Abstract
Kokua Kalihi Valley, a federally qualified health center in Hawaii, collaborated with the National Heart, Lung, and Blood Institute to test the efficacy of community health workers (CHWs) to deliver the Healthy Heart, Healthy Family curriculum to low-income Filipinos with cardiovascular disease (CVD) risk factors. At 12 months, significant improvements were seen in health behaviors, knowledge, and self-efficacy in managing chronic diseases. We also observed decreases in total cholesterol from 186.25 mg/dl to 170.88 mg/dl (p5.001), low-density lipoprotein from 114.43 mg/dl to 103.04 mg/dl (p5.013), and fasting blood glucose from 117.95 mg/dl to 109.07 mg/dl (p5.034). Although these changes were statistically significant, they are small and not clinically meaningful in reducing CVD risk. The high-density lipoprotein was 3.3 mg/dl lower (worse) at 12 months (p5.003), mean values for blood pressure, BMI, and waist circumference increased. Community health workers can be trained to deliver evidence-based curricula that improve health behaviors and increase self-efficacy in managing chronic diseases.
Keywords: Asian Americans, cardiovascular disease, cardiovascular risk factors, community health workers, cultural competency, Filipino Americans, health education
Cardiovascular disease (CVD) is the leading cause of death among Filipino Americans, and CVD mortality rates are higher among Filipino Americans than among other ethnic groups.1 In addition to high prevalence of CVD, Filipino Americans are more likely to have hypertension than other Asian American groups.2 For Filipino Americans who are also facing poverty, limited English language and cultural barriers make preventative care and treatment for CVD especially challenging.
Federally qualified health centers (FQHC) provide preventive and primary care to the uninsured and underserved, with the mission to reduce health disparities and improve outcomes.3 Kokua Kalihi Valley Comprehensive Family Services (KKV) is a FQHC in Kalihi Valley, Honolulu, a health professional shortage area.4 This neighborhood has attracted large populations of immigrants from the Philippines who come to the United States (U.S.) for family reunification, better health care, work, and educational opportunities. More than 30% of KKV’s patients are low-income Filipinos. Many arrive with chronic conditions that have progressed to advanced stages, and arrive uninsured and unable to navigate the U.S. health care system.
Community health workers (CHW) are important in FQHCs, providing assistance to people with low health literacy and limited English proficiency. They are typically from the community they serve, may be bilingual, and have some health or social service training.5 Their educational backgrounds vary, from high school graduates to college degrees. At KKV, CHWs are salaried employees occupying a wide range of positions, including outreach worker, case manager, medical assistant, and educator. Community health workers have various functions that include improving access to care, health education, patient navigation, case management, interpretation, social support, community advocacy, referrals, and linking families to community resources. The use of CHWs as extenders of the chronic care disease management team is essential in helping reduce cultural barriers and improving care coordination for low-income, immigrant clients.6
Healthy Heart, Healthy Family is a curriculum to prevent and control CVD specifically created for Filipino Americans by the National Heart, Lung, and Blood Institute (NHLBI) at the National Institutes of Health,7 adapted from existing NHLBI community group education curricula. The curriculum is designed to be taught by CHWs to small groups of 8–12 people. Eleven educational lessons (Box 1) aim to help participants build skills to make practical, lasting changes to help fight CVD and improve health. Trainers use a facilitative teaching style to keep participants motivated and to promote adult learning. Features include heart-healthy bingo and other interactive activities, cultural adaptations, Tagalog translations, use of picture cards, and six easy-to-read bilingual booklets on heart-healthy living.
The objective of this 12-month study was to evaluate the impact of the CHW-delivered Healthy Heart, Healthy Family curriculum on low-income Filipinos with CVD risk factors in Hawaii. Evaluation measures included 1) clinical outcomes; 2) knowledge of healthy habits; 3) satisfaction with curriculum; 4) quality of life; and 5) self-efficacy.
Box 1. HEALTHY HEART, HEALTHY FAMILY EDUCATIONAL LESSONS.
