Abstract
The transition from pediatric to adult transplant care is a high risk period for non-adherence and poor health outcomes. This article describes a quality improvement initiative integrated into a pediatric liver transplant program that focused on improving outcomes following the transfer from pediatric to adult liver transplant care. Using improvement science methodology, we evaluated the impact of our center's transition readiness skills (TRS) program by conducting a chart review of 45 pediatric liver transplant recipients who transferred to adult transplant care. Medication adherence, clinic attendance, and health status variables were examined for the year pre-transfer and first year post-transfer. 19 recipients transferred without participating in the TRS program (control group) and 26 recipients participated in the program prior to transferring to the adult clinic (TRS group). The TRS group was significantly older at the time of transfer, more adherent with medications, and more likely to attend their first adult clinic visit compared to the control group. Among the TRS group, better adolescent and parent regimen knowledge were associated with greater adherence to post-transfer clinic appointments. Transition planning should focus on the gradual shift in responsibility for health management tasks, including clinic attendance, from parent to adolescent. There may be support for extending transition support for at least 1 year post-transfer to promote adherence.
Keywords: Adherence, Self-management, Transition, Transplant, Pediatrics
Introduction
“Transition” is an active process that addresses the medical, psychosocial, and educational/vocational needs of adolescents as they prepare to move from child- to adult-centered health care, while “transfer” refers to the change in the location where care is provided (Blum et al., 1993; de Silva & Fishman, 2014; Kennedy & Sawyer, 2008; Sawyer, Blair, & Bowes, 1997). During adolescence, the management of a chronic illness typically shifts from the primary responsibility of the parent to self-management by the adolescent (Fredericks et al., 2010; Kieckhefer & Trahms, 2000). Transition readiness can be viewed as an adolescent/young adult's ability to begin and complete the transition process with parent/family and provider support (de Silva & Fishman, 2014). Ultimately, it has been recommended that pediatric patients should not transfer to adult health services unless they have the skills necessary for functioning effectively in the adult health care system (de Silva & Fishman, 2014; Huang et al., 2011). Overall, it is recommended that prior to transferring to adult-centered care, pediatric transplant recipients should be able to describe their health condition, demonstrate a sense of responsibility, and have the capacity to independently manage their health (Bell et al., 2008). In adult care settings, patients are expected to independently discuss medical care with the treatment team, schedule and attend appointments, refill prescriptions, and adhere to medications and treatment recommendations (de Silva & Fishman, 2014; Kennedy, Sloman, Douglass, & Sawyer, 2007). It is recommended that pediatric providers foster the development of self-management skills in their patients, as these skills are integral to the achievement of independence necessary for successful health care transitions.
In order to promote transition readiness, it is necessary to define what constitutes a successful transition to adult care. Initial studies have focused on medical stability and attendance at the first scheduled clinic appointment in the adult center as markers of a successful transition (Annunziato et al., 2007; Nasr, Campbell, & Howatt, 1992; Reid et al., 2004). To initiate the transition process, it is recommended that providers assess the patient's ability to manage their health to the degree necessary to facilitate successful transfer to the adult health care system (Annunziato et al., 2014). During this assessment, it is important to consider the impact of the transition process on medical stability, quality of life, psychosocial functioning, educational/vocational outcomes, and health care utilization rates. This information will allow for patient-centered, individualized transition plans.
Intended Improvement
Within our institution, we identified a gap in our services with respect to preparing our pediatric liver transplant recipients for the transition to adult transplant care. Specifically, feedback from our colleagues in the adult liver transplant clinic suggested that our pediatric patients had poor medication adherence and poor clinic attendance and perhaps were not “ready” for transfer to the adult health care system. Indeed, despite the prevalence of consensus statements and policy papers from numerous pediatric and adult organizations (Blum et al., 1993; Rosen, Blum, Britto, Sawyer, & Siegel, 2003), our program was not systematically addressing transition readiness in our clinic, and we did not have an accepted protocol to guide the transfer from pediatric to adult-centered care. Decisions to transfer care were typically based on patient age, medical stability, patient preference, change in insurance, or repeated failure to attend clinic (i.e., “lost to follow-up”).
In 2006, the Pediatric Committee of the American Society of Transplantation jointly sponsored an international consensus conference on “Adolescent Transition to Adult Care in Solid Organ Transplantation.” Subsequently, this committee recommended that prior to transferring to adult-centered care, the pediatric transplant recipient should demonstrate the ability to independently manage their health, including adhering to their immunosuppressant medications (Bell et al., 2008). Due to the high degree of non-adherence during transition to adult centered care (Foster, 2015), implementing this recommendation may have positive implications upon overall health and quality of life outcomes for transplant recipients.
In response to the identified gaps in service as well as the recommendations set forth by the consensus conference (Bell et al., 2008), our pediatric liver transplant center instituted a quality improvement (QI) initiative, and began the initial phase of developing a transition program focused on the assessment and promotion of health-related knowledge, motivation, and self-management skills. This QI initiative aimed to describe the current state of transition at our institution, implement change, and evaluate the outcomes using a Plan–Do–Study–Act (PDSA) model (Schurman, Gayes, Slosky, Hunter, & Pino, 2015; Taylor et al., 2013). The initial steps of this QI initiative entailed the development and implementation of clinic-based surveys to assess transition readiness skills (TRS) (Fredericks et al., 2010) and transition-related attitudes of our adolescent patients and their parents (Fredericks et al., 2011) in order to document the current state of our program. The goal of this QI project was to increase documented TRS screening to at least 95% for pediatric liver transplant recipients aged C11 years. This goal was adopted due to clinical significance and congruence consensus statements (Bell et al., 2008). It was expected that systematic implementation of standardized TRS assessments would lead to better transition preparation and improved outcomes following the transfer to adult care. This paper describes how standardized and objective measures of transition readiness, adherence, and health status were selected and used to evaluate our pediatric liver transplant clinic transition program.
