Preface
Cryptococcus neoformans is generally considered an opportunistic fungal pathogen because of its tendency to infect immunocompromised individuals, particularly those infected with HIV. However, this view has been challenged by recent discoveries of specialized interactions between the fungus and its mammalian hosts, and by the emergence of the related species Cryptococcus gattii as a primary pathogen of immunocompetent populations. In this Review, we highlight features of cryptococcal pathogens that reveal their adaptation to the mammalian environment. These features include remarkably sophisticated interactions with phagocytic cells to promote intracellular survival, dissemination to the central nervous system and escape, as well as surprising morphological and genomic adaptations such as the formation of polyploid giant cells in the lung.
Fungal pathogens of humans often take advantage of altered host immune status to cause disease. This exploitation of immunocompromised hosts is dramatically illustrated by Cryptococcus neoformans, a pathogen that rose to prominence as the causative agent of cryptococcosis, a life threatening disease that has emerged in parallel with the HIV/AIDS epidemic. Cryptococcosis results from inhalation of fungal cells with subsequent lung infection and pneumonia. In the absence of an effective immune response, the fungus can disseminate to the brain to cause meningoencephalitis with symptoms that include headache, fever, visual problems and altered mental status 1. C. neoformans causes an estimated one million cases of meningoencephalitis globally per year in AIDS patients, leading to approximately 625,000 deaths 2. The bulk of this disease burden is in sub-Saharan Africa, where fatal cases of cryptococcosis may exceed deaths from tuberculosis in some areas 2.
Recently, the link between C. neoformans and immune deficiency has been challenged by the emergence of cryptococcosis in immunocompetent individuals. A variety of C. neoformans, which is now recognized as the distinct species Cryptococcus gattii, is responsible for an ongoing outbreak of infections in otherwise healthy people and animals in Western North America 3–8 (Box 1). Of course, C. neoformans is also capable of infecting immunocompetent people, as demonstrated by the many cases of cryptococcosis documented before the AIDS epidemic 9. The classification of C. gattii and C. neoformans as distinct species is based on phylogenetic studies and the absence of genetic recombination in matings between isolates of each species 8. The emergence of C. gattii as a pathogen of seemingly immunocompetent hosts is particularly striking because this species shares all of the known major C. neoformans virulence traits (Table 1) 10. These include the production of a polysaccharide capsule, formation of the pigment melanin in the cell wall, growth at 37°C and secretion of enzymes such as phospholipase B and urease. The export of virulence factors is mediated in part by extracellular vesicles, sometimes termed “virulence factor delivery bags” (Box 2) 11. The shared properties of these species are somewhat at odds with their host predilections, which indicates a pressing need for a deeper consideration of the mechanisms of cryptococcal virulence and host adaptation.
Box 1. The emergence of Cryptococcus gattii in Western North America.
A dramatic increase in the frequency of C. gattii infections in humans and animals occurred on the east coast of Vancouver Island in British Columbia in 19993. In the subsequent decade, there have been 236 human cases and 19 deaths; in parallel, many cases have occurred in domesticated and wild animals including, curiously, a number of marine mammals 3, 7. C. gattii appears to be spreading beyond British Columbia, or to have a broader distribution than previously appreciated, because there have been ~60 human cases in Oregon and Washington since 2004 5–7, 78. The outbreak is unusual because the fungus was previously found to cause disease mainly in tropical or subtropical regions, rather than temperate regions, and because most of the cases have occurred in people without underlying immunodeficiency.
An extensive collection of C. gattii isolates has been obtained from clinical, veterinary and environmental sources in Western North America 3. Molecular typing has identified four C. gattii genotypes, VGI to VGIV, which may represent cryptic species 3, 4. Of the four types, VGI to VGIII are found in Western North America; the VGII genotype is further divided into the subtypes VGIIa, VGIIb and VGIIc, with VGIIa being the predominant type both in the environment and in patients 3–7. In general, VGIIa shows a high level of virulence in mouse models of cryptococcosis, relative to the other C. gattii genotypes 49, 50, 79.
Table 1.
Major virulence factors and examples of additional functions linked to pathogenesisin C. neoformans
| Major virulence traits |
Description | Refs |
|---|---|---|
| Polysaccharide capsule | The capsule is composed of glucuronxylomannan and galactoxylomannan polysaccharides that are both cell-associated and shed during infection. These polysaccharides have immunomodulatory properties and acapsular mutants are avirulent. Exported mannoproteins are associated with capsule and stimulate the T cell-mediated immune response. | 15, 19, 20, 88 |
| Melanin deposition in the cell wall | The dark pigment, melanin, is synthesized from catecholamine substrates via the activity of copper-dependent laccases. Melanin confers protection against phagocytosis and oxidative killing by macrophages and contributes to extrapulmonary dissemination. | 89– 91 |
| Growth at the mammalian host temperature of 37°C | C. neoformans is relatively thermotolerant compared to many other fungi, and can therefore grow at mammalian body temperatures. Many functions contribute to thermotolerance including components of signaling pathways. | 92, 93 |
| Extracellular enzymes | Several secreted enzymes contribute to virulence. For example, laccases and phospholipase B are located in the cell wall and mediate melanin formation and cell wall integrity, respectively. Phospholipase B also contributes to fungal invasion of host lung tissue and dissemination. Urease catalyzes the hydrolysis of urea to ammonia and carbamate, and this activity enhances the ability of C. neoformans to invade the central nervous system. | 38, 82, 91, 94, 95 |
|
Virulence– related functions |
Description | Refs |
| Resistance to oxidative and nitrosative stress | Cryptococcal cells resist host defenses by producing neutralizing enzymes and additional protective proteins and metabolites. These include superoxide dismutase, a flavohemoglobin denitrosylase, glutathione peroxidase, glutathione reductase, thiol peroxidases, thioredoxins, and trehalose. | 92, 93, 96, 97, 98 |
| Signal transduction pathways | Several signaling pathways contribute to virulence by sensing host conditions, by regulating virulence factor expression and by controlling responses to stress imposed by host temperature and defense mechanisms. These include the cAMP/protein kinase A pathways and mitogen-activated protein kinase (MAPK) pathways for cell wall integrity and stress responses. In addition, the Ca2+ - calcineurin pathway regulates mating, growth at host temperature and virulence. A phosphatidylinositol 3-kinase (PI3K) signaling pathway also regulates melanin formation. | 16, 85, 98, 99 |
| Lipid signaling | Diacylglycerol (DAG) from the sphingolipid pathway activates the transcription factor Atf2 to upregulate expression of the anti-phagocytic protein App1. DAG also activates protein kinase C in the cell wall integrity MAPK pathway to increase melanin formation. | 100 |
| Adaptation to low-oxygen conditions (hypoxia) | The sterol regulatory element binding protein (SREBP) pathway regulates the response to hypoxia, sterol homeostasis and virulence. The pathway also coordinately regulates genes encoding iron and copper uptake functions. | 101 |
| Metabolism and proliferation in the host | Important factors for proliferation in host tissue include enzymes of central carbon metabolism (gluconeogenesis, acetyl-coA synthesis), regulators of capsule and melanin synthesis, and functions to resist phagocytosis. | 77, 90, 102, 103 |
| Mating and sexual development | Mating fertility is associated with virulence in several ways. Cells of the MATα mating type are the most prevalent among clinical and environmental isolates, some MATα strains are more virulent than congenic MATa strains, and mating also controls the formation of infectious spores. | 17, 57, 104 |
| Intracellular trafficking and pH sensing | Virulence is influenced by defects in a variety of intracellular trafficking and subcellular compartment functions, primarily as a result of changes in capsule and melanin formation. These functions include pH sensing, vesicular acidification, vacuolar functions, exocytosis and autophagy. | 15, 85, 86, 99, 105 |
| Iron and copper regulation and uptake | Iron levels influence the expression of uptake functions and all of the major virulence factors via the Cir1 transcription factor. Copper is important for a variety of functions including the multicopper oxidases Cfo1 (iron uptake) and laccase (melanin synthesis). | 14, 106 |
Note that the major virulence factors are shared by C. gattii and it is likely that most of the other virulence-associated functions are conserved between the species.
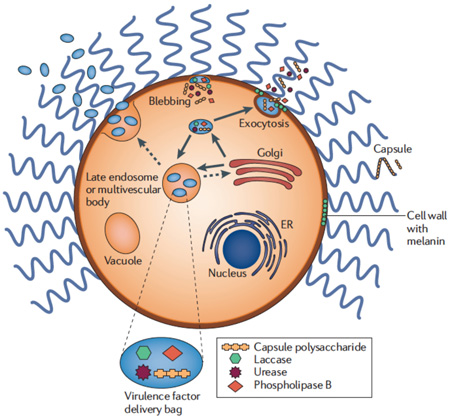
Box 2. Secretion of cryptococcal virulence factors.
The ability of C. neoformans and C. gattii to influence the intracellular environment of macrophages during proliferation, expulsion and transfer between cells is likely dependent on exported fungal factors. Secretion is clearly necessary for cell surface delivery of known virulence factors such as the polysaccharide capsule, the enzyme laccase that synthesizes melanin, and the enzymes phospholipase B and urease. Many of these factors are delivered, at least in part, by membrane bound, extracellular vesicles that have been observed to traverse the cell wall 80–82 (see figure). These so-called “virulence factor delivery bags” may be generated by fusion of multivesicular bodies with the plasma membrane, thus suggesting a role for Golgi-endosomal trafficking, and/or by blebbing from the plasma membrane 11, 15, 81, 82. Although little is known about the intracellular trafficking functions that package virulence factors in vesicles for export, there is some evidence for a role for exocytosis in the export of internally-synthesized capsule polysaccharide and regulation of secretion by the cAMP signaling pathway 15, 83–86. The extracellular vesicles are produced by C. neoformans during infection of the mouse macrophage-like cell line J774.16, and similar vesicles that contain capsule polysaccharide accumulate in the cytoplasm of infected macrophages in vivo and in vitro 43, 81. These phagocytic cells show permeabilization of the phagosomal membrane and it is tempting to speculate that cryptococcal vesicles and/or exported enzymes (e.g., phospholipase B) play a role in this modification 29, 43, 44. The extracellular vesicles from fungal culture supernatants are also internalized by macrophage-like cells (RAW 264.7) and they induced a dose-dependent production of nitric oxide (NO), TNF-α, IL-10, and TGF-β by the cells 87.
