Abstract
Purpose
This study investigated the effect of the chin-down posture on the sequence of swallowing events in healthy adults.
Method
Sixteen healthy participants performed 45 5-ml thin liquid swallows during videofluoroscopy: 5 neutral head position, 30 chin-down posture, and then 10 neutral head position. Eight swallowing events were measured: the time of hyoid burst, bolus head in the pharynx, bolus tail in the pharynx, laryngeal vestibule closure (LVC), upper esophageal sphincter (UES) opening, bolus head in the UES, bolus tail exiting the pharynx, and laryngeal vestibule opening (LVO).
Results
Our key finding is that LVC was one of the first 3 swallowing events in 69% of neutral swallows and in 78% of chin-down swallows (p = .006). Also, LVO occurred last in 14% of chin-down swallows but never occurred last in the preceding neutral swallows (p ≤ .001). Thus, in chin-down swallows, LVC occurred earlier and LVO occurred later.
Conclusions
The chin-down posture may be beneficial for individuals with delayed onset of LVC and reduced duration of the LVC. Future studies are needed to examine this effect in individuals with dysphagia.
Many research studies have explored the sequence of the events of swallowing and have revealed that there is considerable variability between and within healthy individuals (Cook et al., 1989; Gay, Rendell, Spiro, Mosier, & Lurie, 1994; Kendall, 2002; Kendall, Leonard, & McKenzie, 2003; Kendall, McKenzie, Leonard, Gonçalves, & Walker, 2000; Logemann et al., 2000; Logemann, Pauloski, Rademaker, & Kahrilas, 2002; McConnel, Cerenko, Jackson, & Guffin, Jr., 1988; Mendell & Logemann, 2007; Ohmae, Logemann, Kaiser, Hanson, & Kahrilas, 1995). Factors contributing to this variability include bolus volume, bolus consistency, age, and gender (Cook et al., 1989; Kendall, 2002; Kendall et al., 2003; Logemann et al., 2000, 2002; Mendell & Logemann, 2007; Ohmae et al., 1995). In individuals with dysphagia, the sequence of swallowing events is different from normal swallowing, likely due to the underlying swallowing disorder (Bisch, Logemann, Rademaker, Kahrilas, & Lazarus, 1994; Ekberg, 1986). To alleviate these pathophysiologies, patients may be prescribed swallowing therapeutic techniques, such as head and neck postural adjustments (i.e., chin down, head turn) and novel swallowing maneuvers (tongue-hold swallow, effortful swallow; Bulow, Olsson, & Ekberg, 2001; Jones, Knigge, & McCulloch, 2014; Park, Kim, Oh, & Lee, 2012; Solazzo et al., 2012). However, it is not clear how these therapeutic swallowing techniques alter the sequence of swallowing events, whether positively or negatively. It is important to explore these therapeutic techniques in healthy adults to compare treatment effects on the order of swallowing events in future studies with disordered swallowing. Studies in healthy adults could establish a preferred, overall expectation of how the swallowing therapeutic technique should modify swallowing behavior.
The chin-down posture is a widely prescribed swallowing technique used in an attempt to minimize the risk of aspiration in dysphagic populations (Ekberg, 1986; Lewin, Hebert, Putnam, & DuBrow, 2001; Logemann et al., 2008; Nagaya, Kachi, Yamada, & Sumi, 2004; Rasley et al., 1993; Solazzo et al., 2011; Terre & Mearin, 2012). Chin-down swallowing is thought to increase the vallecular space while the epiglottis assumes a more protective position over the laryngeal vestibule (Balou et al., 2014; Ekberg, 1986; Logemann, 1983, 1998). Shanahan, Logemann, Rademaker, Pauloski, and Kahrilas (1993) showed that the chin-down posture eliminated aspiration in 50% of patients with neurologic impairment (Shanahan et al., 1993). We have shown that the chin-down posture increases the duration of laryngeal vestibule closure (LVC) during swallowing, but the effect disappears upon returning to swallowing in the neutral head position (Macrae, Anderson, & Humbert, 2014). Although many timing differences have been shown with the chin-down posture, there is no research detailing how this change occurs relative to other swallowing events. This is important for understanding the functional relevance of changes in LVC during the chin-down posture. For instance, it is unclear whether increased LVC duration in the Macrae et al. (2014) study occurred due to earlier closure, later reopening, or some combination of both. This information is crucial in the interpretation of LVC function because prolonged LVC duration could be most beneficial if it occurs due to earlier onset closure. It has been shown that delayed LVC onset is closely associated with aspiration that occurs before and during the swallow (Park, Kim, Ko, & McCullough, 2010). Thus, it is unknown whether longer LVC durations during chin-down swallowing translate to increased safety, unless its relationship to other swallowing events is examined. If the chin-down posture alters the sequence of swallowing events, it would be prudent to also determine whether these effects are present after returning to swallowing in a neutral head position (also known as “aftereffects”). Aftereffects, which are exaggerated movements that result after a perturbation or manipulation of a function, are important to observe because it is assumed that the effects of postural adjustments do not extend beyond actual performance of the posture.
The purpose of this study was to investigate the effect of the chin-down posture on the sequence of swallowing events in healthy adults. Participants completed a series of swallows in the following three phases: first, neutral position swallowing; second, chin-down position swallowing; and third, return to neutral position swallowing. The goal was to answer three questions: Question 1—Does chin-down swallowing alter the sequence of swallowing events? Question 2—Does the sequence of swallowing events change over the execution of multiple chin-down swallows? Question 3—Are there immediate aftereffects on the swallowing sequence of events when returning to the neutral head position after performing chin-down swallows? Overall, we hypothesized that the swallowing events related to LVC would change during chin-down swallowing (Bulow et al., 1999, 2001). In particular, we expected the following, on the basis of findings from Macrae et al (2014): (a) Longer LVC is due to later laryngeal vestibule opening (LVO), not earlier LVC; (b) any changes in swallowing sequence of events across several chin-down swallows will be stable and not change over time; and (c) no aftereffects would be found upon returning to the neutral head position. Given our emphasis on airway protection, the swallowing measures in this study included hyoid movement, LVC, and bolus flow. Others have shown that bolus clearance and upper esophageal sphincter (UES) function contribute to airway protection (Molfenter & Steele, 2014); therefore, we have included temporal measures of the UES as well.
Methods
Participants
The local institutional review board approved all procedures. Data from all participants were collected by two of the authors (different swallowing kinematic data were derived and published in Macrae et al., 2014). Sixteen participants took part in the study (mean age: 33.2 years; range = 21–54 years; 7 women, 9 men). Participants in this age range were chosen for the study because previous research has indicated that age-related changes in swallowing physiology do not become obvious until 60 to 70 years of age (Fei et al., 2013; Feng et al., 2013; Robbins et al., 2005; Robbins, Levine, Wood, Roecker, & Luschei, 1995). All participants were considered healthy and reported a negative history of swallowing, speech, and voice problems and of neurological injury or disease. No participant reported any previous knowledge of or experience with the chin-down posture.
