Abstract
BACKGROUND
Cigarette smoking is a risk factor for atrial fibrillation (AF), but whether secondhand smoke (SHS) impacts the risk of AF remains unknown.
OBJECTIVE
To determine if SHS exposure is associated with an increased risk of AF.
METHODS
We performed a cross-sectional analysis of data from participants enrolled in the Health eHeart Study, an internet-based, longitudinal cardiovascular cohort study, who completed baseline SHS exposure and medical conditions questionnaires. SHS was assessed through a validated 22-question survey, and prevalent AF was assessed by self-report, with validation of a subset (n=42) by review of electronic medical records.
RESULTS
Of 4,976 participants, 593 (11.9%) reported having AF. In unadjusted analyses, patients with AF were more likely to have been exposed to SHS in utero, as a child, as an adult, at home, and at work. After multivariable adjustment for potential confounders, having had a smoking parent during gestational development (OR 1.37, 95% CI 1.08–1.73, p=0.009) and residing with a smoker during childhood (OR 1.40, 95% CI 1.10–1.79, p=0.007) were each significantly associated with AF. Both positive associations were more pronounced among patients without risk factors for AF (p values for interaction <0.05).
CONCLUSIONS
SHS exposure during gestational development and during childhood was associated with having AF later in life. This association was even stronger in the absence of established risk factors for AF. Our findings indicate that SHS in early life may be an important, potentially modifiable risk factor for the development of AF.
Keywords: Arrhythmia, atrial fibrillation, epidemiology, lone atrial fibrillation, prevention, risk factors, secondhand smoke
Introduction
Atrial fibrillation (AF) affects millions of Americans and is growing in incidence and prevalence.1 It nearly doubles mortality and is one of the most common causes of stroke.2,3 Though the mechanism of AF remains largely unknown, observational analyses have identified age, male sex, white race, hypertension, heart failure, diabetes, obesity, and alcohol consumption as risk factors for AF.4,5 An emerging risk factor for AF is cigarette smoking, which has been linked to the development of AF in both current and former smokers.6,7
Though no studies have been published examining the effect of secondhand smoke (SHS) on AF, SHS exposure is associated with increased cardiovascular disease and mortality.8 It is estimated that SHS exposure increases nonsmokers’ coronary artery disease (CAD) risk by 25% to 30%,9 and the vast majority of deaths in the United States attributed to SHS are from heart disease.10 Protection from SHS through the implementation of smoke-free legislation is rapidly followed by reductions in hospital admissions for acute myocardial infarctions, stroke, and other cardiac events.11–13 Despite progress in reducing smoking prevalence and the resultant SHS exposure, SHS remains a significant hazard in the U.S. and worldwide.14 Current hypotheses regarding the mechanism by which SHS leads to cardiac disease include induction of an inflammatory state,15 direct effects of nicotine on atrial structural remodeling,16,17 and effects on autonomic function.18,19 Each of these mechanisms has also been implicated in the pathogenesis of AF.4,20
Up to 30% of all AF occurs in patients without any clear risk factors.21 While some “lone AF” patients may have an inherited component, the majority do not,22,23 suggesting that some as yet unknown environmental exposure may be important. Given the increasing burden of AF and the need to identify effective prevention strategies, we examined the possible relationship between SHS exposure and the prevalence of AF, hypothesizing that SHS exposure increases the risk of AF.
Methods
Study Design
We performed a cross-sectional analysis of data obtained between March 8, 2013 (enrollment initiation) and November 13, 2014 from consecutive participants enrolled in the Health eHeart Study. The Health eHeart Study is an internet-based, longitudinal, cardiovascular cohort study.
English-speaking adults worldwide with a working email address were eligible for participation. Participants were recruited from the UCSF cardiology and general medicine clinics, other academic institutions, lay press, social media, and through partnerships with advocacy groups and medical organizations, including the American Heart Association. Upon enrollment, participants were prompted to complete a series of questionnaires grouped into “eVisits.” For eVisit1, participants responded to questions pertaining to basic demographics, family history, medical history, activity and well-being, habits and lifestyle, social demographics, and use of technology.
The Health eHeart Study was approved by the University of California, San Francisco Committee on Human Research and all participants provided informed consent obtained electronically via the internet.
