Abstract
Background:
Breast cancer patients frequently experience psychological distress during the chemotherapy period.
Objectives:
This study aimed to evaluate the effect of relaxation with guided imagery on patients with breast cancer.
Patients and Methods:
A two-group, pretest-posttest, quasi-experimental design with a randomized controlled trial was conducted. Sixty-five breast cancer patients from one medical center in Taiwan were enrolled in the study. These patients were randomly assigned to the experimental group (n = 32) or to the control group (n = 33). Both groups received chemotherapy self-care education, but the experimental group also received relaxation with guided imagery training. The training on relaxation with guided imagery was conducted before chemotherapy, and the patients were supplied with a compact disc detailing the performance of relaxation with guided imagery for 20 minutes daily at home for 7 days after chemotherapy.
Results:
The experimental group showed significant decreases in insomnia (-0.34 ± 0.83, P < 0.05), pain (-0.28 ± 0.58, P < 0.05), anxiety (-3.56 ± 2.94, P < 0.00), and depression (-2.38 ± 2.70, P < 0.00) between the pretest and the posttest. Comparing the two groups, statistically significant differences were found in the overall symptom distress (B = 0.11, P < 0.05), insomnia (B = 0.50, P <0.05), depression (B = 0.38, P < 0.05), and numbness in physical symptoms (B = 0.38, P < 0.05), as well as in anxiety (B = 3.08, P < 0.00) and depression (B = 1.86, P < 0.00) in psychological distress. One week of relaxation with guided imagery can significantly improve the overall symptoms of distress, insomnia, depression, physical symptoms, and anxiety, and can decrease psychological distress.
Conclusions:
Relaxation with guided imagery had a positive effect on mediating anxiety and depression in breast cancer patients.
Keywords: Relaxation, Guided Imagery, Breast Cancer, Chemotherapy, Symptom
1. Background
Breast cancer incidence rates are increasing worldwide. Approximately one in eight American women will develop breast cancer during her lifetime (1). When a woman develops breast cancer, she and her family are considerably affected. Currently, chemotherapy remains the first option to control the postoperative progression of cancer to increase the survival rate (2).
The physical and psychological distress symptoms of chemotherapy are common clinical manifestations among cancer patients (3). Distress symptoms for breast cancer patients receiving chemotherapy or radiotherapy include fatigue, insomnia, loss of appetite, nausea, vomiting, changes in appearance, numbness, mild anxiety, and depression (4, 5).
Several studies have confirmed that, during the treatment of cancer patients and through appropriate intervention, complementary therapies can help relieve physical and psychological discomfort (6-9). Guided imagery techniques reduce cognitive, emotional stress, and fatigue (10). In particular, a structured guided imagery disc recorded in advance can be used with positive guided sentences, music, and breathing and relaxation training. This technique is easy, convenient, and not restricted by the activity levels of patients. Relaxation with guided imagery techniques has been applied to cancer patients for several years and has been proved to be useful in relieving the adverse side effects of chemotherapy, such as nausea, vomiting, anxiety, and depression (7, 8, 10-12). Most related studies have examined the effect of relaxation and guided imagery after 3 to 12 weeks. However, patients typically experience the most discomfort 7 to 10 days after receiving chemotherapy because of its side effects.
Several studies have focused on the efficacy of relaxation with guided imagery techniques in controlling physical and psychological distress symptoms (7, 11-13). Serra et al. (14) evaluated the effect of guided imagery on patients undergoing radiation therapy for breast cancer. The results showed a positive effect of guided imagery. Improving the overall care for patients with breast cancer supports the value of incorporating the practices of integrative oncology into standard practice (14).
However, the effects of short-term intervention used in the current practice have seldom been discussed or reported. Therefore, the present study explored the effects of short-term relaxation with guided imagery on breast cancer patients. Our findings can serve as reference for the future care of breast cancer patients to increase the use of these techniques and to improve clinical timeliness.
2. Objectives
This study aimed to explore the effect of relaxation with guided imagery on breast cancer patients.
3. Patients and Methods
This study used a two-group, pretest-posttest, quasi-experimental design to examine the effectiveness of relaxation with guided imagery. The study period was from 2011 to 2012. Patients were randomly assigned to the experimental or the control group. Both groups received chemotherapy self-care education, but the experimental group also received training in relaxation with guided imagery. Each patient in the experimental group received 1 h of relaxation with guided imagery training before chemotherapy and a compact disc (CD) for performing relaxation with guided imagery 20 minutes daily at home for 7 days after chemotherapy. The patients in the control group did not receive guided imagery. The hospital anxiety and depression scale (HADS) and the symptom distress scale (SDS) were administered to the patients in both groups to collect data on symptoms of distress, depression, and anxiety. We completed two questionnaires by conducting face-to-face interviews with patients before chemotherapy and within 10 days after chemotherapy. Each questionnaire was completed in approximately 15 minutes.
MacKay Memorial Hospital Tamshui branch is a private hospital that has 1549 beds. A total of 129 patients were eligible among the 655 identified to have been treated in the period of 2011 to 2012. Among the eligible patients, 28 deaths were recognized and 35 were inaccessible. Accordingly, the population available for research was 66 women. A convenience sample random sampling approach was used to recruit participants from one medical center (MacKay Memorial Hospital Tamshui Branch) in Taiwan. All participants were breast cancer patients.