In this review, we discuss recent discoveries that support the idea that both C. neoformans and C. gattii use specialized mechanisms to adapt to the mammalian host environment and, therefore, should not be seen as ‘opportunistic’ pathogens. These mechanisms include morphological adaptations at the cellular and subcellular level that may facilitate survival and dissemination in the host. In particular, we review the first detailed studies of morphologically differentiated spores as infectious agents and highlight examples of specialized interactions between the fungi and phagocytic cells. Cryptococcus species may also modify the intracellular environment of macrophages using mechanisms involving the delivery of virulence factors by exported vesicles. Recent studies have also revealed a dramatic morphological adaptation involving the formation of polyploid giant cells, as well as genomic changes involving chromosome copy number variation (disomy) that could influence virulence factor expression and antifungal drug resistance. These mechanisms of adaptation support the classification of C. neoformans and C. gattii as pathogens that cause damage in hosts with weak and normal immune responses, respectively 12. For additional information, readers are referred to several excellent recent reviews for other aspects of cryptococcal virulence, sexual development, signaling, and the emergence of C. gattii 3, 6, 10–20. In addition, two comprehensive books on C. neoformans, C. gattii and cryptococcosis have been published, including a new volume last year 21, 22.
Interactions with phagocytic cells
Spores: long suspected agents of infection
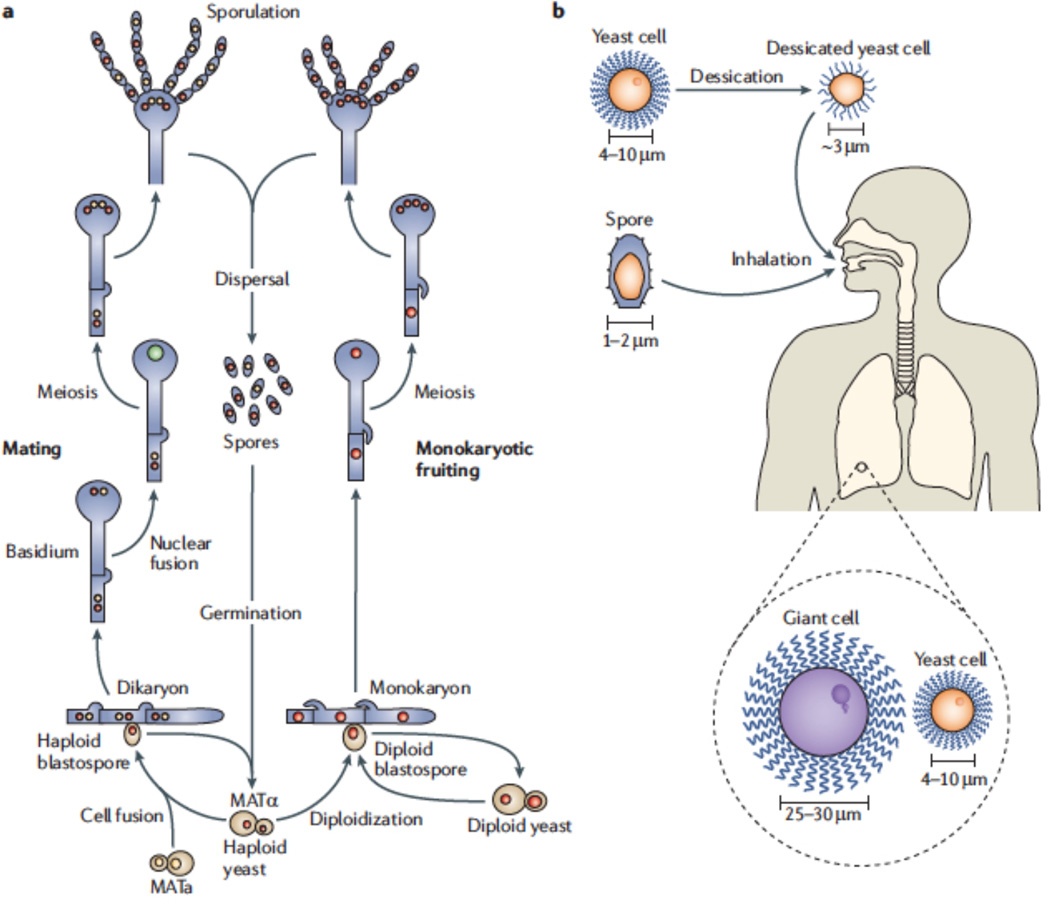
C. neoformans and C. gattii are found in the environment in association with soil, pigeon guano and trees. The cells that are cultured from these sources have a budding, yeast-like morphology and exist in either of two mating types designated MATa and MATα (Figure 1) 17. Mating between MATa and MATα cells generates a filamentous cell type containing nuclei of each parental type, and this dikaryon generates chains of haploid spores following nuclear fusion, meiosis and sporulation 17. Spores can also be generated from sexual reproduction between cells of the MATα mating type. In this case, fusion of cells of the same sex generates a filamentous cell type with nuclei of only the MATα mating type (a monokaryon) and subsequent sexual development generates spores 17, 23. Natural infections generally begin with inhalation of fungal cells and initial pulmonary involvement. Desiccated yeast cells have traditionally been considered the infectious propagules because their small size (< 3 µm compared with 5–10 µm for actively growing yeast cells) would potentially allow deposition deep in the alveoli of the lung 24–26, 28. Similarly, spores have long been suspected to be infectious agents because of their small size (1–2 µm) 24–26, 28 (Figure 1). Given that yeast cells can be more fragile in the environment, spores would seem better suited for both air dispersal and survival. However, spore production has not been observed in nature, although sexual development of the fungus on plants has been demonstrated experimentally 25. Until recently, it was also not possible to test spores for virulence-related properties due to difficulties in separating spores from yeast cells. To overcome this limitation, microdissection and density gradient centrifugation methods have now been employed to separate the cell types, and these approaches should allow spores and their interactions with the host to be characterized 24, 26.
Figure 1. Morphologically distinct cell types contribute to virulence in Cryptococcus neoformans.
Spores and dessicated yeast cells initiate infection upon inhalation. Spores result from either (a) unisexual mating of MATα cells to establish a monokaryotic cell type or (b) mating and cell fusion between cells of opposite (MATa or MATα) mating type and subsequent dikaryon formation. In both cases, sexual development within the filamentous monokaryon or dikaryon results in meiosis and sporulation 13, 17, 57. The spores germinate to produce haploid, yeast-like cells that divide by budding. The yeast cells may become desiccated in the environment such that their small size allows inhalation deep into lung tissue. Germination of spores or vegetative growth of yeast cells in lung tissue results in the proliferation of budding cells and the formation of giant cells in a fraction of the population 30, 55, 58. Note that the cells are not drawn to scale. MAT, mating-type locus.
Purified spores have a thick cell wall and show greater resistance than yeast cells to desiccation, high temperature and oxidative stress 24, 26. The thick spore coat binds to lectins and, surprisingly, to antibodies specific for the capsular polysaccharide glucuronoxylomannan (GXM) that is typically found on yeast cells. Additionally, defects in genes involved in capsule production interfere with spore formation. These results are interesting because the capsule is required for virulence, capsule enlargement occurs in response to host conditions (e.g., elevated CO2 and reduced iron levels) and conditions for sexual development generally do not induce capsule formation 19, 24, 27. In a murine inhalation model of cryptococcosis, spores enriched by micromanipulation or gradient centrifugation are able to cause disease at levels comparable to yeast cells 26, 28. In fact, the spores were quite infectious with a lethal dose as low as 500 cells 26. However, the lungs of mice infected with spores yielded 10-fold fewer fungal cells at three and six days post infection, compared with yeast infections 28. These findings suggest that spores may not resist the innate immune response to the same extent as yeast cells.
It is well established that yeast cells of C. neoformans and C. gattii can survive and proliferate in alveolar macrophages 10, 29. In this context, an evaluation of the interaction between purified spores and phagocytic cells in culture revealed a striking difference from the interactions observed for yeast cells. Spores are readily taken up by murine macrophages or by primary alveolar macrophages in the absence of an opsonin, while yeast cells require prior opsonization 26, 28. Phagocytosis of spores was inhibited by blocking interactions between β-(1,3)-glucan and the pathogen recognition receptor dectin-1, and by blocking CD11b, a component of the leukocyte adhesion receptor CR3 (or CD11b/CD18) 28. Spores rapidly germinate and grow inside phagocytic cells; however, the survival and proliferation of the resulting yeast cells are only possible in the absence of prior activation of the macrophages by lipopolysaccharide and interferon-γ. The observation that spores and yeast cells interact differently with macrophages prompted Botts and Hull to propose that the outcome of infection may be a race between spore germination and activation of the innate immune response 30. They predict that the rate of spore germination may differ for C. neoformans and C. gattii, leading to differential avoidance of initial killing by phagocytic cells as a function of whether the host is immunocompetent or immunocompromised.
Macrophage and monocyte subversion: A strategy for dissemination?