Methods
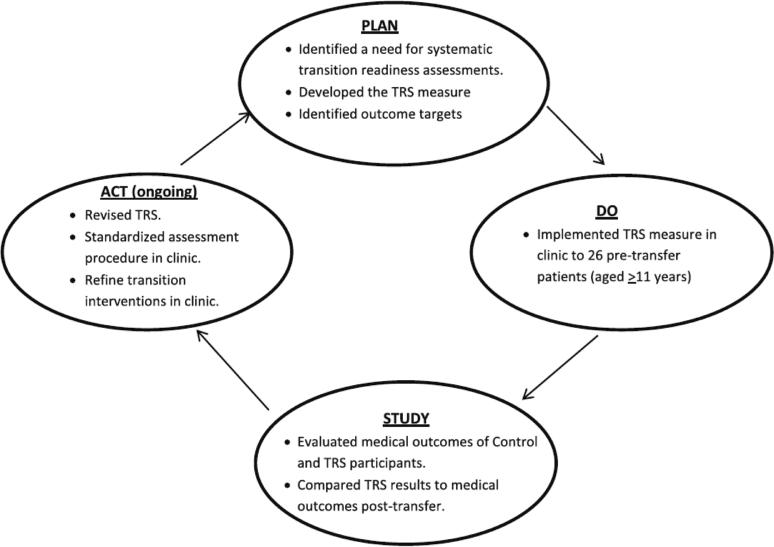
To evaluate the impact of our program, we followed a PDSA cycle (Figure 1), wherein we developed a plan to test the change in outcome (Plan), implemented the program (Do), evaluated the outcomes and consequences (Study), and determined what modifications should be made in our program (Act) (Schurman et al., 2015; Taylor et al., 2013). This quality improvement project was granted exemption by our Institutional Review Board.
Figure 1.
The Plan–Do–Study–Act cycle for transition programming
Planning and Implementing the Intervention
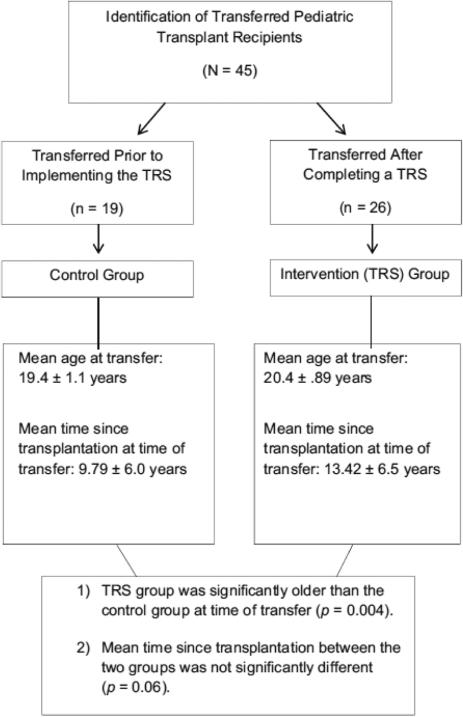
A review of the pediatric liver transplant clinic registry identified all patients who had transferred from the pediatric liver transplant program to the adult liver transplant program between the years 2000–2010 (Figure 2). In 2008, our pediatric liver transplant clinic initiated a TRS program focused on the assessment and promotion of self-management skills, health related knowledge, and adherence (Fredericks et al., 2010). As part of this program, pediatric liver transplant recipients C11 years of age and their parents complete a survey of TRS (Fredericks et al., 2010). Patients completed this survey if they were 11 years of age and older and more than 6 months post-transplant. We included patients as young as 11 years as previous research suggests that the transition of responsibility for health related tasks occurs between the ages of 9 and 17 years, with a mean age of 12 years (American Academy of Pediatrics, American Academy of Family Physicians, & American College of Physicians, Transitions Clinical Report Authoring Group, 2011; de Silva & Fishman, 2014; Shemesh et al., 2004). When present, parents completed a parallel version of the measure.
Figure 2.
Description of pediatric liver transplant recipients who transferred to adult care
In clinic, the TRS surveys are reviewed by members of the multidisciplinary pediatric liver transplant team, comprised of a hepatologist, clinical transplant nurse, pediatric psychologist, social worker, and dietician. Using results from this measure, individualized transition goals are developed in collaboration with liver transplant recipients and their parents. The clinic-based interventions were delivered primarily by a pediatric psychologist and incorporated educational, motivational, behavioral, and organizational strategies to foster the acquisition of self-management skills. Sample goals and interventions are outlined in Table 1.
Table 1.
Sample clinic-based intervention strategies to promote self-management skills and transition readiness
| Domain | Concept | Sample interventions | Sample goals |
|---|---|---|---|
| Health-related knowledge | Disease-specific knowledge Regimen knowledge Health literacy |
Health education Symptom recognition Promote the “Ask Me Three” approach: http://www.npsf.org/askme3 (What is my main problem? What do I need to do? Why is it important for me to do this?) |
Patient will be able to describe the reason for transplant at the next clinic visit Patient will be able to name medications and doses at the next visit Patient will be able to identify symptoms of rejection |
| Behavioral skills | Problem identification, goal setting Communication skills Cues to action Incentives/rewards Stress |
Self-management training Communication skills training Organizational skills (e.g., alarms on phone) Emotional support: coping strategies, stress management |
Patient will set alarms on cell phones to prompt medication administration Patient will assist his mother in filling his pillbox Patient will call in her own prescription refill this month |
Measures
Transition Readiness Skills Survey (TRS)
The TRS is a clinically-derived survey that assesses self-management skills, regimen knowledge and psychosocial adjustment. This measure has been described previously (Fredericks et al., 2010). The adolescent and parent versions of the TRS have demonstrated acceptable internal consistency, with Cronbach's index of internal consistency ranging from ∝ = 0.68–0.81 for the adolescent version (∝ = 0.85 for entire 38-item scale), and ∝ = 0.18–0.75 for the parent version (∝ = 0.75 for the entire 36-item scale) (Fredericks et al., 2010).
