Abstract
Background
The current longitudinal study examined associations between interpersonal potentially traumatic events (PTEs; i.e., sexual or physical assault) and changes in alcohol consumption among incoming college students.
Methods
1197 students (68% female) participating in a university-wide research study were included in analyses. Assessments were administered at three time-points and included measures of alcohol use, PTEs (Life Events Checklist), and a screener for possible PTSD symptoms (abbreviated Primary Care PTSD Screen). Linear growth curve models were fit to the three repeated measures of alcohol quantity and frequency to determine the role of pre-college and college-onset interpersonal PTEs and possible PTSD symptoms on patterns of alcohol use.
Results
Pre-college interpersonal PTE was associated with greater baseline alcohol use for female but not male students. College-onset interpersonal PTE predicted greater alcohol use at concurrent and future assessments for women but not men, beyond the effects of pre-college PTE. Pre-college possible PTSD symptoms did not predict baseline or change in alcohol use.
Conclusions
There may be a stronger and longer-lasting impact of interpersonal PTE for college women compared to men on alcohol phenotypes, although replication in studies oversampling men endorsing interpersonal PTE is needed.
Keywords: Trauma, Posttraumatic stress disorder, Alcohol, Sexual assault, Physical assault
1. Introduction
College students are at high risk for problematic alcohol use. Two-thirds of college students report current (i.e., past month) alcohol use, and nearly half report recent (i.e., past two weeks) binge drinking, a known risk factor for AUDs (AUD) (O’Malley & Johnston, 2002). The 12-month prevalence rate for a DSM-IV AUD (alcohol abuse or dependence) is 20.4% among college students (Blanco et al., 2008), with the median age of onset of lifetime AUDs among adults being 20 years (Kessler et al., 2005). It is important to identify predictors of problem alcohol use in college samples to inform prevention and early intervention efforts.
A history of potentially traumatic events (PTEs) and/or posttraumatic stress disorder (PTSD) symptoms predicts high risk drinking, such as drinking to cope with negative affect (Waldrop et al., 2007), and subsequent AUDs (Kessler et al., 1995). Interpersonal PTEs (e.g., physical and sexual assault/abuse), as opposed to accidental PTEs (e.g., natural disasters, motor vehicle accidents), have a greater relative risk for PTSD (Kessler et al., 1995). Available data suggest that interpersonal PTEs and alcohol use problems could have a cyclical relationship. For example, women exposed to violence who develop alcohol abuse are more vulnerable to revictimization compared to those not abusing alcohol (Messman-Moore & Long, 2003). PTE exposure, particularly interpersonal PTE history, also is related to problem alcohol use among college women (Green et al., 2005). It may be the case that trauma-exposed individuals are more likely to develop AUDs due to motivation to use alcohol to cope with trauma memories and psychiatric symptoms (O’Hare & Sherrer, 2011; Coffey et al., 2002). However, twin and family studies also indicate that interpersonal PTEs and PTSD symptoms share familial liability (i.e., genetic risk and common environment) with alcohol phenotypes, such as alcohol consumption (McLeod et al., 2001), and that PTSD and alcohol dependence share familial liability (Xian et al., 2000).
Longitudinal studies are useful for examining the natural course of associations between trauma and alcohol phenotypes. The majority of longitudinal studies examining associations between interpersonal PTEs and alcohol use have been conducted in all-female samples. For example, Kilpatrick and colleagues found that physical or sexual assault was associated prospectively with increased alcohol use in women (Kilpatrick et al., 1997). Similarly, incapacitated rape has demonstrated prospective associations with increased alcohol use in college women (Kaysen et al., 2006). Other longitudinal studies have not found evidence for an association between interpersonal PTE and alcohol use. For example, intimate partner violence did not significantly predict changes in alcohol use in an all-female sample (Testa, Livingston, & Leonard, 2003). However, the women in this sample ranged in age from 18 to 30 years old (mean = 24 years). It is possible that acute changes in alcohol use are more likely to be evidenced during emerging adulthood (e.g., college), prior to drinking patterns becoming better established.
In one of only a few prospective evaluations of PTEs and alcohol use in mixed-gender college student samples, Read and colleagues demonstrated that a PTE history and PTSD symptoms upon enrollment are related to significantly greater endorsement of negative alcohol-related consequences throughout the first year of college, even after accounting for trait-level neuroticism and demographic characteristics (Read et al., 2012). Furthermore, PTSD symptoms and alcohol use/problems appear to be reciprocally related over time in college student samples (Read, Wardell, & Colder, 2013). In spite of the inclusion of male and female participants, a distinction was not made between interpersonal and accidental PTE types. As such, there was likely significant variability in participants’ PTE experiences.
Taken together, there is a solid empirical basis for the relationship between PTE/PTSD and alcohol use outcomes. However, no studies to our knowledge have examined prospectively the unique influence of new-onset interpersonal PTE, above and beyond a prior history of interpersonal PTE, on changes in alcohol use in a mixed-gender college sample. As such, it is unclear whether a relationship between interpersonal PTE and alcohol use differs by sex. The aim of the current study was to investigate pre-college and college-onset interpersonal PTEs and possible PTSD symptoms in relation to alcohol use trajectories. It was hypothesized that: (1) a pre-college history of interpersonal PTEs and possible PTSD symptoms would be incrementally related (i.e., no interpersonal PTE < interpersonal PTE < possible PTSD symptoms) to increased baseline and rate of change of alcohol use quantity and frequency; and (2) college-onset interpersonal PTEs and possible PTSD symptoms would be incrementally related (i.e., no new interpersonal PTE < new interpersonal PTE < new possible PTSD symptoms) to increased rate of change of alcohol use quantity and frequency, over and above the effects of pre-college PTEs and possible PTSD symptoms. To examine potential sex effects, sex was included as a grouping variable in the models.
