Abstract
The goal of the current study was to examine conflict appraisals and diurnal cortisol production as mediators of the robust association between marital conflict and adolescent adjustment problems. Parents reported their marital conflict and were observed engaging in a marital conflict discussion; they also reported adolescent internalizing and externalizing behaviors. Adolescents (n = 105, 52% female, 10–17 years of age) appraised their parents’ marital conflict and reported their internalizing and externalizing behaviors. After the laboratory visit, adolescents provided four saliva samples on each of 2 consecutive days to assess diurnal cortisol production. More-negative marital conflict predicted more self-blame for parental conflict, which in turn predicted less robust decreases in cortisol across the day. Further, this flattened cortisol production pattern mediated the relationship between greater self-blame for parental conflict and adolescents’ elevated internalizing behaviors. Feeling responsible for parental conflict appears to be particularly damaging in terms of physiological regulation and adjustment, and may therefore be a particularly useful intervention target.
There is increasing recognition that adolescence is a critical period for the etiology and maintenance of mental health trajectories (e.g., Andersen, 2003). During puberty, there are dramatic and cascading changes in body and brain systems (Andersen, 2003), including the overproduction of axons and synapses in the brain’s frontal cortex, followed by dramatic pruning (Giedd et al., 1999). This brain remodeling creates a period of heightened biological sensitivity to environmental influences because the pruning that occurs reflects adaptations to environmental inputs (Crews, He, & Hodge, 2007). This plasticity is adaptive when it allows for the development of structures to deal with environmental conditions (Meaney et al., 1996) and problematic when it creates long-term negative consequences for the processing of environmental stimuli (Bevans, Cerbone, & Overstreet, 2008). These lines of evidence have converged to indicate a pattern whereby “puberty is a key maturational period that sets the stage for potentially a lifetime free from or full of psychopathology” (Andersen, 2003, p. 4).
Potent predictors of the development of mental health and adjustment problems in youth are negative characteristics of the family environment, including high levels of hostile and unresolved conflict between parents (e.g., Zimet & Jacob, 2001). In addition, such negative interparental conflict predicts dysregulated patterns of cortisol production across the day (e.g., Lucas-Thompson & Hostinar, 2013), an important indicator of physiological regulation (Gunnar & Donzella, 2002) and an important predictor of physical and psychological health (Chrousos, 2009). Both dysregulated stress physiology (e.g., Luecken & Lemery, 2004) and the ways that children appraise and perceive their parents’ conflict (Grych, Seid, & Fincham, 1992) have been conceptualized as important mediators of the association between marital conflict and mental health. However, empirical evidence for these mediational pathways is lacking, particularly during the important transitional developmental period of adolescence. Therefore, the goal of the current study was to examine the pathways linking marital conflict to adolescent conflict appraisals, diurnal cortisol production, and mental health (see Figure 1 for the conceptual model guiding the current study).
FIGURE 1.
Conceptual model guiding the current study.
MARITAL CONFLICT AND YOUTH ADJUSTMENT
Parental marital conflict is associated with adjustment problems for children and adolescents (e.g., Zimet & Jacob, 2001). These problems take the form of serious, clinical mental health problems (Turner & Kopiec, 2006), as well as subclinical problems that have serious negative consequences for long-term mental health and functioning (Zimet & Jacob, 2001). Marital conflict explains a significant proportion of variance in externalizing problems, including aggression, vandalism, conduct problems, and delinquency, and variance in internalizing problems, including depression, anxiety, and low self-esteem (e.g., Bornovalova et al., 2014; Lee, Wickrama, & Simons, 2013; Obradović, Bush, & Boyce, 2011). Furthermore, more-negative marital conflict predicts steeper increases in depressive symptoms across adolescence (Papp, 2012). These associations are often evident longitudinally (e.g., Lee et al., 2013) and in diverse types of families (e.g., Oh, Lee, & Park, 2011). In the current study, we examined factors that explain links between marital conflict and both internalizing and externalizing problems.
MARITAL CONFLICT AND YOUTH STRESS PHYSIOLOGY
Broadly, many different types of stressors activate the hypothalamic-pituitary-adrenocortical (HPA) axis, which is a critical part of the human stress response system (e.g., Hostinar & Gunnar, 2013). When the HPA axis is activated, cortisol is produced; in addition, there are well-documented, normative fluctuations in cortisol production across the day. Healthy individuals show peaks in cortisol production shortly after waking up; cortisol levels then decrease steadily across the rest of the day (Stone et al., 2001). Deviations from this pattern are considered signs of HPA axis dysregulation (e.g., Gunnar & Vazquez, 2001) and have been linked to numerous psychological and physical health outcomes (Chrousos, 2009).
Overall, dysregulated physiological regulation can manifest itself through both elevated and dampened cortisol production, depending on factors such as time of measurement and individual characteristics. In the context of stressors, acute elevations in basal cortisol levels are typically evident; however, as stressors become more chronic, cortisol production across the day tends to become flattened, with lower morning levels and higher evening levels, leading to reduced decreases in cortisol production and higher levels of total cortisol output across the day (Miller, Chen, & Zhou, 2007). These patterns likely reflect the self-rectifying feedback mechanisms of the HPA axis; the HPA axis can down-regulate its own production in response to periods of prolonged activation (Hostinar & Gunnar, 2013). The down-regulation of the HPA axis that results in a flattened cortisol production pattern has been referred to as hypocortisolism (Gunnar & Vazquez, 2001) or as the attenuation hypothesis (e.g., Susman, 2006).
Stressful experiences in close relationships are particularly potent triggers of the HPA axis broadly and cortisol production across the day in particular (e.g., Gunnar & Donzella, 2002). As a potent stressor, negative marital conflict likely interferes with children’s abilities to regulate physiological stress systems (Repetti, Taylor, & Seeman, 2002). There is evidence that low levels of family functioning and high levels of marital conflict predict basal or average daily cortisol levels (e.g., Granger et al., 1998; Pendry & Adam, 2007). There is also evidence that low marital functioning produces flattened HPA axis production in terms of cortisol decreases across the day (i.e., blunted decreases) in children. However, this same pattern was not evident for adolescents (Pendry & Adam, 2007). This research suggests potential developmental differences in the effects of marital characteristics on youth stress physiology, an argument in line with evidence about the effects of marital conflict on acute stress reactivity (e.g., Lucas-Thompson, 2012). However, most research linking marital conflict and diurnal cortisol production has focused on children. If marital conflict is in fact associated with attenuated diurnal cortisol production in adolescence, it would be fruitful to investigate the mechanisms that explain this pathway. The current study aimed to fill these gaps in the literature.
YOUTH CONFLICT APPRAISALS AS MEDIATORS OF THE EFFECTS OF MARITAL CONFLICT
In the face of abundant evidence that interparental conflict puts children and adolescents at elevated risk for a variety of mental health and adjustment problems, attention has turned to investigating mechanisms that underlie this pathway. Theorists suggest that the negative cognitive and emotional responses that conflict elicits in children are critical mechanisms (Davies & Cummings, 1994; Grych et al., 1992). Although the characteristics of conflict itself are important, youth appraise conflict in different ways, which results in distinct reactions to conflict and differential influences of conflict on youth outcomes (Grych & Fincham, 1990). The three dimensions of conflict appraisals considered most often are perceptions of conflict properties (e.g., frequency, intensity), self-blame, and threat (Bickham & Fiese, 1997).
In terms of understanding effects of conflict appraisals on youth adjustment, past research suggests that self-blame and threat appraisals are particularly relevant. Feeling threatened by parental conflict is posited to lead to internalizing symptoms like anxiety (Grych et al., 1992). Perceived threat also increases the likelihood that children, especially boys, act out in destructive ways (Grych et al., 1992). In terms of self-blame, conflict that is child centered is more strongly and consistently related to adjustment problems than are other measures of marital conflict (Jouriles et al., 1991). Blaming oneself for parental conflict is posited to increase symptoms of depression and reduce feelings of self-worth (Grych et al., 1992; Oh et al., 2011), as well as increase oppositional behavior (Jouriles et al., 1991). Self-blame is more consistently related to both internalizing and externalizing problems than are threat appraisals (e.g., Fosco & Grych, 2008). Conflict appraisals are more consistently related to adjustment problems than are parents’ reports of conflict (Grych et al., 1992), and threat and self-blame appraisals mediate links between marital conflict and adjustment in children (e.g., Grych et al., 1992) and adolescents (e.g., Mann & Gilliom, 2004). Based on this past research, it is evident that the different dimensions of marital conflict are related in distinct ways to child outcomes. Therefore, in the current study, the unique dimensions of conflict appraisals were considered.
