Abstract
Introduction:
Prescription medicines constitute a significant proportion of total healthcare expenditure in many countries of the world. Nonrational prescribing by healthcare providers contributes significantly to this relatively high proportion. In many developing countries of the world, a significant proportion of the population pays “out of pocket” to access healthcare, sometimes leading to catastrophic healthcare expenditure. Healthcare insurance is a form of healthcare financing that promotes judicious use of the resources and ensuring the cost-effectiveness of interventions through the use of affordable drugs. The main objective of this study was to compare concurrently the prescribing practices in the general outpatients' clinic (noninsured patients) and the National Health Insurance Scheme (NHIS) clinic (patients with insurance coverage).
Materials and Methods:
A cross-sectional study was conducted in the general outpatients' and the “NHIS” clinics of the Ekiti State University Teaching Hospital, Ado-Ekiti, South-western Nigeria. The medical records of patients, who attended these two clinics between the 1st March and 30th June 2014 were retrieved and used for the study.
Results:
The average number of prescribed drugs for patients attending the general outpatients' clinic was 3.9 ± 2.0 while that from the NHIS clinic was 4.1 ± 1.6 (P = 0.24). Prescribing by generic names was done in 48.2 ± 23.8% and 45.8 ± 22.9% of prescriptions from the general outpatients' and NHIS clinic, respectively. Percentage of encounters with antibiotics was 49.4% and 33.6% of patients who attended the NHIS and general outpatients' clinics, respectively.
Conclusion:
There was a trend to having more medicines prescribed and more encounters with antibiotics among patients enrolled under the health insurance scheme.
Keywords: Drug prescription, health insurance, outpatients clinic, rational use of medicines
INTRODUCTION
Prescription medicines constitute a significant proportion of total healthcare expenditure in many countries of the world.1,2 Report from many European countries shows that prescription medicines account for between 10.4% and 27.6% of the total healthcare expenditure.3,4 Nonrational prescribing by healthcare providers contributes significantly to this relatively high proportion. In many developing countries of the world, a significant proportion of the population pays “out of pocket” to access healthcare, sometimes leading to catastrophic healthcare expenditure.5,6 This is at variance with the situation in many developed countries where healthcare insurance covers a large chunk of their population.7,8 Health insurance is a form of healthcare financing where financial resources are pooled together and shared to alleviate the burden of healthcare costs and financial risk of the people. Additional objectives of healthcare insurance are judicious use of the resources and ensuring the cost-effectiveness of interventions through the use of affordable drugs. In Nigeria, the National Health Insurance Scheme (NHIS) was introduced in 2005 to cater for the healthcare needs of the populace.9,10 Initially, the coverage of the NHIS was limited to workers in the formal sectors but has now been expanded to include people in the informal sector of the economy through community-based schemes.11 The scheme has a uniform coverage for all subscribers who pay only 10% of the total cost of medications as co-payment.12 In many hospitals in Nigeria, a dedicated outpatients' clinic has been created to attend only to patients registered under the NHIS. Prescription audits have been conducted in different settings in Nigeria among patients that “paid out of pocket” revealing various forms of nonrational use of medicines.13,14 A study conducted in the North-eastern part of Nigeria looked at the prescribing practice in an outpatients' clinic attending only to patients registered under the NHIS while another Nigerian study compared the prescribing practices in a military hospital before and postintroduction of the NHIS.15,16 To the knowledge of the authors, there is no study comparing the prescribing pattern in the general outpatient department of the hospital (where “out of pocket” payment is the norm) with that in the “NHIS” clinic concurrently. This type of comparison will enable us assess the impact of healthcare insurance on prescribing practices in this facility and may serve as a template for future interventions.
The main objective of this study was to compare concurrently the prescribing practices in the general outpatients' clinic (noninsured patients) and the NHIS clinic (patients with insurance coverage).