Patients who (a) were older than 20 years, (b) had the ability to communicate in Chinese, (c) and received cyclophosphamide, epirubcin, and 5-FU (CEF) chemotherapy for the first time were eligible for inclusion. Power analysis was used to detect the significant difference in the anxiety scores (power at 0.80; alpha at 0.05) of patients. In the study, the sample size was estimated by a pilot study on 20 participants to test the mean and standard deviation (SD) of the anxiety scores. In the experimental and control groups, these anxiety scores were 5.24 (± 2.10) and 4.89 (± 1.91), respectively. We calculated that each group required 30 participants. We randomly assigned 66 subjects to the experimental group (n = 33) and the control group (n = 33). One of the experimental participants who had not been discharged was excluded.
Before the study was initiated, approval was obtained from the ethics committee of MacKay memorial hospital (ID 12MMHIS062), where the study was conducted. All participants were informed about the aims of the study, and they provided their informed consent. The participants were informed that they could withdraw from the study at any time and that all information that they provided would be kept confidential.
Data were collected using the Chinese versions of the HADS and SDS, which were modified from similar research surveys (15-18). Demographic (e.g., age, education, marital status, religion, and employment status) and clinical information (e.g., operation, cancer stage, and previous chemotherapy) were also collected. The HADS, which was developed by Zigmond and Snaith, is used to screen for depression and anxiety in cancer patients (19). The English version of the HADS was translated to Chinese by Leung and was used in the present study; its norm and validation had been previously testified (20). This version consists of seven anxiety items and seven depression items that are rated using four grades: no problem to very serious (0 - 3). The scale was adapted to each patient’s narrative experience, and a higher score indicates higher levels of anxiety and depression (21). Bjelland et al. (2002) conducted a systematic review of many studies and identified a cutoff point of 8/21 for anxiety or depression. The Cronbach’s alpha of the HADS was 0.81 (21).
The SDS, which was developed by Lai et al. (22), is used to measure the degree of patient discomfort during chemotherapy. This scale comprises 23 items that are rated using five grades: no problem to very serious (0 - 4). A higher score indicates a higher number of distress symptoms. The Cronbach’s alpha of the SDS (Chinese version) was 0.89 - 0.91 (22). The Cronbach’s alpha of the SDS (the study) was 0.82.
The relaxation with guided imagery CD was produced by the republic of living adjustment compassion corporation in Taiwan. The training includes guidance in imagining a particular language guide, muscle relaxation and deep breathing exercises, and gradually relaxing the muscles from the head to the soles of the feet. Three physicians and two psychiatric therapists reviewed the relaxation with guided imagery CD preceding the start of the study. Moreover, the researcher consulted some anxiety and depression patients for suggestions. Each patient in the experimental group received 1 h of relaxation with guided imagery training before chemotherapy and 20 min daily at home for 7 days after chemotherapy.
3.1. Statistical Analysis
Data were analyzed using SPSS 17.0 for Windows (SPSS, Inc., Chicago, IL, USA) to perform chi-square tests, Student’s t tests, paired t tests, generalized estimating equation (GEE) analysis, and an independent sample t test and to calculate the Pearson product-moment correlations. All statistical tests were two-sided with P values < 0.05 considered as significant. We used the Kolmogorov–Smirnov test to determine whether a normal distribution exists among the sample. We substituted the individuals’ mean score of the HADS and SDS for the missing data of these questionnaires.
4. Results
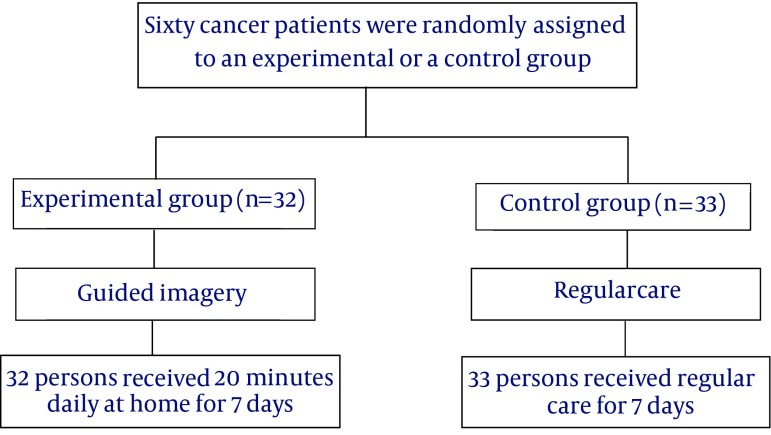
Thirty-two patients were assigned in group 1 and 33 patients in group 2 for analysis (Figure 1). A description of the study participants is presented in Table 1. The average ages of the control group and the experimental group were 52.3 and 49.3 years, respectively. Among the participants in the control group, 75.8% were married, 63.6% were unemployed, 81.8% had a junior college or lower educational level, 93.9% identified with a religion, and 69.7% had undergone cancer surgery. Among the participants in the experimental group, 56.2% were married, 50% were unemployed, 50% had a junior college or lower educational level, 50% had a university or higher educational level, 87.5% identified with a religion, and 65.6% had undergone post cancer surgery. No significant differences were found between the two groups regarding marriage, work, religion, and surgery. The educational levels between the two groups were significantly different (P < 0.01).
