Abstract
IMPORTANCE
Myeloablative allogeneic hematopoietic stem cell transplantation (HSCT) is curative for children with severe sickle cell disease, but toxicity may be prohibitive for adults. Nonmyeloablative transplantation has been attempted with degrees of preparative regimen intensity, but graft rejection and graft-vs-host disease remain significant.
OBJECTIVE
To determine the efficacy, safety, and outcome on end-organ function with this low-intensity regimen for sickle cell phenotype with or without thalassemia.
DESIGN, SETTING, AND PARTICIPANTS
From July 16, 2004, to October 25, 2013, 30 patients aged 16–65 years with severe disease enrolled in this nonmyeloablative transplant study, consisting of alemtuzumab (1 mg/kg in divided doses), total-body irradiation (300 cGy), sirolimus, and infusion of unmanipulated filgrastim mobilized peripheral blood stem cells (5.5–31.7 × 106 cells/kg) from human leukocyte antigen–matched siblings.
MAIN OUTCOMES AND MEASURES
The primary end point was treatment success at 1 year after the transplant, defined as a full donor-type hemoglobin for patients with sickle cell disease and transfusion independence for patients with thalassemia. The secondary end points were the level of donor leukocyte chimerism; incidence of acute and chronic graft-vs-host disease; and sickle cell–thalassemia disease-free survival, immunologic recovery, and changes in organ function, assessed by annual brain imaging, pulmonary function, echocardiographic image, and laboratory testing.
RESULTS
Twenty-nine patients survived a median 3.4 years (range, 1–8.6), with no nonrelapse mortality. One patient died from intracranial bleeding after relapse. As of October 25, 2013, 26 patients (87%) had long-term stable donor engraftment without acute or chronic graft-vs-host disease. The mean donor T-cell level was 48% (95% CI, 34%–62%); the myeloid chimerism levels, 86% (95% CI, 70%–100%). Fifteen engrafted patients discontinued immunosuppression medication with continued stable donor chimerism and no graft-vs-host disease. The normalized hemoglobin and resolution of hemolysis among engrafted patients were accompanied by stabilization in brain imaging, a reduction of echocardiographic estimates of pulmonary pressure, and allowed for phlebotomy to reduce hepatic iron. The mean annual hospitalization rate was 3.23 (95%CI, 1.83–4.63) the year before, 0.63 (95% CI, 0.26–1.01) the first year after,0.19 (95% CI, 0–0.45) the second year after, and 0.11 (95%CI, 0.04–0.19) the third year after transplant. For patients taking long-term narcotics, the mean use per week was 639 mg (95%CI, 220–1058) of intravenous morphine–equivalent dose the week of their transplants and 140 mg (95% CI, 56–225) 6 months after transplant. There were 38 serious adverse events: pain and related management, infections, abdominal events, and sirolimus related toxic effects.
CONCLUSIONS AND RELEVANCE
Among 30 patients with sickle cell phenotype with or without thalassemia who underwent nonmyeloablative allogeneic HSCT, the rate of stable mixed-donor chimerism was high and allowed for complete replacement with circulating donor red blood cells among engrafted participants. Further accrual and follow-up are required to assess longer-term clinical outcomes, adverse events, and transplant tolerance.
TRIAL REGISTRATION
clinicaltrials.gov Identifier: NCT00061568
Sickle cell disease results from a single-nucleotide substitution, leading to valine replacing the normal glutamic acid in the sixth position of the β-globin protein,1 resulting in a propensity toward hemoglobin polymerization and sickling of red blood cells. Sickle cell disease is characterized by anemia, ongoing hemolysis, and acute and chronic vaso-occlusive complications affecting multiple organs. Hydroxyurea and periodic red blood cell transfusions can ameliorate manifestations of sickle cell disease, but hematopoietic stem cell transplantation (HSCT) is the only available curative option to date.2–4 Approximately 400 to 500 children with sickle cell disease worldwide have undergone HSCT after myeloablative conditioning, resulting in a sickle cell disease-free survival of 95% in the most recent series.4 Although the myeloablative conditioning allowed most of these children to achieve complete replacement of their bone marrow by that of their donors (full-donor chimerism), a smaller fraction of them demonstrated a mixture of both recipient and donor cells (mixed chimerism).5–7 This chimeric state proved sufficient for production of donor-type red blood cells and reversion of the sickle cell disease phenotype in the absence of graft-vs-host disease.6
The development of nonmyeloablative conditioning regimens, designed intentionally to allow for stable mixed chimerism, may facilitate safer application of allogeneic HSCT to eligible adults. However, early nonmyeloablative attempts did not achieve reliable long-term donor engraftment,8 were not applied to adults,9 or had severe transplant-related complications.10 Based on the ability to promote T-cell tolerance through mammalian target of rapamycin blockade with rapamycin,11 we explored a nonmyeloablative approach in a pilot group of 10 adults with a median follow-up of 30 months, using alemtuzumab, low-dose radiation, and rapamycin (sirolimus).12 This simplified HSCT regimen has few toxic effects, allows for stable mixed-donor chimerism, and is efficacious in reversing the sickle cell disease phenotype. In the initial report, none had experienced acute or chronic graft-vs-host disease, yet all patients continued taking immunosuppression medication.
We have since amended the protocol to include parameters for withdrawal of immunosuppression after assessment of the primary end point at 1 year and allowed sufficient time to monitor outcome after discontinuing immunosuppression. Additionally, we now describe the accrual of 20 more patients with updated results in the first 10, outcome of HSCT on organ function, and stability of mixed chimerism in the absence of immunosuppression.
Methods
Study Design
This study is a prospective phase 1 and 2 study of a nonmyeloablative allogeneic HSCT regimen for individuals with severe sickle cell disease and β-thalassemia. In 2003, the National Heart, Lung, and Blood Institute’s institutional review board approved the study, which began accrual in 2004 and which is monitored by an independent data safety and monitoring board. All participants gave written informed consent.
Patients 16 years or older with a human leukocyte antigen (HLA)–identical family donor and severe sickle cell phenotype were eligible: homozygous hemoglobin S, compound heterozygous hemoglobin S and C, or compound heterozygous hemoglobin S and β-thalassemia, confirmed by hemoglobin electrophoresis, high-performance liquid chromatography, DNA testing when necessary, or both (Table 1). Indications for transplant included having an end-organ complication (previous cerebrovascular event, sickle nephropathy, tricuspid regurgitant velocity >2.5 m/s, or sickle hepatopathy) or a reversible complication not ameliorated by hydroxyurea (frequent vaso-occlusive crises, acute chest syndrome, osteonecrosis, or red cell alloimmunization).2,13-15 Patients with a detectable antibody to ABO, Rh, or other red blood cell antigen of their donors were excluded. There was no upper age limit to enrollment.
Table 1.