MATERIALS AND METHODS
This was a cross-sectional study conducted in the general outpatients' and the “NHIS” clinics of the Ekiti State University Teaching Hospital, Ado-Ekiti, South-western Nigeria. The medical records of patients, who attended these two clinics between the 1st of March and 30th June 2014 were retrieved and used for the study.
Study setting
The hospital is one of the two tertiary healthcare facilities in Ekiti State that provide medical care for its populace and that of the neighboring states. The hospital is well staffed with consultants in various fields of family medicine, internal medicine, surgery, obstetrics and gynecology, psychiatry, community medicine, and pediatrics. The general outpatients' department (also known as family medicine) is well staffed with its components of nursing staff, house officers, medical officers, registrars, and consultants. The general outpatients' clinic is usually the first point of contact for patients brought directly from home or referred from other healthcare facilities. This department is also responsible for running the “NHIS” clinic that attends to patients with insurance coverage. Patients aged 18 years and above are usually attended to at the general outpatients' clinic while the NHIS clinic offer services to both adult and children because of its peculiar nature.
Selection of cases
The attendance registers of both clinics were retrieved, and the medical records of 50 patients were selected monthly for the period of the study using a regular interval ratio. The information retrieved from the case notes included bio-demographic data, working diagnoses, a list of prescribed drugs, and their routes of administration. The following drug use indicators were assessed using the WHO guidelines on investigation of drug use in health care facilities:17 Average number of drugs per prescription, percentage of encounters with antibiotics, percentage of drugs prescribed by generic name, percentage of encounters with injections, and percentage of drugs prescribed from essential drug list. The National Essential Drug List of Nigeria (5th edition) was used to assess prescription of nationally relevant essential medicines.
Statistical analysis
Data collected were analyzed using Statistical Package for Social Sciences version 17 software (IBM Corporation, Armonk, NY, USA). Results are expressed as means, frequencies, and percentages. Comparison of means and frequencies was done using Student's t-test while Chi-square was used to determine the level of significance of groups of categorical variables with P < 0.05 considered as significant.
Ethical consideration
Ethical approval was obtained from the Hospital Research Ethics Committee before the starting the study.
RESULTS
Medical records (including copies of prescriptions) of 217 and 237 patients were selected from the general outpatients' and NHIS clinics, respectively. The distribution of patients according to sex is shown in Figure 1. Malaria was the most frequently diagnosed disease in the two clinics followed by diseases affecting the respiratory, cardiovascular, and gastrointestinal systems [Figure 2]. The mean age of patients attending the general outpatients' clinic was 45.0 ± 17.1 years while that of the NHIS clinic was 32.9 ± 16.1 years, a statistically significant difference (P< 0.0001). The average number of diagnoses was 1.57 ± 0.6 and 1.59 ± 0.75 in patients attending the NHIS and general outpatients' clinics, respectively (P = 0.75). The average number of prescribed drugs for patients attending the general outpatients' clinic was 3.9 ± 2.0 while that from the NHIS clinic was 4.1 ± 1.6 (P = 0.24).
Figure 1.
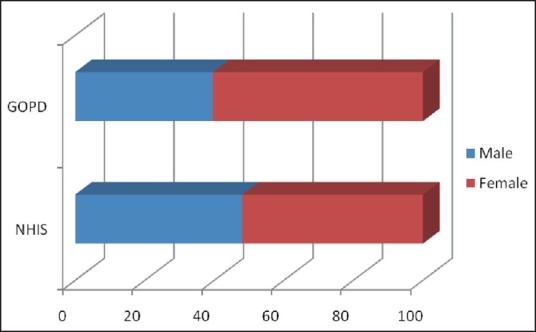
Distribution according to sex
Figure 2.
