Abstract
Purpose
With the increasing prevalence of orthodontic treatment in adults, clear aligner treatments are becoming more popular. The aim of this study was to evaluate the effect of orthodontic treatment on periodontal tissue and to compare orthodontic treatment with fixed appliances (FA) to clear aligner treatment (CAT) in periodontitis patients.
Methods
A total of 35 patients who underwent orthodontic treatment in the Department of Periodontology were included in this study. After periodontal treatment with meticulous oral hygiene education, patients underwent treatment with FA or CAT, and this study analyzed patient outcomes depending on the treatment strategy. Clinical parameters were assessed at baseline and after orthodontic treatment, and the duration of treatment was compared between these two groups.
Results
The overall plaque index, the gingival index, and probing depth improved after orthodontic treatment (P<0.01). The overall bone level also improved (P=0.045). However, the bone level changes in the FA and CAT groups were not significantly different. Significant differences were found between the FA and CAT groups in probing depth, change in probing depth, and duration of treatment (P<0.05). However, no significant differences were found between the FA and CAT groups regarding the plaque index, changes in the plaque index, the gingival index, changes in the gingival index, or changes in the alveolar bone level. The percentage of females in the CAT group (88%) was significantly greater than in the FA group (37%) (P<0.01).
Conclusions
After orthodontic treatment, clinical parameters were improved in the FA and CAT groups with meticulous oral hygiene education and plaque control. Regarding plaque index and gingival index, no significant differences were found between these two groups. We suggest that combined periodontal and orthodontic treatment can improve patients’ periodontal health irrespective of orthodontic techniques.
Keywords: Bone regeneration, Malocclusion, Orthodontics, Periodontitis
Graphical Abstract
INTRODUCTION
Over the past few decades, orthodontic treatment in adults has become more common. The most common orthodontic problems found in periodontally compromised patients include proclination of the maxillary anterior teeth, irregular interdental spacing, rotation, overeruption, migration, loss of teeth, and traumatic occlusion [1].
However, several challenges are associated with the orthodontic treatment of periodontally compromised patients. First, the orthodontic force applied to achieve movement of teeth may aggravate periodontitis in patients with poor oral hygiene. Moreover, fixed appliances and wires make plaque control difficult. Orthodontic treatment is sometimes considered a predisposing factor for periodontal disease, as fixed orthodontic appliances with wire may inhibit plaque control, resulting in increased bacterial aggregation [2]. Second, a fixed appliance is not always aesthetically pleasing for adults, so prothodontic rather than orthodontic treatments are often used. However, orthodontic tooth movement may provide a substantial benefit in periodontal therapy. For example, anterior crowding may prevent patients from properly cleaning proximal tooth surfaces. The correction of these malpositioned teeth permits better access for oral hygiene and can improve the morphology of marginal soft and hard tissues. Combined periodontal and orthodontic treatment has been shown to improve periodontal health and to re-establish well-functioning dentition [3,4]. After proper periodontal therapy, orthodontic treatment can improve both the alveolar bone and soft periodontal tissues [5]. Several studies have shown that patients with reduced but healthy periodontium can undergo orthodontic treatment without aggravating their periodontal conditions under adequate plaque control [3,6,7,8]. One 12-year long-term study showed that orthodontic treatment was no longer contraindicated in adults with severe periodontitis, and suggested that orthodontic treatment actually improved the likelihood of saving and restoring deteriorating dentition [8]. According to a recent systematic review, no clinically significant irreversible periodontal tissue destruction results from the placement of an orthodontic appliance [9].
However, clinical and experimental studies have shown that when inflammation is not fully controlled, orthodontic treatment may trigger the inflammatory process and accelerate the progression of periodontal destruction, leading to further loss of attachment, even in patients with sound oral hygiene [6,10]. Additionally, a recent study showed that orthodontic movement acts synergistically with periodontal disease in periodontal breakdown through upregulation of proinflammatory cytokines [11]. Some contradictory findings regarding the effects of orthodontic appliances on periodontal health are partially due to the heterogeneity of materials and differences in the research methods employed [12]. Several factors may affect the outcomes of studies, such as differences in the types of orthodontic movement, including movement of teeth with infrabony defects, extrusion, intrusion, molar uprighting, movement in edentulous areas, proclination, and the periodontal treatment schedule [1].
Removable clear aligner therapy has recently been introduced into adult orthodontics, and has been found to have several advantages, including improved aesthetic outcomes [13,14,15]. Its main components are clear plastic splints that cover all of the teeth and the marginal aspects of the gingiva and gradually move the teeth into an ideal position. It has been reported that periodontal health is not jeopardized by this treatment, although the clear aligners cover the teeth and partially cover the keratinized gingiva [13]. It has been suggested that this can be attributed to the fact that the aligners are removable, and thus do not impede oral hygiene [14]. However, most studies on clear aligner therapy were performed in young patients with normal periodontium [16,17,18].
The aim of this study was to evaluate the effect of orthodontic treatment on periodontal tissue and to compare the effects of orthodontic treatment with fixed appliances and clear aligner therapy on the clinical parameters of patients with periodontitis.
MATERIALS AND METHODS
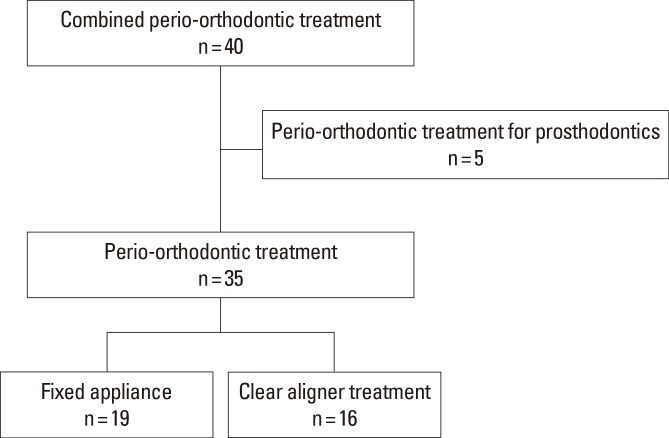
A total of 40 patients (16 men and 24 women) who underwent orthodontic treatment in the Department of Periodontology, Hanyang University College of Medicine between March 2005 and August 2014 were screened for enrollment in this study. Five patients who underwent orthodontic treatment to place implants or prosthodontic treatments in the posterior area were excluded (Figure 1).
Figure 1.
Diagram showing the flow of patients for screening.
Thirty-five patients (14 men and 21 women) with a mean age of 52.97 years (range, 35–74) were included in this study. The study sample was derived from a population of patients who underwent orthodontic treatment in the Department of Periodontology after periodontal treatment. The inclusion criteria were patients with chronic periodontitis who had >2 mm of attachment loss and a probing pocket depth >3 mm [19]. All patients were in good general health with no signs or symptoms of systemic disease. They were all non-smokers, with the exception of one patient. The other exclusion criteria were active infection, the presence of diseases affecting bone metabolism or wound healing, a history of head or neck radiation therapy, the regular use of steroids or other medications affecting bone turnover, and pregnancy. The study protocol was approved by our institutional review board (IRB 2014-11-026-001).