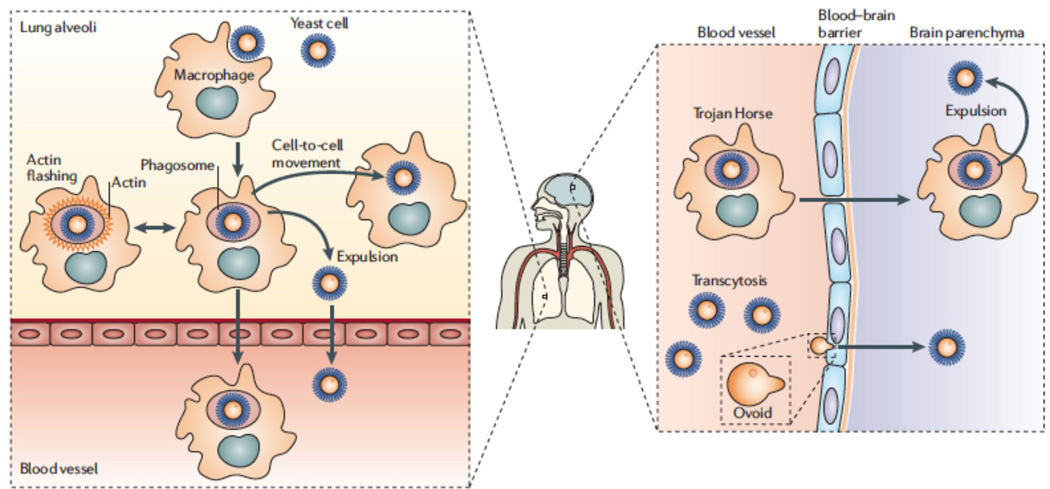
Following initial pulmonary infection, C. neoformans and C. gattii commonly disseminate and cross the blood-brain barrier (BBB) to cause meningoencephalitis (Figure 2) 10, 31–36. Accumulating evidence indicates that C. neoformans can cross the BBB by transcytosis through the endothelial cells that line the blood vessels in the brain 31–33, 36. This process involves the direct uptake of the fungal cells by the endothelial cells and transmigration through the cytoplasm to reach the brain. There is also evidence that the fungal cells can cross the endothelium by a “Trojan horse” strategy that involves migration of phagocytic cells containing cryptococci 35. It is not yet known whether one of these mechanisms is favored over the other, and presumably these same processes also facilitate C. gattii entry into the brain.
Figure 2. Interactions of fungal cells with phagocytic cells and dissemination through the blood brain barrier.
a | Fungal cells in the lung are readily phagocytosed by alveolar macrophages and other phagocytic cells such as neutrophils. However, the subpopulation of giant cells in the lungs is refractory to phagocytosis and may remain extracellular 55, 58. In the absence of immune clearance, the fungus proliferates both intracellularly and extracellularly 29. b | The fungal cells may escape from the phagosomes of macrophages by an expulsion mechanism that maintains the viability of both cell types 41, 45. c | The expulsion process can also result in cell to cell movement of the fungus when expulsion results in passage of yeast cells between adjacent macrophages 44, 46. d | Fungal cells may be contained within macrophages by transient inhibition of expulsion by actin cage formation (caging) 47. Free fungal cells or those present in phagocytic cells enter the bloodstream and reach the central nervous system 35, 36. e | Once in the microcapillaries of the brain, evidence is accumulating that fungal cells cross the endothelium via a ‘Trojan horse’ mechanism, inside phagocytic cells 35. f | Observations by intravital microscopy also support an additional mechanism whereby the fungal cells cross the capillary endothelium by direct transcytosis 36. It has been proposed that a morphological change occurs during this process. Specifically, the spherical yeast cells adopt a more ovoid shape at the site of initial interaction with endothelial cells 36. g | Expulsion of yeast cells into the brain parenchymal may occur following delivery by phagocytic cells.
The recent application of intravital microscopy (IVM) to examine interactions between C. neoformans and mouse brain capillaries provides strong support for direct transcytosis of endothelial cells 36. Specifically, IVM revealed that C. neoformans cells appeared in brain capillaries within 3 to 4 seconds after tail vein injection and that the cells came to an abrupt stop in vessels of comparable diameter to the cryptococcal cells. The apparent mechanical trapping of the fungal cells did not depend on their viability or ability to produce capsule, and sudden stopping was also observed for polystyrene microspheres and the nonpathogenic yeast Saccharomyces cerevisiae. More detailed observations with spinning disk confocal IVM allowed detection of active transmigration of fungal cells across the brain microvasculature. In this situation, viability of the cells was essential but proliferation was not needed, as a defect in proliferative capacity due to a temperature sensitive mutation did not block transmigration. Interestingly, the fungal cells displayed a distinct ovoid, budded morphology during transmigration suggesting that a specific morphological change may occur as part of the process (Figure 2). It would be interesting to study if turgor pressure is involved in this morphological change, which could then be reminiscent of the mechanisms of host penetration by plant pathogenic fungi (e.g., during appressorium formation) 36, 37.
The transcytosis of a urease-defective mutant of C. neoformans was also examined to demonstrate a role for this enzyme in increasing the number of transmigration sites into the brain 36. Previous studies had implicated urease in cryptococcal virulence and identified a role for this enzyme in sequestering fungal cells in microcapillary beds in the brain 38. The mechanism by which urease production facilitates fungal spread into the brain is not known but could involve local ammonia production that influences interactions with endothelial cells (e.g., increased adherence or toxicity) 38. Mice infected with urease-producing strains had a higher fungal burden in the brain and reduced survival compared with the urease-defective mutant 36. These trends were reduced in mice treated with the urease inhibitor flurofamide, thus indicating the therapeutic potential of blocking transmigration.
Evidence for the other mechanism of crossing the BBB, the “Trojan horse” strategy, comes from recent experiments that also explored the involvement of blood monocytes (Figure 2) 35. Specifically, Charlier et al. optimized phagocytosis of C. neoformans cells by bone marrow-derived monocytes and compared the dissemination of fungal cells pre-loaded in phagocytes following tail vein injection into mice with the dissemination of free yeast cells 35. They found that the fungal burdens in the brains of infected mice were comparable at one and six hours after infection, but that the load was approximately four-fold higher at 24 hours for the mice that received phagocytosed cells. This result suggests that association with monocytes promotes the ability of C. neoformans to cross the BBB. In addition, experiments involving depletion of phagocytes by clodronate treatment of infected mice resulted in reduced fungal loads in all organs tested (i.e., brain, lungs and spleen) 35. Phagocytes may therefore play a prominent role in reseeding tissues with cryptococcal cells, an idea that is consistent with earlier work demonstrating that fungal cells can be recovered from circulating monocytes, and that fungemia can occur even after a period of fungal cell clearance 39, 40.
The “Trojan horse” mechanism of dissemination may be facilitated by interactions between fungal and phagocytic cells that involve expulsion from, and cell-to-cell transfer between, macrophages containing internalized yeast (Figure 2). C. neoformans can survive the harsh environment of the phagosome, and the development of massive C. neoformans-containing phagosomes has been observed in macrophages, suggesting that an early yeast proliferation stage commences in these vesicles 41–46. Both C. neoformans and C. gattii can escape from host macrophages in a non-destructive expulsion process that leaves both the host and the pathogen viable 41, 44–46. Expulsion appears to occur when a mature phagosome containing one or more fungal cells fuses with the plasma membrane to release the yeast into the extracellular space. Primary human macrophages show a higher rate of expulsion than the murine macrophage-like cell line J774, and expulsion is not influenced by the activation state of the macrophages nor by inhibitors of phagosome maturation (e.g., concanamycin and chloroquine) 41, 45. In fact, expulsion appears to follow phagosome-lysosome fusion and may be strictly coordinated by, or dependent on, the pathogen because active extrusion from macrophages was not observed with killed C. neoformans 41, 45. Giant phagosomes have also been observed in macrophages undergoing expulsion, leading to speculation that C. neoformans may alter the membrane properties of phagosomes 41. This may be part of a fungal strategy to promote dissemination and to avoid host cell death that would trigger inflammation. In fact, cell-to-cell transfer of yeast between macrophages was observed, and this process might also contribute to latent persistence of the pathogen in host cell populations and potentially promote transport across the BBB 44, 46.
A recent study provided additional insight into the interactions at the phagosomal membrane that may determine whether the outcome of phagocytosis is either non-lytic escape or containment and intracellular persistence 47. A time-lapse examination of murine or primary human macrophages containing cryptococcal cells and expressing actin tagged with GFP revealed the occurrence of cycles of actin polymerization (identified as actin “flashes”) that formed transient cytoskeletal ‘cages’ around phagosomes (Figure 2). The actin flashes appeared to be nucleated by the Arp2/3 complex upon activation by WASP proteins and the process did not interfere with phagosome maturation. The possibility that actin polymerization might be a barrier to expulsion was tested by using agents that depolymerize (cytochalasin D) or stabilize (jasplakinolide) actin. Actin flashing was found to inversely correlate with expulsion, a result consistent with a possible transient inhibition of expulsion by actin cage formation. The use of fluorescent dextran as a probe of phagosome membrane integrity also revealed that 95% of phagosomes become permeablized prior to expulsion and that an actin flash immediately follows this event. Overall, this study reveals intimate intracellular interactions that resemble processes employed by bacterial pathogens to subvert the actin cytoskeleton in phagocytic cells (e.g., the actin assembly and disassembly that occurs on phagosomes containing Listeria monocytogenes prior to bacterial escape into the cytoplasm) 48.
