Abstract
Background
Social service interventions have been implemented in many countries to help people living with HIV (PLHIV) and household members cope with economic burden as a result of reduced earning or increased spending on health care. However, the evidence for specific interventions—economic strengthening and legal services—on key health outcomes has not been appraised.
Methods
We searched electronic databases from January 1995 to May 2014 and reviewed relevant literature from resource-limited settings on the impact of social service interventions on mortality, morbidity, retention in HIV care, quality of life, and ongoing HIV transmission and their cost-effectiveness.
Results
Of 1685 citations, 8 articles reported the health impact of economic strengthening interventions among PLHIV in resource-limited settings. None reported on legal services. Six of the 8 studies were conducted in sub-Saharan Africa: 1 reported on all 5 outcomes and 2 reported on 4 and 2 outcomes, respectively. The remaining 5 reported on 1 outcome each. Seven studies reported on quality of life. Although all studies reported some association between economic strengthening interventions and HIV care outcomes, the quality of evidence was rated fair or poor because studies were of low research rigor (observational or qualitative), had small sample size, or had other limitations. The expected impact of economic strengthening interventions was rated as high for quality of life but uncertain for all the other outcomes.
Conclusions
Implementation of economic strengthening interventions is expected to have a high impact on the quality of life for PLHIV but uncertain impact on mortality, morbidity, retention in care, and HIV transmission. More rigorous research is needed to explore the impact of more targeted intervention components on health outcomes.
Keywords: economic strengthening, social services, mortality, morbidity, retention, quality of life, developing countries
INTRODUCTION
The vast evidence of the impact of HIV/AIDS on livelihoods has prompted efforts to invest in social services to protect the vulnerable and/or to improve the life and living conditions of HIV-infected and HIV-affected individuals. Despite the availability of antiretroviral therapy (ART), HIV infection and its associated financial challenges reduce household capacity to earn income and the ability to purchase basic necessities, and push affected households deeper into poverty.
Countries most affected by the HIV epidemic, especially in resource-limited settings (RLS), generally lack proper social protection and welfare systems to support needy populations. The UNAIDS Outcome Framework: Business Case 2009–2011 called for enhancing social protection— defined as “all public and private initiatives that provide income or consumption transfers to the poor, protect the vulnerable against livelihood risks, and enhance the social status and rights of the marginalized; with the overall objective of reducing the economic and social vulnerability of poor, vulnerable, and marginalized groups”1 —for people affected by HIV.2,3 Furthermore, the UNAIDS Investment Framework highlighted that investments in social protection are necessary to achieve the vision of zero new HIV infections, zero discrimination, and zero AIDS-related deaths.3 The UNAIDS Business Case on Social Protection2,3 and the United Nations Children’s Fund report on HIV-sensitive social protection4 concluded that social protection interventions have the potential to reduce vulnerability to HIV infection and strengthen the livelihood of affected individuals and household economies.
Social service interventions for people living with HIV (PLHIV) include services aimed to provide financial protection to or strengthen economic capacity and promote social well-being of PLHIV. Interventions include economic strengthening activities and legal services.5. These services have been applied to HIV programs with mixed results. For example, a social cash transfer program in Malawi resulted in improvements in household economy and well-being for PLHIV.6 A randomized control trial also in Malawi found that women who received cash transfer had a lower prevalence of HIV infection than the control group.7 However, a systematic review of 12 studies that assessed the impact of income-generation activities in low- and middle-income countries on behavioral, psychological, social, care, or biological outcomes related to HIV prevention was inconclusive.8 Therefore, evidence gaps remain, in particular, regarding the impact of these interventions on key HIV outcomes such as mortality and morbidity.
To assess the evidence gaps on the impact of social service interventions on HIV outcomes, we reviewed evidence to answer 2 key questions: Do social service interventions—specifically income-generation activities, livelihood and legal services—3 social service interventions listed in the PEPFAR technical considerations5 —have an impact on mortality, morbidity, retention in HIV care, quality of life, and prevention of ongoing HIV transmission? And are these interventions cost-effective?
REVIEW METHODS
This review is part of a broader evaluation of 13 care and support interventions offered to PLHIV in RLS. The list of interventions and general methods of review are described fully in the introductory article to this supplement.9
Social service interventions include (1) social assistance programs, for example, asset and cash transfers, (2) asset growth and protection, for example, group and individual savings and legal services (including rights, ownership) to protect vulnerable groups, and (3) income growth, for example, business loans, skills training, and income-generating activities.10 For this review, we focused on 2 main categories: economic strengthening and legal services. Consideration of these resulted in a list of specific search terms (Table 1).
TABLE 1.