Assessment of Secondhand Smoke Exposure
SHS exposure was assessed through a validated24 22-question survey (Appendix) inquiring about exposure in utero, in childhood, and in adulthood in various environments, such as home, work, and social settings. Elements of the survey were qualitative, assessing the presence of any regular exposure to SHS, while other aspects were quantitative, assessing years and hours per day of exposure in various settings, as well as number of smokers in home environment. The questions chosen are recommended for examining SHS exposure given their documented reliability and previous validation with biomarkers, such as cotinine in the plasma, urine, or cord blood.24
Assessment of Atrial Fibrillation
Prevalent AF was assessed by self-report in the survey of baseline medical conditions included in eVisit 1. Participants were asked “Have you ever been told by a doctor or nurse that you have, or have been treated for, atrial fibrillation (in the past or currently)?” with possible responses being “yes,” “no,” and “don’t know.” Responses of “don’t know” were treated as missing. In order to validate self-report of AF in our cohort, we reviewed the electronic medical records of a subset of our study population. All Health eHeart Study participants who had provided electronic HIPAA consent using a mobile application, either in response to an email campaign or from participation in another sub-study, and who had received care at the University of California, San Francisco (n=42) were included in the validation study. A fourth year medical student and a graduate of the UCSF Advanced Training in Clinical Research program (SD) under the supervision of a board certified cardiac electrophysiologist (GMM) reviewed every physician note, procedure note, 12-lead electrocardiogram report (previously reviewed by a board certified cardiologist), and Holter study (previously reviewed by a board certified cardiologist) in the electronic medical records of these participants. The criteria for diagnosis of AF were physician documentation of the presence or past history of the disease or electrocardiographic (12-lead or Holter) evidence of AF.
Participants who responded “yes” to having AF were then prompted to complete an additional survey regarding AF symptoms, diagnosis, and treatment. Participants were asked “Are you in atrial fibrillation all the time?” Responses of “yes” and “no, it has stopped because of a shock to my heart or because of a medication” were treated as persistent AF. Responses of “no, it comes and goes on its own” were treated as paroxysmal AF. Responses of “don’t know” were treated as missing.
Covariate Ascertainment
Self-identified race was categorized as white, black, Asian/Pacific Islander, Hispanic, or other. Self-identified gender was classified as male or female. Education was described as high school or less, some college, bachelor’s degree, or post-graduate. Smoking status was defined as never, past, or current smoking, with past or current smoking requiring at least 1 cigarette per day or a total of 100 lifetime cigarettes. Years of smoking was defined as total lifetime years of regular cigarette smoking. Number of alcoholic drinks per week currently consumed was obtained through self-report. A history of diabetes mellitus (DM) hypertension (HTN), CAD, and congestive heart failure (CHF) was ascertained from the medical conditions survey. CAD was also defined by a history of angina or myocardial infarction.
Statistical Analysis
Continuous variables with a normal distribution are presented as means ± standard deviations and were compared using t-tests. Non-normally distributed continuous variables were presented as medians with interquartile ranges and were compared using the Wilcoxon rank- sum test. The associations between categorical variables were determined using chi-square tests.
Logistic regression was used to examine the relationships between individual SHS exposure variables and prevalent AF. The two SHS exposure questions where participants answered “yes,” “no,” or “don’t know” were dichotomized, with “don’t know” classified as no exposure in order to err on the side of specificity. A sensitivity analysis was performed wherein participants that answered “don’t know” were excluded, and no meaningful differences were noted. The question pertaining to in utero exposure was dichotomized so that having a mother, father, or both parents who smoked during a participant’s gestation was classified as having experienced exposure. In additional analyses, effects specific to maternal (combining “mother” and “both” as affirmative) and paternal (combining “father” and “both” as affirmative) smoking in utero were also analyzed. Categorical questions regarding the frequency of SHS exposure outside the home or work place in the past year were dichotomized into exposed versus unexposed. Categorical questions regarding the frequency of irritation of the eyes or throat from smoke were also dichotomized into yes or no responses. Numerical data, such as hours or days of exposure, were treated as continuous measures. The outcome of prevalent AF was dichotomized as yes or no, with answers of “don’t know” treated as missing (n=91, 1.8%).
Associations between AF and SHS responses with unadjusted p values < 0.10 using logistic regression were selected for multivariable analysis. Based on previous literature and biological plausibility, the following covariates were included in these multivariable models: baseline age, sex, race, smoking status (never/past/current), years of smoking, number of alcoholic beverages per week, DM, HTN, history of MI, CAD, and CHF.
The primary outcome was any AF. Additional analyses were performed to assess paroxysmal and persistent AF as outcomes. In order to examine effects specific to AF patients without cardiovascular comorbidities, a secondary outcome was “lone AF.” Lone AF was defined as AF in individuals <60 years of age without baseline diabetes mellitus, hypertension, coronary artery disease, or congestive heart failure. To assess differential effects of SHS on lone AF and other AF, the interaction between the presence of at least one cardiovascular risk factor (versus none) and SHS on the presence of AF was tested.
Data were analyzed using Stata 13 (StataCorp, College Station, TX, USA). A two-tailed p<0.05 was considered statistically significant.