Adherence
A multi-method assessment of the adolescent's adherence to immunosuppressant medications and clinic visits in the year pre-transfer and the year post-transfer from pediatric to adult care was conducted using a retrospective review of the patient's electronic medical record. In practice, these measures of adherence, along with measures of psychosocial adjustment, were evaluated to determine transfer readiness in both the TRS and control groups. Specifically, patients who demonstrated independent self-management skills (i.e., primary responsibility for the management of health care needs) with optimal medication adherence were deemed ready to transfer to the adult clinic. Patients with poor self-management skills and documented non-adherence were identified and an individualized treatment plan was developed prior to transferring to the adult clinic.
Immunosuppressant Levels
The degree of fluctuation in immunosuppressant blood levels has been used to assess the variability of medication administration, with higher fluctuations indicating medication non-adherence (Annunziato et al., 2013; Fredericks, Lopez, Magee, Shieck, & Opipari-Arrigan, 2007; Schäfer-Keller, Steiger, Bock, Denhaerynck, & De Geest, 2008; Shemesh et al., 2000, 2004; Supelana et al., 2014; Venkat, Nick, Wang, & Bucuvalas, 2008). Data from routine laboratory monitoring of tacrolimus and cyclosporine blood levels were obtained from the participant's medical record. Immunosuppressant levels obtained during inpatient hospitalization stays were not included in the analyses. Standard deviations (SD) of consecutive blood levels obtained retrospectively were calculated. Participants were considered adherent to their immunosuppressant medications if their tacrolimus SD were\2.0 and if their cyclosporine SD levels\30.0 (Bucuvalas & Alonso, 2005; Fredericks et al., 2007, 2008; Schäfer-Keller et al., 2008).
Clinic Attendance
Adherence to clinic visits was assessed by comparing actual clinic attendance to the frequency recommended by the transplant team. The rates of clinic attendance for the year pre-transfer and for the year post-transfer were obtained from the recipient's electronic medical record. Participants were considered adherent to clinic visits if they attended 85% or more of their scheduled clinic appointments. This definition is consistent with the pediatric adherence literature (Rapoff, 1999), and previous work in pediatric liver transplantation, wherein the rate of clinic attendance was significantly related to hospital admissions, liver biopsies, and rejection episodes (Fredericks et al., 2007).
Health Status
Measures of adolescent/young adult health outcomes including liver panel tests [aspartate aminotransferase (AST), alanine aminotransferase (ALT), total bilirubin (TBili)], graft function, frequency of hospital admissions, liver biopsies, episodes of rejection, and mortality were obtained for the year pre-transfer and the first year post-transfer to the adult clinic. Health status variables were extracted from the recipient's electronic medical record. Participants were considered to be within normal limits for liver function if their AST values were ≤35 U/L, ALT values were ≤60 U/L, and Tbili values were ≤26 mg/dL. Elevated liver panels are typically indicative of liver damage, including the possibility of disease recurrence or graft rejection. These values were determined based on previous research (Ng et al., 2012) and consultation with our pediatric transplant team.
Factors for Successful Transition
A variety of factors were evaluated to determine the proportion of liver transplant recipients who “successfully transitioned” into adult care. Participants were classified as “successfully transitioned” if they demonstrated a combination of optimal medication adherence, measured by SD of immunosuppressant blood levels (tacrolimus SD <2 and cyclosporine SD <30), clinic attendance (>85 %), attendance at the first scheduled adult clinic appointment, and normal liver function tests during the first year post-transfer. These definitions were selected based on clinical significance and relevant adherence literature (Bucuvalas & Alonso, 2005; Fredericks et al., 2007, 2008; Rapoff, 1999; Schäfer-Keller et al., 2008). The proportion of successfully transitioned recipients in TRS group versus the control group was compared.
Study of the Intervention
With the implementation of this QI project, we successfully administered the TRS to 71 pediatric liver transplant recipients C11 years of age, representing 98.6% of the patient population within the targeted age group. We conducted a chart review to identify pediatric liver transplant recipients who transferred to adult transplant care between 2000 and 2010 in order to evaluate our clinic's transition program. We identified 19 recipients who transferred prior to the implementation of the TRS, and 26 recipients who transferred after completing a TRS in clinic (N = 45 transfers). Medication adherence, clinic attendance, and health status variables were examined for the year pre-transfer and first year post-transfer. For the 26 patients who completed the TRS screening measure, we also examined associations between domains on the TRS and post-transfer outcomes.
Data Analysis
Measures of adherence and health status were analyzed using descriptive statistics (e.g. means, SD). Univariate analyses were used to assess between group differences and changes over time. Pearson's product moment correlation coefficients were calculated whenever the assumptions underlying parametric statistical testing were met. Given the skewness of the TRS, Spearman's Rank Correlation, Mann–Whitney U, and Wilcoxon Signed Ranks tests were conducted to examine the associations and changes over time for scores on the TRS domains for the intervention group, measures of adherence, health outcomes, demographic factors including age, and time since transplantation. All analyses were conducted using the SPSS version 21.0 statistical package.
Results
Participant Demographics
Control Group
Nineteen pediatric liver transplant recipients transferred from pediatric to adult care prior to the initiation of our transition program and without a formal assessment of TRS (Figure 2). The mean age at the time of transfer was 19.99 ± 1.31 years, and the mean time since first transplantation at the time of transfer was 9.99 ± 5.97 years. Two recipients experienced a 2nd transplant prior to transferring care due to primary non-function, which is a postoperative condition characterized by absence of hepatic recovery due to various insults during organ recovery, preservation or revascularization. All liver transplant recipients were more than 1 year post-transplant prior to transferring care.