Search Terms
| Social Services–Specific Search Terms | ||
|---|---|---|
| Economic | Legal rights | Income generation |
| Economic status | Job development | Vocational training |
| Economic strengthening |
Rights | Gender equality |
| Livelihood program |
Integrated HIV and livelihood programs |
Job creation |
| Vocational education |
Livelihood | Livestock support |
| Voucher | Community savings groups | Social protection |
| Life skills | Loan | Local economic development |
| Market linkages | Microcredit | Microenterprise |
| Microfinance | Microfranchising | Micro-insurance |
| Vocational guidance |
Career counseling | Business development service |
| Entrepreneurship | Apprenticeship | Asset transfer |
| Cash for work | Cash transfer | Economic empowerment |
| Economic advancement |
Skills training | Sustainable livelihood |
| Financial management |
Agriculture | Land rights |
| Legal service | Property ownership | Ownership |
| Legal activities | ||
Search Strategy and Search Terms
We conducted a systematic search of the literature using Medline (through PubMed), EMBASE, Global Health, Cumulative Index to Nursing and Allied Health Literature, Sociological Abstracts, and African Index Medicus for the period from January 1995 to May 2014. We applied general search terms for HIV and outcomes and a geographic filter for RLS as described in the introductory article to this supplement.9 Additional Medical Subject Headings terms that were used for these specific interventions are listed in Table 1.
Inclusion Criteria
We included studies with multiple types of study designs (experimental, observational, or qualitative) that fulfilled the following criteria: (1) evaluated one or more social service interventions as defined above, (2) conducted in RLS, and (3) reported on at least one of the key outcomes of interest: mortality, morbidity, retention in HIV care, quality of life (QOL), or HIV transmission. Studies that evaluated the associated costs and cost-effectiveness of interventions were also included.
Evaluation of Abstracts and Identification of Relevant Studies
We scanned the citations and abstracts identified by the search to identify studies that seemed to address economic strengthening or legal services and at least one of the outcomes of interest. For these “eligible studies,” full text articles were obtained and reviewed to identify those that in fact fulfilled the inclusion criteria (“included studies”). Costing or cost-effectiveness information and studies when available were also considered.
Data Abstraction and Analysis
For each study that fulfilled the inclusion criteria, we abstracted year of publication, study design, study period and country, number and type of participants, specific intervention and outcomes. The quality of the evidence from each of the included studies for each outcome of interest was summarized based on the type of study and other factors such as the number of study participants and internal and external validity of the study data. The overall quality of evidence was rated as strong, medium, or weak. Qualitative studies were rated on a scale of I to IV based on methods adapted from Daly et al,11 ranging from generalizable studies (scored I) to those weaker designs such as single case studies (scored IV).
We did not attempt to perform a meta-analysis because of heterogeneity of included studies. We instead grouped and summarized studies for areas of interest for each outcome. We rated the overall quality of evidence for each outcome as good, fair, or poor based on the criteria developed in advance. We then rated the expected intervention impact on each outcome—based on the magnitude of effect reported in individual studies, the quality of the body of evidence (all studies addressing each outcome), and consistency of results across the studies—as high, moderate, low, or uncertain (more details regarding rating of quality of evidence for individual studies, and quality of evidence and expected impact for each outcome can be found in the introductory article in this supplement).9
RESULTS
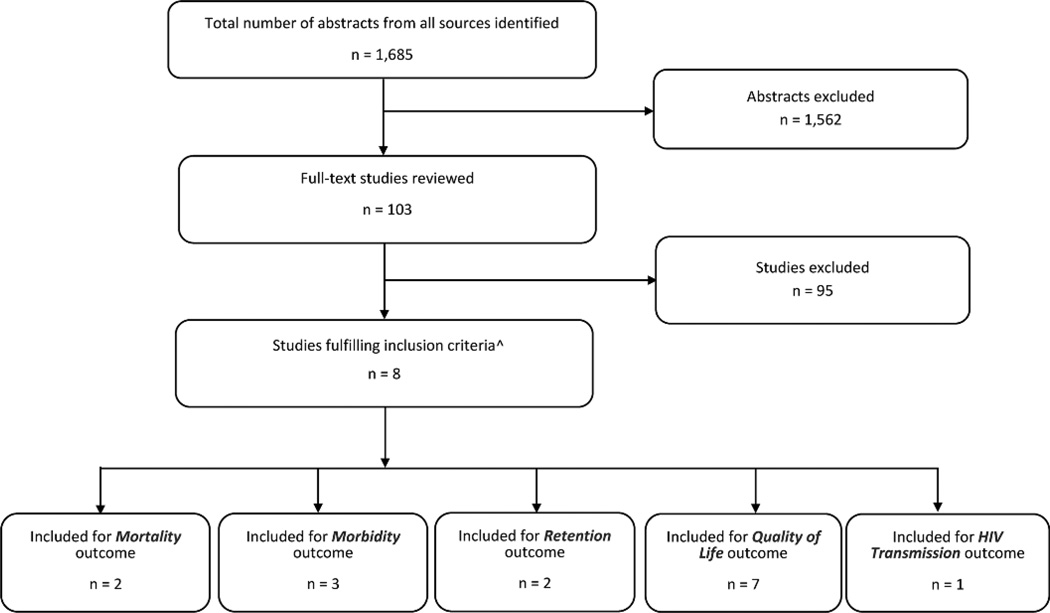
A total of 1685 citations and abstracts were identified in the initial search. Of those, 103 were considered as “eligible.” Eight of these articles met all inclusion criteria (“included studies,” Fig. 1).