Enhanced intracellular parasitism and the immune response to C. gattii
The ability of cryptococcal cells to reside in and escape from macrophages may also be a contributing factor in the emergence of C. gattii infections in Western North America (Box 1). This idea is supported by the examination of a large collection of C. gattii isolates, including several from the epicenter of the outbreak on Vancouver Island in British Columbia, that revealed an association between high intracellular proliferation rates (IPR) in macrophages and virulence 49. An in vitro assay for IPR was developed to monitor pathogen cell numbers after phagocytosis by murine macrophage-like cells or human primary macrophages. The most common genotype of C. gattii isolates from British Columbia (designated VGIIa) showed higher proliferation rates than other C. gattii isolates from around the world, although the higher rates were comparable to those of some C. neoformans isolates. For the C. gattii isolates, the higher proliferation rate also correlated with enhanced virulence in a murine inhalation model of cryptococcosis. Transcriptional profiling of 24 C. gattii strains, using cells recovered from within macrophages, also demonstrated that elevated mitochondrial transcripts correlated with higher IPR and virulence 49. Interestingly, a tubular mitochondrial morphology rather than a globular organization was also observed in fungal cells after phagocytosis, and this structure also correlated with higher IPR. Mitochondrial fusion may account for the tubular morphology and potentially contribute to the efficient repair of mitochondrial DNA damage resulting from oxidative conditions in phagosomes 49.
Although the association between mitochondrial gene expression, morphology and IPR is fascinating and suggests that a specific adaptation led to increased virulence, further work is needed to understand C. gattii infections in the context of the innate immune response and human disease. For example, strains of several C. gattii genotypes (VGI, VGIIa, VGIIb and VGIIc; see Box 1) are responsible for the human and animal cases in Western North America, and some strains representing the VGIIb genotype had a lower IPR but still caused fatalities in patients in BC 5, 7, 49. In addition, strains representing the C. gattii genotypes found on Vancouver Island (VGI, VGIIa and VGIIb) fail to trigger the same level of protective inflammatory response compared with a representative C. neoformans strain 50. The reduced inflammation was correlated with inhibition or failure to provoke the migration of neutrophils into sites of infection, and reduced elicitation of protective cytokines such as TNF-α. Despite the differences in immune responses, the representative VGIIa strain with a high IPR showed similar virulence in mice compared with a C. neoformans strain, while the other two C. gattii strains (VGI and VGIIb) had reduced virulence 49, 50 . These results suggest that the ability of C. gattii to evade or suppress the protective immune response could influence virulence and potentially contribute to infections in immunocompetent hosts. The underlying basis of differences in the immune response to C. gattii and C. neoformans, as well as the relevance of mouse models to human cryptococcosis, await targeted investigation.
Morphological and genomic adaptations during infection
Cryptococcal giant cells
Depending on environmental conditions, cryptococcal cells can undergo different morphological transitions including the formation of filaments from parental yeast cells during mating, enlargement of the capsule in response to environmental and host factors, and expansion of cell size to form giant cells during infection (Figure 1) 17, 19, 51–58. Giant yeast cells as large as 40 to 50 µm in diameter have been seen in clinical samples, and were first discovered in the lungs, brain and meninges of a cryptococcosis patient; in this case, the recovered cells were found to regain normal size during subsequent in vitro culture 51. As mentioned above, cells with a yeast-like morphology and a size from 5–10 µm are the most common cell type found in infected tissue. Thermal stress may be a factor in cell enlargement because another “giant cell” isolate from human brain tissue produced cells of typical small size in vitro at 25°C, but produced cells that were 25 µm in diameter at 35°C 52. Size heterogeneity has also been documented for cryptococcal cells during mouse pulmonary infections, with the identification of both giant and very small “micro” cells in tissue sections 59. Two recent studies solidified our appreciation of giant cell formation as a prominent feature of cryptococcal infections, and revealed important new insights into the properties of these unusual cells 55, 58. In both studies, giant cells were detected in the lung tissue of infected mice and were recovered by bronchoalveolar lavage to allow characterization of the cells.
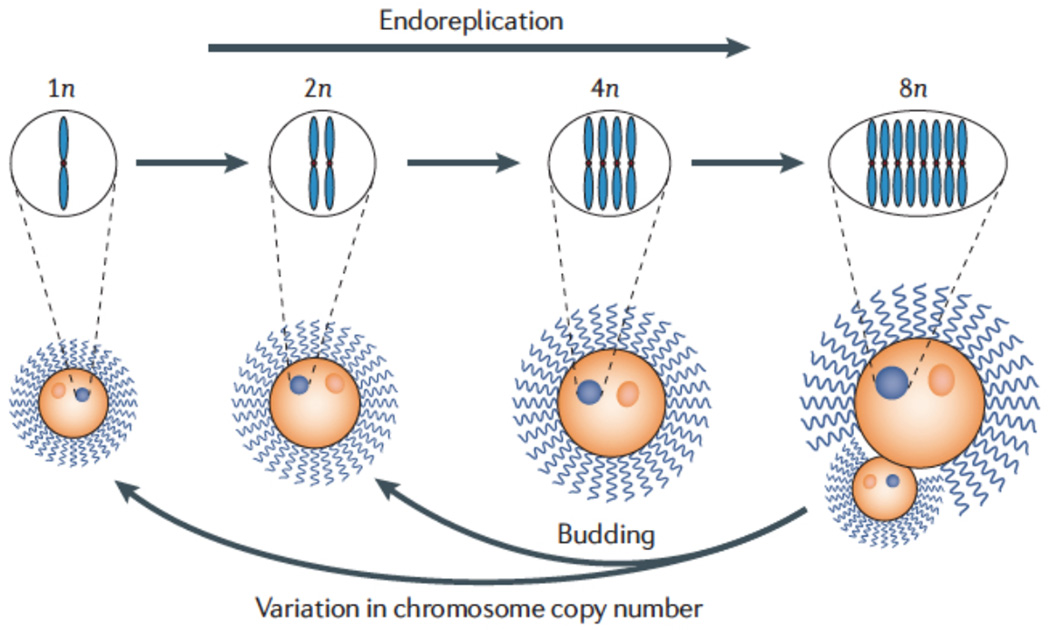
Zaragoza et al. found that giant cells (25 – 30 µm in diameter) were produced in the lungs of infected mice at three weeks post-infection by ten different cryptococcal strains and in four different mouse strains 55. The proportion of giant cells ranged from 10 to 80% of the total fungal cell count in the lung, depending on infection time, overall fungal burden, and pulmonary inflammation. In general, the proportion of giant cells was higher in mice that received a low inoculum and showed reduced symptoms and lower inflammation. The giant size of the cells was maintained ex vivo, and smaller cells were produced by budding on solid culture medium. Similarly, Okagaki et al. observed giant cells ranging in diameter from > 10 µm up to 50–100 µm (capsule sizes were highly variable), accounting for ~20% of the lung cryptococcal burden as early as one day post-infection 58. Giant cells were mainly found in lung tissue but a few were also observed in the spleen and brain at later time points. Both studies found that the larger cells were polyploid and uninucleate, suggesting that they arise from DNA replication without concomitant cell fission (Figure 3).
Figure 3. Giant cell formation and variation in genome copy number.
The majority of yeast cells isolated from clinical and environmental sources have a haploid (1N) genome copy number, although diploid (2N) isolates can be obtained at a frequency of ~8% 17, 53, 74. These appear to be the result of mating interactions between strains with A and D capsular serotypes, and some of these strains are aneuploid (e.g., 2N-1) 70. The giant cell formation observed in infected lung tissue is accompanied by endoreplication resulting in elevated genome copy number (e.g., tetraploid (4N), octaploid (8N), etc.) without mitosis 55, 58. The small cells produced by budding from giant cells may be haploid or diploid cells. The variation in ploidy for giant cells reflects dynamic expansions and contractions of genome copy number. In addition, the observed aneuploidy (e.g., 2N-1, 1N+1) for some clinical and environmental isolates may be a result of chromosome copy number variation that occurs during transitions of cells of different ploidies 62,70.
Interestingly, the pheromone-response and cAMP-dependent signaling pathways both appear to regulate giant cell formation. The response to pheromones during mating in C. neoformans is controlled by components of a mitogen-activated protein kinase (MAPK) cascade that includes cell surface receptors, guanine nucleotide-binding proteins (G proteins), protein kinases and transcription factors 13, 57. Okagaki et al. showed that co-infection of both mating types resulted in an increase in giant cell production only among the MATa cells; this response was dependent on Ste3a, the G-protein coupled receptor involved in pheromone sensing 58. The increase in cell size probably inhibits the ability of MATa cells to translocate from the lungs to the brain and this precludes successful CNS infection. However, cells may increase in size after entry into the CNS because enlarged cells have been observed in a brain abscess from a patient, as described above 52. In the absence of MATα cells, other factors and signaling pathways besides the response to pheromones may regulate giant cell formation including temperature and nutrients. For example, the cAMP pathway mediates nutrient sensing in C. neoformans and regulates mating, capsule formation and melanin production 13, 16, 60. Zaragoza et al. showed that giant cell formation was dependent on cAMP-dependent signaling by examining the process in an adenylate cyclase (cac1) mutant that was defective in cAMP production 55. Additionally, constitutive activation of the cAMP signaling pathway was previously found to result in the production of enlarged cells, increased capsule size, and hypervirulence in animal models 60.
Giant cell formation may be part of the defense strategy that allows C. neoformans to evade the initial host immune response, establish lung infection and thus prolong survival within the host. Similar strategies may be employed by other fungal pathogens, such as Pneumocystis and Coccidioides spp., and there are conceptual similarities with dimorphic fungi that employ the hyphal to yeast transition to establish disease 61. Both recent studies of giant cells found that they were not phagocytosed, as opposed to yeast cells, and therefore may represent a resistant subpopulation that persists in an extracellular state 55, 58. These studies also showed that infections with lower inocula generally resulted in a greater proportion of giant cells, as might be expected in hosts with chronic or latent infections. It is also possible that small cells, such as the “micro” cells identified in infected mouse lungs, might be more readily engulfed by phagocytes and disseminated 59.