Baseline Characteristics of Study Participants (N=30)
| Characteristics | No. (%) of Patients |
|---|---|
| Age at transplant, y | |
| Median (range) | 28.5 (17–65) |
| No. | |
| ≤20 | 3 (10) |
| 21–30 | 14 (47) |
| 31–40 | 6 (20) |
| ≥41 | 7 (23) |
| Men | 16 (53) |
| Women | 14 (47) |
| Indications for HSCTa | |
| Vaso-occlusive crisis | 23 (77) |
| Tricuspid regurgitant jet velocity, m/s | 13 (43) |
| 2.6 to 2.9 | 8 (27) |
| ≥3.0 | 5 (17) |
| CNS disease | 9 (30) |
| Stroke or silent infarct | 5 (17) |
| Stenotic or irregular arteries | 2 (7) |
| TIA | 1 (3) |
| Moya moya | 1 (3) |
| Acute chest syndrome, No. (%) | 7 (23) |
| Avascular necrosis ≥2 joints | 7 (23) |
| Sickle nephropathy, serum creatinine ≥1.3 mg/dL | 4 (13) |
| Comorbid conditions | |
| Serum ferritin >1000 ng/mL | 15 (50) |
| Hepatopathy | 6 (20) |
| Bridging fibrosis or cirrhosis | 3 (10) |
| Hepatitis C | 2 (7) |
| Direct bilirubin >20 mg/dL | 1 (3) |
| Proteinuria only, serum creatinine <1.3 mg/dL | 4 (13) |
| DLCO <50% | 3 (10) |
| Prior treatment | |
| Hydroxyurea | 28 (93) |
| Simple/exchange red cell transfusions | 16 (53) |
Abbreviations: CNS, central nervous system; DLCO, diffusion capacity of carbon monoxide; HSCT, hematopoietic stem cell transplantation; TIA, transient ischemic attack.
SI conversion factors: to convert bilirubin, from mg/dL to µmol/L, multiply by 17.104; creatinine from mg/dL to µmol/L, multiply by 88.4; ferritin from ng/mL to pmol/L, multiply by 2.247;
13 patients (43%) have 3 indications with at least 1 comorbid condition; 9 patients (30%) have 2 indications with at least 1 comorbid condition; 2 patients (7%) have 1 indication with at least 1 comorbid condition.
Donors underwent 5 to 6 days of granulocyte colony-stimulating factor (filgrastim) mobilization (10–16 µg/kg/d), followed by large-volume peripheral blood leukapheresis to collect a goal of 10 × 106 or more of CD34 cells per kilogram of the recipient’s weight, and the products were cryopreserved.16 Alemtuzumab was given as 0.03 mg/kg 7 days before, 0.1 mg/kg 6 days before, and 0.3 mg/kg 5, 4, and 3 days before the procedure. Total-body irradiation of 300 rad was given as a single dose 2 days before the procedure; radiation shielding was applied to male gonads. Sirolimus loading began the day before the procedure, targeting a trough level of 10 to 15 ng/mL for the first 3 to 4 months, near 10 ng/mL for the remainder of the first year, and 5 to 10 ng/mL from the second year thereafter. Granulocyte colony-stimulating factor–mobilized peripheral blood stem cells were infused on the day of the procedure. Supportive care guidelines have been standardized for individuals undergoing allogeneic HSCT at our facility and include globally accepted measures such as antimicrobial prophylaxis to prevent herpes virus reactivation (acyclovir), candida infection (nystatin), pneumocystis (sulfamethoxazole-trimethoprim), prompt evaluation and treatment for neutropenic fever, and frequent monitoring and preemptive treatment for cytomegalovirus DNA in the peripheral blood.17,18 Our protocol was amended to allow tapering immunosuppression at 1 year only if donor T-cell chimerism reached more than 50% in the absence of graft-vs-host disease.
Additional sickle cell disease–specific strategies were followed. Hydroxyurea was maintained until the day before the preparative regimen. Red blood cell exchange was performed to target hemoglobin S levels of less than30%prior to the preparative regimen. When possible, platelet counts were maintained at more than 50 × 109/L and hemoglobin between 9 and 10 g/dL. Granulocyte colony-stimulating factor was not administered due to attendant morbidity and mortality in sickle cell disease.19 Last, 250 mg of penicillin V-potassium was given twice daily from transplant day until patients completed pneumococcal vaccinations.
The primary end point was the proportion of individuals with treatment success at 1 year, defined as full donor-type hemoglobin on hemoglobin electrophoresis for patients with sickle cell disease and transfusion independence for patients with thalassemia. Secondary end points included the level of donor leukocyte chimerism to maintain graft survival and hematologic values within the normal range, incidence of acute and chronic graft-vs-host disease, overall survival and disease free survival (absence of sickle cell disease or thalassemia) at 1 year or the most recent follow-up, transplant-related mortality, immunologic recovery, and quality of life and neuropsychologic function assessment. Annual magnetic resonance imaging and angiography of the brain, pulmonary function test, echocardiogram, and laboratory testing were done to assess changes in end-organ function.
Laboratory and Chimerism Analysis
Hematologic, chemistry (including liver and renal-specific testing), and lymphocyte subset parameters were performed at the Clinical Laboratory Improvement Amendments–certified laboratory at our institution. Peripheral blood cells CD3 and CD14 or CD15were positively selected using immunomagnetic beads to estimate lymphoid and myeloid chimerism, respectively. Presence of donor leukocytes was assessed by polymerase chain reaction (PCR) methods as previously described.12,20 Hemoglobin electrophoresis and extended phenotyping for minor red cell antigens were also used to determine donor red cell chimerism. These laboratory tests were performed frequently in the first 6 months after HSCT, then annually when the parameters became stable.
Statistical Analysis
Data are reported as means (95%confidence intervals) or medians (range). A paired t test, t test, Fisher exact test, Wilcoxon signed rank test, or mixed-model regression was used to compare data where appropriate. The significance level was set at P < .05. All statistical testing was 2-sided, and no multiplicity was corrected. Analyses were performed using SAS version 9.3 statistical software and JMP version 8.0 (both SAS Institute Inc).
Results
Patient Characteristics and Short-term Outcome
As of October 25, 2013, HLA typing was performed in the siblings of 287 patients (details of accrual are depicted in eFigure 1 in the Supplement). Thirty patients underwent transplantation; initial results about the first 10 were reported earlier.12 Two patients had heterozygous hemoglobin S and C, 1 patient had HbSβ+-thalassemia, 1 patient had HbSβ0- thalssemia, and 1 transfusion-dependent β-thalassemia intermedia (Pesaro class 2); the remainder had homozygous hemoglobin S. Twenty-two patients (73%) had 2 or more indications with at least 1 comorbid condition (Table 1). All donors, including 19 individuals with the sickle cell trait, experienced bone pain, headaches, and fatigue, typical of granulocyte colony-stimulating factor administration. There were no granulocyte colony-stimulating factor–related unanticipated adverse events, severe adverse events, or technical difficulties with HSC products collected from those with the sickle trait as previously reported.16 Recipients received a median of 14.6 × 106 CD34 cells (95% CI, 13.2–18.1 × 106) and a median of 3.5 × 108 CD3 cells (95%CI, 3.4–4.8 × 108) per kilogram of body weight.