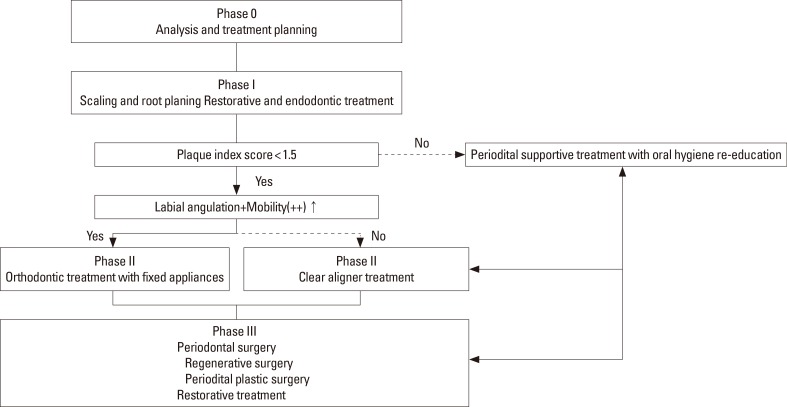
All patients demonstrated minor incisor malalignment or pathologic tooth movement in the maxillary or mandibular incisors without evidence of posterior bite collapse. From the stage of treatment planning, all cases were discussed with an orthodontist at the Department of Orthodontics with careful consideration given to the patients’ primary needs. For the diagnostic setup, the study casts were duplicated and the malaligned or pathologically migrated teeth were carefully cut from the model. The teeth were then waxed back onto the model in an ideal position. After scaling and root planing as well as continuous education regarding mechanical supragingival plaque control, each patient was re-evaluated. If the patient’s oral hygiene was poor (plaque index >1.5), education on oral hygiene and periodontal treatment were repeated prior to orthodontic treatment. After completion of the initial periodontal therapy, minor tooth movement was carried out for the anterior teeth. With the exception of patients who had to choose fixed appliances due to lager labial inclinations or mobile anterior teeth the types of orthodontic appliances were assigned according to patient preference after detailed explanations about the advantages and disadvantages of the two techniques.
Clinical parameters
In order to assess the safety and effectiveness of clear aligners in comparison to a fixed appliances, clinical parameters were recorded before and after orthodontic treatment. The measurements included: (1) Plaque index [20], assessed at four sites (mesiobuccal, mid-buccal, distobuccal, and lingual); (2) Gingival index [21], assessed at four sites (mesiobuccal, mid-buccal, distobuccal, and lingual); (3) the probing depth, measured at six sites (mesiobuccal, mid-buccal, distobuccal, mesiolingual, mid-lingual, and distolingual) and rounded to the nearest millimeter following probing with a pressure of approximately 0.25 N; and (4) the duration of treatment, defined as the time from direct bonding of brackets on the teeth to when the resin-wire splint was bonded on the palatal or lingual side of teeth for retainers in the orthodontic treatments with fixed appliances (FA) group. In the clear aligner treatment (CAT) group, the duration of treatment was defined as the time from the first aligner delivery to the time of retainer bonding to the teeth. The severity of irregularities was classified from grade 5 to grade 0 according to the amount of malalignment or the degree of pathologic migration.
Orthodontic treatment with fixed appliances
Initial records including intraoral photographs and intraoral radiographs were collected before orthodontic procedures (Figure 2A and C). For minor tooth movement, brackets were bonded from canine to canine in the maxilla or the mandible. The first arch wire placed was a 16-mm A-NiTi round wire for leveling. In cases of crowed anterior teeth, progressive interproximal stripping was performed with topical fluoride application to prevent proximal caries within the limits of enamel thickness. When the preliminary alignment had been completed and the wire had passively engaged the brackets, a stiffer round wire was placed at three-week intervals. An auxiliary spring or power chain was also used for space control. After correction of the malalignment, an impression for a retainer was taken. All patients received a resin-wire splint for a retainer (Figure 2B and D).
Figure 2.
Orthodontic treatment with fixed appliances. (A) Intraoral photograph before orthodontic treatment. (B) Intraoral photograph after orthodontic treatment. (C) Periapical radiograph before orthodontic treatment. (D) Periapical radiograph after orthodontic treatment.
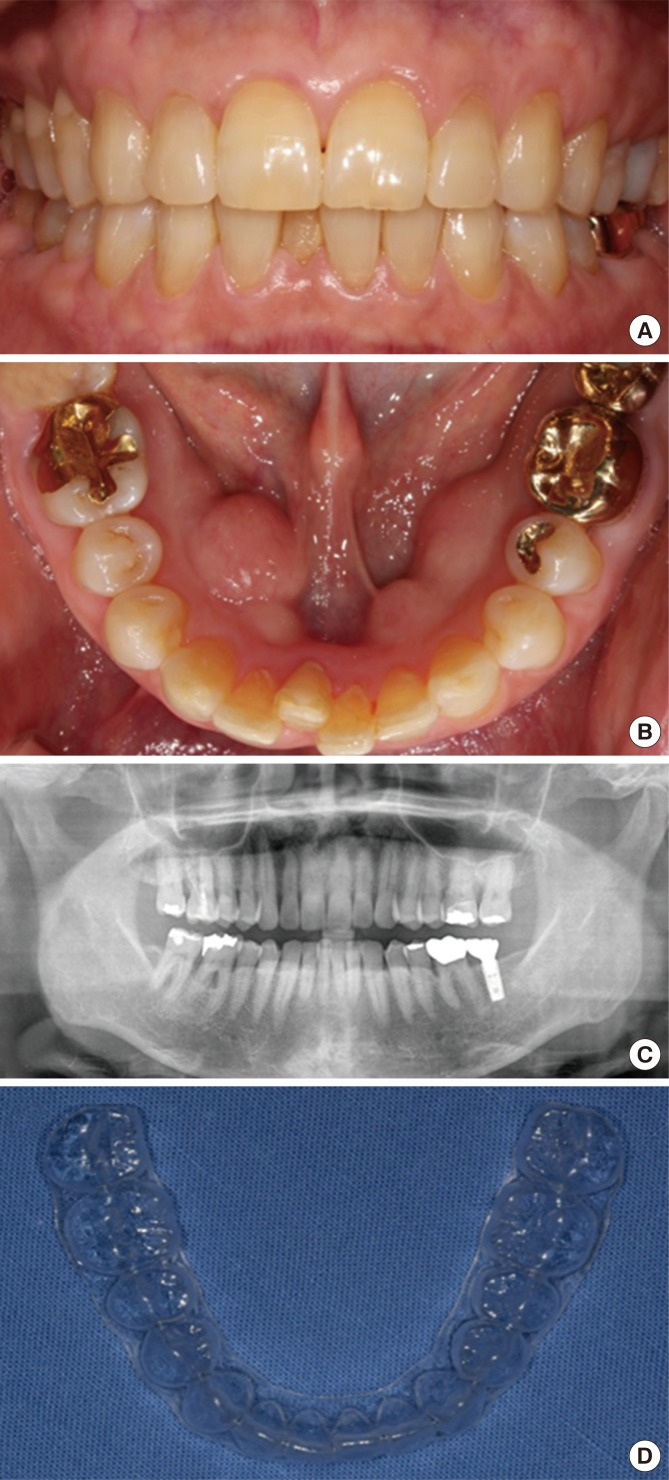
Clear aligner treatment
Initial records were collected, including polyvinyl siloxane impressions, intraoral photographs, and intraoral radiographs (Figure 3). At the following visit, the first aligner was delivered with detailed instructions to wear it full-time except while eating, drinking, and brushing. All patients were asked to change aligners every two weeks (Figure 3D) [17]. At each subsequent visit, professional teeth cleaning was performed with re-education on oral hygiene if needed. In cases of crowding, interproximal stripping was performed in the same manner. After the orthodontic treatment, impressions for a retainer were taken. The resin-wire splint was bonded on the palatal or lingual side in order to retain well-aligned teeth (Figure 4).
