Abstract
Objective
To develop an expandable knowledge base of reusable knowledge related to self-management of diabetes that can be used as a foundation for patient-centric decision support tools.
Materials and methods
The structure and components of the knowledge base were created in participatory design with academic diabetes educators using knowledge acquisition methods. The knowledge base was validated using scenario-based approach with practicing diabetes educators and individuals with diabetes recruited from Community Health Centers (CHCs) serving economically disadvantaged communities and ethnic minorities in New York.
Results
The knowledge base includes eight glycemic control problems, over 150 behaviors known to contribute to these problems coupled with contextual explanations, and over 200 specific action-oriented self-management goals for correcting problematic behaviors, with corresponding motivational messages. The validation of the knowledge base suggested high level of completeness and accuracy, and identified improvements in cultural appropriateness. These were addressed in new iterations of the knowledge base.
Discussion
The resulting knowledge base is theoretically grounded, incorporates practical and evidence-based knowledge used by diabetes educators in practice settings, and allows for personally meaningful choices by individuals with diabetes. Participatory design approach helped researchers to capture implicit knowledge of practicing diabetes educators and make it explicit and reusable.
Conclusion
The knowledge base proposed here is an important step towards development of new generation patient-centric decision support tools for facilitating chronic disease self-management. While this knowledge base specifically targets diabetes, its overall structure and composition can be generalized to other chronic conditions.
Keywords: Diabetes mellitus (C18.452.394.750), Knowledge bases (L01.224.065.480), Decision-support systems(L01.700.508.300.190), Community-based participatory research (H01.770.644.193)
1. Introduction
Diabetes is an epidemic that currently affects more than 8% of the United States population, with disadvantaged and ethnic minority groups at greater risk for incidence and poorer outcomes [1–5]. Self-management is critical for those living with diabetes [6–8]; there is strong evidence that self-management can help patients to optimize metabolic control, prevent and manage complications, and improve quality of life and clinical outcomes in a cost-effective manner [9,10]. Problem solving is a fundamental skill in diabetes self-management [11], with considerable evidence for its positive impact on self-management behaviors and glycemic control [12]. Yet engaging in effective self-management and developing robust problem-solving skills is challenging [13]. It is documented that 50–80% of adults with diabetes have significant knowledge and skill deficits [14].
Informatics tools can help individuals and their healthcare providers make complex decisions regarding both medical treatment strategies and self-care [15, 16]. Clinical decision support (CDS) tools are increasingly becoming the standard of care and an integral part of electronic health records (EHR) [17, 18]. In the context of diabetes care and management, clinician computerized decision support tools (CCDS) traditionally aid practitioners by facilitating adherence to current diabetes care guidelines via prompts and reminders [19–21], providing recommendations for medication based on patient-specific data [3], and facilitating patient clinician shared clinical decision-making in regards to choice of treatment using communication and/or visual aids [21–26]. Patient computerized decision support (PCDS) target patients rather than clinicians. PCDS tools in diabetes have been used to provide patients with real time feedback on physiological data (e.g., blood glucose), make recommendations regarding medication and insulin regimen, encourage adherence to self-care behaviors, and provide motivation along with strategies for addressing barriers to lifestyle changes [27–32]. Notably, PCDS tools are different from other self-management tools that mostly focus on diabetes self-monitoring and do not provide any decision support. In addition to these, there are several examples of electronic interventions that more directly target problem solving. For example, Glasgow et al. [8, 33] utilized a CD-ROM application that specifically focused on problem solving and self-efficacy. This study compared theory-based tailored self-management (TSM) to computer-aided enhanced usual care (UC) and found that the TSM led to significantly more weight loss and behavior changes than the UC.
One of the necessary components of any decision support tool is the availability of formalized and computable knowledge related to the clinical domain of interest. In the context of clinician-centric tools, this knowledge usually includes clinical guidelines [18]. In the case of diabetes, there are several examples of diabetes-specific guidelines and ontologies [34–37]. In the context of patient-centric tools, however, this knowledge usually resides in the minds of practicing diabetes educators, who assist with diabetes self-management. While many of the patient-centric interventions for diabetes problem solving and decision support described above include consistent types of knowledge structures (e.g., common barriers to lifestyle changes, goals for diabetes self-management, problem-solving strategies for behavior change, and motivation to persist with behavior changes [8,29,38–41]) few of them present any formal ontology-based organization of knowledge.
The project described in this paper is the first step in a comprehensive research program to develop and evaluate new generation informatics interventions for facilitating problem solving in diabetes self-management. The first step of this research was to develop a formal organization of diabetes-specific self-management knowledge that could serve as a foundation for such interventions. The knowledge needed to be nuanced enough to facilitate such daily self-management behaviors as choosing meals and exercise, and account for common barriers to engaging in these behaviors. It was important that the knowledge base is culturally and linguistically sensitive, and accounts for differences in individuals’ levels of literacy, current behaviors, and preferences regarding these behaviors. In the following sections we outline the participatory design process utilized for the development of the knowledge base, describe its essential components, and discuss results of a validation study with practicing diabetes educators and individuals with diabetes recruited from Community Health Centers in New York City.
2. Materials and methods
2.1. Settings
This work was conducted in collaboration with Clinical Directors Network [42], a well-established primary care practice-based research network (PBRN), and conducted with two CDN-member Health Centers (Morris Heights Health Center, Bronx, NY and Joseph P. Addabbo Health Center, Queens, NY), both of which are Federally Qualified Health Centers (FQHCs) funded by Health Resources and Services Administration (HRSA) [43]. Morris Heights Health Center (MHHC) has had a record of distinction as the major provider of health care to Morris Heights and the surrounding areas of the Bronx since 1981. MHHC provides quality primary healthcare services to all members of the community, including the medically, socially and economically disadvantaged—from medical and dental services to counseling. Morris Heights Health Center is recognized as a Level III Patient Centered Medical Home by the National Committee for Quality Assurance (NCQA) and is accredited by the Joint Commission. MHHC currently serves more than 48,000 patients annually.