Results
At the time of this analysis, there were 6,863 participants enrolled in the study, of whom 4,976 had completed the baseline SHS exposure and medical conditions questionnaires. Of these participants, 593 (11.9%) reported having AF, of whom 271 (45.7%) reported persistent AF and 275 (46.4%) reported paroxysmal AF. Of the 42 Health eHeart participants with medical records at UCSF who provided electronic HIPAA consent, 25 indicated having AF. Of those, 100% had AF documented by a physician in their electronic medical record (sensitivity of 100%, exact 95% CI 86%–100%), and none of the 17 without self-reported AF had any record of AF (specificity 100%, exact 95% CI 80%–100%). Participants with AF were on average more likely to be older, male, white, past smokers, have longer smoking histories, and have a history of DM, HTN, CAD, and CHF (Table 1).
Table 1.
Baseline Characteristics of Health eHeart Study Participants by Prevalent Atrial Fibrillation
| Atrial Fibrillation (n=593) | No Atrial Fibrillation (n=4,383) | P Value | |
|---|---|---|---|
| Mean Age (years) | 62.3 + 11.4 | 49.1 + 15.1 | <0.001 |
| Male | 324 (54.64%) | 1,904 (43.34%) | <0.001 |
| Race/Ethnicity | |||
| White | 534 (90.1%) | 3,487 (79.6%) | <0.001 |
| Black | 8 (1.4%) | 95 (2.2%) | |
| Asian/Pacific Islander | 19 (3.2%) | 335 (7.6%) | |
| Hispanic | 17 (2.9%) | 266 (6.1%) | |
| Other/Multiple | 15 (2.5%) | 200 (4.6%) | |
| Education | |||
| High School or Less | 33 (6.1%) | 174 (4.2%) | 0.052 |
| Some College | 98 (18.2%) | 678 (16.4%) | |
| Bachelor’s Degree | 180 (33.3%) | 1,326 (32.0%) | |
| Post-Graduate | 229 (42.4%) | 1,967 (47.5%) | |
| Smoking Status | |||
| Never Smoker | 308 (52.7%) | 2,909 (66.5%) | <0.001 |
| Past Smoker | 255 (43.6%) | 1,288 (29.5%) | |
| Current Smoker | 22 (3.8%) | 176 (4.0%) | |
| Median Total Years Smoked Among Past & Current Smokers (IQR) | 18 (9–29) | 12 (6–23) | <0.001 |
| Median Number of Alcoholic Drinks per Week (IQR) | 4 (1–9) | 4 (1–7) | 0.295 |
| Diabetes Mellitus | 60 (10.1%) | 273 (6.3%) | <0.001 |
| Hypertension | 307 (52.2%) | 1,443 (33.1%) | <0.001 |
| Coronary Artery Disease | 149 (25.2%) | 547 (12.5%) | <0.001 |
| Congestive Heart Failure | 94 (16.0%) | 136 (3.1%) | <0.001 |
IQR denotes interquartile range.
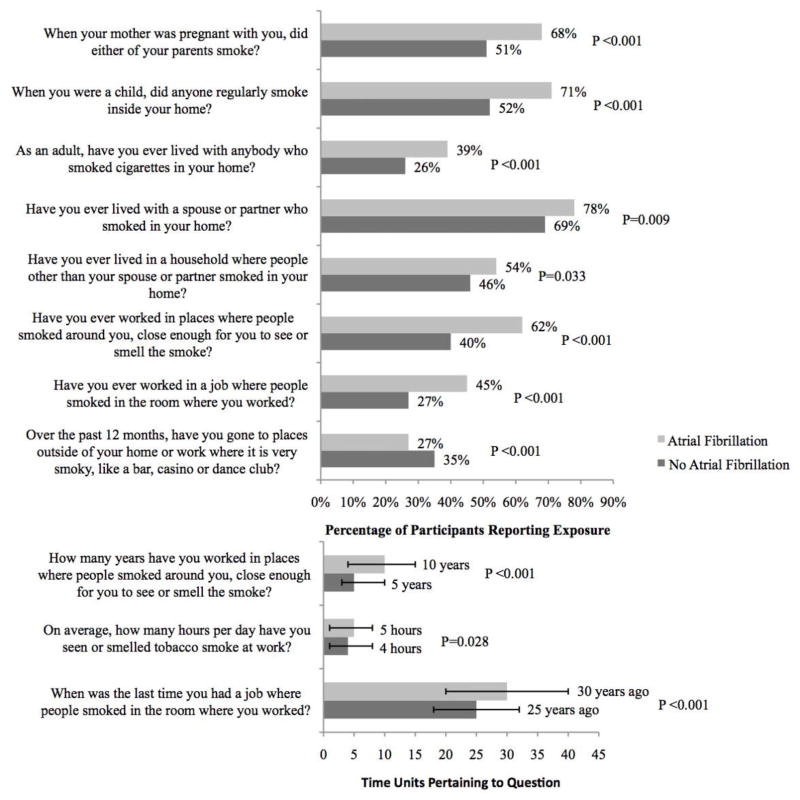
In unadjusted analyses, participants with AF were more likely to have been exposed to SHS in utero, as a child, as an adult, at home and at work, and to have been exposed for a longer period of time at work. However, those without AF were more likely to have visited social environments with significant SHS (Figure 1). When in utero exposure was separated by parent, both having a mother or a father that smoked during that time were each associated with AF (50% of those with AF exposed to maternal smoke compared to 32% of those without AF, p<0.001; 66% of those with AF exposed to paternal smoke compared to 48% of those without AF, p<0.001).