2. Materials and methods
2.1. Participants and procedure
Participants included the first cohort of Spit for Science, a university-wide, longitudinal research study at Virginia Commonwealth University (VCU) investigating substance use and emotional health in college students (Dick et al., 2014). The VCU Institutional Review Board approved all study procedures, and informed consent was obtained from all participants. Study data were collected and managed using REDCap (Research Electronic Data Capture), hosted at Virginia Commonwealth University (Harris et al., 2009). REDCap is a secure, web-based application that provides: (1) an interface for data entry; (2) audit trails for tracking data manipulation and export procedures; (3) automated export procedures to common statistical packages; and (4) procedures for importing data from external sources.
Incoming freshmen age 18 and older in fall 2011 (N = 3623) were invited via e-mail to participate in the web-based study. 2056 students (57%) completed the initial survey (wave 1) and were invited for a follow-up survey in spring 2012 (wave 2; n = 1558, 76%). All wave 1 participants also were invited to complete a follow-up survey in spring 2013 (wave 3; n = 1346, 59%). Participants were compensated $10 and a t-shirt at each assessment. Participants were included in analyses if they had non-missing data for key study variables at one or more time points (final n = 1197, 44.1%).
2.2. Measures
2.2.1. Alcohol consumption
Past 30-day alcohol use frequency was assessed on a 5-point scale ranging from 1 (“Never”) to 5 (“Four or more times a week”). Participants were provided information regarding what constitutes a “standard drink.” Past 30-day alcohol use quantity was then assessed as the average number of standard drinks consumed on a typical drinking day and was assessed on a 6-point scale, ranging from 1 (“None”) to 6 (“10 or more drinks”). Individuals endorsing no lifetime alcohol use were assigned the past 30-day values of “Never” for frequency and “None” for quantity.
2.2.2. PTEs
An abbreviated Life Events Checklist (Gray et al., 2004) assessed: natural disasters, physical assaults, sexual assaults, other unwanted or uncomfortable sexual experiences, and transportation accidents. At wave 1, if a participant endorsed having ever experiencing a physical assault, sexual assault, or other unwanted sexual experience, they were determined to have a pre-college history of interpersonal PTE. At wave 2, participants were asked to indicate whether they had experienced each PTE “after [they] started college.” At wave 3, participants indicated if they had experienced each PTE in the past 12 months (i.e., since wave 2). Participants endorsing an interpersonal PTE at wave 2 or 3 were determined to have a college-onset PTE. Participants who endorsed an accidental PTE but no interpersonal PTE were included in analyses with participants who endorsed no history of PTE.
2.2.3. Possible PTSD symptoms
Due to limited available space within a large, university-wide assessment battery, a PTSD screener item was adapted from the Primary Care PTSD Screen (PC-PTSD) (Prins et al., 2003) and assessed whether the participants with a PTE history had experienced potential symptoms of PTSD. Specifically, the item asked, “Have any of these experiences resulted in any of the following symptoms: Nightmares about it, tried hard not to think about it or went out of your way to avoid situations that reminded you of it, constantly on guard, watchful, or easily startled, or felt numb or detached from others, activities, or your surroundings?” Endorsement at wave 1 indicated a pre-college history of possible PTSD symptoms. At waves 2 and 3, participants with new PTE were queried with regard to possible PTSD symptoms since the last assessment, with endorsement indicating college-onset possible PTSD symptoms.
2.3. Statistical analysis
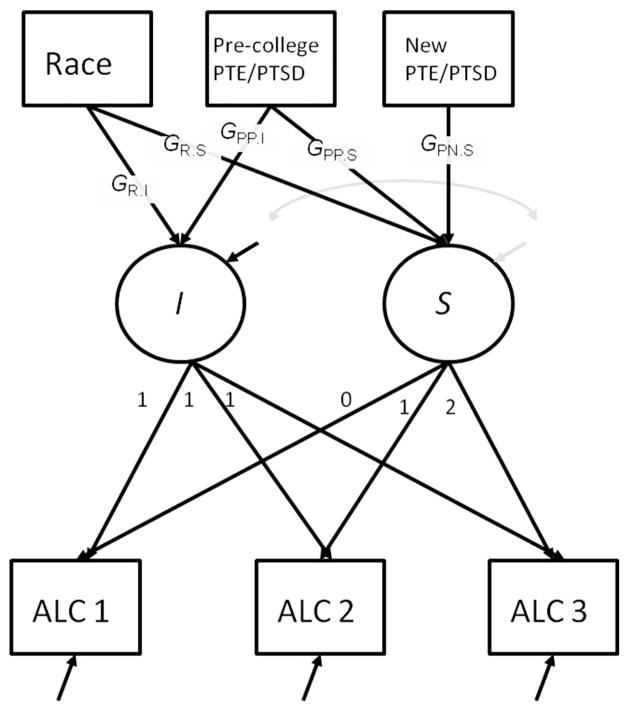
Growth Curve Models (GCM) (Bollen & Curran, 2006) were used to model changes in the alcohol use frequency and quantity and the effects of the covariates on these changes. Linear growth curves were fit to three repeated measurements of alcohol use, with separate models being fit for alcohol use frequency and quantity variables. In Fig. 1, ALC1 to ALC3 represent the alcohol use variables (frequency or quantity) measured at the initial assessment at 2011 fall semester (wave 1), freshmen follow-up at 2012 spring semester (wave 2), and sophomore follow-up at 2013 spring semester (wave 3), respectively. Because time was centered at the initial assessment, the Interceptor factor (I) represents the baseline level of alcohol use at the initial assessment, with all factor loadings fixed to one. The linear slope (S) factor represents the rate of change by fixing its factor loadings to linearly increasing constants, 0, 1, and 2 for first, second, and third wave of assessments, respectively.
Fig. 1.