Knowledge is power: Know your risk for heart disease
Act in time to heart attack signs
Get energized! Say YES to physical activity
Help your heart: Control your high blood pressure
Be heart smart: Keep your cholesterol in check
Keep your heart in mind: Aim for a healthy weight
Protect your heart: Prevent and control diabetes
Welcome heart healthy eating into your home
Eat in a heart healthy way—Even when time or money is tight
Take control of your health: Enjoy living smoke free
Review and graduation
Methods
Study design
A one-group pre-post-test, design was used. Institutional review board approval was obtained from the University of Hawaii. A total of 99 participants provided written consent for participation and review of their medical records.
Participant recruitment
Recruitment strategies included informational flyers and posters, direct invitation by KKV physicians, and community outreach. From June 2008 to July 2009, 99 Filipinos adults with CVD risk factors (such as hypertension, diabetes, high cholesterol, obesity, family history, smoking, and sedentary lifestyle) were recruited.
CHW recruitment and training
Three CHWs from KKV attended a training sponsored by NHLBI and the Health Resources and Services Administration to learn how to lead the program, and later trained eight other CHWs. A total of 11 CHWs participated in this study. All were fluent in English, Tagalog, and/or Ilokano, the two Filipino languages spoken in Hawaii. Five occupied social service positions, four were medical assistants, and two were educators. As part of their job description at KKV, CHWs perform home visits and outreach to a panel of 20–25 clients, so have a good understanding of the context within which behavior change needs to take place.
Activities
The curriculum was delivered to six small groups of participants, each with two CHW facilitators. Sessions, each two hours in duration, were held weekly for 11 consecutive weeks. Incentives (water bottles and pedometers) and healthy snacks were provided. Mean attendance was seven sessions, with 65% of participants attending nine or more sessions. To encourage participants to adopt recommendations for exercise, physical activity (e.g., twice weekly Chairobics) and community gardening programs were offered and led by CHWs. After the 11 weeks, CHWs organized monthly activities promoting heart-healthy behaviors around themes such as Heart Day, Family Day, and Mother’s Day.
Measures
Most measures were provided with the curriculum. Demographic variables included age, gender, education, marital status, primary language, time in U.S., poverty level, insurance, and housing. Participation in sessions, exercise, and monthly activities was tracked. Data to assess effectiveness were collected at baseline, 6 months, and 12 months. Disease and medication histories were taken, and clinical measures included weight, height, body mass index (BMI), waist circumference, blood pressure, fasting blood glucose, fasting lipid profile, and glycosylated hemoglobin. A pre-post health habits survey was used. The 25 food consumption questions (scored on a 4-point scale from 15never to 45most of the time) asked about sodium consumption, fat consumption, and weight management. Nine items on physical activity, three on smoking, and four on alcohol use were scored yes/no or ordinally. Thirteen knowledge items were scored yes/no/don’t know. The final item was a story about a family whose members were at different stages of readiness to adopt a healthy lifestyle, based on the Transtheoretical Model of Behavior Change.8
We supplemented the NHLBI forms with two other validated tools. The six-item Stanford Self-efficacy Scale for chronic diseases asked about the level of confidence a participant had in managing his/her disease and keeping symptoms from interfering with daily activities. Response options were on a Likert scale from 1=not at all confident to 10=totally confident.9 The 16-item Flanagan Quality of Life Scale (QOLS) asked participants to rate their life in relation to five conceptual domains: material and physical well-being; relationships; social, community, and civic activities; personal development; and fulfillment and recreation.10 It is scored on a Likert scale from 1=terrible to 7=delighted. The QOLS, created originally by American psychologist John Flanagan in the 1970s, has been adapted for use in chronic illness groups. It is a valid instrument for measuring quality of life across patient groups and cultures and is conceptually distinct from health status or other causal indicators of quality of life.11
Analysis
Data were analyzed using SPSS.12 To assess changes in knowledge, behavioral, and clinical measures, we compared baseline and 12-month values using paired t-tests for continuous variables and chi-squared tests for categorical variables. Clinical data were adjusted for age and gender based on the 2000 Census.