FIGURE 1.
Total number of citations identified by the search; those screened; those retrieved in full text (eligible studies); and those remaining and used the answer of the review questions (included studies). Numbers below in outcome section add up to more than 8 since some studies addressed more than one outcome.
Table 2 shows the key findings and the quality of evidence for each of the 8 included studies by outcome. All 8 studies addressed economic strengthening interventions. One article reported on all 5 outcomes,12 and 2 reported on 4 and 2 outcomes, respectively.13,16 The remaining 5 reported on 1 outcome each. Six of the 8 studies were conducted in sub-Saharan Africa, 1 in Peru, and the other in Thailand. The sample size of included studies ranged from 29 to 20,387 respondents. Six used qualitative methods, 1 used mixed methods, 1 was a matched case–control, and 1 used program monitoring data. None of the studies addressed legal services.
TABLE 2.
Assessment of Individual Studies—Impact of Social Services by Outcome
| Study Characteristics |
||||
|---|---|---|---|---|
| Citation | Study Design | Study Period, Country |
No. Participants | Key Findings (Magnitude of Effect (HR, OR, RR, RD and 95% CI) or Other Description) |
| Mortality | ||||
| Okello et al12 | Secondary analysis of program data |
2003–2010, Ethiopia | 20,387 PLHIV enrolled CBHC program between 2003 (program inception) and September 2010 (evaluation) and a control sample of 30,512 who did not receive CBHC |
Overall, among 20,387 PLHIV enrolled in CBHC, annual mortality rate declined from 10% in 2005 to 0.7% in December 2009 (no comparison data for mortality and adherence was reported, therefore adherence and mortality benefits could not be attributed to CHBC) |
| After implementation of CBHC, 99% of clients self- reported good adherence (took >95% of prescribed doses) to their ART |
||||
| Muñoz et al13 | Matched case-control | December, 2005–April, 2007, Peru | 120 (60 community-based accompaniment with supervised ART (CASA), incl. 12 mo of DOT-HAART, microfinance assistance and/or psychosocial support and 60 matched controls) |
CASA recipients were more likely to live longer (median time from enrolment to death, 106.5 vs. 99 days, HR = 0.29, 95% CI: 0.12 to 0.75), be on HAART (86.7% vs. 51.7%, P < 0.01), to achieve virologic suppression (66.7% vs. 46.7%, P= 0.03), to report adherence to HAART (79.3% vs. 44.1%, P < 0.01), and among TB patients, to complete TB treatment (81.8% vs. 48.6%, P < 0.01) compared with controls |
|
Only 16.7% of CASA recipients received microfinance assistance |
||||
| Morbidity | ||||
| Okello et al12 | Quasi-experimental design used to measure outcomes and impact of CHBC |
2003–2010, Ethiopia | 2667 (1195 received CHBC including income generation [intervention], and 1482 controls [did not receive program benefits] matched using propensity scoring |
In the 2168 matched pairs, CBHC participants were also more likely to report an opportunistic infection in the previous 6 mo (54.5% vs. 46.2%, P = 0.000) Among CBHC participants, no data were reported on who was involved in income-generating activities (community savings and loans groups), the intervention of specific interest in this review |
| Pandit et al14 | Routine program monitoring data; Qualitative (FGD) |
February–July, 2007, Kenya | 29 PLHIV got a microfinanced loan for an irrigation pump and related farming guidance, loans, and training. FGD with 18 farmers 12 mo after intervention |
From program data (n = 29): no significant differences in body mass index and CD4 count between baseline and 12 mo after the intervention. There was a trend toward improvement in CD4 counts for those below 200 cells/mcL at baseline but the effect of ART cannot be excluded |
| From FGD (n = 18): Most mentioned that the program provided increased food for consumption in the home and modest improvement in income |
||||
| Repayment of loan from participants was very poor, 50% failed to make any repayment, because 80% of patients were on ART, the benefit from economic support was impossible to evaluate. OIs and other comorbidities were reported at 12 mo after the intervention, but not at the baseline |
||||
| Muñoz et al13 | Matched case-control | December 4, 2005–April 4, 2007, Peru |
120, see above | Among TB patients (55% of CASA participants, 58.3% of controls) with 81.8% of individuals completed treatment in the CASA group compared with 48.6% among controls, χ2= 15.6, P < 0.01 There was a nonsignificant difference in mean change in CD4 cell count from baseline to 24 mo in CASA recipients compared with nonrecipients (239.7 ± 133.6 vs. 300.7 ± 208.5; χ2 = −1.50) |
| Retention in care | ||||
| Okello et al12 | See above | See above | 2667 (1195 received CHBC income generation [intervention] and 1482 controls |