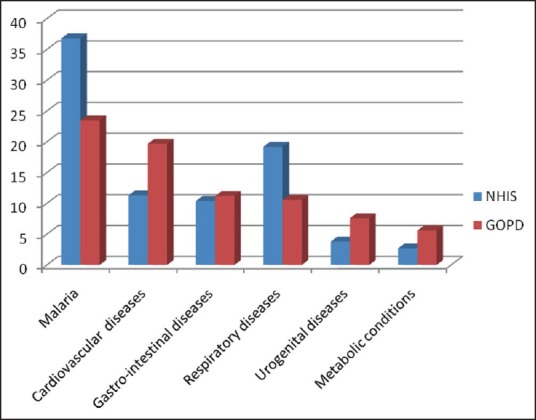
Comparison of diagnosed conditions
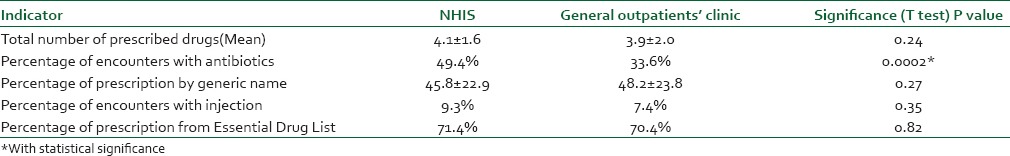
About a third of patients from both clinics had more than four medications prescribed. Figure 3 shows the grading of a number of prescribed drugs according to the number of prescribed drugs. The classes of drugs prescribed for patients from the two clinics are shown in Figure 4. Prescribing by generic names was done in 48.2 ± 23.8% and 45.8 ± 22.9% of prescriptions from the general outpatients' and NHIS clinic, respectively. A comparison of the difference between the two means did not show any statistically significant difference (P = 0.27). Percentage of encounters with antibiotics was 49.4% and 33.6% of patients who attended the NHIS and general outpatients' clinics, respectively. Percentage of encounters with injections was 9.3% and 7.4% of patients from the NHIS and general outpatients' clinics, respectively.
Figure 3.
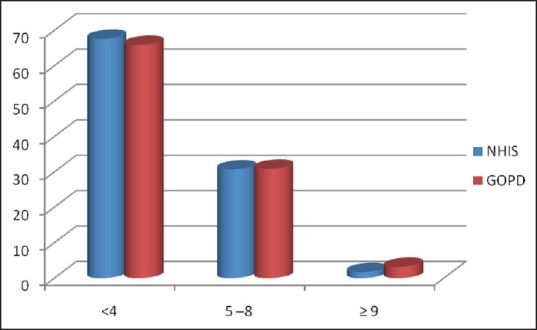
Classification according to number of prescribed drugs
Figure 4.
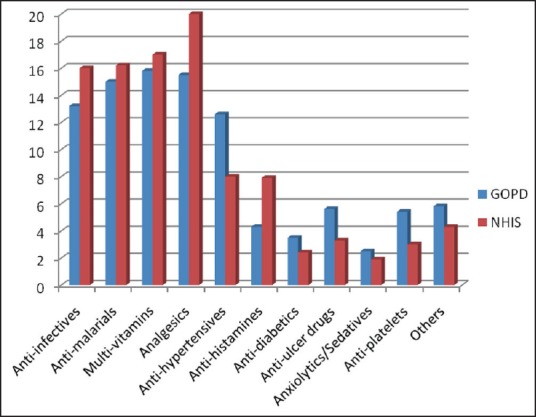
Classes of prescribed drugs
Prescribing from the Nigerian national essential drug list was done in 70.4% and 71.4% of all cases from the general outpatients' and NHIS clinics, respectively. Table 1 summarizes the comparison between the two groups of patients.
Table 1.