There were no acute sickle cell–related complications, hepatic sinusoidal obstructive syndrome, or cerebral complications from immunosuppression. The median duration of neutropenia (neutrophil level, <0.5 × 109 cells/L) was 16 days (range, 6–21), and the median neutrophil nadir was 0.12 × 109 cells/L, similar to levels that have been previously reported.12 For the pretransplant red cell exchange, the median number of red cell units was 7 (range, 1–9). From the start of the conditioning regimen to day 45, the median number of red cell units was 6 (range, 0–15); the single-donor apheresis platelet units, 4 (range, 0–19). Except for 6 patients for whom it was not required, first-line intravenous antibiotics were administered for febrile neutropenia.
Later in the first 100 days after HSCT, most patients had sirolimus–related adverse events such as arthralgia or hypertriglyceridemia. Four of 30 patients received preemptive treatment for cytomegalovirus due to either more than 1000 copies/mL or a low-level positive PCR with coinciding fever suggesting possible infection. These 4 patients had undetectable cytomegalovirus by PCR and discontinued treatment after a week. Beyond 1 year after HSCT, 2 patients experienced dermatomal zoster, and 1 patient had suspected herpes virus reactivation in the gastrointestinal tract. There was no Epstein-Barr virus–associated posttransplant lymphoproliferative disorder. One patient who received interferon and ribavirin for 9 months before HSCT and had 19 days of neutropenia was treated with antifungal therapy for presumed pulmonary disease, suggested by imaging.
HSCT Outcomes
As of October 25, 2013, 29 patients were alive with a median follow-up of 3.4 years (range, 1–8.6). Donor leukocyte engraftment was observed in 26 patients. At 1 year after HSCT, our primary end point analysis, 25 patients (83%) had full donor-type hemoglobin. One patient had detectable anti-Jka antibody to donor red blood cells before transplant and was supported by transfusions up to 1.5 years after the transplant. Eventually, the patient had full donor red cell engraftment and was transfusion free at 2 years after HSCT. Four patients had temporary donor engraftment, subsequent graft rejection, and recovery with sickle cell disease (eTable 1B in the Supplement). One relapsed patient with a history of stroke and moya moya disease died following an intracranial hemorrhage 7 months after graft rejection (10 months after HSCT).
Hemoglobin levels improved after HSCT (Table 2). The mean hemoglobin levels for women before HSCT were 81 g/L (95% CI, 73–89) vs 127 g/L (95% CI, 118–136) after HSCT (at the most recent follow-up). For men, they were 89 g/L (95% CI, 84–93) before HSCT vs 137 g/L (95% CI, 123–151) after HSCT (P < .001). Markers of hemolysis also improved. The respective mean before vs after HSCT values were reticulocyte count, 182 × 109 cells/L (95% CI, 145–220) vs 85 × 109 cells/L (95% CI, 53–117); total bilirubin, 2.7 mg/dL (95% CI, 1.7–3.7) vs 0.9 mg/dL (95% CI, 0.4–1.5); and lactate dehydrogenase, 324 U/L (95% CI, 272–375) vs 202 U/L (95% CI, 182–221; P < .001 for all 3 parameters). (To convert bilirubin from mg/dL to µmol/L, multiply by 17.104; lactate dehydrogenase from U/L to µKat/L, multiply by 0.0167 to U/L.) The recipients achieved the same percentage of hemoglobin S and A as their donors a year after HSCT (recipients of AA [normal adult] donors, 0%; recipients of AS [sickle traits] donors, 35.3%, 95% CI, 30.6%–40.1%) and at the most recent follow-up (AA donors 0%, AS donors 39.8%, 95% CI, 35.1%–44.4%).
Table 2.
Hematologic and Hemolytic Parameters Before and After Hematopoietic Stem Cell Transplantation Among 26 Engrafted Patients
| Reference Range | Mean (95% CI) | |||||
|---|---|---|---|---|---|---|
| Pre-HSCT (n = 30) |
Exchange (n = 30)a |
6 Month (n = 26) |
1 Year (n = 26) |
Most Recent (n = 23) |
||
| Hemoglobin | ||||||
| Women | ||||||
| g/dL | 11.2–15.7 | 8.1 (7.3–8.9) | 8.8 (8.4–9.3) | 10.8 (9.8–11.8) | 11.9 (11.2–12.6) | 12.7 (11.8–13.6) |
| g/L | 112–157 | 81 (73–89) | 88 (84–93) | 108 (98–118) | 119 (112–126) | 127 (118–136) |
| Men | ||||||
| g/dL | 13.7–17.5 | 8.9 (8.4–9.3) | 9.3 (8.8–9.7) | 12.0 (10.9–13.2) | 12.1 (11.0–13.3) | 13.7 (12.3–15.1) |
| g/L | 137–175 | 89 (84–93) | 93 (88–97) | 120 (109–132) | 121 (110–133) | 137 (123–151) |
| Lactate dehydrogenase | ||||||
| U/L | 113–226 | 324 (272–375) | 305 (253–358) | 239 (211–267) | 198 (179–217) | 202 (182–221) |
| µkat/L | 1.7–3.4 | 5.4 (4.5–6.3) | 5.1 (4.2–6.0) | 4.0 (3.5–4.5) | 3.3 (3.0–3.6) | 3.4 (3.0–3.7) |
| Total bilirubin | ||||||
| mg/dL | 0.1–1.0 | 2.7 (1.7–3.7) | 2.7 (1.5–4.0) | 0.7 (0.5–0.9) | 0.7 (0.3–1.0) | 0.9 (0.4–1.5) |
| µmol/L | 5–21 | 46.2 (29.4–62.9) | 46.9 (25.6–68.1) | 12.2 (9.1–15.3) | 11.6 (5.6–17.5) | 15.8 (6.4–25.2) |
| Reticulocyte | ||||||
| 109 cells/L | 16–78 | 182 (145–220) | 136 (106–166) | 84 (64–105) | 76 (54–98) | 85 (53–117) |
| Homozygous hemoglobin S, % | ||||||
| Sickle trait donors | 35–41 | 63.7 (52.9–74.4) | 33.0 (29.4–36.7) | 31.5 (25.3–37.8) | 35.3 (30.6–40.1) | 39.8 (35.1–44.4) |
| Normal adult hemoglobin donors | 0 | 56.2 (30.4–81.9) | 22.3 (14.6–30.0) | 0.0 (0.0–0.0) | 0.0 (0.0–0.0) | 0.0 (0.0–0.0) |
Pre-HSCT denotes approximately 1 month before hematopoietic stem cell transplant (HSCT); exchange, after red cell exchange procedure; 6 mo, 6 mo after HSCT; 1 year, 1 year after HSCT; and most recent, at the most recent follow-up (median, 3.6 years; range, 1.0–8.4).
