweat and breathe hard, such as bicycling, fast dancing, or similar aerobic activities?”)(4, 5, 9).
Cognition
Children’s cognitive performance was assessed via the Cognitive Assessment System (CAS) (52), with scoring via software designed by the test creators (CAS Rapid Score 1.0, 51) reported in Standard Scores (normative mean of 100 and standard deviation of 15). The CAS has demonstrated excellent validity and reliability, and is standardized by gender and age on a large representative sample of 5 to 17 year old U.S. children stratified for gender, ethnicity and race, parental education, classroom placement, region, and community setting (52). Each of four scales is comprised of three subtests. The Planning scale assesses higher-order executive function processes (i.e., strategy generation and application, self-regulation, intentionality, and utilization of knowledge; internal reliability r = .88). The Attention scale subtests require focused, selective cognitive activity and resistance to distraction (r = .88). The Simultaneous scale subtests involve spatial and logical questions that contain nonverbal and verbal content (r = .93). The Successive scale subtests require the analysis or recall of stimuli arranged in sequence and the formation of sounds in order (r = .93). Full Scale is a global composite scale. Thus, it is considered a valid measure of cognitive ability that in combination with a standardized achievement test, can qualify a child for educational services to address a learning disability. The CAS was implemented by a staff member with graduate-level training in Psychology. Cognitive testing was typically done after school for both the normal-weight and overweight groups.
Statistical Methods
Data were analyzed with IBM SPSS Statistics 21 at an alpha level of .05. Data were screened for violations of assumptions. Children in each group were matched to peers in the comparison group (normal weight active vs. overweight inactive; normal weight inactive vs. overweight inactive; normal weight active vs. normal weight inactive) on race, sex, age, parental marital status, and parental education. Paired t-tests and McNemar’s exact χ2 tests were conducted to compare matched groups on demographic characteristics to ensure group balance; on physical activity and health measures (anthropometrics, fatness, and heart rate), to verify the intended contrast between groups; and on cognitive scores to test hypotheses.
Results
Descriptive statistics by group comparison are presented in Table 1. None of the children were reported to have a learning problem such as attention-deficit disorder, or taking medication for such a disorder.
Physically active normal weight vs. inactive overweight children
Twenty-four physically active, normal weight children were matched identically to overweight, inactive children on race, gender, and parental marital status, and as closely as possible on age and parental education. Therefore, weight status and activity level were isolated as the primary differences between groups. The groups did not differ on age (p = .86) or parental education (p = .45). As expected, the active normal weight children had lower BMI z scores and adiposity (p < .001 for both), a lower resting heart rate (p = .045), more self-reported vigorous physical activity (p < .001), and greater parent-reported participation in physical activity programs (p < .01) than overweight inactive children. The active normal weight children had higher scores than inactive overweight children on CAS Planning (mean difference = 9.3 ± 16; t(23) = 2.8, p = .01) and Attention scales (mean difference = 7.7 ± 14; t(23) = 2.7, p = .01). The groups did not differ on Simultaneous, Successive, or Full Scale scores. CAS scores by group comparison are presented in Table 1 and Figure 1.
Figure 1.
Planning and Attention Scale means (standard error) from Cognitive Assessment System by matched group comparison. *p < .05.
Inactive normal weight vs. inactive overweight children
Twenty-one inactive, normal weight children were matched identically to overweight inactive children on race, gender, parental marital status and education, and as closely as possible on age. Therefore, weight status was isolated as the primary difference between groups. The groups did not differ on age (p = .59). As expected, the normal weight children had lower BMI z scores and adiposity (p < .001 for both), with similar resting heart rate and self-reported vigorous physical activity compared to their overweight peers. Children in the inactive normal weight group had higher CAS Attention scores (mean difference = 13 ± 20; t(20) = 3.0, p = .008), and marginally higher Full Scale scores (mean difference = 8 ± 20; t(20) = 1.9, p = .079) than inactive overweight children. The groups did not differ on the Planning, Simultaneous or Successive scales.
