INTRODUCTION
Carl Zeiss was the first company to commercially introduce a fundus camera in 1926 with a 20-degrees field of view1. As technology evolved, 30-degrees became the standard field of view in ophthalmology, and now fundus cameras, which use up to 50–55 degrees fields of view are widely used in clinical practice. Imaging angles or views wider than 50-degrees have been referred to as “wide-field” or “wide-angle”1. Recently the term “ultra-wide field” has come to popularity although the exact definition and area of the retina imaged is not clearly defined.
Confocal scanning laser ophthalmoscopy (cSLO) is an imaging technology that uses laser light to raster scan the retina, instead of a bright white flash used in standard fundus cameras, which provides better comfort to the patient. The reflected light is then captured through a small aperture (confocal pinhole) blocking the scattered light, giving a sharp, better quality and high contrast image2. This technology, coupled with a spectral-domain optical coherence tomography (SD-OCT) makes up the multi-modal imaging of the Spectralis HRA+ OCT (Heidelberg Engineering, Carlsbad, CA). It has a replaceable 30 × 30-degrees standard lens and a 55-degrees wide field lens. Recently, the company introduced a noncontact ultra-wide field (UWF) lens system that is capable of imaging from equator to equator and sufficient to image important details in the retinal periphery, such as vascular abnormalities anterior to the equator.
This paper aimed to evaluate the quality and usability of Heidelberg Engineering’s recent addition of the noncontact ultra wide field lens system to image retinal and choroidal pathology, especially those in the mid and far periphery using different imaging modalities, namely, fundus autofluorescence (FAF), fluorescein angiography (FA), and indocyanine green angiography (ICGA).
METHODS
This was a retrospective review of images taken using a confocal scanning laser ophthalmoscope coupled with an SD-OCT device (Spectralis HRA+ OCT, Heidelberg Engineering) from October 2013 to January 2014) at the Jacobs Retina Center, University of California San Diego (UCSD) Shiley Eye Institute. Written informed consent was obtained for each patient. Institutional Review Board (IRB) approval was acquired for the review and analysis of patient data and images.
A total of 58 eyes underwent imaging using the Spectralis HRA+ OCT ultra-wide field noncontact lens, in addition to the standard 30 × 30-degrees lens and the 55-degrees wide-angle lens. Central images were initially obtained centered on the fovea. Views of the far periphery were obtained in the areas of interest, by directing the camera (non-contact) in the appropriate direction. Imaging modalities taken simultaneously were fluorescein angiography (FA) and indocyanine green angiography (ICGA)3. Two experienced observers masked to the diagnoses evaluated and compared images taken by the three different lenses. We used fundus landmarks to determine the size of the ultra-wide field imaging lens. We measured retinal landmarks in a 30-degrees fundus image in horizontal and vertical direction. We determined the size of the landmarks in degrees. Subsequently, we measured the same landmarks in the ultra-wide field image and extrapolated the size of the entire image.
RESULTS
58 eyes were evaluated. Using directional ultra-wide field view and montaging software, we could image the retina up to a diameter of 28mm allowing a field of view to include the equator and some structures anterior to it. In the montage image of the periphery, we were able to image 135 degrees horizontally and 129 degrees vertically. The native resolution of 1,536x1,536 was sufficient to see important retinal details including vascular abnormalities like peripheral and macular retinal neovascularizations, areas of nonperfusion, CME and disc leakage in patients with CRVO and BRVO (figure 1). Macular and peripheral microaneurysms in patients with diabetic retinopathy (figure 2). When centered on the fovea, we were able to identify the source of leakage in a CSR patient (figure 3) and on ICG we were able to identify the temporal vortex veins (figure 4). In patients with age related macular degeneration we were able to demonstrate dye leakage in the fovea on UWF image that is comparable to the 30-degrees image on late phase (figure 5).