Figure 1.
Summary of secondhand smoke exposures in those with and without atrial fibrillation. Values are reported as percentages for yes/no questions and medians for numeric responses. Y error bars denote interquartile ranges. Questions are limited to a priori selected criteria (see text).
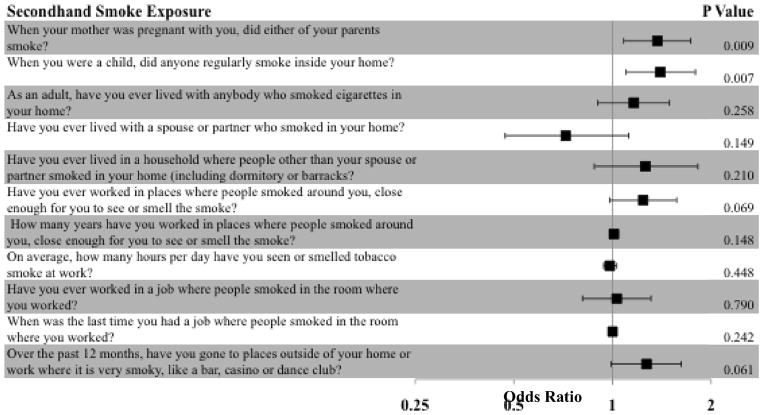
After multivariable adjustment for potential confounders, having had a smoking parent during gestational development (OR 1.37, 95% CI 1.08–1.73, p=0.009) and residing with a smoker during childhood (OR 1.40, 95% CI 1.10–1.79, p=0.007) were each significantly associated with AF (Figure 2). The results were similar when in utero SHS exposure from the mother (OR 1.39, 95% CI 1.00–1.74, p=0.052) or from the father (OR 1.39, 95% CI 1.09–1.76, p=0.008) as compared to having had no smoking parents were analyzed separately. Additionally, adjusting for education did not meaningfully affect our results.
Figure 2.
Odds ratios for atrial fibrillation by secondhand smoke exposure. The odds ratios for atrial fibrillation (black square) after adjusting for age, sex, race, smoking status, years of smoking, alcohol consumption, diabetes, hypertension, coronary artery disease, and congestive heart failure. Y error bars denote 95% confidence intervals.
When examining persistent AF and paroxysmal AF as separate outcomes, we found that in utero exposure and childhood exposure were each significantly associated with persistent AF before and after adjustment (adjusted OR 1.43, 95% CI 1.01–2.01, p=0.042 and adjusted OR 1.46, 95% CI 1.02–2.07, p=0.036 respectively). In utero and childhood SHS exposure were each significantly associated with paroxysmal AF in unadjusted analyses; however, these associations lost significance after adjustment (OR 1.29, 95% CI 0.94–1.78, p=0.114; OR 1.29, 95% CI 0.93–1.79, p=0.128).
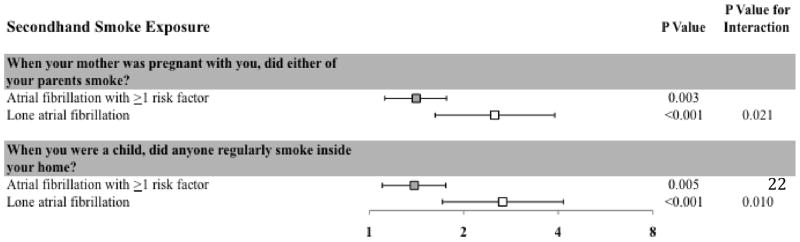
We performed interaction analyses to determine whether the presence or absence of at least one risk factor for AF (including age >60, DM, HTN, CAD, and CHF) modified the relationship between SHS and AF. This analysis showed that both gestational and childhood exposure were more strongly associated with AF (p values for interaction of 0.021 and 0.010 respectively) in the absence of known AF risk factors (Figure 3). Again, these results were similar, with stronger effects observed in the absence of known AF risk factors, when in utero SHS exposure from the mother or from the father were analyzed separately (p values for interaction of 0.035 and 0.043 respectively).