The Joseph P. Addabbo Family Health Center, Inc. was established in 1987 and provides comprehensive health services to the poor, the medically indigent and/or medically underserved residents in the county of Queens, New York. The Health Center is licensed by the State of New York as an Article 28 Diagnostic and Treatment Center (DT + C) and has recently received certification as a NCQA Level 3-Medical Home.
2.2. Participants
Both Columbia University’s and Clinical Directors Network’s Institutional Review Boards reviewed and approved the study.
In order to ensure that the knowledge base includes the most current evidence in regards to diabetes self-management, our research team included two academic diabetes educators (ADEs); one was trained as a nurse, and the other a registered dietitian (A.S. and T.D.). Both have extensive practice and research experience in diabetes education. These educators served as domain experts in the development of the knowledge base.
Practicing diabetes educators (PDEs) were recruited from the clinical staff of the participating FQHCs; all participants were professionally trained as nurses or nutritionists; all were AADE-certified diabetes educators and had at least 6 months of experience delivering group or individual diabetes education. The terms ADE and PDE are used in the context of this paper simply to differentiate between those diabetes educators that participated in development of the knowledge base as a member of the research team (ADE) and those who participated in validation of the knowledge base as a practitioner in the FQHCs (PDE).
Individuals with diabetes were recruited using the following inclusion criteria: (1) age between 18 and 65 years; (2) a diagnosis of type 2 diabetes; (3) proficiency in either English or Spanish. We excluded women with gestational diabetes and individuals who had serious illness (e.g., cancer diagnosis with active treatment, advanced stage heart failure, multiple sclerosis identified in their patient chart) or cognitive impairment. The practicing diabetes educators and individuals with diabetes were recruited from the same two participating FQHCs.
2.3. Knowledge base development
The knowledge base described in this paper was developed using a combination of inductive and deductive methods. Inductively, the research team utilized a participatory design approach that involved experienced diabetes educators and individuals with diabetes. This inductive, exploratory approach allowed the research team to observe and identify knowledge utilized by diabetes educators in guiding their patients; the knowledge elements discovered through this inductive approach are based on the everyday lives of people living with diabetes and the health professionals who support them. Deductively, it was grounded in a framework of problem-solving in diabetes proposed by Hill-Briggs [21] and supported by guidelines and recommendations for diabetes self-management and education from the American Diabetes Association (ADA) and American Association of Diabetes Educators (AADE) [9,37,44,45]. Specifically, we used this approach to evaluate the structure and content of the emerging knowledge base on its consistency with the problem-solving framework and its components and with the existing guidelines. Our particular focus in this work was on individuals with diabetes from economically disadvantaged areas and representatives of ethnic minorities—those at increased risk for diabetes.
During the knowledge base development, knowledge engineers on the research team (H.C. and L.M.) held 4 initial 1 h long knowledge acquisition working sessions with ADEs to capture the practical knowledge experts gained through years of advising individuals with diabetes. Using think-aloud methods, domain experts discussed typical problems their patients encountered in their daily lives, and the information they used to help their patients engage in problem-solving. The research team used these initial sessions to identify basic knowledge components and develop a model of knowledge related to problem solving. The model was refined after comparing it with those existing in the literature on diabetes problem-solving. After the initial sessions, ADEs continued to complete the individual knowledge components according to the model using structured knowledge acquisition documents. Working group sessions were used to discuss and form consensus on the information provided by the ADEs. This process was repeated multiple times throughout the project (at least bi-weekly over a 4-month period) until both domain experts and knowledge engineers were satisfied that the process had yielded a knowledge base that was representative of the information needed to support an individual patient’s problem-solving in diabetes self-management.
2.4. Knowledge base validation
The resulting knowledge base was evaluated on a set of criteria typical for evaluation of formal representations of knowledge. The criteria included its domain accuracy, completeness, appropriateness, and clarity. Table 1 includes the evaluation criteria and their target audience used for evaluation.
Table 1.
Measures of evaluation for the knowledge base.
| Metric | Key question to assess the metric | Assessed by |
|---|---|---|
| Domain accuracy | Is the diabetes specific information in the knowledge base correct? | Practicing diabetes educators |
| Completeness | Is the information in the knowledge base representative of the full range of knowledge that exists on this topic? | Practicing diabetes educators |
| Appropriateness | Is the information presented in the knowledge base relevant and useful? | Patients |
| Clarity | Is the information in the knowledge base presented in a concise manner that is easy to comprehend? | Patients |
Domain accuracy and completeness of knowledge base. To evaluate domain accuracy and completeness of the knowledge base, researchers held two separate focus groups with 8 practicing diabetes educators at the participating FQHCs. Practicing diabetes educators were different from the academic diabetes educators used to build the knowledge base and did not participate in its initial development. Each focus group lasted for 1.5 h and included 4 practicing diabetes educators. During each session, practicing diabetes educators were presented with case-scenarios based on selected glycemic patterns and asked to illustrate how they would help a patient to problem-solve around these patterns. This included the discussion of potential causes (behavioral triggers) and recommendations (action-oriented goals). All solutions and knowledge components mentioned by the PDEs were recorded on flipcharts and later transcribed into digital form. Next, the PDEs reviewed the knowledge elements in the knowledge base and assessed them for accuracy and completeness. Finally, the PDEs were asked to identify any knowledge elements that were missing.
Appropriateness and clarity of knowledgebase. To assess appropriateness and clarity of the knowledge in the knowledge base and its potential acceptance by individuals with diabetes (patients), researchers conducted 5 semi-structured interviews with individuals with diabetes recruited from the participating FQHCs. Each patient was interviewed separately. All interviews lasted for 1 h each.