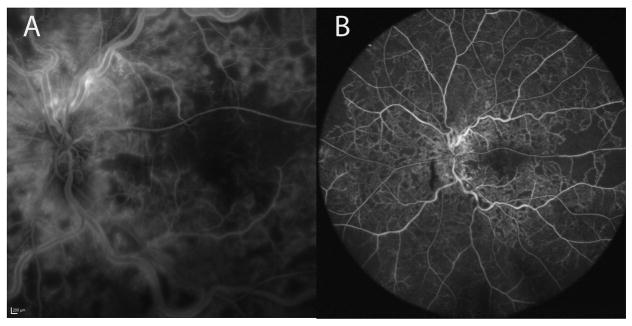
Figure 1.
A. 30-degrees image of the left macula showing disc leakage, venous tortuosity, macular edema and areas of non-perfusion of a CRVO patient. B. UWF image of the same patient showing identifiable disk leakage, macular edema, numerous areas of non-perfusion and venous tortuosity.
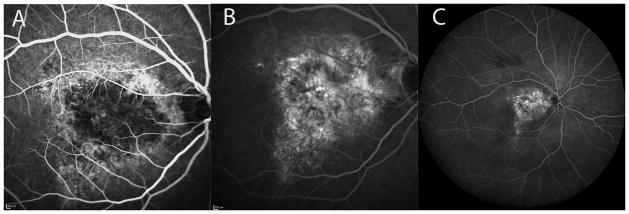
Figure 2.
A. 55-degrees image of the right eye showing retinal neovascularization, microaneurysms, DME and some laser burns in diabetic retinopathy. B. UWF image of the same patient showing identifiable retinal neovascularization both macular and nasal, microaneurysms, DME and laser burns.
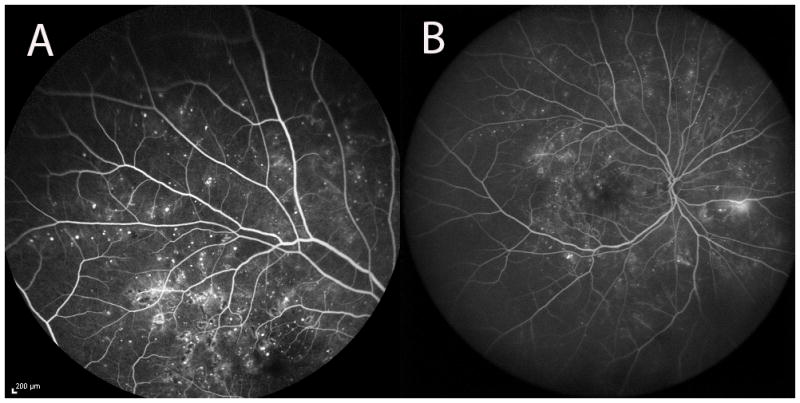
Figure 3.
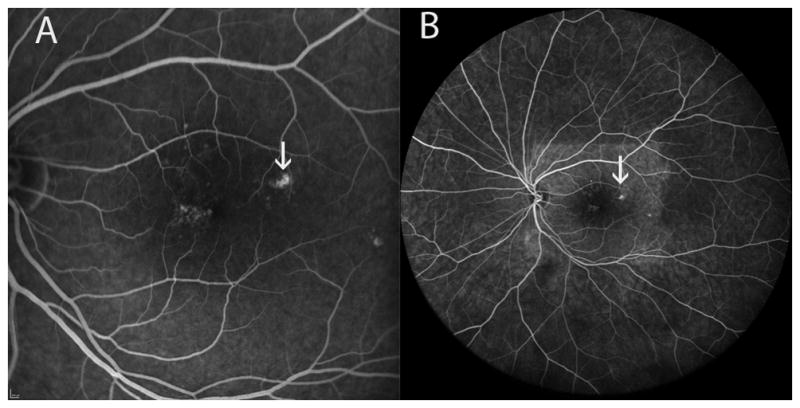
Comparing images from 30-degrees (A) and UWF image (B) we were able to identify the source of leakage in a patient with CSR on the UWF image. Note on image B the rectangular hyperfluorescent shape over the macula-this is the area of the 30-degrees FA image taken before the UWF image.
Figure 4.
ICG image of the left eye in a patient with choroidal nevus showing the temporal vortex veins.
Figure 5.
A and B images are early and late phase, respectively, 30-degrees images of the right eye in a patient with Wet AMD showing late phase leakage. C. UWF late phase image of the same patient demonstrating leakage as seen in 30 × 30-degrees image.