Conflict appraisals may also mediate links between marital conflict and stress physiology; however, there is not yet empirical evidence for this theoretically rooted mediational pathway. Broadly, stressor appraisals are critical in determining physiological responses to stressful experiences (Kemeny, 2003). The only study to investigate the role of conflict appraisals in diurnal cortisol production indicated that emerging adults who felt more self-blame for parental conflict displayed lower levels early in the day and blunted decreases in levels across the day (Lucas-Thompson & Hostinar, 2013); other appraisal dimensions (of conflict properties and threat) were not related to diurnal cortisol. However, in this study, only appraisals (and not marital conflict per se) were considered. Therefore, it is unknown whether appraisals mediate links between marital conflict and stress physiology, or whether flattened patterns of diurnal cortisol production are also evident in adolescence, which is an important issue given evidence for developmental differences in the effects of marital conflict on youth (Cummings, Zahn-Waxler, & Radke-Yarrow, 1981; Lucas-Thompson, 2012; Lucas-Thompson & Goldberg, 2011). To fill these gaps in our knowledge, the goal of the current study was to examine the pathways linking marital conflict, conflict appraisals, and diurnal cortisol production.
PHYSIOLOGICAL FUNCTIONING AS A MEDIATOR OF THE EFFECTS OF MARITAL CONFLICT
As marital conflict is a potentially chronic stressor, theory emphasizes the negative influence of conflict on children’s abilities to effectively and appropriately regulate physiological stress functioning (Luecken & Lemery, 2004; Repetti et al., 2002). There have been multiple arguments that disruptions in physiological functioning mediate associations between marital conflict and adjustment problems (Heim & Nemeroff, 2001; Repetti et al., 2002; Susman, 2006). Although there is relatively little empirical evidence supporting this mediational pathway, the existing evidence has supported the argument that marital conflict is related to child maladjustment indirectly through cortisol reactivity (e.g., Davies, Sturge-Apple, Cicchetti, & Cummings, 2007).
There are many reasons that disruptions in HPA axis regulation may lead to the development of mental health problems. Dysregulation in physiological functioning may be linked with disruptions in brain and behavioral functioning (Roozendaal & McGaugh, 1996). Specific to internalizing and externalizing behaviors, a more-active HPA axis may reflect a tendency to withdraw, in part because internalizing problems may be rooted in lower stress-reactive thresholds (Kagan, Reznick, & Snidman, 1987). In contrast, blunted HPA axis activity may reflect a tendency to approach, perhaps because externalizing behaviors may be rooted in much higher stress-reactive thresholds (e.g., Rogeness, Javors, Maas, & Macedo, 1990).
Empirical evidence from samples of children has generally supported these hypotheses. Children with internalizing, behavioral inhibition, or social problems tend to have higher levels of morning and/or afternoon cortisol levels than other children (e.g., Scerbo & Kolko, 1994; Smider et al., 2002). Internalizing behaviors are also related to flattened levels of cortisol production across the day (Klimes-Dougan, Hastings, Granger, Usher, & Zahn-Waxler, 2001; Shirtcliff & Essex, 2008). In addition, higher levels of morning cortisol predict increases over time in children’s mental health problems (Shirtcliff & Essex, 2008; Smider et al., 2002). In contrast, externalizing problems are generally related to lower morning and/or basal cortisol levels (Scerbo & Kolko, 1994; Shirtcliff, Granger, Booth, & Johnson, 2005; Tennes, Kreye, Avitable, & Wells, 1986), particularly for boys (McBurnett et al., 1991). However, associations between cortisol and externalizing behaviors are more mixed than are associations between cortisol and internalizing behaviors (see Smider et al., 2002 for a review).
Comparatively, there is scant and mixed evidence for links between diurnal cortisol and adjustment in adolescence. For example, in preadolescence, low morning cortisol predicts more symptoms of conduct disorder (Vanyukov et al., 1993), but aggression is not related to plasma basal cortisol levels (Schulz, Halperin, Newcorn, Sharma, & Gabriel, 1997). In addition, with few exceptions (e.g., Smider et al., 2002), developmental research investigating diurnal cortisol and adjustment has focused on children selected for high levels of adjustment problems. The few studies to test stress physiology as a mediator of marital conflict effects on adjustment have focused on acute reactivity rather than diurnal functioning. These findings are mixed in that they provide support for cortisol reactivity as a mediator (Davies et al., 2007; Koss et al., 2013) and moderator (El-Sheikh, Keiley, Erath, & Dyer, 2013; Obradović et al., 2011) of the links between marital conflict and adjustment. Finally, the association between conflict appraisals and adjustment is not mediated by diurnal cortisol production in emerging adulthood (Lucas-Thompson & Hostinar, 2013), raising the question of whether these processes change during adolescence. Accordingly, the goal of this study was to investigate links of marital conflict, conflict appraisals, and stress physiology with internalizing and externalizing behaviors in a community sample of adolescents.
THE CURRENT STUDY
Based on the literature reviewed, we hypothesized that higher levels of marital conflict would predict more-negative conflict appraisals, which in turn would predict flattened patterns of diurnal cortisol production (Figure 1). We also hypothesized that patterns of diurnal cortisol production would be related, likely in distinct ways, to externalizing and internalizing behaviors. Last, we hypothesized that physiological functioning would at least partially mediate links between conflict appraisals and adjustment.
METHOD
Participants
Two-parent families with at least one child between 10 and 17 years of age were recruited from the community (Twin Cities, Minnesota) through advertisements for a larger study on family relationships and stress. Adolescents and both of their parents participated. There were 153 adolescents (from 98 families) in the larger study; included in this study were 105 adolescents (from 70 families) who provided diurnal cortisol samples. This subsample of adolescents (52% female; Mage = 12.80, SD = 2.16) was ethnically diverse: Of those who reported ethnicity (9% did not), 54% were Caucasian, 23% reported multiple ethnic backgrounds, 16% were African American, 6% were Asian American, and 1% was Hispanic American. Most families were intact (79%), but stepparent families were included if the adults had been married or cohabitating for at least 2 years (M = 16.25 years, SD = 5.73). Yearly family income ranged from $3,375 to $450,000 (Mdn = $75,000, SD $61,488.09). On average, parents had completed an associate’s degree (or vocational training beyond high school; 17% of mothers and 16% of fathers had obtained an associate’s degree).
Procedure
Families first visited the laboratory in the afternoon. After providing informed consent and assent, youth and parents were taken to separate rooms to complete a variety of tasks. Each family member separately filled out questionnaires using Audio Computer Assisted Self Interview software. Family members were each paid $20 for participation; an additional $10 covered transportation. At the end of the visit, adolescents were asked if they would be willing to provide saliva samples across 2 consecutive and similar (in terms of schedule) days close in time to the visit (for an additional $10). The saliva sample collection was explained and practiced. Participants were told that they could put the swab anywhere except between their gums and lips and were instructed to leave swabs in for 3 min. Participants were told that it was essential to collect samples at different but specific times of day: immediately after waking (before eating and drinking anything other than water), 30 min after awakening, at 4 p.m., and at bedtime (before brushing teeth). On average, adolescents took saliva samples at 7:42 a.m. (SD = 161 min), 8:18 a.m. (SD = 157 min), 4:26 p.m. (SD = 79.45 min), and 9:30 p.m. (SD = 415 min). Compliance (in terms of taking samples at the correct times) was encouraged by sending reminders via text or e-mail 15 min before each sample was supposed to be provided (programmed based on participant estimates of when they would wake up and go to sleep on the collection days). In addition, research assistants emphasized the importance of knowing exactly when samples were collected, and so participants were instructed to provide specific information about when each sample was provided. Participants were asked to freeze samples until they were ready to be returned, at which point samples were mailed back to the laboratory in mailers provided by the study team, and then frozen. Each day that participants collected saliva samples, they also filled out a short questionnaire about health behaviors known to affect cortisol (e.g., medication, sleep).
While at the laboratory, parents engaged in two marital interactions (in a counterbalanced order). Behavior during only the standardized and widely used interaction (described next) was considered for the purposes of the current study. There were no differences in behavior based on the order in which the interaction tasks were completed (ts <1.05, ps >.30). In the standardized task, parents individually rated common areas of disagreement, and the most conflict-producing topics were chosen for them to try to resolve for 15 min (e.g., Kiecolt-Glaser et al., 1996). This interaction was videotaped and later coded (see next) for conflict behaviors.
Measures
Parent-Reported Marital Conflict
Two questionnaires were used to gather parent reports of the frequency/intensity and resolution of marital conflict. The five-item Conflict subscale of the Braiker-Kelley Partnership Questionnaire (Braiker & Kelley, 1979) was used to measure the frequency and intensity of marital conflict; the mean of each participant’s responses was calculated. The Resolution sub-scale from the Kerig Conflicts and Problem-Solving Scales (Kerig, 1996) was used to gather information about the typical outcomes of disagreements. For this second subscale, resolutions are proportionally weighted based on whether they are positive and result in increased intimacy (multiplied by 2), unclear or partial (no weighting), or negative and result in increased hostility (multiplied by −2). With respect to both conflict frequency/intensity and conflict resolution, an average of both parents’ scores was utilized for each variable (maternal and paternal conflict frequency/ intensity scores, r = .55, p <.001, and conflict resolution scores, r = .46, p <.001, were significantly intercorrelated).
Observed conflict behavior
Based on behavior during the marital conflict interaction, each parent was rated based on the degree to which specific positive (constructive) and negative (destructive) conflict behaviors were displayed (0 = absent to 2 = very strong display; Cummings, Kouros, & Papp, 2007; Lucas-Thompson, 2012). A negative conflict-tactics score was created by summing ratings of nonverbal and verbal anger, defensiveness, distress, physical aggression, threat, pursuit, insult, and withdrawal. A positive conflict-tactics score was computed by summing ratings of support, physical affection, calm discussion, problem solving, and humor. Different observers coded mothers and fathers. An average of both parents’ conflict behavior was calculated (maternal and paternal conflict behavior were significantly correlated: rs >0.41, ps <.001). There was adequate reliability prior to consensus coding (ICCs >0.82).