Figure 3.
Clear aligner treatment. (A) Frontal and (B) occlusal intraoral photograph before clear aligner treatment. (C) Panoramic radiograph before orthodontic treatment. (D) The clear plastic splints that cover all of the teeth and the marginal aspects of the gingiva and gradually move the teeth into an ideal position.
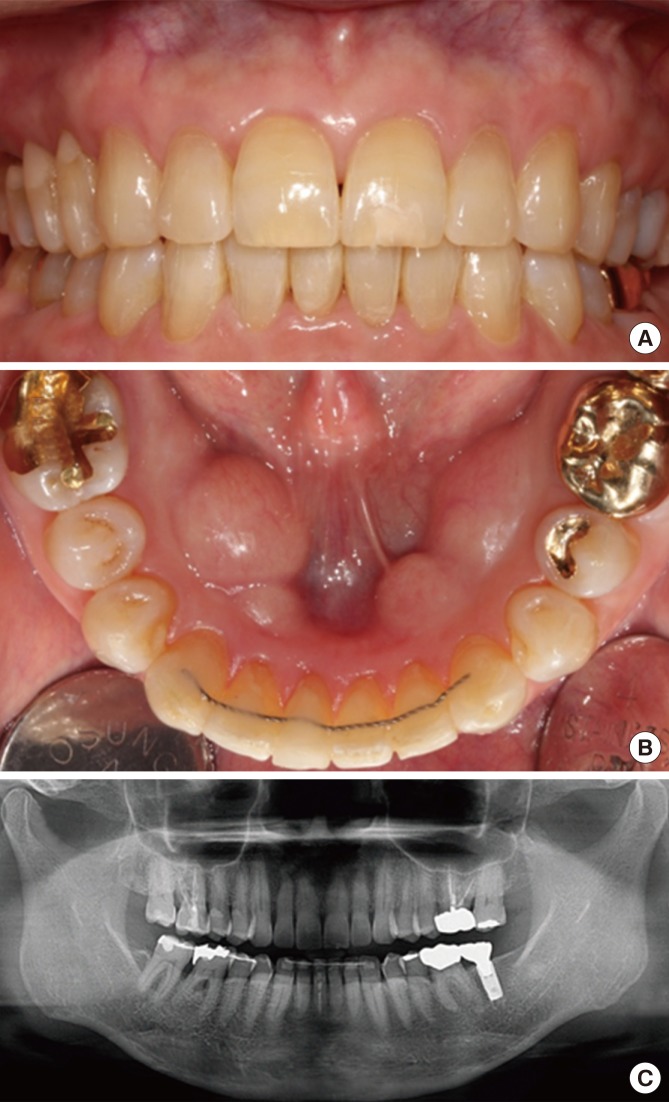
Figure 4.
Clear aligner treatment. (A) Frontal and (B) occlusal intraoral photograph after clear aligner treatment. (C) Panoramic radiograph after orthodontic treatment.
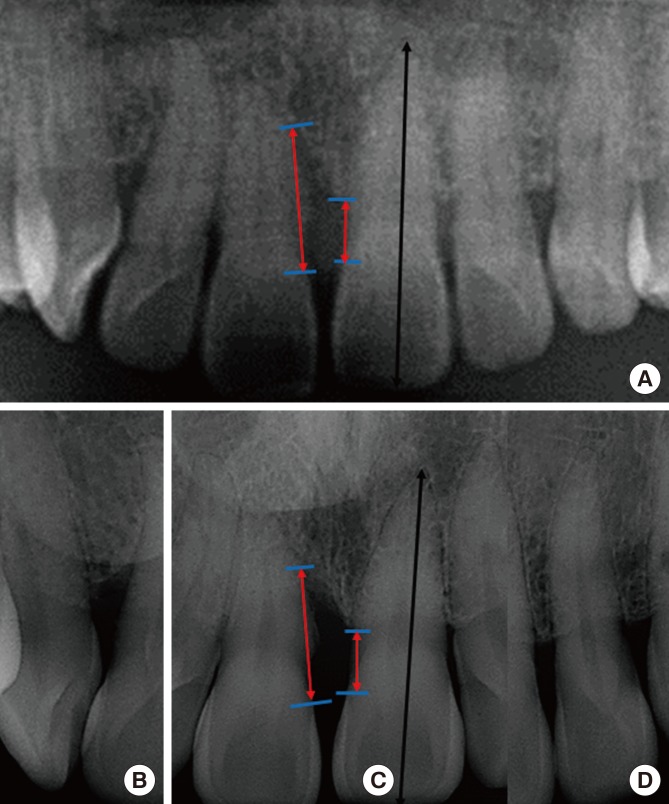
Radiographic measurements to assess alveolar bone levels
The alveolar crestal bone level was evaluated at the mesial and distal sites of all teeth before and after orthodontic treatment. Preoperative and postoperative panoramic radiographs were used to evaluate the exact bone level, which was reconfirmed with additional periapical radiographs (Figure 5) [22]. Panoramic and periapical radiographs were imported into Analysis Toolkit (Adobe Photoshop CS6, Adobe Systems Inc., San Jose, CA, USA). Two blinded examiners measured the distances between the cemento-enamal junction and the most coronal level of the alveolar bone for all sets of radiographs twice. The measurements were repeated with a time interval of at least two weeks between assessments. The mean of the four measurements was used as the alveolar bone level. If the difference in measurements between the two examiners was greater than 0.1 mm, they jointly reanalyzed the alveolar bone level to reach a consensus.
Figure 5.
(A) Preoperative and postoperative panoramic radiographs were used to evaluate the exact bone level, which was reconfirmed with (B-D) additional periapical radiographs.
Interexaminer reliability
All clinical parameters were examined by one periodontist. Radiographic measurements were performed by two blinded examiners. All radiographic measurements were repeated after an interval of at least two weeks. Bland-Altman plots and intraclass correlation coefficients were used to evaluate the reproducibility of the alveolar bone level measurements.
Statistical analysis
Statistical analysis was performed using a commercially available software program (SPSS version 21.0, IBM Corp., Armonk, NY, USA). Thirteen patients in each group were required to achieve a power of 80% for the primary endpoint. Metric variables (e.g., age) were reported as means with standard deviations (SD). The Kolmogorov-Smirnov one-sample tests were performed to assess whether the data were normally distributed. The Wilcoxon signed-rank test was used to evaluate the changes in clinical parameters after orthodontic treatment. The chi-square test was used to evaluate the relationship between the male-to-female ratio and the orthodontic technique used, as well as the relationship between the male-to-female ratio and differences in sites. Comparisons between orthodontic treatment with a fixed appliance and clear aligner treatment were evaluated using the Mann-Whitney U tests. The correlations among clinical parameters were identified using Spearman correlation coefficients. The level of significance chosen for all statistical tests was P<0.05.