Intervention (TRS) Group
Twenty-six pediatric liver transplant recipients completed the TRS prior to transferring to the adult transplant clinic. Fifteen parents completed parallel versions. The remaining 11 recipients attended clinic independently and did not have a parent present to complete the TRS. The mean age at the time of transfer was significantly older than the control group at 20.86 ± 0.83 years (p = .024). The average time since transplantation when transferred to the adult clinic was 13.47 ± 6.51 years, which was not significantly different than the control group (p = .06). Three recipients had experienced a 2nd transplant prior to transferring care due to primary non-function (n = 2) and disease recurrence (n = 1) related to medication non-adherence. All liver transplant recipients were more than 1 year post-transplant prior to transferring care.
Health Status
Table 2 outlines the health status of the pediatric liver transplant recipients following the transfer of care. There were no significant changes in number of biopsy proven rejections (BPR) or number of hospitalizations following the transfer from pediatric to adult centered care for either the control group or the TRS group. There were no significant differences in health status between control group and the TRS group within the first year of transfer.
Table 2.
Participant demographics and medication information
| Total group | TRS group | Control group | p value | Univariate analyses | |
|---|---|---|---|---|---|
| Mean age at transfer (in years) | 20.49 (1.13) | 20.86 (.83) | 19.99 (1.31) | .024* | Z = –2.264 |
| N = 45 | n = 26 | n = 19 | U = 148.5 | ||
| Mean time since transplant at transfer (in years) | 12.00 (6.46) | 13.47 (6.51) | 9.99 (5.97) | .085 | Z = 1.724 |
| N = 45 | n = 26 | n = 19 | U = 172.00 | ||
| Number of pre-transfer BPR (% of participants with 1 or more BPR) | 5 (6.6 %) | 1 (3.8 %) | 4 (10.6 %) | .366 | Z = –.903 |
| N = 45 | n = 26 | n = 19 | U = 230.00 | ||
| Number of post-transfer BPR (% of participants with 1 or more BPR) | 3 (4.6 %) | 0 (0 %) | 3 (10.6 %) | .101 | Z = –1.641 |
| N = 44 | n = 25 | n = 19 | U = 212.50 | ||
| Number of deaths post transfer | 2 | 1 | 1 | .822 | Z = –.225 |
| N = 45 | n = 26 | n = 18 | U = 243.50 | ||
| Number of participants with pre-transfer graft loss | 0 | 0 | 0 | – | – |
| N = 45 | n = 26 | n = 19 | |||
| Number of participants with post-transfer graft loss | 2 | 1 | 1 | .844 | Z = –.197 |
| N = 44 | n = 25 | n = 18 | U = 234.50 | ||
| Number of undetectable IST values pre | 12 | 8 | 4 | .08 | Z = –1.75 |
| N = 44 | n = 25 | n = 19 | U = 179.00 | ||
| Number of undetectable IST values post | 11 | 4 | 7 | .245 | Z = –.798 |
| N = 44 | n = 26 | n = 18 | U = 211.5 |
BPR biopsy-proven rejection, IST immunosuppressant therapy
p < 0.05
Adherence to Medications and Clinic Attendance
In the first year following the transfer of care, the proportion of patients adherent to medications did not significantly differ between the TRS and control groups (45 vs. 42.1%, U = 184.5, p = .857). The percentage of patients who were adherent to clinic visits in the first year post-transfer also did not significantly differ between the TRS and control groups (44 vs. 68.4%, U = 179.5, p = .111) (Table 3).
Table 3.
Adherence patterns across the TRS and control groups
| Total group | TRS group | Control group | p value | ||
|---|---|---|---|---|---|
| Percent of clinic adherence (≥85 %) pre-transfer | 40.9 | 38.5 | 44.4 | .695 | Z = –.392 |
| N = 44 | n = 26 | n = 18 | U = 220.00 | ||
| Percent of clinic adherence (≥85 %) post-transfer | 54.5 | 44.0 | 68.4 | .111 | Z = –1.593 |
| N = 44 | n = 25 | n = 19 | U = 179.5 | ||
| Clinic attendance rate pre-transfer | 66.82 | 69.57 | 62.84 | .547 | Z = –.602 |
| N = 44 | n = 26 | n = 18 | U = 209.50 | ||
| Clinic attendance rate post-transfer | 81.60 | 77.29 | 87.28 | .138 | Z = –1.484 |
| N = 44 | n = 25 | n = 19 | U = 180.50 | ||
| Percent attended first clinic visit | 77.3 | 92 | 57.9 | .008* | Z = –2.643 |
| N = 44 | n = 25 | n = 19 | U = 156.5 | ||
| % IST adhere pre | 52.3 | 60 | 42.1 | .245 | Z = –1.164 |
| N = 44 | n = 25 | n = 19 | U = 195.00 | ||
| % IST adhere post | 43.6 | 45 | 42.1 | .857 | Z = –.180 |
| N = 39 | n = 20 | n = 19 | U = 184.5 |
IST immunosuppressant therapy
p < 0.01
However, a significantly higher percentage of liver transplant recipients in the TRS group attended their first adult clinic appointment when compared to recipients in the control group (92 vs. 57.9, U = 156.6, p = .008). The control group also had a significant increase in the rate of clinic attendance from the year pre-transfer to the year post-transfer, (Z = −2.281, p = .023), unlike the TRS group, which did not demonstrate a significant change in clinic attendance rate (Z = −1.447, p = .148).
Group Differences
Overall, seven (15.5%) patients were classified as “successful transitions.” Of the 26 patients who participated in the TRS program, 6 (23%) were “successful” compared to only 1 of the 19 patients (5.3 %) who transferred without a transition program (p = .1). With respect to the transfer of care, 92% percent of the recipients in TRS group attended their first adult clinic visit, compared to 57% of the recipients in the control group (p = .008). In retrospect, only eleven (24.4%) recipients evidenced optimal medication adherence, clinic attendance, and health status in the year prior to transferring to adult care, with no significant differences between the TRS and Control groups (30.7 vs. 15.8%, p = .2).