Conflict Appraisals
Youth appraisals of parental conflict were assessed using the Children’s Perceptions of Interparental Conflict Scale (Grych et al., 1992), an internally consistent, reliable, and valid measure of conflict appraisals (Grych et al., 1992) that has been validated for use through late adolescence (Bickham & Fiese, 1997). The Children’s Perceptions of Interparental Conflict Scale is a 49-item questionnaire that assesses nine dimensions of inter-parental conflict: frequency, intensity, resolution, threat, coping efficacy, content (child related or non–child related), stability, self-blame, and triangulation (or the likelihood of the conflict involving the child). Answer choices are “true,” “sort of true,” and “false”; after reverse scoring, higher scores reflect more-negative conflict appraisals. Following past research (e.g., Bickham & Fiese, 1997), high scores on Conflict Properties (dimensions of frequency, intensity, resolution, stability, and triangulation; 28 items, Cronbach’s α = 0.91) represent appraisals that parental marital conflict occurs frequently, is intensely hostile, is not well resolved, is caused by stable factors, and is likely to make the child feel caught in the middle; the Conflict Properties scale has also been used previously to measure exposure to conflict (Grych, Fincham, Jouriles, & McDonald, 2000). High scores on Threat (dimensions of threat and coping efficacy; 12 items, Cronbach’s α = 0.83) represent appraisals that children are threatened by and unable to cope with parental conflict. Finally, high scores on Self-Blame (content and self-blame; nine items, Cronbach’s α = 0.66) represent appraisals that marital conflict is about the child and for which the child blames him- or herself.
Diurnal Cortisol
Saliva samples were assayed for cortisol at the University of Trier. Samples were first centrifuged at 2,000 g for 10 min. Then, salivary cortisol levels were determined by a solid phase time-resolved fluorescence immunoassay with flouromeric end point detection. The intra-assay coefficient of variation was between 4.0% and 6.7%, and the corresponding interassay coefficients of variation were between 7.1% and 9.0%. All samples were assayed in duplicate and averaged. To reduce the error in sampling cortisol on only 1 day, at each sampling time point (wake-up, 30 min after awakening, 4 p.m., and bedtime), the values across the two collection days were averaged.
Adolescent Reports of Internalizing Behaviors (Symptoms of Depression and Anxiety)
Adolescents self-reported their symptoms of depression using the Center for Epidemiological Studies Depression Scale (Radloff, 1977), a widely used, reliable, and valid measure of depressive symptoms. The scale consists of 20 questions that assess depressive symptoms from the last week. The scale is 4 points, ranging from 0 (rarely or none of the time) to 3 (most or all of the time). A depressive symptoms score was created by summing all 20 items (after appropriate reverse scoring); higher scores represent more depressive symptoms (Cronbach’s α = 0.85). Scores of 16 or above are considered to be clinically significant depression. This criterion was met by 38 adolescents.
Adolescents reported their anxiety symptoms using the Revised Children’s Manifest Anxiety Scale (Reynolds & Richmond, 1978), a reliable and valid measure of the general anxiety experienced by children and adolescents (Reynolds, 1980). Adolescents answered 28 questions (e.g., “I worry about what is going to happen”) as “yes” or “no.” Mean scores were calculated such that higher scores reflected more symptoms of anxiety (Cronbach’s α = 0.83). Scores of 19 or above are considered to be clinically significant levels of anxiety (Stellard, Velleman, Langsford, & Baldwin, 2001); this criterion was met by nine adolescents. For use in analyses, reports of depressive symptoms and anxiety symptoms were standardized and averaged to represent internalizing behaviors.
Adolescent Reports of Externalizing Behaviors
Adolescents reported on their externalizing behaviors using the Youth Self Report, a well-validated and reliable measure of adolescent behavior problems (Achenbach & Edelbrock, 1987). Adolescents rated a series of statements in terms of how well they describe themselves (not true, somewhat/sometimes true, or very/ often true). An externalizing score was created by summing responses to the Attention Problems, Delinquency, and Aggressive subscales (Cronbach’s α = 0.86).
Parent-Reported Internalizing and Externalizing Behaviors
Both mothers and fathers reported on their child’s internalizing and externalizing behaviors via the Child Behavior Checklist (Achenbach, 1991), a well-validated, reliable, internally consistent and widely used parent-report measure of adjustment problems (Achenbach, 1999; Davies et al., 2007). Parents rated a series of statements in terms of how well they describe their adolescent (not true, somewhat/sometimes true, or very/often true). An internalizing score was created for each parent based on the sum of parent responses to the Anxious/Depressed, Withdrawn, and Somatic Problems subscales. Three adolescents met cutoffs for internalizing problems based on both mother and father reports. An externalizing score was created for each parent based on the sum of parent responses to the Attention Problems, Delinquency, and Aggressive subscales. Both maternal (Cronbach’s α: internalizing = 0.86, externalizing = 0.91) and paternal (Cronbach’s α: internalizing = 0.83, and externalizing = 0.93) reports were internally consistent. Nine and 12 adolescents met cutoffs for clinical levels of externalizing problems based on maternal and paternal reports, respectively.
Analytic Plan
Data Preparation
All variables were tested for normality; the observed negative conflict behavior, appraisal, cortisol, internalizing, and externalizing variables were skewed and therefore log-transformed.
Missing Data
To test whether data were missing completely at random (MCAR), Little’s MCAR test was used on the larger sample of 153 participants. Little’s MCAR test was not significant, χ2(559) = 592.35, p = .16, suggesting that data on primary variables were missing completely at random.
Potential Confounding Variables
We tested whether each of the health behavior and demographic variables was a significant predictor of the cortisol intercept or slope if the predictor was fixed (age; sex; ethnicity; weight; wake time; prescription and nonprescription drug use; hours of sleep the nights before; consumption of fruits, vegetables, or breakfast the days of sample collection) or by adding paths to individual cortisol values if the predictors were time-varying and had a different value at each sampling time (dairy, caffeine, and chips intake in the hour before sample collection). Each predictor was tested by itself. The only significant paths were the effect of wake time on the cortisol slope and of dairy consumption on the afternoon cortisol sample; thus these covariates were the only ones included in subsequent analyses.
Demographic controls were included as covariates of marital conflict and adjustment. There were ethnic differences in marital conflict in the current study; therefore, a White versus non-White variable was included as a covariate of marital conflict. Family income was also included as a covariate in all models. Because of the range of ages and pubertal statuses represented in this sample, pubertal status was included as a control variable in all models and was measured using the Pubertal Development Scale (Peterson, Crockett, Richards, & Boxer, 1988). When correlations between the covariates and primary variables of interest were non-significant, they were constrained to equal 0 in the models (when doing so did not significantly alter model fit).
Statistical Analyses
Correlations were used to examine bivariate associations. Mplus (version 7, Muthén & Muthén, 1998–2012) was used to model a latent growth model representing change in cortisol across the day; structural equation modeling (SEM) was used to examine relations among the constructs. SEM was used (a) so that simultaneous paths could be estimated, and (b) so that latent factors could be used to capture common variance in marital conflict and cortisol parameters, thus parsing out some of the measurement error in individual variables. We adopted a bottom-up approach to model testing by (a) testing the fit of the cortisol latent growth model, (b) using confirmatory factor analysis to build a marital conflict latent factor, and (c) testing the conceptual model (Figure 1).
The latent growth model was nonlinear to capture the change in cortisol across the day; slope parameters were set to 0, free, 1, and free. This approach is consistent with prior literature and reflects the nonlinear nature of diurnal cortisol production (e.g., McArdle & Epstein, 1987). Means of the intercepts/slopes and variances were free to vary. In the SEM models, the unique effects of each dimension of conflict appraisals were examined; however, these dimensions were allowed to covary with each other. To adjust for the clustering of youth within families, we accounted for dependence in the statistical model by adjusting the standard errors using a sandwich estimator (Carle, 2009; D’Onofrio et al., 2010; Koning, Lugtig, & Vollebergh, 2014; Osztovits et al., 2011). Maximum likelihood estimation was used throughout.
Because of the small sample size relative to the number of paths necessary to test the entirety of the conceptual model, the model was tested in two steps. First, we tested whether conflict appraisals mediated associations between marital conflict and diurnal cortisol production. Second, we tested whether stress physiology mediated associations between conflict appraisals and adjustment (considering internalizing and externalizing behaviors separately). In addition to testing the conceptual model to provide evidence for mediation, we tested mediation in two additional steps. First, we used percentile bootstrap tests of mediation (Hayes & Preacher, 2010) to test the significance of mediated pathways, a strategy appropriate given the relatively small sample size in the current study (Hayes, 2009). Second, we conducted tests to determine if reverse mediation models (i.e., whether cortisol mediated links between conflict and appraisals, and whether adjustment mediated links between appraisals and cortisol) provided an equal or better fit to the data as compared to the proposed conceptual model; these models were tested to provide a more rigorous test of the proposed directionality of variable relations. Because these mediation and reverse mediation models were not nested models, it was not possible to conduct difference testing in terms of model fit. Instead, as was appropriate, we compared model fit of the different models, including comparison of the Akaike Information Criterion (AIC) and Bayesian Information Criterion (BIC), which allow for the comparison of nonnested models and are most useful when examined in conjunction with each other (Kuha, 2004).