Procedure
Participants were informed of all procedures before initiation of the study. Each participant performed 45 swallows across three phases: Phase 1, neutral position (five swallows); Phase 2, chin-down posture (30 swallows); and Phase 3, neutral position (10 swallows). Thirty swallows were predicted to be adequate to show gradual changes, due to previous research showing changes with 26 swallows (Humbert et al., 2013).
Head angle was not controlled during the chin-down position as performance of the position aimed to mimic clinical presentation and instruction. A large variance in head angle occurs when individuals are provided with basic instruction on how to perform chin-down posture (Steele, Hung, Sejdic, Chau, & Fraser, 2011). However, prior to initiating study procedures, participants were educated on how to depress their chins with minimal forward neck movement to ensure that they performed the chin-down position instead of a head-forward position (neck flexion without head flexion, as per Okada et al., 2007). The investigators monitored participant positioning throughout the procedures to ensure that an appropriate chin-down posture was maintained.
Participants were seated upright in a chair. A flexible tube was taped to the chin with the tip of the tube positioned loosely in the anterior oral cavity. Boluses of 5 ml thin liquid barium (Varibar, EZEM, Melville, NY) were delivered to the participants through the use of a syringe that was connected to this tube. The tube was necessary to eliminate the need to adjust the head between neutral and chin-down posture positions (i.e., as would be needed with cup swallows), therefore allowing participants to maintain the same chin-down posture throughout Phase 2. The tube also allowed the researcher to deliver the bolus from a distance, preventing the researcher from being in the field of view of the videofluoroscopy. Each bolus was delivered to the mouth over a 2-s period. A liquid bolus was used to eliminate the need for mastication and therefore minimize videofluoroscopy exposure time. A bolus of 5 ml was considered sufficient to induce a swallow without filling the participant up over 45 swallows. The interswallow interval was 7 s throughout the study, including 5 s for postswallow rest and 2 s for bolus delivery).
A timed presentation was coordinated with the three phases of the study, including a visual and auditory countdown (5 s), followed by an audio prompt that cued participants to swallow. The participants were asked to hold the bolus in their mouths until they heard the prompt to swallow. This allowed the videofluoroscopic recordings to be synced with the swallows. Visual cues (laptop) were combined with auditory cues for all 45 swallows due to the inability of participants to see the visual cues in the chin-down posture. For each swallow, a “swallow” screen was displayed for 2 s followed by the 5-s countdown. There was also an auditory cue to indicate when participants should switch from the neutral position to chin-down posture (Phase 2) and when to return to the postposture neutral position (Phase 3). Before commencing the procedures, to familiarize the participant, each person performed two trial swallows in each of the three study phases. The aim of these practice swallows was to acquaint the participant with the timing of the interswallow interval and the overall study procedures prior to initiation of videofluoroscopy. All participants were able to accurately follow all commands in the study.
Videofluoroscopy
Swallows were recorded with continuous videofluoroscopy acquired in the sagittal plane with a video capture rate of 30 frames per second. All image sequences were viewed during the study on a monitor and exported to an image processing system, where they were archived for off-line analysis. The field of view included the upper esophagus, UES, subglottal air column, laryngeal vestibule, pharynx, and oral cavity. Data analysis was performed by viewing the images along with a simultaneously recorded time code.
Data Analysis
Measures
Eight measures were used to investigate the sequence of events of swallowing in both the neutral and chin-down positions. These measures were chosen because they represent several bolus flow and kinematic events that are important during swallowing. We measured the following:
Hyoid burst. The first superior and/or anterior burst of motion of the hyoid bone.
Bolus head in pharynx. The first frame when the head of the bolus passes the ramus of the mandible.
Tail enter pharynx. The first frame when the bolus tail passes the ramus of the mandible.
LVC. The first frame when the laryngeal vestibule is closed and no airspace can be seen through the hyo-laryngeal structures. True vocal fold closure could not be measured because of the use of videofluoroscopy (Ohmae et al., 1995).
UES open. The first frame when the UES opens, identified by the presence of either airspace just prior to bolus entry into the UES or bolus entry into the UES.
Head into UES. The first frame of bolus entry into the UES (sometimes the same frame as the time of UES opening). When barium rests on top of a closed UES, the head of the barium bolus in this region is “U” shaped. However, when the UES opens, the head of the barium bolus is funneled in and becomes an elongated “V” shape. The first frame where the barium bolus head takes an elongated V shape was identified as the frame of the bolus head in the UES.
Tail exit pharynx. This measure was defined as the first frame at which the tail of the bolus passes the inferior point on a predefined cervical vertebra that is just below the level of the UES. One specific cervical vertebra was identified for each participant and used throughout all swallows for that participant.
LVO. First frame when the laryngeal vestibule reopens and airspace can be visualized as the epiglottis begins its return to rest position.
Analysis
A laboratory technician trimmed each videofluoroscopy recording into 45 individual swallowing clips and randomly assigned each clip a unique four-digit numerical code. Two experienced researchers completed frame-by-frame, blinded analyses of swallowing kinematics. A third investigator unblinded the data and put all swallowing events into chronological order in two different formats. The first format was simply to determine the order of each event (one through eight; ordinal data) for each swallow. The second format was to analyze each event relative to swallow onset, defined as the hyoid burst (in milliseconds; ratio data). The hyoid bone was chosen as the reference measure because it is often the first event of the swallow and because it is measured reliably during analyses (Cook et al., 1989). This second format provided both the order of events and the time intervals between events.
Comparisons and Statistical Analyses
Nonparametric statistics were used to determine differences in the ordinal data, whereas parametric statistics were used to reveal differences in ratio data. The data were broken down in two different ways (study design in Figure 1):
Figure 1.
Study design showing number of swallows, swallow type (by position), and categorization of data groupings as three phases or four periods.
One comparison is Three Phases, where all swallows within a phase were averaged and compared (Phase 1, neutral; Phase 2, chin down; and Phase 3, return to neutral). Another comparison is Four Periods, where distinct periods among the phases were extracted, averaged, and compared. We used “N” to represent “neutral,” and “P” represents “chin-down position.” These four periods included:
N1—Baseline neutral swallows (all five swallows in Phase 1).
P1—Early chin-down period (first five chin-down swallows in Phase 2).
P2—Late chin-down period (last five chin-down swallows in Phase 2).
N2—Return to neutral swallows (first five swallows in Phase 3).