Association Between TRS and Post-transfer Adherence
Adolescent Self-report
Among the adolescents who completed the TRS, scores on the regimen knowledge domain positively correlated with mean clinic attendance rate post-transfer (rs = .648, p<.001) suggesting that increased regimen knowledge is associated with better adherence to clinic appointments following the transfer of care. Adolescent's self-reported regimen knowledge was significantly negatively correlated with mean AST and ALT levels post transfer (rs = −.457, p = .022; rs = −.578, p = .002, respectively). Additionally, the total score on the adolescent TRS was significantly negatively associated with mean ALT levels post transfer (rs = −.415, p = .039). This suggests that overall perception of transition readiness is associated with normal liver function values post transfer. Finally, the adolescent psychosocial domain was significantly negatively correlated with the presence of undetectable liver function values, often indicating regimen non-adherence (rs = −.412, p = .041). These results suggest that greater psychosocial functioning is associated with the presence of fewer undetectable liver function values post-transfer. No other domains on the adolescent version of the TRS were associated with post-transfer adherence or health within the first year in the adult transplant clinic.
Parent Report
Parent reports on the TRS domain measuring parent demonstrated knowledge was positively correlated with mean clinic attendance rate post transfer (rs = .596, p = .025). These results suggest that greater parent demonstrated knowledge was associated with better clinic attendance. The TRS parent self-management domain measures the parent's perceptions of their adolescent's skills. Parent reports of adolescent regimen knowledge domain, and overall parent total score on the TRS was significantly positively correlated with tacrolimus SD levels post transfer (rs = .738, p = .037; rs = .902, p = .002; rs = .805, p = .016, respectively). This suggests that parents’ perception of their adolescent's self-management skills, regimen knowledge, and overall transition readiness are inconsistent with the adolescent's medication adherence as measured by immunosuppressant variability. No other domain on the parent version of the TRS was associated with post-transfer adherence.
Discussion
There is concern that medical complications increase following the transfer from pediatric to adult-centered care, perhaps in part due to medication non-adherence (Foster, 2015; Nuzio, Tizzard, & Vajro, 2014; Watson, 2000, 2005). Thus, there is a need to develop strategies to assess adolescents’ and young adults’ readiness to move to an adult-centered clinic (Bell et al., 2008; LaRosa, Glah, Baluarte, & Meyers, 2011; McDonagh & Kelly, 2007). In response to an identified gap in service, we developed a transition program, wherein we began to systematically assess and promote TRS prior to the transfer to adult care.
The results of this quality improvement initiative demonstrated that the TRS program was successful in assessing 98% of pediatric liver transplant recipients >11 years. Recipients who completed the TRS prior to transferring care had higher clinic attendance following the transfer to adult care compared to those who did not complete a transition readiness assessment prior to the transfer of care. In addition, among the adolescents in the TRS group, higher regimen knowledge and psychosocial functioning was associated with better medication adherence and clinic attendance. Indeed, the majority of adolescents within the TRS group successfully attended their first adult clinic appointment, as opposed to half of the adolescents in the control group.
Unfortunately, across all patients, only 15% met criteria for a “successful transition”, with the majority of these patients being within the TRS group. In retrospect, less than 25% of recipients across groups evidenced optimal medication adherence, clinic attendance, and health status in the year prior to transferring to adult care. Of note, the definition of a successful transition was made retrospectively, and these benchmarks were not utilized as criteria for transfer. Nevertheless, this underscores the importance of assessing these domains prior to transferring care, as these patients may be at risk for poor outcomes following a change in health care settings. In addition, adherence declined following the transfer of care for the TRS group and remained suboptimal for the control group. This suggests that the assessment of TRS may not be sufficient to promote adherence following the transfer of care. It is recommended that future research and QI initiatives target the promotion of self-management skills and adherence following the transfer of care within the adult programs.
There are numerous potential barriers to transferring care, which may arise at the level of the patient, parent/ family, and the pediatric and adult provider (LaRosa et al., 2011). Thus, there is growing support for a multidimensional assessment of patients, parents and providers, as transition is more than the individual's age (Annunziato et al., 2011; Reed-Knight, Blount, & Gilleland, 2014; Schwartz, Tuchman, Hobbie, & Ginsberg, 2011). An assessment of transition readiness involves the early identification and remediation of potential challenges to the transfer of care such as medical stability, regimen adherence, psychosocial functioning, insurance coverage, transportation, and the availability of an adult provider. A recent study surveying a nationally representative sample of parents of adolescents and young adults aged 13–30 indicated that although a majority of these parents believe that their adolescent should begin seeing an adult care provider at age 18 or younger, only 30% actually reported that their adolescents transferred to an adult care setting by age 18. Further, although 85% of parents were confident that their adolescents ages 18–19 were taking medications correctly, there was less confidence in an adolescent's knowledge of when to go to the ER, how to complete a medical history including a medication list, how to make a doctor's appointment, and what services are covered by their insurance. Clearly, there is a need to prepare adolescents and young adults for independent health care management prior to transferring care (Fredericks et al. 2014).
There are frequently cited challenges to routinely assessing transition readiness, including time, resources, and lack of validated measures (Okumura et al., 2010; Zhang, Ho, & Kennedy, 2014). Ideally, the assessment of transition-related skills would be conducted using well validated measures in the context of standard clinical care. While there is not an accepted “gold standard” transition tool, there is a growing literature supporting measures that assess domains of self-management and transition readiness (Davis, Brown, Taylor, Epstein, & McPheeters, 2014; Ferris et al., 2012; Fredericks et al., 2010; Gilleland, Amaral, Mee, & Blount, 2012; Reed-Knight et al., 2014; Sawicki et al., 2011, Zhang et al., 2014).