Figure 3.
Odds ratios for atrial fibrillation stratified by the presence of cardiovascular risk factors. The adjusted odds ratios for the associations between secondhand smoke and atrial fibrillation, stratified by the presence (grey square) or absence (white square) of at least one of the following risk factors: age >60, diabetes mellitus (DM), hypertension (HTN), coronary artery disease (CAD), or congestive heart failure (CHF). Odds ratios are adjusted for age, sex, race, smoking status, years of smoking, alcohol consumption, DM, HTN, CAD, and CHF. Y error bars denote 95% confidence intervals.
Discussion
We found that SHS, particularly when present during development and early childhood, was statistically significantly associated with the presence of AF. This relationship was particularly strong in the absence of known AF risk factors, suggesting a direct connection between SHS in early life and AF pathophysiology.
Past research on tobacco and AF has focused on the effects of active smoking, providing the foundation for the hypothesis tested in the current study. The Rotterdam Study, a population-based cohort of older adults, was the first to demonstrate an association between past and current cigarette smoking and an increased risk of AF.7 Later research from the Atherosclerosis Risk in Communities study found that, among more than 15,000 participants, current smokers demonstrated almost 2 times the risk of AF as compared to never smokers.6 Past smokers also had an increased risk of AF, albeit lower than those who continued to smoke. Furthermore, the cumulative amount of smoking in cigarette-years was correlated with an increased risk of developing AF.
Though current research into the mechanism of the effect of SHS on AF is lacking, theories abound as to how SHS may predispose individuals to arrhythmias. Nicotine itself has been linked to cardiac arrhythmias,17 including AF,25 and several canine16 and human studies26 have demonstrated that nicotine leads to atrial fibrosis and atrial structural remodeling, processes known to promote AF.4,27 In addition, SHS may lead to autonomic dysfunction,19 thereby potentially predisposing to cardiac arrhythmias.18 Exactly how such early exposure to SHS may influence the propensity to develop AF later in life remains unknown.
While SHS itself may lead to risk factors for AF, such as ischemic heart disease, this did not appear to be the underlying mechanism for the increased risk of AF observed with prior SHS exposure, given that we adjusted for CAD. Our findings that gestational and early life SHS exposure possibly increase one’s risk of lone AF are particularly interesting given the hypothesized alternate mechanism underlying lone AF. Though our point estimates favored an effect of early life SHS on both persistent and paroxysmal AF, they indicate that our findings may be driven more by persistent AF. This may suggest that the effects of SHS involve the substrate of the atria more so than intermittent triggers of the arrhythmia. Overall our results indicate that SHS exposure during these critical periods may double one’s odds of having AF as an adult, in the absence of any of the known cardiac risk factors for AF. Given that anywhere between 11 and 30% of AF patients have none of the traditional risk factors21,28 and therefore cannot be helped by preventive therapies such as reducing blood pressure or preventing heart failure, this is a population that may benefit the most by the identification of novel modifiable risk factors. In addition, lone AF can be viewed in many ways as “pure AF”-developing in the absence of any existing heart disease- and may serve as a window into understanding processes that are specific to atrial pathophysiology.