Effects of covariates on initial level and rate of change of alcohol use. Note: The I factor represents the intercept of alcohol variables (ALC1 through ALC3) regressed on age, by fixing the factor loadings from I to alcohol variables at zero. The S factor represents the linear slope of the regression by fixing the factor loadings from S to alcohol variables to values correspond to time (0, 1, and 2).
The model in Fig. 1 includes three covariates: race, experience of interpersonal PTE, and possible PTSD symptoms before (PTE/PTSD: pre-college) and after (PTE/PTSD: new) starting college. Race was coded into five categories — White, Asian, Black, Latino, and Other. Four dummy variables were created (reference group = White). Each PTE/PTSD variable had three levels – no interpersonal PTE (None), interpersonal PTE without PTSD (PTE), and interpersonal PTE with possible PTSD symptoms (PTSD) – dummy coded into two variables (reference group = PTE). Race/ethnicity and pre-college interpersonal PTE/PTSD predicted both I and S factors. College-onset interpersonal PTE and possible PTSD symptoms predicted only the S factor, because their assessments were subsequent to the initial assessment of alcohol use.
Sex was used as a grouping variable. To examine potential differences of growth factors and effects of covariates, sex-specific parameters were estimated, and the difference in each parameter between sexes was tested using the Wald test (H0: βmale = βfemale). Mplus 7.11 (Muthen & Muthen, 1998–2012) was used for model fitting, and parameters were estimated using the Weighted Least Square estimator with mean- and variance-adjusted chi-squared test statistics (WLSMV).
3. Results
3.1. Descriptive statistics
Of the 1006 participants included in current analyses, 68.2% (n = 686) were female, compared to 59.3% in the full Cohort 1 sample, partly due to higher retention rates in females than males. Race/ethnicity rates were: 51.7% (n = 520) White, 0.5% (n = 5) American Indian/Alaskan Native, 15.7% (n = 158) Asian, 20.9% (n = 210) Black/African American, 4.9% (n = 49) Hispanic/Latino, 5.5% (n = 55) more than one race, 0.6% (n = 6) Native Hawaiian/Pacific Islander, and 0.3% (n = 3) unknown. Race/ethnicity was largely comparable to the full Cohort 1 sample and the full undergraduate student body (Dick et al., 2014).
Included and excluded participants were compared on key variables. No notable differences were observed for alcohol use frequency. Alcohol quantity differed between included and excluded participants at wave two, with included participants more likely to endorse mid categories (“3 or 4 drinks” and “5 or 6 drinks”) and less likely to endorse highest (“10 or more”) or lowest (“none”) categories (χ2 = 13.36, df = 5, p = .020). Race/ethnicity was similarly distributed in both groups. Females were overrepresented in included participants (68.0% and 53.5% in the included and excluded samples, respectively, χ2 = 46.26, df = 1, p < .001). Interpersonal PTE differed between included and excluded participants at the second and third waves, with included participants more likely to endorse interpersonal PTEs (30.4% vs. 8.6%, χ2 = 90.39, df = 1, p < .001 at wave 2 and 20.8% vs. 12.7%, χ2 = 5.94, df = 1, p = .015 at wave 3).
Table 1 presents alcohol consumption and PTE data at each wave by sex. Endorsement of any alcohol use increased over time, but endorsements of the heaviest use categories decreased. Males and females did not differ on pre-college PTE (χ2 = .003, df = 1, p = .995). Females were more likely to endorse pre-college possible PTSD symptoms than males (χ2 = 44.67, df = 1, p < .001). At wave 2, females were more likely than males to endorse new-onset interpersonal PTEs (χ2 = 6.62, df = 1, p = .010) and possible PTSD symptoms (χ2 = 4.053, df = 1, p = .044). At wave 3, females were more likely than males to endorse new-onset interpersonal PTE (χ2 = 3.725, df = 1, p = .054) and possible PTSD symptoms (χ2 = 12.352, df = 1, p < .001).
Table 1.
Alcohol use, interpersonal potentially traumatic events (PTE), and possible PTSD symptoms endorsement by assessment waves.
| Wave 1
|
Wave 2
|
Wave 3
|
||||
|---|---|---|---|---|---|---|
| Male | Female | Male | Female | Male | Female | |
| Alcohol use frequency (%)a | ||||||
| Never | 43.8 | 45.6 | 28.8 | 28.6 | 21.3 | 19.0 |
| Monthly or less | 19.4 | 19.8 | 24.1 | 29.9 | 18.4 | 29.4 |
| 2–4 times/month | 12.2 | 13.0 | 25.0 | 25.9 | 25.3 | 24.1 |
| 2–3 times/week | 7.8 | 6.9 | 14.7 | 11.5 | 16.9 | 10.8 |
| 4+ times/week | 4.1 | 3.5 | 2.8 | .7 | 3.1 | 1.2 |
| Alcohol use quantity (%)b | ||||||
| None | 32.5 | 31.3 | 21.9 | 19.8 | 14.4 | 10.5 |
| 1 or 2 | 10.6 | 15.7 | 12.2 | 22.2 | 11.9 | 23.9 |
| 3 or 4 | 11.9 | 13.3 | 22.5 | 26.8 | 19.1 | 26.5 |
| 5 or 6 | 6.6 | 7.4 | 19.7 | 14.9 | 19.7 | 10.6 |
| 7, 8, or 9 | 6.6 | 1.5 | 9.4 | 3.4 | 9.1 | 2.9 |
| 10 or more | 4.7 | 1.7 | 3.4 | 0.4 | 3.1 | .4 |
| Interpersonal PTE/possible PTSD symptoms (%) | ||||||
| No PTE | 55.0 | 54.8 | 71.9 | 64.1 | 69.7 | 66.0 |
| PTE-only | 30.0 | 15.0 | 15.0 | 15.7 | 9.7 | 7.4 |
| PTE + PTSD | 15.0 | 30.2 | 8.8 | 15.9 | 4.4 | 11.8 |
| Interpersonal PTE types endorsed (%)c | ||||||
| Physical assault | 33.9 | 23.5 | 14.7 | 8.7 | 8.7 | 7.4 |
| Sexual assault | 3.7 | 82.9 | 3.0 | 48.8 | 2.5 | 42.7 |
| Unwanted sexual experience | 10.0 | 26.4 | 11.1 | 24.7 | 10.1 | 16.6 |
Note:
Alcohol use frequency = “How often do you have a drink containing alcohol?”