Donor Leukocyte Chimerism
The sustained donor leukocyte engraftment rate was observed in 26 of 30 patients, resulting in a disease-free survival of 87%. There constitution of donor myeloid-cell (CD14 or CD15) chimerism was more rapid than that of the T-cell (CD3) compartment, with both compartments reaching plateau at 12 to 18 months after transplant. At the median follow-up of 3.6 years, the mean donor myeloid-cell chimerism was 86% (95% CI, 70%–100%) and the T cell, 48%(95% CI, 34%–62%). No participant reached 100% donor in both compartments.
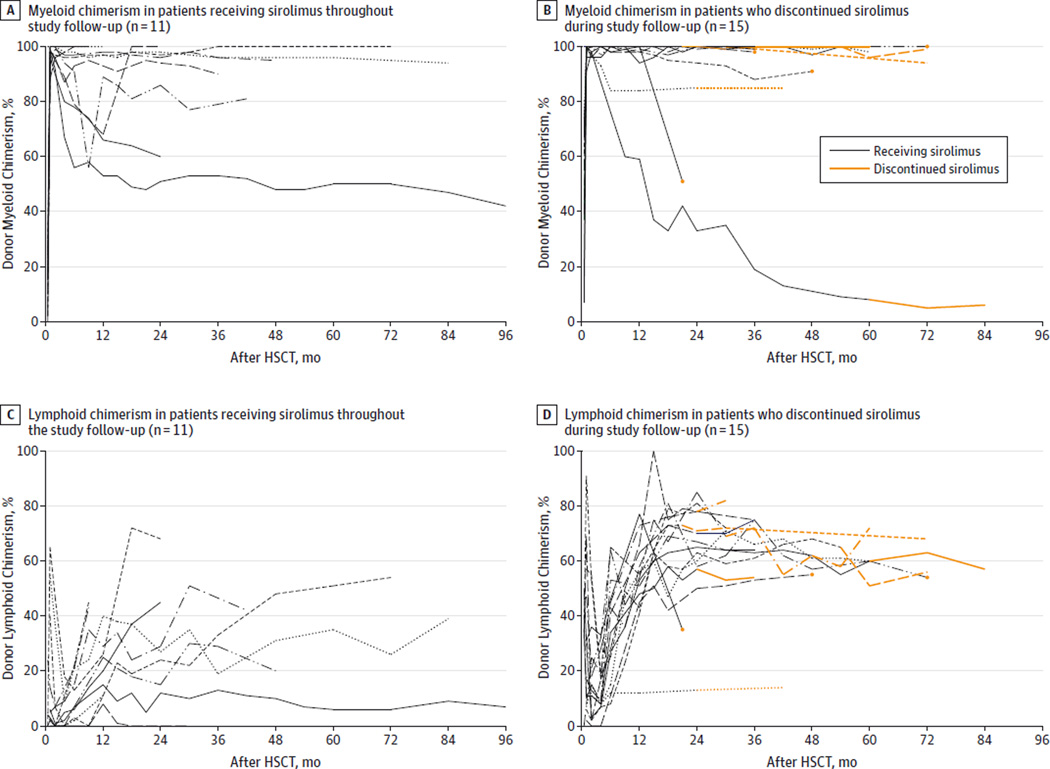
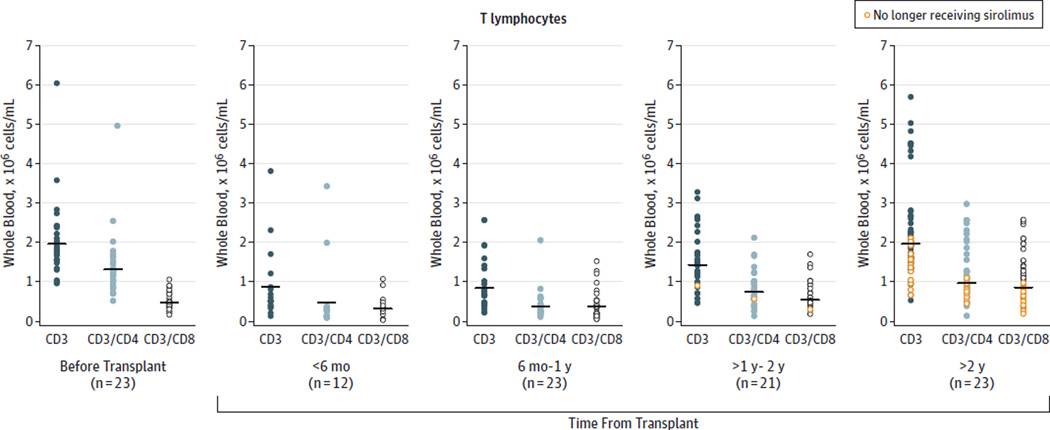
The median duration of immunosuppression was 2.1 years (range, 1.0–8.4). Cessation of immunosuppression medication was allowed a year after HSCT if donor CD3 chimerism was more than 50%. Six of the first 10 patients (median, 2.4 years range, 0.6–4), 5 of the second 10 patients (median, 1.2 years; range, 0.4–1.9), and 4 of the last 10 patients (median, 0.8 years; range, 0.3–1) continued without taking immunosuppression medication. Myeloid chimerism was similar in those who were receiving or not receiving immunosuppression medication (Figure 1A and 1B). Lymphoid chimerism differed between those receiving or not immunosuppression medication as expected, given the requirement for more than 50% lymphoid chimerism before weaning (Figure 1C and 1D). One patient discontinued immunosuppression treatment independently despite having lymphoid chimerism of less than 50%. The percentage of donor chimerism, hemoglobin S, and total hemoglobin remained stable after cessation of immunosuppression medication. During the gradual decrease of sirolimus trough levels in those continuing medication, we observed that T-cell recovery was gradual in the first year and plateaued during the second year after HSCT (Figure 2).
Figure 1. Donor Leukocyte Engraftment After Hematopoietic Stem Cell Transplantation (HSCT).
Eleven patients who were still receiving immunosuppression medication (sirolimus) are shown in panels A (myeloid) and C (lymphoid). Fifteen patients who later discontinued immunosuppression medication are shown in panels B and D. The orange lines and data points represent values after patients ceased immunosuppression medication. At the very early time points, eg, 1 month after transplant when patients began to shows signs of white blood cell engraftment, there often were not sufficient numbers of leukocytes for chimerism analysis. Thus not all time points include all 26 data points. At later time point, some patients could not travel back at the half-year marks (eg, 2.5, 3.5, or 4.5 year) for chimerism analysis; thus, there are fewer data points at those times.