Despite advances in the prevention of cardiovascular disease, we still have no primary prevention strategies for AF, the most common arrhythmia.29 Furthermore, our treatments for AF do not address the root cause of the disease but rather attempt to minimize the cardiac and thromboembolic sequelae. It appears that the most straightforward approach to prevention would be lifestyle modification if habits and behaviors that predispose one to AF could be identified. While risk factors thus far have focused on the individual potentially destined to future AF, this research suggests that parental behaviors may also be important. Indeed, these new findings may serve as extra motivation for smoking parents to quit, as it demonstrates that their behaviors could have significant effects on their adult offspring. Our discovery is in line with a growing body of evidence indicating that fetal and childhood exposure to parental smoking may produce long-term cardiovascular aberrations in exposed progeny, even when assessed in adulthood.30,31 A recent study found that childhood exposure to SHS, assessed by parental self-report and serum cotinine levels, was associated with an increased risk of developing carotid atherosclerotic plaque in adulthood.32
Several limitations of our study must be acknowledged. Specifically, due to the cross-sectional nature of the study design, we were able to investigate prevalent but not incident AF and cannot attribute causality to SHS exposure. However, since early life SHS exposure likely preceded the development of any AF, there is temporality inherent to the relationship. In addition, residual confounding is always a concern in observational studies. Though we adjusted for all potential confounders available to us, certain possible confounding variables, such as obesity, were unavailable. Residual confounding due to cigarette smoking is a possibility. While we adjusted for smoking status classified as never, past, or current and for number of years of smoking, data regarding the number of pack years was not available. Another concern is the use of self-report for SHS exposure. Questionnaires remain the most common method of assessing SHS exposure and have been validated as an accurate measure of SHS exposure using biomarkers.24 Studies have shown that adults are able to produce reliable, accurate responses regarding their exposures during adulthood and childhood, including whether either parent smoked during the mother’s pregnancy.33 Nonetheless, the survey has not been validated against direct measures of in utero exposure. Another important limitation of the survey is that it did not assess quantitative, only qualitative, exposure in utero and in childhood and does not further characterize the time frame or duration of the exposure. Although recall bias may be present if those with AF attribute their disease to prior exposures, this was unlikely operative here as participants had no knowledge of how the SHS exposure information would be studied. Using self-report to assess AF is a limitation and may lead to some misclassification of our outcome. We do not believe misclassification of the outcome should differ according to SHS exposure and should therefore also bias our results towards the null (i.e. it would be expected to result in false negative and not false positive results). It is possible that early exposure to SHS is associated with an increase in medical illnesses in general and therefore an increase in the frequency of physician visits, leading to higher rates of AF detection in the exposed group. However, given the significant interaction with lone AF (a stronger association among those with fewer cardiovascular comorbidities), it would appear that other illnesses are not driving this association. Furthermore, while the UCSF cohort used to validate our measure of self-reported AF may not be representative of the whole cohort, all participants with available medical record data accurately reported the presence or absence of AF. While only a small fraction of our participants had electronic medical record data available (0.6%), the lower end of the 95% confidence intervals demonstrate robustly high sensitivities and specificities even in the “worst case scenario.” Another limitation to our AF ascertainment is the inability to assess AF burden. As we examined the responses to multiple SHS-related questions, the possibility of false positive results arises due to multiple comparisons. To mitigate these effects, we utilized a priori criteria to determine which questions to examine in multivariable analyses. The associations between SHS-related responses and AF were nearly all in the same direction, a consistency that makes false positive results based on multiple comparisons unlikely. Finally, the Health eHeart Study sample is less racially and ethnically diverse and of a higher socioeconomic status than the U.S. population, so care must be taken in applying these results to other populations with different characteristics. However, this lack of generalizability should not affect the internal validity of our findings.
Conclusions
In our study of nearly 5,000 Health eHeart participants, SHS exposure during gestational development and during childhood were both associated with having AF later in life. Furthermore, this association was even stronger in the absence of established risk factors for AF. These findings indicate that SHS may be an important, potentially modifiable risk factor for the development of AF, operating outside of known mechanisms for the arrhythmia. Finally, this research suggests that parental behaviors may be critical in the future development of this disease in offspring. Further research into the mechanism underlying this relationship is needed.
Supplementary Material
Clinical Perspectives.
Our study is the first to report the effects of secondhand smoke (SHS) on atrial fibrillation (AF) and more generally, the first description of an influence of parental behavior on AF risk. We found that SHS exposure during gestational development and during childhood were each associated with having AF later in life, adding to previous literature linking early exposure to parental smoking with future cardiovascular disease. Significantly, the association between SHS and AF was even stronger in the absence of traditional risk factors—in “lone” AF. This finding could potentially shed light on AF pathophysiology outside of known mechanisms.
Given that there are no primary prevention strategies for AF, the discovery of modifiable risk factors is important. We hope that these findings will encourage future research into the effects of SHS, which may reveal novel mechanisms underlying AF and consequently new therapeutic targets. Furthermore, despite significant decreases in the prevalence of smoking, tobacco use remains a significant obstacle to health in the U.S. and worldwide. We hope to contribute additional reasons to counsel patients to abstain from cigarette smoking and to protect their families from SHS.
Acknowledgments
This research was made possible in part by the Clinical and Translational Research Fellowship Program (CTRFP), a program of UCSF’s Clinical and Translational Science Institute (CTSI) that is sponsored in part by the National Center for Advancing Translational Sciences, National Institutes of Health, through UCSF-CTSI Grant Number TL1 TR000144 and the Doris Duke Charitable Foundation (DDCF).
ABBREVIATIONS
- AF
atrial fibrillation
- CAD
coronary artery disease
- CHF
congestive heart failure
- DM
diabetes mellitus
- HTN
hypertension
- SHS
secondhand smoke
Footnotes
The contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH, UCSF or the DDCF.