Figure 1. Flow Chart.
Table 1. Demographic Characteristics (N = 65)a.
| Variables | Experimental (n = 32) | Control (n = 33) | χ2 | P |
|---|---|---|---|---|
| Age, y | 49.28 ± 9.62 | 52.27 ± 11.58 | 0.26 | |
| Marital status | 0.41 | 0.52 | ||
| Single | 14 (43.8) | 8 (24.2) | ||
| Married | 18 (56.2) | 25 (75.8) | ||
| Work | 0.74 | 0.39 | ||
| No | 16(50) | 21 (63.6) | ||
| Yes | 16 (50) | 12 (36.4) | ||
| Education | 10.69 | .001** | ||
| Junior college or less | 16 (50) | 27(81.8) | ||
| University or above | 16 (50) | 6 (18.2) | ||
| Religion | 0.22 | 0.64 | ||
| No | 4 (12.5) | 2 (6.1) | ||
| Yes | 28 (87.5) | 31 (93.9) | ||
| Surgery | 3.19 | 0.2 | ||
| No | 11 (34.4) | 10 (30.3) | ||
| Yes | 21 (65.6) | 23 (69.7) | ||
| Stage of disease | 0.31 | 0.58 | ||
| Early stage | 27 (84.4) | 33 (100) | ||
| Late stage | 5 (15.6) | - |
aData are presented as mean ± SD or No. (%).
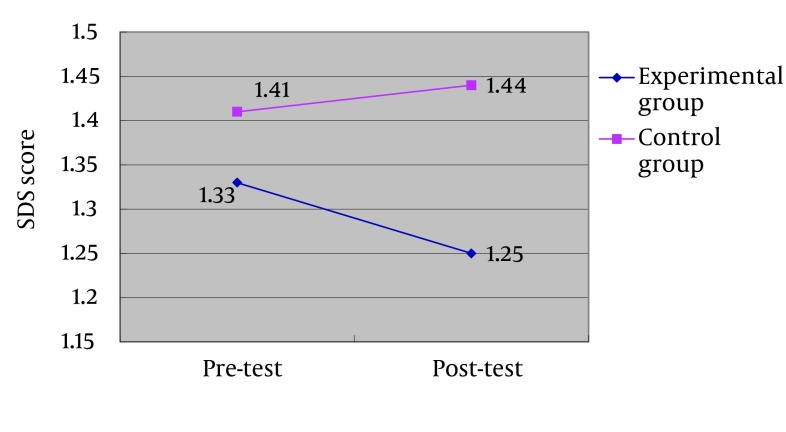
In our study, the SDS scores of the participants before chemotherapy were 1.33 and 1.44 in the experimental group and in the control group, respectively. According to the results of a pretest-posttest comparison in both groups, the patients in the control group experienced significant increase in nausea (P < 0.05), vomiting (P < 0.05), appetite loss (p < 0.05), constipation (p < 0.05), abdominal distension (P <0.05), and heartburn (P < 0.05) between the pretest and the posttest. By contrast, the experimental group exhibited a significant decrease between the pretest and the posttest in insomnia (P < 0.05), pain (P < 0.05), restlessness (P < 0.05), inability to concentrate (P < 0.05), numbness (P < 0.05), anxiety (p < 0.00), and depression (P < 0.00) (Table 2).
Table 2. Differences in the SDS and HADS Between the Pretest and the Posttest in Each Group (N = 65).
| Variables | Experimental (n = 32) | Control (n = 33) | ||||||
|---|---|---|---|---|---|---|---|---|
| Pretest | Posttest | Differences (posttest-pretest) | T | Pretest | Posttest | Differences (posttest–pretest) | T | |
| Symptom distress | 1.33 ± 0.31 | 1.25 ± 0.19 | -0.09 ± 0.24 | 1.91 | 1.41 ± 0.22 | 1.44 ± 0.22 | 0.06 ± 0.28 | -0.8 |
| Nausea | 1.38 ± 0.66 | 1.44 ± 0.62 | 0.06 ± 0.72 | -0.5 | 1.33 ± 0.54 | 1.58 ± 0.61 | 0.24 ± 0.56 | -2.5 a |
| Vomiting | 1.09 ± 0.30 | 1.16 ± 0.45 | 0.06 ± 0.50 | -0.7 | 1.06 ± 0.24 | 1.33 ± 0.54 | 0.27 ± 0.63 | -2.5a |
