Abstract
Introduction:
In order to control serious pulpal pain following odontogenic infections in pregnant women, endodontic treatment may become necessary. The aim of this study was to assess the perception of dentists about rendering endodontic treatment to pregnant women.
Materials and Methods:
This was a cross-sectional study of resident doctors in the different dental specialties in Nigeria preparing for the various levels of the fellowship examinations of the West Africa College of Surgeons and the National Postgraduate Medical College of Nigeria. Data were collected by the means of a 17-itemed questionnaire which sought information on respondents' demography, their considerations while rendering endodontic treatment to the pregnant patients and their perceptions of the safety of endodontic treatment in pregnancy. The data collected were analyzed using the Statistical Package for Social Science version 21.0.
Results:
With regards to the safety of endodontic treatment during pregnancy, 91.8% considered it safe, and this was not statistically significant in relation to the specialty or status of the respondent. Majority (77.0%) agreed they would undertake a root canal treatment on a pregnant patient with all respondents in restorative dentistry, prosthodontics, periodontics, and pedodontics in the affirmative while all in oral pathology would refuse to do such (P = 0.0001).
Conclusion:
Dental residents are aware of the safety of endodontic treatment in pregnant women. However, gaps exist in their knowledge, bringing to the fore, the need for inclusion of pregnancy-specific training in the dental postgraduate curriculum.
Keywords: Dental residents, endodontic treatment, pregnancy
INTRODUCTION
Pregnancy does not translate to being medically compromised; therefore dental treatment should not be denied simply because a woman is pregnant. The pregnant woman who presents for dental care may require special considerations.1 Therefore, the management of these patients may require adjustments in the timing and type of dental treatment, as well as in the drugs to be prescribed.2 Proper risk assessments should be done for the mother and fetus. The following should be considered: Risk of teratogenicity in the fetus due to drugs taken by the mother, susceptibility to supine hypotensive syndrome as a result of a decrease in blood pressure and cardiac output while the patient is in a supine position, and the potential danger of disseminated vascular coagulopathy due to increase in clotting factors.1
Oral health during pregnancy has, for long, been a focus of concern 3 with obstetricians acknowledging its importance and attendant effect on pregnancy outcomes.4,5 The physiologic changes in pregnancy include changes in the oral cavity with an attendant increase in susceptibility to oral infections.6 Also, increased consumption of carbohydrates, increased acid in the mouth from vomiting and reduced production of saliva and possibly too, increased acidity of saliva have been believed to increase the risk of dental caries in pregnancy.7 A study found that pregnant women were 1.97 times more likely to suffer from dental caries than the nonpregnant women.8 A 74.5% prevalence of dental caries among the pregnant women was observed in a study by Mahmud et al.9
Usually, pregnant patients are not immunocompromised; however, there is suppression of the maternal immune system in response to the fetus 6 subsequently causing a decrease in cell-mediated immunity, as well as natural killer cell activity.10 With the foregoing, odontogenic infections have the potential to progress rapidly to deep-space infections eventually compromising the oropharyngeal airway.10 In addition, pregnant women may also receive a prescription and/or over-the-counter analgesics to control serious pulpal pain. Abuse of these drugs rather than receiving the appropriate dental treatment may have deleterious effects on the fetus and the pregnant mother. Therefore, it is imperative that odontogenic infections should be treated promptly at any time during pregnancy. One of the possible treatment options is endodontic treatment involving the extirpation of the diseased pulp. Endodontic treatment may entail the use of radiographs, local anesthetic agents, root canal irrigants, intra-canal medications, and drugs (analgesics and antibiotics).