Active normal weight vs. inactive normal weight children
Sixteen physically active normal weight children were matched identically to inactive normal weight children on race, gender and parental education level, and as closely as possible on age and parent marital status. Therefore, activity level was isolated as the primary difference between groups. The active group was slightly older, though this did not reach statistical significance (mean difference = 0.5 ± 1.0 year; t(15) = 1.9, p = .082). The groups did not differ on parental marital status (p > .99). As expected, the active group had a lower resting heart rate than the inactive children (mean difference = 9.5 ± 11 bpm, t(15) = 3.6, p = .003). The active children had similar BMI z-scores (p = .39) and marginally lower adiposity (mean difference = 2.7 ± 5.0%, t(15) = 2.1, p = .050) compared to their inactive peers. While the active group reported more days with bouts of vigorous physical activity compared to their inactive peers, this was not a significant difference (mean difference = 0.9 ± 2.7 days/week, t(15) = 1.3, p = .21). Parents of active children reported significantly greater participation by the child in structured physical activity programs than did parents of the inactive group (mean difference = 2.6 ± 1.1 hours/week, t(11) = 2.4, p = .037), all but one of whom reported zero hours/week in physical activity programs. The active children had higher CAS Planning scores than the inactive children (mean difference = 11 ± 14; t(15) = 3.0, p = .008) and marginally higher Attention scores (7.0 ± 13; t(15) = 2.1, p = .056). The groups did not differ on CAS Simultaneous, Successive, or Full Scale scores.
Discussion
This study compared children on participation in organized physical activity programs (active vs inactive) and on weight status (normal weight vs overweight or obese), after matching to reduce bias from demographic factors. Organized physical activity and weight status were each independently associated with distinct aspects of cognition. Active, normal weight children demonstrated a substantial cognitive advantage over their inactive peers (whether normal weight or overweight) on 2 of 4 cognitive scales which tap executive function (not memory or gestalt processing). A more specific contrast isolating physical activity revealed an independent association of higher-order executive function (CAS Planning) with physical activity. Thus, participation in extracurricular physical activity programs was associated with cognitive advantage, independent of weight status and potential confounders (i.e., age, race, gender, parent education, and parent marital status).
In a complementary comparison, weight status was contrasted in matched groups of inactive children. This revealed a selective and substantial cognitive advantage for the normal weight group on selective attention (i.e., the Attention scale of the CAS), with no difference on Planning, a measure designed to tap higher-order aspects of executive function. Thus normal weight status was independently linked with less distractibility, but not higher-order executive function, when compared to overweight children at a similar low level of physical activity participation and fitness. Thus, both physical activity and weight status showed large, consistent, and mutually independent relationships with aspects of cognitive function in these children.
As mentioned earlier, overweight status has been described as an easily measurable marker of inactivity (16). Thus, the link between overweight and poorer cognition in the non-experimental literature may in fact reflect the benefits of habitual physical activity. Statistical control to address such confounding has been used in this literature, but have not answered this question, due to reliance on fitness as a proxy for physical activity (13, 16, 37, 58). A correlational study associated greater adiposity with worse inhibition (NoGo task), independent of fitness level (37); however, physical activity was not assessed. Another cross-sectional study tested independent associations of adiposity and fitness with cognition in children (58). That study found that adiposity was independently associated with cognitive flexibility, and fitness with both inhibition and cognitive flexibility; however, physical activity was not measured.
The current study results show that weight status was separable from physical activity in its association with cognition. This study used a different, more reliable type of cognitive measurement (a reliable standardized psychometric test made up of several subtests tapping common functions, vs. individual laboratory tasks), and made novel comparisons -- adiposity vs. weight status, and fitness vs. physical activity. In contrast to the current findings, the modeling study did not confirm an association of adiposity with selective attention (flanker task), whereas the current study linked overweight status with greater distractibility (58). This may be due to greater sensitivity in this study owing to greater contrast between weight status and physical activity groups. The current study used a design approach rather than statistical adjustment to better examine closely related factors separately and more effectively eliminate potential confounders (63).