Figure 2. Subsets of T-Lymphocytes Recovery After Hematopoietic Stem Cell Transplantation Among Engrafted Patients.
Each data point represents data value for that patient at that time point. The black bars represent the means.
Graft vs Host Disease
Although the follow-up was less than 2 years for 3 patients, no patient has developed acute or chronic graft-vs-host disease. Furthermore, no graft-vs-host disease was observed in the 15 patients after stopping immunosuppression medication.
Graft Failure
Four patients had temporary donor engraftment for 1 to 3 months after HSCT, then graft failure and subsequent autologous recovery. Three women received grafts from men. There were no differences between these 4 patients and the engrafted patients with respect to median age, CD34 cell dose, CD3 cell dose, pre-HSCT mean serum ferritin, and red cell alloimmunization (eTables 1A, B, C in the Supplement). The early post-HSCT engraftment data in graft failure vs engrafted patients indicated lower percentages of donor CD14 or CD15 and CD3 cells at 2 months. After autologous recovery, these 4 patients had fetal hemoglobin levels in the desired range (eTable 1D in the Supplement), similar to previous reports.
Outcome of Organ Function and Disease
Nine patients who previously had had a stroke or had abnormal central nervous system vessels did not develop stroke or bleeding peritransplant. Subsequent post-HSCT annual brain magnetic resonance imaging and angiography among participants with sustained engraftment remained unchanged. In contrast, 1patient who had relapsed died from recurrent stroke. One patient with prior distant and infrequent history of complex partial seizure was not taking antiseizure medication before HSCT and had 2 self-limited episodes 2 and 3 months after HSCT. The patient started taking levetiracetam and has not had subsequent seizures.
Patients with tricuspid regurgitant velocity higher than 2.5 m/s, prior acute chest syndrome, or low diffusion capacity of carbon monoxide tolerated conditioning without episodes of worsening dyspnea or declines in oxygenation. Their mean tricuspid regurgitant velocity before HSCT of 2.84 m/s (95%, CI 2.71–2.99) decreased to 2.57 m/s (95% CI, 2.44–2.69) 1 month, to 2.43 m/s (95% CI, 2.12–2.70) 1 year, and to 2.33 (95% CI, 2.14–2.51) 3 years after HSCT (P = .01 for tricuspid regurgitant velocity 2.6–2.9 m/s, and P < .001 for tricuspid regurgitant velocity ≥3 m/s, mixed-model regression). The mean 6-minute walk test of 455 m (95% CI, 244–665) before HSCT increased to 504 m (95% CI, 206–801) 1 year and to 507 m (95% CI, 332–681) 3 years after HSCT (P = .41,mixed-model regression).
Approximately two-thirds of the 30 patients who received transplants had variable increases in transaminases and alkaline phosphatase after HSCT, presumably due to the conditioning regimen, iron overload, higher serum triglycerides from sirolimus, or other transplant medications. No specific treatment was instituted because these liver function parameters gradually improved. Prophylactic ursodiol was administered to 6 patients with a pretransplant history of hepatitis C, hyperbilirubinemia, or bridging fibrosis or cirrhosis.
Fifteen patients with ferritin levels greater than 1000 ng/mL (to convert ferritin from ng/mL to pmol/L, multiply by 2.247), 7 patients had ferritin levels between 1000 and 2000 ng/mL, and 3, greater than 4000 ng/mL. Nine patients consented to a liver biopsy with histology available for 8 patients: 5 had mild chronic portal inflammation without fibrosis; 1, inflammation with bridging fibrosis; and 2, inflammation with cirrhosis. Seven patients had adequate specimen for quantitative iron analysis. Their liver iron concentration ranged from 16 to 23.8 mg/g of dry liver weight (mean, 18.8). Large volume phlebotomy was initiated to correct iron overload between 3 and 6 months after HSCT. Seven patients have completed phlebotomy with ferritin levels lower than 300 ng/mL; 6 of the remaining patients continued to undergo phlebotomy.
Among the 4 patients with sickle nephropathy, there was no worsening of the previously established decline in renal function. Two women and 2 men were able to have children naturally after transplant.
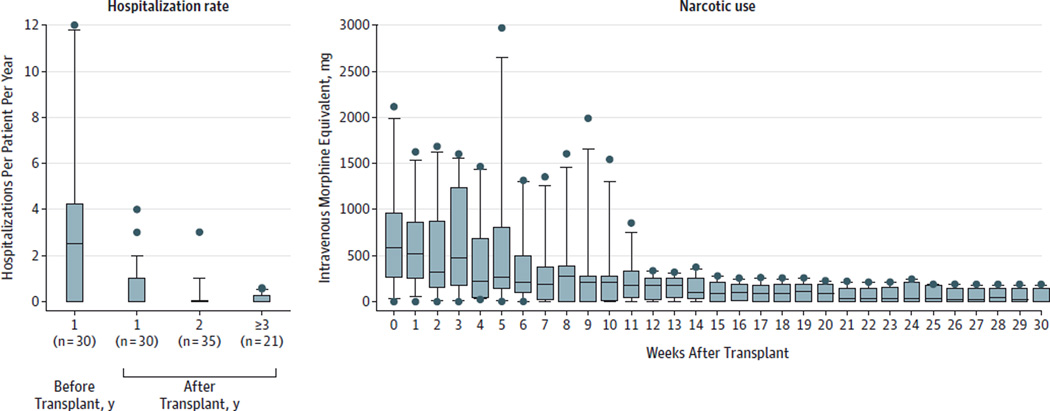
The mean hospitalization rate per patient per year for the entire cohort in the year preceding HSCT was 3.23 times (95% CI, 1.83–4.63), all were sickle cell disease–related complications. Seven patients had 5 or more hospitalizations; 13 had between 1 and4hospitalizations (Figure 3A). The post-HSCT hospitalizations were all captured through serious adverse events reporting (eTable 2 in the Supplement). Thirty-eight serious adverse events occurred in the patients who had received transplants, pain and related management were the most common (n = 15, eg, arthralgias, myalgias, narcotics withdrawal), followed by infections (n = 6, eg, cytomegalovirus, Clostridium difficile), abdominal events (n = 6, eg, pain, ulcer, pancreatitis), and sirolimus-related toxicities (n = 5, eg, arthralgia, pneumonitis).
Figure 3. Hospitalization Rate and Narcotics Use.