Results
The mean age of the 99 participants enrolled in the study was 68.5 years, with a median of 69 years and a range of 25–85 years; 16.2% were male and 83.8% were female (Table 1). Seventy percent were at or below 100% of federal poverty level. Most participants lived with extended family, and only 3% lived in public housing. Nearly half had limited education, of eighth-grade or less. The sample had a mean time in the U.S. of 15.9 years, and 77% were from the Northern Philippines. Tagalog was the first language for about 8%, and Ilokano was the first language of most others. Participants had many risk factors for CVD; for example, 81.5% had high cholesterol, 81.5% had hypertension, 34.8% had diabetes, 32.6% had family history of CVD, 40.2% were overweight, and 15.2% were obese.
Table 1.
BASELINE CHARACTERISTRICS OF INITIAL SAMPLE, DROPOUTS, AND FINAL SAMPLE
| Characteristic | Initial sample n=99 |
Dropouts n=7 |
Final sample n=92 |
|
|---|---|---|---|---|
| Gender | Male | 16 (16.2%) | 1 (14.3%) | 15 (16.3%) |
| Female | 83 (83.8%) | 6 (85.7%) | 77 (83.7%) | |
| Public housing resident |
No | 96 (97.0%) | 6 (85.7%) | 90 (97.8%) |
| Poverty level (federal) |
< 100% | 70 (70.7%) | 5 (71.4%) | 65 (70.7%) |
| 100–199% | 17 (17.2%) | 1 (14.3%) | 16 (16.2%) | |
| 200 or higher | 10 (101%) | 1 (14.3%) | 9 (9.1%) | |
| Education | 8th grade or less | 48 (48.5%) | 1 (14.3%) | 47 (51.1%) |
| High school graduate | 24 (24.3%) | 1 (14.3%) | 21 (22.8%) | |
| 1–3 years of college | 14 (14.1%) | 3 (42.9%) | 11 (12.0) | |
| College graduate | 13 (13.1%) | 0 | 13 (14.1%) | |
| Primary language | Tagalog | 8 (8.1%) | 1 (14.3%) | 7 (7.6%) |
| Ilokano | 81 (81.8%) | 6 (85.7%) | 75 (81.5%) | |
| Both | 6 (6.1%) | 0 | 6 (6.5%) | |
| Other | 4 (4.0%) | 0 | 4 (4.3%) | |
| Cardio Vascular Disease risk factors |
High cholesterol | 81 (81.8%) | 6 (85.7%) | 75 (81.5%) |
| Hypertension | 80 (80.8%) | 6 (85.7%) | 74 (81.5%) | |
| Diabetes | 34 (34.3%) | 2 (28.6%) | 32 (34.8%) | |
| Family history | 32 (32.3%) | 2 (28.6%) | 30 (32.6%) | |
| Overweight | 39 (39.4%) | 2 (28.6%) | 37 (40.2%) | |
| Obese | 15 (15.32) | 1 (14.3%) | 14 (15.2%) | |
| Sedentary | 14 (14.1%) | 1 (14.3%) | 13 (14.1%) | |
| Smoking | 5 (5.0%) | 0 | 5 (5.4%) |
Between baseline and the 12-month follow up, seven participants were lost to follow up. Thus, analysis of over-time changes was limited to 92 individuals for whom we had complete data. There were no significant differences in demographic characteristics of the full (n=99) and follow-up (n=92) groups. The seven participants who dropped out shared central characteristics (six were female and the majority spoke Ilokano, and had many risk factors for CVD (see Table 2).
Table 2.