Conflicts of interest: Dr. Marcus has received research support from the NIH, PCORI, SentreHeart, Medtronic and Pfizer and is a consultant for and holds equity in InCarda.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Naccarelli GV, Varker H, Lin J, Schulman KL. Increasing prevalence of atrial fibrillation and flutter in the United States. The American journal of cardiology. 2009;104:1534–9. doi: 10.1016/j.amjcard.2009.07.022. [DOI] [PubMed] [Google Scholar]
- 2.Fuster V, Ryden LE, Cannom DS, et al. ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Circulation. 2006;114:e257–354. doi: 10.1161/CIRCULATIONAHA.106.177292. [DOI] [PubMed] [Google Scholar]
- 3.Chugh SS, Blackshear JL, Shen WK, Hammill SC, Gersh BJ. Epidemiology and natural history of atrial fibrillation: clinical implications. Journal of the American College of Cardiology. 2001;37:371–8. doi: 10.1016/s0735-1097(00)01107-4. [DOI] [PubMed] [Google Scholar]
- 4.Andrade J, Khairy P, Dobrev D, Nattel S. The clinical profile and pathophysiology of atrial fibrillation: relationships among clinical features, epidemiology, and mechanisms. Circulation research. 2014;114:1453–68. doi: 10.1161/CIRCRESAHA.114.303211. [DOI] [PubMed] [Google Scholar]
- 5.Dewland TA, Olgin JE, Vittinghoff E, Marcus GM. Incident atrial fibrillation among Asians, Hispanics, blacks, and whites. Circulation. 2013;128:2470–7. doi: 10.1161/CIRCULATIONAHA.113.002449. [DOI] [PubMed] [Google Scholar]
- 6.Chamberlain AM, Agarwal SK, Folsom AR, et al. Smoking and incidence of atrial fibrillation: results from the Atherosclerosis Risk in Communities (ARIC) study. Heart rhythm : the official journal of the Heart Rhythm Society. 2011;8:1160–6. doi: 10.1016/j.hrthm.2011.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Heeringa J, Kors JA, Hofman A, van Rooij FJ, Witteman JC. Cigarette smoking and risk of atrial fibrillation: the Rotterdam Study. American heart journal. 2008;156:1163–9. doi: 10.1016/j.ahj.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 8.Wells AJ. Passive smoking as a cause of heart disease. Journal of the American College of Cardiology. 1994;24:546–54. doi: 10.1016/0735-1097(94)90315-8. [DOI] [PubMed] [Google Scholar]
- 9.Committee on Secondhand Smoke Exposure and Acute Coronary Events IoM. Secondhand Smoke Exposure and Cardiovascular Effects: Making Sense of the Evidence. National Academy of Sciences; Washington, DC: 2009. [Google Scholar]
- 10.Prochaska JJ, Benowitz NL, Glantz SA, Hudmon KS, Grossman W. Cardiology Rx for Change: improving clinical attention to tobacco use and secondhand smoke exposure in cardiology. Clinical cardiology. 2011;34:738–43. doi: 10.1002/clc.20982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lightwood JM, Glantz SA. Declines in acute myocardial infarction after smoke-free laws and individual risk attributable to secondhand smoke. Circulation. 2009;120:1373–9. doi: 10.1161/CIRCULATIONAHA.109.870691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Meyers DG, Neuberger JS, He J. Cardiovascular effect of bans on smoking in public places: a systematic review and meta-analysis. Journal of the American College of Cardiology. 2009;54:1249–55. doi: 10.1016/j.jacc.2009.07.022. [DOI] [PubMed] [Google Scholar]
- 13.Tan CE, Glantz SA. Association between smoke-free legislation and hospitalizations for cardiac, cerebrovascular, and respiratory diseases: a meta-analysis. Circulation. 2012;126:2177–83. doi: 10.1161/CIRCULATIONAHA.112.121301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Veeranki SP, Mamudu HM, Zheng S, et al. Secondhand smoke exposure among never-smoking youth in 168 countries. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2015;56:167–73. doi: 10.1016/j.jadohealth.2014.09.014. [DOI] [PubMed] [Google Scholar]
- 15.Barnoya J, Glantz SA. Cardiovascular effects of secondhand smoke: nearly as large as smoking. Circulation. 2005;111:2684–98. doi: 10.1161/CIRCULATIONAHA.104.492215. [DOI] [PubMed] [Google Scholar]
- 16.Shan H, Zhang Y, Lu Y, et al. Downregulation of miR-133 and miR-590 contributes to nicotine-induced atrial remodelling in canines. Cardiovascular research. 2009;83:465–72. doi: 10.1093/cvr/cvp130. [DOI] [PubMed] [Google Scholar]