The association of the Attention scale with body fat and physical activity is consistent with previous work in children (11, 37) but inconsistent with a randomized controlled trial of physical training, where a 3 mo aerobic exercise intervention in overweight inactive children selectively improved executive function; that is, benefit was shown on the Planning scale, but not the Attention scale of the CAS (19). It is possible but not yet demonstrated that normal weight children who undergo an exercise program would show improvement on the CAS Attention scale. Another randomized controlled trial of physical activity in children used the Stroop Color and Word Test; however the final experimental result have not been reported (8, 26). Other reports from the same trial reported no differential effect of exercise vs control condition on flanker and go/no-go task performance, but significant exercise benefits on a different color-shape switch task (10, 22, 34). The CAS Attention scale includes a similar switching task, which most theorists consider a measure of cognitive flexibility, a core executive function (20, 48). However, the neo-Lurian conceptualization of the CAS, a more psychometrically robust measure than single neuropsychological tasks, considers the Attention scale a reflection of brainstem function (i.e., alertness) rather than prefrontal cortex circuitry (15). Increased alertness due to sympathetic activation explains some of the cognitive benefits induced by acute bouts of physical activity (45). The precise definition of executive function remains a topic of debate, and the evidence for cognitive benefits of aerobic training in children is still limited (71).
While aerobic fitness is an obvious candidate mechanism between children’s physical activity and cognitive ability or academic achievement, there is little support for this hypothesis. A meta-analysis of studies on this question did not support fitness as a mediator of the effect of physical activity on cognition (23); neither did the only study that reported testing this hypothesis in children (14). Rather, the animal literature suggests a direct effect of physical activity stimulating neuro- and angiogenesis through growth factors such as brain-derived neurotrophic factor (BDNF) (33). However, only one study has found evidence of changes in BDNF mediating improved cognition due to exercise training, and that only in the septuagenarian subset of older adults studied (46). Interestingly, BDNF is also linked with regulation of body weight. Like insulin and leptin, BDNF is both a neurotrophic factor and a regulator of energy homeostasis, as shown in human and animal work (28, 32, 47). Obese individuals have higher BDNF levels, perhaps as a result of positive energy balance (excess caloric intake), or in relation to fat mass (28, 57, 61). Another possible mechanism recently demonstrated in the animal literature includes obesity-induced inflammation hindering brain function; inflammation was induced by surgical fat implantation, and blunted by exercise (21). Another possible mechanism or mediator is sleep. Sleep disturbances associated with obesity are linked with a cognitive disadvantage similar in severity to those observed in this study (10 points on an IQ scale) (42), and aerobic training has been shown to improve sleep-disordered breathing (i.e. snoring) in overweight children (18). These mechanisms were not examined in this study, however.
This study adds to the existing literature by comparing weight status vs physical activity associations with children’s cognition, with matching on potential confounders and isolation of physical activity and weight status, thus demonstrating truly independent relationships with these distinct factors. This study controls these factors more effectively by design than previous work using statistical adjustment to try to isolate independent associations (58). In the current study, groups were matched by race, and overweight (mostly obese) status was linked with dramatically greater adiposity. This is important given population differences in lean mass that cause Blacks to be more likely to be classified as overweight despite normal levels of adiposity (25). Objective verification of participation by organized physical activity program staff (for 88% of the active children) is a strong behavioral measurement of physical activity. Age-appropriate physical activity self-reports and state of the art measures of adiposity and cognition were employed in this study. The Cognitive Assessment System is especially advantageous as it has been shown to be reliable and stable across populations and generates a comprehensive battery of scores specific to distinct aspects of cognitive functioning, enabling the identification of selective associations for physical activity and weight status with cognition (53).