A, Median hospital admission rate per patient a year before, 1 year after, 2 years after HSCT, and 3 years after Hematopoietic Stem Cell transplantation (HSCT) and later per year. B, Among 11 participants who took narcotics long-term, median intravenous morphine equivalent doses of narcotics per week are shown with respect to time after HSCT. The boxes refer to 25th and 75th percentile; the whiskers, 10th and 90th percentile; and the dots, values outside the 10th and 90th percentile.
Eleven patients were taking narcotics long-termat the time of transplant (taking long- and short-acting narcotics for ≥ 3 months). During the week they were hospitalized and received their HSCT, the mean narcotics use per week was 639 mg of intravenous morphine–equivalent dose (95% CI, 220–1058). The dosage decreased to 140 mg (95% CI, 56–225) 6 months after the transplant (Figure 3B, eFigure 2 in the Supplement). Six participants who were taking narcotics long-term without irreversible bone or joint damage were successfully weaned from narcotics.
Discussion
In this article, we extend our previous results and show that this HSCT procedure can be applied to older adults, even those with severe comorbid conditions, and that it leads to a high rate of mixed donor chimerism without acute or chronic graft-vs-host disease at the most recent follow-up. These data reinforce the low toxicity of this regimen, especially among patients with significant end-organ dysfunction. There were transplant-related infections in 6 patients, such as C difficile and cytomegalovirus, and sirolimus-related toxicities in 5 patients. Fifteen of the 38 adverse events after HSCT were related to pain, which was expected, given that several of our patients had a vascular necrosis or were dependent on narcotics—neither would be immediately corrected by the transplant procedure.
Our leukocyte engraftment rate of 87% in adults is similar to that of our previous report12 and remains comparable with that observed after myeloablative conditioning in children who underwent the procedure in Belgium (94%),3 France (95.5%),4 and the United States (91.5%).6 Although all of our patients had mixed-donor chimerism, immunosuppression was discontinued in those with more than 50% levels of donor CD3 cells. In most centers, when mixed chimerism is observed, donor T cells are provoked into rejecting recipient hematopoiesis by withdrawal of immunosuppression or by donor lymphocyte infusions. Although this appears effective in driving to complete donor chimerism, this strategy results in high rates of graft-vs-host disease in adult patients.21–25 Additionally, the largest study examining nonmyeloablative transplantation in children with sickle cell disease demonstrated rejection in all 6 patients with mixed chimerism after early withdrawal of calcineurin-based immunosuppression.8 Our protocol thus initially dictated an immunosuppression taper only if 100% donor CD3 chimerism was achieved in the absence of graft-vs-host disease. When we observed no such patients with 100% donor CD3 chimerism but stable levels of mixed CD3 chimerism for years, we tested short-term sirolimus in the murine model and determined its efficacy in supporting stable mixed chimerism.26 We then modified the protocol to allow an immunosuppression taper in the setting of mixed chimerism with more than 50% donor CD3 chimerism.
The 15 patients who discontinued immunosuppression medication continued to have stable mixed chimerism without graft-vs-host disease. These results suggest functional tolerance between donor and recipient cells and demonstrate that mixed chimerism can be stable long-term, regardless of whether the patients are taking immunosuppression medication. This finding is potentially important because stable mixed chimerism is rarely achieved in previously untreated patients with nonmyeloablative conditioning.8,15 Indeed, we did not use the prevailing strategy donor-lymphocyte infusions to shift to full-donor lymphoid chimerism when withdrawal of immunosuppression did not promote such a shift, due to the substantial risk of graft-vs-host disease.21–25,27 The majority of engrafted participants (15 of 26) continued without immunosuppression medication with stable mixed chimerism and no acute or chronic graft-vs-host disease. Additionally, the use of peripheral blood stem cells has been associated with higher rates of chronic graft-vs-host disease using myeloablative conditioning,28 yet our results are quite different. We hypothesize that the long half-life of alemtuzumab, which depletes recipient and eventually donor lymphocytes (in vivo T-cell depletion), and single-agent sirolimus over calcineurin inhibitors, which promotes tolerance via signal 2 blockade, are the primary reasons for this beneficial effect.29 This study brings closer the desired goal of correcting the sickle cell disease phenotype in the absence of long-term immunosuppression or graft-vs-host disease. Further studies on the role of regulatory T cells in these mixed chimeric patients and details of lymphocyte function are ongoing.
The engraftment data from these patients also indicated that donor CD14 or CD15 cells correlate red cell engraftment better than CD3 or whole blood leukocytes. A few patients had CD3 chimerism as low as 0% and CD14 or CD15 chimerism higher than 50%, yet they had full donor erythroid chimerism by high-performance liquid chromatography and extended red cell phenotyping for donor erythrocyte antigen. One patient had donor CD14 or CD15 chimerism of19% and still had full donor erythroid cells. This observation likely reflects the advantage of donor red blood cells with normal half-life compared with the very short half-life of sickle red blood cells. Our results corroborated previous reports of mixed chimerism.5–7
Sickle cell disease can damage multiple organs and dramatically shorten the lifespan of affected individuals.30–33 In patients with previous brain injury, this HSCT regimen has the advantage of not requiring pharmacokinetic monitoring or seizure prevention. Brain imaging of our patients was unchanged over time. We are currently performing serial testing on neurocognitive function before and after transplant to determine the effects of sickle cell disease reversal. In patients with prior pulmonary complications, 300 rad of total-body irradiation and the unmanipulated graft, which contained hemolyzed red blood cells, also did not cause acute pulmonary complications.34 Over time, there was significant improvement in tricuspid regurgitant velocity, which may reflect the increase in hemoglobin as previously demonstrated in patients with heart failure.35 Hospitalizations were reduced after transplantation for the entire cohort, as was the use of narcotics. Importantly, all patients without irreversible bone or joint damage were able to completely discontinue narcotics.
Many of our patients had iron overload and other liver injury before transplant. Although the patients had transient increases in serum liver markers during and after the transplant process, they were asymptomatic and required no treatment. Several of them had severe liver injury that would preclude them from a more intensive preparative HSCT regimen. Our regimen offered an efficacious alternative to these otherwise transplant-ineligible patients. The normalization of hemoglobin has also enabled large-volume phlebotomy to be performed. The significant reduction in ferritin levels suggested that much of the iron burden has been relieved and the long-term effects of iron overload should be minimized.
The first limitation of this study is that this HSCT regimen was applied only to those with HLA-matched related donors; unfortunately the majority of patients with sickle cell disease or β-thalassemia do not have this option.15 We and other researchers are actively optimizing HSCT regimen using alternative donors, such as half-matched (haploidentical) donors, and although engraftment rates are currently lower, nearly all patients have a potential haploidentical donor.36 Another limitation is the long-term immunosuppression in those HSCT recipients who had donor CD3 chimerism less than 50%. Although 3 patients developed thyroiditis and none a secondary malignancy after HSCT, these concerns remain with 300 rad of total-body irradiation and prolonged immunosuppression.