Changes in ploidy during infection
Desnos-Ollivier et al. recently reported that mixed infections and changes in the ploidy (number of sets of chromosomes) of C. neoformans cells during cryptococcosis are more common than previously thought 62. This group analyzed a collection of unpurified clinical C. neoformans isolates and found mixed infections in nine of 49 patients (18.4%). These mixed infections involved strains of different mating type, serotype, genotype and ploidy. The majority of patients had infections with haploid strains of serotype A and mating type MATα (designated Aα strains), in association with haploid strains of the D serotype, or with diploid strains (serotypes AA or AD or DD). Cryptococcosis is thought to often occur by reactivation of latent infections in immunosuppressed hosts, and the different genotypes could have been acquired at the same time or at different times. Multilocus sequence typing (MLST) was employed to determine whether haploid and AD hybrid diploid isolates in the same patient were acquired by inhalation of multiple strains from the environment and whether ploidy changes occurred in the patient 62. The results indicated that three of the patients had been coinfected with different strains from the environment, whereas diploidization seemed to have occurred during infection in other patients. Experimental infections in mice with tagged strains confirmed the possibility of changes in ploidy, and indicated that diploid strains arose from endoreplication rather than cell fusion 62.
Chromosome copy number variation
The increase in ploidy as a result of giant cell formation and endoreplication indicates that considerable cryptococcal genome variability can occur during infection. This variability could influence virulence at several levels, including resistance to the immune response, disease progression, dissemination and latency. This is because changes in ploidy and aneuploidy are known to influence growth, gene expression and antifungal drug sensitivity in other fungi 63–65. Changes in karyotype have been documented among sequential cryptococcal isolates from individual patients, and these changes include chromosome rearrangements or deletions 66.
Detailed examination of genome variability is possible now because sequences are available for two serotype D strains (B3501A and JEC21) 67 and one serotype A strain (H99) of C. neoformans 68, and two strains of C. gattii (WM276 and R265) 69. These genomes have been used in comparative genome hybridization (CGH) experiments to characterize genome variability between strains of different mating type, molecular subtype and ploidy in C. neoformans and C. gattii 70. Importantly, this work revealed unexpected disomy for chromosome 13 in two C. neoformans clinical haploid strains and preferential retention of the serotype A version of chromosome 1 in three naturally occurring C. neoformans AD diploid strains 70. A survey of additional fresh clinical isolates also revealed disomy at other chromosomes (G. Hu and J. Kronstad, unpublished data). It is therefore tempting to speculate that disomy represents an intermediate state in the transition between haploid, diploid and higher ploidy levels that arise during giant cell formation and endoreplication in infected tissue (Figure 3).
As in S. cerevisiae and Candida albicans, chromosome copy number variation in C. neoformans and C. gattii may contribute to phenotypic and virulence differences between variants 63, 65, 70. An interesting example comes from the recent use of CGH to document disomy for specific chromosomes in serotype A and D strains that display heteroresistance to azole antifungal drugs 71. Heteroresistance is the emergence of a resistant minor subpopulation within a single colony of a susceptible strain, and it has been demonstrated for strains of the A and D serotype of C. neoformans and for C. gattii strains 71, 72. CGH revealed that this type of drug resistance was achieved by disomy of multiple chromosomes, and removal of fluconazole drug pressure resulted in loss of high-level resistance and a return to monosomy. In particular, duplication of chromosome 1, which carries the known genes involved in azole drug resistance (AFR1 and ERG11), led to elevated expression of these genes and resistance 71. Changes in chromosome number may therefore be an important factor for resistance to fluconazole during prolonged maintenance therapy.
Further characterization of the impact of genome variation on phenotype will likely provide insights into cryptococcal virulence, survival in the host and microevolution. Although a link between genome variability, aneuploidy and phenotypic switching has not been established, switch variants with smooth or mucoid colony phenotypes have been characterized in C. neoformans and C. gattii. These variants do show differences in virulence, their ability to provoke an immune response, and interactions with phagocytic cells 73.
Summary and future directions
Discoveries in the past five years hint that pathogenic cryptococcal species show a previously under appreciated level of sophistication during infection of mammalian host cells and tissues. At the initial stage of infection, it now appears that spores of C. neoformans are readily phagocytosed and rapidly germinate inside phagocytic cells. The availability of purified spores will allow a number of outstanding questions to be addressed, including whether the speed of germination relative to the activation of the innate immune response influences the outcome of infection for C. neoformans and C. gattii. A detailed characterization of spore-specific molecules, their expression during differentiation and their interactions with host proteins will now be possible. Such molecules may serve as key reagents to search for the elusive spores in the environment and therefore garner further evidence for mating in nature beyond the isolation of AD and AA hybrid strains 74.
The formation of giant cells during initial lung infection and the accompanying innate immune response may represent a strategy to allow a subpopulation of fungal cells to avoid phagocytosis and persist extracellularly. It will be interesting to discover the in vitro and in vivo signals and differentiation mechanisms that lead to giant cell formation and the processes by which daughter cells are formed. In particular, methods are needed to produce giant cells in culture so that the process can be dissected using molecular genetic tools. It is striking that the ploidy changes accompanying giant cell formation were discovered coincidentally with mixed infections, endoreplication and aneuploidy in clinical isolates. These studies reveal an unexpected level of genome plasticity that apparently involves shifts in genome copy number to reach the octaploid state (and potentially higher copy number). This plasticity could also lead to a myriad of chromosome complements, as indicated by disomic strains of clinical origin. Such shifts in chromosome copy number have an unpredictable impact on gene expression that could influence virulence, adaptation to the host immune response and proliferation in specific host niches. Studies in S. cerevisiae, for example, indicate that aneuploidy can provide heritable variation that contributes to phenotypic adaptation and an advantage in the response to stress 75. In addition, the changes in ploidy associated with giant cells are reminiscent of increases and decreases in ploidy described for hapatocytes 76. These liver cells undergo a dynamic process of polyplization, ploidy reduction and aneuploidy (called the ploidy conveyor) that could possibly be part of a response to liver injury and regeneration 76.
Once an infection has been established, the dynamics of cryptococcal mobility into and out of phagocytic cells contributes to survival and dissemination. The intracellular battleground in the phagosome may turn out to involve some of the molecular strategies already discovered for intracellular bacterial pathogens. This certainly appears to be the case for actin flashing and the expulsion of fungal cells from phagocytes. The pathogen and host factors that are involved in expulsion and the subversion of phagocytic cells for persistence, dissemination and crossing the BBB via the Trojan horse mechanism are as yet unknown. The latest information on intracellular proliferation reveals a correlation between survival, virulence and mitochondrial morphology for C. gattii. Many questions remain about the link between morphological responsiveness and virulence, and the relative importance of this trait for C. gattii versus C. neoformans. In general, much of our information about interactions with the host comes from studies with C. neoformans and, although extrapolation to C. gattii is often warranted, there are considerable opportunities for comparison of the species.
Finally, dissemination to the brain is a hallmark of cryptococcosis, and C. neoformans cells have now been caught in the act of crossing the BBB. The relative contribution of transcytosis versus the Trojan horse mechanism remains to be determined, but the ability to visualize transcytosis opens up new possibilities for exploring the fungal factors involved. The role of urease has already been demonstrated and similar approaches could be used to examine the numerous mutants in collections that will soon include all the non-essential C. neoformans genes 77. In particular, it is fascinating that transcytosis may involve a morphological transition with similarities to processes in other fungi, including plant pathogens. The molecular basis of this transition and the signals involved are of great interest.
Online Summary.
Methods have been developed to separate the spores (1–2 µm in diameter) that result from sexual development and meiosis in Cryptococcus neoformans away from the parental yeast cells (5–10 µm). The spores are infectious, as long suspected, and they are readily phagocytized by macrophages in the absence of an opsonin, while yeast cells require prior opsonization.
C. neoformans and C. gattii disseminate from the lung and cross the blood-brain barrier (BBB) to cause meningoencephalitis. The fungal cells cross the BBB directly by transcytosis through endothelial cells lining vessels in the brain, and by a “Trojan horse” strategy that involves transport in phagocytic cells.
Intracellular cryptococcal cells residing in phagosomes can escape their phagocytic host cells by expulsion and by cell-to-cell transfer between macrophages. Cycles of actin polymerization (actin “flashes”) appear to form transient cages around phagosomes and these may serve as a barrier to expulsion.
Cryptococcus gattii has emerged as a pathogen of immunocompetent people and animals in Western North America. The associated C. gattii strains appear to have a high intracellular proliferation rates in macrophages that is correlated with their virulence, and they trigger a reduced protective inflammatory response compared with a representative C. neoformans strain.
Recent studies have characterized a sub-population of giant cells (> 10 µm up to 50 – 100 µm) that accounts for ~20% of the cryptococcal burden during lung infection. These cells are polyploid and resistant to phagocytosis.
Studies with fresh isolates of C. neoformans from AIDS patients revealed that changes in ploidy resulting from endoreplication and mixed infections during cryptococcosis are more common than previously thought. In addition, comparative genome hybridization results indicate that clinical isolates and strains that display antifungal drug resistance can harbor disomic chromosomes.
Glossary
- Capsule
Cryptococcal cells are surrounded by polysaccharides composed of glucuronoxylomannan (GXM) and galactoxylomannan (GalXM).
- Serotypes
Classification of isolates based on antibody recognition of the polysaccharide capsule and yielding serotypes A, D and AD for C. neoformans, and serotypes B and C for C. gattii.
- Mating types
Cryptococcal cells have one of two possible mating types, designated MATa and MATα, that fuse to initiate sexual development leading to spore formation.
- Opsonization
The binding of an antibody or other protein to the surface of pathogen cell to target it for phagocytosis.
- Meningoencephalitis
A combination of infection and inflammation of the meninges, the membranes surrounding the central nervous system, and the brain itself.
- Melanin
A brown or black polymer deposited in the fungal cell wall and resulting in part from the catalytic activity of the enzyme laccase on substrates such as L-dopamine.
- Dectin-1
A receptor protein on the surface of immune effector cells that recognizes β-glucans on fungal cell walls to trigger an antifungal defense response.