For transition to be successful, it is essential that self-management skills are routinely assessed to allow learning opportunities to occur prior to receiving adult centered care. Results of this project suggest parent reports of their adolescent's self-management skills, regimen knowledge, and overall transition readiness were related to adolescent medication non-adherence. This suggests that parents may perceive that their adolescents are more advanced in their skills than they actually are, and may prematurely allow adolescents to assume responsibility over medication administration. Of note, parent reports were not obtained for those adolescents who presented in clinic independently; thus, this may represent a skewed sample. Rather than relying on parent and adolescent self-report of transition skills, direct assessment of regimen knowledge and self-management skills would allow providers to correct misinformation and provide education in the context of a clinic visit.
Transition readiness assessment should be used to guide skill-based instruction to improve the likelihood that adolescents and young adults will experience optimal outcomes during and after the transfer to adult care. This assessment should be comprehensive and integrative focusing on improvements in a patient's health related knowledge, decision-making skills, independence, and assertiveness (Samyn, 2012). The use of a transition readiness tool should guide instructional opportunities to prepare pediatric patients for a successful transition to adult health care. There is a need for transition readiness tools that are easy to use, have adequate levels of sensitivity and specificity, and have utility in goal setting and transition readiness interventions.
Future Directions
This report includes an initial investigation into the utility of transition readiness assessments using the TRS (Fredericks et al., 2010) and the impact of a transition program on post-transfer outcomes. Improvements notwithstanding, this QI project did have limitations. As noted, transition readiness assessment was not systematically assessed or documented in medical records prior to the initiation of this QI program. Our primary medication adherence and clinic attendance outcome measures were also not reliably documented. The use of clinical data that is already being collected as part of routine practice (e.g., laboratory data, medical record information) is standard for QI initiatives, but can pose challenges from a reliability and validity perspective, particularly if there is evidence of unreliability in the documentation. In addition, as this was a QI cycle rather than a randomized controlled trial, the comparisons between our TRS group and our historical control group should be interpreted with caution. Prior to the initiation of our TRS program, there was no previously defined “readiness to transfer” criteria and the transfer was based primarily on age rather self-management skills. However, this cycle did not specifically target adherence. Future cycles will include an examination of adherence data as part of transition readiness, although non-adherence may be a persistent problem that may not be completely ameliorated prior to transferring care. The current QI program focused on TRS and did not directly target adherence, which was assessed via laboratory blood values. Because this was a relatively healthy and medically stable group of patients, there may not have been enough variability to detect differences in health status and adherence patterns. It may be that differences in health outcomes may not be detected within the first year post-transfer, suggesting that longer follow-up may be warranted after the transfer of care.
This report outlines describes results from an ongoing QI initiative. We are currently engaged in continued evaluation and revision of our transition program. The TRS survey used in this first cycle was not sufficient to predict successful transfer to adult care, thus we are evaluating a revised assessment measure using an iterative process involving repeated assessments and documentation of TRS in the medical record. It is unclear if the lack of predictive utility relates to the measure, the definition of success, or other factors. We are collaborating with adult transplant team providers to identify targets and evaluate the impact of transition readiness interventions on adherence and health outcomes following the transfer of care. It is recommended that future research continue to investigate the feasibility and efficacy of transition programming in order to promote optimal long-term outcomes for children and adolescents with chronic health conditions as they transfer to adult care.
Acknowledgments
This work was supported in part by a K23 award from the National Institutes of Health (Grant Number DK090202) to EMF.
Footnotes
Compliance with Ethical Standards
Conflict of interest Emily M. Fredericks, John C. Magee, Sally J. Eder, Jessica R. Sevecke, Dawn Dore-Stites, Victoria Shieck, and M. James Lopez declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study. Informed consent was waived as our Institutional Review Board determined that this quality improvement program was exempt from review.
References
- American Academy of Pediatrics, American Academy of Family Physicians, American College of Physicians, & Transitions Clinical Report Authoring Group Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2011;128:182–200. doi: 10.1542/peds.2011-0969. [DOI] [PubMed] [Google Scholar]
- Annunziato RA, Baisley MC, Arrato N, Barton C, Henderling F, Arnon R, Kerkar N. Strangers headed to a strange land? A pilot study of using a transition coordinator to improve transfer from pediatric to adult services. Journal of Pediatrics. 2013;163:1628–1633. doi: 10.1016/j.jpeds.2013.07.031. [DOI] [PubMed] [Google Scholar]