Alcohol use quantity = “How many drinks containing alcohol do you have on a typical day when you are drinking?”
Among the sub-set of participants endorsing a pre-existing (wave 1) or new-onset (waves 2–3) interpersonal PTE.
3.2. Estimating trajectories of alcohol use quantity and frequency
In a GCM without covariates, wave 1 alcohol use frequency did not differ between males and females (difference = 0.005, p = 0.95). Alcohol use frequency increased overall (i.e., means of the S factor were greater than zero; .264, p < .001 in males and .200, p < .001 in females). A slightly higher mean of the S factor was estimated in males, but constraining the mean of S factor equal across sex did not result in a significant difference in chi-squared statistics (Δχ2 = 3.185, df = 1, p = .074). Because the variance of S factor was estimated negative or near zero, it was fixed to zero. Results from GCM of alcohol use quantity showed a similar pattern. Initial alcohol use quantity was not different between males and females. Means of S factors indicated that alcohol use quantity increased (.213, p < .001 in males and .160, p < .001 in females). A higher mean of S factor estimated in male students did not result in a statistically significant difference (Δχ2 = 2.290, df = 1, p = .130). Correlations between I and S factors were negative in both males (−.699, p = .003) and females (−.668, p = .001), meaning that those who endorse higher initial levels of alcohol use quantity tend to have slower rates of increase.
3.3. Interpersonal PTE and possible PTSD symptoms predicting alcohol use trajectories
Table 2 summarizes the estimates of growth factors and covariate effects from the model described in Fig. 1 for alcohol use frequency. Thus, the growth models with covariates were fit with the variance of S factor fixed at zero because residual variances of S factor were estimated near zero or negative in both alcohol use frequency and quantity. This also led to the covariance between I and S factor being fixed to zero. Constraining the effects of race on the slope factor did not result in a significant difference in chi-squared statistic (Δχ2 = 12.673, Δdf = 8, p = .124), so they were dropped. The fit of resulting model was acceptable (RMSEA = .042, CFI = .977, and TLI = .922). The effect of race indicated that the initial levels were lower in Asians and Black participants, compared to White participants, in both males and females. Pre-college interpersonal PTE was associated with greater initial level of drinking frequency in females only. Pre-college PTE-only and PTE + PTSD groups did not differ in initial level. No difference between pre-college history of PTE with and without PTSD was observed for the rate of change. College-onset interpersonal PTE, compared to No PTE, was associated with increased rate of change, with no difference observed between PTE-only and PTE + PTSD. The last column of Table 2 provides results of the tests for the difference in the corresponding parameter by sex, for the parameter of which p-values were less than .1 in either males or females. For alcohol use frequency, although different patterns of significant parameters appeared between sexes, none of differences in the parameters between sexes was tested significant.
Table 2.
Effects of covariates on growth factors for alcohol use frequency.
| Male | Female | Equality testsa
|
||||||
|---|---|---|---|---|---|---|---|---|
| p2 | p | |||||||
| Growth factors | Meanc | [95% CI] | p | Mean | [95% CI] | p | ||
| I | 0.00 | . | . | 0.04 | [−0.35, 0.43] | .841 | ||
| S | 0.18 | [0.01, 0.35] | .045 | 0.00 | [−0.15, 0.15] | .976 | 2.38 | .122 |
| Race | Beta | [95% CI] | p | Beta | [95% CI] | p | ||
| On I (GR.I)b | ||||||||
| Asian | −0.67 | [−0.92, −0.42] | <.001 | −0.39 | [−0.57, −0.21] | <.001 | 3.17 | .075 |
| Black | −0.37 | [−0.69, −0.05] | .024 | −0.21 | [−0.36, −0.06] | .007 | 0.81 | .367 |
| Latino | 0.12 | [−0.50, 0.74] | .694 | −0.12 | [−0.40, 0.16] | .390 | ||
| Other | −0.24 | [−0.81, 0.33] | .411 | −0.17 | [−0.38, 0.04] | .117 | ||
| PTE/PTSD | Beta | [95% CI] | p | Beta | [95% CI] | p | ||
| Pre-college on I (GPP.I) | ||||||||
| PTE vs. none | −0.02 | [−0.31, 0.27] | .894 | 0.26 | [0.04, 0.48] | .022 | 2.26 | .133 |
| PTE vs. PTSD | 0.11 | [−0.29, 0.51] | .601 | 0.14 | [−0.09, 0.37] | .226 | ||
| Pre-college on S (GPP.S) | ||||||||
| PTE vs. none | 0.02 | [−0.12, 0.16] | .767 | −0.10 | [−0.22, 0.02] | .089 | 1.70 | .192 |
| PTE vs. PTSD | 0.00 | [−0.24, 0.24] | .985 | 0.01 | [−0.12, 0.14] | .922 | ||
| New on S (GPN.S) | ||||||||
| PTE vs. none | 0.22 | [0.06, 0.38] | .007 | 0.17 | [0.06, 0.28] | .005 | 0.32 | .568 |
| PTE vs. PTSD | −0.05 | [−0.25, 0.15] | .610 | −0.09 | [−0.21, 0.03] | .149 | ||
Null hypothesis of each test was H0: βmale = βfemale, and the degree of freedom was 1.