AGE-ADJUSTED CLINICAL MEASURES AT BASELINE AND 12 MONTHS (N=92)
| Variable | Baseline | 12 Months | p-value | Standard error |
|---|---|---|---|---|
| Total Cholesterol (mg/dl) | 186.25 | 170.88 | .001 | 4.399 |
| Low density lipoprotein (mg/dl) | 114.43 | 103.04 | .013 | 4.401 |
| High density lipoprotein (mg/dl) | 44.29 | 40.99 | .003 | 1.069 |
| Triglycerides (mg/dl) | 139.86 | 136.51 | .610 | 6.541 |
| Systolic BP (mmHg) | 122.60 | 124.87 | .376 | 2.471 |
| Diastolic BP (mmHg) | 74.24 | 74.29 | .922 | 1.208 |
| Hemoglobin A1C (%) | 6.65 | 6.61 | .317 | 0.045 |
| Body Mass Index | 28.56 | 30.73 | .457 | 2.898 |
| Waist circumference (cms) | 36.23 | 36.63 | .182 | 0.298 |
| Fasting blood glucose (mg/dl) | 117.95 | 109.07 | .034 | 4.080 |
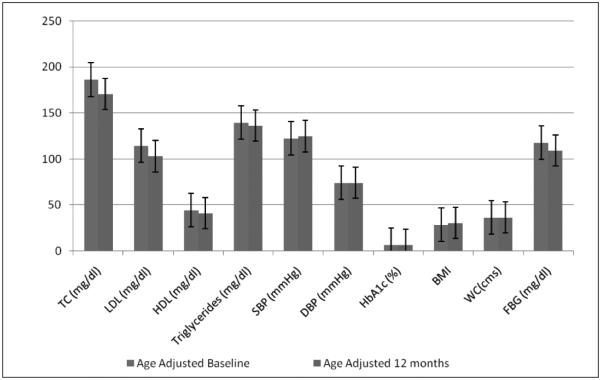
Participants showed small improvements on three of the clinical measures, which were adjusted for age and gender based on the 2000 U.S. Census (Table 2 and Figure 1). Mean total cholesterol decreased from 186.25 mg/dl at baseline to 170.88 mg/dl at 12 months (p5.001); mean low-density lipoprotein decreased from 114.43 mg/dl to 103.04 mg/dl (p5.013); and mean fasting blood glucose decreased from 117.95 mg/dl to 109.07 mg/dl, (p5.034). However, the high-density lipoprotein (HDL) was 3.3 mg/ dl lower (worse) at 12 months (p5.003). Although these changes were statistically significant, they are small and not clinically meaningful in reduction of CVD risk. Additionally, the mean value for hemoglobin A1C (%) did not change. At 12 months, mean values for BMI and waist circumference had increased, but increases were not statistically significant.
Figure 1.
Clinical measures at baseline and 12 months (n= 92).
TC = Total cholesterol
LDL = Low-density lipoprotein
HDL = High-density lipoprotein
SBP = Systolic blood pressure
DBP = Diastolic blood pressure
HbA1c = Glycosylated hemoglobin
BMI = Body mass index
WC = Waist circumference
FBG = Fasting blood glucose
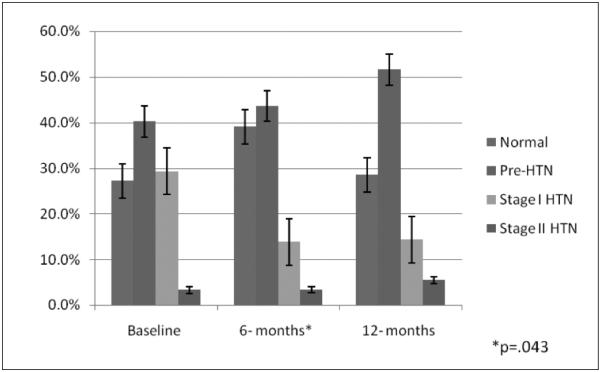
Blood pressure reductions were seen at six months, but were not sustained at 12 months. The mean systolic blood pressure decreased from 122.60 mmHg at baseline to 116.61 mmHg at six months (p5.001), and mean diastolic blood pressure decreased from 74.24 mmHg at baseline to 71.35 mmHg at six months (p5.03). Between base-line and six months, there was also a significant decrease (p5.043) in the proportion of participants who were categorized as either being normotensive, pre-hypertensive, or as Stage 1 and 2 hypertensive (Figure 2). These improvements were not sustained, as mean blood pressure readings at 12 months were very similar to those at baseline (124.87 mmHg and 74.29 mmHg, respectively).