The present study also has a few limitations that warrant mention. Active overweight children were not studied here; this group is important to include in future studies. Examiners were not blinded to group assignment, and different recruitment strategies were used for the overweight inactive and normal weight children who may have attended different schools. However, children were matched closely on relevant demographic characteristics and were from the same community. While children were not matched by school, we assessed whether the local school system they were enrolled in, which differ in quality (4th, 5th, and 7rd decile of students nationally, (29, 30)), differed by group. The only imbalance was in the normal-weight active vs. overweight inactive comparison, favoring the overweight children with more enrolled in the better school system than the normal-weight children (p = .02, data not shown). This is in the opposite direction to our findings; thus we do not believe this can account for our results. School system representation was otherwise comparable across groups (p = .65, .72 in chi square analyses), mostly drawing from low-income schools with free or reduced cost meals. Normal weight active children were mainly recruited from extracurricular physical activity programs, and normal weight inactive children were recruited from other sources. In fact, only one parent of a normal weight inactive child in this study reported any physical activity program participation by their child. While there was no objective quantification of the precise amount of physical activity (e.g., accelerometry), the groups were clearly distinct on this factor based on objective verification of program participation with parental confirmation, supplemented by child self-report of physical activity. Although resting heart rate is only a proxy for physical fitness, differences in resting heart rate between active and inactive groups further confirm that the contrast of physically active vs. inactive peers was achieved. A future study might match children in triples or quadruples, rather than pairs, to enable use of a correlated samples ANOVA with an omnibus significance test to reduce risk of type 1 error in pairwise comparisons.
The structured extracurricular athletic programs (e.g., yoga, golf, tennis, soccer, gymnastics, etc.) normal weight active children in the current study were recruited from each include use of goals, rules, and strategies, interaction with prosocial staff and peers, and a variety of other benefits associated with quality after-school programs, whether active or inactive (59). This raises the possibility that the cognitive advantage of this group over inactive peers independent of weight status may be due to non-movement qualities of the extracurricular physical activity programs. This potential confounding of physical activity benefits with programmatic benefits is ubiquitous in the children’s physical activity and mental health literature and makes it difficult to identify whether the mechanism of impact is neurobiological benefits of movement per se, cognitive challenges inherent to the physical activity (e.g., predicting trajectory of balls in the air, anticipating opponents’ strategy, motor sequencing), or whether they are attributable to other aspects of quality after school programs.
Conclusions
Regular physical activity may be necessary for children to function at their full potential. This may be particularly important for overweight or poorly fit children who are therefore at a disadvantage. Brain changes consistent with improved neural function have been demonstrated in normal weight and overweight children in response to physical activity programs (19, 34, 43, 44, 62). The current study moves the literature on physical health and cognition forward by utilizing a matched-pairs design to address a heretofore unanswered question in the literature. Findings show independent associations of physical activity and weight status on executive function in children (weight status with selective attention, and physical activity with higher-order planning processes). This supports the priority to act to stem the unwavering epidemic of obesity in children. Modest changes in weight trajectory (not necessarily weight loss) are enough to bring elementary school-age children back into normal weight status, which may have important benefits independent of physical activity (27).
Acknowledgments
Funding for the study was provided by NIH grants R01 DK070922, R01 HL087923, and the Medical College of Georgia Research Institute.
Footnotes
The authors report no conflicts of interest.
References
- 1.Blaes A, Baquet G, Fabre C, Van Praagh E, Berthoin S. Is there any relationship between physical activity level and patterns, and physical performance in children? Int J Behav Nutr Phys Act. 2011;8:122. doi: 10.1186/1479-5868-8-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bouchard C, Daw EW, Rice T, et al. Familial resemblance for VO2max in the sedentary state: the HERITAGE family study. Med Sci Sport Exer. 1998;30(2):252–258. doi: 10.1097/00005768-199802000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Bouchard C, Rankinen T. Individual differences in response to regular physical activity. Med Sci Sports Exerc. 2001;33(6 Suppl):S446–S451. doi: 10.1097/00005768-200106001-00013. discussion S52-3. [DOI] [PubMed] [Google Scholar]
- 4.Brener ND, Collins JL, Kann L, Warren CW, Williams BI. Reliability of the Youth Risk Behavior Survey Questionnaire. Am J Epidemiol. 1995;141(6):575–580. doi: 10.1093/oxfordjournals.aje.a117473. [DOI] [PubMed] [Google Scholar]
- 5.Brener ND, Kann L, Kinchen SA, et al. Methodology of the Youth Risk Behavior Surveillance System. MMWR Recomm Rep. 2004;53(RR-12):1–13. [PubMed] [Google Scholar]
- 6.Buck SM, Hillman CH, Castelli DM. The relation of aerobic fitness to Stroop task performance in preadolescent children. Med Sci Sports Exerc. 2008;40(1):166–172. doi: 10.1249/mss.0b013e318159b035. [DOI] [PubMed] [Google Scholar]
- 7.Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100(2):126–131. [PMC free article] [PubMed] [Google Scholar]
- 8.Castelli DM, Hillman CH, Hirsch J, Hirsch A, Drollette E. FIT Kids: Time in target heart zone and cognitive performance. Prev Med. 2011;(52 Suppl 1):S55–S59. doi: 10.1016/j.ypmed.2011.01.019. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. 2001 Youth Risk Behavior Survey. 2003 Oct 7; Available from: www.cdc.gov/yrbss.