Fit of the SEM models was assessed by examining the chi-square test (which ideally is nonsignificant), the root mean square error of approximation (RMSEA; adequate fit is indicated by values under .08), the comparative fit index (CFI; adequate fit is indicated by values greater than .95), and the standardized root mean square residual (SRMR; adequate fit is indicated by values less than .08; Hu & Bentler, 1998).
RESULTS
Correlations, means, and standard deviations are presented in Table 1. Parent-reported marital conflict and negative conflict behavior were significantly and positively associated, and parent-reported conflict resolution was significantly negatively associated, with parent-reported externalizing behaviors. There were no other bivariate associations between marital conflict and adjustment. All of the marital conflict indicators were significantly related to conflict appraisals in the expected direction; the exception was that positive conflict behavior was not significantly related to self-blame appraisals. In addition, conflict appraisals were significantly related to all of the adjustment indicators (such that more-negative conflict appraisals were associated with higher levels of adjustment problems), except the association between threat appraisals and parent-reported internalizing behaviors was not significant.
TABLE 1.
Descriptive Statistics for and Correlations Between Main Variables of Interest
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Parent-Reported Conflict Frequency | 1 | .56*** | .44** | −.30*** | .32*** | .27** | .56** | .01 | −.12 | .08 | .13 | .11 | .16† | .12 | .17* |
| 2. Parent-Reported Conflict Resolution | 1 | −.40*** | .31*** | −.19* | −.22** | −.39*** | .04 | −.04 | −.13 | −.12 | −.07 | −.07 | −.07 | −.25** | |
| 3. Observed Negative Conflict Behaviora | 1 | −.60** | .20* | .18* | .30** | −.06 | −.20 | −.01 | .16 | .04 | .16† | −.11 | .18* | ||
| 4. Observed Positive Conflict Behavior | 1 | −.16 | −.21* | −.29** | .12 | .19 | .01 | −.21* | −.02 | −.06 | .02 | −.07 | |||
| 5. Self-Blame Appraisalsa | 1 | .41** | .48** | −.19 | −.14 | .12 | .25* | .29** | .19* | .26* | .36** | ||||
| 6. Threat Appraisalsa | 1 | .50** | −.06 | −.02 | −.01 | .18 | .39** | .07 | .27* | .20* | |||||
| 7. Conflict Property Appraisalsa | 1 | −.11 | −.08 | .05 | .25* | .36** | .28** | .41** | .20* | ||||||
| 8. Cortisol 1a | 1 | .30** | .30** | .02 | .17 | .17 | −.19 | −.11 | |||||||
| 9. Cortisol 2a | 1 | .15 | −.24* | .11 | .07 | −.09 | −.14 | ||||||||
| 10. Cortisol 3a | 1 | .28** | .17 | .11 | −.10 | −.01 | |||||||||
| 11. Cortisol 4a | 1 | .21 | .24* | .13 | .16 | ||||||||||
| 12. Youth-Reported Internalizinga | 1 | .31** | .50** | .23* | |||||||||||
| 13. Parent-Reported Internalizinga | 1 | .24* | .38** | ||||||||||||
| 14. Youth-Reported Externalizinga | 1 | .29** | |||||||||||||
| 15. Parent-Reported Externalizinga | 1 | ||||||||||||||
| M | 2.80 | 3.87 | .40 | 4.1 | .10 | .19 | .20 | .94 | 1.06 | .47 | −.04 | −.04 | 5.56 | 14.31 | .31 |
| SD | 1.22 | 5.13 | .34 | 1.34 | .09 | .10 | .11 | .28 | .29 | .28 | .45 | .94 | 4.87 | 8.92 | 1.21 |
Variable log-transformed to ameliorate the effects of significant skew.
p <.10.
p <.05.
p <.01.
p <.001.
In terms of bivariate associations with cortisol, positive marital conflict behavior was negatively related, and self-blame appraisals and conflict property appraisals were positively related, to cortisol levels at bedtime; there were no other significant associations between marital conflict or conflict appraisals and cortisol. There were also few significant bivariate correlations between adjustment and cortisol; the only significant (and positive) correlation was between cortisol levels at bedtime and parent-reported internalizing behaviors.
Testing the Cortisol Growth Model
The latent growth model for cortisol was tested in Mplus as described; dairy consumption at 4 p.m. and wake time were kept as covariates. The covariance between intercept and slope was significant, β = −.013, SE = .006, p = .019, and was therefore kept in the growth model. Latent growth model fit was adequate, χ2 = 5.99, p = .11, RMSEA =. 09, CFI = .91, SRMR = .06. This model included increases from Time 1 to Time 2 and then decreases from Time 2 to Time 3 and from Time 3 to Time 4, consistent with the well-documented pattern of cortisol production across the day (Stone et al., 2001). Therefore, this model specification was kept in subsequent analyses.
Results of the Confirmatory Factor Analysis
A latent factor was created to estimate Marital Conflict. The confirmatory factor analysis showed adequate model fit for the measurement model, such that this factor was well defined by the indicators; all standardized paths (factor loadings) were significant and relatively strong. The factor loadings for parent-reported conflict frequency/intensity, parent-reported conflict resolution, observed negative behavior, and observed positive behavior were .78, .71, .55, and −.39, respectively; all p values were less than .001. In addition, this measurement model had excellent fit: χ2 = 0.30, p = .59, RMSEA = .00, CFI = 1.00, SRMR = .01.
Testing the Conceptual Model
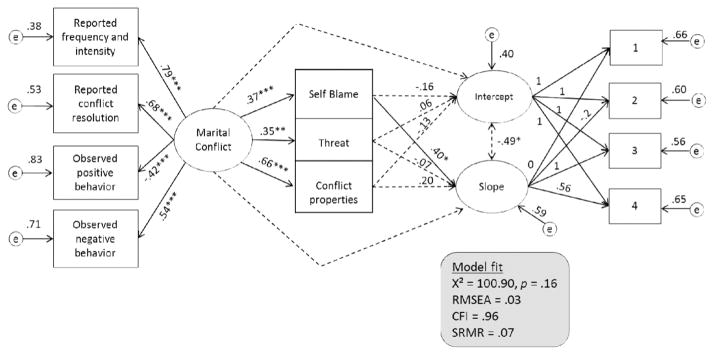
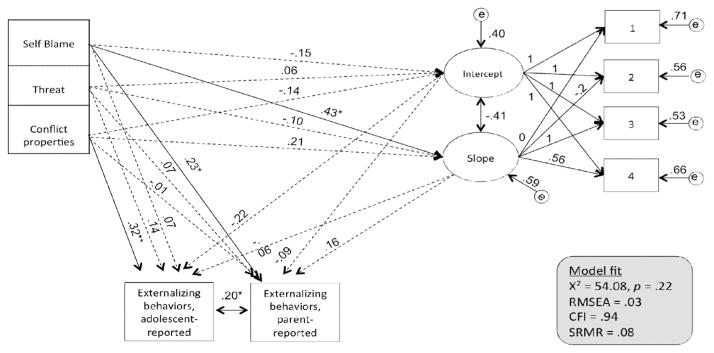
The conceptual model (Figure 1) was tested in two steps: (a) examining marital conflict, conflict appraisals, and diurnal cortisol production; and (b) examining conflict appraisals, diurnal cortisol, and adjustment. Goodness-of-fit indices suggested that the resulting models provided an excellent fit between model and data (see Figures 2 and 4 for model fit indices).
FIGURE 2.
Results of the structural equation model testing the associations between marital conflict, conflict appraisals, and diurnal cortisol production. Note: Standardized estimates for paths are displayed; solid arrows reflect significant paths, whereas dashed arrows reflect nonsignificant paths. The following pathways were modeled but were not displayed in the figure for simplicity: paths from ethnicity (Est. = −.39, p <.01) and family income (Est. = −.18, p = .14) to marital conflict, from wake time to cortisol slope (Est. = .24, p = .10), from dairy consumption to the afternoon cortisol sample (Est. = .28, p <.01), and from pubertal status to cortisol slope (Est. = .27, p <.05), conflict property appraisals (Est. = .35, p <.001), and wake time (Est. = −.17, p <.05). In addition, correlations between each pairwise combination of self-blame, conflict properties, and threat were included (Estimates ranging from .30 to .42, p <.001). Pathways between pubertal status and all other variables were nonsignificant and therefore constrained to 0. Pathways from marital conflict to cortisol level and slope were also non-significant and therefore constrained to 0. RMSEA = root mean square error of approximation; CFI = comparative fit index; SRMR = standardized root mean square residual. *p <.05. **p <.01. ***p <.001.