Figure 2.
Stages of hypertension at baseline, 6 months, and 12 months (n=92).
Changes in self-efficacy scores are shown in Table 3. Statistically significant improvements were seen in participants’ confidence in managing fatigue (p5.005), emotional distress (p5.01), and keeping CVD from affecting everyday life (p5.013). Improvements were seen in confidence to manage physical discomfort and reduce doctor visits, but these were not statistically significant. There were no significant changes in the quality of life of the participants except for in material comforts.
Table 3.
SELF-EFFICACY FOR MANAGING CHRONIC DISEASE (N=92)
| Variable | Baseline | 12 months | p-value | Standard error |
|---|---|---|---|---|
| Fatigue | 7.69 | 8.38 | .005 | .239 |
| Physical discomfort | 7.76 | 8.25 | .062 | .256 |
| Emotional distress | 7.56 | 8.77 | .01 | 1.029 |
| Other health problems | 7.73 | 8.13 | .13 | .261 |
| Reduce doctor visits | 8.19 | 8.56 | .068 | .198 |
| Keep illness from affecting everyday life | 8.10 | 8.63 | .013 | .212 |
Findings from the health habits questionnaire revealed significant improvements on nine of the 25 food consumption items. For example, compared with baseline, significantly greater proportions of participants were reading nutrition labels, eating fruits for dessert, snacking on vegetables and fruits, replacing salt with herbs and spices, using monounsaturated and polyunsaturated cooking oils, and baking instead of frying at 12 months (Table 4). Additionally, the number of participants performing physical activity in the form of aerobic exercise increased from 16.7% at baseline to 43.2% at 12 months (p<.001). Only five participants reported smoking at baseline, and this number did not change. Eight reported drinking alcohol at baseline, but only three reported drinking at the 12-month follow up.
Table 4.
FREQUENCY AND PROPORTION PERFORMING HEALTH BEHAVIORS ALL OR MOST OF THE TIME (N=92)
| Behavior | Baseline n (%) |
12 months n (%) |
p-value |
|---|---|---|---|
| Use vegetable oil spray | 40 (43.5%) | 56 (60.9%) | .002 |
| Read nutrition labels | 52 (56.5%) | 65 (70.7%) | .02 |
| Remove the skin off the chicken | 46 (50%) | 70 (76.1%) | <.001 |
| Use monounsaturated and polyunsaturated cooking oils |
64 (69.6%) | 74 (80.4%) | .03 |
| Aerobic exercise | 15 (16.7%) | 36 (39.1%) | <.001 |
| Replace salt with herbs and spices | 5 (5.5%) | 15 (16.3%) | .02 |
| Snack on fruits and vegetables | 56 (60.9%) | 73 (79.4%) | .001 |
| Bake instead of fry | 31 (33.7%) | 55 (59.8%) | <.001 |
| Eat fruits for dessert | 55 (59.8) | 74 (80.4%) | .001 |
Compared with baseline, significantly greater proportions of participants got correct answers on 12 of the 13 CVD knowledge questions at 12 months and felt more confident in their abilities to cook heart-healthy foods (Table 5). On the stages-of-change story questions, significantly more participants reported identifying with family members in the preparation, action, and maintenance stages of readiness (p<.001), rather than the pre-contemplation and contemplation stages (not shown in table). Of the 92 participants, all but three reported being satisfied or very satisfied with the curriculum, and 91% reported sharing curriculum information with their families (not shown in table).
Table 5.