Parameter names in the parentheses (GR.I, GR.S, GPP.I, GPP.S, GPN.S) correspond to the parameter labels in Fig. 1.
Because I and S factors were regressed on covariates, they estimate the mean of I and S factors when all covariates are equal to zero, i.e. in White participants without PTE.
The growth model of alcohol use quantity with covariates is summarized in Table 3. The model fit the data well (RMSEA = .026, CFI = .993, and TLI = .990). Asian and Black participants had lower initial levels and greater rates of change compared to White participants. Pre-college interpersonal PTE was associated with greater initial level and slower rate of change for females only. College-onset interpersonal PTE was associated with increased rate of change for males and females. Possible PTSD symptoms did not influence initial level or rate of change beyond interpersonal PTE alone. Tests of equalities of parameters indicated that differences in effects of some races on initial level (Asian vs. White and Latino vs. White) and on the rate of change (Asian vs. White and Black vs. White) between sexes were significant. None of the sex differences in PTE/PTSD effects were statistically significant.
Table 3.
Effects of covariates on growth factors for alcohol use quantity.
| Male | Female | Equality testsa
|
||||||
|---|---|---|---|---|---|---|---|---|
| χ2 | p | |||||||
| Growth factors | Meanc | [95% CI] | p | Mean | [95% CI] | p | ||
| I | 0.00 | . | . | −0.15 | [−0.52, 0.22] | .432 | ||
| S | 0.08 | [−0.12, 0.28] | .430 | 0.04 | [−0.08, 0.16] | .483 | ||
| Race | Beta | [95% CI] | p | Beta | [95% CI] | p | ||
| On I (GR.I)b | ||||||||
| Asian | −0.74 | [−1.06, −0.42] | <.001 | −0.31 | [−0.52, −0.10] | .003 | 4.78 | .029 |
| Black | −0.65 | [−1.06, −0.24] | .002 | −0.32 | [−0.51, −0.13] | .001 | 2.04 | .154 |
| Latino | 0.60 | [−0.07, 1.27] | .081 | −0.22 | [−0.56, 0.12] | .219 | 4.42 | .036 |
| Other | −0.10 | [−0.79, 0.59] | .769 | −0.21 | [−0.48, 0.06] | .125 | ||
| On S (GR.S) | ||||||||
| Asian | 0.24 | [0.07, 0.41] | .004 | 0.04 | [−0.06, 0.14] | .481 | 4.40 | .036 |
| Black | 0.37 | [0.15, 0.59] | .001 | 0.12 | [0.02, 0.22] | .014 | 4.06 | .044 |
| Latino | −0.19 | [−0.45, 0.07] | .155 | 0.13 | [−0.06, 0.32] | .202 | ||
| Other | 0.09 | [−0.32, 0.50] | .660 | 0.08 | [−0.08, 0.24] | .324 | ||
| PTE/PTSD | Beta | [95% CI] | p | Beta | [95% CI] | p | ||
| I on pre-college (GPP.I) | ||||||||
| PTE vs. none | 0.07 | [−0.37, 0.23] | .669 | 0.27 | [0.06, 0.48] | .011 | 3.18 | .075 |
| PTE vs. PTSD | 0.13 | [−0.27, 0.53] | .516 | 0.12 | [−0.10, 0.34] | .299 | ||
| S on pre-college (GPP.S) | ||||||||
| PTE vs. none | 0.00 | [−0.17, 0.17] | .977 | −0.14 | [−0.24, −0.04] | .010 | 1.88 | .171 |
| PTE vs. PTSD | 0.01 | [−0.22, 0.24] | .908 | −0.03 | [−0.14, 0.08] | .549 | ||
| S on new (GPN.S) | ||||||||
| PTE vs. none | 0.20 | [0.06, 0.34] | .003 | 0.12 | [0.05, 0.19] | .002 | 1.16 | .282 |
| PTE vs. PTSD | −0.07 | [−0.24, 0.10] | .390 | −0.05 | [−0.13,0.03] | .276 | ||
Null hypothesis of each test was H0: βmale = βfemale, and the degree of freedom was 1.
Parameter names in the parentheses (GR.I, GR.S, GPP.I, GPP.S, GPN.S) correspond to the parameter labels in Fig. 1.
Because I and S factors were regressed on covariates, they estimate the mean of I and S factors when all covariates are equal to zero, i.e. in White participants without PTE.
3.4. Influence of new interpersonal PTE on alcohol use frequency and quantity
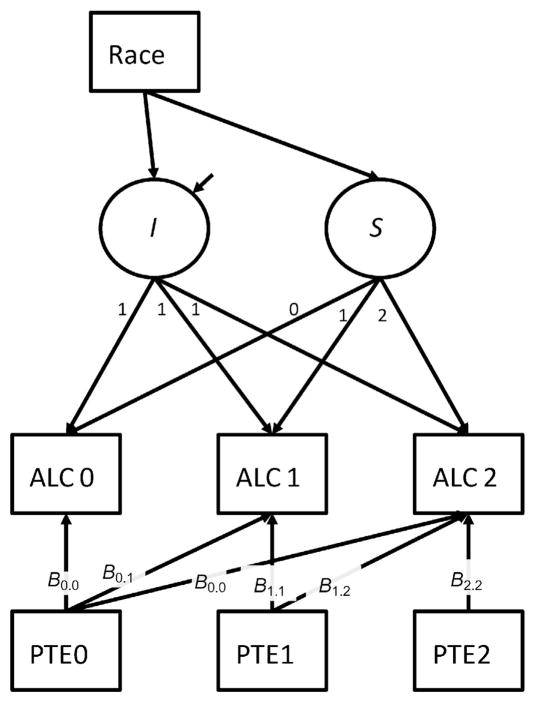
Given a lack of effect of possible PTSD symptoms beyond that of PTE, PTE with and without possible PTSD symptoms were combined. In addition, interpersonal PTE was treated as a time-varying covariate. In the model illustrated in Fig. 2, PTE0, PTE1, and PTE2 are binary variables that represent whether an individual experienced interpersonal PTE pre-college, during the first year of college, and during the second year of college, respectively. The paths from interpersonal PTE to alcohol use variables represent the effects of experiencing an interpersonal PTE on alcohol use, over and above the overall growth estimated by growth factors and effects of previous experiences of PTEs. Because subsequent events cannot affect preceding alcohol use, only paths from preceding PTE experience to concurrent and subsequent alcohol use were included in the model.