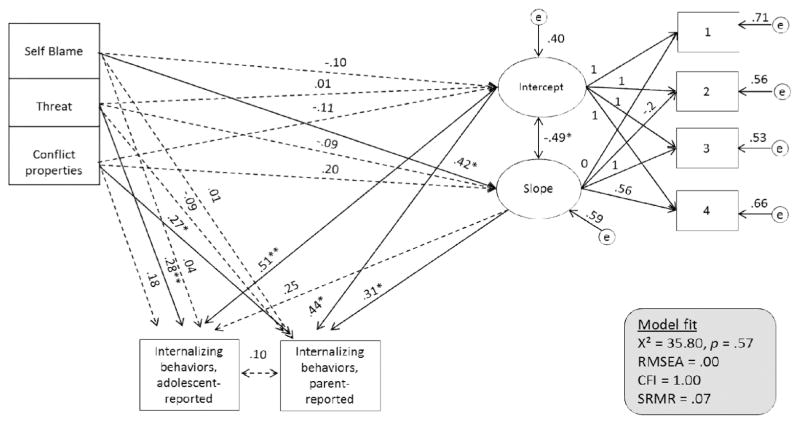
FIGURE 4.
Results of the structural equation model testing the associations between conflict appraisals, diurnal cortisol production, and internalizing behaviors. Note: Standardized estimates for paths are displayed; solid arrows reflect significant paths, whereas dashed arrows reflect nonsignificant paths. The following pathways were modeled but were not displayed in the figure for simplicity: paths from wake time to the cortisol slope (Est. = .30, p <.05) and dairy consumption to the afternoon cortisol sample (Est. = .32, p <.001); correlations between each pairwise combination of self-blame, conflict properties, and threat (Estimates ranging from .41 to .51, p <.001); paths between income and conflict properties (Est. = −.18, p <.01), threat appraisals (Est. = −.13, p <.05), and cortisol slope (Est. = −.36, p <.05); paths between income and other variables were nonsignificant and therefore constrained to 0. RMSEA = root mean square error of approximation; CFI = comparative fit index; SRMR = standardized root mean square residual. *p <.05. **p <.01.
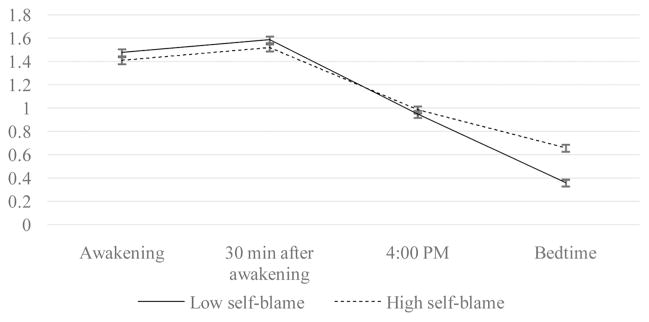
As shown in Figure 2, more-negative marital conflict predicted more-negative appraisals of conflict properties (e.g., frequency, intensity), as well as more feelings of self-blame and threat related to parental conflict. In addition, adolescents who felt responsible for their parents’ conflict displayed blunted decreases in cortisol production across the day. The average slope was negative (−0.807), suggesting that, on average, there were decreases in cortisol across the day, as expected. The positive association between self-blame and cortisol slope indicated that self-blame predicted more-positive change across the day (i.e., less pronounced decreases). To better understand the nature of this association, high and low levels of self-blame (based on a median split) were plotted in relation to cortisol levels across the day (see Figure 3). This plot indicated that this difference in cortisol slopes based on self-blame was due to elevated levels of cortisol production before bedtime for adolescents with high levels of self-blame. In addition, examination of the coefficients suggested an indirect path from marital conflict to self-blame to cortisol slope; bootstrap tests suggested that self-blame was a significant mediator of the association between marital conflict and cortisol slopes, Estimate = .012, 95% confidence interval [.01, .06]. R2 statistics for all endogenous observed variables in this model were significant at the p < .05 level, with the one exception of threat appraisals which showed trending significance (p = .068). The model explained higher levels of variance in cortisol and conflict property appraisals (34%–43%), and more modest levels of variance in threat and self-blame appraisals (12%–14%).
FIGURE 3.
Self-blame (median split used to determine high vs. low groups) and diurnal cortisol production. Note: Error bars represent standard errors.
The second portion of the conceptual model involved testing two separate structural equation models, one examining internalizing outcomes and one examining externalizing outcomes. In terms of internalizing outcomes (see Figure 4), adolescents with higher awakening cortisol levels had significantly greater internalizing problems, as measured by both parent reports and adolescent self-reports. In addition, adolescents with dampened decreases in cortisol across the day were reported by their parents to have greater internalizing behaviors. Cortisol slope was not related to adolescent reports of their own internalizing behaviors. Conflict property appraisals were also positively associated with parent-reported internalizing behaviors. Because appraisals of self-blame predicted dampened cortisol slopes, which in turn predicted parent-reported internalizing behaviors, we examined whether cortisol slope was a significant mediator of the link between self-blame and internalizing behaviors. The bootstrap test of mediation revealed that blunted cortisol slope was a significant mediator of the effects of more self-blame on adolescents’ elevated internalizing problems, Estimate = 4.26, 95% confidence interval [0.92, 9.60]. R2 statistics for all endogenous observed variables in this model were significant at the p <.05 level, with the one exception of parent ratings of internalizing which showed trending significance (p = .083). The model explained 34% of the variance in cortisol, 38% of the variance in youth ratings of internalizing behaviors, and 23% of the variance in parent ratings of internalizing behaviors.
In terms of externalizing behaviors (see Figure 5), adolescents who reported more self-blame for parental conflict were reported by their parents to engage in more externalizing behaviors. However, there were no associations between cortisol and externalizing behaviors. This model explained 26% of the variance in youth ratings of externalizing behaviors (p <.05) and 16% of the variance in parent ratings of externalizing behaviors (p <.01).
FIGURE 5.
Results of the structural equation model testing the associations between conflict appraisals, diurnal cortisol production, and externalizing behaviors. Note: Standardized estimates are displayed; solid arrows reflect significant paths whereas dashed arrows reflect nonsignificant paths. The following pathways were modeled but were not displayed for simplicity: paths from wake time to cortisol slope (Est. = .30, p <.05) and from dairy consumption to the afternoon cortisol sample (Est. = .31, p <.001); correlations between each pairwise combination of self-blame, conflict properties, and threat (Estimates ranging from .41 to .52, p <.001); paths between income and conflict properties (Est. = −.18, p <.01), threat appraisals (Est. = −.13, p <.05), and cortisol slope (Est. = −.36, p <.05); paths between income and other variables were nonsignificant and therefore constrained to 0; correlations between pubertal status and youth ratings of externalizing (Est. = .26, p <.05) and conflict property appraisals (Est. = .25, p <.001); paths between pubertal status and other variables were nonsignificant and therefore constrained to 0. RMSEA = root mean square error of approximation; CFI = comparative fit index; SRMR = standardized root mean square residual. *p <.05. **p <.01.
Reverse Mediation
To explore reverse mediation in Figure 2, we examined diurnal cortisol as a mediator of the association between conflict and conflict appraisals. The reverse mediation model demonstrated worse model fit than the original proposed mediation model with respect to all model fit estimates: χ2 = 103.59, p = .01; RMSEA = .05, CFI = .89, SRMR = .08. In addition, the proposed mediation model also suggested better fit in terms of AIC (1267.95) and BIC (1427.15) than did the reverse mediation model (AIC = 1276.61; BIC = 1441.82). urthermore, there was no evidence for mediation in this alternative model, because marital conflict was not related to cortisol intercept or slope (ps >.67). With regard to Figure 4, we examined internalizing behaviors as a mediator of the links between conflict appraisals and cortisol. The reverse model once again indicated poorer model fit than the original proposed model, although fit remained good, χ2= 41.31, p= .25, RMSEA = .03, CFI = .97, SRMR = .07. AIC (1367.01), and BIC (1530.65) values also indicated a poorer fit than those in the original model (AIC = 1356.06, BIC = 1513.65). Finally, both pathways of interest fell to nonsignificance, thus there was no evidence of mediation in the reverse model.
DISCUSSION
The goal of the current study was to examine the extent to which conflict appraisals mediated associations between marital conflict and dysregulated diurnal cortisol production patterns, as well as whether diurnal cortisol production explained links between conflict appraisals and adjustment. These mediational pathways are theoretically relevant (Grych et al., 1992; Repetti et al., 2002) but empirically understudied, particularly in adolescence, a critical period for the development of mental health trajectories (Andersen, 2003). Results suggested that self-blame for parental conflict was the conflict appraisals dimension most consistently related to diurnal cortisol production and adjustment. Marital conflict had indirect effects on blunted cortisol slopes through self-blame appraisals. Further, self-blame appraisals had indirect effects on internalizing behaviors (as reported by parents) through blunted diurnal cortisol slopes.