Comparison of the WHO core prescribing indicators between the two groups of patients
DISCUSSION
The prescribing pattern in the two clinics was not significantly different in this study. The lower mean age of patients from the NHIS clinic is due to the fact that both adult and pediatric patients are attended to in the NHIS clinic whereas only adult patients are seen in the general outpatients' clinic. The mean number of prescribed drugs found in the general outpatients' and NHIS clinic 3.9 and 4.1, respectively. A comparison of drug prescribing practices during a pre- and post-insurance era in a Nigerian hospital found the mean prescribed drugs to be 3.0 and 2.6, respectively.16 Okoro and Shekariin a study conducted in the NHIS clinic of a tertiary healthcare facility in the North-east Nigeria recorded a mean number of prescribed drugs to be 3.4.15 Results from similar general prescription audits conducted in Nigeria showed average number of prescribed drugs between 3.0 and 4.0.13,18,19 The difference between the observed values may be due to the status of healthcare facilities where these studies were carried out; some of the studies were conducted in secondary level healthcare facilities. In a Chinese study comparing drug prescribing practices among two groups of patients (with and without community health insurance), the mean number of prescribed drugs observed was 4.6 and 3.1, respectively.20
Polypharmacy has several definitions, but that which defines it as the prescription of more than four medications is the most commonly used.21,22 Polypharmacy has serious implications on the health and financial state of patients as it may lead to the occurrence of adverse drug reactions and increased healthcare costs.23,24 The proportion of patients who had more than four drugs prescribed in this study was 32.4% and 34.1% in the NHIS and GOPD clinics, respectively. This is more than 16.7% and 15.6% observed during the pre- and post-insurance era in a Nigerian military hospital.16 Our hospital evolved from a secondary health care center to tertiary care center less than a decade ago as most doctors are yet to adapt to the new modalities of patients' care. More so, the same group of doctors from the general outpatients' department also attends to patients in both clinics.
Nonrational prescription and use of antibiotics have been associated with increased antimicrobial resistance and healthcare expenditure.25,26 The likelihood of having an antibiotic prescribed was higher among patients who were seen at the NHIS clinic (49.4% vs. 33.6%). Okoro and Shekari in a study conducted at a health insurance clinic in the North-eastern part of Nigeria found that 56.2% of all encounters had antibiotics prescribed. The percentage of encounters with antibiotics was comparable to other studies conducted in regular outpatients' clinics in other parts of Nigeria; 34.4% and 35% in studies conducted in the Kano, North-west Nigeria and Lagos, South-west, respectively.16,19 Sun et al. also found a higher number of encounters with prescribed antibiotics (72.4%) in patients who had community health insurance when compared to those without (59.3%).20 This relatively high rate of antibiotic prescription in patients from the NHIS clinic may be due to patients' demand for the drugs and the fact that only 10% of the medication fees are paid as co-payment.
The low rate of injections among the two groups of patients is in keeping with recent trends; the percentage of encounters with injection use in an earlier cited Nigerian study fell from 23.9% (2009) to 8.9% (2012).16 The relatively high prevalence level of diseases such as hepatitis B and HIV infection among the populace has re-enforced the need for safe injection practices among healthcare practitioners in Nigeria.
Prescribing by generic name has been identified as a way of reducing health care costs and makes it more cost-effective.27,28 Prescribing by generic name was done in 48.2% and 45.8% of prescriptions from the general outpatients' and NHIS clinic respectively; slightly higher than 42.7% and 43.8% found in earlier Nigerian studies.18,19 However, our values are lower than the 51.5% found in an NHIS clinic in Northern Nigeria and 96.1% recorded in a study conducted in China.15,29 The concept of essential medicines was introduced to help streamline the number of drugs deployed within the healthcare system in order to improve rational prescribing and reducing healthcare costs. In this study, 70.4% and 71.4% of all prescribed medications in the general outpatients' clinic and NHIS clinic were from the Nigerian National Essential Drug List. This is close to 67.1% reported in a health insurance clinic of a teaching hospital in the North-east Nigeria.15
CONCLUSION
The prescribing practice of physicians is affected to some extent by the health insurance status of their patients as has been shown in this study. There was a trend to having more medicines prescribed and more encounters with antibiotics among patients enrolled with the health insurance scheme. There is a need for additional training on the rational use of medicines for all prescribers and especially those attending to this category of patients.