Fig. 2.
Effect of interpersonal potentially traumatic events (PTE) on subsequent alcohol use.
Table 4 summarizes the result for alcohol use frequency. The model fit was acceptable (RMSEA = .061, CFI = .980, and TLI = .975). In males, pre-college interpersonal PTE was associated with greater initial alcohol use frequency, but did not influence alcohol use frequency at either follow-up. College-onset interpersonal PTE did not influence concurrent or future reports of alcohol use frequency. In females, pre-college interpersonal PTE was associated with greater alcohol use frequency at the initial and first follow-up assessments. The same pattern was observed for college-onset interpersonal PTE endorsed at the first follow-up assessment, whereby endorsement predicted greater alcohol use frequency at the concurrent and second follow-up assessments. However, interpersonal PTE experienced during the second follow-up was not associated with concurrent alcohol use frequency.
Table 4.
Effect of interpersonal potentially traumatic events (PTE) on alcohol use frequency and quantity.
| Male
|
p | Female
|
p | |||
|---|---|---|---|---|---|---|
| Beta | [95% CI] | Beta | [95% CI] | |||
| Alcohol use frequency | ||||||
| On Pre-college PTE | ||||||
| Wave 1 (B0.0)a | 0.33 | [0.01, 0.65] | 0.043 | 0.30 | [0.10, 0.50] | 0.003 |
| Wave 2 (B0.1) | −0.05 | [−0.32, 0.22] | 0.729 | 0.23 | [0.09, 0.37] | 0.002 |
| Wave 3 (B0.2) | 0.15 | [−0.09, 0.38] | 0.213 | 0.11 | [−0.05, 0.27] | 0.162 |
| On PTE at wave 2 on | ||||||
| Wave 2 (B1.1) | 0.16 | [−0.23, 0.54] | 0.426 | 0.25 | [0.07, 0.44] | 0.007 |
| Wave 3 (B1.2) | 0.17 | [−0.18, 0.52] | 0.335 | 0.24 | [0.06, 0.43] | 0.010 |
| On PTE at wave 3 on | ||||||
| Wave 3 (B2.2) | 0.14 | [−0.20, 0.47] | 0.428 | 0.11 | [−0.08, 0.30] | 0.254 |
| Alcohol use quantity | ||||||
| On Pre-college PTE | ||||||
| Wave 1 (B0.0)a | 0.36 | [0.02, 0.71] | 0.040 | 0.34 | [0.14, 0.54] | 0.001 |
| Wave 2 (B0.1) | −0.05 | [−0.30, 0.20] | 0.705 | 0.18 | [0.05, 0.31] | 0.006 |
| Wave 3 (B0.2) | 0.04 | [−0.17, 0.26] | 0.692 | 0.04 | [−0.07, 0.15] | 0.505 |
| On PTE at wave 2 | ||||||
| Wave 2 (B1.1) | 0.24 | [−0.16, 0.63] | 0.240 | 0.17 | [0.01, 0.33] | 0.043 |
| Wave 3 (B1.2) | 0.10 | [−0.24, 0.44] | 0.557 | 0.27 | [0.14, 0.40] | 0.000 |
| On PTE at wave 3 | ||||||
| Wave 3 (B2.2) | 0.23 | [−0.08, 0.54] | 0.141 | 0.05 | [−0.10, 0.19] | 0.525 |
Parameter names in the parentheses (B0.0, B0.1, B0.2, B1.1, B1.2, and B2.2) correspond to the parameter names in Fig. 2.
The model for alcohol use quantity evidenced the similar pattern (Table 4). The model fit was acceptable (RMSEA = .060, CFI = .972, and TLI = .961). In males, pre-college interpersonal PTE was associated with greater initial alcohol use quantity, but no other significant associations were detected. In female students, pre-college interpersonal PTE history was associated with greater alcohol use quantity at the initial and first follow-up assessments. College-onset interpersonal PTE endorsed at the first follow-up assessment was associated with increased alcohol use quantity at the concurrent and second follow-up assessments.
4. Discussion
This study examined longitudinally the impact of new interpersonal PTE, beyond baseline PTE, on changes in alcohol consumption in a sample of college women and men. Two sets of longitudinal models were conducted, the first to examine pre-college interpersonal PTE and possible PTSD symptoms history in relation to initial college alcohol use and rate of change of alcohol use during the first two years of college. Second, the effect of college-onset interpersonal PTE was examined in relation to changes in alcohol use.
In the first set of models, pre-college interpersonal PTE was related to greater wave 1 (i.e., first semester) alcohol use for women but not men. This is consistent with a recent epidemiologic study indicating that the relationship between PTE history and alcohol use phenotypes may be stronger for women compared to men (Kachadourian, Pilver, & Potenza, In press). Pre-college PTE was not related to rate of change of alcohol use across the follow-up assessments, with the exception of PTE being related to slower rate of change of alcohol use quantity for women. Given that freshman women with pre-college PTE were drinking more heavily than their non-exposed peers at wave 1, it is possible that their peers gradually “caught up” over time. In spite of observed sex differences, tests of equality in parameters indicated that the effects of pre-college interpersonal PTE on I and S could be equated across sex without resulting in significant changes in model fit. Other studies also have not detected sex differences in college samples (Read et al., 2012). However, given the imbalance in the sample sizes between male and female students (68% female) and the increased rates of interpersonal PTEs experienced by female students, the results of the equality tests might have been distorted.