Patients were presented with case-based scenarios that included a variety of conditions or symptoms a person living with diabetes might experience. The scenarios were informed by our previous qualitative studies with the same patient populations and were culturally and socially tailored to the participating communities. Patients were directed through the information the knowledge base would provide in response to these scenarios for solving a specific diabetes management related problem. Patients were asked questions about whether they found the information to be interesting and relevant in the context of their lives, as well as if they felt the information was easy to understand and presented in a logical order.
2.5. Data analysis
Validation of the knowledge base according to the metrics described in Section 2.4 was conducted using applied thematic analysis. Data from all focus groups with practicing diabetes educators were compiled to create one dataset to assess domain accuracy and completeness of the knowledge base and data from semi-structured interviews with patients were combined to create a second dataset to assess appropriateness and clarity. Focus groups and interviews were not audio recorded, in order to avoid inhibiting any free exchange, especially given that diabetes educators were providing information at their place of employment and patients were providing personal information in a setting in which they receive healthcare; instead two interviewers took extensive field notes, a methodology that has been proven to be effective in situations where audio or video recording is not ideal [46]. In addition, the researchers used flipcharts to record all comments and recommendations made by diabetes educators during the focus groups. After each validation session, researchers transferred all comments and recommendations into their respective datasets.
After all data were collected, researchers conducted applied thematic analysis, following an inductive methodology described by Guest et al. [47]. Two researchers, (LM and HC) first independently reviewed all data for familiarization and then independently reviewed a second time to identify emerging themes, after which they met to cross-reference themes and agree on final themes. Themes identified are presented in section 3.3, expressed as recommendations for improvement of the knowledge base.
3. Results
The goal of this study was to develop a knowledge base that could be used for the design of informatics tools for facilitating problem-solving in diabetes self-management and to validate the knowledge base for accuracy, completeness, appropriateness, and clarity.
3.1. Diabetes problem-solving knowledge base
As a result of the activities described above (Section 2), the researchers identified four main knowledge elements that are fundamental to problem-solving in diabetes self-management. Table 2 provides examples of information provided for each knowledge type.
Table 2.
Knowledge types represented in knowledgebase.
| Knowledge Type | Definition | Example |
|---|---|---|
| Problem patternsa | Patterns of high and low values for blood glucose necessary in order for patients to know what blood glucose values are problematic and could benefit from problem solving. | High after breakfast blood glucose value |
| Behavioral triggersa | Behaviors that may be related to the observation of high or low blood glucose patterns. | I often eat high fat foods for breakfast |
| Contextual education | Information about how each of the behavioral triggers is related to blood glucose patterns, provided in the context of the blood glucose problem pattern chosen (e.g., time of day, proximity to meal). This information helps the patient to understand why this particular behavior matters to the blood glucose values they have observed. | Foods like bacon and sausage and fried foods like hash brown potatoes are high in fat. High fat foods delay the digestion of food. As a result, you can have high blood sugar many hours after breakfast. Reduce fat in your diet to help your body return to normal blood sugar levels faster. |
| Motivational messages serve the purpose of encouraging patients to continue to engage in problem solving and feel empowered to consider the information in the context of their lives and explore to continue to understand how their body deals with diabetes. | Think about ways you can incorporate this into your lifestyle. | |
| Action-oriented recommendationsa | Action-oriented recommendations that provide the patient with options for how they can change behavior related to a specific problem with observed blood glucose values. | If the morning is a busy time of day for you, prepare hard-boiled eggs in advance. They are quick, nutritious and delicious. |
| Plan ahead for times that you eat out. Choose low fat breakfast protein such as low fat cheese or a boiled egg. Or, add other foods that are high in fiber, like berries and apples. | ||
| Try to reserve high fat foods for special occasions. When you eat them, try to reduce your portion size. | ||
| Try to have protein that is low in fat for breakfast. Choose turkey sausage instead of bacon or roasted potatoes instead of fried potatoes. | ||
| If your breakfast options are limited, reduce your portion size and add foods high in protein and fiber. For example add some nuts and berries to your breakfast. |
Indicates a knowledge category where a patient is presented with a range of options. The subsequent information is relevant to the decisions made at each decision point.
3.1.1. Glycemic problem patterns
Consistent with previous research, knowledge acquisition activities with academic diabetes educators suggested that much of problem-solving in diabetes self-management is triggered by undesirable patterns in blood glucose reading. These patterns are systematic and are based on blood glucose averages at a specific time point, for example before breakfast, across several days, rather than on an individual reading. Patterns are bi-directional as they can be either above or below the recommended target range. Finally, they are context-specific as they depend on the time of day and the activities that preceded them (e.g., the recommended ranges differ for fasting blood glucose (BG) values and BG values recorded after meals). We identified eight common problem patterns that corresponded to times of day when individuals typically test their BG: upon waking, before and after each meal (i.e., break-fast, lunch, dinner), and before bedtime.
3.1.2. Behavioral triggers
Once the problematic patterns are identified, a critical step in the problem-solving process is development of connections between individuals’ activities (such as meals and exercise) and corresponding changes in BG values. These connections emerge as individuals reflect on their past behaviors and compare them with their self-management goals. To facilitate this process, diabetes educators often prompt individuals with questions that address these possible behaviors. For example, for somebody who is experiencing a systematically high blood glucose readings after break-fast, the questions might focus on timing and composition of their breakfast (e.g., “Do you usually include protein in your breakfast?”), amount and quality of sleep, general well being, adherence to the prescribed medication regimen, and timing and composition of an evening meal. These possible reasons were included in the knowledge base as “Behavioral triggers” and organized into four categories: nutrition, physical activity, medication related (e.g., forgot to take a scheduled medication dose), and other lifestyle factors (e.g., sleep, stress). Three of these categories (nutrition, physical activity, and medication) are consistent with the behaviors required for problem-solving in diabetes management proposed by other researchers [21]. The last category—lifestyle, was added to include behaviors related to sleep, stress, and other factors that can influence blood glucose. Because it is possible that one behavioral trigger can be related to altered blood glucose values at different time points, the knowledge base allows for non-linear relationships (one-to-many and many-to-one correspondence) between problems and behavioral triggers.