In the 2168 matched pairs, CBHC participants (intervention) were more likely than non-CBHC participants (controls) to have been diagnosed with HIV longer than 3 years (68.5% vs. 58.2%, P < 0.001) but were less likely to be receiving ART (90.1% vs. 94.6%, P < 0.001). However, if on ART, they were more likely to have been on it for >2 years (56.4% vs. 48.9%) |
| Muñoz et al13 | See above | See above | 120, see details above | At 2 years, 92.9% (52/56) of PLHIV who received CASA (that included microfinance assistance) who started HAART remained on HAART, compared with 56.4% (31 of 55) in the control group (χ2 = 17.7, P < 0.01) As noted above, only 16.7% of CASA recipients received microfinance assistance, the intervention of interest in this review |
| QOL | ||||
| Okello et al12 | See above | See above | 2667. QOL between intervention and control was assessed by change in physical conditions, psychologic conditions, level of dependency, social relations and household savings |
The programme significantly improved clients’ QOL. Composite median overall QOL score* was higher in the intervention group (CBHC) than in the control group (11.87 vs. 11.47 P = 0.000), with significant differences in measures for independence (P = 0.025), social relations (P = 0.000), and the environment for PLHIV (P= 0.029). More clients in intervention reported improved household savings than those in control group (36.9% vs. 20.7%, P= 0.000) |
| Holmes et al15 | Qualitative methods were used to evaluate a pilot village savings and loan scheme |
June–September, 2008, Cote d’lvore |
66 PLHIV participants of a village savings and loan scheme were involved in IDIs, FGDs, and KIIs |
Overall, the intervention improved psychosocial well-being, sense of belonging, positive outlook of life, such as reduced resource-based discrimination; improved health because financial possibility in receiving ongoing treatment; expanded social support network with gained economic status; increased economic independence and economic sufficiency; improved perception of PLHIV; improved reach to PLHIV |
| Datta and Njuguna16 | Qualitative | 2008, Kenya | FGDs and Structured interviews with recipients of microcredits |
Improvement of economic well-being, but reflected also in improved social standing, and physical and psychologic wellness of the clients |
|
No information about how many was interviewed. About 90% of microcredit beneficiaries were women |
||||
| Viravaidya et al17 | Qualitative | 2004–2006, Thailand | 155 PLHA answered QOL questionnaire in 2004 and 132 in 2006 of 630 PLHA and HIV-negative partners who received microcredit loans through the Positive- Partnership Project |
The project led to improved QOL and economic conditions for PLHIV, raised visibility and acceptance of PLHIV. From 2004–2006, there was improvement in QOL (5.3– 7.0); and in different domains: economic (5.2–7.0), social (5.5–8.2), physical (6.0–7.9), and mental (5.8–7.8) as measured by a bamboo step ladder scale (1–10 highest). The project led to improved economic security among PLHIV, increased involvement of community leaders and pairing HIV negative and positive individuals reduced the stigma and discrimination. Increased involvement of community leaders and pairing reduced the stigma and discrimination |
| Miller et al6 | Qualitative | 2008, Malawi | 24 | Responded reported positive impacts on personal health (41.7%), improved ability to obtain ARVs (35.7%); food security (70.8%) and gained economic well- being personally or for families. Increased inclusion by the community. However, respondents were interviewed at one time point, rather than followed longitudinally. There was no control group |
| Muñoz et al13 | See above | See above | 120, see details above | Changes in psychosocial indicators were greater at 24 mo for CASA participants vs. controls, regarding reduced stigma (P < 0.01) and social support (P < 0.01). No differences of changes in QOL, depression, and self- efficacy were observed between groups |
| Wagner et al18 | Qualitative | 2010, Uganda | 30 adults receiving ART and microcredit | Most respondents described positive psychologic effects of the loans, indicating that they felt “happy” or “hopeful.” There was stigma reduction and increased social standing —65% of the respondents described receiving greater support and respect from the community, others reported an expanded social network and increased social invitations and popularity. Effects were less in women. However, some participants reported negative effects: stressed out and more anxious because of the responsibility to repay the loans |
| HIV transmission | ||||
| Datta and Njuguna16 | Qualitative | 2008, Kenya | Impact was assessed in 108 of 221 loan beneficiaries (49%) |