We answered Question 1 (Does chin-down swallowing alter the sequence of swallowing events?) in two different ways. First, we compared the means between Phase 1 (neutral) and Phase 2 (chin down). Second, to understand the early effects of chin down, we compared N1 to P1.
To answer Question 2 (Does the sequence of swallowing events change over the execution of multiple chin-down swallows?), we completed two types of comparisons. First, we determined whether a linear trend exists throughout the 30 chin-down swallows. Second, we compared the means of early versus late chin-down swallows (P1 vs. P2).
We answered Question 3 (“Are there immediate aftereffects on the swallowing sequence of events when returning to the neutral head position after performing chin-down swallows?”) by comparing N1 to N2.
Statistical analyses were conducted with SPSS (Version 22). For the ordinal data (swallow events 1–8), a Friedman test was used to handle the dependent, nonparametric data (α < 0.05). Pairwise comparisons were run with a Wilcoxon signed-rank test, when main effects were significant. Ratio data (swallow events compared with hyoid burst in milliseconds) were analyzed with a linear mixed-effects model (Gelman & Hill, 2007) to estimate the effects of chin-down posturing on each measure. To model each measure, we determined whether there was a time period/fixed effect that was relevant to the question (i.e., Question 3 compared the means of two time periods: N1 and N2) and allowed the intercept of each person to vary. Trial number was used as a covariate to estimate trends in the data. Confidence intervals (95%) were calculated for the estimated effects to indicate the degree of uncertainty in the estimation of the parameters. Pairwise comparisons generated by the software were used in the case of statistically significant fixed effects. The Sidak method was used to correct for multiple comparisons. The software outputs adjusted p values using this method, so that any p value less than .05 can be considered statistically significant. For nonparametric Wilcoxon pairwise comparisons (3), an adjusted alpha value of p = .016 was used for significance to deal with multiple comparisons. Interrater reliability (20% of the data) and intrarater reliability (5% of the data) were analyzed using single-measure intraclass correlation coefficients. The statistical measure, Cohen's d, was determined for effect size when comparing means.
Results
A total of 315 (out of a possible 320) swallows were included in the analyses. Five swallows were excluded due to poor image quality. Every participant completed the study without reported adverse effects. Inter- and intrarater reliability showed excellent agreement between raters (≥ .91) and within raters (≥ .89). The following results are provided as either ordinal data (absolute order of event, nonparametric statistics) or ratio data (data in milliseconds where each measure is relative to hyoid burst time). Results are also separated by the two groupings (three phases or four periods), where applicable. Means, standard deviations, and probability values can be found in Table 1, Table 2, Table 3, and Table 4, and descriptive data in frequencies (%) can be found in Tables 5 and 6 for ordinal data.
Table 1.
Means, standard deviations, and p values of main effects for ordinal data (swallow events 1–8) for Phase 1 (5 neutral swallows), Phase 2 (30 chin-down swallows), and Phase 3 (10 neutral swallows).
| Ordinal data (absolute order of events) | 3 Phases | M | SD | Main effects (p) |
|---|---|---|---|---|
| Hyoid burst | Neutral (Phase 1) | 1.45 | 0.593 | < .001 |
| Chin down (Phase 2) | 1.48 | 0.715 | ||
| Return to neutral (Phase 3) | 1.51 | 0.604 | ||
| Bolus head in pharynx | Neutral (Phase 1) | 1.65 | 0.532 | .038 |
| Chin down (Phase 2) | 1.78 | 0.493 | ||
| Return to neutral (Phase 3) | 1.59 | 0.518 | ||
| UES open | Neutral (Phase 1) | 3.69 | 0.493 | < .303 |
| Chin down (Phase 2) | 3.76 | 0.467 | ||
| Return to neutral (Phase 3) | 3.73 | 0.471 | ||
| Laryngeal vestibule closure | Neutral (Phase 1) | 3.49 | 1.043 | < .001 |
| Chin down (Phase 2) | 3.21 | 1.146 | ||
| Return to neutral (Phase 3) | 3.47 | 0.992 | ||
| Bolus head in UES | Neutral (Phase 1) | 4.73 | 0.477 | < .008 |
| Chin down (Phase 2) | 4.80 | 0.439 | ||
| Return to neutral (Phase 3) | 4.74 | 0.507 | ||
| Bolus tail enter pharynx | Neutral (Phase 1) | 5.95 | 0.352 | < .607 |
| Chin down (Phase 2) | 5.97 | 0.282 | ||
| Return to neutral (Phase 3) | 5.94 | 0.453 | ||
| Laryngeal vestibule open | Neutral (Phase 1) | 6.99 | 0.112 | < .001 |
| Chin down (Phase 2) | 7.13 | 0.367 | ||
| Return to neutral (Phase 3) | 7.03 | 0.260 | ||
| Bolus tail exit pharynx | Neutral (Phase 1) | 7.99 | 0.112 | < .001 |
| Chin down (Phase 2) | 7.86 | 0.358 | ||
| Return to neutral (Phase 3) | 7.94 | 0.261 |
Note. UES = upper esophageal sphincter.
Table 2.
Means, standard deviations, and p values and F statistics of fixed effects for ratio data (milliseconds relative to hyoid burst) for Phase 1 (5 neutral swallows), Phase 2 (30 chin-down swallows), and Phase 3 (10 neutral swallows).
| Ratio data (events relative to hyoid burst) | 3 Phases | M (ms) | SD | Fixed effects |
|
|---|---|---|---|---|---|
| p | F | ||||
| Bolus head in pharynx | Neutral (Phase 1) | 16 | 83 | .428 | 0.942 |
| Chin down (Phase 2) | 20 | 97 | |||
| Return to neutral (Phase 3) | 7 | 111 | |||
| Laryngeal vestibule closure | Neutral (Phase 1) | 139 | 68 | < .001 | 8.2 |
| Chin down (Phase 2) | 82 | 168 | |||
| Return to neutral (Phase 3) | 136 | 89 | |||
| UES open | Neutral (Phase 1) | 146 | 48 | < .001 | 52.1 |
| Chin down (Phase 2) | 152 | 57 | |||
| Return to neutral (Phase 3) | 156 | 55 | |||
| Bolus head in UES | Neutral (Phase 1) | 153 | 52 | < .001 | 52.5 |
| Chin down (Phase 2) | 161 | 59 | |||
| Return to neutral (Phase 3) | 161 | 56 | |||
| Bolus tail enter pharynx | Neutral (Phase 1) | 290 | 81 | < .001 | 63.0 |
| Chin down (Phase 2) | 301 | 95 | |||
| Return to neutral (Phase 3) | 306 | 87 | |||
| Laryngeal vestibule open | Neutral (Phase 1) | 580 | 87 | < .001 | 382.8 |
| Chin down (Phase 2) | 619 | 100 | |||
| Return to neutral (Phase 3) | 603 | 78 | |||
| Bolus tail exit pharynx | Neutral (Phase 1) | 686 | 75 | < .001 | 464.6 |
| Chin down (Phase 2) | 686 | 98 | |||
| Return to neutral (Phase 3) | 717 | 98 | |||
Note. UES = upper esophageal sphincter.
