Introduction
Prostate cancer (PCa) is the most common non-cutaneous malignancy in men.1 Although a large proportion of patients diagnosed with PCa will be cured by definitive local therapy (i.e. radical prostatectomy or radiation therapy), many will go on to develop metastatic disease. The sensitive detection of metastatic sites is of critical importance, as there is growing evidence that patients with a limited number of disease foci may benefit from directed treatment such as stereotactic ablative radiation.2–4
Bony metastases from PCa are most often imaged with planar whole body bone scan utilizing the radiotracer 99mTc-methylene diphosphonate (99mTc-MDP). Efforts at improving the sensitivity and specificity of this modality have included the introduction of single-photon emission computed tomography (SPECT) alone or in combination with X-ray computed tomography (SPECT/CT), which provides tomographic images with enhanced anatomic localization and lesion characterization.5–7 Further, the improved spatial resolution and intrinsic ability to quantify findings on positron emission tomography (PET) has also come to the forefront of imaging bone metastases in the form of Na18F PET/CT, which has been found to improve both sensitivity and specificity for the evaluation of bone metastases relative to 99mTc-MDP bone scan.8–10
An alternative to 99mTc-MDP and Na18F is 18F-DCFPyL, a small molecule inhibitor of prostate specific membrane antigen (PSMA) that has been shown to have high uptake at sites of metastases in patients with advanced PCa.11 A single case report with a similar PSMA-targeted agent noted correlation between Na18F PET/CT and the PSMA ligand prior to therapy with 223Ra.12 In this report, we compare the sensitivity of 99mTc-MDP bone scan, Na18F PET/CT and 18F-DCFPyL PET/CT for detecting sites of osseous metastases in a single patient with progressive castration resistant PCa.
Case Report
The patient is a 45-year-old gentleman who had first presented approximately two years prior to the time of PET imaging with an elevated prostate-specific antigen (PSA) level of 39 ng/mL and suspected clinically localized PCa. Transrectal biopsy demonstrated PCa in every core up to Gleason 5+4=9. As the patient had no definitive evidence of metastasis on conventional imaging, he proceeded to undergo a radical retropubic prostatectomy, demonstrating extraprostatic extension, seminal vesicle invasion and positive bilateral pelvic lymph nodes. Post-prostatectomy his PSA was 10.5 ng/mL and he subsequently received treatment with leuprolide and docetaxel, resulting in PSA response to 1.0 ng/mL. The patient then enrolled in a series of clinical trials and received, in succession, Sipuleucel-T, anti-PD-L1 therapy, and enzalutamide, with persistent elevations in PSA as high as 15.6 ng/mL but decreasing to 1.0 ng/mL on enzalutamide. At this point in his treatment course, the patient was imaged with whole-body planar 99mTc-MDP bone scan, Na18F PET/CT, and 18F-DCFPyL PET/CT. Imaging with 18F-DCFPyL PET/CT was done after Institutional Review Board approval under the auspices of an exploratory investigational new drug application (eIND #121064). The imaging protocol used for whole body imaging with 18F-DCFPyL PET/CT has been previously described.13
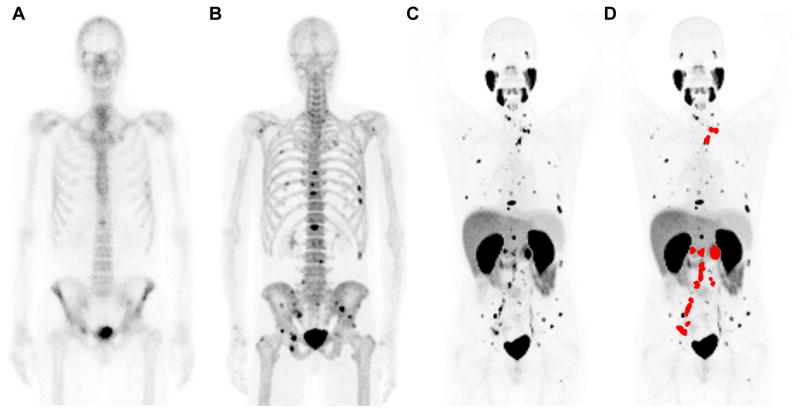
Figure 1 includes an anterior projection whole body 99mTc-MDP bone scan image, an anterior maximum intensity projection (MIP) image from the Na18F PET scan, and an anterior MIP from the 18F-DCFPyL PET scan. For 99mTc-MDP and Na18F, the normal biodistribution is predominantly bone, with some uptake and excretion within the kidneys and bladder. For 18F-DCFPyL, the normal biodistribution includes the lacrimal glands, salivary glands, liver, spleen, proximal small bowel, kidneys, and bladder. Unlike the other two modalities, the 18F-DCFPyL scan demonstrates uptake in lymph nodes as well as bone lesions; the sites of abnormal radiotracer uptake within lymph nodes have been color-coded red in part (D) so as to emphasize the comparable lesions in bone, which remain black.