- CD11b/CD18
A member of the integrin adhesion receptor family on leukocytes that recognizes fungal mannose and β-glucans molecules.
- Appressorium
A differentiated cell type that functions as an infection structure to mechanically penetrate the host surface, as typically employed by fungal pathogens to penetrate plant cell walls.
- Blood brain barrier
A barrier that is created by endothelial cells connected by tight junctions in capillaries of the central nervous system, and that restricts the passage of solutes and microbes into the brain.
- Intravital microscopy
A technique for direct microscopic observations of cellular interactions in the tissue of an anesthetized animal. When coupled with spinning disk confocal microscopy, the method allows images of optical sections of cells to be collected in narrow focal planes with minimal interference from out of focus regions.
- Arp2/3 complex
This seven-member protein complex is a major component of the actin cytoskeleton, and the actin-related proteins Arp2 and Arp3 function in the nucleation of new actin filaments.
- WASP proteins
A family of proteins named after the Wiskott-Aldrich Syndrome which results from mutations in the WAS gene. WASP proteins bind to and activate the Arp2/3 proteins for subsequent nucleation of actin filaments.
- Intracellular proliferation rate
A measure of the relative intracellular parasitism that results from dividing the maximum intracellular number of fungal cells in phagocytes by the initial number of cells at the start of an experiment.
- Polyploidy
A number of sets of chromosomes in a cell that is elevated relative to the typical haploid (one set) or diploid (two sets) conditions.
- Aneuploidy
An unusual complement of chromosomes such as the disomic state arising from two copies of a particular chromosome in a cell.
- Heteroresistance
A reversible adaptive resistance to an antimicrobial drug such that a subpopulation of cells displays the ability to grow in the presence of the drug.
- Endoreplication
DNA replication without subsequent mitosis that results in clear doubling events for the genome.
References
- 1.Brizendine KD, Pappas PG. Cryptococcal meningitis: Current approaches to management in patients with and without AIDS. Curr. Infect. Dis. Rep. 2010;12:299–305. doi: 10.1007/s11908-010-0113-4. [DOI] [PubMed] [Google Scholar]
- 2. Park BJ, et al. Estimation of the current global burden of cryptococcal meningitis among persons living with HIV/AIDS. AIDS. 2009;23:525–530. doi: 10.1097/QAD.0b013e328322ffac. This study provides the first global view of the burden of cryptococcosis and reveals that there are ~1 million cases per year resulting in ~625,000 deaths. The highest burden is in sub-Saharan Africa.
- 3.Bartlett KH, Kidd SE, Kronstad JW. The emergence of Cryptococcus gattii in British Columbia and the Pacific Northwest. Curr. Infect. Dis. Rep. 2008;10:58–65. doi: 10.1007/s11908-008-0011-1. [DOI] [PubMed] [Google Scholar]
- 4.Byrnes EJ, 3rd, et al. Molecular evidence that the range of the Vancouver Island outbreak of Cryptococcus gattii infection has expanded into the Pacific Northwest in the United States. J. Infect. Dis. 2009;199:1081–1086. doi: 10.1086/597306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Byrnes EJ, 3rd, et al. Emergence and pathogenicity of highly virulent Cryptococcus gattii genotypes in the northwest United States. PLoS Pathog. 2010;6:e1000850. doi: 10.1371/journal.ppat.1000850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Datta K, et al. Spread of Cryptococcus gattii into Pacific Northwest region of the United States. Emerg. Infect. Dis. 2009;15:1185–1191. doi: 10.3201/eid1508.081384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Galanis E, Macdougall L. Epidemiology of Cryptococcus gattii, British Columbia, Canada, 1999–2007. Emerg. Infect. Dis. 2010;16:251–257. doi: 10.3201/eid1602.090900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kwon-Chung KJ, Boekhout T, Fell JW, Diaz M. Proposal to conserve the name Cryptococcus gattii against C. hondurianus and C. bacillisporus (Basidiomycota, Hymenomycetes, Tremellomycetidae) Taxon. 2002;51:804–806. [Google Scholar]
- 9.Mitchell TG, Perfect JR. Cryptococcosis in the era of AIDS--100 years after the discovery of Cryptococcus neoformans . Clin. Microbiol. Rev. 1995;8:515–548. doi: 10.1128/cmr.8.4.515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sorrell TC. Cryptococcus neoformans variety gattii . Med. Mycol. 2001;39:155–168. [PubMed] [Google Scholar]
- 11.Casadevall A, Nosanchuk JD, Williamson P, Rodrigues ML. Vesicular transport across the fungal cell wall. Trends Microbiol. 2009;17:158–162. doi: 10.1016/j.tim.2008.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Casadevall A, Pirofski LA. The damage-response framework of microbial pathogenesis. Nat. Rev. Microbiol. 2003;1:17–24. doi: 10.1038/nrmicro732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Idnurm A, et al. Deciphering the model pathogenic fungus Cryptococcus neoformans . Nat. Rev. Microbiol. 2005;3:753–764. doi: 10.1038/nrmicro1245. [DOI] [PubMed] [Google Scholar]
- 14.Jung WH, Kronstad JW. Iron and fungal pathogenesis: a case study with Cryptococcus neoformans . Cell. Microbiol. 2008;10:277–284. doi: 10.1111/j.1462-5822.2007.01077.x. [DOI] [PubMed] [Google Scholar]
- 15.Doering TL. How sweet it is! Cell wall biogenesis and polysaccharide capsule formation in Cryptococcus neoformans . Annu. Rev. Microbiol. 2009;63:223–247. doi: 10.1146/annurev.micro.62.081307.162753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kozubowski L, Lee SC, Heitman J. Signalling pathways in the pathogenesis of Cryptococcus. Cell. Microbiol. 2009;11:370–380. doi: 10.1111/j.1462-5822.2008.01273.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lin X. Cryptococcus neoformans: morphogenesis, infection, and evolution. Infect. Genet. Evol. 2009;9:401–416. doi: 10.1016/j.meegid.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 18.Ma H, May RC. Virulence in Cryptococcus species. Adv. Appl. Microbiol. 2009;67:131–190. doi: 10.1016/S0065-2164(08)01005-8. [DOI] [PubMed] [Google Scholar]
- 19.Zaragoza O, et al. The capsule of the fungal pathogen Cryptococcus neoformans . Adv. Appl. Microbiol. 2009;68:133–216. doi: 10.1016/S0065-2164(09)01204-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Voelz K, May RC. Cryptococcal interactions with the host immune system. Eukaryot. Cell. 2010;9:835–846. doi: 10.1128/EC.00039-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Casadevall A, Perfect JR. Cryptococcus neoformans. Washington, D.C.: American Society for Microbiology Press; 1998. [Google Scholar]
- 22.Heitman J, Kozel TR, Kwon-Chung KJ, Perfect JR, Casadevall A, editors. Cryptococcus: From Human Pathogen to Model Yeast. Washington D.C.: American Society for Microbiology Press; 2010. [Google Scholar]
- 23.Lin X, Hull CM, Heitman J. Sexual reproduction between partners of the same mating type in Cryptococcus neoformans . Nature. 2005;434:1017–1021. doi: 10.1038/nature03448. [DOI] [PubMed] [Google Scholar]
- 24.Botts MR, Giles SS, Gates MA, Kozel TR, Hull CM. Isolation and characterization of Cryptococcus neoformans spores reveal a critical role for capsule biosynthesis genes in spore biogenesis. Eukaryot. Cell. 2009;8:595–605. doi: 10.1128/EC.00352-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xue C, Tada Y, Dong X, Heitman J. The human fungal pathogen Cryptococcus can complete its sexual cycle during a pathogenic association with plants. Cell Host Microbe. 2007;1:263–273. doi: 10.1016/j.chom.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 26. Velagapudi R, Hsueh YP, Geunes-Boyer S, Wright JR, Heitman J. Spores as infectious propagules of Cryptococcus neoformans . Infect. Immun. 2009;77:4345–4355. doi: 10.1128/IAI.00542-09. This article and reference 24 describe the development of methods to isolate and characterize spores.
- 27.Vartivarian SE, et al. Regulation of cryptococcal capsular polysaccharide by iron. J. Infect. Dis. 1993;167:186–190. doi: 10.1093/infdis/167.1.186. [DOI] [PubMed] [Google Scholar]
- 28. Giles SS, Dagenais TR, Botts MR, Keller NP, Hull CM. Elucidating the pathogenesis of spores from the human fungal pathogen Cryptococcus neoformans . Infect. Immun. 2009;77:3491–3500. doi: 10.1128/IAI.00334-09. This article and reference 26 provide evidence that spores are infectious agents and analyze the interactions of spores with phagocytic cells. This article also describes initial studies of spore surface molecules such as β-1,3 glucan and macrophage receptors that include dectin-1.
- 29.Feldmesser M, Kress Y, Novikoff P, Casadevall A. Cryptococcus neoformans is a facultative intracellular pathogen in murine pulmonary infection. Infect. Immun. 2000;68:4225–4237. doi: 10.1128/iai.68.7.4225-4237.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Botts MR, Hull CM. Dueling in the lung: how Cryptococcus spores race the host for survival. Curr. Opin. Microbiol. 2010;13:437–442. doi: 10.1016/j.mib.2010.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chang YC, et al. Cryptococcal yeast cells invade the central nervous system via transcellular penetration of the blood-brain barrier. Infect. Immun. 2004;72:4985–4995. doi: 10.1128/IAI.72.9.4985-4995.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shea JM, Kechichian TB, Luberto C, Del Poeta M. The cryptococcal enzyme inositol phosphosphingolipid-phospholipase C confers resistance to the antifungal effects of macrophages and promotes fungal dissemination to the central nervous system. Infect. Immun. 2006;74:5977–5988. doi: 10.1128/IAI.00768-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kechichian TB, Shea J, Del Poeta M. Depletion of alveolar macrophages decreases the dissemination of a glucosylceramide-deficient mutant of Cryptococcus neoformans in immunodeficient mice. Infect. Immun. 2007;75:4792–4798. doi: 10.1128/IAI.00587-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Charlier C, Chrétien F, Baudrimont M, Mordelet E, Lortholary O, Dromer F. Capsule structure changes associated with Cryptococcus neoformans crossing of the blood-brain barrier. Am. J. Pathol. 2005;166:421–432. doi: 10.1016/S0002-9440(10)62265-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Charlier C, et al. Evidence of a role for monocytes in dissemination and brain invasion by Cryptococcus neoformans . Infect. Immun. 2009;77:120–127. doi: 10.1128/IAI.01065-08. Convincing evidence is presented to support the Trojan horse mechanism for crossing the blood brain barrier by C. neoformans and for a general role for monocytes in tissue seeding.