Table 3.
Means, standard deviations, and p values of main effects for ordinal data (swallow events 1–8) for neutral (N1; five neutral swallows), chin-down early (P1; early or first five chin-down swallows), chin-down late (P2; late or last five chin-down swallows), and return to neutral (N2; first five return to neutral swallows).
| Ordinal data (absolute order of events) | 4 Periods | M | SD | Main effects (p) |
|---|---|---|---|---|
| Hyoid burst | N1 | 1.45 | 0.593 | < .001 |
| P1 | 1.48 | 0.677 | ||
| P2 | 1.48 | 0.695 | ||
| N2 | 1.47 | 0.574 | ||
| Bolus head in pharynx | N1 | 1.65 | 0.532 | .088 |
| P1 | 1.78 | 0.547 | ||
| P2 | 1.76 | 0.486 | ||
| N2 | 1.62 | 0.514 | ||
| Laryngeal vestibule closure | N1 | 3.49 | 1.043 | .004 |
| P1 | 3.09 | 1.052 | ||
| P2 | 3.18 | 1.125 | ||
| N2 | 3.46 | 1.01 | ||
| UES open | N1 | 3.69 | 0.493 | .05 |
| P1 | 3.81 | 0.455 | ||
| P2 | 3.81 | 0.482 | ||
| N2 | 3.73 | 0.445 | ||
| Bolus head in UES | N1 | 4.73 | 0.477 | < .09 |
| P1 | 4.89 | 0.392 | ||
| P2 | 4.82 | 0.474 | ||
| N2 | 4.72 | 0.505 | ||
| Bolus tail enter pharynx | N1 | 5.95 | 0.352 | .724 |
| P1 | 5.95 | 0.316 | ||
| P2 | 5.94 | 0.434 | ||
| N2 | 6 | 0 | ||
| Laryngeal vestibule open | N1 | 6.99 | 0.112 | < .001 |
| P1 | 7.19 | 0.395 | ||
| P2 | 7.09 | 0.367 | ||
| N2 | 7.05 | 0.222 | ||
| Bolus tail exit pharynx | N1 | 7.99 | 0.112 | < .001 |
| P1 | 7.81 | 0.395 | ||
| P2 | 7.86 | 0.383 | ||
| N2 | 7.95 | 0.226 |
Note. UES = upper esophageal sphincter.
Table 4.
Means, standard deviations, and p values of main effects for ordinal data (swallow events 1–8) for neutral (N1; five neutral swallows), chin-down early (P1; early or first five chin-down swallows), chin-down late (P2; late or last five chin-down swallows), and return to neutral (N2; first five return to neutral swallows).
| Ratio data (events relative to hyoid burst in ms) | 4 Periods | M | SD | Fixed effects |
|
|---|---|---|---|---|---|
| p | F | ||||
| Bolus head in pharynx | N1 | 16 | 83 | .940 | .133 |
| P1 | 28 | 79 | |||
| P2 | 16 | 99 | |||
| N2 | 3 | 132 | |||
| Laryngeal vestibule closure | N1 | 139.59 | 67.98 | .437 | .908 |
| P1 | 75.24 | 165.33 | |||
| P2 | 82.83 | 145.53 | |||
| N2 | 130.35 | 88.44 | |||
| UES open | N1 | 146.19 | 47.85 | .986 | .048 |
| P1 | 151.14 | 51.48 | |||
| P2 | 152.13 | 57.42 | |||
| N2 | 154.11 | 52.8 | |||
| Bolus head in UES | N1 | 153.12 | 49.5 | .952 | .113 |
| P1 | 160.38 | 52.8 | |||
| P2 | 160.05 | 56.1 | |||
| N2 | 158.73 | 52.8 | |||
| Bolus tail enter pharynx | N1 | 290.07 | 79.2 | .977 | .068 |
| P1 | 301.95 | 92.4 | |||
| P2 | 290.73 | 85.8 | |||
| N2 | 304.26 | 89.1 | |||
| Laryngeal vestibule open | N1 | 580.47 | 85.8 | .611 | .607 |
| P1 | 622.05 | 102.3 | |||
| P2 | 603.57 | 75.9 | |||
| N2 | 609.51 | 79.2 | |||
| Bolus tail exit pharynx | N1 | 686.07 | 75.24 | .808 | .324 |
| P1 | 689.7 | 102.3 | |||
| P2 | 719.4 | 100.32 | |||
| N2 | 663.3 | 69.3 | |||
Note. UES = upper esophageal sphincter.
Table 5.
Ordinal data for 3 phases showing percent occurrence of each swallowing measure as Events 1 through 8.
| Swallowing measure | Phase | 1st | 2nd | 3rd | 4th | 5th | 6th | 7th | 8th |
|---|---|---|---|---|---|---|---|---|---|
| Hyoid burst | Neutral (Phase 1) | 60 | 35 | 5 | |||||
| Chin down (Phase 2) | 64 | 22 | 14 | ||||||
| Return to neutral (Phase 3) | 55 | 40 | 5 | ||||||
| Bolus in pharynx | Neutral (Phase 1) | 38 | 59 | 3 | |||||
| Chin down (Phase 2) | 25 | 71 | 4 | ||||||
| Return to neutral (Phase 3) | 42 | 57 | 1 | ||||||
| Laryngeal vestibule closure | Neutral (Phase 1) | 3 | 5 | 61 | 5 | 25 | 1 | ||
| Chin down (Phase 2) | 10 | 7 | 57 | 5 | 21 | ||||
| Return to neutral (Phase 3) | 2 | 4 | 64 | 5 | 25 | ||||
| UES open | Neutral (Phase 1) | 1 | 29 | 70 | |||||
| Chin down (Phase 2) | 26 | 72 | 2 | ||||||
| Return to neutral (Phase 3) | 28 | 71 | 1 | ||||||
| Bolus head in UES | Neutral (Phase 1) | 1 | 25 | 74 | |||||
| Chin down (Phase 2) | 24 | 74 | 2 | ||||||
| Return to neutral (Phase 3) | 2 | 24 | 73 | 1 | |||||
| Bolus tail in pharynx | Neutral (Phase 1) | 1 | 1 | 98 | |||||
| Chin down (Phase 2) | 2 | 97 | 1 | ||||||
| Return to neutral (Phase 3) | 1 | 99 | |||||||
| Laryngeal vestibule open | Neutral (Phase 1) | 1 | 99 | ||||||
| Chin down (Phase 2) | 1 | 85 | 14 | ||||||
| Return to neutral (Phase 3) | 1 | 95 | 4 | ||||||
| Bolus tail exit pharynx | Neutral (Phase 1) | 1 | 99 | ||||||
| Chin down (Phase 2) | 14 | 86 | |||||||
| Return to neutral (Phase 3) | 1 | 8 | 91 |
Note. UES = upper esophageal sphincter.