Microcredit recipients reported changing their behavior and reducing chances of infection and re-infection, in addition to promoting their ability to adhere to treatment. Loan beneficiaries became agents of positive living and encouraged other affected persons to seek treatment and support services, and live positively |
| Quality of Evidence for Individual Studies |
|||||
|---|---|---|---|---|---|
| Study Characteristics Citation |
Validity (High/Good moderate, or Poor/low) |
Quality of Evidence (Strong Medium Weak) |
Evidence from Economic Evaluation (Yes or No) |
Comments | |
| Internal | External | ||||
| Mortality | |||||
| Okello et al12 | Low (111 excluded from intervention and 398 from control group |
High | Weak (no comparison) | No data | |
| Muñoz et al13 | Low | Moderate | Medium: main limitation was small sample size and nonrandomized control group |
No data | We included VL suppressions, being and adhering to ART and completion of TB treatment as mortality outcomes |
| Morbidity | |||||
| Okello et al12 | Low: 111 intervention and 398 control were excluded |
Moderate | Medium | No data | |
| Pandit et al14 | Low | N/A, majority were men (75%) |
Weak | No data | |
| Retention in care | |||||
| Muñoz et al13 | Low | Moderate | Medium | No data | |
| Okello et al12 | Low | Moderate | Weak | No data | |
| Muñoz et al13 | Low | Moderate | Weak | ||
| QOL | |||||
| Okello et al12 | Low | Moderate | Medium | No data | |
| Holmes et al15 | Low | N/A | Weak | No data | |
| Datta and Njuguna16 | Low | N/A | Weak | No data | |
| Viravaidya et al17 | Low | N/A | Weak | No data | |
| Miller et al6 | Low | N/A | Weak | No data | |
| Muñoz et al13 | Low | Moderate | Weak | No data | |
| Wagner et al18 | Low | N/A | Weak | No data | |
| HIV transmission | |||||
| Datta and Njuguna16 | Low | N/A | Weak | No data | Authors do not state how many were actually interviewed |
WHO QOL measurement tool (WHO 2005) was adapted and the following domains were assessed: physical condition (pain, discomfort, energy, sleep, and rest); psychologic condition (positive and negative feelings, self-esteem, and acceptance of body image); independence (ability to perform daily activities, mobility and dependence on medications to function); and social relationships (satisfaction with personal relationships, dependence on others for basic needs, and perception of change in attitudes of the community toward PLHIV).
CI, confidence interval; FGDs, focus group discussions; HR, hazard ratio; IDIs, in-depth interviews; KII, key-informant interviews; OIs, opportunistic infections.
Key Outcomes, Quality of the Evidence, and Expected Impact Outcomes
Mortality
Two studies reported on mortality outcomes.12,13 Okello et al reported data from an evaluation of a Community and Home-Based Care (CHBC) program implemented in 13 urban and periurban communities in 4 of 11 regions of Ethiopia. A sample of 2168 drawn from 20,387 individuals enrolled in the CHBC program between 2003 (program inception) and September 2010 (evaluation) and from 30,512 who were not enrolled into the program—1084 intervention participants matched by propensity scoring to 1084 controls—were compared. Program participants were trained in methods of income generation and enrolled in community self-help, and savings and loans groups. Evaluation of the program revealed a decrease in mortality from a baseline of 10% in 2005 to 0.7% in 2009. The authors did not report how many clients received which interventions. The authors acknowledged a major limitation of the study regarding the benefits of the economic strengthening interventions: because of the lack of comparative baseline data for the control group in 2005 and the increased use of ART in the interim, the mortality benefit could not be attributed to the economic strengthening interventions. In addition, a significant number of program participants were excluded from the analysis.
In a study conducted by Muñoz et al13 in Peru, 60 adults starting ART who participated in a Community-based Accompaniment with a Supervised Antiretroviral program (CASA) were matched by age, primary referral criteria, and baseline CD4 cell count with 60 controls who did not participate in CASA. CASA interventions included 12 months of directly observed therapy, ART, microfinance and assistance, and/or participation in a psychosocial support group based on need. Clinical and psychosocial outcomes were assessed at 24 months. In comparison to the control, the CASA participants were more likely to be on highly active antiretroviral therapy (HAART), 86.7% vs. 51.7%, P < 0.01; to achieve virologic suppression, 66.7% vs. 46.7%, P = 0.03; and to report higher adherence to HAART, 79.3% vs. 44.1%, P < 0.01. Implementing CASA was associated with a higher chance of survival; however, the findings were confounded by more patients being on ART. Additionally, only 16.7% of CASA participants were reported to have received micro-finance assistance.