3.1.3. Contextual education
While the main focus of problem solving is introducing behavioral adjustments that address specific problems, it has a secondary goal of helping individuals to develop a deeper understanding of their diabetes and blood glucose control—its physiology, the dynamics of insulin production, and the impact of different behaviors on blood glucose levels. When education messages are presented at the moment when individuals are actively engaged in problem-solving, and are tailored to the specific problem in a just-in-time manner, individuals are more likely to internalize what they have learned, than if it were presented through generic didactic lectures [48]. Contextual education was developed as a set of short (3–4 sentences) explanations tailored to the specific problem and behaviors.
During knowledge acquisition, our research team observed that diabetes educators often provide motivation and social support to their patients in tandem with more technical and clinical information. Thus, motivational messages were explicitly defined as a subcategory of contextual information. These messages were included in the knowledge base to encourage patients’ continuing engagement in problem solving and help them feel empowered to use their new knowledge in the context of their lives and explore how their body works to regulate blood glucose levels.
3.1.4. Action-oriented recommendations
Finally, for each behavioral trigger, the knowledge base included a set of choices for alternative behaviors that could lead to improvement in blood glucose readings. Domain experts emphasized that this information must be action-oriented, in order to help the patient determine exactly what new behavior to adopt. In addition, they suggested the importance of personal choice and flexibility. As a result, for each behavioral trigger, the knowledge base included two to five distinct options that individuals could select from. Importantly, because of our focus on economically disadvantaged populations, the action-oriented recommendations include not only positive self-management behaviors, but also suggestions for overcoming common barriers to engaging in such behaviors. For example, instead of suggesting “Include more vegetables”, the knowledge base includes such recommendations as “Include a side vegetable with every lunch. Make sure it covers half of your plate. For example, add a cup of steamed frozen vegetables and a salad.”
Each data category is an extension of the general theoretical model of problem-solving.
3.2. Theoretical orientation of the knowledge base
In addition to the diabetes-specific knowledge base, the problem-solving model of Hill-Briggs identifies three other components of problem solving: (1) problem-solving process, (2) problem-solving orientation, and (3) transfer of past experience. In this section we show how the proposed knowledge base addresses and incorporates these additional components.
3.2.1. Problem-solving process
According to Hill-Briggs [21], problem-solving in diabetes self-management relies on individuals’understanding of problem-solving skills and process. Previous research has proposed five main steps of the problem-solving process: (1) identifying the problem, (2) generating alternative solutions, (3) selecting a solution/decision-making, (4) implementing a solution, and (5) evaluating the outcome [21]. The components of the knowledge base described above (Section 3.1) are consistent with this process; however, they include an additional component—behavioral triggers. These triggers present a link between problematic blood glucose patterns and alternative solutions, as they suggest possible reasons for patterns and narrow down the selection of plausible solutions.
3.2.2. Problem-solving orientation
Problem-solving orientation refers to the way patients feel about problem solving, their self-efficacy and motivation towards problem-solving tasks [21]. Researchers observed that in practice, diabetes educators aid patients in problem-solving by tailoring their education and recommendations to individuals’ current level of knowledge, their current behaviors, and their willingness to change these behaviors. As a result, the knowledge model was designed to support tailored delivery of information. Information in the knowledge base was tailored to support individuals with diabetes having varying levels of (1) nutritional knowledge specific to diabetes, (2) current exercise, (3) current nutrition behavior, (4) motivation to change these behaviors (assessed separately for diet and exercise), and (5) existing diabetes medication regimen. v
3.2.3. Transfer of past experience
While there are direct relationships between specific glycemic patterns and a set of behaviors that may contribute to them, there are many similarities in what causes high or low blood glucose readings at different times of day. For example, if excessive amount of carbohydrates at breakfast may impact blood glucose after break-fast, the effect will be replicated at a lunch that also includes excessive amount of carbohydrates. To facilitate transfer of knowledge between different glycemic patterns, the researchers ensured that the general categories of behavioral triggers and recommendations were consistent throughout the knowledge base.
3.3. Knowledge base validation
Results from the thematic analysis are presented below. Given the purpose of this validation study, themes that emerged from the applied thematic analysis generally included agreement, disagreement, and advice for adaptation of features of the knowledge base (e.g., behavioral triggers, action-oriented goals) as well as personal reflections on how content provided in the knowledge base resonated with life experiences and was easy to understand. Below we discuss these findings including both quantitative assessment (for such criteria as domain accuracy and completeness), and qualitative assessment (for such criteria as appropriateness and clarity of knowledge).
Domain accuracy and completeness of knowledge base. Practicing diabetes educators (PDEs) assessed the knowledge base on its accuracy and completeness using case-scenarios. Overall, PDEs found information presented in the knowledge base to be accurate and similar to the information they provide to their patients in face-to-face encounters. They also found the structure of the knowledge categories to be consistent with their expectations. Additionally, they expressed that relevant thematic concepts were represented. They were particularly pleased to see the category “lifestyle” that included stress and quality of sleep among others, because they felt that these factors are often overlooked.
For the accuracy measures, there were no specific corrections or mentions of inaccurate information in the knowledge base, which led us to conclude that the proposed knowledge base was 100% accurate.