Past research has provided evidence that low levels of family functioning predict basal or average daily cortisol levels (Granger et al., 1998; Pendry & Adam, 2007), as well as less-robust decreases in cortisol production across the day, particularly for children (Pendry & Adam, 2007). In addition, in emerging adulthood, self-blame for parental conflict is related to flattened diurnal cortisol production patterns (Lucas-Thompson & Hostinar, 2013). The current study adds to our knowledge by demonstrating that similar patterns are evident in adolescence and provides evidence that these flattened patterns of cortisol production linked with self-blame appear to be driven by elevated evening levels of cortisol production. Furthermore, the current study contributes evidence that self-blame for parental conflict mediates links between marital conflict and diurnal cortisol production. The results of the current study are consistent with theory (Grych et al., 1992) and empirical evidence that conflict appraisals mediate effects of interparental conflict on adjustment outcomes (e.g., Mann & Gilliom, 2004). However, the current study also extends our knowledge by providing the first empirical evidence that conflict appraisals—specifically, appraisals of being responsible for parental conflict—mediate effects of marital conflict on diurnal cortisol production. The results of this study, combined with those of past research (Lucas-Thompson & Hostinar, 2013), suggest that self-blame for parental conflict is a dimension related to conflict exposure that is particularly likely to produce dampened HPA axis functioning. Dampened or attenuated HPA axis functioning is an indicator of physiological dysregulation (e.g., Gunnar & Vazquez, 2001) that has been linked to numerous psychological and physical health outcomes (Chrousos, 2009).
Interestingly, neither conflict property nor threat appraisals were related to diurnal cortisol production. However, past research on HPA axis activation and functioning more broadly has suggested that threat—particularly feelings of uncontrollable, social threat—is a very potent activator of the HPA axis (Dickerson & Kemeny, 2004). It may be that feeling threatened by parental conflict activates different fear systems than does social threat; for instance, the measure of threat appraisals asks youth to report about fear to self or parents during marital conflict. Social threat, in contrast, reflects issues such as social evaluation and threats to social esteem and/or status and has been linked to elevated waking cortisol levels and internalizing problems (Dickerson & Kemeny, 2004). However, it is also possible that threat and/or conflict property appraisals surrounding marital conflict are related to other indicators of physiological functioning, such as acute cortisol reactivity, or that adolescents in the present sample did not experience particularly high levels of threat (e.g., fear for their safety) related to their parents’ conflict.
Although all of the dimensions of conflict appraisals were related to adjustment, different appraisals were related to different indicators of adjustment problems. Appraisals of conflict properties and threat were related to internalizing but not externalizing behaviors. In line with conceptualizations about the role of appraisals in producing problematic adjustment outcomes (e.g., Grych et al., 1992), exposure to frequent and threatening conflict may interfere with effective coping and result in greater symptoms of depression and anxiety. Self-blame was also the only conflict appraisal dimension related to both externalizing and internalizing behaviors, although it was related to parent- and not to adolescent-reported behaviors. This finding is in line with past research suggesting that self-blame is more consistently related to adjustment problems than are threat or conflict property appraisals (Fosco & Grych, 2008), as well as evidence that self-blame is linked to both externalizing and internalizing problems (Grych et al., 1992; Jouriles et al., 1991; Oh et al., 2011). However, given the cross-sectional nature of the current study, it is also possible that child-centered conflict is more likely in families in which youth have more adjustment problems; in other words, self-blame for parental conflict may be linked with adjustment problems—particularly those that parents perceive and report—because these problems increase parental conflict about child-rearing.
In addition, the results of the current study suggested that flattened cortisol slopes mediated associations between self-blame appraisals and parent-reported internalizing behaviors, in line with a common theoretical argument about the mechanisms by which conflict produces adjustment problems (Heim & Nemeroff, 2001; Repetti et al., 2002; Susman, 2006). Past research has suggested that children with internalizing problems often display higher morning and/or afternoon cortisol levels (e.g., Scerbo & Kolko, 1994; Smider et al., 2002) or flattened patterns of cortisol production across the day (Klimes-Dougan et al., 2001; Shirtcliff & Essex, 2008). In the current study, self-blame appraisals predicted dampened cortisol slopes, apparently driven by higher evening cortisol levels, which then predicted more internalizing behaviors. In addition, the results suggest that internalizing behaviors are related to similar patterns of flattened patterns of cortisol production in a community sample in which there was a range of severity in internalizing problems.
Although theory posits that individuals with externalizing behaviors display blunted HPA axis functioning (Kagan et al., 1987), and there is some empirical evidence supporting this position (Scerbo & Kolko, 1994; Shirtcliff et al., 2005; Tennes et al., 1986), the associations between cortisol and externalizing behaviors are more mixed than are associations between cortisol and internalizing behaviors (Smider et al., 2002). In the current study, neither awakening cortisol levels nor changes in cortisol levels across the day were related to externalizing behaviors. It may be that diurnal cortisol production patterns are associated with more serious, perhaps clinical levels of behavior problems. For instance, several of the studies that have provided evidence for a link between blunted HPA axis activity and externalizing behaviors have focused on children recruited because they displayed high levels of behavior problems (e.g., Scerbo & Kolko, 1994). There is also evidence that there is a fair degree of intraindividual variability in basal cortisol levels and that estimating the proportion of variance in cortisol production that is attributable to statelike versus traitlike dimensions may be fruitful in understanding links between cortisol production and adjustment (Shirtcliff et al., 2005).
LIMITATIONS
Although important and novel, there are several limitations of the current study. The sample was relatively small; therefore, it was not possible to test the entire conceptual model in one step. In addition, though the sample was diverse in socioeconomic status and ethnicity, more serious types of marital conflict and adjustment problems may have been underrepresented. Although cortisol was measured on multiple days, which reduces error inherent in measuring cortisol at only one time point (MacArthur Research Network on Stress and Health, 2000), future research would benefit from examining intraindividual variability in cortisol in relation to marital conflict and adjustment. We accounted for wake time in analyses, but including time-since-waking as a time-varying covariate can also be helpful in accounting for individual variations in cortisol collection times. An additional methodological limitation involved the internal consistency of the measure of self-blame for parental conflict, which was less than ideal, but was in line with estimates from past studies (e.g., Lucas-Thompson & Hostinar, 2013). Past studies have also found that this dimension of conflict appraisals is less internally consistent than others (e.g., Bickham & Fiese, 1997; Lucas-Thompson & Hostinar, 2013). Finally, it is ideal to test mediational models with measures separated over time; the correlational and cross-sectional nature of the current study precludes causal conclusions. Future studies investigating associations between marital conflict appraisals, stress physiology, and adjustment over time would contribute important information about the causal pathways explaining how chronic negative family environments predict adjustment and mental health problems.
CONCLUSIONS
Despite these limitations, the current study provides new and important information about marital conflict and diurnal cortisol production in adolescence, suggesting that marital conflict indirectly predicts blunted decreases in cortisol production over the day through youth appraisals of blame and responsibility for parental conflict and that self-blame appraisals indirectly predict parent-reported internalizing behaviors through flattened diurnal cortisol slopes. Although direct evidence for these pathways was not provided in the current study, integrating across models, the results imply that marital conflict could indirectly relate to internalizing behaviors through self-blame appraisals and flattened cortisol slopes; future research will be needed to examine this possibility. Together with past research (Jouriles et al., 1991; Lucas-Thompson & Hostinar, 2013), the current study suggests that, particularly in adolescence, feeling responsible for parental conflict may be particularly damaging for patterns of physiological and behavioral regulation. Given the importance of adolescence for the establishment of mental health trajectories with life-long consequences (Andersen, 2003), these results suggest that adolescents who feel self-blame for parental conflict may suffer in terms of their long-term mental health and functioning. The results also underscore potential causal pathways linking marital conflict, negative conflict appraisals, stress physiology, and internalizing behaviors, specifically that self-blame mediates links between marital conflict and diurnal cortisol production, and flattened cortisol slopes mediate links between self-blame and internalizing behaviors—even in a community sample. Therefore, attempts to improve the long-term health and functioning of adolescents should focus on the ways that conflict is appraised as well as physiological regulation in the context of day-to-day functioning.