Figure 1.
(A) Anterior projection whole body planar 99mTc-MDP bone scan, (B) anterior view of the MIP from the Na18F PET, (C) anterior view of the MIP from the 18F-DCFPyL PET, and (D) anterior view of the MIP from the 18F-DCFPyL PET with sites of abnormal radiotracer uptake within lymph nodes masked with a red overlay. Note the increasing number of visible lesions with Na18F PET relative to 99mTc-MDP bone scan and with 18F-DCFPyL PET relative to either of the other two modalities.
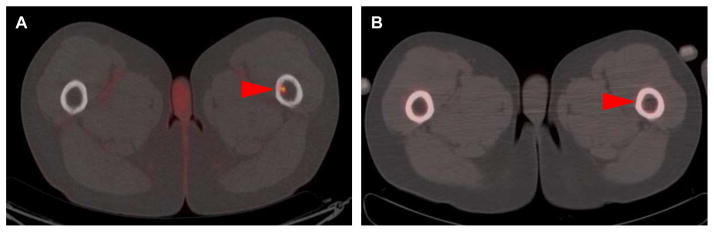
All three imaging studies were centrally reviewed by experienced nuclear medicine readers (SPR and MSJ) and a consensus was reached as to sites of abnormal uptake suspicious for osseous metastatic disease. In all, 89 bone lesions were identified on at least one modality. Planar 99mTc-MDP bone scan revealed 12 suspicious sites, Na18F demonstrated 39 suspicious sites, and 18F-DCFPyL was notable for 87 suspicious sites of abnormal radiotracer uptake within the bones. Assuming all 89 lesions to be true positive would yield a sensitivity of 13.5% for bone scan, 43.8% for Na18F PET/CT and 97.7% for 18F-DCFPyL PET/CT. Lesions that were occult on 99mTc-MDP bone scan and Na18F PET/CT but were apparent with 18F-DCFPyL included lesions entirely within the marrow cavity of the affected bone (Figure 2) as well as subtle sites of abnormal cortical-based uptake (Figure 3).
Figure 2.
(A) Axial fused 18F-DCFPyL PET/CT and (B) axial fused Na18F PET/CT images through the proximal thighs demonstrating a lesion with intense 18F-DCFPyL uptake in the marrow space of the left femur that is occult with Na18F (red arrowheads).
Figure 3.