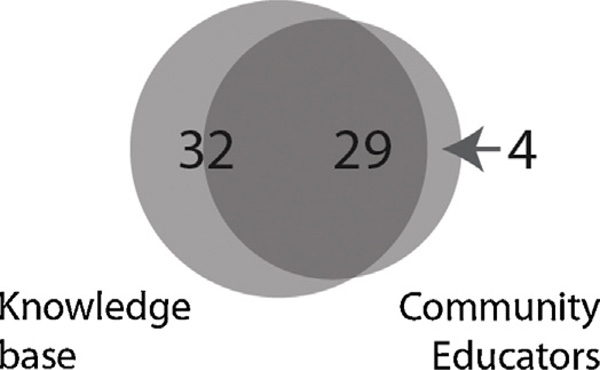
In regards to completeness, for the case-based scenarios, there were 61 total recommendations in the knowledge base; during think-aloud activities, PDEs independently identified 29 of them (46%) (see Fig. 1). Consequently, 54% of the knowledge elements included in the knowledge base were above and beyond topics identified by educators. Of all the recommendations provided by practicing diabetes educators, 12% (4 of 33) were not included in the knowledge base and were thus analyzed by domain experts on the research team for relevance and inclusion in the knowledge base. Educators expressed appreciation that most of the recommendations they could think of had been represented in the knowledge base. They also were in agreement with those recommendations that were in the knowledge base that they did not include on their list.
Fig. 1.
Completeness of the knowledge base: overlap of the recommendations included in the knowledgebase and those identified by diabetes educators during validation of the knowledge base.
In regards to the appropriateness of knowledge elements, PDEs did not find any of them to be inappropriate. However, they provided valuable feedback about how to enhance item readability and cultural sensitivity. Suggestions from PDEs included examples of foods (healthy and unhealthy) that are socially and culturally relevant for the patient population; tips for coping with stress and managing emotional state, encouragement to take small incremental steps for improvement; and ways to address common patient misconceptions.
Appropriateness and clarity of knowledge base. To assess the appropriateness and clarity of the knowledge base, 5 patients (2 black, 3 Latino, mean age 50 years) were presented with case-based scenarios related to the knowledge base as part of their participation in individual semi-structured interviews.
Patients felt the information in the knowledge base was informative and relevant to their daily experience living with diabetes. Users expressed particular appreciation for the variety of choices for glycemic patterns, problematic behaviors that may cause them (behavioral triggers), and goals. Patients reported that seeing new behavioral goals for every glycemic problem helped them to think that these problems were solvable. Patients appeared to have a good understanding of what solutions would be feasible for their situation; however, most expressed an open-minded approach to trying new solutions that they had never previously considered.
Patients found the order in which information was presented to be clear and easy to understand. However, they did make several recommendations for areas of improvement. Specifically, they made recommendations in regards to culturally inappropriate or irrelevant meal choices, and suggested replacing them with more culturally sensitive alternatives. In addition, they recommended including more examples of unhealthy foods, as well as healthy ones. Moreover, the patients recommended including more explicit information on barriers to engaging in healthy behaviors, such as financial considerations, and ways to address them. Finally, they made comments in regards to length and readability of text, particularly within contextual education.
All recommendations were incorporated in the revised version of the knowledge base. In addition, the research team utilized a communications expert to assure that reading comprehension was at a 6–9th grade reading level for all materials. While our original goal was to reach 5th level reading level, inclusion of terms specific to diabetes self-management, such as “diabetes” and “carbohydrate” led to a somewhat higher reading level.
4. Discussion
CCDS tools have become the standard of care and an essential integral part of medicine in the age of Health Information Technologies and electronic health records [17,18]. Multiple studies have shown the benefits of CCDS tools and their impact on patient care [49]. The development of these tools is dependent on availability of systematic, structured, computable knowledge that could be used to assess various clinical scenarios and generate appropriate context-sensitive recommendations [18,50,51]. Although there is a growing number of PCDS tools for self-management of chronic diseases, there have been few attempts to collect, organize, and share knowledge in this arena or to establish a common framework that works across conditions. In the context of diabetes, such knowledge usually resides in the minds of experienced diabetes educators and is a result of their experience helping their patients-solve various problems related to diabetes self-management.
In this project, we took the first step towards developing a formal representation of knowledge required for problem-solving in diabetes self-management. The result is an extensive collection of different problems related to diabetes self-management, particularly to glycemic control, behaviors that commonly contribute to these problems, contextual education that explains the connection between problems and behaviors, and recommendations for alternative behaviors that may improve blood glucose readings. Our reliance on participatory design methods helped to ensure that the knowledge base met our criteria of accuracy, completeness, appropriateness, and clarity. The knowledge base incorporates practice-based knowledge, clinical practice recommendations for diabetes self-management, and theoretical aspects of problem-solving in diabetes self-management. Results of the initial validation with individuals living with diabetes and practicing, community-based diabetes educators suggest that individuals could use the knowledge base to guide problem-solving and decision-making related to the self-management of diabetes, and potentially apply this approach to other chronic diseases that benefit from enhanced levels of patients self-management.
This work has several important implications. First, it can enable the design of a new generation of informatics interventions for facilitating problem-solving in diabetes self-management that incorporate the unique benefits of decision-support tools. Not unlike CCDS tools that rely on clinical ontologies and guidelines for recognizing opportunities for warnings and recommendations in clinical practice, such tools could expand opportunities for delivery of intelligent recommendations based on individuals’ daily blood glucose readings while taking into consideration other factors that my influence patient behaviors. Moreover, such tools can have an additional advantage as they can coach the users in the problem-solving process and acquisition of the skills for problem-solving in diabetes self-management. Furthermore, this knowledge base can open new possibilities for the design of self-monitoring technologies that are particularly popular among supporters of the Quantified Self movement [52]. Specifically it can help both patients and providers to contextualize and analyze the data collected by these technologies (for example, by mapping these data to behavioral triggers in the knowledge base) and translate these data into actionable insights. Finally, the methodology employed in this project can be replicated for other chronic diseases that rely on extensive patient self-management and problem solving skills.