Table 6.
Ordinal data for 4 periods (neutral [N1], chin-down early [P1], chin-down late [P2], return to neutral [N2]) showing percent occurrence of each swallowing measure as Events 1 through 8.
| Swallowing measure | Period | 1st | 2nd | 3rd | 4th | 5th | 6th | 7th | 8th |
|---|---|---|---|---|---|---|---|---|---|
| Hyoid burst | N1 | 60 | 35 | 5 | |||||
| P1 | 62 | 28 | 10 | ||||||
| P2 | 63 | 25 | 11 | ||||||
| N2 | 58 | 39 | 4 | ||||||
| Bolus in pharynx | N1 | 38 | 59 | 3 | |||||
| P1 | 28 | 66 | 6 | ||||||
| P2 | 27 | 71 | 3 | ||||||
| N2 | 39 | 60 | 1 | ||||||
| LVC | N1 | 3 | 5 | 61 | 5 | 25 | 1 | ||
| P1 | 10 | 6 | 62 | 8 | 14 | ||||
| P2 | 10 | 4 | 64 | 1 | 21 | ||||
| N2 | 4 | 1 | 65 | 4 | 26 | ||||
| UES open | N1 | 1 | 29 | 70 | |||||
| P1 | 22 | 76 | 3 | ||||||
| P2 | 23 | 73 | 4 | ||||||
| N2 | 28 | 73 | |||||||
| Bolus head in UES | N1 | 1 | 25 | 74 | |||||
| P1 | 14 | 84 | 3 | ||||||
| P2 | 22 | 75 | 4 | ||||||
| N2 | 1 | 24 | 75 | ||||||
| Bolus tail in pharynx | N1 | 1 | 1 | 98 | |||||
| P1 | 3 | 97 | |||||||
| P2 | 4 | 1 | 92 | 3 | |||||
| N2 | 100 | ||||||||
| Laryngeal vestibule open | N1 | 1 | 99 | ||||||
| P1 | 81 | 19 | |||||||
| P2 | 3 | 86 | 12 | ||||||
| N2 | 95 | 5 | |||||||
| Bolus tail exit pharynx | N1 | 1 | 99 | ||||||
| P1 | 19 | 81 | |||||||
| P2 | 1 | 11 | 88 | ||||||
| N2 | 1 | 6 | 93 |
Note. LVC = laryngeal vestibule closure; UES = upper esophageal sphincter.
Main Effects
Three Phases
Ordinal data. Six kinematic swallowing measures were significantly different, including the time of hyoid burst (p < .001), bolus head in the pharynx (p < .038), LVC (p < .001), LVO (p < .001), bolus head in the UES (p = .008), and the time the bolus tail exited the pharynx (p < .001; see Table 1).
Ratio data. For differences by milliseconds (each event relative to hyoid burst), all measures, except the time the bolus head entered the pharynx, were different, including the time of UES opening (p < .001; LVC, p < .001), head into UES (p < .001), bolus tail entering the pharynx (p < .001; LVO, p < .001), and bolus tail exiting pharynx (p < .001; see Table 2).
Four Periods
Ordinal data. LVC (p = .004), LVO (p < .001), and the order that the bolus tail exited the pharynx (p < .001) were different among N1, P1, P2, and N2 (see Table 3).
Ratio data. No statistically significant differences were found (see Table 4).
Pairwise Comparisons
Question 1: Does Chin-Down Swallowing Alter the Sequence of Swallowing Events?
Three Phases
Ordinal data. Nonparametric statistics identified statistically significant pairwise differences between Phase 1 and Phase 2 (hyoid burst, LVC, LVO, bolus head in UES, bolus head in pharynx, and bolus tail exit pharynx; all ps ≤ .001). However, the effect sizes were small (Cohen's d range = .05–.256) for all measures except the time of LVO and bolus tail exiting the pharynx. Therefore, hyoid burst, LVC, bolus head in pharynx, and bolus head in UES will not be discussed further. Medium effect sizes were found for the time the bolus tail exited the pharynx (Cohen's d = .50) and for LVO (Cohen's d = .52). Compared with neutral swallows, the 30 chin-down swallows had later LVO onset (see Table 5 and Figure 2). During Phase 1, LVO was the seventh event 99% of the time, but during chin down (Phase 2), LVO was the seventh event 85% of the time and the eighth event 14% of the time. During chin-down swallowing, the bolus tail exited the pharynx earlier than in neutral swallowing (see Table 5 and Figure 2). During Phase 1, the bolus tail exited the pharynx last (eighth event) 99% of the time, but during chin-down swallowing (Phase 2), the bolus tail exited the pharynx last 86% of the time and seventh 14% of the time.
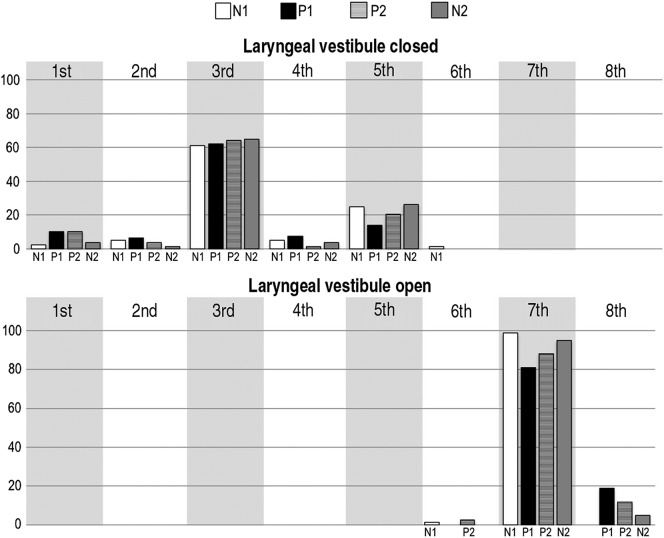
Figure 2.
The frequency (%) of each swallowing measure is plotted as events 1 through 8 by the three-phase groupings, including: Phase 1, neutral position (five swallows); Phase 2, chin-down position (30 swallows); and Phase 3, return to neutral position (10 swallows). Asterisk indicates statistical significance. UES = upper esophageal sphincter; LVC = laryngeal vestibule closure; LVO = laryngeal vestibule open.
Ratio data. Parametric statistics did not reveal any significant differences between Phase 1 (neutral) and Phase 2 (chin down) for kinematic events relative to hyoid burst.