Radiographs are very important during endodontic treatment. They are required for proper diagnosis, determination of working length, proper obturation, and posttreatment evaluation. Intraoral radiographs are safe for pregnant patients as the X-rays are directed to the mouth and not the abdomen, along with the use of protective measures such as high-speed film, collimation, filtration, lead apron, and a thyroid collar.11 It has been proposed that, concerned pregnant patients be reassured that in all cases requiring such imaging, the As Low As Reasonably Achievable (ALARA) principle will be practised, and only radiographs necessary for diagnosis and treatment will be obtained.12 X-ray radiation exposure during pregnancy totaling <5-10 cGy, and a full mouth series of dental radiographs of only 8 × 10-4 cGy has been reported to show no increase in congenital anomalies or intrauterine growth retardation.11,13,14
Local anesthetics are relatively safe when administered properly and in the correct amount during pregnancy.10 The quantity of anesthetic agent administered could be a probable cause for concern among endodontists. This may be because of the uncertainty of the initial dose administered being ineffective in achieving anesthesia, thus requiring an additional anesthetic agent to make the patient feel more comfortable. Pain incurred during treatment may induce stress which could be more damaging to the fetus than the effect (s) of additional quantities of anesthetic agent. Most anesthetic agents contain the vasoconstrictor epinephrine which is a category C drug. This drug has been studied in amount of up to 0.1 mg added to local anesthetics. No unusual side effects or complications were reported following its use for epidural anesthesia during labor.15 It has been reported that the local anesthetic with epinephrine administered as an intravascular injection may, at least supposedly, cause a deficiency of uteroplacental blood flow.10 However, for a healthy pregnant patient, the 1:100,000 epinephrine concentration used in dentistry, administered by proper aspiration technique and limited to the minimal dose required, is safe.16
Endodontic treatment in pregnancy is directed towards controlling disease, maintaining a healthy oral environment, and preventing potential problems that could occur later in the pregnancy or during the postpartum period.16 It has been asserted that neither the cleansing irrigant, hypochlorite nor root canal filling materials used in endodontic treatment is detrimental to the fetus.17 The initial 3 months of pregnancy are considered vital to the growth of the fetus. It has been recommended that any avoidable treatment in the first trimester should be moved to the next trimester to prevent any threat of untoward effects of dental treatment.10 By the end of the first trimester, organogenesis is complete, the uterine size is not large enough to make sitting on the dental chair uncomfortable and nausea has generally waned. These make the second trimester an ideal period to undertake endodontic treatment. However, extensive elective endodontic procedures should be postponed until after delivery.
Dentists frequently have to face the anxiety associated with the safety of the dental treatment during pregnancy18, as well as the need to eliminate the odontogenic infection. Assessment of the potential risk in rendering endodontic treatment during pregnancy is important while paying attention to the physiologic changes associated with pregnancy. Probably due to the wrong suppositions propagated following the lack of proper information, dentists are wary of rendering treatment to pregnant women.19,20 Reviews on amalgam fillings and periodontal therapy have been reported 21 but there is a paucity of studies reviewing perceptions of endodontic treatment in the pregnant woman. This study to assess the perception of dentists about endodontic treatment during pregnancy thus became imperative as the purpose of this study.
MATERIALS AND METHODS
This cross-sectional study was carried out among the resident doctors in the different dental specialties in Nigeria preparing for the various levels of the fellowship examinations of the West Africa College of Surgeons and the National Postgraduate Medical College of Nigeria, who attended the revision course in Lagos State in September 2012 and April 2013. A pretested, self-administered questionnaire was used for the data collection. The 17-itemed questionnaire sought information on respondents' demography, their considerations while rendering endodontic treatment to the pregnant patients and their perceptions of the safety of endodontic treatment in pregnancy.
The data collected were analyzed using the IBM Statistical Package for Social Science (SPSS) for windows version 21.0. Armonk NY: IBM Corp. The results were presented as tables and cross-tabulations. The nonparametric analysis in the form of Chi-square test was carried out for statistical significance with P< 0.05 considered statistically significant.
RESULTS
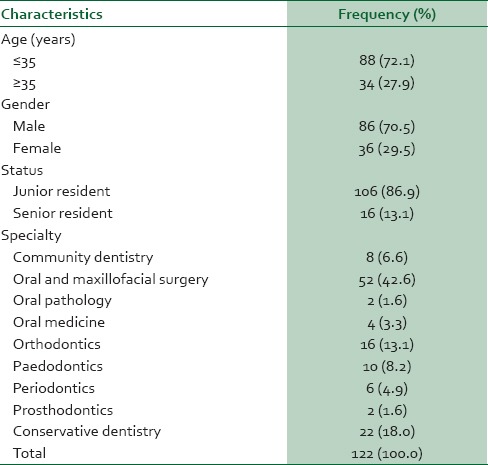
The majority (72.1%) of the respondents were <35 years of age. There was a male dominance with a male:female ratio of 1:0.42. Most (86.9%) of the respondents were junior residents and 42.6% were residents in oral and maxillofacial surgery [Table 1].