The knowledge base discussed here has several limitations that we plan to address with future work. First, while the development of the knowledge base is the first critical step towards computable knowledge representations, further work is required to formalize the structure of the knowledge and the relationships between its different elements. To this end, we are currently developing a more formal, extendable ontology of diabetes self-management behaviors and a set of computable guidelines following the example of such influential guideline engines as Sage [53]. Second, the current knowledge base is optimized to use blood glucose levels captured through self-monitoring as an input and a precondition to decision-support. At the same time, self-monitoring in diabetes often includes capture of many different activities, for example diet and exercise. To connect these captured behaviors with triggers already identified, more explicit and computable behavioral norms need to be established and integrated into the knowledge base. These will help to assess individuals’ captured behaviors on their risk factor, and further narrow down the space of possible solutions.
In addition, the complex nature of diabetes and the many diverse behavioral factors associated with diabetes outcomes present challenges to establishing a comprehensive diabetes self-management knowledgebase. While practicing diabetes educators deemed the knowledgebase discussed here relatively complete, it can be extended beyond its current state, and its current target population of underserved minority adults with type 2 diabetes. To that end, we have built mechanisms for further extending the knowledge base using input from practicing diabetes educators and individuals with diabetes. Moreover, while action-oriented recommendations may suggest actionable steps towards alleviating problems related to glycemic control, they are not specifically tailored to different barriers individuals may encounter when trying to implement the recommendations. In the future, we plan to expand the knowledge base to explicitly include choice of a barrier that would precede a choice of a corrective action. Notably, not all problem solving in diabetes self-management evolves around problematic blood glucose readings. A typical problem solving scenario may involve an individual with diabetes faced with a situation in which the choices available to them are inconsistent with their self-management goals (for example a social gathering where all the food served is rich in carbohydrates). While the current knowledge base does not incorporate knowledge in regards to these types of problem solving situations, we believe it could be extended to incorporate them in the future.
Finally, the knowledge base presents the opportunity to incorporate subjective impressions of diabetes educators and individuals with diabetes on comparative appropriateness and effectiveness of different knowledge elements, in particular, effectiveness of different behavioral goals. To that end, we are currently incorporating mechanisms for social curating of content, which will allow individuals to express their approval of knowledge elements (“like” them), and leave comments on different elements of the knowledge base.
The studies described in this paper have several limitations. First of all, they were conducted with a limited set of participants, including both individuals with diabetes and diabetes educators recruited from three Community Health Centers. This could limit the generalizability of the findings to other settings and participants. In addition, this work focused only on individuals with type 2 diabetes; future research could determine its applicability to individuals with other types of diabetes. Finally, the validation study was conducted in settings removed from individuals’ daily experiences; future research could assess its feasibility in a more ecologically valid environment.
5. Conclusion
The purpose of this study was to develop a theoretically sound knowledge base for problem-solving in diabetes. The target community in this study is one that suffers disproportionately from high prevalence of diabetes and poor diabetes related outcomes, and may be less likely than other groups to successfully implement the recommendations provided by diabetes self-management education. Combination of theory-driven and participatory design approaches led to the knowledge base that is theoretically grounded and incorporates practical knowledge of experienced diabetes educators. Such knowledge base can enable a new class of patient-centric decision-support tools that help individuals make daily decisions regarding self-management of diabetes. While the knowledge base is specific to diabetes self-management, its organization and structure can be extended to other chronic diseases beyond diabetes.
Acknowledgements
This work was funded by the National Library of Medicine (NLM) Training Grant in Biomedical Informatics at Columbia University, T15 LM007079, and National Institute of Diabetes and Digestive and Kidney Disease (NIDDK) grant, R01DK090372.
Footnotes
Conflict of interest
The authors have no competing interests for this publication.
Contributors
There are no collaborators beyond the co-authors of the paper
Contributorship
All authors designed the study. HCL and LM served as main research investigators in conducting all the described research activities, and preparing early drafts of the manuscript. AS and PD served as domain experts and academic diabetes educators and were chiefly responsible for developing the knowledge included in the knowledge base, and editing the manuscript. AC and JT served as liaisons with the participating FQHCs, participated in the validation sessions, and edited the manuscript. EM provided feedback on the design of participatory design activities and provided feedback on the manuscript. RK and GH provided feedback on the design of the knowledge base and research activities and edited the manuscript.
Competing interests
The authors have no competing interests for this publication.