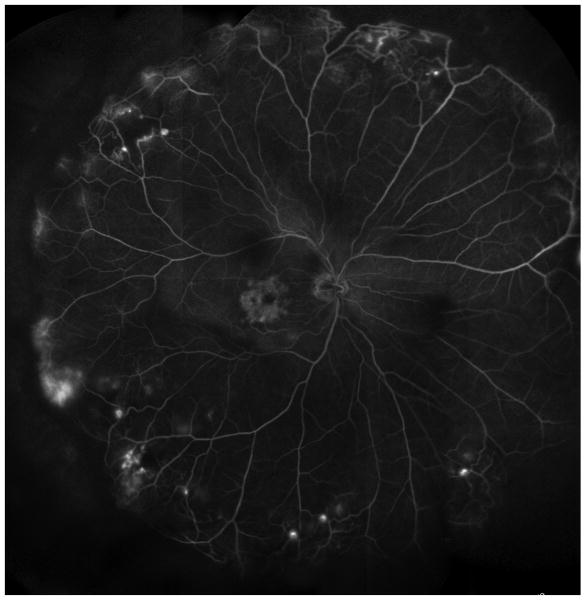
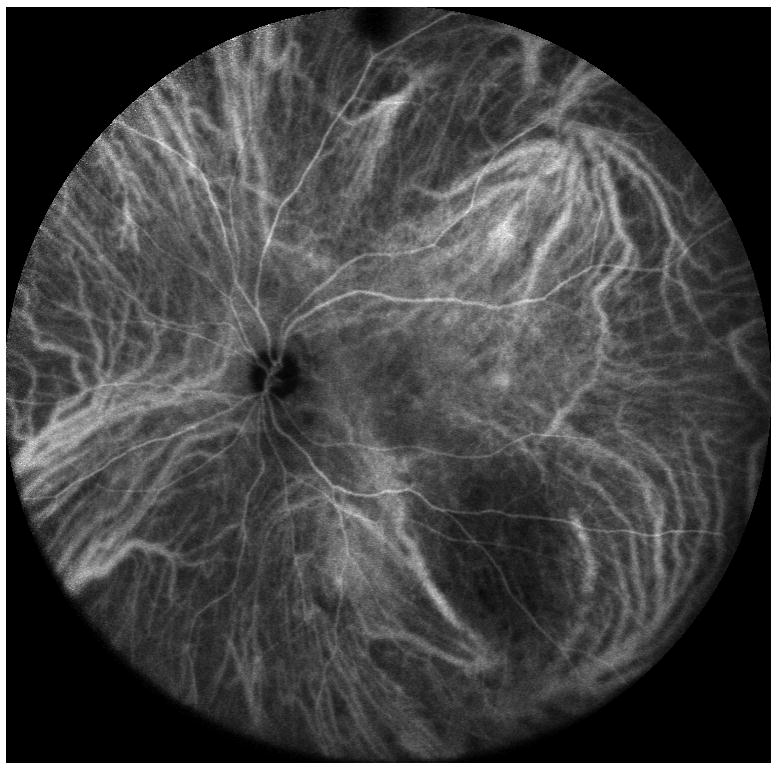
(figure 6) Montage image using directional UWF view of the right eye of a 44-year-old patient showing telangiectasia of the peripheral vessels anterior to the equator with areas of non-perfusion, leakage and CME.
Figure 6.
Montage image using the UWF lens showing 344.65 mm2 of retinal area including telangiectasia of the peripheral retinal vessels with areas of non-perfusion, leakage and CME.
In table 1 using a p-value <0.1, we found that the 102 degrees lens (ultra-wide field) is inferior to the 30 degrees lens in detecting subfoveal CNV and inferior to both 30 and 55 degrees lenses in detecting drusen with high inter-observer agreement. The rest of the statistics shows 102 degrees lens was either equivocal or not inferior (no statistical difference) to both 30 × 30 and 55-degrees lenses with high to perfect inter-observer agreement.