RESULTS
The demographic information of patients is presented in Table 1. The mean age of the 35 patients included was 52.97±9.42 years (range, 35–74 years) at the start of orthodontic treatment. A total of 21 patients (60%) were female. Seven patients (37%) in the FA group were female, compared to 14 patients (88%) in the CAT group (Table 2). The gender ratio was significantly different in the FA and CAT groups (P<0.01). Twenty-two patients (63%) underwent treatment of the mandible. In both groups, orthodontic treatment was performed more frequently on the mandible than the maxilla. Eleven patients (58%) in the FA group and 11 patients (69%) in the CAT group underwent treatment of the mandible.
Table 1. Demographic and clinical data of the patients.
| Patients | Variable | N |
|---|---|---|
| Age (Years) | Minimum age | 35 |
| Maximum age | 74 | |
| (Mean±SD) | (52.97±9.42) | |
| Gender | Male | 14 |
| Female | 21 | |
| Sites | Maxilla | 13 |
| Mandible | 22 | |
| Smoking | Non-smoker | 34 |
| Smoker | 1 | |
| Type of irregularity | Crowding | 21 |
| Spacing | 4 | |
| Pathologic migration | 10 | |
| Severity of irregularity | Grade 1 | 0 |
| Grade 2 | 4 | |
| Grade 3 | 13 | |
| Grade 4 | 13 | |
| Grade 5 | 5 | |
| Type of technique | Fixed appliances | 19 |
| Clear aligner treatment | 16 | |
| Type of chronic periodontitis | Generalized slight | 2 |
| Generalized moderate | 21 | |
| Generalized severe | 12 | |
| Regenerative surgery | No | 22 |
| Pre-orthodontic surgery | 5 | |
| Post-orthodontic surgery | 8 | |
| Total | 35 |
SD: standard deviation, N: number of patients, Generalized slight: 1 to 2 mm of clinical attachment loss, Generalized moderate: 3 to 4 mm of clinical attachment loss, Generalized severe: >5 mm of clinical attachment loss.
Table 2. Comparison between orthodontic treatment with fixed appliances and clear aligner treatment (n=35).
| Clinical parameters | Total | FA | CAT | P-value |
|---|---|---|---|---|
| Number of patients | 35 | 19 | 16 | |
| Age (years) | 52.97±9.42 | 51.78±7.44 | 54.38±11.45 | NS |
| Male/Female (Female%) | 14/21 (60%) | 12/7 (37%) | 2/14 (88%) | 0.002 |
| Mx/Mn (Mn%) | 13/22 (63%) | 8/11 (58%) | 5/11 (69%) | NS |
| Change in Plaque index | 0.28±0.27 | 0.38±0.28 | 0.16±0.22 | NS |
| Baseline | 1.34±0.36 | 1.41±0.36 | 1.26±0.36 | NS |
| Post-treatment | 1.03±0.32 | 1.02±0.29 | 1.04±0.37 | NS |
| Change in gingival index | 0.08±0.06 | 0.08±0.06 | 0.10±0.06 | NS |
| Baseline | 0.56±0.11 | 0.59±0.13 | 0.52±0.06 | NS |
| Post-treatment | 0.48±0.12 | 0.52±0.14 | 0.43±0.06 | NS |
| Change in Probing depth | 0.35±0.34 | 0.48±0.34 | 0.20±0.29 | 0.008 |
| Baseline | 2.58±0.78 | 3.01±0.77 | 2.08±0.43 | 0.001 |
| Post-treatment | 2.23±0.72 | 2.53±0.78 | 1.88±0.44 | 0.005 |
| Change in Bone level | 0.39±0.62 | 0.54±0.69 | 0.22±0.49 | NS |
| Baseline | 3.53±1.26 | 4.02±1.48 | 2.94±0.56 | 0.015 |
| Post-treatment | 3.13±0.95 | 3.48±1.10 | 2.72±0.51 | 0.018 |
| Duration of treatment (months) | 5.01±2.20 | 4.16±1.71 | 6.03±2.34 | 0.017 |
FA: orthodontic treatment with fixed appliances, CAT: clear aligner treatment, Mx: maxilla, Mn: mandible,
NS: statistically not significant.
Comparison between orthodontic treatments with fixed appliances versus clear aligners
The overall plaque index scores were 1.34±0.36 and 1.03±0.32 at baseline and after orthodontic treatment, respectively (Table 2). A statistically significant difference was found between baseline and after orthodontic treatment (P<0.01) (Figure 6). Overall, the change in the plaque index was 0.28±0.27. The change in plaque index scores in the FA group (0.38±0.28) was greater than in the CAT group (0.16±0.22), although this difference was not statistically significant.
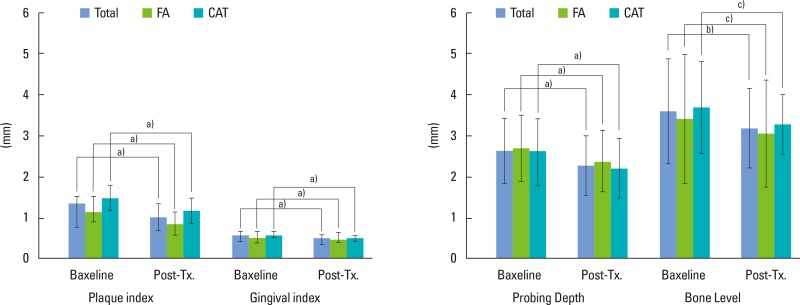
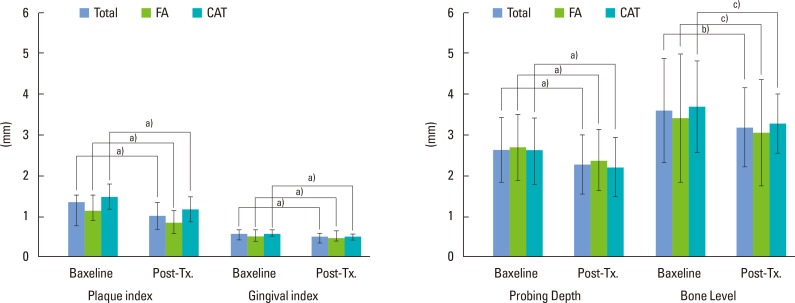
Figure 6.
Changes in clinical parameters. The plaque index and gingival index scores were improved after orthodontic treatment (a) P<0.01). The probing depth decreased after orthodontic treatment (a) P<0.01). The overall bone level changes showed significant differences between baseline and after orthodontic treatment (b)P=0.045). However, the bone level changes in the FA and CAT groups did not show any significant differences after orthodontic treatment (c)P>0.05). FA: fixed appliance, CAT: clear aligner treatment.
The overall gingival index scores improved from 0.56±0.11 at baseline to 0.48±0.12 after orthodontic treatment (P<0.01) (Figure 6). After orthodontic treatment, the gingival index score in the FA group (0.59±0.13) was higher than in the CAT group (0.52±0.06), although this difference was not statistically significant differences.
The overall probing depths decreased from 2.58±0.78 mm to 2.23±0.72 mm after orthodontic treatment (P<0.01) (Figure 6). The probing depth of the FA group was 3.01±0.77 mm and 2.53±0.78 mm at baseline and after treatment, respectively, while the probing depth of the CAT group was 2.08±0.43 mm and 1.88±0.44 mm at baseline and after treatment, respectively. A statistically significant difference was found between the FA and CAT groups with regard to the change in probing depth (0.48±0.34 mm vs. 0.20±0.29 mm; P<0.01).