References
- Achenbach TM. Manual for the child behavior checklist: 4–18 and 1991 profile. Burlington, VT: Department of Psychiatry, University of Vermont; 1991. [Google Scholar]
- Achenbach TM. The Child Behavior Checklist and related instruments. In: Maruish ME, editor. The use of psychological testing for treatment planning and outcomes assessment. 2. Mahwah, NJ: Erlbaum; 1999. pp. 429–466. [Google Scholar]
- Achenbach TM, Edelbrock CS. Manual for the youth self-report and profile. Burlington, VT: University Associates in Psychiatry; 1987. [Google Scholar]
- Andersen SL. Trajectories of brain development: Point of vulnerability or window of opportunity? Neuroscience and Biobehavioral Reviews. 2003;27:3–18. doi: 10.1016/S0149-7634(03)00005-8. [DOI] [PubMed] [Google Scholar]
- Bevans K, Cerbone A, Overstreet S. Relations between recurrent trauma exposure and recent life stress and salivary cortisol among children. Development and Psychopathology. 2008;20:257–272. doi: 10.1017/S0954579408000126. [DOI] [PubMed] [Google Scholar]
- Bickham NL, Fiese BH. Extension of the children’s perceptions of interparental conflict scale for use with late adolescents. Journal of Family Psychology. 1997;11:246–250. doi: 10.1037/0893-3200.11.2.246. [DOI] [Google Scholar]
- Bornovalova MA, Cummings JR, Hunt E, Blazei R, Malone S, Iacono WG. Understanding the relative contributions of direct environmental effects and passive genotype–environment correlations in the association between familial risk factors and child disruptive behavior disorders. Psychological Medicine. 2014;44:831–844. doi: 10.1017/S0033291713001086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braiker H, Kelley H. Conflict in the development of close relationships. In: Burgess R, Huston T, editors. Social exchange and developing relationships. San Diego, CA: Academic Press; 1979. pp. 135–168. [Google Scholar]
- Carle AC. Fitting multilevel models in complex survey data with design weights: Recommendations. BMC Medical Research Methodology. 2009;9:49. doi: 10.1186/1471-2288-9-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chrousos GP. Stress and disorders of the stress system. Nature Reviews Endocrinology. 2009;5:374–381. doi: 10.1038/nrendo.2009.106. [DOI] [PubMed] [Google Scholar]
- Crews F, He J, Hodge C. Adolescent cortical development: A critical period of vulnerability for addiction. Pharmacology Biochemistry and Behavior. 2007;86:189–199. doi: 10.1016/j.pbb.2006.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings EM, Kouros CD, Papp LM. Marital aggression and children’s responses to everyday interparental conflict. European Psychologist. 2007;12:17–28. doi: 10.1027/1016-9040.12.1.17. [DOI] [Google Scholar]
- Cummings EM, Zahn-Waxler C, Radke-Yarrow M. Young children’s responses to expressions of anger and affection by others in the family. Child Development. 1981;52:1274–1282. doi: 10.2307/1129516. [DOI] [Google Scholar]
- Davies PT, Cummings EM. Marital conflict and child adjustment: An emotional security hypothesis. Psychological Bulletin. 1994;116:387–411. doi: 10.1037/0033-2909.116.3.387. [DOI] [PubMed] [Google Scholar]
- Davies PT, Sturge-Apple ML, Cicchetti D, Cummings EM. The role of child adrenocortical functioning in pathways between interparental conflict and child maladjustment. Developmental Psychology. 2007;43:918–930. doi: 10.1037/0012-1649.43.4.918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson SS, Kemeny ME. Acute stressors and cortisol responses: A theoretical integration and synthesis of laboratory research. Psychological Bulletin. 2004;130:355–391. doi: 10.1037/0033-2909.130.3.355. [DOI] [PubMed] [Google Scholar]
- D’Onofrio BM, Singh AL, Iliadou A, Lambe M, Hultman CM, Neiderhiser JM, Lichtenstein P. A quasi-experimental study of maternal smoking during pregnancy and offspring academic achievement. Child Development. 2010;81:80–100. doi: 10.1111/j.1467-8624.2009.01382.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Sheikh M, Keiley M, Erath S, Dyer WJ. Marital conflict and growth in children’s internalizing symptoms: The role of autonomic nervous system activity. Developmental Psychology. 2013;49:92–108. doi: 10.1037/a0027703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fosco GM, Grych JH. Emotional, cognitive, and family systems mediators of children’s adjustment to interparental conflict. Journal of Family Psychology. 2008;22:843–854. doi: 10.1037/a0013809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giedd JN, Blumenthal J, Jeffries NO, Castellanos FX, Liu H, Zijdenbos A, Rapoport JL. Brain development during childhood and adolescence: A longitudinal MRI study. Nature Neuroscience. 1999;2:861–863. doi: 10.1038/13158. [DOI] [PubMed] [Google Scholar]
- Granger DA, Serbin LA, Schwartzman A, Lehoux P, Cooperman J, Ikeda S. Children’s salivary cortisol, internalising behaviour problems, and family environment: Results from the Concordia longitudinal risk project. International Journal of Behavioral Development. 1998;22:707–728. doi: 10.1080/016502598384135. [DOI] [Google Scholar]
- Grych JH, Fincham FD. Marital conflict and children’s adjustment: A cognitive-contextual framework. Psychological Bulletin. 1990;108:267–290. doi: 10.1037/0033-2909.108.2.267. [DOI] [PubMed] [Google Scholar]
- Grych JH, Fincham FD, Jouriles EN, McDonald R. Interparental conflict and child adjustment: Testing the mediational role of appraisals in the cognitive-contextual framework. Child Development. 2000;71:1648–1661. doi: 10.1111/1467-8624.00255. [DOI] [PubMed] [Google Scholar]
- Grych JH, Seid M, Fincham FD. Assessing marital conflict from the child’s perspective: The children’s perception of interparental conflict scale. Child Development. 1992;63:558–572. doi: 10.2307/1131346. [DOI] [PubMed] [Google Scholar]
- Gunnar MR, Donzella B. Social regulation of the cortisol levels in early human development. Psychoneuroendocrinology. 2002;27:199–220. doi: 10.1016/S0306-4530(01)00045-2. [DOI] [PubMed] [Google Scholar]
- Gunnar MR, Vazquez DM. Low cortisol and a flattening of expected daytime rhythm: Potential indices of risk in human development. Development and Psychopathology. 2001;13:515–538. doi: 10.1017/S0954579401003066. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs. 2009;76:408–420. doi: 10.1080/03637750903310360. [DOI] [Google Scholar]
- Hayes AF, Preacher KJ. Quantifying and testing indirect effects in simple mediation models when the constituent paths are nonlinear. Multivariate Behavioral Research. 2010;45:627–660. doi: 10.1080/00273171.2010.498290. [DOI] [PubMed] [Google Scholar]
- Heim C, Nemeroff CB. The role of childhood trauma in the neurobiology of mood and anxiety disorders: Preclinical and clinical studies. Biological Psychiatry. 2001;49:1023–1039. doi: 10.1016/s0006-3223(01)01157-x. [DOI] [PubMed] [Google Scholar]
- Hostinar CE, Gunnar MR. The developmental psychobiology of stress and emotion in childhood. In: Weiner IG, Freedheim DK, Lerner RM, editors. Handbook of psychology. 2. Hoboken, NJ: Wiley; 2013. pp. 121–141. [Google Scholar]
- Hu LT, Bentler PM. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods. 1998;3:424–453. doi: 10.1037/1082-989X.3.4.424. [DOI] [Google Scholar]
- Jouriles EN, Murphy CM, Farris AM, Smith DA, Richters JE, Waters E. Marital adjustment, parental disagreements about child rearing, and behavior problems in boys: Increasing the specificity of the marital assessment. Child Development. 1991;62:1424–1433. doi: 10.2307/1130816. [DOI] [PubMed] [Google Scholar]
- Kagan J, Reznick JS, Snidman N. The physiology and psychology of behavioral inhibition in children. Child Development. 1987;58:1459–1473. doi: 10.2307/1130685. [DOI] [PubMed] [Google Scholar]
- Kemeny ME. The psychobiology of stress. Current Directions in Psychological Science. 2003;12:124–129. doi: 10.1111/1467-8721.01246. [DOI] [Google Scholar]
- Kerig PK. Assessing the links between interparental conflict and child adjustment: The conflicts and problem-solving scales. Journal of Family Psychology. 1996;10:454–473. doi: 10.1037/0893-3200.10.4.454. [DOI] [Google Scholar]
- Kiecolt-Glaser JK, Newton T, Cacioppo JT, MacCallum RC, Glaser R, Malarkey WB. Marital conflict and endocrine function: Are men really more physiologically affected than women? Journal of Consulting and Clinical Psychology. 1996;64:324–332. doi: 10.1037/0022-006X.64.2.324. [DOI] [PubMed] [Google Scholar]
- Klimes-Dougan B, Hastings PD, Granger DA, Usher BA, Zahn-Waxler C. Adrenocortical activity in at-risk and normally developing adolescents: Individual differences in salivary cortisol basal levels, diurnal variation, and responses to social challenges. Development and Psychopathology. 2001;13:695–719. doi: 10.1017/S0954579401003157. [DOI] [PubMed] [Google Scholar]
- Koning IM, Lugtig P, Vollebergh WAM. Differential effects of baseline drinking status: Effects of an alcohol prevention program targeting students and/or parents (PAS) among weekly drinking students. Journal of Substance Abuse Treatment. 2014;46:522–527. doi: 10.1016/j.jsat.2013.11.003. [DOI] [PubMed] [Google Scholar]
- Koss KJ, George MRW, Davies PT, Cicchetti D, Cummings EM, Sturge-Apple ML. Patterns of children’s adrenocortical reactivity to interparental conflict and associations with child adjustment: A growth mixture modeling approach. Developmental Psychology. 2013;49:317–326. doi: 10.1037/a0028246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuha J. AIC and BIC: Comparisons of assumptions and performance. Sociological Methods & Research. 2004;33:188–229. doi: 10.1177/0049124103262065. [DOI] [Google Scholar]
- Lee TK, Wickrama KAS, Simons LG. Chronic family economic hardship, family processes and progression of mental and physical health symptoms in adolescence. Journal of Youth and Adolescence. 2013;42:821–836. doi: 10.1007/s10964-012-9808-1. [DOI] [PubMed] [Google Scholar]
- Lucas-Thompson R. Marital conflict exposure in relation to adolescent emotional and physiological stress responses: Evidence for different patterns of dysregulation. Journal of Research on Adolescence. 2012;22:704–721. [Google Scholar]
- Lucas-Thompson RG, Goldberg WA. Family relationships and children’s stress responses. Advances in Child Development and Behavior. 2011;40:243–299. doi: 10.1016/b978-0-12-386491-8.00007-4. [DOI] [PubMed] [Google Scholar]
- Lucas-Thompson RG, Hostinar CE. Family income and appraisals of parental conflict as predictors of psychological adjustment and diurnal cortisol in emerging adulthood. Journal of Family Psychology. 2013;27:784–794. doi: 10.1037/a0034373. [DOI] [PubMed] [Google Scholar]
- Luecken LJ, Lemery KS. Early caregiving and physiological stress responses. Clinical Psychology Review. 2004;24:171–191. doi: 10.1016/j.cpr.2004.01.003. [DOI] [PubMed] [Google Scholar]
- MacArthur Research Network on Stress and Health. Salivary cortisol measurement. 2000 Retrieved from http://www.macses.ucsf.edu/research/allostatic/salivarycort.php.