| Xerostomia | 1.75 ± 0.84 | 1.78 ± 0.66 | 0.03 ± 0.74 | -0.2 | 1.70 ± 0.73 | 1.70 ± 0.73 | 0.00 ± 0.90 | 0 |
| Decreased appetite | 1.44 ± 0.72 | 1.50 ± 0.72 | 0.06 ± 0.56 | -0.6 | 1.42 ± 0.71 | 1.70 ± 0.77 | 0.27 ± 0.63 | -2.5 a |
| Mucositis | 1.16 ± 0.45 | 1.09 ± 0.30 | -0.06 ± 0.56 | 0.63 | 1.12 ± 0.33 | 1.06 ± 0.48 | -0.06 ± 0.50 | 0.7 |
| Dysphagia | 1.03±.18 | 1.03 ± 0.18 | 0.00 ± 0.25 | 0 | 1.12 ± 0.42 | 1.00 ± 0.00 | -0.12 ± 0.42 | 1.68 |
| Constipation | 1.28 ± 0.52 | 1.38 ± 0.61 | 0.09 ± 0.69 | -0.8 | 1.42 ± 0.71 | 1.82 ± 1.07 | 0.39 ± 1.00 | -2.3 a |
| Diarrhea | 1.06 ± 0.25 | 1.06 ± 0.35 | 0.00 ± 0.25 | 0 | 1.18 ± 0.39 | 1.27 ± 0.57 | 0.09 ± 0.52 | -1 |
| Insomnia | 1.84 ± 1.11 | 1.50 ± 0.62 | -0.34 ± 0.83 | 2.35a | 1.94 ± 1.12 | 2.09 ± 1.23 | 0.15 ± 1.12 | -0.8 |
| Pain | 1.81 ± 0.78 | 1.53 ± 0.57 | -0.28 ± 0.58 | 2.74a | 1.91 ± 0.88 | 1.79 ± 0.86 | -0.12 ± 1.11 | 0.63 |
| Fatigue | 1.63 ± 0.79 | 1.53 ± 0.62 | -0.09 ± 0.64 | 0.83 | 2.15 ± 0.80 | 1.94 ± 0.61 | -0.21 ± 0.78 | 1.56 |
| Dyspnea | 1.13 ± 0.42 | 1.03 ± 0.18 | -0.09 ± 0.390 | 1.36 | 1.18 ± 0.53 | 1.15 ± 0.36 | -0.03 ± 0.53 | 0.33 |
| Chest tightness | 1.22 ± 0.42 | 1.13 ± 0.34 | -0.09 ± 0.39 | 1.36 | 1.33 ± 0.60 | 1.33 ± 0.54 | 0.00 ± 0.61 | 0 |
| Cough | 1.25 ± 0.44 | 1.19 ± 0.40 | -0.06 ± 0.35 | 1 | 1.33 ± 0.65 | 1.15 ± 0.44 | -0.18 ± 0.58 | 1.79 |
| Abdominal distension | 1.28 ± 0.63 | 1.13 ± 0.34 | -0.16 ± 0.63 | 1.41 | 1.18 ± 0.47 | 1.42 ± 0.61 | 0.24 ± 0.50 | -2.8 b |
| Heartburn | 1.09 ± 0.53 | 1.22 ± 0.49 | 0.13 ± 0.42 | -1.7 | 1.15 ± 0.36 | 1.39 ± 0.66 | 0.24 ± 0.66 | -2.1a |
| Restless | 1.53 ± 0.67 | 1.19 ± 0.40 | -0.34 ± 0.70 | 2.78 a | 1.55 ± 0.62 | 1.45 ± 0.71 | -0.09 ± 0.84 | 0.62 |
| Inattention | 1.41 ± 0.67 | 1.13 ± 0.42 | -0.28 ± 0.63 | 2.51 a | 1.55 ± 0.79 | 1.52 ± 0.67 | -0.03 ± 0.68 | 0.26 |
| Depression | 1.56 ± 0.72 | 1.16 ± 0.37 | -0.41 ± 0.67 | 3.46 b | 1.45 ± 0.71 | 1.42 ± 0.79 | -0.03 ± 0.68 | 0.26 |
| Numbness | 1.81 ± 0.86 | 1.44 ± 0.67 | -0.38 ± 0.79 | 2.68 a | 1.42 ± 0.61 | 1.42 ± 0.56 | 0.00 ± 0.61 | 0 |
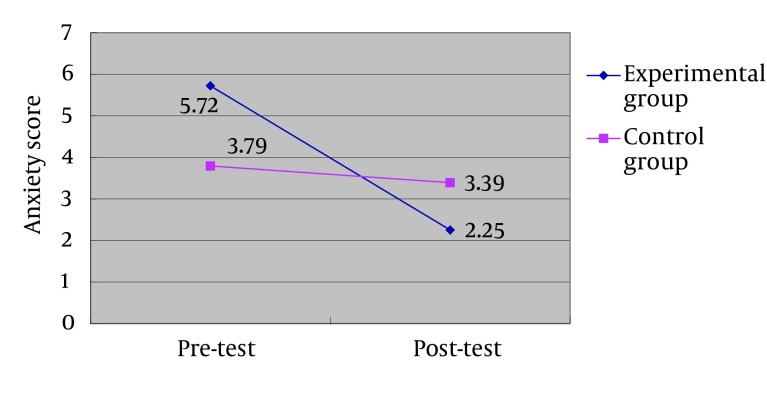
| Anxiety | 5.72 ± 3.48 | 2.25 ± 1.80 | -3.56 ± 2.94 | 6.46 b | 3.79 ± 2.96 | 3.39 ± 3.23 | -0.39 ± 2.42 | 0.93 |
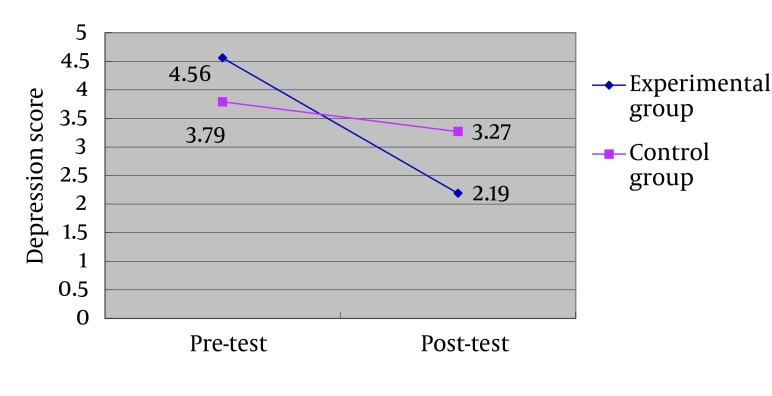
| Depression | 4.56 ± 3.05 | 2.19 ± 1.49 | -2.38 ± 2.70 | 4.98 b | 3.79 ± 2.53 | 3.27 ± 2.13 | -0.52 ± 1.99 | 1.49 |
aP < 0.05.
bP < 0.01.