References
- 1.Cleveringa FGW, Gorter KJ, van den Donk M, Pijman PLW, Rutten GEHM. Task delegation and computerized decision support reduce coronary heart disease risk factors in type 2 diabetes patients in primary care. Diabetes Technol. Ther. 2007;9:473–481. doi: 10.1089/dia.2007.0210. [DOI] [PubMed] [Google Scholar]
- 2.Filippi A, et al. Effects of an automated electronic reminder in changing the antiplatelet drug-prescribing behavior among Italian general practitioners in diabetic patients: an intervention trial. Diabetes Care. 2003;26:1497–1500. doi: 10.2337/diacare.26.5.1497. [DOI] [PubMed] [Google Scholar]
- 3.O’Connor PJ, et al. Impact of electronic health record clinical decision support on diabetes care: a randomized trial. Ann. Fam. Med. 2011;9:12–21. doi: 10.1370/afm.1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Toobert DJ, et al. Outcomes from a multiple risk factor diabetes self-management trial for Latinas: ¡Viva Bien! Ann. Behav. Med. 2011;41:310–323. doi: 10.1007/s12160-010-9256-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hill-Briggs F, et al. Effect of problem-solving-based diabetes self-management training on diabetes control in a low income patient sample. J. Gen. Intern. Med. 2011;26:972–978. doi: 10.1007/s11606-011-1689-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lorig K, Ritter PL, Villa FJ, Armas J. Community-based peer-led diabetes self-management: a randomized trial. Diabetes Educ. 2009;35:641–651. doi: 10.1177/0145721709335006. [DOI] [PubMed] [Google Scholar]
- 7.Amoako E, Skelly AH, Rossen EK. Outcomes of an intervention to reduce uncertainty among African American women with diabetes. West. J. Nurs. Res. 2008;30:928–942. doi: 10.1177/0193945908320465. [DOI] [PubMed] [Google Scholar]
- 8.Glasgow RE, et al. Randomized effectiveness trial of a computer-assisted intervention to improve diabetes care. Diabetes Care. 2005;28:33–39. doi: 10.2337/diacare.28.1.33. [DOI] [PubMed] [Google Scholar]
- 9.American Association of Diabetes Educators. AADE7™ Self-Care Behaviors. 2012 http://www.diabeteseducator.org/ProfessionalResources/AADE7/index.html. [Google Scholar]
- 10.Mulcahy K, et al. Diabetes self-management education core outcomes measures. Diabetes Educ. 2003;29:768–770. 773–784, 787–788. doi: 10.1177/014572170302900509. Passim. [DOI] [PubMed] [Google Scholar]
- 11.Haas L, et al. National standards for diabetes self-management education and support. Diabetes Care. 2012;36:S100–S108. doi: 10.2337/dc13-S100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fitzpatrick SL, Schumann KP, Hill-Briggs F. Problem solving interventions for diabetes self-management and control: a systematic review of the literature. Diabetes Res. Clin. Pract. 2013;100:145–161. doi: 10.1016/j.diabres.2012.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paterson B, Thorne S. Expert decision making in relation to unanticipated blood glucose levels. Res. Nurs. Health. 2000;23:147–157. doi: 10.1002/(sici)1098-240x(200004)23:2<147::aid-nur7>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 14.Norris SL, Engelgau, Narayan K. Effectiveness of self-management training in type 2 diabetes: a systematic review of randomized controlled trials. Diabetes Care. 2001;24:561–587. doi: 10.2337/diacare.24.3.561. [DOI] [PubMed] [Google Scholar]
- 15.Lau F, Kuziemsky C, Price M, Gardner J. A review on systematic reviews of health information system studies. J. Am. Med. Inf. Assoc. 2010;17:637–645. doi: 10.1136/jamia.2010.004838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roshanov PS, et al. Features of effective computerised clinical decision support systems: meta-regression of 162 randomised trials. BMJ. 2013;346:f657. doi: 10.1136/bmj.f657. [DOI] [PubMed] [Google Scholar]
- 17.Blumenthal D, Tavenner M. The ‘meaningful use’ regulation for electronic health records. New Eng. J. Med. 2010;363:501–504. doi: 10.1056/NEJMp1006114. [DOI] [PubMed] [Google Scholar]
- 18.Musen MA, Middleton B, Greenes RA. In: Biomedical Informatics. Shortliffe EH, Cimino JJ, editors. London: Springer; 2014. pp. 643–674. http://link.springer.com/chapter/10.1007/978-1-4471-4474-822. [Google Scholar]
- 19.Hill-Briggs F, Gemmell L. Problem solving in diabetes self-management and control: a systematic review of the literature. Diabetes Educ. 2007;33:1032–1050. doi: 10.1177/0145721707308412. discussion 1051–1052. [DOI] [PubMed] [Google Scholar]
- 20.Fitzpatrick SL, Schumann KP, Hill-Briggs F. Problem solving interventions for diabetes self-management and control: a systematic review of the literature. Diabetes Res. Clin. Pract. 2013;100:145–161. doi: 10.1016/j.diabres.2012.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hill-Briggs F. Problem solving in diabetes self-management: a model of chronic illness self-management behavior. Ann. Behav. Med. 2003;25:182–193. doi: 10.1207/S15324796ABM2503_04. [DOI] [PubMed] [Google Scholar]
- 22.Holbrook A, et al. Individualized electronic decision support and reminders to improve diabetes care in the community: compete II randomized trial. CMAJ. 2009;181:37–44. doi: 10.1503/cmaj.081272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Peterson KA, et al. Improving diabetes care in practice: findings from the translate trial. Diabetes Care. 2008;31:2238–2243. doi: 10.2337/dc08-2034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Meigs JB, et al. A controlled trial of web-based diabetes disease management: the MGH diabetes primary care improvement project. Diabetes Care. 2003;26:750–757. doi: 10.2337/diacare.26.3.750. [DOI] [PubMed] [Google Scholar]