Four Periods
Ordinal data. Nonparametric pairwise comparisons revealed statistically significant differences between N1 (five neutral swallows) and P1 (first five chin-down swallows) for LVC and LVO (see Figure 3). LVC occurred earlier during the early chin-down swallows compared with the N1 (neutral) swallows (p = .006), although the effect size was somewhat small (d = .4). LVC was one of the first three events 69% of the time in N1 swallows and 78% of the time in P1 swallows (see Table 6 and Figure 3). Conversely, LVO occurred later during the P1 swallows (first five chin-down swallows) compared with the N1 swallows (p ≤ .001), with a medium effect size (d = .7). LVO was the seventh event in 99% of N1 swallows, but in P1 swallows, it was the seventh event in 81% of the time and the eighth event 19% of the time (see Table 6 and Figure 3).
Figure 3.
The frequency (%) of each swallowing measure is plotted as events 1 through 8 across the four periods, including: all five neutral position swallows (N1), the first five chin-down swallows (P1), the last five chin-down swallows (P2), and the swallows during the return to the neutral position (N2).
Question 2: Does the Sequence of Swallowing Events Change Over the Execution of Multiple Chin-Down Swallows?
Three Phases
No trends across the 30 chin-down swallows were found.
Four Periods
Ordinal data. For comparisons between P1 (first five chin-down swallows) and P2 (last five chin-down swallows), only the LVO measure was significant (see Figures 2A and 2B). The order of LVO was significantly later during the first five chin-down swallows compared with the last five chin-down swallows (p = .016) with small effect sizes (d = .3). This difference was characterized by LVO that occurred more frequently as the seventh (81%) and eighth (19%) event in P1 swallows. In P2 swallows, LVO occurred as the sixth (3%), seventh (86%), and eighth (11%) swallowing events.
Question 3: Are There Immediate Aftereffects on the Swallowing Sequence of Events When Returning to the Neutral Head Position After Performing Chin-Down Swallows?
No measure was different for this comparison.
Discussion
Understanding the underlying mechanisms of the chin-down posture is critical due to its popular application to individuals with dysphagia in clinical practice. Although different aspects of the technique have been investigated in numerous studies, there are inconsistent findings regarding how chin-down swallowing alters swallowing function (Ekberg, 1986; Lewin et al., 2001; Logemann et al., 2008; Nagaya et al., 2004; Rasley et al., 1993; Solazzo et al., 2011; Terre & Mearin, 2012). Reaching some resolution on this topic will allow clinicians to be more specific in their prescription of chin-down swallowing to distinct dysphagia characteristics.
To add clarity on how chin-down swallowing alters swallowing airway function, we compared swallowing sequence of events between neutral position swallows and chin-down position swallows. Our results further explain our previous findings that the duration of LVC is longer during the chin-down posture compared with the neutral posture (Macrae et al., 2014). The data in the current study show that chin-down swallowing causes LVC to occur earlier in the swallow and LVO to occur later in the swallow. This effect remains stable across all 30 chin-down swallows for LVC, but not for LVO. Instead, the laryngeal vestibule opens significantly earlier by the end of the series of chin-down swallows compared with the beginning, approaching neutral position timing.
Based on the findings of this study, patients with impairments of LVC could benefit from chin-down swallowing. In Macrae et al. (2014), the duration to the onset of LVC (time between hyoid burst and LVC) was unchanged with chin-down swallowing (also supported in the present study). However, when we examined the absolute order of the events of the swallow (i.e., without using hyoid burst as a reference measure), LVC onset occurred consistently earlier among the order of the events of the swallow during chin-down swallowing. Thus, we report that chin-down swallowing causes earlier onset of LVC and could be helpful in patients with delayed LVC onset.
Overall, it has been shown in several studies that the duration of LVC is highly responsive to sensory input during swallowing. In a review of several research studies, Molfenter and Steele (2012) have concluded that the duration of LVC is strongly influenced by changes in bolus volume. It is hypothesized that a larger bolus dwells in the pharynx longer, so LVC remains closed longer to protect the airway. However, because we controlled bolus volume, our data suggest that longer LVC duration during chin-down swallowing is likely not due to changing sensory input about the bolus.
We posit that LVC onset may have occurred earlier because the hyoid bone and larynx are positioned more closely to one another when the chin is down toward the chest (Bulow et al., 1999, 2001). The approximation of these two structures is an important contributor to LVC (Fink, 1976; Fink, Martin, & Rohrmann, 1979), so chin-down swallowing might ease the process of achieving LVC by decreasing the amount of hyo-laryngeal travel time needed to achieve closure. Furthermore, Welch et al. (1993) reported narrowing of the laryngeal inlet during chin down swallowing (Welch, Logemann, Rademaker, & Kahrilas, 1993). It is plausible that the onset of bolus head entry into the pharynx could influence the reaction time of LVC onset; however, we found no difference in the timing of bolus head entry into the pharynx between neutral and chin-down swallowing. The time that the bolus head enters the pharynx is influenced by posterior lingual porpulsive forces. Hori et al. (2011) found several differential outcomes in maximal magnitude of tongue pressure in chin-down swallowing among three swallow types (dry, 5 ml, and 15 ml), but fewer differences among these three swallow types were found in neutral head position swallowing (Hori et al., 2011). This suggests that differences in the onset of bolus head entry into the pharynx might be found when measured across different bolus types or relative to lingual function rather than to swallowing kinematics.
LVO differed between neutral and chin-down positions, as well as during the chin-down position. These changes could be due to overcompensation at the start of chin-down swallowing in response to the novelty of the experience. Then, during the course of the maneuver, perhaps our healthy participants began to modify behavior to one that more similarly resembled neutral position swallowing (optimization), perhaps requiring less effort. The notion of optimization has been explored previously in swallowing (Humbert, Lokhande, Christopherson, German, & Stone, 2012) and could be the result of resuming a more efficient motor plan (most similar to a baseline neutral swallow) that does not involve unnecessarily long durations of LVC. It is less likely that longer durations of LVC during chin-down swallowing are a response to sensory cues from the bolus, because the bolus tail exited the pharynx earlier during chin-down swallows compared with neutral position swallows. Thus, LVO onset was likely not responding to a bolus that was dwelling in the pharynx for an extended period of time.
Study Limitations
This study included only younger healthy participants with no history of speech, swallowing, or neurological problems. Though studying younger healthy participants is often the first step in analyzing whether dysphagia techniques have potential (Logemann, 2005), it is unclear whether healthy older adults or individuals with dysphagia would follow the same pattern as younger healthy participants. Future research should replicate this study in healthy older adults and in individuals with dysphagia.