FREQUENCY AND PROPORTION WITH CORRECT ANSWERS ON CVD KNOWLEDGE (N=92)
| Question | Baseline n (%) |
12 months n (%) |
p-value |
|---|---|---|---|
| Can high waist measure increase risk of Cardio Vascular Disease? |
42 (45.7%) | 56 (60.9%) | .03 |
| Can Body Mass Index tell you if you are overweight? |
41 (44.6%) | 69 (75.0%) | <.001 |
| Does your liver make all the cholesterol your bodyneeds to keep you healthy? |
26 (28.3%) | 56 (60.1%) | <.001 |
| Can eating foods high in sodium increase your risk of Hypertension? |
67 (72.3%) | 88 (95.6%) | <.001 |
| Does lard have a low amount of saturated fat? | 27 (29.3%) | 59 (64.1%) | <.001 |
| Can eating too much saturated fat and trans fat raise your cholesterol? |
63 (68.4%) | 82 (89.1%) | <.001 |
| Is blood pressure of 140/90 considered high? | 71 (77.2%) | 84 (91.3%) | .003 |
| Do people know their cholesterol is high because they have gained weight? |
72 (78.3%) | 82 (89.1%) | .056 |
| Is being physically active a way to reduce your risk for health disease? |
79 (85.9) | 87 (94.6%) | .036 |
| Do you think only people with high blood cholesterol should follow a health healthy diet? |
53 (57.6%) | 69 (75.0%) | .009 |
| Can nonsmokers die from secondhand smoke? | 70 (76.1%) | 85 (82.4%) | <.001 |
| Is having a fasting blood sugar of 126 mg/dl or higher considered diabetes? |
44 (47.8%) | 71 (77.2%) | <.001 |
| Is having a waist measurement greater than 35 inches healthy for a woman? |
33 (35.9%) | 53 (57.6%) | .002 |
| How confident are you in your ability to cook heart healthy foods?a |
59 (64.1%) | 77 (83.7%) | .003 |
Shown are those who were confident or very confident.
We compared knowledge and health habit outcomes across the six intervention groups because groups were conducted by different CHWs. Group 2 participants, who had the poorest health habits at baseline, showed the most gains. Other groups showed more modest gains. Overall, however, this analysis suggested that CHWs did an equitable job of improving knowledge and health behaviors.
Discussion
Our study produced several important findings. First, the Healthy Heart, Healthy Family curriculum designed for Filipino Americans was attractive to and appreciated by low-income Filipino immigrants in Hawaii. In addition to CVD risk factors, our participants presented with many challenges, including limited English proficiency, low health literacy, poverty, and unfamiliarity with CVD risk and the U.S. health care system. The low attrition rate and the active and sustained engagement of the participants in this program suggest that the curriculum resonated well with this group.
Second, the study shows that CHWs were able to learn the curriculum and train others in the curriculum. The Healthy Heart Healthy Family manual guided their delivery and served as a valuable training resource to promote behavior modification and help participants build skills to make practical and lasting changes to fight heart disease.
Employing CHWs in program delivery also conferred other benefits. For example, we attribute the low attrition and high participation rates to the linguistic and cultural competence of the CHWs, including one CHW who has been working at KKV for nearly 30 years and is well connected within the Filipino community. Because our CHWs knew the participants’ culture and their CHW roles, they were able to reinforce the curriculum’s messages through regular outreach and support. They also were success- ful in linking participants to services at the FQHC, including clinical care and health promotion activities. Finally, the CHWs were familiar with Filipino cultural values of pakikisama (togetherness), bayanihan (community spirit), and utang-na-loob (obligation and reciprocity). They overtly recognized and encouraged these values, which helped foster cohesiveness between the CHWs and the participants. Education and group wellbeing both are highly valued in Filipino culture. Thus, participants developed a sense of responsibility to the group and the CHW instructors, which facilitated their retention and active participation in the program.