We observed significant treatment effects of relaxation with guided imagery on SDS and HADS among breast cancer patients undergoing first-time CEF chemotherapy. A GEE was used to adjust for the effects of heterogeneity in education. Significant differences were found between the two groups in overall symptom distress (P < 0.05) and in specific physical symptoms, namely, insomnia (P < 0.05), abdominal distension (P < 0.00), depression (P < 0.05), and numbness (P <0.05). Significant differences were also observed in psychological symptoms, namely, anxiety (P < 0.00) and depression (P < 0.00) (Table 3) (Figures 2 - 4).
Table 3. Effectiveness of Relaxation and Guided Imagery in SDS and HADS (N = 65)a.
| Variables | β | SE | 95% Wald CI | P |
|---|---|---|---|---|
| Symptom distress | 0.11 | 0.06 | -0.22 ~ 0.00 | 0.04b |
| Nausea | 0.18 | 0.16 | -0.49 ~ 0.13 | 0.25 |
| Vomiting | 0.21 | 0.14 | -0.48 ~ 0.06 | 0.13 |
| Xerostomia | -0.03 | 0.2 | -0.36 ~ 0.43 | 0.88 |
| Decreased appetite | 0.21 | 0.15 | -0.50 ~ 0.08 | 0.15 |
| Mucositis | 0 | 0.13 | -0.26 ~ 0.25 | 0.99 |
| Dysphagia | -0.12 | 0.08 | -0.04 ~ 0.29 | 0.15 |
| Trismus | 0.03 | 0.03 | -0.09 ~ 0.03 | 0.31 |
| Constipation | 0.3 | 0.21 | -0.71 ~ 0.11 | 0.15 |
| Diarrhea | 0.09 | 0.1 | -0.29 ~ 0.11 | 0.36 |
| Dysuria | 0.06 | 0.04 | -0.14 ~ 0.02 | 0.15 |
| Insomnia | 0.5 | 0.24 | -0.97 ~ -0.03 | 0.04b |
| Pain | 0.16 | 0.22 | -0.58 ~ 0.26 | 0.46 |
| Fatigue | -0.12 | 0.17 | -0.22 ~ 0.46 | 0.5 |
| Drowsiness | -0.18 | 0.17 | -0.16 ~ 0.52 | 0.3 |
| Dyspnea | 0.06 | 0.11 | -0.29 ~ 0.16 | 0.58 |
| Chest tightness | 0.09 | 0.13 | -0.34 ~ 0.15 | 0.45 |
| Cough | -0.12 | 0.14 | -0.67 ~ -0.13 | 0.32 |
| Abdominal distension | 0.4 | 0.14 | -0.38 ~ 0.15 | 0.001c |
| Heartburn | 0.12 | 0.14 | -0.67 ~ -0.13 | 0.39 |
| Restless | 0.25 | 0.19 | -0.62 ~ 0.12 | 0.18 |
| Inability to concentrate | 0.25 | 0.16 | -0.57 ~ 0.07 | 0.12 |
| Depression | 0.38 | 0.16 | -0.70 ~ -0.05 | 0.02b |
| Numbness | 0.38 | 0.17 | -0.72 ~ -0.04 | 0.03b |
| Anxiety | 3.08 | 0.67 | -4.39 ~ -1.76 | 0.001c |
| Depression | 1.86 | 0.58 | -3.00 ~ -0.72 | 0.001c |
aGeneralized Estimating Equations (GEE) (GEE) adjusted education, Group (Control group = reference).
bP < 0.05.
cP < 0.01.
Figure 2. Results of the SDS Score (Mean) Between the Pretest and the Posttest in Each Group.
Figure 4. Results of the Depression Score (Mean) Between the Pretest and the Posttest in Each Group.
Figure 3. Results of the Anxiety Score (Mean) Between the Pretest and the Posttest in Each Group.
The factors affecting the effectiveness of relaxation with guided imagery indicated that relaxation with guided imagery relieved physical and mental discomfort. No significant differences in marriage status, employment, education, religion, surgery, and disease stage were observed. Age was moderately correlated with the effect of guided imagery on anxiety and depression (r = 0.49, P < 0.05; r = 0.41, P < 0.05). These results indicated that relaxation with guided imagery relieved anxiety and depression to a great extent in relatively older populations (Table 4).