- 10.Chaddock-Heyman L, Erickson KI, Voss MW, et al. The effects of physical activity on functional MRI activation associated with cognitive control in children: a randomized controlled intervention. Front Hum Neurosci. 2013;7:72. doi: 10.3389/fnhum.2013.00072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chaddock L, Pontifex MB, Hillman CH, Kramer AF. A review of the relation of aerobic fitness and physical activity to brain structure and function in children. J Int Neuropsychol Soc. 2011;17(6):975–985. doi: 10.1017/S1355617711000567. [DOI] [PubMed] [Google Scholar]
- 12.Colcombe SJ, Kramer AF. Fitness effects on the cognitive function of older adults: a meta-analytic study. Psychol Sci. 2003;14(2):125–130. doi: 10.1111/1467-9280.t01-1-01430. [DOI] [PubMed] [Google Scholar]
- 13.Cottrell LA, Northrup K, Wittberg R. The extended relationship between child cardiovascular risks and academic performance measures. Obesity (Silver Spring) 2007;15(12):3170–3177. doi: 10.1038/oby.2007.377. [DOI] [PubMed] [Google Scholar]
- 14.Crova C, Struzzolino I, Marchetti R, et al. Cognitively challenging physical activity benefits executive function in overweight children. J Sports Sci. 2014;32(3):201–211. doi: 10.1080/02640414.2013.828849. [DOI] [PubMed] [Google Scholar]
- 15.Das JP. A neo-Lurian approach to assessment and remediation. Neuropsychol Rev. 1999;9(2):107–116. doi: 10.1023/a:1025611924842. [DOI] [PubMed] [Google Scholar]
- 16.Datar A, Sturm R, Magnabosco JL. Childhood overweight and academic performance: national study of kindergartners and first-graders. Obes Res. 2004;12(1):58–68. doi: 10.1038/oby.2004.9. [DOI] [PubMed] [Google Scholar]
- 17.Davis CL, Cooper S. Fitness, fatness, cognition, behavior, and academic achievement among overweight children: do cross-sectional associations correspond to exercise trial outcomes? Prev Med. 2011;(52 Suppl 1):S65–S69. doi: 10.1016/j.ypmed.2011.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Davis CL, Tkacz J, Gregoski M, Boyle CA, Lovrekovic G. Aerobic exercise and snoring in overweight children: a randomized controlled trial. Obesity (Silver Spring) 2006;14(11):1985–1991. doi: 10.1038/oby.2006.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Davis CL, Tomporowski PD, McDowell JE, et al. Exercise improves executive function and achievement and alters brain activation in overweight children: a randomized, controlled trial. Health Psychol. 2011;30(1):91–98. doi: 10.1037/a0021766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Diamond A. Executive functions. Annu Rev Psychol. 2013;64:135–168. doi: 10.1146/annurev-psych-113011-143750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Erion JR, Wosiski-Kuhn M, Dey A, et al. Obesity elicits interleukin 1-mediated deficits in hippocampal synaptic plasticity. J Neurosci. 2014;34(7):2618–2631. doi: 10.1523/JNEUROSCI.4200-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Espy KA. The Shape School: Assessing executive function in preschool children. Dev Neuropsychol. 1997;13:495–499. [Google Scholar]
- 23.Etnier JL, Nowell PM, Landers DM, Sibley BA. A meta-regression to examine the relationship between aerobic fitness and cognitive performance. Brain Res Brain Res Rev. 2006;52(1):119–130. doi: 10.1016/j.brainresrev.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 24.Fedewa AL, Ahn S. The effects of physical activity and physical fitness on children’s achievement and cognitive outcomes: a meta-analysis. Res Q Exerc Sport. 2011;82(3):521–535. doi: 10.1080/02701367.2011.10599785. [DOI] [PubMed] [Google Scholar]