The overall alveolar bone level was improved (Figure 6). However, the bone level changes in the FA and CAT groups after orthodontic treatment were not significantly different. In the FA group, the alveolar bone level was 4.02±1.48 mm and 3.48±1.10 mm at baseline and after orthodontic treatment, respectively. No statistically significant difference was found in the change of alveolar bone level between the FA group (0.54±0.69 mm) and the CAT group (0.22±0.49 mm).
The total duration of orthodontic treatment was 5.01±2.20 months. The treatment duration of the FA group (4.16±1.71 months) was shorter than that of the CAT group (6.03±2.34 months) (P<0.05).
Comparison between the maxilla and the mandible treatment groups
Orthodontic treatment was more frequently performed on the mandible (n=22) than the maxilla (n=13) (Table 3). The mean age of patients who had orthodontic treatments on the mandible was 55.5±9.86 years. Patients who underwent orthodontic treatment on the mandible were significantly older than those who underwent orthodontic treatment on the maxilla (P<0.05). In the mandible group, 14 of 22 patients (64%) were female, while seven of 13 patients (54%) were female in the maxilla group. However, there was no significant difference in the percentage of patients who underwent CAT treatment between these groups. The plaque index scores in the mandible group were higher than those in the maxilla group at baseline (P=0.013) and after orthodontic treatment (P=0.003). Nonetheless, no statistically significant differences were observed between these two groups with regard to changes in the plaque index. The gingival index scores of the maxilla and the mandible groups did not show any significant differences at baseline or after orthodontic treatment. Likewise, no significant differences were found between these two groups in the change of the gingival index, probing depth, alveolar bone level change, and the duration of treatment.
Table 3. Comparison between the maxilla and the mandible treatment groups (n=35).
| Clinical Parameters | Total | Maxilla | Mandible | P-value |
|---|---|---|---|---|
| Number of patients | 35 | 13 | 22 | |
| Age (years) | 52.97±9.42 | 48.69±7.05 | 55.5±9.86 | 0.026 |
| Male/Female (Female%) | 14/21 (60%) | 6/7 (54%) | 8/14 (64%) | NS |
| FA/CAT (CAT%) | 19/16 (46%) | 8/5 (38%) | 11/11 (50%) | NS |
| Change in plaque index | 0.28±0.27 | 0.29±0.26 | 0.28±0.29 | NS |
| Baseline | 1.34±0.36 | 1.12±0.36 | 1.47±0.30 | 0.013 |
| Post-treatment | 1.03±0.32 | 0.83±0.26 | 1.15±0.30 | 0.003 |
| Change in gingival index | 0.08±0.06 | 0.08±0.07 | 0.09±0.05 | NS |
| Baseline | 0.56±0.11 | 0.54±0.15 | 0.57±0.07 | NS |
| Post-treatment | 0.48±0.12 | 0.47±0.16 | 0.48±0.08 | NS |
| Change in probing depth | 0.35±0.34 | 0.30±0.25 | 0.38±0.39 | NS |
| Baseline | 2.58±0.78 | 2.64±0.79 | 2.55±0.79 | NS |
| Post-treatment | 2.23±0.72 | 2.34±0.74 | 2.17±0.71 | NS |
| Change in bone level | 0.39±0.62 | 0.36±0.46 | 0.42±0.71 | NS |
| Baseline | 3.53±1.26 | 3.35±1.55 | 3.63±1.09 | NS |
| Post-treatment | 3.13±0.95 | 2.99±1.27 | 3.21±0.72 | NS |
| Treatment period (months) | 5.01±2.20 | 4.85±2.44 | 5.11±2.10 | NS |
FA: orthodontic treatment with fixed appliances, CAT: clear aligner treatment, NS: statistically not significant.
Interexaminer reliability
The interexaminer evaluation of radiographic measurements using Bland-Altman plots showed good agreement. The intraclass correlation coefficient of radiographic measurements at baseline was 0.929. After orthodontic treatment, the intraclass correlation coefficient of two radiographic measurements was 0.940. For radiographic measurements, the interexaminer evaluation showed high reliability.
Correlation among clinical parameters
No significant correlation was found between the duration of treatment and patient age (Table 4). The duration of orthodontic treatment was significantly related to gingival index scores at baseline. The duration of treatment was also negatively correlated with the probing depth at baseline, but this correlation was not statistically significant.
Table 4. Spearman’s correlation coefficients between clinical parameters and treatment duration.
| Correlations | r | P-value |
|---|---|---|
| Treatment duration with age | -0.041 | 0.814 |
| Treatment duration with PlIPre | -0.156 | 0.370 |
| Treatment duration with GIPre | -0.336 | 0.048 |
| Treatment duration with PDPre | -0.247 | 0.153 |
| Treatment duration with BLPre | -0.111 | 0.550 |
| Bone level change with age | 0.03 | 0.862 |
| Bone level change with PlIPre | 0.436 | 0.009 |
| Bone level change with GIPre | 0.391 | 0.020 |
| Bone level change with Pdpre | 0.389 | 0.038 |
| Bone level change with BLPre | 0.622 | <0.001 |
r: Spearman's correlation coefficient, PlIPre: plaque index at baseline, GIPre: gingival index at baseline, PDPre: probing depth at baseline, BLPre: alveolar bone level at baseline.
Changes in alveolar bone level were significantly correlated with plaque index scores, gingival index scores, probing depths, and alveolar bone level at baseline (P=0.009, P=0.020, P=0.038, and P<0.001, respectively). However, no correlation was found between changes in alveolar bone level and patient age.
DISCUSSION
The aim of this study was to evaluate the effect of orthodontic treatment on periodontal tissue and to compare two different orthodontic treatments in patients with periodontitis. The effects of orthodontic treatment were evaluated depending both on the technique and the treatment site.
After orthodontic treatment, the overall plaque index, gingival index, and probing depth improved (P<0.01). The overall bone level also improved (P=0.45). However, bone level changes over the course of treatment showed no significant differences in the FA and CAT groups.
The plaque index improved in both groups following orthodontic treatment, but no statistically significant differences were observed between the FA and CAT groups. Statistically significant differences were found between the FA and CAT groups regarding probing depth. Miethke and Vogt [13] reported that the plaque index scores of patients with fixed appliances were significantly higher than those of patients with clear aligners at baseline and at three different evaluation time points. However, they found no statistically significant differences in probing depth between patients with fixed appliances and those with clear aligners. They also emphasized that oral hygiene improved over the course of their study, which may have been due repeated instructions, motivation, and professional oral hygiene support.
Regarding the alveolar bone level, we expected some alveolar bone loss after orthodontic treatment. We found, however, that the alveolar bone level improved in both groups. We took panoramic radiographs before orthodontic treatment and within six months after the orthodontic treatment. The duration of treatment was not long enough to observe alveolar bone change. Intraoral radiographs were used to calculate the exact alveolar bone level, and no significant differences were found between examiners, Kim et al. [22] reported that determining the prognosis for bone loss is possible using panoramic radiographs, and that additional intraoral films may be helpful when rapid changes in bone level are expected. In 11 patients, alveolar bone loss was observed, while in 23 patients, the alveolar bone level improved. Therefore, it may be suggested that meticulous root planing and oral hygiene education during the course of orthodontic treatment enhanced the periodontal outcomes in both the FA and CAT groups.