Implications for clinical practice and policy
The result of this study has clearly shown a trend toward more polypharmacy in patients registered under the NHIS in Nigeria. This serves as an early warning indicator of nonrational prescribing which could negate the expected economic benefits of the scheme and expose patients to the adverse effects of polypharmacy. Early interventions by the health authorities to correct this trend through training and retraining of prescribers, also, prescribing by generic name for patients under the health insurance scheme should be encouraged as this will help in achieving the economic objectives of the NHIS.
Study limitations
This study may have issues with the accuracy of data since we used the past medical records of patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We are grateful to the staff of medical records of the hospital for their assistance in retrieving the patients' records.
REFERENCES
- 1.Chen CL, Chen L, Yang WC. The influences of Taiwan's generic grouping price policy on drug prices and expenditures: Evidence from analysing the consumption of the three most-used classes of cardiovascular drugs. BMC Public Health. 2008;8:118. doi: 10.1186/1471-2458-8-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ess SM, Schneeweiss S, Szucs TD. European healthcare policies for controlling drug expenditure. Pharmacoeconomics. 2003;21:89–103. doi: 10.2165/00019053-200321020-00002. [DOI] [PubMed] [Google Scholar]
- 3.Barry M, Tilson L, Ryan M. Pricing and reimbursement of drugs in Ireland. Eur J Health Econ. 2004;5:190–4. doi: 10.1007/s10198-004-0225-6. [DOI] [PubMed] [Google Scholar]
- 4.Sax P. Spending on medicines in Israel in an international context. Isr Med Assoc J. 2005;7:286–91. [PubMed] [Google Scholar]
- 5.Odeyemi IA, Nixon J. Assessing equity in health care through the National Health Insurance Schemes of Nigeria and Ghana: A review-based comparative analysis. Int J Equity Health. 2013;12:9. doi: 10.1186/1475-9276-12-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oyibo PG. Out-of-pocket payment for health services: Constraints and implications for government employees in Abakaliki, Ebonyi State, South east Nigeria. Afr Health Sci. 2011;11:481–5. [PMC free article] [PubMed] [Google Scholar]
- 7.Atun R, Aydin S, Chakraborty S, Sümer S, Aran M, Gürol I, et al. Universal health coverage in Turkey: Enhancement of equity. Lancet. 2013;382:65–99. doi: 10.1016/S0140-6736(13)61051-X. [DOI] [PubMed] [Google Scholar]
- 8.Rajmil L, Fernández de Sanmamed MJ. Universal health-care coverage in Europe. Lancet. 2012;380:1644. doi: 10.1016/S0140-6736(12)61942-4. [DOI] [PubMed] [Google Scholar]
- 9.National Health Insurance Scheme Decree No 35 of 1999. Laws of the Federation of Nigeria. [Last accessed on 2015 Mar 5]. Available from: http://www.law.org/National%20Health%20Insurance%20Scheme%20Decree.htm .