Conclusions
In this series of patients who underwent a simplified HSCT regimen to date, stable mixed-donor chimerism and reversal of sickle cell disease phenotype was achieved in the majority of patients. Engrafted patients continued to be disease-free and without graft-vs-host disease. The majority of engrafted patients no longer taking immunosuppression medication had continued stable chimerism and disease reversion without graft-vs-host disease, suggesting tolerance to donor cells. Further accrual and follow-up is required to assess longer-term clinical outcomes, adverse events, and transplant tolerance.
Supplementary Material
Acknowledgments
Funding/Support: This work is supported by the intramural research program of the National Institute of Diabetes and Digestive and Kidney Diseases and the National Heart, Lung, and Blood Institute at the National Institutes of Health (NIH).
Role of the Sponsor: The sponsor had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Additional Contributions: We thank Terri Wakefield, MS, at NIH for protocol support; Rosario Di Maggio, MD, of Azienda Ospedaliera Universitaria Policlinico “Paolo Giaccone,” Palermo, Italy, for data collection; the clinical staff, the Department of Transfusion Medicine, Department of Laboratory Medicine, Radiation Oncology, and the liver disease team at the NIH Clinical Center for patient care. No one received compensation for their role in the study.
Footnotes
Author Contributions: Dr Tisdale had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Hsieh, Rodgers, Powell, Tisdale.
Acquisition, analysis, or interpretation of data: Hsieh, Fitzhugh, Weitzel, Link, Coles, Zhao, Powell, Tisdale.
Drafting of the manuscript: Hsieh, Fitzhugh, Weitzel, Link, Zhao, Tisdale.
Critical revision of the manuscript for important intellectual content: Hsieh, Fitzhugh, Weitzel, Coles, Zhao, Rodgers, Powell, Tisdale.
Statistical analysis: Hsieh, Weitzel, Zhao.
Obtained funding: Rodgers, Tisdale.
Administrative, technical, or material support: Fitzhugh, Weitzel, Link, Coles, Rodgers, Tisdale.
Study supervision: Link, Rodgers, Tisdale.
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
REFERENCES
- 1.Pauling L, Itano HA. Sickle cell anemia a molecular disease. Science. 1949;110(2865):543–548. doi: 10.1126/science.110.2865.543. [DOI] [PubMed] [Google Scholar]
- 2.Walters MC, Patience M, Leisenring W, et al. Bone marrow transplantation for sickle cell disease. N Engl J Med. 1996;335(6):369–376. doi: 10.1056/NEJM199608083350601. [DOI] [PubMed] [Google Scholar]
- 3.Vermylen C, Cornu G, Ferster A, et al. Haematopoietic stem cell transplantation for sickle cell anaemia: the first 50 patients transplanted in Belgium. Bone Marrow Transplant. 1998;22(1):1–6. doi: 10.1038/sj.bmt.1701291. [DOI] [PubMed] [Google Scholar]
- 4.Bernaudin F, Socie G, Kuentz M, et al. SFGM-TC. Long-term results of related myeloablative stem-cell transplantation to cure sickle cell disease. Blood. 2007;110(7):2749–2756. doi: 10.1182/blood-2007-03-079665. [DOI] [PubMed] [Google Scholar]
- 5.Andreani M, Nesci S, Lucarelli G, et al. Long-term survival of ex-thalassemic patients with persistent mixed chimerism after bone marrow transplantation. Bone Marrow Transplant. 2000;25(4):401–404. doi: 10.1038/sj.bmt.1702151. [DOI] [PubMed] [Google Scholar]
- 6.Walters MC, Patience M, Leisenring W, et al. Multicenter Investigation of Bone Marrow Transplantation for Sickle Cell Disease. Stable mixed hematopoietic chimerism after bone marrow transplantation for sickle cell anemia. Biol Blood Marrow Transplant. 2001;7(12):665–673. doi: 10.1053/bbmt.2001.v7.pm11787529. [DOI] [PubMed] [Google Scholar]
- 7.Andreani M, Testi M, Gaziev J, et al. Quantitatively different red cell/nucleated cell chimerism in patients with long-term, persistent hematopoietic mixed chimerism after bone marrow transplantation for thalassemia major or sickle cell disease. Haematologica. 2011;96(1):128–133. doi: 10.3324/haematol.2010.031013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Iannone R, Casella JF, Fuchs EJ, et al. Results of minimally toxic nonmyeloablative transplantation in patients with sickle cell anemia and beta-thalassemia. Biol Blood Marrow Transplant. 2003;9(8):519–528. doi: 10.1016/s1083-8791(03)00192-7. [DOI] [PubMed] [Google Scholar]
- 9.Krishnamurti L, Kharbanda S, Biernacki MA, et al. Stable long-term donor engraftment following reduced-intensity hematopoietic cell transplantation for sickle cell disease. Biol Blood Marrow Transplant. 2008;14(11):1270–1278. doi: 10.1016/j.bbmt.2008.08.016. [DOI] [PubMed] [Google Scholar]
- 10.van Besien K, Bartholomew A, Stock W, et al. Fludarabine-based conditioning for allogeneic transplantation in adults with sickle cell disease. Bone Marrow Transplant. 2000;26(4):445–449. doi: 10.1038/sj.bmt.1702518. [DOI] [PubMed] [Google Scholar]
- 11.Zheng Y, Collins SL, Lutz MA, et al. A role for mammalian target of rapamycin in regulating T cell activation versus anergy. J Immunol. 2007;178(4):2163–2170. doi: 10.4049/jimmunol.178.4.2163. [DOI] [PubMed] [Google Scholar]
- 12.Hsieh MM, Kang EM, Fitzhugh CD, et al. Allogeneic hematopoietic stem-cell transplantation for sickle cell disease. N Engl J Med. 2009;361(24):2309–2317. doi: 10.1056/NEJMoa0904971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Powars DR, Elliott-Mills DD, Chan L, et al. Chronic renal failure in sickle cell disease: risk factors, clinical course, and mortality. Ann Intern Med. 1991;115(8):614–620. doi: 10.7326/0003-4819-115-8-614. [DOI] [PubMed] [Google Scholar]
- 14.Gladwin MT, Sachdev V, Jison ML, et al. Pulmonary hypertension as a risk factor for death in patients with sickle cell disease. N Engl J Med. 2004;350(9):886–895. doi: 10.1056/NEJMoa035477. [DOI] [PubMed] [Google Scholar]
- 15.Hsieh MM, Fitzhugh CD, Tisdale JF. Allogeneic hematopoietic stem cell transplantation for sickle cell disease: the time is now. Blood. 2011;118(5):1197–1207. doi: 10.1182/blood-2011-01-332510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kang EM, Areman EM, David-Ocampo V, et al. Mobilization, collection, and processing of peripheral blood stem cells in individuals with sickle cell trait. Blood. 2002;99(3):850–855. doi: 10.1182/blood.v99.3.850. [DOI] [PubMed] [Google Scholar]