The duration of treatment in the FA group was shorter than in the CAT group. Pavoni et al. [16] compared orthodontic treatment with self-ligating brackets and clear aligners, and found no differences in the treatment duration between groups (1.8 years for both groups), indicating that clear aligner treatment is not faster than fixed appliances. All of the patients included in this study experienced anterior crowding or pathologic migration in the anterior area of the maxilla or the mandible. We aimed to correct the anterior irregularity and improve both the aesthetics and the periodontal condition. Therefore, we attempted to shorten the duration of orthodontic treatment to prevent the worsening of periodontitis. In addition, the patients who were treated with fixed appliances had difficulties with oral hygiene and poorer aesthetics. In the CAT group, some patients had difficulty wearing the clear aligner for nearly 23 hours each day. Proffit et al. [23] suggested that adjunctive orthodontic tooth movement would take longer than six months and should be avoided. In this study, we excluded patients who had orthodontic treatments performed in the Department of Orthodontics. Therefore, the duration of treatment was shorter than has been previously reported [16].
We also divided patients into two groups according to the treatment site. On average, patients in the mandible group were older than those in the maxilla group. Anterior crowding may be more common in the mandible than in the maxilla with older age. Stanaitytė et al. [24] reported that the condition of the periodontium may influence the stability of the lower incisors, and that destructive changes in the periodontium may allow unbalanced muscular forces to produce pressure on the lower incisors. Notably, mandibular dental arch crowding is also more common in females because males have significantly longer and wider dental arch dimensions, which was confirmed in our study. Another longitudinal study also showed that subjects with class I molars and canines had a shorter arch length of the mandible [25]. Moreover, anterior crowding in the mandible makes it difficult to clean the teeth well. The plaque index scores in the mandible group were higher than those of the maxilla group both at baseline and after orthodontic treatment. However, the plaque index scores did not change to a significantly different extent between the two groups. Likewise, no significant differences were found in the gingival index, probing depth, alveolar bone level, or the duration of treatment according to the treatment site.
In orthodontic tooth movement, bone resorption occurs by removing alveolar bone from the path of the moving dental root, which is dangerous in periodontally compromised patients [26]. It has been suggested that different combinations of cell-cell and cell-matrix interactions occur via orthodontic forces [26,27].
Most contemporary fixed orthodontic appliances use light continuous forces as part of orthodontic mechanotherapy to achieve tooth movement. The characteristic feature of continuous interrupted tooth movement is formation of new bone layers in the richly cellular tissue at the entrance of open marrow spaces as soon as the tooth movement stops. A histochemical study showed that the application of continuous force produced concomitant alveolar bone resorption and formation at the pressure areas in rat molars [28].
In contrast, it has been shown that tooth movement in clear aligner therapy occurs via intermittent forces applied by the aligners [29]. In their analysis, Cattaneo et al. [30] reported that light continuous orthodontic forces are perceived as intermittent by the periodontium. Additionally, it was reported that weak intermittent forces could effectively induce receptor activator of nuclear factor kappa-B ligand activity via IL-1ß expression with less damage in the periodontal ligament cell [31]. However, an animal study [11] has demonstrated that orthodontic movement acts synergistically with periodontal disease, involving periodontal breakdown through the upregulation of proinflammatory cytokines.
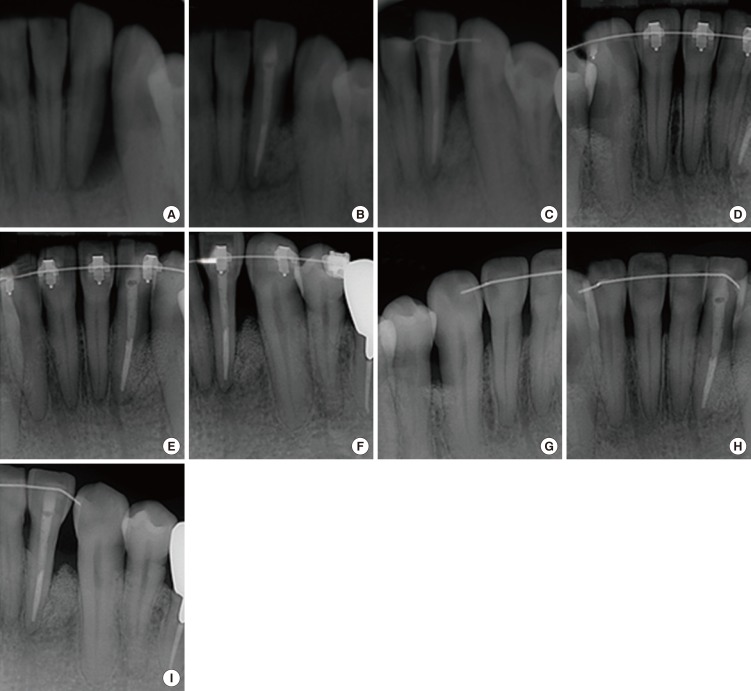
In the present study, 10 patients underwent flap operations as part of regenerative surgery before or after the orthodontic treatment. Some controversy exists regarding the timing of regenerative surgery [32,33,34,35,36]. Several clinical studies [8,33] have shown good results with orthodontic treatment 10–14 days after regenerative surgery. Passanezi et al. [35] reported that a guided tissue regeneration procedure after nine months of periodontal therapy involving open flap surgery and the orthodontic treatment showed radiographic bone filling. In an animal study [37], orthodontic tooth movement was observed three months after grafting with bovine bone graft material, and inactive filler material was found in the pressure site after 12 months of orthodontic treatment. Recently, Ahn et al. [38] reported that bone grafts placed in the surgical defect not only allowed immediate force application for accelerated orthodontic tooth movement with favorable periodontal regeneration outcomes, but also decrease the risk of inhibited orthodontic tooth movement in the case of delayed force application after surgery. Roberts and Chase [39] reported that orthodontic movement appeared to be effective in increasing the mitotic activity of the periodontal ligament cells. Additionally, Melsen et al. [40] found that the combination of periodontal treatment with orthodontic intrusion and good oral hygiene resulted in new attachment in an animal study. In cases where an intrabony defect remains after the combination of periodontal regenerative surgery and orthodontic treatment, further periodontal surgery may be needed to correct the bone defect. Therefore, in this study, most of the regenerative operations were performed after the orthodontic treatment with the exception of several cases (Figure 7). Moreover, a flap operation as part of regenerative surgery has the effect of a supracrestal fibrotomy for the prevention of the relapse of rotated or protruded teeth (Figure 8). Another synergic effect is the splinting effect of a resin wire-bonded retainer in regenerative periodontal surgery.
Figure 7.
Combined periodontal and orthodontic treatment. (A) A periapical radiograph showing an apical radiolucent lesion. (B) After endodontic treatment, regenerative periodontal surgery was performed using demineralized bovine bone mineral. (C) As part of successful regenerative surgery, the resin-wire splint was bonded to the neighboring teeth for more than six months. (D-F) Three years after the regenerative surgery, orthodontic treatment with a fixed appliance was initiated. (G-I) Periapical radiographs four years after orthodontic treatment with a fixed appliance.