While performing the chin-down posture, participants maintained the same position throughout the 30 swallows and swallows are cued throughout our paradigm. This is unlike real-life application, where individuals would alternate between neutral and chin-down postures throughout a meal while swallowing spontaneously. Alternating head movements could lead to different results. Last, participants only performed 30 chin-down swallows before transitioning back to the neutral position. It is possible that a variation in the sequence of events could be observed if the posture was performed over a longer (or shorter) period of time.
Conclusion
This study provides empirical evidence of the changes of the sequence of swallowing events from a neutral head position to a chin-down posture. Differences were revealed in the events of airway closure between chin-down and neutral swallowing (LVC and LVO), as well as during the execution of multiple chin-down swallows (LVO). Our results showed that the chin-down posture could be appropriate for individuals with delayed onset of LVC or short duration of LVC. However, the effect could be transient when performed repeatedly and does not appear to generalize to subsequent swallows in the head-neutral position.
Acknowledgments
Funding for this investigation was provided by the National Institute on Deafness and Other Communication Disorders and the National Center for Medical Rehabilitation Research (5K23DC010776-05, 1R01DC01428501A1), as well as the American Heart Association (14BGIA20380348). All listed funding was awarded to Ianessa A. Humbert (Principal Investigator).
Funding Statement
Funding for this investigation was provided by the National Institute on Deafness and Other Communication Disorders and the National Center for Medical Rehabilitation Research (5K23DC010776-05, 1R01DC01428501A1), as well as the American Heart Association (14BGIA20380348). All listed funding was awarded to Ianessa A. Humbert (Principal Investigator).
References
- Balou M., McCullough G. H., Aduli F., Brown D., Stack B. C. Jr., Snoddy P., & Guidry T. (2014). Manometric measures of head rotation and chin tuck in healthy participants. Dysphagia, 29, 25–32. doi:10.1007/s00455-013-9472-y [DOI] [PubMed] [Google Scholar]
- Bisch E. M., Logemann J. A., Rademaker A. W., Kahrilas P. J., & Lazarus C. L. (1994). Pharyngeal effects of bolus volume, viscosity, and temperature in patients with dysphagia resulting from neurologic impairment and in normal subjects. Journal of Speech and Hearing Research, 37, 1041–1059. [DOI] [PubMed] [Google Scholar]
- Bulow M., Olsson R., & Ekberg O. (1999). Videomanometric analysis of supraglottic swallow, effortful swallow, and chin tuck in healthy volunteers. Dysphagia, 14, 67–72. [DOI] [PubMed] [Google Scholar]
- Bulow M., Olsson R., & Ekberg O. (2001). Videomanometric analysis of supraglottic swallow, effortful swallow, and chin tuck in patients with pharyngeal dysfunction. Dysphagia, 16, 190–195. [DOI] [PubMed] [Google Scholar]
- Cook I. J., Dodds W. J., Dantas R. O., Kern M. K., Massey B. T., Shaker R., & Hogan W. J. (1989). Timing of videofluoroscopic, manometric events, and bolus transit during the oral and pharyngeal phases of swallowing. Dysphagia, 4, 8–15. [DOI] [PubMed] [Google Scholar]
- Ekberg O. (1986). Posture of the head and pharyngeal swallowing. Acta Radiologica: Diagnosis, 27, 691–696. [DOI] [PubMed] [Google Scholar]
- Fei T., Polacco R. C., Hori S. E., Molfenter S. M., Peladeau-Pigeon M., Tsang C., & Steele C. M. (2013). Age-related differences in tongue-palate pressures for strength and swallowing tasks. Dysphagia, 28, 575–581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng X., Todd T., Lintzenich C. R., Ding J., Carr J. J., Ge Y., … Butler S. G. (2013). Aging-related geniohyoid muscle atrophy is related to aspiration status in healthy older adults. Journal of Gerontology: Series A: Biological Sciences and Medical Sciences, 68, M853–M860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fink B. R. (1976). The median thyrohyoid “fold”: A nomenclatural suggestion. Journal of Anatomy, 122, 697–699. [PMC free article] [PubMed] [Google Scholar]
- Fink B. R., Martin M. W., & Rohrmann C. A. (1979). Biomechanics of the human epiglottis. Acta Oto-Laryngologica, 87, 554–559. [DOI] [PubMed] [Google Scholar]
- Gay T., Rendell J. K., Spiro J., Mosier K., & Lurie A. G. (1994). Coordination of oral cavity and laryngeal movements during swallowing. Journal of Applied Physiology, 77(1), 357–365. [DOI] [PubMed] [Google Scholar]
- Gelman A., & Hill J. (2007). Data analysis using regression and multilevel hierarchical models. New York, NY: Cambridge University Press. [Google Scholar]
- Hori K., Tamine K., Barbezat C., Maeda Y., Yamori M., Muller F., & Ono T. (2011). Influence of chin-down posture on tongue pressure during dry swallow and bolus swallows in healthy subjects. Dysphagia, 26(3), 238–245. doi:10.1007/s00455-010-9292-2 [DOI] [PubMed] [Google Scholar]
- Humbert I. A., Christopherson H., Lokhande A., German R., Gonzalez-Fernandez M., & Celnik P. (2013). Human hyolaryngeal movements show adaptive motor learning during swallowing. Dysphagia, 28, 139–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humbert I. A., Lokhande A., Christopherson H., German R., & Stone A. (2012). Adaptation of swallowing hyo-laryngeal kinematics is distinct in oral vs. pharyngeal sensory processing. Journal of Applied Physiology, 112, 1698–1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones C. A., Knigge M. A., & McCulloch T. M. (2014). Speech pathologist practice patterns for evaluation and management of suspected cricopharyngeal dysfunction. Dysphagia, 29(3), 322–339. doi:10.1007/s00455-013-9513-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendall K. A. (2002). Oropharyngeal swallowing variability. The Laryngoscope, 112, 547–551. [DOI] [PubMed] [Google Scholar]
- Kendall K. A., Leonard R. J., & McKenzie S. W. (2003). Sequence variability during hypopharyngeal bolus transit. Dysphagia, 18, 85–91. doi:10.1007/s00455-002-0086-z [DOI] [PubMed] [Google Scholar]
- Kendall K. A., McKenzie S., Leonard R. J., Gonçalves M. I., & Walker A. (2000). Timing of events in normal swallowing: A videofluoroscopic study. Dysphagia, 15, 74–83. doi:10.1007/s004550010004 [DOI] [PubMed] [Google Scholar]