Table 1.
Demographic characteristics of the respondents
The majority (86.9%) thought that appropriate treatment of dental pain and infection was important in pregnancy. While rendering such treatment, 82% were aware that the pregnant patient should be positioned in a special way [Table 2] with 36.1% recommending that the pregnant patient's positioning should allow her head to be higher than her feet.
Table 2.
Responses regarding dental treatment among pregnant women
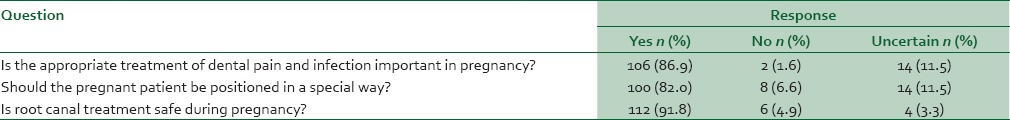
With regards to the safety of endodontic treatment during pregnancy, 91.8% considered it safe [Table 2] and this was not statistically significant in relation to the specialty or status of the respondent. However, 52.4% of the respondents recommended that the ideal period to carry out endodontic treatment was the second trimester while 21.3% thought that any time during pregnancy was safe if endodontic treatment was indicated.
Table 3 displays the responses of respondents concerning agents employed in the course of endodontic treatment. The majority (77.0%) of the respondents felt use of local anesthetic with epinephrine was safe in pregnancy. All the females were certain of the safety of local anesthetic with epinephrine, and this was statistically significant (P = 0.03). All the respondents in oral medicine and orthodontics considered the use of local anesthetic with epinephrine in pregnancy safe while respondents in oral pathology were uncertain, and this was statistically significant (P = 0.0001). This had no statistically significant relationship with the status of the respondents.
Table 3.
Responses regarding agents employed during endodontic treatment in pregnancy
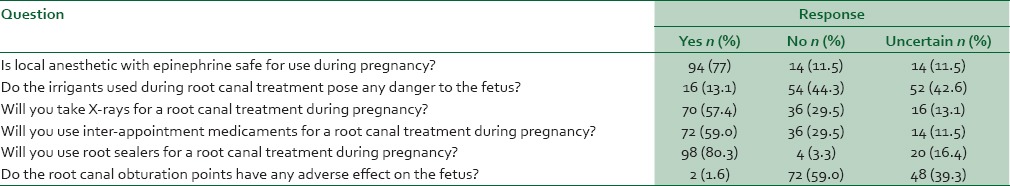
As regards the safety of the use of irrigants during root canal treatment, 13.1% of the respondents thought that their use posed some danger to the fetus while 42.6% were uncertain of any danger their use posed. This was statistically significant in relation to the specialty of the respondents (P = 0.02) with a majority of respondents who thought that it was not safe being oral and maxillofacial surgery residents. In the same vein, it was statistically significant in relation to the gender of the respondents with no female agreeing that irrigants used during endodontic treatment posed any danger to the fetus (P = 0.006). However, there was no statistically significant association between the status of the respondents and their perception of the safety of irrigants use.
More than half (57.4%) of the respondents agreed they would expose dental X-rays for a root canal treatment procedure during pregnancy. The majority of those who were uncertain if they would expose X-rays for a root canal treatment during pregnancy were residents in oral and maxillofacial surgery, and this was statistically significant (P = 0.002). Likewise, 59.0% agreed that they would place interappointment medicaments during a root canal treatment procedure in pregnancy. The majority of the respondents in restorative, periodontics, pedodontics, prosthodontics, and orthodontics specialties were willing to use interappointment medicaments during root canal treatment on the pregnant patient while all those in oral pathology were uncertain and this was statistically significant (P = 0.0001). Also statistically significant was the association of gender with the use of interappointment medicaments for a root canal treatment during pregnancy with more females agreeing (P = 0.01) but no such association with the status of the respondents.