The overall quality of these 2 studies was rated poor based on study limitations noted above. The expected impact of the economic strengthening interventions on mortality was rated as uncertain (Table 3).
TABLE 3.
Summary Evidence From All Studies by Outcome
| Overall Quality of Evidence |
Impact of the Intervention |
|||
|---|---|---|---|---|
| Studies (No. Addressing Each Outcome and References) |
Overall Quality of the Body of Evidence (Good, Fair, Poor) |
Expected Impact (High, Moderate, Low, Uncertain) |
Comments | |
| Mortality | 2 (12,13) | Poor: 1 study (Okello et al) used secondary program data with no comparison, and Munoz et al was limited |
Uncertain: Both studies show beneficial effects of the different economic strengthening interventions on mortality, adherence to ART, and viral load suppression |
It’s difficult to clearly conclude that the benefits reported were due to the intervention in part because social support components were given in combination with other services that impact the outcomes |
| Morbidity | 3 (12–14s) | Poor: The 3 studies differed in study design, offered different interventions, and reported on different outcomes |
Uncertain: Okello et al reported worse outcomes in the intervention [more OIs (58% vs. 45.5% P < 0.01)] than in the control, whereas Pandit et al did not show significant differences |
The articles reviewed for this outcome used different measure of morbidity and addressed the intervention to different populations. Among target populations, only a few people received the intervention |
| Retention in care |
2 (12,13) | Poor: The same limitations as noted above. Additional biases were likely introduced in the way participants were selected |
Uncertain: Although both studies showed that patients who received different economic strengthening interventions were on ART longer than in control, it is only in the Munoz et al study where this may be attributed to the intervention |
Results from several large cohorts demonstrate sustained retention especially in ART patients |
| QOL | 7 (6,12,13,15–18) | Fair: There were significant methodological issues in almost all studies that addressed and reported on QOL |
High: Evidence from all 7 studies shows that the social support interventions such as microcredit/loans to targeted PLHIV led to improvements in the different measures of QOL. The evidence from the 7 studies is consistent and shows that the intervention if implemented successfully is likely to have a high impact in the settings studied |
Studies used different measures of QOL. All reported outcomes would have an impact on QOL for PLHIV directly or indirectly |
| HIV transmission |
1 (16) | Poor: The single study reported on behavior change and intermediate outcome and not objective measures of transmission |
Uncertain: Available data from a single qualitative study show that microcredit recipients changed sexual behavior to reduce chances of infecting others. It is unclear if these findings are replicable |
|
There were no economic evaluations.
Morbidity
Three studies reported morbidity outcomes.12–14 The studies differed in study design, offered different interventions, and assessed outcomes differently. In the Ethiopia study noted above,12 in which program participants were trained in income generation and enrolled in community self-help, and savings and loans groups, results were mixed. Among CHBC participants, improvement in health status (from being bedridden to being physically mobile) was reported, although data were not available for the non-CHBC participants. One weakness of this study is that unequal numbers of participants were excluded from the final analysis: 111 (9.2%) of those who participated in CHBC and 398 (26.2%) of those who did not. In addition, among CHBC participants, authors did not report how many participated in the community savings and loan groups, the outcome of particular interest in this review.
The study by Munoz et al13 in Peru, demonstrated only a nonsignificant difference in the mean change in CD4 cell count from baseline to 24 months in CASA recipients compared with nonrecipients (239.7 ± 133.6 vs. 300.7 ± 208.5; χ2 = −1.50, P > 0.05). However, among a subgroup of tuberculosis patients, 81.8% of CASA participants were cured compared with 48.6% of controls (χ2 = 15.6, P < 0.01). Findings from this study may have limited generalizability because patients with tuberculosis (56.7% of patients) were targeted for enrolment.
In a Kenya cohort study14 of 29 PLHIV who received a loan and training, there was no significant change in body mass index or CD4 count between the baseline and after 12 months. Focus group discussions conducted with some of the participants revealed that the program improved food consumption and income, although loan repayment was poor.
The quality of evidence from the 3 studies was rated as poor because of the limited number of studies and weaknesses in the individual studies. All studies were observational and findings could not be generalizable. The expected impact on morbidity was rated as uncertain (Table 3).
Retention in HIV Care
Okello et al12 reported that CHBC recipients were on ART longer, a measure of retention. Muñoz et al13 reported that 92.9% of CASA recipients who started ART remained on HAART, compared with 56.4% in the control group (χ2 = 17.7, P < 0.01) at the end of 2 years. As noted, only a small proportion of those who participated in CASA received any microfinance support.