- 36. Shi M, et al. Real-time imaging of trapping and urease-dependent transmigration of Cryptococcus neoformans in mouse brain. J. Clin. Invest. 2010;120:1683–1693. doi: 10.1172/JCI41963. Intravital microscopy demonstrated that C. neoformans cells are mechanically trapped in mouse brain capillaries and actively transmigrate to the brain parenchyma.
- 37.Wilson RA, Talbot NJ. Under pressure: investigating the biology of plant infection by Magnaporthe oryzae . Nat. Rev. Microbiol. 2009;7:185–195. doi: 10.1038/nrmicro2032. [DOI] [PubMed] [Google Scholar]
- 38.Olszewski MA, et al. Urease expression by Cryptococcus neoformans promotes microvascular sequestration, thereby enhancing central nervous system invasion. Am. J. Pathol. 2004;164:1761–1771. doi: 10.1016/S0002-9440(10)63734-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lortholary O, et al. Fungemia during murine cryptococcosis sheds some light on pathophysiology. Med. Mycol. 1999;37:169–174. [PubMed] [Google Scholar]
- 40.Chretien F, et al. Pathogenesis of cerebral Cryptococcus neoformans infection after fungemia. J. Infect. Dis. 2002;186:522–530. doi: 10.1086/341564. [DOI] [PubMed] [Google Scholar]
- 41.Alvarez M, Casadevall A. Phagosome extrusion and host-cell survival after Cryptococcus neoformans phagocytosis by macrophages. Curr. Biol. 2006;16:2161–2165. doi: 10.1016/j.cub.2006.09.061. [DOI] [PubMed] [Google Scholar]
- 42.Levitz SM, et al. Cryptococcus neoformans resides in an acidic phagolysosome of human macrophages. Infect. Immun. 1999;67:885–890. doi: 10.1128/iai.67.2.885-890.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tucker SC, Casadevall A. Replication of Cryptococcus neoformans in macrophages is accompanied by phagosomal permeabilization and accumulation of vesicles containing polysaccharide in the cytoplasm. Proc. Natl. Acad. Sci. U. S. A. 2002;99:3165–3170. doi: 10.1073/pnas.052702799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Alvarez M, Casadevall A. Cell-to-cell spread and massive vacuole formation after Cryptococcus neoformans infection of murine macrophages. BMC Immunol. 2007;8:16. doi: 10.1186/1471-2172-8-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ma H, Croudace JE, Lammas DA, May RC. Expulsion of live pathogenic yeast by macrophages. Curr. Biol. 2006;16:2156–2160. doi: 10.1016/j.cub.2006.09.032. [DOI] [PubMed] [Google Scholar]
- 46.Ma H, Croudace JE, Lammas DA, May RC. Direct cell-to-cell spread of a pathogenic yeast. BMC Immunol. 2007;8:15. doi: 10.1186/1471-2172-8-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Johnston SA, May RC. The human fungal pathogen Cryptococcus neoformans escapes macrophages by a phagosome emptying mechanism that is inhibited by Arp2/3 complex-mediated actin polymerisation. PLoS Pathog. 2010;6:e1001041. doi: 10.1371/journal.ppat.1001041. Phagosomes containing cryptococcal cells show repeated cycles of actin polymerization that are cages that may temporarily inhibit expulsion of the fungal cells.
- 48.Yam PT, Theriot JA. Repeated cycles of rapid actin assembly and disassembly on epithelial cell phagosomes. Mol. Biol. Cell. 2004;15:5647–5658. doi: 10.1091/mbc.E04-06-0509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Ma H, et al. The fatal fungal outbreak on Vancouver Island is characterized by enhanced intracellular parasitism driven by mitochondrial regulation. Proc. Natl. Acad. Sci. U. S. A. 2009;106:12980–12985. doi: 10.1073/pnas.0902963106. Isolates from the outbreak have an increased capacity to proliferate in macrophages and they show an altered mitochondrial morphology after phagocytosis. These results suggest that intracellular parasitic capability is an important component of the outbreak.
- 50. Cheng PY, Sham A, Kronstad JW. Cryptococcus gattii isolates from the British Columbia cryptococcosis outbreak induce less protective inflammation in a murine model of infection than Cryptococcus neoformans . Infect. Immun. 2009;77:4284–4294. doi: 10.1128/IAI.00628-09. The first examination of immune response to the outbreak isolates demonstrates reduced production of pro-inflammatory cytokines and neutrophil infiltration in the lungs of mice infected with C. gattii when compared with C. neoformans.
- 51.Cruickshank JG, Cavill R, Jelbert M. Cryptococcus neoformans of unusual morphology. Appl. Microbiol. 1973;25:309–312. doi: 10.1128/am.25.2.309-312.1973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Love GL, Boyd GD, Greer DL. Large Cryptococcus neoformans isolated from brain abscess. J. Clin. Microbiol. 1985;22:1068–1070. doi: 10.1128/jcm.22.6.1068-1070.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sia RA, Lengeler KB, Heitman J. Diploid strains of the pathogenic basidiomycete Cryptococcus neoformans are thermally dimorphic. Fungal Genet. Biol. 2000;29:153–163. doi: 10.1006/fgbi.2000.1192. [DOI] [PubMed] [Google Scholar]
- 54.Zaragoza O, Fries BC, Casadevall A. Induction of capsule growth in Cryptococcus neoformans by mammalian serum and CO(2) Infect. Immun. 2003;71:6155–6164. doi: 10.1128/IAI.71.11.6155-6164.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zaragoza O, et al. Fungal cell gigantism during mammalian infection. PLoS Pathog. 2010;6:e1000945. doi: 10.1371/journal.ppat.1000945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nielsen K, et al. Cryptococcus neoformans {alpha} strains preferentially disseminate to the central nervous system during coinfection. Infect. Immun. 2005;73:4922–4933. doi: 10.1128/IAI.73.8.4922-4933.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hsueh YP, Heitman J. Orchestration of sexual reproduction and virulence by the fungal mating-type locus. Curr. Opin. Microbiol. 2008;11:517–524. doi: 10.1016/j.mib.2008.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Okagaki LH, et al. Cryptococcal cell morphology affects host cell interactions and pathogenicity. PLoS Pathog. 2010;6:e1000953. doi: 10.1371/journal.ppat.1000953. Along with reference 55, this study provides the first detailed characterization of giant cells and reveals their resistance to phagocytosis and their polyploid genome content.
- 59.Feldmesser M, Kress Y, Casadevall A. Dynamic changes in the morphology of Cryptococcus neoformans during murine pulmonary infection. Microbiol. 2001;147:2355–2365. doi: 10.1099/00221287-147-8-2355. [DOI] [PubMed] [Google Scholar]
- 60.D’Souza CA, et al. Cyclic AMP-dependent protein kinase controls virulence of the fungal pathogen Cryptococcus neoformans . Mol. Cell Biol. 2001;21:3179–3191. doi: 10.1128/MCB.21.9.3179-3191.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Klein BS, Tebbets B. Dimorphism and virulence in fungi. Curr. Opin. Microbiol. 2007;10:314–319. doi: 10.1016/j.mib.2007.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Desnos-Ollivier M, et al. Mixed infections and in vivo evolution in the human fungal pathogen Cryptococcus neoformans . mBio. 2010;1:e00091–e00010. doi: 10.1128/mBio.00091-10. An intriguing survey of fresh isolates demonstrated that mixed infections with strains of different mating type, serotype and genotype are present in approximately 20% of patients. This study also revealed that transitions between haploid and diploid states can occur during infection.
- 63.Torres EM, et al. Effects of aneuploidy on cellular physiology and cell division in haploid yeast. Science. 2007;317:916–924. doi: 10.1126/science.1142210. [DOI] [PubMed] [Google Scholar]
- 64.Galitski T, Saldanha AJ, Styles CA, Lander ES, Fink GR. Ploidy regulation of gene expression. Science. 1999;285:251–254. doi: 10.1126/science.285.5425.251. [DOI] [PubMed] [Google Scholar]
- 65.Selmecki A, Forche A, Berman J. Genomic plasticity of the human fungal pathogen Candida albicans . Eukaryot. Cell. 2010;9:991–1008. doi: 10.1128/EC.00060-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Fries BC, Chen F, Currie BP, Casadevall A. Karyotype instability in Cryptococcus neoformans infection. J. Clin. Microbiol. 1996;34:1531–1534. doi: 10.1128/jcm.34.6.1531-1534.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Loftus BJ, et al. The genome of the basidiomycetous yeast and human pathogen Cryptococcus neoformans . Science. 2005;307:1321–1324. doi: 10.1126/science.1103773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kavanaugh LA, Fraser JA, Dietrich FS. Recent evolution of the human pathogen Cryptococcus neoformans by intervarietal transfer of a 14-gene fragment. Mol. Biol. Evol. 2006;23:1879–1890. doi: 10.1093/molbev/msl070. [DOI] [PubMed] [Google Scholar]
- 69. D’Souza CA, et al. Genome variation in Cryptococcus gattii, an emerging pathogen of immunocompetent hosts. mBio. doi: 10.1128/mBio.00342-10. (in press) This paper reports the genome sequences of strains representing the VGI and VGII genotypes of C. gattii as well as comparative genome hybridization experiments to examine variation in avirulent, fluconazole-resistant and outbreak isolates.