- Mann BJ, Gilliom LA. Emotional security and cognitive appraisals mediate the relationship between parents’ marital conflict and adjustment in older adolescents. The Journal of Genetic Psychology. 2004;165:250–271. doi: 10.3200/GNTP.165.3.250-271. [DOI] [PubMed] [Google Scholar]
- McArdle JJ, Epstein D. Latent growth-curves within developmental structural equation models. Child Development. 1987;58:110–133. doi: 10.2307/1130295. [DOI] [PubMed] [Google Scholar]
- McBurnett K, Lahey BB, Frick PJ, Risch C, Loeber R, Hart EL, Hanson KS. Anxiety, inhibition, and conduct disorder in children: II. Relation to salivary cortisol. Journal of the American Academy of Child & Adolescent Psychiatry. 1991;30:192–196. doi: 10.1097/00004583-199103000-00005. [DOI] [PubMed] [Google Scholar]
- Meaney MJ, Diorio J, Francis D, Widdowson J, LaPlante P, Caldji C, Plotsky PM. Early environmental regulation of forebrain glucocorticoid receptor gene expression: Implications for adrenocortical responses to stress. Developmental Neuroscience. 1996;18:49–60. doi: 10.1159/000111395. [DOI] [PubMed] [Google Scholar]
- Miller GE, Chen E, Zhou ES. If it goes up, must it come down? Chronic stress and the hypothalamic-pituitary-adrenocortical axis in humans. Psychological Bulletin. 2007;133:25–45. doi: 10.1037/0033-2909.133.1.25. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 7. Los Angeles, CA: Muthén & Muthén; 1998–2012. [Google Scholar]
- Obradović J, Bush NR, Boyce WT. The interactive effect of marital conflict and stress reactivity on externalizing and internalizing symptoms: The role of laboratory stressors. Development and Psychopathology. 2011;23:101–114. doi: 10.1017/S0954579410000672. [DOI] [PubMed] [Google Scholar]
- Oh KJ, Lee S, Park SH. The effects of marital conflict on Korean children’s appraisal of conflict and psychological adjustment. Journal of Child and Family Studies. 2011;20:444–451. doi: 10.1007/s10826-010-9411-6. [DOI] [Google Scholar]
- Osztovits J, Horváth T, Littvay L, Steinbach R, Jermendy Á, Tárnoki Á, Jermendy G. Effects of genetic vs. environmental factors on cardiovascular autonomic function: A twin study. Diabetic Medicine. 2011;28:1241–1248. doi: 10.1111/j.1464-5491.2011.03363.x. [DOI] [PubMed] [Google Scholar]
- Papp LM. Longitudinal associations between parental and children’s depressive symptoms in the context of interparental relationship functioning. Journal of Child and Family Studies. 2012;21:199–207. doi: 10.1007/s10826-011-9463-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pendry P, Adam EK. Associations between parents’ marital functioning, maternal parenting quality, maternal emotion and child cortisol levels. International Journal of Behavioral Development. 2007;31:218–231. doi: 10.1177/0165025407074634. [DOI] [Google Scholar]
- Peterson AC, Crockett L, Richards M, Boxer A. A self-report measure of pubertal status: Reliability, validity, and initial norms. Journal of Youth and Adolescence. 1988;17:117–133. doi: 10.1007/BF01537962. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Repetti RL, Taylor SE, Seeman TE. Risky families: Family social environments and the mental and physical health of offspring. Psychological Bulletin. 2002;128:330–366. doi: 10.1037/0033-2909.128.2.330. [DOI] [PubMed] [Google Scholar]
- Reynolds CR. Concurrent validity of what I think and feel: The revised children’s manifest anxiety scale. Journal of Consulting and Clinical Psychology. 1980;48:774–775. doi: 10.1037/0022-006X.48.6.774. [DOI] [PubMed] [Google Scholar]
- Reynolds CR, Richmond BO. What I think and feel: A revised measure of children’s manifest anxiety. Journal of Abnormal Child Psychology. 1978;6:271–280. doi: 10.1007/BF00919131. [DOI] [PubMed] [Google Scholar]
- Rogeness GA, Javors MA, Maas JW, Macedo CA. Catecholamines and diagnoses in children. Journal of the American Academy of Child and Adolescent Psychiatry. 1990;29:234–241. doi: 10.1097/00004583-199003000-00012. [DOI] [PubMed] [Google Scholar]
- Roozendaal B, McGaugh JL. Amygdaloid nuclei lesions differentially affect glucocorticoid-induced memory enhancement in an inhibitory avoidance task. Neurobiology of Learning and Memory. 1996;65:1–8. doi: 10.1006/nlme.1996.0001. [DOI] [PubMed] [Google Scholar]
- Scerbo AS, Kolko DJ. Salivary testosterone and cortisol in disruptive children: Relationship to aggressive, hyperactive, and internalizing behaviors. Journal of the American Academy of Child & Adolescent Psychiatry. 1994;33:1174–1184. doi: 10.1097/00004583-199410000-00013. [DOI] [PubMed] [Google Scholar]
- Schulz KP, Halperin JM, Newcorn JH, Sharma V, Gabriel S. Plasma cortisol and aggression in boys with ADHD. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:605–609. doi: 10.1097/00004583-199705000-00010. [DOI] [PubMed] [Google Scholar]
- Shirtcliff EA, Essex MJ. Concurrent and longitudinal associations of basal and diurnal cortisol with mental health symptoms in early adolescence. Developmental psychobiology. 2008;50:690–703. doi: 10.1002/dev.20336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shirtcliff EA, Granger DA, Booth A, Johnson D. Low salivary cortisol levels and externalizing behavior problems in youth. Development and Psychopathology. 2005;17:167–184. doi: 10.1017/S0954579405050091. [DOI] [PubMed] [Google Scholar]
- Smider NA, Essex MJ, Kalin NH, Buss KA, Klein MH, Davidson RJ, Goldsmith HH. Salivary cortisol as a predictor of socioemotional adjustment during kindergarten: A prospective study. Child Development. 2002;73:75–92. doi: 10.1111/1467-8624.00393. [DOI] [PubMed] [Google Scholar]
- Stellard P, Velleman R, Langsford J, Baldwin S. Coping and psychological distress in children involved in road traffic accidents. British Journal of Clinical Psychology. 2001;40:197–208. doi: 10.1348/014466501163643. [DOI] [PubMed] [Google Scholar]
- Stone AA, Schwartz JE, Smyth J, Kirschbaum C, Cohen S, Hellhammer D, Grossman S. Individual differences in the diurnal cycle of salivary free cortisol: A replication of flattened cycles for some individuals. Psychoneuroendocrinology. 2001;26:295–306. doi: 10.1016/S0306-4530(00)00057-3. [DOI] [PubMed] [Google Scholar]
- Susman EJ. Psychobiology of persistent antisocial behavior: Stress, early vulnerabilities and the attenuation hypothesis. Neuroscience & Biobehavioral Reviews. 2006;30:376–389. doi: 10.1016/j.neubiorev.2005.08.002. [DOI] [PubMed] [Google Scholar]
- Tennes K, Kreye M, Avitable N, Wells R. Behavioral correlates of excreted catecholamines and cortisol in second-grade children. Journal of the American Academy of Child Psychiatry. 1986;25:764–770. doi: 10.1016/S0002-7138(09)60193-X. [DOI] [PubMed] [Google Scholar]
- Turner HA, Kopiec K. Exposure to interparental conflict and psychological disorder among young adults. Journal of Family Issues. 2006;27:131–158. doi: 10.1177/0192513X05280991. [DOI] [Google Scholar]
- Vanyukov MM, Moss HB, Plail JA, Blackson T, Mezzich AC, Tarter RE. Antisocial symptoms in preadolescent boys and in their parents: Associations with cortisol. Psychiatry Research. 1993;46:9–17. doi: 10.1016/0165-1781(93)90003-Y. [DOI] [PubMed] [Google Scholar]
- Zimet DM, Jacob T. Influences of marital conflict on child adjustment: Review of theory and research. Clinical Child and Family Psychology Review. 2001;4:319–335. doi: 10.1023/A:1013595304718. [DOI] [PubMed] [Google Scholar]