In relation to the use of root sealers for a root canal treatment during pregnancy, majority (80.3%) admitted they would use them, and this was statistically significant in relation to the specialty of the respondents (P = 0.0001). All respondents in prosthodontics, pedodontics, and orthodontics affirmed they would use root sealers while those in oral pathology were not certain.
When asked if root canal obturation points could have any adverse effect on the fetus, only 1.6% claimed they could, and these participants were in restorative dentistry and this was statistically significant (P = 0.005).
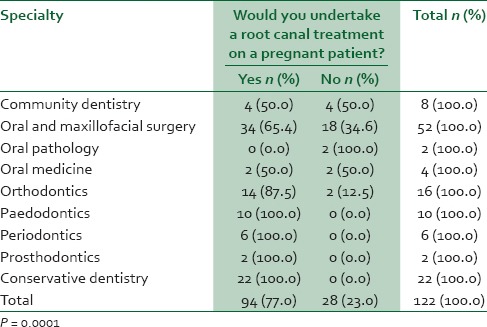
Majority (77.0%) agreed they would undertake a root canal treatment on a pregnant patient with all respondents in restorative dentistry, prosthodontics, periodontics, and pedodontics in the affirmative while all in oral pathology would refuse to do such (P = 0.0001, Table 4).
Table 4.
Relating undertaking a root canal treatment on a pregnant patient with specialty
DISCUSSION
Understanding the physiologic changes associated with pregnancy, as well as the effects of dental procedures including radiography and drug use on the pregnant patients and the developing fetus is requisite in rendering dental treatment to pregnant patients.22
The male preponderance in this study is similar to other Nigerian studies 23,24 reflecting that there is still a male-domination of the dental profession in Nigeria. Oral and maxillofacial surgery was the most enrolled specialty among residents in this study. This may be due to the fact that it was one of the first specialties of dentistry to be developed in Nigeria.
The importance of appropriate treatment of dental pain and infection has been well-emphasized, and this was affirmed in this study. It has been advocated that endodontic treatment, when indicated, should not be deferred till after delivery to avoid the inappropriate long-term use of analgesics to relieve pain.16 However, proper positioning of the pregnant patient during dental treatment is necessary, given the likelihood of hypotensive syndrome and the attendant loss of consciousness. In this study, the need for this proper positioning of pregnant women during dental treatment was recognized by a majority but only a few had an idea of which was the best position. This reflects a gap in knowledge among residents who are in active, specialization training and who are expected to be up-to-date with current trends.
Dental treatment, including endodontic treatment, has been certified safe in pregnancy. Nevertheless, it has been recommended that elective procedures be avoided until the end of pregnancy and for only emergency treatment to be given or if possible, be delayed until the second trimester.22 The findings of this study suggest that dental residents have a clue of the timing of dental treatment for the pregnant patient. However, this level of awareness is insufficient.
Studies have not reported adverse events associated with rendering endodontic treatment. Local anesthetic with vasoconstrictor can be safely administered to the pregnant patients during the dental treatment 25 but aspiration must always be done to minimize the likelihood of intravascular injection.26 Dental residents seem to be conversant with this especially as most dental procedures require the use of local anesthetic. The scope of oral medicine specialty consists of the nonsurgical management of oral diseases where applicable and includes the use of pharmacological agents in the management of dental conditions. Therefore, it is not surprising that all the residents in oral medicine were conversant with the safety of the use of local anesthetic with epinephrine in pregnancy.
Not much has been reported on the use of endodontic irrigants for root canal treatment during pregnancy, and this was reflected in the varied opinions regarding the safety of endodontic irrigants use in pregnancy. It is imperative therefore that research into the possible adverse effects of endodontic irrigants in pregnancy be looked into, this will provide informed choices for dentists while selecting which irrigant to use for root canal treatment procedures in pregnant women. A lot has been done to ascertain the safety of dental X-rays during pregnancy. However, a reasonable percentage of dental residents in this study were not confident exposing X-rays for root canal treatment procedures on pregnant women. There is the need for more emphasis on the safety of dental X-rays and the use of protective measures such as the use of modern imaging machines (with low-dose, high-yield radio-diagnosis), high-speed films, collimation, filtration, lead aprons, and a thyroid lead collars.