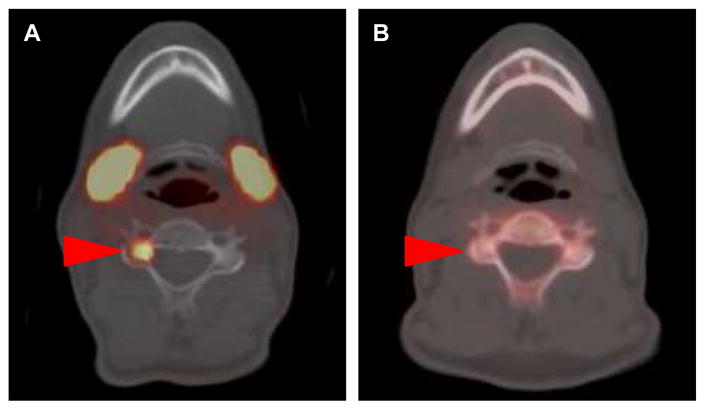
(A) Axial fused 18F-DCFPyL PET/CT and (B) axial fused Na18F PET/CT images through the C5 level of the cervical spine with a lesion in the right lateral mass that is clearly visible with 18F-DCFPyL but demonstrates no uptake on the Na18F scan (red arrowheads).
Discussion
We directly compared 99mTc-MDP bone scan and Na18F PET/CT to an 18F-labeled PSMA-targeted PET radiotracer for the detection of bone lesions in metastatic PCa. The sensitivity for bone lesions with 18F-DCFPyL appears to be markedly higher than the sensitivity of these traditional bone imaging modalities. This preliminary observation may be a result of the difference in the biological mechanism of the radiotracers—whereas 99mTc-MDP and Na18F localize on the basis of bony reaction in response to the presence of metastatic disease, 18F-DCFPyL binds directly to tumor cells. Thus, early lesions or those centered within the marrow cavity, which have not caused a bony reaction may only be visible with 18F-DCFPyL PET/CT. This apparent improved sensitivity is particularly important in regards to the comparison with Na18F PET/CT, which is considered by many to be the standard for diagnosing osseous metastatic disease and has demonstrated an ability to profoundly impact the management of PCa patients.10 If these findings can be confirmed in a larger patient cohort, the approach to imaging PC patients with suspected metastatic disease to the bone will need to be re-thought. A previous report with a similar agent also suggested at least similar sensitivity between Na18F PET/CT and PSMA-targeted PET/CT.12
An obvious limitation of this work is that histopathologic proof of the bone lesions identified on any of the modalities is lacking and was beyond the scope of this observational report. Larger, prospective studies comparing 99mTc-MDP bone scan, Na18F PET/CT and 18F-DCFPyL PET/CT with clinical and imaging follow-up are needed to definitively assess if PSMA-targeted 18F-DCFPyL PET/CT truly has enhanced sensitivity for bone metastases.
Conclusions
The results from this case report are highly encouraging that PSMA-targeted PET/CT with small molecules such as 18F-DCFPyL may offer improved sensitivity for the detection of early/subtle bone metastatic disease relative to either 99mTc-MDP bone scan or Na18F PET/CT. These findings warrant confirmation in a larger study.
Clinical Practice Points.
Imaging of bone metastases in prostate cancer has traditionally involved planar 99mTc-MDP bone scan with or without the use of supplemental tomographic imaging. More recently, Na18F PET/CT has been found to have improved sensitivity and specificity for sites of osseous metastatic involvement.
PSMA is a cell surface enzyme that is highly expressed in prostate cancer and has been explored as a target for prostate cancer imaging.
In this case report, we found that PSMA-based PET/CT with the small molecule 18F-DCFPyL detected a large number of bony lesions that were occult on 99mTc-MDP bone scan and Na18F PET/CT.
PSMA-targeted PET/CT may offer improved sensitivity by binding directly to tumor cells, as opposed to localizing to sites of bony reaction.
This preliminary finding should be further explored in larger studies.