Third, our findings confirmed that CHW interventions can improve participant knowledge and behavior.6,13 Many immigrants to the U.S. are unfamiliar with CVD risk factors, but are eager to learn about ways to prevent and control disease. Many are also unfamiliar with the U.S. health care system, and benefit greatly from the ability of the CHWs to understand them, help increase their health care knowledge and skills, and improve their access to care.13
Fourth, we demonstrated that CHW interventions can lead to improvements in healthy behaviors. People of all ethnicities and cultures suffer from CVD. In a 52-country study, Yusef et al. confirmed that abnormal lipid values, smoking, hypertension, diabetes, abdominal obesity, psychosocial factors, low fruit and vegetable consumption, and lack of regular physical activity account for most of the CVD risk in all ages and both sexes worldwide.14 Unfortunately, we did not realize the meaningful clinical outcomes we were hoping for, possibly because of the advanced age of the participants and the short follow-up (12 months).
Limitations of this study were its small sample size and the fact that data on health habits were collected from participants and may be subject to recall bias. Additionally, participants may have over-reported their adherence to program recommendations in an effort to please the CHWs (social desirability bias). Further, there was no attempt at randomization and no control group due to limited funds for this study. Because the Health Heart, Healthy family promoted a low-salt and low-cholesterol diet, it is possible that some participants restricted fats dramatically, which could have contributed to the increase in HDL (as some low fat diets decrease HDL apolipoprotein transport rates).15
The study’s strengths include its unique setting and population whose CVD needs have not been studied previously. Although the population of Asian Americans in the U.S. has increased dramatically over the last few decades, limited data are available on Filipinos and their heart health.16 We present a successful model of education and services delivered by CHWs that positively improved knowledge of cardiovascular health and behaviors to reduce CVD risk among low-income, immigrant Filipinos.
Poor health of people worldwide is largely associated with poverty, overcrowding, poor hygiene, and environmental contamination, aggravated by inadequate health promotion and disease prevention. As these groups move from traditional to modern lifestyles, they acquire diseases such as obesity, cardiovascular disease, and diabetes.17 Common traits of successful CVD programs include dedicated focus on the population, widespread community involvement (often through the employment of indigenous CHWs), and regularly scheduled contact between the program and participants.18 Community health workers are increasingly important as health educators and as bridges between the health care system and underserved communities.
The cultural and bilingual tools of CHWs enable them to build trust, serve as health care navigators, and connect clients to clinical and health promotion services. We demonstrated that CHWs can be trained to deliver an evidence-based, CVD risk-reducing curriculum to Filipino Americans. Although participants did not realize improvements in clinical measures, they gained knowledge about CVD risk and improved CVD-risk- related behaviors.
Acknowledgments
The research reported in this study was supported by grant H80CS00776-06-03, National Heart, Lung, and Blood Institute (NHLBI) and Health Resources and Services Administration (HRSA)/Bureau of Primary Health Care (BPHC) collaboration.
Contributor Information
Ritabelle Fernandes, Kokua Kalihi Valley Comprehensive Family Services in Honolulu.
Kathryn L. Braun, Office of Public Health Studies at the John A. Burns School of Medicine, University of Hawaii.
Jovonni R. Spinner, Division of Application of Research Discoveries, National Heart, Lung, and Blood Institute, National Institutes of Health in Bethesda, Maryland.
Cynthia Sturdevant, Kokua Kalihi Valley Comprehensive Family Services in Honolulu.
Sharonne J. Ancheta, Kokua Kalihi Valley Comprehensive Family Services in Honolulu.
Sheryl R. Yoshimura, Kokua Kalihi Valley Comprehensive Family Services in Honolulu.
Merlita Compton, Kokua Kalihi Valley Comprehensive Family Services in Honolulu.
Jo-Hsi Wang, Kokua Kalihi Valley Comprehensive Family Services in Honolulu.
Carolyn J. Lee, Kokua Kalihi Valley Comprehensive Family Services in Honolulu.