Table 4. Related Factors Affecting the Effectiveness of Relaxation and Guided Imagery in SDS and HADS (N = 32)a.
| Variables | n | Symptom Distress | Anxiety | Depression | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | t/r | P | Mean | t/r | P | Mean | t/r | P | ||
| Age, y | 32 | -0.09 ± 0.24 | -0.11 | 0.56 | -3.56 ± 2.94 | 0.49 | 0.01 b | -2.38 ± 2.7 | 0.41 | 0.02 c |
| Marital status | 0.27 | 0.79 | 0.46 | 0.65 | -1 | 0.92 | ||||
| Single | 14 | -0.08 ± 0.19 | -3.29 ± 2.4 | -2.43± 2.34 | ||||||
| Married | 18 | -0.1 ± 0.28 | -3.78 ± 3.35 | -2.33 ± 3.01 | ||||||
| Job | 0.22 | 0.83 | 1.74 | 0.09 | 0.52 | 0.61 | ||||
| No | 16 | -0.08 ± 0.22 | -2.69 ± 2.6 | -2.13 ± 2.25 | ||||||
| Yes | 16 | -0.1 ± 0.27 | -4.44 ± 3.08 | -2.63 ± 3.14 | ||||||
| Education | -0.27 | 0.78 | -0.48 | 0.64 | -0.39 | 0.7 | ||||
| Junior college or less | 16 | -0.11 ± 0.23 | -3.81 ± 3.04 | -2.56 ± 2.85 | ||||||
| University or above | 16 | -0.08 ± 0.26 | -3.31 ± 2.92 | -2.19 ± 2.61 | ||||||
| Religion | 1.55 | 0.13 | 1.34 | 0.19 | 1.09 | 0.28 | ||||
| No | 4 | 0.08 ± 0.14 | -1.75 ± 3.3 | -1 ± 3.83 | ||||||
| Yes | 28 | -0.12 ± 0.25 | -3.82 ± 2.86 | -2.57 ± 2.53 | ||||||
| Surgery | -0.57 | 0.58 | 0.52 | 0.6 | -0.67 | 0.51 | ||||
| No | 11 | -0.13 ± 0.33 | -3.18 ± 3.06 | -2.82 ± 2.56 | ||||||
| Yes | 21 | -0.08 ± 0.19 | -3.76 ± 2.93 | -2.14 ± 2.8 | ||||||
| Stage of disease | 1.44 | 0.16 | . | 1.5 | 0.15 | |||||
| Early stage | 27 | -0.07 ± 2.4 | -3.44 ± 2.89 | 0.52 | 0.61 | -2.07 ± 2.34 | ||||
| Late stage | 5 | -0.23 ± 0.38 | -4.2 ± 3.49 | -4 ± 4.12 | ||||||
aData are presented as mean ± SD.
bP < 0.01.
cP < 0.05.
5. Discussion
The results of this study indicates that 20 minutes of daily home relaxation with guided imagery for 7 days has a significant effect on overall symptoms of distress, insomnia, bloating, numbness, anxiety, and depression on breast cancer patients undergoing first-time chemotherapy. By contrast, the control group experienced a significant increase in nausea, vomiting, appetite loss, constipation, abdominal distension, and heartburn between the pretest and the posttest. Patients who received relaxation with guided imagery had a relatively low score of physical and psychological distress after chemotherapy, thus suggesting that 20 min of daily relaxation with guided imagery for 7 days enhanced the control of physical and psychological distress symptoms. This result is supported by those of previous studies that focused on the long-term effect of relaxation with guided imagery (7, 12, 23-28).
Relaxation may exert beneficial effects by diverting patients’ attention from the side effects of chemotherapy distress, relieving muscle tension, and guiding relaxing thoughts using guided imagery. The combination of relaxation and guided imagery may benefit patients because it is effective in reducing post chemotherapy side effects. Previous studies have demonstrated that these types of attentional diversion strategies are effective in reducing physical and psychological symptoms of distress and in improving pain control (29).
The result shows that age is correlated with the effect of guided imagery on anxiety and depression. Therefore, relaxation with guided imagery relieves anxiety and depression to a great extent in older people. Guided imagery can indeed be used for the elderly.
We hypothesize that one week of relaxation with guided imagery can significantly reduce physical and psychological distress. However, many other factors such as the type of treatment, intervention execution time, manner of treatment and treatment times, and physical and psychological distress symptoms may have affected the results. The findings of this study provide evidence of the effectiveness of relaxation with guided imagery in controlling physical and psychological symptom distress after chemotherapy among Taiwanese breast cancer patients.
The findings confirm the observations made in a previous study that oncology nurses can teach relaxation with guided imagery techniques, which patients can easily learn and apply (30). These interventions can aid health professionals in developing and taking responsibility for clinically managing the adverse effects of chemotherapy. Nurses who are closely associated with patients and remain with them longer than any other health professionals feel frustrated with their inability to assist patients in coping with the side effects of chemotherapy. Relaxation with guided imagery can increase the sphere of competence and skills of oncology nursing staff and enable oncology nurses to apply holistic models of health care (28).
The results of our study suggest that 20 minutes of daily relaxation at home with guided imagery for 7 days after chemotherapy can reduce overall symptoms of distress, insomnia, bloating, numbness, and other symptoms of depression and distress. Moreover, relaxation with guided imagery relieves anxiety and depression related to chemotherapy. Older age is positively associated with the effectiveness of relaxation with guided imagery in alleviating anxiety and depression. In addition, previous chemotherapy experiences negatively affect the effectiveness of relaxation with guided imagery in reducing anxiety.