- 17.Nakamura R, Cortez K, Solomon S, et al. High-dose acyclovir and pre-emptive ganciclovir to prevent cytomegalovirus disease in myeloablative and non-myeloablative allogeneic stem cell transplantation. Bone Marrow Transplant. 2002;30(4):235–242. doi: 10.1038/sj.bmt.1703648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tomblyn M, Chiller T, Einsele H, et al. Center for International Blood and Marrow Research; National Marrow Donor program; European Blood and Marrow Transplant Group; American Society of Blood and Marrow Transplantation; Canadian Blood and Marrow Transplant Group; Infectious Diseases Society of America; Society for Healthcare Epidemiology of America; Association of Medical Microbiology and Infectious Disease Canada; Centers for Disease Control and Prevention. Guidelines for preventing infectious complications among hematopoietic cell transplantation recipients: a global perspective. Biol Blood Marrow Transplant. 2009;15(10):1143–1238. doi: 10.1016/j.bbmt.2009.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fitzhugh CD, Hsieh MM, Bolan CD, Saenz C, Tisdale JF. Granulocyte colony-stimulating factor (G-CSF) administration in individuals with sickle cell disease: time for a moratorium? Cytotherapy. 2009;11(4):464–471. doi: 10.1080/14653240902849788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nollet F, Billiet J, Selleslag D, Criel A. Standardisation of multiplex fluorescent short tandem repeat analysis for chimerism testing. Bone Marrow Transplant. 2001;28(5):511–518. doi: 10.1038/sj.bmt.1703162. [DOI] [PubMed] [Google Scholar]
- 21.Srinivasan R, Takahashi Y, McCoy JP, et al. Overcoming graft rejection in heavily transfused and allo-immunised patients with bone marrow failure syndromes using fludarabine-based haematopoietic cell transplantation. Br J Haematol. 2006;133(3):305–314. doi: 10.1111/j.1365-2141.2006.06019.x. [DOI] [PubMed] [Google Scholar]
- 22.Chalandon Y, Passweg JR, Schmid C, et al. Chronic Leukemia Working Party of European Group for Blood and Marrow Transplantation. Outcome of patients developing GVHD after DLI given to treat CML relapse: a study by the Chronic Leukemia Working Party of the EBMT. Bone Marrow Transplant. 2010;45(3):558–564. doi: 10.1038/bmt.2009.177. [DOI] [PubMed] [Google Scholar]
- 23.Marsh RA, Vaughn G, Kim MO, et al. Reduced-intensity conditioning significantly improves survival of patients with hemophagocytic lymphohistiocytosis undergoing allogeneic hematopoietic cell transplantation. Blood. 2010;116(26):5824–5831. doi: 10.1182/blood-2010-04-282392. [DOI] [PubMed] [Google Scholar]
- 24.Bar M, Sandmaier BM, Inamoto Y, et al. Donor lymphocyte infusion for relapsed hematological malignancies after allogeneic hematopoietic cell transplantation: prognostic relevance of the initial CD3+ T cell dose. Biol Blood Marrow Transplant. 2013;19(6):949–957. doi: 10.1016/j.bbmt.2013.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Anurathapan U, Pakakasama S, Rujkijyanont P, et al. Pretransplant immunosuppression followed by reduced-toxicity conditioning and stem cell transplantation in high-risk thalassemia: a safe approach to disease control. Biol Blood Marrow Transplant. 2013;19(8):1259–1262. doi: 10.1016/j.bbmt.2013.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fitzhugh CD, Weitzel RP, Hsieh MM, et al. Sirolimus and post-transplant Cy synergistically maintain mixed chimerism in a mismatched murine model. Bone Marrow Transplant. 2013;48(10):1335–1341. doi: 10.1038/bmt.2013.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Childs R, Clave E, Contentin N, et al. Engraftment kinetics after nonmyeloablative allogeneic peripheral blood stem cell transplantation: full donor T-cell chimerism precedes alloimmune responses. Blood. 1999;94(9):3234–3241. [PubMed] [Google Scholar]
- 28.Anasetti C, Logan BR, Lee SJ, et al. Blood and Marrow Transplant Clinical Trials Network. Peripheral-blood stem cells versus bone marrow from unrelated donors. N Engl J Med. 2012;367(16):1487–1496. doi: 10.1056/NEJMoa1203517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Waickman AT, Powell JD. Mammalian target of rapamycin integrates diverse inputs to guide the outcome of antigen recognition in T cells. J Immunol. 2012;188(10):4721–4729. doi: 10.4049/jimmunol.1103143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wierenga KJ, Hambleton IR, Lewis NA. Survival estimates for patients with homozygous sickle-cell disease in Jamaica: a clinic-based population study. Lancet. 2001;357(9257):680–683. doi: 10.1016/s0140-6736(00)04132-5. [DOI] [PubMed] [Google Scholar]
- 31.Steinberg MH, Barton F, Castro O, et al. Effect of hydroxyurea on mortality and morbidity in adult sickle cell anemia: risks and benefits up to 9 years of treatment. JAMA. 2003;289(13):1645–1651. doi: 10.1001/jama.289.13.1645. [DOI] [PubMed] [Google Scholar]
- 32.Quinn CT, Rogers ZR, Buchanan GR. Survival of children with sickle cell disease. Blood. 2004;103(11):4023–4027. doi: 10.1182/blood-2003-11-3758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Powars DR, Chan LS, Hiti A, Ramicone E, Johnson C. Outcome of sickle cell anemia: a 4-decade observational study of 1056 patients. Medicine (Baltimore) 2005;84(6):363–376. doi: 10.1097/01.md.0000189089.45003.52. [DOI] [PubMed] [Google Scholar]
- 34.Fitzhugh CD, Unno H, Hathaway V, et al. Infusion of hemolyzed red blood cells within peripheral blood stem cell grafts in patients with and without sickle cell disease. Blood. 2012;119(24):5671–5673. doi: 10.1182/blood-2011-11-392654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Anker SD, Comin Colet J, Filippatos G, et al. FAIR-HF Trial Investigators. Ferric carboxymaltose in patients with heart failure and iron deficiency. N Engl J Med. 2009;361(25):2436–2448. doi: 10.1056/NEJMoa0908355. [DOI] [PubMed] [Google Scholar]
- 36.Bolaños-Meade J, Fuchs EJ, Luznik L, et al. HLA-haploidentical bone marrow transplantation with posttransplant cyclophosphamide expands the donor pool for patients with sickle cell disease. Blood. 2012;120(22):4285–4291. doi: 10.1182/blood-2012-07-438408. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.