Notes
- 1.National Institutes of Health . Asian American and Pacific Islander workshops summary report on cardiovascular health (NIH Pub no. 00-3793) U.S. Department of Health and Human Services; Bethesda, MD: 2000. [Google Scholar]
- 2.Ye J, Rust G, Baltrus P, et al. Cardiovascular risk factors among Asian Americans: results from a national health survey. Ann Epidemiol. 2009 Oct;19(10):718–23. doi: 10.1016/j.annepidem.2009.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.O’Malley AS, Forrest CB, Politzer RM, et al. Health care trends, 1994–2001: what do they portend for the federal growth initiative? Health Aff. 2005 Mar-Apr;24(2):465–72. doi: 10.1377/hlthaff.24.2.465. [DOI] [PubMed] [Google Scholar]
- 4.Heath Resources and Services Administration . Shortage. Heath Resources and Services Administration; Washington, DC: 2011. [Google Scholar]
- 5.Love MB, Gardner K, Legion V. Community health workers: who they are and what they do. Health Educ Behav. 1997 Aug;24(4):510–22. doi: 10.1177/109019819702400409. [DOI] [PubMed] [Google Scholar]
- 6.Zuvekas A, Nolan L, Tumaylle C, et al. Impact of community health workers on access, use of services, and patient knowledge and behavior. J Ambulatory Care Manage. 1999 Oct;22(4):33–44. doi: 10.1097/00004479-199910000-00007. [DOI] [PubMed] [Google Scholar]
- 7.U.S. Department of Health and Human Services . Healthy heart, healthy family: a community health worker’s manual for the Filipino community. U.S. Department of Health and Human Services; Bethesda, MD: 2010. [Google Scholar]
- 8.McLeroy KR, Bibeau D, Steckler A, et al. An ecological perspective on health promotion program. Health Educ Q. 1988 Winter;15(4):351–77. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 9.Lorig KR, Sorbel DS, Ritter PL, et al. Effect of a self-management program for patients with chronic disease. Eff Clin Pract. 2001 Nov-Dec;4(6):256–62. [PubMed] [Google Scholar]
- 10.Flannagan JC. Measurement of quality of life: current state of the art. Arch Phys Med Rehabil. 1982 Feb;63(2):56–59. [PubMed] [Google Scholar]
- 11.Burckhardt CS, Anderson KL. QOLS: reliability, validity and utilization. Health Qual Life Outcomes. 2003 Oct 23;1:60. doi: 10.1186/1477-7525-1-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.IBM Corporation . IBM SPSS Statistics version 20. IBM Corporation; Armonk, NY: 2011. [Google Scholar]
- 13.Agency for Health Care Research and Quality Outcomes of community health worker interventions. Evid Rep Technol Assess. 2009 Jun;(181):1–144. A1–2, B1–14 passim. [PMC free article] [PubMed] [Google Scholar]
- 14.Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case control study. Lancet. 2004 Sep 11;364(9438):937–52. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 15.Brinton EA, Eisenberg S, Breslow JL. A low-fat diet decreases high density lipoprotein (HDL) cholesterol levels by decreasing HDL apolipoprotein transport rates. J Clin Invest. 1990 Jan;85(1):144–51. doi: 10.1172/JCI114405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.National Heart, Lung, and Blood Institute Report on a National Heart, Lung, and Blood Institute Workshop: heterogeneity in cardiometabolic risk in Asian American in the U.S. J Am Coll Cardiol. 2010 Mar 9;55(10):966–73. doi: 10.1016/j.jacc.2009.07.075. [DOI] [PubMed] [Google Scholar]
- 17.Gracey M, King M. Indigenous health part 1. Determinants and disease patterns. Lancet. 2009 Jul 4;374(9683):65–75. doi: 10.1016/S0140-6736(09)60914-4. [DOI] [PubMed] [Google Scholar]
- 18.Huffman MD, Galloway JM. Cardiovascular health in indigenous communities: successful programs. Heart Lung Circ. 2010 May-Jun;19(5–6):351–60. doi: 10.1016/j.hlc.2010.02.013. [DOI] [PubMed] [Google Scholar]