Pre-college possible PTSD symptoms was not associated with greater initial or rate of change of alcohol use beyond an interpersonal PTE history alone. The PTSD screener may not have been valid in a college sample, or the experience of interpersonal PTE may be a more potent predictor of alcohol use in college students. Some past studies have not found evidence for an effect of PTE on substance use disorders in the absence of PTSD (Chilcoat & Breslau, 1998). Future study of the nuanced relationships among PTE type, PTSD symptoms, and alcohol use in young adults is needed.
In the second set of models, college-onset interpersonal PTE (treated as a time-varying covariate) was examined in relation to changes in alcohol use. This model estimated the effects of interpersonal PTE at each time point on concurrent and subsequent alcohol use. For men, pre-college PTE with or without possible PTSD symptoms significantly predicted initial alcohol consumption (i.e., first semester); however, college-onset interpersonal PTE did not impact concurrent or subsequent levels of use. For women, pre-college PTE with or without possible PTSD symptoms significantly predicted increased alcohol consumption at the initial and first (i.e., freshman spring) follow-up appointments. Furthermore, college-onset PTE, above and beyond pre-college PTE, significantly predicted increased alcohol quantity and frequency at the concurrent and subsequent follow-up assessments.
Interpersonal PTE may have a more salient and longer-lasting impact on alcohol use for women compared to men. Stronger associations between PTE and alcohol use in women could be explained by a greater propensity to use alcohol as a coping strategy (Fossos et al., 2011). Additional prospective studies examining mechanisms linking PTE and alcohol consumption in women are needed, particularly given that greater alcohol use places women at risk for additional interpersonal PTEs (Mouilso, Fischer, & Calhoun, 2012).
More generally, college-onset interpersonal PTE was particularly high among female students (28.7% and 21.5% in the first and second years of college, respectively). Evaluation of (a) strategies for preventing interpersonal PTE (e.g., sexual assault) among potential perpetrators, and (b) protective strategies (e.g., decreasing alcohol use in high-risk situations) for college women who may become targets of assault is needed. Further, investigation of secondary prevention efforts among college women with interpersonal PTE is critical for buffering against the negative impact of these events.
The current study has a number of limitations. First, we had a single-item screener assessing possible PTSD symptoms. Continuous measures of PTSD symptoms would be useful in replication studies. Second, we did not have an assessment of PTE severity, which could have influenced observed sex differences. Third, the current study relied on self-report assessment. As such, we were not able to determine psychiatric diagnoses for the sample at each of the time points, limiting our ability to interpret the present findings. Future studies utilizing multi-method designs (e.g., clinical laboratory paradigms) also would inform our understanding of potential mechanisms linking interpersonal PTE and alcohol phenotypes. Fourth, we were not able to examine the role of type of alcohol (e.g., beer, liquor) typically consumed as a factor in our models. Future studies examining potential changes in preferred alcoholic beverage may add useful information to this literature. Finally, the present study was limited by the high rate of missing data. Thus, although the initial study sample was largely representative to the VCU student body, the analyses were conducted on 44.1% of the sample due to missingness, a result of both university and study attrition. It is possible that the students experiencing the most severe changes in substance use or psychiatric functioning were more likely to drop out of the study or drop out of the university. Additional empirical efforts to understand attrition from university-wide research studies would be useful for better understanding such samples.
The current study provides novel evidence for prospective links between interpersonal PTE and alcohol consumption among female college students. Future studies examining potential mechanisms underlying this relationship will facilitate prevention and early intervention efforts.
HIGHLIGHTS.
Pre-college interpersonal trauma predicts greater first semester alcohol use for female students.
College-onset interpersonal trauma predicts greater concurrent and future alcohol consumption for female students.
Associations between interpersonal trauma and alcohol use may be more salient for women than men.
Almost a quarter of college women endorsed interpersonal trauma during the first two years of college.
Acknowledgments
Role of funding sources
Spit for Science: The VCU Student Survey is funded by R37AA011408 (PI: Kendler) from the National Institute on Alcohol Abuse and Alcoholism, with support for Dr. Dick through K02AA018755. Additional support for the project was obtained through the National Institutes of Health P20AA107828, Virginia Commonwealth University, and UL1RR031990 from the National Center for Research Resources and National Institutes of Health Roadmap for Medical Research. These funding sources had no role in the analysis or interpretation of the data, writing of the manuscript, or the decision to submit the paper for publication.
We would like to thank the VCU students for making this study a success, as well as the many VCU faculty, students, and staff who contributed to the design and implementation of the project. Spit for Science: The VCU Student Survey is funded by R37AA011408 (to K. Kendler) from the National Institute on Alcohol Abuse and Alcoholism, with support for Dr. Dick through K02AA018755. Additional support for the project was obtained through the National Institutes of Health P20AA107828, Virginia Commonwealth University, and UL1RR031990 from the National Center for Research Resources and National Institutes of Health Roadmap for Medical Research. Dr. Berenz is supported by the National Institute on Alcohol Abuse and Alcoholism (4R00AA022385) and a NARSAD Young Investigator Award from the Brain and Behavior Research Foundation. Dr. Amstadter is supported by grants R01AA020179, BBRF 20066, R01MH101518, and P60MD002256.
Footnotes
Contributors
Dr. Berenz, Dr. Cho, Dr. Amstadter, and Dr. Dick developed the idea for this manuscript and data analytic plan. Dr. Berenz and Dr. Cho wrote the primary draft of this manuscript. Dr. Kendler and Dr. Dick designed and executed the primary study and data collection effort. All authors have contributed to and approved the final manuscript.
Conflict of interest
The authors have nothing to disclose.