- 25.Flegal KM, Ogden CL, Yanovski JA, et al. High adiposity and high body mass index-forage in US children and adolescents overall and by race-ethnic group. Am J Clin Nutr. 2010;91(4):1020–1026. doi: 10.3945/ajcn.2009.28589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Golden CJ, Freshwater SM. A Manual for Clinical and Experimental Uses. Chicago: Stoelting; 1978. Stroop Color and Word Test. [Google Scholar]
- 27.Goldschmidt AB, Wilfley DE, Paluch RA, Roemmich JN, Epstein LH. Indicated prevention of adult obesity: how much weight change is necessary for normalization of weight status in children? JAMA Pediatrics. 2013;167(1):21–26. doi: 10.1001/jamapediatrics.2013.416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gray J, Yeo GS, Cox JJ, et al. Hyperphagia, severe obesity, impaired cognitive function, and hyperactivity associated with functional loss of one copy of the brain-derived neurotrophic factor (BDNF) gene. Diabetes. 2006;55(12):3366–3371. doi: 10.2337/db06-0550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Greene JP, McGee JB, George W. Bush Institute Global Report Card Technical Appendix. Dallas: George W. Bush Institute; 2011. [Google Scholar]
- 30.Greene JP, McGee JB. When the best is mediocre: Developed countries far outperform our most affluent suburbs. Educ Next. 2012;12(1):34–40. [Google Scholar]
- 31.Gunstad J, Spitznagel MB, Paul RH, et al. Body mass index and neuropsychological function in healthy children and adolescents. Appetite. 2008;50(2–3):246–251. doi: 10.1016/j.appet.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 32.Han JC, Liu QR, Jones M, et al. Brain-derived neurotrophic factor and obesity in the WAGR syndrome. N Engl J Med. 2008;359(9):918–927. doi: 10.1056/NEJMoa0801119. 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hillman CH, Erickson KI, Kramer AF. Be smart, exercise your heart: exercise effects on brain and cognition. Nat Rev Neurosci. 2008;9(1):58–65. doi: 10.1038/nrn2298. [DOI] [PubMed] [Google Scholar]
- 34.Hillman CH, Pontifex MB, Castelli DM, et al. Effects of the FITKids randomized controlled trial on executive control and brain function. Pediatrics. 2014;134(4):e1063–e1071. doi: 10.1542/peds.2013-3219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Institute of Medicine. Educating the Student Body: Taking Physical Activity and Physical Education to School. Washington, DC: The National Academies Press; 2013. Available from: http://www.iom.edu/Reports/2013/Educating-the-Student-Body-Taking-Physical-Activity-and-Physical-Education-to-School.aspx. [PubMed] [Google Scholar]
- 36.Janssen I, Leblanc AG. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act. 2010;7:40. doi: 10.1186/1479-5868-7-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kamijo K, Khan NA, Pontifex MB, et al. The relation of adiposity to cognitive control and scholastic achievement in preadolescent children. Obesity (Silver Spring) 2012;20(12):2406–2411. doi: 10.1038/oby.2012.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kamijo K, Pontifex MB, Khan NA, et al. The association of childhood obesity to neuroelectric indices of inhibition. Psychophysiology. 2012;49(10):1361–1371. doi: 10.1111/j.1469-8986.2012.01459.x. [DOI] [PubMed] [Google Scholar]
- 39.Kamijo K, Pontifex MB, Khan NA, et al. The negative association of childhood obesity to cognitive control of action monitoring. Cereb Cortex. 2014;24(3):654–662. doi: 10.1093/cercor/bhs349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Katzmarzyk PT, Malina RM, Song TM, Bouchard C. Physical activity and health-related fitness in youth: a multivariate analysis. Med Sci Sports Exerc. 1998;30(5):709–714. doi: 10.1097/00005768-199805000-00011. [DOI] [PubMed] [Google Scholar]