Table 1.
| 55 degree McN p-value (Kappa) | 102 degree McN p-value (Kappa) | |
|---|---|---|
| Subfoveal CNV 30 deg 55 deg |
NDP (1.0) | 0.06 (0.80) 0.50 (0.65) |
| Macular DBH 30 deg 55 deg |
0.50 (0.65) | 0.50 (0.65) NDP (1.0) |
| Peripheral DBH 30 deg 55 deg |
NDP (1.0) | 0.50 (0.73) 0.50 (0.73) |
| Disc Edema 30 deg 55 deg |
NDP (1.0) | NDP (1.0) NDP (1.0) |
| Drusen 30 deg 55 deg |
NDP (1.0) | 0.00(0.72) 0.06 (0.69) |
| GA 30 deg 55 deg |
NDP (1.0) | NDP (1.0) NDP (1.0) |
| CSR hot spot 30 deg 55 deg |
NDP (1.0) | NDP (1.0) NDP (1.0) |
| Microaneurysm 30 deg 55 deg |
NDP (1.0) | 1.00 (0.95) 1.00 (0.94) |
| Macular Edema 30 deg 55 deg |
NDP (1.0) | 0.13 (0.85) 0.25 (0.86) |
| Macular Ischemia 30 deg Peripheral Ischemia 55 deg |
1.00 (0.94) | 1.00 (0.88) 1.00 (0.94) |
| NVD and NVE 30 deg 55 deg |
NDP (1.00) | NDP (1.00) NDP (1.00) |
| Peripheral vasculitis 55 deg | 0.50 (0.48) |
(deg-degrees, NDP – No Discordant Pair)
An advantage of using the Spectralis over a dedicated wide angle device, like the Optos UWF SLO produtcs, is that higher resolution image of an area of interest can be obtained by switching to the standard Spectralis 30-degrees lens (5 microns/pixel) versus the lower nominal resolution of the usable 55-degrees wide-angle lens of the Spectralis (10 microns/pixel) or Optos (14 microns/pixel on standard view and 11 microns/pixel on high-resolution view) system lenses. The lens could be used for oral2 or intravenous fluorescein angiography and other imaging modalities. Both instruments allow to zoom and pan through the image content at higher magnification or zoom level. The Spectralis software allows a zoom level of up to 8x. Overall image size is only limited by the size of the monitor used to view the images and can vary between systems.
DISCUSSION
Images taken from Ultra-wide field noncontact lens system of Heidelberg Spectralis permits a 102 degrees field of view which can be used in a directional manner to image the far periphery and montaged4 to cover equator to equator of the retina or in our experience a 135 degrees field of view of the retina or 344.65 mm2 of retinal area. The device allows for AF, IR, IVFA, Oral FA and ICG ultra-wide field views enabling visualization and localization of important choroidal and retinal structures from equator to equator. Optos-type scanning laser ophthalmoscopes claims to image 200 internal degrees of the retina. Standard ophthalmic imaging devices measure the external angle of light incident on the pupil to express field of view. Optos is the only device using an internal angle of view centered on the center of curvature of the eye. In order to compare the field of view of the Optos SLO to conventional fundus cameras, we have to convert the internal field of view angle to the external field of view angle. Using the formula by Atkinson and Mazo5 the Optos SLO has an equivalent external field of view angle of approximately 135 degrees.
Witmer and colleagues compared the Optos instrument to the ultra-widefield lens of the Spectralis SLO. They measured the number of pixel in each image. However, such a comparison does not accurately estimate the field of view covered by the device. They did make a notation in each image to the largest extent of the retinal vasculature in each quadrant of the image. They noted that the Spectralis UWF lens allowed more distal visualization in the superior and inferior direction, while the Optos SLO allowed more distal visualization in the nasal and temporal quadrant1. However, this extent was not quantified. This is not surprising, as the aspect ratio of the Optos SLO image is rectangular while the Spectralis UWF lens image is a perfect circle. In contrast to the methods by Witmer and colleagues, in our study we measured the extent of visualization based on imaging landmarks.