The female residents in this study exhibited a better knowledge of the use of local anesthetics, interappointment medicaments, and endodontic irrigants. This may be because women tend to be interested in or concerned with medication use in pregnancy. The specialty of training tends to boost confidence in rendering treatment to pregnant patients. Endodontics is a subspecialty in restorative dentistry in Nigeria, so residents in this specialty tended to display more confidence by their eagerness to render endodontic treatment to pregnant patients.
The hierarchical status of the respondents did not play any role in the outcomes of all the questions asked. This shows that increased clinical exposure, experience, and knowledge did not influence the perception of dental residents toward rendering endodontic treatment to the pregnant women.
Limitations exist in the ability to generalize the findings of this study given the fact that some specialties such as oral medicine and oral pathology were poorly represented in the study. In addition, the authors recognize that specific agents used as irrigants, sealers, and obturating points were not enquired about. This could have thrown more light on the depth of knowledge of the respondents about these materials and their use in endodontic treatment in pregnancy.
CONCLUSION
The findings of the study suggest that dental residents are aware of the safety of endodontic treatment in pregnant women. However, there are gaps in knowledge with regards to the proper positioning of pregnant women, the timing of treatment, the safety of the use of irrigants, and radiographic exposure for pregnant women. It is imperative that the postgraduate training should include pregnancy-specific, confidence-boosting knowledge for better endodontic treatment of the pregnant women.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Cengiz SB. The pregnant patient: Considerations for dental management and drug use. Quintessence Int. 2007;38:e133–42. [PubMed] [Google Scholar]
- 2.Mishkin DJ, Johnson KE, Jared T. Dental diseases. In: Gleicher N, editor. Principles and Practice of Medical Therapy in Pregnancy. Stamford, Connecticut: Appleton and Large; 1998. pp. 1093–5. [Google Scholar]
- 3.American College of Obstetricians and Gynecologists Practice Bulletin. Clinical management guidelines for obstetriciangynecologists. Gestational diabetes. Obstet Gynecol. 2004;98:525–38. [Google Scholar]
- 4.Enabulele JE, Ibhawoh LO. Awareness of obstetrics residents of the oral health component of management of nausea and vomiting in pregnancy. BMC Pregnancy Childbirth. 2014;14:388. doi: 10.1186/s12884-014-0388-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Enabulele JE, Ibhawoh LO. Perceptions and practices regarding perinatal oral health: A survey of ante-natal care physicians. Niger Res J Clin Sci. 2012;2:141–8. [Google Scholar]
- 6.Gordon MC. Maternal physiology in pregnancy. In: Gabbe SG, Niebyl JR, Simpson J, editors. Obstetrics: Normal and Problem Pregnancies. 4th ed. New York: Churchill Livingstone; 2002. pp. 63–91. [Google Scholar]
- 7.Cucó G, Fernández-Ballart J, Sala J, Viladrich C, Iranzo R, Vila J, et al. Dietary patterns and associated lifestyles in preconception, pregnancy and postpartum. Eur J Clin Nutr. 2006;60:364–71. doi: 10.1038/sj.ejcn.1602324. [DOI] [PubMed] [Google Scholar]
- 8.Christensen LB, Jeppe-Jensen D, Petersen PE. Self-reported gingival conditions and self-care in the oral health of Danish women during pregnancy. J Clin Periodontol. 2003;30:949–53. doi: 10.1034/j.1600-051x.2003.00404.x. [DOI] [PubMed] [Google Scholar]