Acknowledgments
We gratefully acknowledge technical support from the Imaging Response Assessment Team (IRAT) lab at the Sidney Kimmel Comprehensive Cancer Center as well as financial support from CA134675, CA183031 and philanthropic funds to The James Buchanan Brady Urological Institute.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65:5–29. doi: 10.3322/caac.21254. [DOI] [PubMed] [Google Scholar]
- 2.Conde Moreno AJ, Ferrer Albiach C, Muelas Soria R, González Vidal V, García Gómez R, Albert Anteguera M. Oligometastases in prostate cancer: restaging stage IV cancers and new radiotherapy options. Radiat Oncol. 2014;9:258. doi: 10.1186/s13014-014-0258-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reyes DK, Pienta KJ. The biology and treatment of oligometastatic cancer. Oncotarget. 2015;6:8491–8524. doi: 10.18632/oncotarget.3455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ost P, Jereczek-Fossa BA, As NV, et al. Progression-free survival following stereotactic body radiotherapy for oligometastatic prostate cancer treatment-naïve recurrence: a multi-institutional analysis. Eur Urol. 2015 doi: 10.1016/j.eururo.2015.07.004. in press. [DOI] [PubMed] [Google Scholar]
- 5.Helyar V, Mohan HK, Barwick T, et al. The added value of multislice SPECT/CT in patients with equivocal bony metastasis from carcinoma of the prostate. Eur J Nucl Med Mol Imaging. 2010;37:706–713. doi: 10.1007/s00259-009-1334-3. [DOI] [PubMed] [Google Scholar]
- 6.Giovanella L, Castellani M, Suriano S, et al. Multi-field-of-view SPECT is superior to whole-body scanning for assessing metastatic bone disease in patients with prostate cancer. Tumori. 2011;97:629–633. doi: 10.1177/030089161109700515. [DOI] [PubMed] [Google Scholar]
- 7.Palmedo H, Marx C, Ebert A, et al. Whole-body SPECT/CT for bone scintigraphy: diagnostic value and effect on patient management in oncological patients. Eur J Nucl Med Mol Imaging. 2014;41:59–67. doi: 10.1007/s00259-013-2532-6. [DOI] [PubMed] [Google Scholar]
- 8.Schirrmeister H, Guhlmann A, Elsner K, et al. Sensitivity in detecting osseous lesions depends on anatomic localization: planar bone scintigraphy versus 18F PET. J Nucl Med. 1999;40:1623–1629. [PubMed] [Google Scholar]
- 9.Poulsen MH, Petersen H, Høilund-Carlen PF, et al. Spine metastases in prostate cancer: comparison of technetium-99m-MDP whole-body bone scintigraphy, [(18) F]choline positron emission tomography (PET)/computed tomography (CT) and [(18) F]NaF PET/CT. BJU Int. 2014;114:818–823. doi: 10.1111/bju.12599. [DOI] [PubMed] [Google Scholar]
- 10.Hillner BE, Siegel BA, Hanna L, Duan F, Shields AF, Coleman RE. Impact of 18F-fluoride PET in patients with known prostate cancer: initial results from the National Oncologic PET Registry. J Nucl Med. 2014;55:574–581. doi: 10.2967/jnumed.113.130005. [DOI] [PubMed] [Google Scholar]
- 11.Szabo Z, Mena E, Rowe SP, et al. Initial evaluation of [(18)F]DCFPyL for prostate-specific membrane antigen (PSMA)-targeted PET imaging of prostate cancer. Mol Imaging Biol. 2015;17:565–574. doi: 10.1007/s11307-015-0850-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Uprimny C, Kroiss A, Nilica B, et al. (68)Ga-PSMA ligand PET versus (18)F-NaF PET: evaluation of response to (223)Ra therapy in a prostate cancer patient. Eur J Nucl Med Mol Imaging. 2015;42:362–363. doi: 10.1007/s00259-014-2922-4. [DOI] [PubMed] [Google Scholar]
- 13.Rowe SP, Gorin MA, Hammers HJ, et al. Imaging of metastatic clear cell renal cell carcinoma with PSMA-targeted 18F-DCFPyL PET/CT. Ann Nucl Med. 2015 doi: 10.1007/s12149-015-1017-z. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]