- Annunziato RA, Emre S, Shneider B, Barton C, Dugan CA, Shemesh E. Adherence and medical outcomes in pediatric liver transplant recipients who transition to adult services. Pediatric Transplantation. 2007;11:608–614. doi: 10.1111/j.1399-3046.2007.00689.x. [DOI] [PubMed] [Google Scholar]
- Annunziato RA, Freiberger D, Martin K, Helcer J, Fitzgerald C, Lefkowitz DS. An empirically based practice perspective on the transition to adulthood for solid organ transplant recipients. Pediatric Transplantation. 2014;18:794–802. doi: 10.1111/petr.12359. [DOI] [PubMed] [Google Scholar]
- Annunziato RA, Parkar S, Dugan CA, Barsade S, Arnon R, Miloh T, Shemesh E. Brief report: Deficits in health care management skills among adolescent and young adult liver transplant recipients transitioning to adult care settings. Journal of Pediatric Psychology. 2011;36:155–159. doi: 10.1093/jpepsy/jsp110. [DOI] [PubMed] [Google Scholar]
- Bell LE, Bartosh SM, Davis CL, Dobbels F, Al-Uzri A, Lotstein D, Dharnidharka VR. Adolescent transition to adult care in solid organ transplantation: A consensus conference report. American Journal of Transplantation. 2008;8:2230–2242. doi: 10.1111/j.1600-6143.2008.02415.x. [DOI] [PubMed] [Google Scholar]
- Blum RW, Garell D, Hodgman CH, Jorissen TW, Okinow NA, Orr DP, Slap GB. Transition from childcentered to adult health-care systems for adolescents with chronic conditions—A position paper of the society for adolescent medicine. Journal of Adolescent Health. 1993;14:570–576. doi: 10.1016/1054-139x(93)90143-d. [DOI] [PubMed] [Google Scholar]
- Bucuvalas JC, Alonso E. Health-related quality of life in liver transplant recipients. Current Opinion in Organ Transplantation. 2005;10(2):77–80. [Google Scholar]
- Davis AM, Brown RF, Taylor JL, Epstein RA, McPheeters ML. Transition care for children with special health care needs. Pediatrics. 2014;134:900–908. doi: 10.1542/peds.2014-1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Silva PS, Fishman LN. Transition of the patient with IBD from pediatric to adult care—An assessment of current evidence. Inflammatory Bowel Diseases. 2014;20:1458–1464. doi: 10.1097/MIB.0000000000000045. [DOI] [PubMed] [Google Scholar]
- Ferris ME, Harward DH, Bickford K, Layton JB, Ferris MT, Hogan SL, Hooper SR. A clinical tool to measure the components of health-care transition from pediatric care to adult care: The UNC TR(x)ANSITION scale. Renal Failure. 2012;34:744–753. doi: 10.3109/0886022X.2012.678171. [DOI] [PubMed] [Google Scholar]
- Foster BJ. Heightened graft failure risk during emerging adulthood and transition to adult care. Pediatric Nephrology. 2015;30(4):567–576. doi: 10.1007/s00467-014-2859-7. [DOI] [PubMed] [Google Scholar]
- Fredericks EM, Dore-Stites D, Lopez MJ, Well A, Shieck V, Freed GL, Magee JC. Transition of pediatric liver transplant recipients to adult care: Patient and parent perspectives. Pediatric Transplantation. 2011;15:414–424. doi: 10.1111/j.1399-3046.2011.01499.x. [DOI] [PubMed] [Google Scholar]
- Fredericks EM, Dore-Stites D, Well A, Magee JC, Freed GL, Shieck V, Lopez MJ. Assessment of transition readiness skills and adherence in pediatric liver transplant recipients. Pediatric Transplantation. 2010;14:944–953. doi: 10.1111/j.1399-3046.2010.01349.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredericks EM, Lopez MJ, Magee JC, Shieck V, Opipari-Arrigan L. Psychological functioning, nonadherence and health outcomes after pediatric liver transplantation. American Journal of Transplantation. 2007;7:1974–1983. doi: 10.1111/j.1600-6143.2007.01878.x. [DOI] [PubMed] [Google Scholar]
- Fredericks EM, Magee JC, Opipari-Arrigan L, Shieck V, Well A, Lopez MJ. Adherence and health-related quality of life in adolescent liver transplant recipients. Pediatric Transplantation. 2008;12(3):289–299. doi: 10.1111/j.1399-3046.2008.00901.x. [DOI] [PubMed] [Google Scholar]
- Fredericks EM, Singer DC, Kauffman AD, Gebremariam A, Matos-Moreno A, Clark SJ, Davis MM. Can their 18-year-olds make a doctor's appointment? Half of parents say no. C.S. Mott Children‘s Hospital National Poll on Children's Health. University of Michigan; 2014. http://mottnpch.org/sites/default/files/documents/121514_transitioncare.pdf. [Google Scholar]
- Gilleland J, Amaral S, Mee L, Blount R. Getting ready to leave: Transition readiness in adolescent kidney transplant recipients. Journal of Pediatric Psychology. 2012;37:85–96. doi: 10.1093/jpepsy/jsr049. [DOI] [PubMed] [Google Scholar]
- Nuzio SG, Tizzard SA, Vajro P. Tips and hints for the transition: What adult hepatologists should know when accept teens with a pediatric hepatobiliary disease. Clinics and Research in Hepatology and Gastroenterology. 2014;38:277–283. doi: 10.1016/j.clinre.2014.03.012. [DOI] [PubMed] [Google Scholar]
- Huang JS, Gottschalk M, Pian M, Dillon L, Barajas D, Bartholomew LK. Transition to adult care: Systematic assessment of adolescents with chronic illnesses and their medical teams. Journal of Pediatrics. 2011;159:994–998. doi: 10.1016/j.jpeds.2011.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy A, Sawyer S. Transition from pediatric to adult services: Are we getting it right? Current Opinion in Pediatrics. 2008;20:403–409. doi: 10.1097/MOP.0b013e328305e128. [DOI] [PubMed] [Google Scholar]
- Kennedy A, Sloman F, Douglass JA, Sawyer SM. Young people with chronic illness: The approach to transition. Internal Medicine Journal. 2007;37(8):555–560. doi: 10.1111/j.1445-5994.2007.01440.x. [DOI] [PubMed] [Google Scholar]
- Kieckhefer GM, Trahms CM. Supporting development of children with chronic conditions: From compliance toward shared management. Pediatric Nursing. 2000;26:354–363. [PubMed] [Google Scholar]