References
- Blanco C, et al. Mental health of college students and their non-college-attending peers: results from the national epidemiologic study on alcohol and related conditions. Archives of General Psychiatry. 2008;65(12):1429–1437. doi: 10.1001/archpsyc.65.12.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bollen KA, Curran PJ. Latent Curve Models: A Structural Equation Perspective. Hoboken, NJ: John Wiley & Sons, Inc; 2006. [Google Scholar]
- Chilcoat HD, Breslau N. Posttraumatic stress disorder and drug disorders: testing causal pathways. Archives of General Psychiatry. 1998;55:913–917. doi: 10.1001/archpsyc.55.10.913. [DOI] [PubMed] [Google Scholar]
- Coffey SF, et al. Trauma and substance cue reactivity in individuals with comorbid posttraumatic stress disorder and cocaine or alcohol dependence. Drug and Alcohol Dependence. 2002;65(2):115–127. doi: 10.1016/s0376-8716(01)00157-0. [DOI] [PubMed] [Google Scholar]
- Dick DM, et al. Spit for science: launching a longitudinal study of genetic and environmental influences on substance use and emotional health at a large US university. Frontiers in Genetics. 2014;5:47. doi: 10.3389/fgene.2014.00047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fossos N, et al. Coping motives as a mediator of the relationship between sexual coercion and problem drinking in college students. Addictive Behaviors. 2011;36(10):1001–1007. doi: 10.1016/j.addbeh.2011.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray MJ, et al. Psychometric properties of the life events checklist. Assessment. 2004;11(4):330–341. doi: 10.1177/1073191104269954. [DOI] [PubMed] [Google Scholar]
- Green BL, et al. Effects of adolescent trauma exposure on risky behavior in college women. Psychiatry. 2005;68(4):363–378. doi: 10.1521/psyc.2005.68.4.363. [DOI] [PubMed] [Google Scholar]
- Harris PA, et al. Research electronic data capture (REDCap) — a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kachadourian LK, Pilver CE, Potenza MN. Trauma, PTSD, and binge and hazardous drinking among women and men: findings from a national study. Journal of Psychiatric Research. doi: 10.1016/j.jpsychires.2014.04.018. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaysen D, et al. Incapacitated rape and alcohol use: a prospective analysis. Addictive Behaviors. 2006;31:1820–1832. doi: 10.1016/j.addbeh.2005.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, et al. Posttraumatic stress disorder in the national comorbidity survey. Archives of General Psychiatry. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kessler RC, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, et al. A 2-year longitudinal analysis of the relationship between violent assault and substance abuse in women. Journal of Consulting and Clinical Psychology. 1997;65:834–847. doi: 10.1037//0022-006x.65.5.834. [DOI] [PubMed] [Google Scholar]
- McLeod DS, et al. Genetic and environmental influences on the relationship among combat exposure, posttraumatic stress disorder symptoms, and alcohol use. Journal of Traumatic Stress. 2001;14(2):259–275. doi: 10.1023/A:1011157800050. [DOI] [PubMed] [Google Scholar]
- Messman-Moore TL, Long PJ. The role of childhood sexual abuse sequelae in the sexual revictimization of women: an empirical review and theoretical reformulation. Clinical Psychology Review. 2003;23(4):537–571. doi: 10.1016/s0272-7358(02)00203-9. [DOI] [PubMed] [Google Scholar]
- Mouilso ER, Fischer S, Calhoun KS. A prospective study of sexual assault and alcohol use among first-year college women. Violence and Victims. 2012;27(1):78–94. doi: 10.1891/0886-6708.27.1.78. [DOI] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus User’s Guide. 7. Los Angeles, CA: Muthen & Muthen; 1998–2012. [Google Scholar]
- O’Hare T, Sherrer M. Drinking motives as mediators between PTSD symptom severity and alcohol consumption in persons with severe mental illnesses. Addictive Behaviors. 2011;36(5):465–469. doi: 10.1016/j.addbeh.2011.01.006. [DOI] [PubMed] [Google Scholar]
- O’Malley PM, Johnston LD. Epidemiology of alcohol and other drug use among American college students. Journal of Studies on Drugs and Alcohol. 2002;14:23–39. doi: 10.15288/jsas.2002.s14.23. [DOI] [PubMed] [Google Scholar]
- Prins A, et al. The primary care PTSD screen (PC-PTSD): development and operating characteristics. Primary Care Psychiatry. 2003;9:9–14. [Google Scholar]
- Read JP, et al. Trauma and posttraumatic stress symptoms predict alcohol and other drug consequence trajectories in the first year of college. Journal of Consulting and Clinical Psychology. 2012;80(3):426–439. doi: 10.1037/a0028210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read JP, Wardell JD, Colder CR. Reciprocal associations between PTSD symptoms and alcohol involvement in college: a three-year trait-state-error analysis. Journal of Abnormal Psychology. 2013;122(4):984–997. doi: 10.1037/a0034918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Testa M, Livingston JA, Leonard KE. Women’s substance use and experiences of intimate partner violence: a longitudinal investigation among a community sample. Addictive Behaviors. 2003;28(9):1649–1664. doi: 10.1016/j.addbeh.2003.08.040. [DOI] [PubMed] [Google Scholar]
- Waldrop AE, et al. Triggers for cocaine and alcohol use in the presence and absence of posttraumatic stress disorder. Addictive Behaviors. 2007;32(3):634–639. doi: 10.1016/j.addbeh.2006.06.001. [DOI] [PubMed] [Google Scholar]
- Xian H, et al. Genetic and environmental influences on posttraumatic stress disorder, alcohol, and drug dependence in twin pairs. Drug and Alcohol Dependence. 2000;61(1):95–102. doi: 10.1016/s0376-8716(00)00127-7. [DOI] [PubMed] [Google Scholar]