The quality of the evidence from those 2 studies was rated as poor based on the same limitations for the mortality and morbidity outcomes as described above. In addition, retention was not a primary outcome and was reported only for patients who started ART. Although both studies showed that patients in the intervention group were on ART longer than those in the control group, only findings from the Munoz study can possibly be attributed to the intervention. However, only 16.7% of CASA recipients in that study received microfinance assistance. The expected impact on retention in care was judged as uncertain (Table 3).
Quality of Life
Seven studies reported on QOL as an outcome of social service interventions (Table 2). Five were qualitative6,15–18 and had small sample sizes ranging from 24 in the Malawi study6 to 155 in a Thai study.17 Okello et al12 studied 2667 participants and reported improvement in the composite median overall QOL scores for patients who were enrolled in the CHBC program compared with those who did not receive CHBC (11.87 vs. 11.47, P < 0.001). Improvements were observed in feeling of independence (P= 0.025), social relations (P < 0.001), and “the environment” (P = 0.029) (assessed by computing changes in (1) the physical and social environment, (2) financial resources, (3) access to health care, (4) transportation, and (5) participation in leisure/recreation activities). The CHBC participants also reported improved household savings compared with the control group (36.9% vs. 20.7%, P < 0.001). Holmes et al studied a cohort of PLHIV who participated in a village savings and loan scheme and reported improved social well-being, reduced stigmatization, and increasing members’ sense of dignity and self-worth. All other studies reported improvement in various measures of QOL, such as psychologic wellness,16 economic, social, physical, and mental benefits as measured by a step ladder scale,17 and reduction in frequency of symptoms. Only 1 study reported an adverse outcome that participants worried about repayment of the loan.18
The overall quality of evidence from all 7 studies was rated as fair based on methodologic limitations in almost all studies. However, all studies show that the social support interventions, for example, microcredit/loans led to improvements in different measures of QOL. Participants or recipients of the social service interventions reported more independence, improved savings that translate to better QOL, reduced stigma, improved social and psychosocial well-being, and in a general, positive outlook on life. Although all 7 studies used different scales or measures to define QOL, the interventions were associated with improved QOL, and therefore the expected impact was rated as high (Table 3).
HIV Transmission
Only the Datta and Njuguna16 study reported findings that have implications for HIV transmission. Microcredit recipients reported changing their sexual behaviour, potentially resulting in reduced chances of infecting their sexual partner(s). These benefits were in addition to promoting their ability to adhere to treatment. Loan recipients became agents of positive living and encouraged other affected persons to seek treatment and support services, and to live positively. We equated a decrease in high-risk sexual behavior as an intermediate outcome to a reduction in potential HIV transmission. Based on findings from only 1 qualitative study, the quality of evidence was rated as poor, and the evidence available is not adequate to estimate the impact of the study in different settings. The study reported only intermediate outcomes such as behaviour change without any objective measure of transmission. The expected impact was rated as uncertain.
DISCUSSION
Evidence supporting the impact of economic strengthening interventions and legal services on HIV clinical outcomes in developing countries is limited. Eight studies included in this review evaluated the impact of economic strengthening interventions on mortality, morbidity, retention in care, QOL, and ongoing HIV transmission. No studies assessing the impact of legal services on stated outcomes were identified through this review, and no studies addressing cost-effectiveness of social services interventions were found. The quality of the evidence was rated as poor or fair overall because the studies used study methods of low rigor, and most of the studies had other limitations. Nonetheless, all studies showed associations between economic strengthening interventions and HIV care outcomes. The expected impact of these interventions was rated as high for QOL. The evidence on the impact of the interventions on mortality, morbidity, retention in care, and HIV transmission was inconclusive, and the expected impact on these outcomes was therefore rated as uncertain.
The impact of economic strengthening interventions in non-HIV–infected people has been well studied. A Cochrane review investigating the impact of conditional cash transfers on access to care and health outcomes reported a number of health benefits for the poor.19 Although there was evidence for a positive impact on access to health services, nutritional status, and other health outcomes such as self-reported episodes of illness, the authors reported that it was not possible to attribute the effects to the cash incentives specifically. Another study,8 by Kennedy et al, similarly appraised the evidence of income-generation interventions on HIV prevention but the evidence was inconclusive. To our knowledge, this is the first review to appraise evidence of economic strengthening interventions in HIV-infected population on 5 HIV outcomes: mortality, morbidity, retention in care, QOL, and HIV transmission.