- LaRosa C, Glah C, Baluarte HJ, Meyers KEC. Solidorgan transplantation in childhood: Transitioning to adult health care. Pediatrics. 2011;127:742–753. doi: 10.1542/peds.2010-1232. [DOI] [PubMed] [Google Scholar]
- McDonagh JE, Kelly DA. Trans-plan-sition! Transplantation and transition. Pediatric Transplantation. 2007;11:578–581. doi: 10.1111/j.1399-3046.2007.00756.x. [DOI] [PubMed] [Google Scholar]
- Nasr SZ, Campbell C, Howatt W. Transition program from pediatric to adult care for cystic fibrosis patients. Journal of Adolescent Health. 1992;13:682–685. doi: 10.1016/1054-139x(92)90063-h. [DOI] [PubMed] [Google Scholar]
- Ng VL, Alonso EM, Bucuvalas JC, Cohen G, Limbers CA, Varni JW, Anand R. Health status of children alive 10 years after pediatric liver transplantation performed in the US and Canada: Report of the studies of pediatric liver transplantation experience. The Journal of Pediatrics. 2012;160:820–826. e823. doi: 10.1016/j.jpeds.2011.10.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okumura MJ, Kerr EA, Cabana MD, Davis MM, Demonner S, Heisler M. Physician views on barriers to primary care for young adults with childhood-onset chronic disease. Pediatrics. 2010;125:e748–e754. doi: 10.1542/peds.2008-3451. [DOI] [PubMed] [Google Scholar]
- Rapoff MA. Adherence to pediatric medical regimens. Kluwer Academic/Plenum Press; New York: 1999. [Google Scholar]
- Reed-Knight B, Blount RL, Gilleland J. The transition of health care responsibility from parents to youth diagnosed with chronic illness: A developmental systems perspective. Families, Systems, & Health. 2014;32:219–234. doi: 10.1037/fsh0000039. [DOI] [PubMed] [Google Scholar]
- Reid GJ, Irvine MJ, McCrindle BW, Sananes R, Ritvo PG, Siu SC, Webb GD. Prevalence and correlates of successful transfer from pediatric to adult health care among a cohort of young adults with complex congenital heart defects. Pediatrics. 2004;113:197–205. doi: 10.1542/peds.113.3.e197. [DOI] [PubMed] [Google Scholar]
- Rosen DS, Blum RW, Britto M, Sawyer SM, Siegel DM. Transition to adult health care for adolescents and young adults with chronic conditions: Position paper of the society for adolescent medicine. Journal of Adolescent Health. 2003;33:309–311. doi: 10.1016/s1054-139x(03)00208-8. [DOI] [PubMed] [Google Scholar]
- Samyn M. Optimizing outcomes for pediatric recipients. Liver Transplantation. 2012;18:S34–S38. doi: 10.1002/lt.23543. [DOI] [PubMed] [Google Scholar]
- Sawicki GS, Lukens-Bull K, Yin X, Demars N, Huang IC, Livingood W, Wood D. Measuring the transition readiness of youth with special healthcare needs: Validation of the TRAQ transition readiness assessment questionnaire. Journal of Pediatric Psychology. 2011;36:160–171. doi: 10.1093/jpepsy/jsp128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawyer SM, Blair S, Bowes G. Chronic illness in adolescents: Transfer or transition to adult services? Journal Paediatric Child Health. 1997;33:88–90. doi: 10.1111/j.1440-1754.1997.tb01005.x. [DOI] [PubMed] [Google Scholar]
- Schurman JV, Gayes LA, Slosky L, Hunter ME, Pino FA. Publishing quality improvement work in clinical practice in pediatric psychology: The “why” and“how to”. Clinical Practice in Pediatric Psychology. 2015;3:80–91. [Google Scholar]
- Schwartz LA, Tuchman LK, Hobbie WL, Ginsberg JP. A social-ecological model of readiness for transition to adult-oriented care for adolescents and young adults with chronic health conditions. Child: Care, Health and Development. 2011;37(6):883–895. doi: 10.1111/j.1365-2214.2011.01282.x. [DOI] [PubMed] [Google Scholar]
- Schäfer-Keller P, Steiger J, Bock A, Denhaerynck K, De Geest S. Diagnostic accuracy of measurement methodsto assess non-adherence to immunosuppressive drugs in kidney transplant recipients. American Journal of Transplantation. 2008;8:616–626. doi: 10.1111/j.1600-6143.2007.02127.x. [DOI] [PubMed] [Google Scholar]
- Shemesh E, Shneider BL, Savitzky JK, Arnott L, Gondolesi GE, Krieger NR, Emre S. Medication adherence in pediatric and adolescent liver transplant recipients. Pediatrics. 2004;113:825–832. doi: 10.1542/peds.113.4.825. [DOI] [PubMed] [Google Scholar]
- Shemesh E, Lurie S, Stuber ML, Emre S, Patel Y, Vohra P, Shneider BL. A pilot study of posttraumatic stress and nonadherence in pediatric liver transplant recipients. Pediatrics. 2000;105:E29. doi: 10.1542/peds.105.2.e29. [DOI] [PubMed] [Google Scholar]
- Supelana C, Annunziato RA, Schiano TD, Anand R, Vaidya S, Chuang K, Shemesh E. Medication level variability index predicts rejection, possibly due to nonadherence, in adult liver transplant recipients. Liver Transplantation. 2014;20:1168–1177. doi: 10.1002/lt.23930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor MJ, McNicholas C, Nicolay C, Darzi A, Bell D, Reed JE. Systematic review of the application of the plan–do–study–act method to improve quality in healthcare. BMJ Quality & Safety. 2013 doi: 10.1136/bmjqs-2013-001862. doi:10.1136/bmjqs-2013-001862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venkat VL, Nick TG, Wang Y, Bucuvalas JC. An objective measure to identify pediatric liver transplant recipients at risk for late allograft rejection related to non-adherence. Pediatric Transplantation. 2008;12:67–72. doi: 10.1111/j.1399-3046.2007.00794.x. [DOI] [PubMed] [Google Scholar]
- Watson AR. Non-compliance and transfer from paediatric to adult transplant unit. Pediatric Nephrology. 2000;14:469–472. doi: 10.1007/s004670050794. [DOI] [PubMed] [Google Scholar]
- Watson AR. Problems and pitfalls of transition from paediatric to adult renal care. Pediatric Nephrology. 2005;20(2):113. doi: 10.1007/s00467-004-1763-y. [DOI] [PubMed] [Google Scholar]
- Zhang LF, Ho JS, Kennedy SE. A systematic review of the psychometric properties of transition readiness assessment tools in adolescents with chronic disease. BMC Pediatrics. 2014;14:4. doi: 10.1186/1471-2431-14-4. [DOI] [PMC free article] [PubMed] [Google Scholar]