- 41.Keeley TJH, Fox KR. The impact of physical activity and fitness on academic achievement and cognitive performance in children. Int Rev Sport Exerc Psychol. 2009;2:198–214. [Google Scholar]
- 42.Kohler MJ, Lushington K, van den Heuvel CJ, Martin J, Pamula Y, Kennedy D. Adenotonsillectomy and neurocognitive deficits in children with Sleep Disordered Breathing. PloS One. 2009;4(10):e7343. doi: 10.1371/journal.pone.0007343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Krafft CE, Pierce JE, Schwarz NF, et al. An eight month randomized controlled exercise intervention alters resting state synchrony in overweight children. Neuroscience. 2014;256:445–455. doi: 10.1016/j.neuroscience.2013.09.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Krafft CE, Schaeffer DJ, Schwarz NF, et al. Improved frontoparietal white matter integrity in overweight children is associated with attendance at an after-school exercise program. Dev Neurosci. 2014;36(1):1–9. doi: 10.1159/000356219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lambourne K, Tomporowski P. The effect of exercise-induced arousal on cognitive task performance: a meta-regression analysis. Brain Res. 2010;1341:12–24. doi: 10.1016/j.brainres.2010.03.091. [DOI] [PubMed] [Google Scholar]
- 46.Leckie RL, Oberlin LE, Voss MW, et al. BDNF mediates improvements in executive function following a 1-year exercise intervention. Front Hum Neurosci. 2014;8:985. doi: 10.3389/fnhum.2014.00985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Levin BE. Neurotrophism and energy homeostasis: perfect together. Am J Physiol Regul Integr Comp Physiol. 2007;293(3):R988–R991. doi: 10.1152/ajpregu.00434.2007. [DOI] [PubMed] [Google Scholar]
- 48.Lezak MD, Howieson DB, Loring DW. Neuropsychological Assessment. 4th ed. New York: Oxford University Press; 2004. [Google Scholar]
- 49.Li Y, Dai Q, Jackson JC, Zhang J. Overweight is associated with decreased cognitive functioning among school-age children and adolescents. Obesity. 2008;16(8):1809–1815. doi: 10.1038/oby.2008.296. [DOI] [PubMed] [Google Scholar]
- 50.Malina RM, Bouchard C, Bar-Or O. Growth, maturation, and physical activity. 2nd ed. Champaign, IL: Human Kinetics; 2004. [Google Scholar]
- 51.Naglieri JA. CAS Rapid Score. Centreville, VA: NL Associates; 2002. [Google Scholar]
- 52.Naglieri JA, Das JP. Cognitive Assessment System: Interpretive handbook. Itasca, IL: Riverside Publishing; 1997. [Google Scholar]
- 53.Naglieri JA, Das JP. Planning, Attention, Simultaneous, Successive (PASS) Theory: A Revision of the Concept of Intelligence. In: Flanagan DP, Harrison PL, editors. Contemporary Intellectual Assessment: Theories, Tests, and Issues. New York: Guilford Press; 2005. pp. 120–135. [Google Scholar]
- 54.Ness AR, Leary SD, Mattocks C, et al. Objectively measured physical activity and fat mass in a large cohort of children. PLoS Med. 2007;4(3):476–484. doi: 10.1371/journal.pmed.0040097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ogden CL, Kuczmarski RJ, Flegal KM, et al. Centers for Disease Control and Prevention 2000 growth charts for the United States: Improvements to the 1977 National Center for Health Statistics version. Pediatrics. 2002;109(1):45–60. doi: 10.1542/peds.109.1.45. [DOI] [PubMed] [Google Scholar]
- 56.Peters H, Whincup PH, Cook DG, Law C, Li L. Trends in resting pulse rates in 9–11-year-old children in the UK 1980–2008. Arch Dis Child. 2014;99(1):10–14. doi: 10.1136/archdischild-2013-304699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pillai A, Bruno D, Sarreal AS, et al. Plasma BDNF levels vary in relation to body weight in females. PLoS One. 2012;7(7):e39358. doi: 10.1371/journal.pone.0039358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pontifex MB, Kamijo K, Scudder MR, et al. V. The differential association of adiposity and fitness with cognitive control in preadolescent children. Monogr Soc Res Child Dev. 2014;79(4):72–92. doi: 10.1111/mono.12131. [DOI] [PubMed] [Google Scholar]