Daily relaxation at home involving guided imagery is beneficial to patients as it can help patients cope with overall symptom distress, depression, and distress and be useful for breast cancer patients during chemotherapy. The main limitations of this study are the use of only hospitalized patients, the small sample size, and the short duration. Therefore, the findings cannot be generalized to the general population. Further research should involve using a larger sample size and additional measurements, biological indicators (e.g., salivary cortisol), and immunocytochemistry to improve measurement accuracy and the generalizability of the findings.
Acknowledgments
We would like to thank the participants from the oncology ward of MacKay memorial hospital for their support and cooperation.
Footnotes
Authors’ Contribution:Shu-Fen Chen: data collection and designing and writing the manuscript, Hsiu-Ho Wang: writing the manuscript and serving as a counselor, Hsing-Yu Yang: data analysis, Ue-Lin Chung: supervisor and as well as design.
References
- 1.DeSantis C, Ma J, Bryan L, Jemal A. Breast cancer statistics, 2013. A Cancer J Clin. 2014;64(1):52–62. doi: 10.3322/caac.21203. [DOI] [PubMed] [Google Scholar]
- 2.Park IH, Lee KS, Ro J. Effects of second and subsequent lines of chemotherapy for metastatic breast cancer. Clin Breast Cancer. 2015;15(1):e55–62. doi: 10.1016/j.clbc.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 3.Olver IN, Eliott JA, Koczwara B. A qualitative study investigating chemotherapy-induced nausea as a symptom cluster. Support Care Cancer. 2014;22(10):2749–56. doi: 10.1007/s00520-014-2276-2. [DOI] [PubMed] [Google Scholar]
- 4.Zainal NZ, Nik-Jaafar NR, Baharudin A, Sabki ZA, Ng CG. Prevalence of depression in breast cancer survivors: a systematic review of observational studies. Asian Pac J Cancer Prev. 2013;14(4):2649–56. doi: 10.7314/apjcp.2013.14.4.2649. [DOI] [PubMed] [Google Scholar]
- 5.Kim IR, Cho J, Choi EK, Kwon IG, Sung YH, Lee JE, et al. Perception, attitudes, preparedness and experience of chemotherapy-induced alopecia among breast cancer patients: a qualitative study. Asian Pac J Cancer Prev. 2012;13(4):1383–8. doi: 10.7314/apjcp.2012.13.4.1383. [DOI] [PubMed] [Google Scholar]
- 6.Gaston-Johansson F, Fall-Dickson JM, Nanda JP, Sarenmalm EK, Browall M, Goldstein N. Long-term effect of the self-management comprehensive coping strategy program on quality of life in patients with breast cancer treated with high-dose chemotherapy. Psychooncology. 2013;22(3):530–9. doi: 10.1002/pon.3031. [DOI] [PubMed] [Google Scholar]
- 7.Nazik E, Nazik H, Api M, Kale A, Aksu M. Complementary and alternative medicine use by gynecologic oncology patients in Turkey. Asian Pac J Cancer Prev. 2012;13(1):21–5. doi: 10.7314/apjcp.2012.13.1.021. [DOI] [PubMed] [Google Scholar]
- 8.Sait KH, Anfinan NM, Eldeek B, Al-Ahmadi J, Al-Attas M, Sait HK, et al. Perception of patients with cancer towards support management services and use of complementary alternative medicine--a single institution hospital-based study in Saudi Arabia. Asian Pac J Cancer Prev. 2014;15(6):2547–54. doi: 10.7314/apjcp.2014.15.6.2547. [DOI] [PubMed] [Google Scholar]
- 9.Wang HH, Chung UL. Use of Complementary and Alternative Medicine Among Breast Cancer Survivors in Taiwan. Asian Pac J Cancer Prevent. 2012;13(9):4789–92. doi: 10.7314/apjcp.2012.13.9.4789. [DOI] [PubMed] [Google Scholar]
- 10.Lee MH, Kim DH, Yu HS. The effect of guided imagery on stress and fatigue in patients with thyroid cancer undergoing radioactive iodine therapy. Evid Based Complement Alternat Med. 2013;2013:130324. doi: 10.1155/2013/130324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bigham E, McDannel L, Luciano I, Salgado-Lopez G. Effect of a Brief Guided Imagery on Stress. Biofeedback. 2014;42(1):28–35. doi: 10.5298/1081-5937-42.1.07. [DOI] [Google Scholar]
- 12.Isa MR, Moy FM, Abdul Razack AH, Zainuddin ZM, Zainal NZ. Impact of applied progressive deep muscle relaxation training on the level of depression, anxiety and stress among prostate cancer patients: a quasi-experimental study. Asian Pac J Cancer Prev. 2013;14(4):2237–42. doi: 10.7314/apjcp.2013.14.4.2237. [DOI] [PubMed] [Google Scholar]
- 13.Hoffman CJ, Ersser SJ, Hopkinson JB, Nicholls PG, Harrington JE, Thomas PW. Effectiveness of mindfulness-based stress reduction in mood, breast- and endocrine-related quality of life, and well-being in stage 0 to III breast cancer: a randomized, controlled trial. J Clin Oncol. 2012;30(12):1335–42. doi: 10.1200/JCO.2010.34.0331. [DOI] [PubMed] [Google Scholar]