- 9.Mahmud SZ, Uddin MM, Begum F. Assessment of common oral and dental diseases among pregnant women at Dhaka City in Bangladesh. South Am J Med. 2014;2:165–77. [Google Scholar]
- 10.Giglio JA, Lanni SM, Laskin DM, Giglio NW. Oral health care for the pregnant patient. J Can Dent Assoc. 2009;75:43–8. [PubMed] [Google Scholar]
- 11.Richards AG, Colquitt WN. Reduction in dental X-ray exposures during the past 60 years. J Am Dent Assoc. 1981;103:713–8. doi: 10.14219/jada.archive.1981.0378. [DOI] [PubMed] [Google Scholar]
- 12.Katz VL. Prenatal care. In: Scott JR, Gibbs RS, Karlan BY, Haney AF, editors. Danforth's Obstetrics and Gynecology. 9th ed. Philadelphia: Lippincott, Williams & Wilkins; 2003. pp. 43–8. [Google Scholar]
- 13.Brent RL. The effect of embryonic and fetal exposure to x-ray, microwaves, and ultrasound: Counseling the pregnant and nonpregnant patient about these risks. Semin Oncol. 1989;16:347–68. [PubMed] [Google Scholar]
- 14.Guidelines for Perinatal Care. 6th ed. IL: Elk Grove Village; 2007. American Academy of Pediatrics/American College of Obstetrics and Gynecology; pp. 211–2. [Google Scholar]
- 15.Gurbet A, Turker G, Kose DO, Uckunkaya N. Intrathecal epinephrine in combined spinal-epidural analgesia for labor: Dose-response relationship for epinephrine added to a local anesthetic-opioid combination. Int J Obstet Anesth. 2005;14:121–5. doi: 10.1016/j.ijoa.2004.12.002. [DOI] [PubMed] [Google Scholar]
- 16.Little JW, Falace DA, Miller CS, Rhodus NL. Dental Management of the Medically Compromised Patient. 7th ed. St. Louis: C.V. Mosby; 2008. pp. 268–78. (456). [Google Scholar]
- 17.Risks Associated and Best Strategy for Root Canal Treatment During Pregnancy. [Last accessed on 2013 Jun 20]. Available from: http://www.monashdentalgroup.com.au/endodontic/risks-associatedandbest-strategy-for-root-canal-treatment-duringpregnancy/
- 18.Women's Oral Health Issues. Chicago, IL: American Dental Association; 2006. [Last accessed on 2013 Dec 20]. American Dental Association (ADA) Council on Access, Prevention and Interprofessional Relations. Available from: http://www.ada.org/section/professional/pdfs/healthcare_women'spdf . [Google Scholar]
- 19.Amini H, Casimassimo PS. Prenatal dental care: A review. Gen Dent. 2010;58:176–80. [PubMed] [Google Scholar]
- 20.Detman LA, Cottrell BH, Denis-Luque MF. Exploring dental care misconceptions and barriers in pregnancy. Birth. 2010;37:318–24. doi: 10.1111/j.1523-536X.2010.00427.x. [DOI] [PubMed] [Google Scholar]
- 21.Achtari MD, Georgakopoulou EA, Afentoulide N. Dental care throughout pregnancy: What a dentist must know. Oral Health Dent Manag. 2012;11:169–76. [PubMed] [Google Scholar]
- 22.Garg N, Garg A. Pregnancy considerations in dentistry. Indian J Res Dent. 2014;1:8–11. [Google Scholar]
- 23.Onyeaso CO, Dosumu EB, Obuekwe O. Postgraduate dental education in Nigeria: Professional knowledge self assessed in relationship to skills among resident dental surgeons in Nigerian teaching hospitals. Niger J Med. 2004;13:18–25. [PubMed] [Google Scholar]
- 24.Okoh M, Enabulele J. Gender trend in practice and job satisfaction among the resident dentists in University of Benin Teaching Hospital. Int J Biomed Health Sci. 2011;7:7–15. [Google Scholar]
- 25.Haas DA, Pynn BR, Sands TD. Drug use for the pregnant or lactating patient. Gen Dent. 2000;48:54–60. [PubMed] [Google Scholar]
- 26.Haas DA. An update on local anesthetics in dentistry. J Can Dent Assoc. 2002;68:546–51. [PubMed] [Google Scholar]