- 10.Onoka CA, Hanson K, Hanefeld J. Towards universal coverage: A policy analysis of the development of the National Health Insurance Scheme in Nigeria. Health Policy Plan. 2014 doi: 10.1093/heapol/czu116. pii: czu116. [DOI] [PubMed] [Google Scholar]
- 11.Odeyemi IA. Community-based health insurance programmes and the National Health Insurance Scheme of Nigeria: Challenges to uptake and integration. Int J Equity Health. 2014;13:20. doi: 10.1186/1475-9276-13-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.NHIS. Operational Guidelines. Abuja: National Health Insurance Scheme; 2005. [Google Scholar]
- 13.Akande TM, Ologe MO. Prescription pattern at a secondary health care facility in Ilorin, Nigeria. Ann Afr Med. 2007;6:186–9. doi: 10.4103/1596-3519.55699. [DOI] [PubMed] [Google Scholar]
- 14.Etuk EU, Egua MA, Muhammad AA. Prescription pattern of antimalarial drugs in children below 5 years in a tertiary health institution in Nigeria. Ann Afr Med. 2008;7:24–8. doi: 10.4103/1596-3519.55688. [DOI] [PubMed] [Google Scholar]
- 15.Okoro RN, Shekari BG. Physicians' drug prescribing patterns at the National Health Insurance Scheme unit of a teaching hospital in the North Eastern Nigeria. Arch Pharm Pract. 2013;4:3. [Google Scholar]
- 16.Adebayo ET, Hussain NA, Ajanaku VS. Influence of health insurance on rational use of drugs. TAF Prev Med Bull. 2013;12:511–8. [Google Scholar]
- 17.World Health Organization. (WHO/DAP/93.1) Geneva: WHO; 1993b. How to Investigate Drug Use in Health Facilities. Selected Drug Use Indicators. [Google Scholar]
- 18.Adebayo ET, Hussain NA. A baseline study of drug prescribing practices in a Nigerian military hospital. Niger J Clin Pract. 2009;12:268–72. [PubMed] [Google Scholar]
- 19.Tamuno I, Fadare JO. Drug prescription pattern in a Nigerian tertiary hospital. Trop J Pharm Res. 2012;11:146–52. [Google Scholar]
- 20.Sun X, Jackson S, Carmichael GA, Sleigh AC. Prescribing behaviour of village doctors under China's New Cooperative Medical Scheme. Soc Sci Med. 2009;68:1775–9. doi: 10.1016/j.socscimed.2009.02.043. [DOI] [PubMed] [Google Scholar]
- 21.Gnjidic D, Hilmer SN, Blyth FM, Naganathan V, Waite L, Seibel MJ, et al. Polypharmacy cutoff and outcomes: Five or more medicines were used to identify community-dwelling older men at risk of different adverse outcomes. J Clin Epidemiol. 2012;65:989–95. doi: 10.1016/j.jclinepi.2012.02.018. [DOI] [PubMed] [Google Scholar]
- 22.Kuijpers MA, van Marum RJ, Egberts AC, Jansen PA. OLDY (OLd people Drugs & dYsregulations) Study Group. Relationship between polypharmacy and underprescribing. Br J Clin Pharmacol. 2008;65:130–3. doi: 10.1111/j.1365-2125.2007.02961.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Köberlein J, Gottschall M, Czarnecki K, Thomas A, Bergmann A, Voigt K. General practitioners' views on polypharmacy and its consequences for patient health care. BMC Fam Pract. 2013;14:119. doi: 10.1186/1471-2296-14-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Salazar JA, Poon I, Nair M. Clinical consequences of polypharmacy in elderly: Expect the unexpected, think the unthinkable. Expert Opin Drug Saf. 2007;6:695–704. doi: 10.1517/14740338.6.6.695. [DOI] [PubMed] [Google Scholar]
- 25.Llor C, Bjerrum L. Antimicrobial resistance: Risk associated with antibiotic overuse and initiatives to reduce the problem. Ther Adv Drug Saf. 2014;5:229–41. doi: 10.1177/2042098614554919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nguyen KV, Thi Do NT, Chandna A, Nguyen TV, Pham CV, Doan PM, et al. Antibiotic use and resistance in emerging economies: A situation analysis for Viet Nam. BMC Public Health. 2013;13:1158. doi: 10.1186/1471-2458-13-1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.King DR, Kanavos P. Encouraging the use of generic medicines: Implications for transition economies. Croat Med J. 2002;43:462–9. [PubMed] [Google Scholar]
- 28.Puig-Junoy J. Impact of European pharmaceutical price regulation on generic price competition: A review. Pharmacoeconomics. 2010;28:649–63. doi: 10.2165/11535360-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 29.Wang H, Li N, Zhu H, Xu S, Lu H, Feng Z. Prescription pattern and its influencing factors in Chinese county hospitals: A retrospective cross-sectional study. PLoS One. 2013;8:e63225. doi: 10.1371/journal.pone.0063225. [DOI] [PMC free article] [PubMed] [Google Scholar]