- 14.Serra D, Parris CR, Carper E, Homel P, Fleishman SB, Harrison LB, et al. Outcomes of guided imagery in patients receiving radiation therapy for breast cancer. Clin J Oncol Nurs. 2012;16(6):617–23. doi: 10.1188/12.CJON.617-623. [DOI] [PubMed] [Google Scholar]
- 15.Teunissen SC, de Graeff A, Voest EE, de Haes JC. Are anxiety and depressed mood related to physical symptom burden? A study in hospitalized advanced cancer patients. Palliat Med. 2007;21(4):341–6. doi: 10.1177/0269216307079067. [DOI] [PubMed] [Google Scholar]
- 16.Genc F, Tan M. Symptoms of patients with lung cancer undergoing chemotherapy and coping strategies. Cancer Nurs. 2011;34(6):503–9. doi: 10.1097/NCC.0b013e31820b7024. [DOI] [PubMed] [Google Scholar]
- 17.Tang PL, Wang C, Hung MF, Lin HS. Assessment of symptom distress in cancer patients before and after radiotherapy. Cancer Nurs. 2011;34(1):78–84. doi: 10.1097/NCC.0b013e3181f04ac8. [DOI] [PubMed] [Google Scholar]
- 18.Carey M, Noble N, Sanson-Fisher R, MacKenzie L. Identifying psychological morbidity among people with cancer using the Hospital Anxiety and Depression Scale: time to revisit first principles? Psychooncology. 2012;21(3):229–38. doi: 10.1002/pon.2057. [DOI] [PubMed] [Google Scholar]
- 19.Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatrica Scandinavic. 1983;67(6):361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 20.Bikmoradi A, Seifi Z, Poorolajal J, Araghchian M, Safiaryan R, Oshvandi K. Effect of inhalation aromatherapy with lavender essential oil on stress and vital signs in patients undergoing coronary artery bypass surgery: A single-blinded randomized clinical trial. Complement Ther Med. 2015;23(3):331–8. doi: 10.1016/j.ctim.2014.12.001. [DOI] [PubMed] [Google Scholar]
- 21.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. J Psycho Res. 2002;52(2):69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 22.Lai YH, Chang JT, Keefe FJ, Chiou CF, Chen SC, Feng SC, et al. Symptom distress, catastrophic thinking, and hope in nasopharyngeal carcinoma patients. Cancer Nurs. 2003;26(6):485–93. doi: 10.1097/00002820-200312000-00008. [DOI] [PubMed] [Google Scholar]
- 23.Yang XL, Li HH, Hong MH, Kao HS. The effects of Chinese calligraphy handwriting and relaxation training in Chinese Nasopharyngeal Carcinoma patients: a randomized controlled trial. Int J Nurs Stud. 2010;47(5):550–9. doi: 10.1016/j.ijnurstu.2009.10.014. [DOI] [PubMed] [Google Scholar]
- 24.Eremin O, Walker MB, Simpson E, Heys SD, Ah-See AK, Hutcheon AW, et al. Immuno-modulatory effects of relaxation training and guided imagery in women with locally advanced breast cancer undergoing multimodality therapy: a randomised controlled trial. Breast. 2009;18(1):17–25. doi: 10.1016/j.breast.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 25.Bergerot CD, Clark KL, Nonino A, Waliany S, Buso MM, Loscalzo M. Course of distress, anxiety, and depression in hematological cancer patients: Association between gender and grade of neoplasm. Palliat Support Care. 2015;13(2):115–23. doi: 10.1017/S1478951513000849. [DOI] [PubMed] [Google Scholar]
- 26.Lengacher CA, Johnson-Mallard V, Post-White J, Moscoso MS, Jacobsen PB, Klein TW, et al. Randomized controlled trial of mindfulness-based stress reduction (MBSR) for survivors of breast cancer. Psychooncology. 2009;18(12):1261–72. doi: 10.1002/pon.1529. [DOI] [PubMed] [Google Scholar]
- 27.Lengacher CA, Kip KE, Barta M, Post-White J, Jacobsen PB, Groer M, et al. A pilot study evaluating the effect of mindfulness-based stress reduction on psychological status, physical status, salivary cortisol, and interleukin-6 among advanced-stage cancer patients and their caregivers. J Holist Nurs. 2012;30(3):170–85. doi: 10.1177/0898010111435949. [DOI] [PubMed] [Google Scholar]
- 28.Molassiotis A, Yung HP, Yam BM, Chan FY, Mok TS. The effectiveness of progressive muscle relaxation training in managing chemotherapy-induced nausea and vomiting in Chinese breast cancer patients: a randomised controlled trial. Support Care Cancer. 2002;10(3):237–46. doi: 10.1007/s00520-001-0329-9. [DOI] [PubMed] [Google Scholar]
- 29.Kwekkeboom KL, Hau H, Wanta B, Bumpus M. Patients' perceptions of the effectiveness of guided imagery and progressive muscle relaxation interventions used for cancer pain. Complement Ther Clin Pract. 2008;14(3):185–94. doi: 10.1016/j.ctcp.2008.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Boehm LB, Tse AM. Application of guided imagery to facilitate the transition of new graduate registered nurses. J Contin Educ Nurs. 2013;44(3):113–9. doi: 10.3928/00220124-20130115-16. [DOI] [PMC free article] [PubMed] [Google Scholar]