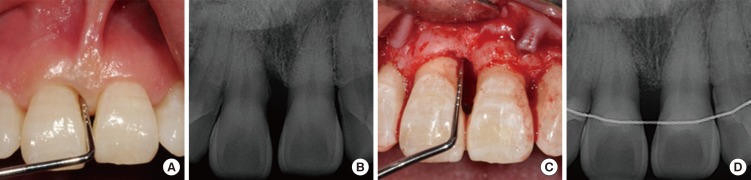
Figure 8.
Combined periodontal and orthodontic treatment. (A) Before orthodontic treatment, periodontal probing showed approximately 7 mm of attachment loss at the mesiobuccal point of right anterior incisor. (B) Periapical radiograph before orthodontic treatment. (C, D) After orthodontic treatment, a flap operation as part of regenerative surgery showed radiographic bone filling with the effect of a supracrestal fibrotomy for preventing relapse.
In this study, despite a patient preference for CAT and our efforts for randomization, we could not avoiding using CAT for severely mobile or labially inclined teeth. One case was converted from CAT to FA due to severe labial inclination of the lower anterior teeth with moderate attachment loss. This was a retrospective study that had difficulties in controlled randomization for ethical reasons, thereby involving a risk of bias. Therefore, a prospective randomized controlled study would be helpful in order to more precisely evaluate the outcomes of orthodontic treatment with FA and CAT in patients with periodontitis.
In the decision-making process regarding orthodontic treatment in patients with periodontitis, the clinical attachment level, the mobility of teeth, and the inclination of incisors should be considered (Figure 9). In addition, the cooperation of patients is crucial for CAT in patients with periodontitis. Most of all, continuous and repeated professional tooth cleansing and oral hygiene education are the most important factor for successful combined periodontal and orthodontic treatment.
Figure 9.
The decision-making process regarding orthodontic treatment in patients with periodontitis.
Within the limitations of this study, we suggest that combined periodontal and orthodontic treatment can improve patients’ periodontal health irrespective of orthodontic techniques. With the exception of cases where CAT cannot be applied, such as severely mobile or inclined teeth, both FA and CAT can be used for combined periodontal and orthodontic treatment. After orthodontic treatment, clinical parameters improved in both the FA and CAT groups in combination with meticulous oral hygiene education and repeated plaque control. Regarding plaque index and gingival index, no significant differences were found between these two groups. Additionally, our results suggest that after regenerative surgery, the use of a resin wire retainer for retention may have a synergic effect on the success of combined periodontal and orthodontic treatment. However, future studies evaluating the relationship between fixed retainers and oral hygiene in patients with periodontitis are needed.
ACKNOWLEDGMENTS
I offer special thanks to Prof. Kyu-Rhim Chung of Ajou University. I would also like to thank Prof. Jae-Joong Lim of the Department of Orthodontics for orthodontic advice and Dr. Sung-Hee Cho, Ju-Ryun Chung, and radiologic technician Seong-Jin Ahn of Hanyang University for their assistance in radiographic analysis.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Gkantidis N, Christou P, Topouzelis N. The orthodontic-periodontic interrelationship in integrated treatment challenges: a systematic review. J Oral Rehabil. 2010;37:377–467. doi: 10.1111/j.1365-2842.2010.02068.x. [DOI] [PubMed] [Google Scholar]
- 2.Türkkahraman H, Sayin MO, Bozkurt FY, Yetkin Z, Kaya S, Onal S. Archwire ligation techniques, microbial colonization, and periodontal status in orthodontically treated patients. Angle Orthod. 2005;75:231–237. doi: 10.1043/0003-3219(2005)075<0227:ALTMCA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 3.Boyd RL, Leggott PJ, Quinn RS, Eakle WS, Chambers D. Periodontal implications of orthodontic treatment in adults with reduced or normal periodontal tissues versus those of adolescents. Am J Orthod Dentofacial Orthop. 1989;96:191–199. doi: 10.1016/0889-5406(89)90455-1. [DOI] [PubMed] [Google Scholar]
- 4.Chou YH, Du JK, Chou ST, Hu KF, Tsai CC, Ho KY, et al. An interdisciplinary treatment approach combining orthodontic forced eruption with immediate implant placement to achieve a satisfactory treatment outcome: a case report. Clin Implant Dent Relat Res. 2013;15:113–133. doi: 10.1111/j.1708-8208.2011.00363.x. [DOI] [PubMed] [Google Scholar]
- 5.Liu XF, Pan XG, Shu R. A preliminary study of combined periodontal-orthodontic approach for treating labial displacement of incisors in patients with periodontal diseases. Shanghai Kou Qiang Yi Xue. 2008;17:264–270. [PubMed] [Google Scholar]
- 6.Artun J, Urbye KS. The effect of orthodontic treatment on periodontal bone support in patients with advanced loss of marginal periodontium. Am J Orthod Dentofacial Orthop. 1988;93:143–151. doi: 10.1016/0889-5406(88)90292-2. [DOI] [PubMed] [Google Scholar]
- 7.Nelson PA, Artun J. Alveolar bone loss of maxillary anterior teeth in adult orthodontic patients. Am J Orthod Dentofacial Orthop. 1997;111:328–362. doi: 10.1016/s0889-5406(97)70192-6. [DOI] [PubMed] [Google Scholar]
- 8.Re S, Corrente G, Abundo R, Cardaropoli D. Orthodontic treatment in periodontally compromised patients: 12-year report. Int J Periodontics Restorative Dent. 2000;20:31–40. [PubMed] [Google Scholar]
- 9.Bollen AM, Cunha-Cruz J, Bakko DW, Huang GJ, Hujoel PP. The effects of orthodontic therapy on periodontal health: a systematic review of controlled evidence. J Am Dent Assoc. 2008;139:413–435. doi: 10.14219/jada.archive.2008.0184. [DOI] [PubMed] [Google Scholar]
- 10.Wennström JL, Stokland BL, Nyman S, Thilander B. Periodontal tissue response to orthodontic movement of teeth with infrabony pockets. Am J Orthod Dentofacial Orthop. 1993;103:313–322. doi: 10.1016/0889-5406(93)70011-C. [DOI] [PubMed] [Google Scholar]
- 11.Boas Nogueira AV, Chaves de Souza JA, Kim YJ, Damião de Sousa-Neto M, Chan Cirelli C, Cirelli JA. Orthodontic force increases interleukin-1β and tumor necrosis factor-α expression and alveolar bone loss in periodontitis. J Periodontol. 2013;84:1319–1345. doi: 10.1902/jop.2012.120510. [DOI] [PubMed] [Google Scholar]
- 12.van Gastel J, Quirynen M, Teughels W, Carels C. The relationships between malocclusion, fixed orthodontic appliances and periodontal disease. A review of the literature. Aust Orthod J. 2007;23:121–130. [PubMed] [Google Scholar]
- 13.Miethke RR, Vogt S. A comparison of the periodontal health of patients during treatment with the Invisalign system and with fixed orthodontic appliances. J Orofac Orthop. 2005;66:219–248. doi: 10.1007/s00056-005-0436-1. [DOI] [PubMed] [Google Scholar]