We use directional imaging with 55 degrees lens for certain retinal diseases to view the peripheral retina, with 102 degrees UWF lens this was detected and documented with no difficulty and the detail was clear enough to make the conclusion or diagnosis. 102 degrees UWF lens is good for screening except for evaluating subfoveal CNV and drusen. Evaluating for subfoveal CNV and drusen should be done using a higher magnification lens system. FAF with UWF lens, in our experience, did not give a very informative picture and was not evaluated further.
Wide-field fundus imaging can be done with a dedicated ultra wide-field camera system (Optos), using an accessory lens to expand the imaging field of a standard noncontact fundus camera or SLO6 or with a confocal SLO with a noncontact ultra-wide field lens system. The latter can be directed to the far peripheral retina and montage images to create, in our experience, a 135 degrees field of view of the retina with the Spectralis UWF lens system. The advantage of this lens system is it can easily be switched for a higher resolution lens system (30-degrees and 55-degree) for areas of special interest. While both Optos and Spectralis systems are able to take simultaneous FA and ICG images without manually switching between imaging modalities, the Spectralis UWF lens system does not give a good FAF image but has excellent 30-degrees and 55-degrees FAF images. UWF imaging modalities understandably increases the field of view of the far peripheral retina as reported by Wessel et al7. They found that UWF imaging shows 3.2 times more total retinal area than the seven standard field (7SF) developed by the Diabetic Retinopathy Study8. In this study by Wessel, they used the Optos device and reported capturing 3.9 times more area of non-perfusion, 1.9 times more area of NV, 3.8 times more area of laser burns (pan retinal photocoagulation) than that of 7SF. As stated earlier, the Optos captures around 135 degrees field of view when converted to the more common way of measuring standard ophthalmic imaging devices, which is the same with Spectralis UWF lens system using a directional imaging system and montaging.
Acknowledgments
Funding/Support: This study was supported by NIH grants R01EY007366, R01EY018589, R01EY016323 (DUB) and NEI vision core grant P30EY022589, and Research to Prevent Blindness. The funding organizations had no role in the design or conduct of this research.
Footnotes
Financial Disclosures:
No applicable financial disclosures.
References
- 1.Matthew T, Witmer MD, Szilárd Kiss MD. Wide-field Imaging of the Retina. Survey of Ophthalmology. 2013 Mar-Apr;58:143–154. doi: 10.1016/j.survophthal.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 2.Garcia CR, Rivero ME, Bartsch D-U, et al. Oral Fluorescein Angiography with the Confocal Scanning Laser Ophthalmoscope. Ophthalmology. 1999;106(6):1114–8. doi: 10.1016/S0161-6420(99)90264-6. [DOI] [PubMed] [Google Scholar]
- 3.Freeman WR, Bartsch D-U, Mueller AJ, et al. Simultaneous Indocyanine Green and Fluorescein Angiography Using a Confocal Scanning Laser Ophthalmoscope. Archives of Ophthalmology. 1998;116(4):455–463. doi: 10.1001/archopht.116.4.455. [DOI] [PubMed] [Google Scholar]
- 4.Rivero ME, Bartsch DU, Otto T, Freeman WR. Automated scanning laser ophthalmoscope image montages of retinal diseases. Ophthalmology. 1999 Dec;106(12):2296–300. doi: 10.1016/S0161-6420(99)90529-8. [DOI] [PubMed] [Google Scholar]
- 5.Atkinson A, Mazo C. Imaged Area of the Retina. www.optos.com/global/documents/casestudies_imagedareaoftheretina.pdf.
- 6.Staurenghi G, Viola F, Mainster MA, et al. Scanning laser ophthalmoscopy and angiography with a wide-field contact lens system. Arch Ophthalmol. 2005 Feb;123(2):244–52. doi: 10.1001/archopht.123.2.244. [DOI] [PubMed] [Google Scholar]
- 7.Wessel MM, Aaker GD, Parlitsis G, et al. Ultra-wide-field angiography improves the detection and classification of diabetic retinopathy. Retina. 2012 Apr;32(4):785–91. doi: 10.1097/IAE.0b013e3182278b64. [DOI] [PubMed] [Google Scholar]
- 8.Diabetic Retinopathy Study Research Group. Design methods and baseline results. DRS report no 6. Invest Ophthalmol. 1991;21:149–209. [Google Scholar]