- 59.Posner JK, Vandell DL. Low-income children’s after-school care: are there beneficial effects of after-school programs? Child Dev. 1994;65(2 Spec No):440–456. [PubMed] [Google Scholar]
- 60.Reitan RM. Trail making test results for normal and brain-damaged children. Percept Mot Skills. 1971;33(2):575–581. doi: 10.2466/pms.1971.33.2.575. [DOI] [PubMed] [Google Scholar]
- 61.Roth CL, Elfers C, Gebhardt U, Muller HL, Reinehr T. Brain-derived neurotrophic factor and its relation to leptin in obese children before and after weight loss. Metabolism. 2013;62(2):226–234. doi: 10.1016/j.metabol.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 62.Schaeffer DJ, Krafft CE, Schwarz NF, et al. An 8-month exercise intervention alters frontotemporal white matter integrity in overweight children. Psychophysiology. 2014;51(8):728–33. doi: 10.1111/psyp.12227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Shadish WR, Cook TD, Campbell DT. 2nd ed. New York: Houghton Mifflin; 2002. Experimental and Quasi-Experimental Designs for Generalized Causal Inference. [Google Scholar]
- 64.Sibley BA, Etnier JL. The relationship between physical activity and cognition in children: A meta-analysis. Pedi Exerc Sci. 2003;15(3):243–256. [Google Scholar]
- 65.Skinner AC, Skelton JA. Prevalence and trends in obesity and severe obesity among children in the United States, 1999–2012. JAMA Pediatrics. 2014;168(6):561–566. doi: 10.1001/jamapediatrics.2014.21. [DOI] [PubMed] [Google Scholar]
- 66.Suchy Y. Executive functioning: overview, assessment, and research issues for non-neuropsychologists. Ann Behav Med. 2009;37(2):106–116. doi: 10.1007/s12160-009-9097-4. [DOI] [PubMed] [Google Scholar]
- 67.Syväoja HJ, Tammelin TH, Ahonen T, Kankaanpää A, Kantomaa MT. The associations of objectively measured physical activity and sedentary time with cognitive functions in school-aged children. PLoS One. 2014;9(7):e103559. doi: 10.1371/journal.pone.0103559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tomporowski PD, Davis CL, Miller PH, Naglieri J. Exercise and children’s intelligence, cognition, and academic achievement. Educ Psychol Rev. 2008;20(2):111–131. doi: 10.1007/s10648-007-9057-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.van der Niet AG, Hartman E, Smith J, Visscher C. Modeling relationships between physical fitness, executive functioning, and academic achievement in primary school children. Psychol Sport Exerc. 2014;15(4):319–325. [Google Scholar]
- 70.van der Niet AG, Smith J, Scherder EJ, Oosterlaan J, Hartman E, Visscher C. Associations between daily physical activity and executive functioning in primary school-aged children. J Sci Med Sport. 2014 Sep;:18. doi: 10.1016/j.jsams.2014.09.006. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 71.Verburgh L, Konigs M, Scherder EJ, Oosterlaan J. Physical exercise and executive functions in preadolescent children, adolescents and young adults: a meta-analysis. Br J Sports Med. 2014;48(12):973–979. doi: 10.1136/bjsports-2012-091441. [DOI] [PubMed] [Google Scholar]
- 72.Welk GJ, Jackson AW, Morrow JR, Jr, Haskell WH, Meredith MD, Cooper KH. The association of health-related fitness with indicators of academic performance in Texas schools. Res Q Exerc Sport. 2010;81(3 Suppl):S16–S23. doi: 10.1080/02701367.2010.10599690. [DOI] [PubMed] [Google Scholar]