- 70. Hu G, et al. Comparative hybridization reveals extensive genome variation in the AIDS-associated pathogen Cryptococcus neoformans . Genome Biol. 2008;9:R41. doi: 10.1186/gb-2008-9-2-r41. The genome sequences of serotype A and D strains were employed in comparative studies to characterize genomic variability in strains of different molecular subtypes and in AD hybrid strains. The analysis provided the first demonstration of disomy in clinical isolates of the A serotype that causes the majority of infections in AIDS patients.
- 71. Sionov E, Lee H, Chang YC, Kwon-Chung KJ. Cryptococcus neoformans overcomes stress of azole drugs by formation of disomy in specific multiple chromosomes. PLoS Pathog. 2010;6:e1000848. doi: 10.1371/journal.ppat.1000848. This study revealed that extensive disomy is associated with drug resistance and that chromosomes encoding the target of fluconazole inhibition (Erg11) or a drug efflux pump (Afr1) have elevated copy number in resistant isolates.
- 72.Varma A, Kwon-Chung KJ. Heteroresistance of Cryptococcus gattii to fluconazole. Antimicrob. Agents Chemother. 2010;54:2303–2311. doi: 10.1128/AAC.00153-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Guerrero A, Jain N, Wang X, Fries BC. Cryptococcus neoformans variants generated by phenotypic switching differ in virulence through effects on macrophage activation. Infect. Immun. 2010;78:1049–1057. doi: 10.1128/IAI.01049-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lin X, Patel S, Litvintseva AP, Floyd A, Mitchell TG, Heitman J. Diploids in the Cryptococcus neoformans serotype A population homozygous for the alpha mating type originate via unisexual mating. PLoS Pathog. 2009;5:e1000283. doi: 10.1371/journal.ppat.1000283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Rancati G, et al. Aneuploidy underlies rapid adaptive evolution of yeast cells deprived of a conserved cytokinesis motor. Cell. 2008;135:879–893. doi: 10.1016/j.cell.2008.09.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Duncan AW, et al. The ploidy conveyor of mature hepatocytes as a source of genetic variation. Nature. 2010;467:707–710. doi: 10.1038/nature09414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Liu OW, et al. Systematic genetic analysis of virulence in the human fungal pathogen Cryptococcus neoformans . Cell. 2008;135:174–188. doi: 10.1016/j.cell.2008.07.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Centers for Disease Control and Prevention (CDC) Emergence of Cryptococcus gattii--Pacific Northwest, 2004–2010. MMWR. 2010;59:865–868. [PubMed] [Google Scholar]
- 79.Fraser JA, et al. Same-sex mating and the origin of the Vancouver Island Cryptococcus gattii outbreak. Nature. 2005;437:1360–1364. doi: 10.1038/nature04220. [DOI] [PubMed] [Google Scholar]
- 80.Eisenman HC, Frases S, Nicola AM, Rodrigues ML, Casadevall A. Vesicle-associated melanization in Cryptococcus neoformans . Microbiol. 2009;155:3860–3867. doi: 10.1099/mic.0.032854-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Rodrigues ML, et al. Vesicular polysaccharide export in Cryptococcus neoformans is a eukaryotic solution to the problem of fungal trans-cell wall transport. Eukaryot. Cell. 2007;6:48–59. doi: 10.1128/EC.00318-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Rodrigues ML, et al. Extracellular vesicles produced by Cryptococcus neoformans contain protein components associated with virulence. Eukaryot. Cell. 2008;7:58–67. doi: 10.1128/EC.00370-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Yoneda A, Doering TL. A eukaryotic capsular polysaccharide is synthesized intracellularly and secreted via exocytosis. Mol Biol Cell. 2006;17:5131–5140. doi: 10.1091/mbc.E06-08-0701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Yoneda A, Doering TL. An unusual organelle in Cryptococcus neoformans links luminal pH and capsule biosynthesis. Fungal Genet. Biol. 2009;46:682–687. doi: 10.1016/j.fgb.2009.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hu G, et al. Transcriptional regulation by protein kinase A in Cryptococcus neoformans . PLoS Pathog. 2007;3:e42. doi: 10.1371/journal.ppat.0030042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Panepinto J, et al. Sec6-dependent sorting of fungal extracellular exosomes and laccase of Cryptococcus neoformans . Mol. Microbiol. 2009;71:1165–1176. doi: 10.1111/j.1365-2958.2008.06588.x. [DOI] [PubMed] [Google Scholar]
- 87.Oliveira DL, et al. Extracellular vesicles from Cryptococcus neoformans modulate macrophage functions. Infect. Immun. 2010;78:1601–1609. doi: 10.1128/IAI.01171-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Levitz SM, Specht CA. The molecular basis for the immunogenicity of Cryptococcus neoformans mannoproteins. FEMS Yeast Res. 2006;6:513–524. doi: 10.1111/j.1567-1364.2006.00071.x. [DOI] [PubMed] [Google Scholar]
- 89.Nosanchuk JD, Casadevall A. Impact of melanin on microbial virulence and clinical resistance to antimicrobial compounds. Antimicrob. Agents Chemother. 2006;50:3519–3528. doi: 10.1128/AAC.00545-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Panepinto JC, Williamson PR. Intersection of fungal fitness and virulence in Cryptococcus neoformans. FEMS Yeast Res. 2006;6:489–498. doi: 10.1111/j.1567-1364.2006.00078.x. [DOI] [PubMed] [Google Scholar]
- 91.Zhu X, Williamson PR. Role of laccase in the biology and virulence of Cryptococcus neoformans . FEMS Yeast Res. 2004;5:1–10. doi: 10.1016/j.femsyr.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 92.Perfect JR. Cryptococcus neoformans: the yeast that likes it hot. FEMS Yeast Res. 2006;6:463–468. doi: 10.1111/j.1567-1364.2006.00051.x. [DOI] [PubMed] [Google Scholar]
- 93.Brown SM, Campbell LT, Lodge JK. Cryptococcus neoformans, a fungus under stress. Curr. Opin. Microbiol. 2007;10:320–325. doi: 10.1016/j.mib.2007.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Siafakas AR, et al. Cell wall-linked cryptococcal phospholipase B1 is a source of secreted enzyme and a determinant of cell wall integrity. J. Biol. Chem. 2007;282:37508–37514. doi: 10.1074/jbc.M707913200. [DOI] [PubMed] [Google Scholar]
- 95.Cox GM, Mukherjee J, Cole GT, Casadevall A, Perfect JR. Urease as a virulence factor in experimental cryptococcosis. Infect. Immun. 2000;68:443–448. doi: 10.1128/iai.68.2.443-448.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.de Jesús-Berríos M, Liu L, Nussbaum JC, Cox GM, Stamler JS, Heitman J. Enzymes that counteract nitrosative stress promote fungal virulence. Curr. Biol. 2003;13:1963–1968. doi: 10.1016/j.cub.2003.10.029. [DOI] [PubMed] [Google Scholar]
- 97.Cox GM, Harrison TS, McDade HC, Taborda CP, Heinrich G, Casadevall A, Perfect JR. Superoxide dismutase influences the virulence of Cryptococcus neoformans by affecting growth within macrophages. Infect. Immun. 2003;71:173–180. doi: 10.1128/IAI.71.1.173-180.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Gerik KJ, Bhimireddy SR, Ryerse JS, Specht CA, Lodge JK. PKC1 is essential for protection against both oxidative and nitrosative stresses, cell integrity, and normal manifestation of virulence factors in the pathogenic fungus Cryptococcus neoformans . Eukaryot. Cell. 2008;7:1685–1698. doi: 10.1128/EC.00146-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hu G, et al. PI3K signaling of autophagy is required for starvation tolerance and virulence of Cryptococcus neoformans . J. Clin. Invest. 2008;118:1186–1197. doi: 10.1172/JCI32053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Rhome R, Del Poeta M. Lipid signaling in pathogenic fungi. Annu. Rev. Microbiol. 2009;63:119–131. doi: 10.1146/annurev.micro.091208.073431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Bien CM, Espenshade PJ. Sterol regulatory element binding proteins in fungi: hypoxic transcription factors linked to pathogenesis. Eukaryot. Cell. 2010;9:352–359. doi: 10.1128/EC.00358-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Fan W, Kraus PR, Boily MJ, Heitman J. Cryptococcus neoformans gene expression during murine macrophage infection. Eukaryot. Cell. 2005;4:1420–1433. doi: 10.1128/EC.4.8.1420-1433.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Hu G, Cheng P-Y, Sham A, Perfect JR, Kronstad JW. Metabolic adaptation in Cryptococcus neoformans during early murine pulmonary infection. Mol. Microbiol. 2008;69:1456–1475. doi: 10.1111/j.1365-2958.2008.06374.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Lin X, Heitman J. The biology of the Cryptococcus neoformans species complex. Annu. Rev. Microbiol. 2006;60:69–105. doi: 10.1146/annurev.micro.60.080805.142102. [DOI] [PubMed] [Google Scholar]
- 105.O’Meara TR, et al. Interaction of Cryptococcus neoformans Rim101 and protein kinase A regulates capsule. PLoS Pathog. 2010;6:e1000776. doi: 10.1371/journal.ppat.1000776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Jung WH, Sham A, White R, Kronstad JW. Iron regulation of the major virulence factors in the AIDS-associated pathogen Cryptococcus neoformans . PLoS Biol. 2006;4:e410. doi: 10.1371/journal.pbio.0040410. [DOI] [PMC free article] [PubMed] [Google Scholar]