- Lewin J. S., Hebert T. M., Putnam J. B., & DuBrow R. A. (2001). Experience with the chin tuck maneuver in postesophagectomy aspirators. Dysphagia, 16, 216–219. [DOI] [PubMed] [Google Scholar]
- Logemann J. A. (1983). Evaluation and treatment of swallowing disorders. San Diego, CA: College-Hill Press. [Google Scholar]
- Logemann J. A. (1998). Evaluation and treatment of swallowing disorders (2nd ed.). Austin, TX: Pro-Ed. [Google Scholar]
- Logemann J. A. (2005). The role of exercise programs for dysphagic patients. Dysphagia, 20, 139–140. [DOI] [PubMed] [Google Scholar]
- Logemann J. A., Gensler G., Robbins J., Lindblad A. S., Brandt D., Hind J. A., … Miller Gardner P. J. (2008). A randomized study of three interventions for aspiration of thin liquids in patients with dementia or Parkinson's disease. Journal of Speech, Language, and Hearing Research, 51, 173–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logemann J. A., Pauloski B. R., Rademaker A. W., Colangelo L. A., Kahrilas P. J., & Smith C. H. (2000). Temporal and biomechanical characteristics of oropharyngeal swallow in younger and older men. Journal of Speech, Language, and Hearing Research, 43, 1264–1274. doi:1092-4388/00/4305-1264 [DOI] [PubMed] [Google Scholar]
- Logemann J. A., Pauloski B. R., Rademaker A. W., & Kahrilas P. J. (2002). Oropharyngeal swallow in younger and older women: Videofluoroscopic analysis. Journal of Speech, Language, and Hearing Research, 45, 434–445. doi:1092-4388/02/4503-0434 [DOI] [PubMed] [Google Scholar]
- Macrae P., Anderson C., & Humbert I. (2014). Mechanisms of airway protection during chin-down swallowing. Journal of Speech, Language, and Hearing Research, 57(4), 1251–1258. doi:10.1044/2014_JSHLR-S-13-0188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McConnel F. M. S., Cerenko D., Jackson R. T., & Guffin T. N. Jr. (1988). Timing of major events of pharyngeal swallowing. Archives of Otolaryngology—Head & Neck Surgery, 114, 1413–1418. [DOI] [PubMed] [Google Scholar]
- Mendell D. A., & Logemann J. A. (2007). Temporal sequence of swallow events during the oropharyngeal swallow. Journal of Speech, Language, and Hearing Research, 50, 1256–1271. doi:1092-4388/07/5005-1256 [DOI] [PubMed] [Google Scholar]
- Molfenter S. M., & Steele C. M. (2012). Temporal variability in the deglutition literature. Dysphagia, 27, 162–177. doi:10.1007/s00455-012-9397-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molfenter S. M., & Steele C. M. (2014). Kinematic and temporal factors associated with penetration-aspiration in swallowing liquids. Dysphagia, 29(2), 269–276. doi:10.1007/s00455-013-9506-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagaya M., Kachi T., Yamada T., & Sumi Y. (2004). Video-fluorographic observations on swallowing in patients with dysphagia due to neurodegenerative diseases. Nagoya Journal of Medical Science, 67, 17–23. [PubMed] [Google Scholar]
- Ohmae Y., Logemann J. A., Kaiser P., Hanson D. G., & Kahrilas P. J. (1995). Timing of glottis closure during normal swallow. Head & Neck, 17, 394–402. [DOI] [PubMed] [Google Scholar]
- Okada S., Saitoh E., Palmer J. B., Matsuo K., Yokoyama M., Shigeta R., & Baba M. (2007). What is the chin-down posture? A questionnaire survey of speech language pathologists in Japan and the United States. Dysphagia, 22(3), 204–209. doi:10.1007/s00455-006-9073-0 [DOI] [PubMed] [Google Scholar]
- Park J.-W., Kim Y., Oh J.-C., & Lee H.-J. (2012). Effortful swallowing training combined with electrical stimulation in post-stroke dysphagia: A randomized controlled study. Dysphagia, 27, 521–527. doi:10.0007/s00455-012-9403-3 [DOI] [PubMed] [Google Scholar]
- Park T., Kim Y., Ko D. H., & McCullough G. (2010). Initiation and duration of laryngeal closure during the pharyngeal swallow in post-stroke patients. Dysphagia, 25, 177–182. [DOI] [PubMed] [Google Scholar]
- Rasley A., Logemann J. A., Kahrilas P. J., Rademaker A. W., Pauloski B. R., & Dodds W. J. (1993). Prevention of barium aspiration during videofluoroscopic swallowing studies: Value of change in posture. American Journal of Roentgenology, 160, 1005–1009. [DOI] [PubMed] [Google Scholar]
- Robbins J., Gangnon R. E., Theis S. M., Kays S. A., Hewitt A. L., & Hind J. A. (2005). The effects of lingual exercise on swallowing in older adults. Journal of the American Geriatrics Society, 53, 1483–1489. [DOI] [PubMed] [Google Scholar]
- Robbins J., Levine R., Wood J., Roecker E. B., & Luschei E. (1995). Age effects on lingual pressure generation as a risk factor for dysphagia. Journal of Gerontology: Series A: Biological Sciences and Medical Sciences, 50, M257–M262. [DOI] [PubMed] [Google Scholar]
- Shanahan T. K., Logemann J. A., Rademaker A. W., Pauloski B. R., & Kahrilas P. J. (1993). Chin-down posture effect on aspiration in dysphagic patients. Archives of Physical Medicine and Rehabilitation, 74, 736–739. [DOI] [PubMed] [Google Scholar]
- Solazzo A., Del Vecchio L., Reginelli A., Monaco L., Sagnelli A., Monsorro M., … Grassi R. (2011). Search for compensation postures with videofluoromanometric investigation in dysphagic patients affected by amyotrophic lateral sclerosis. Radiologia Medica, 116, 1083–1094. [DOI] [PubMed] [Google Scholar]
- Solazzo A., Monaco L., Del Vecchio L., Tamburrini S., Iacobellis F., Berritto D., … Grassi R. (2012). Investigation of compensatory postures with videofluoromanometry in dysphagia patients. World Journal of Gastroenterology, 18(23), 2973–2978. doi:10.3748/wjg.v18.i23.2973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steele C. M., Hung D., Sejdic E., Chau T., & Fraser S. (2011). Variability in execution of the chin-down maneuver by healthy adults. Folia Phoniatrica et Logopaedica, 63, 36–42. [DOI] [PubMed] [Google Scholar]
- Terre R., & Mearin F. (2012). Effectiveness of chin-down posture to prevent tracheal aspiration in dysphagia secondary to acquired brain injury: A videofluoroscopy study. Neurogastroenterology and Motility, 24, 414–419. [DOI] [PubMed] [Google Scholar]
- Welch M. V., Logemann J. A., Rademaker A. W., & Kahrilas P. J. (1993). Changes in pharyngeal dimensions effected by chin tuck. Archives of Physical Medicine and Rehabilitation, 74, 178–181. [PubMed] [Google Scholar]