- 14.Miethke RR, Brauner K. A Comparison of the periodontal health of patients during treatment with the Invisalign system and with fixed lingual appliances. J Orofac Orthop. 2007;68:223–254. doi: 10.1007/s00056-007-0655-8. [DOI] [PubMed] [Google Scholar]
- 15.Boyd RL. Periodontal and restorative considerations with clear aligner treatment to establish a more favorable restorative environment. Compend Contin Educ Dent. 2009;30:280–282. [PubMed] [Google Scholar]
- 16.Pavoni C, Lione R, Laganà G, Cozza P. Self-ligating versus Invisalign: analysis of dento-alveolar effects. Ann Stomatol (Roma) 2011;2:23–30. [PMC free article] [PubMed] [Google Scholar]
- 17.Drake CT, McGorray SP, Dolce C, Nair M, Wheeler TT. Orthodontic tooth movement with clear aligners. ISRN Dent. 2012;2012:657973. doi: 10.5402/2012/657973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kravitz ND, Kusnoto B, Agran B, Viana G. Influence of attachments and interproximal reduction on the accuracy of canine rotation with Invisalign. A prospective clinical study. Angle Orthod. 2008;78:682–689. doi: 10.2319/0003-3219(2008)078[0682:IOAAIR]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 19.Savage A, Eaton KA, Moles DR, Needleman I. A systematic review of definitions of periodontitis and methods that have been used to identify this disease. J Clin Periodontol. 2009;36:458–525. doi: 10.1111/j.1600-051X.2009.01408.x. [DOI] [PubMed] [Google Scholar]
- 20.Silness J, Loe H. Periodontal Disease in Pregnancy. Ii. Correlation between Oral Hygiene and Periodontal Condtion. Acta Odontol Scand. 1964;22:121–156. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- 21.Loe H, Silness J. Periodontal Disease in Pregnancy. I. Prevalence and Severity. Acta Odontol Scand. 1963;21:533–584. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 22.Kim TS, Obst C, Zehaczek S, Geenen C. Detection of bone loss with different X-ray techniques in periodontal patients. J Periodontol. 2008;79:1141–1150. doi: 10.1902/jop.2008.070578. [DOI] [PubMed] [Google Scholar]
- 23.Proffit WR, Fields HW. Contemporary orthodontics. 2nd ed. St. Louis: Mosby; 1992. pp. 554–606. [Google Scholar]
- 24.Stanaitytė R, Trakinienė G, Gervickas A. Do wisdom teeth induce lower anterior teeth crowding? A systematic literature review. Stomatologija. 2014;16:15–23. [PubMed] [Google Scholar]
- 25.Bishara SE, Treder JE, Damon P, Olsen M. Changes in the dental arches and dentition between 25 and 45 years of age. Angle Orthod. 1996;66:417–439. doi: 10.1043/0003-3219(1996)066<0417:CITDAA>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 26.Krishnan V, Davidovitch Z. Cellular, molecular, and tissue-level reactions to orthodontic force. Am J Orthod Dentofacial Orthop. 2006;129:469.e1–4722. doi: 10.1016/j.ajodo.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 27.Davidovitch Z, Nicolay OF, Ngan PW, Shanfeld JL. Neurotransmitters, cytokines, and the control of alveolar bone remodeling in orthodontics. Dent Clin North Am. 1988;32:411–446. [PubMed] [Google Scholar]
- 28.Bonafe-Oliveira L, Faltin RM, Arana-Chavez VE. Ultrastructural and histochemical examination of alveolar bone at the pressure areas of rat molars submitted to continuous orthodontic force. Eur J Oral Sci. 2003;111:410–416. doi: 10.1034/j.1600-0722.2003.00067.x. [DOI] [PubMed] [Google Scholar]
- 29.Rossini G, Parrini S, Castroflorio T, Deregibus A, Debernardi CL. Efficacy of clear aligners in controlling orthodontic tooth movement: a systematic review. Angle Orthod. 2015;85:881–890. doi: 10.2319/061614-436.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cattaneo PM, Dalstra M, Melsen B. Strains in periodontal ligament and alveolar bone associated with orthodontic tooth movement analyzed by finite element. Orthod Craniofac Res. 2009;12:120–128. doi: 10.1111/j.1601-6343.2009.01445.x. [DOI] [PubMed] [Google Scholar]
- 31.Nakao K, Goto T, Gunjigake KK, Konoo T, Kobayashi S, Yamaguchi K. Intermittent force induces high RANKL expression in human periodontal ligament cells. J Dent Res. 2007;86:623–631. doi: 10.1177/154405910708600708. [DOI] [PubMed] [Google Scholar]
- 32.Diedrich PR. Guided tissue regeneration associated with orthodontic therapy. Semin Orthod. 1996;2:39–45. doi: 10.1016/s1073-8746(96)80038-7. [DOI] [PubMed] [Google Scholar]
- 33.Cardaropoli D, Re S, Manuzzi W, Gaveglio L, Cardaropoli G. Bio-Oss collagen and orthodontic movement for the treatment of infrabony defects in the esthetic zone. Int J Periodontics Restorative Dent. 2006;26:553–562. [PubMed] [Google Scholar]
- 34.Ogihara S, Marks MH. Enhancing the regenerative potential of guided tissue regeneration to treat an intrabony defect and adjacent ridge deformity by orthodontic extrusive force. J Periodontol. 2006;77:2093–2193. doi: 10.1902/jop.2006.003159. [DOI] [PubMed] [Google Scholar]
- 35.Passanezi E, Janson M, Janson G, Sant’Anna AP, de Freitas MR, Henriques JF. Interdisciplinary treatment of localized juvenile periodontitis: a new perspective to an old problem. Am J Orthod Dentofacial Orthop. 2007;131:268–344. doi: 10.1016/j.ajodo.2005.03.025. [DOI] [PubMed] [Google Scholar]
- 36.Rossini G, Parrini S, Castroflorio T, Deregibus A, Debernardi CL. Periodontal health during clear aligners treatment: a systematic review. Eur J Orthod. 2015;37:539–582. doi: 10.1093/ejo/cju083. [DOI] [PubMed] [Google Scholar]
- 37.Araújo MG, Carmagnola D, Berglundh T, Thilander B, Lindhe J. Orthodontic movement in bone defects augmented with Bio-Oss. An experimental study in dogs. J Clin Periodontol. 2001;28:73–80. doi: 10.1034/j.1600-051x.2001.280111.x. [DOI] [PubMed] [Google Scholar]
- 38.Ahn HW, Ohe JY, Lee SH, Park YG, Kim SJ. Timing of force application affects the rate of tooth movement into surgical alveolar defects with grafts in beagles. Am J Orthod Dentofacial Orthop. 2014;145:486–581. doi: 10.1016/j.ajodo.2013.12.021. [DOI] [PubMed] [Google Scholar]
- 39.Roberts WE, Chase DC. Kinetics of cell proliferation and migration associated with orthodontically-induced osteogenesis. J Dent Res. 1981;60:174–255. doi: 10.1177/00220345810600021501. [DOI] [PubMed] [Google Scholar]
- 40.Melsen B, Agerbaek N, Eriksen J, Terp S. New attachment through periodontal treatment and orthodontic intrusion. Am J Orthod Dentofacial Orthop. 1988;94:104–120. doi: 10.1016/0889-5406(88)90358-7. [DOI] [PubMed] [Google Scholar]