- 25.Denig P, Dun M, Schuling J, Haaijer-Ruskamp FM, Voorham J. The effect of a patient-oriented treatment decision aid for risk factor management in patients with diabetes (PORTDA-diab): study protocol for a randomised controlled trial. Trials. 2012;13:219. doi: 10.1186/1745-6215-13-219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.MacLean CD, et al. The vermont diabetes information system (VDIS): study design and subject recruitment for a cluster randomized trial of a decision support system in a regional sample of primary care practices. Clin Trials. 2004;1:532–544. doi: 10.1191/1740774504cn051oa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wilkinson MJ, Nathan AG, Huang ES. Personalized decision support in type 2 diabetes mellitus: current evidence and future directions. Curr. Diab. Rep. 2013;13:205–212. doi: 10.1007/s11892-012-0348-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Quinn CC, et al. WellDoc™ mobile diabetes management randomized controlled trial: change in clinical and behavioral outcomes and patient and physician satisfaction. Diabetes Technol. Ther. 2008;10:160–168. doi: 10.1089/dia.2008.0283. [DOI] [PubMed] [Google Scholar]
- 29.Glasgow RE, et al. Twelve-month outcomes of an internet-based diabetes self-management support program. Patient Educ. Couns. 2012;87:81–92. doi: 10.1016/j.pec.2011.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Christian JG, et al. Clinic-based support to help overweight patients with type 2 diabetes increase physical activity and lose weight. Arch. Intern. Med. 2008;168:141–146. doi: 10.1001/archinternmed.2007.13. [DOI] [PubMed] [Google Scholar]
- 31.Liang X, et al. Effect of mobile phone intervention for diabetes on glycaemic control: a meta-analysis. Diabet. Med. 2011;28:455–463. doi: 10.1111/j.1464-5491.2010.03180.x. [DOI] [PubMed] [Google Scholar]
- 32.Costa BM, Fitzgerald KJ, Jones KM, Am TD. Effectiveness of IT-based diabetes management interventions: a review of the literature. BMC Fam. Pract. 2009;10:72. doi: 10.1186/1471-2296-10-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Glasgow RE, et al. Effects of a brief computer-assisted diabetes self-management intervention on dietary, biological and quality-of-life outcomes. Chronic Illness. 2006;2:27–38. doi: 10.1177/17423953060020011001. [DOI] [PubMed] [Google Scholar]
- 34.Chalortham N, Buranarach M, Supnithi T. Ontology Development for Type II Diabetes Mellitus Clinical Support System; Conference Ontology Development for Type II Diabetes Mellitus Clinical Support System; 2009. http://text.hlt.nectec.or.th/marut/papers/dcare kicss2009.pdf. [Google Scholar]
- 35.Shahar Y, Das AK, Tu SW, Kraemer FB, Musen MA. Knowledge-based temporal abstraction for diabetic monitoring. Proc. Annu. Symp. Comput. Appl. Med. Care. 1994;69:7–701. [PMC free article] [PubMed] [Google Scholar]
- 36.Inzucchi SE, et al. Management of Hyperglycemia in Type 2 Diabetes: A Patient-Centered Approach Position Statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) Dia Care DC 120413. 2012 doi: 10.2337/dc12-0413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.American Diabetes Association. Standards of Medical Care in Diabetes-2014. Diabetes Care. 2014;37:S14–S80. doi: 10.2337/dc14-S014. [DOI] [PubMed] [Google Scholar]
- 38.Trief PM, Teresi JA, Eimicke JP, Shea S, Weinstock RS. Improvement in diabetes self-efficacy and glycaemic control using telemedicine in a sample of older, ethnically diverse individuals who have diabetes: the IDEATel project. Age Ageing. 2008;38:219–225. doi: 10.1093/ageing/afn299. [DOI] [PubMed] [Google Scholar]
- 39.Lorig K, et al. Online diabetes self-management program A randomized study. DiaCare. 2010;33:5–1281. doi: 10.2337/dc09-2153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mulvaney SA, Ritterband LM, Bosslet L. Mobile intervention design in diabetes: review and recommendations. Curr. Diab. Rep. 2011;11:486–493. doi: 10.1007/s11892-011-0230-y. [DOI] [PubMed] [Google Scholar]
- 41.Horan PP, Yarborough MC, Besigel G, Carlson DR. Computer-assisted self-control of diabetes by adolescents. Diabetes Educ. 1990;16:205–211. doi: 10.1177/014572179001600311. [DOI] [PubMed] [Google Scholar]
- 42.Clinical Directors Network. at http://www.cdnetwork.org/. [Google Scholar]
- 43.Sardell A. Clinical networks and clinician retention: the case of CDN. J. Commun. Health. 1996;21:437–451. doi: 10.1007/BF01702604. [DOI] [PubMed] [Google Scholar]
- 44.Haas L, et al. National standards for diabetes self-management education and support. Diabetes Care. 2014;37(Suppl. 1):S144–S153. doi: 10.2337/dc14-S144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.AADE7™-American Association of Diabetes Educators. at http://www.diabeteseducator.org/ProfessionalResources/AADE7/index.html. [Google Scholar]
- 46.Pedersen ED. A Qualitative Study of the Electronic Commerce Process: An Emic Perspective of Electronic Commerce Entrepreneurs. ProQuest. 2007 2015. [Google Scholar]
- 47.(Stephen) Guest GS, MacQueen KM, Namey EE. Applied Thematic Analysis. SAGE Publications, Inc.; 2011. 2015. [Google Scholar]
- 48.Glazier RH, Bajcar J, Kennie NR, Willson K. A systematic review of interventions to improve in socially disadvantaged populations. Diabetes Care. 2006;29:1675–1688. doi: 10.2337/dc05-1942. [DOI] [PubMed] [Google Scholar]
- 49.Bright TJ, et al. Effect of clinical decision—support systems A systematic review. Ann. Intern. Med. 2012;157:29–43. doi: 10.7326/0003-4819-157-1-201207030-00450. [DOI] [PubMed] [Google Scholar]
- 50.Sittig DF, et al. Grand challenges in clinical decision support. J. Biomed. Inform. 2008;41:387–392. doi: 10.1016/j.jbi.2007.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sittig DF, Singh H. Electronic health records and national patient-safety goals. New Eng. J. Med. 2012;367:1854–1860. doi: 10.1056/NEJMsb1205420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Quantified Self—Self Knowledge Through Numbers. Quantified Self. at http://Quantifiedself.com/. [Google Scholar]
- 53.Tu SW, et al. The SAGE guideline model: achievements and overview. J. Am. Med. Inform. Assoc. 2007;14:589–598. doi: 10.1197/jamia.M2399. [DOI] [PMC free article] [PubMed] [Google Scholar]