- 17.D’Alessandro A, Boeckelmann I, Hammwhoner M, Goette A. Nicotine, cigarette smoking and cardiac arrhythmia: an overview. European journal of preventive cardiology. 2012;19:297–305. doi: 10.1177/1741826711411738. [DOI] [PubMed] [Google Scholar]
- 18.Pope CA, 3rd, Eatough DJ, Gold DR, et al. Acute exposure to environmental tobacco smoke and heart rate variability. Environmental health perspectives. 2001;109:711–6. doi: 10.1289/ehp.01109711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Felber Dietrich D, Schwartz J, Schindler C, et al. Effects of passive smoking on heart rate variability, heart rate and blood pressure: an observational study. International journal of epidemiology. 2007;36:834–40. doi: 10.1093/ije/dym031. [DOI] [PubMed] [Google Scholar]
- 20.Smit MD, Maass AH, De Jong AM, Muller Kobold AC, Van Veldhuisen DJ, Van Gelder IC. Role of inflammation in early atrial fibrillation recurrence. Europace : European pacing, arrhythmias, and cardiac electrophysiology : journal of the working groups on cardiac pacing, arrhythmias, and cardiac cellular electrophysiology of the European Society of Cardiology. 2012;14:810–7. doi: 10.1093/europace/eur402. [DOI] [PubMed] [Google Scholar]
- 21.Wyse DG, Van Gelder IC, Ellinor PT, et al. Lone atrial fibrillation: does it exist? Journal of the American College of Cardiology. 2014;63:1715–23. doi: 10.1016/j.jacc.2014.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Marcus GM, Smith LM, Vittinghoff E, et al. A first-degree family history in lone atrial fibrillation patients. Heart rhythm : the official journal of the Heart Rhythm Society. 2008;5:826–30. doi: 10.1016/j.hrthm.2008.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ellinor PT, Lunetta KL, Glazer NL, et al. Common variants in KCNN3 are associated with lone atrial fibrillation. Nature genetics. 2010;42:240–4. doi: 10.1038/ng.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Avila-Tang E, Elf JL, Cummings KM, et al. Assessing secondhand smoke exposure with reported measures. Tobacco control. 2013;22:156–63. doi: 10.1136/tobaccocontrol-2011-050296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Choragudi NL, Aronow WS, DeLuca AJ. Nicotine gum-induced atrial fibrillation. Heart disease. 2003;5:100–1. doi: 10.1097/01.hdx.0000061700.11321.1a. [DOI] [PubMed] [Google Scholar]
- 26.Goette A, Lendeckel U, Kuchenbecker A, et al. Cigarette smoking induces atrial fibrosis in humans via nicotine. Heart (British Cardiac Society) 2007;93:1056–63. doi: 10.1136/hrt.2005.087171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goette A, Juenemann G, Peters B, et al. Determinants and consequences of atrial fibrosis in patients undergoing open heart surgery. Cardiovascular research. 2002;54:390–6. doi: 10.1016/s0008-6363(02)00251-1. [DOI] [PubMed] [Google Scholar]
- 28.Brand FN, Abbott RD, Kannel WB, Wolf PA. Characteristics and prognosis of lone atrial fibrillation. 30-year follow-up in the Framingham Study. JAMA : the journal of the American Medical Association. 1985;254:3449–53. [PubMed] [Google Scholar]
- 29.Marcus GM. Predicting incident atrial fibrillation: an important step toward primary prevention. Archives of internal medicine. 2010;170:1874–5. doi: 10.1001/archinternmed.2010.426. [DOI] [PubMed] [Google Scholar]
- 30.Geerts CC, Bots ML, Grobbee DE, Uiterwaal CS. Parental smoking and vascular damage in young adult offspring: is early life exposure critical? The atherosclerosis risk in young adults study. Arteriosclerosis, thrombosis, and vascular biology. 2008;28:2296–302. doi: 10.1161/ATVBAHA.108.173229. [DOI] [PubMed] [Google Scholar]
- 31.Geerts CC, Bots ML, van der Ent CK, Grobbee DE, Uiterwaal CS. Parental smoking and vascular damage in their 5-year-old children. Pediatrics. 2012;129:45–54. doi: 10.1542/peds.2011-0249. [DOI] [PubMed] [Google Scholar]
- 32.West HW, Juonala M, Gall SL, et al. Exposure to Parental Smoking in Childhood is Associated with Increased Risk of Carotid Atherosclerotic Plaque in Adulthood: The Cardiovascular Risk in Young Finns Study. Circulation. 2015 doi: 10.1161/CIRCULATIONAHA.114.013485. [DOI] [PubMed] [Google Scholar]
- 33.Coultas DB, Peake GT, Samet JM. Questionnaire assessment of lifetime and recent exposure to environmental tobacco smoke. American journal of epidemiology. 1989;130:338–47. doi: 10.1093/oxfordjournals.aje.a115340. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.