Apart from the impact on QOL, this review did not show the impact of economic strengthening interventions on the other outcomes—mortality, morbidity, retention in care, and HIV transmission. It is possible that better-designed studies would have shown more benefit of these interventions; it is also possible that such interventions have different benefits for population groups other than those included in these studies or have impacts that go beyond the patient outcomes assessed in this review. For example, PLHIV enrolled in the Ethiopia study used the resources not only for themselves but also for their household members.
Limitations
Studies included in this review had several limitations, and the findings of this review should be interpreted carefully. For example, the types of interventions and the number of PLHIV who received the interventions varied. The majority of studies were observational, qualitative, had small sample size, and varying study durations of a few months to a few years. Selection of participants within individual studies was not standardized between those who received the interventions and those who did not, potentially impacting the strength of evidence. Confounding of results by other services offered to the intervention groups, such as increased use of ART, makes interpretation of the results difficult. Additionally, some studies targeted only men and others only women; results may therefore not be generalizable to the broader population.
Assessing some of the outcomes was in itself difficult. To accommodate the range of possible interventions and outcomes, adopting broader definitions was necessary. For example, in the study by Okello et al,12 we equated disclosure of HIV-positive status to potential reduction of HIV transmission. However, neither Okello et al nor other studies that reported this outcome measured or reported any biologic markers.
Economic strengthening interventions that result in increased available income might be expected to impact lives of PLHIV to some extent, but the mechanisms and time required to achieve the outcomes are not clear. These and other factors may have influenced the results of this review.
Research Gaps
This review found limited evidence for economic strengthening interventions and argues for more rigorous studies and program evaluations of existing and future programs. There are several areas for further research.
First, the efficacy of these social service interventions is unclear, given the significant potential for confounding in the studies reviewed. Well-designed studies targeting social service interventions with strict inclusion criteria and defined outcomes are needed.
Second, none of the studies included in this review assessed costs associated with the interventions or evaluated the cost-effectiveness of the interventions on key HIV outcomes.
Third, none of the studies addressed sustainability of interventions. Although it is not a focus of this review, interventions rolled out should be sustainable. Research that addresses feasibility and sustainability of interventions would inform decision making regarding the scale-up of economic strengthening interventions that are found to be effective.
Fourth, included studies may not target population groups with the greatest need and those that may benefit most from the interventions. For example, those in the lowest-income categories, women and others may be the most appropriate beneficiaries of economic strengthening interventions. Such research is urgently needed to better inform future guidance and policy. It is possibly more relevant and pragmatic to assess the impact of interventions targeting specific needs rather than broad economic strengthening interventions.
Programmatic Considerations for Implementation
To fully maximize the potential benefits of economic strengthening and other support services in the community, it is important to ensure that a compendium of available services and a functioning referral and linkage system are available. Support to PLHIV to access locally available community resources through referrals and networking is necessary.
Programs that are already underway could be strengthened by including routine collection of outcome data that could inform the value of the programs. Studies and programs should involve relevant key stakeholders and national ministries for ownership and sustainability. Strengthening program monitoring and evaluation would be important to assess how the support has been provided and implemented, its impact (direct and indirect), costs of interventions, and the appropriate level of technical support required to implement the interventions.
CONCLUSIONS
This review has summarized available information on economic strengthening activities for PLHIV in RLS despite evidence gaps on the impact of these interventions on key clinical outcomes. Based on our review of current evidence and review criteria, economic strengthening interventions are likely to have a high impact on QOL but uncertain impact on mortality, morbidity, retention in care, and ongoing HIV transmission. Methodologic limitations, however, affected the quality of evidence from these studies. Better-designed studies and more rigorous program evaluations on HIV outcomes are needed to assess the impact of these interventions on key outcomes for PLHIV in RLS.
ACKNOWLEDGMENTS
The authors thank Gail Bang and Emily Weyant for conducting the literature searches.
Supported by the President’s Emergency Plan for AIDS Relief (PEPFAR) through the Centers for Disease Control and Prevention (CDC), the Health Resources and Services Administration (HRSA), and the United States Agency for International Development (USAID).
The findings and conclusions in this article are those of the authors and should not be construed to represent the positions of the US Department of State’s Office of the U.S. Global AIDS Coordinator, the U.S. Centers for Disease Control and Prevention, the Health Resources and Services Administration, or the United States Agency for International Development or the U.S. Federal Government.
Footnotes
The authors have no funding or conflicts of interest to disclose.
REFERENCES
- 1.Sabates-Wheeler R, Devereux S. Transformative social Protection: the Currency of social Justice. In: Barrientos A, Hulme D, editors. Social Protection for the Poor and Poorest. Basingstoke, United Kingdom: Palgrave Macmillan; 2008. pp. 64–84. [Google Scholar]
- 2.UNAIDS. [Accessed August 1, 2014];UNAIDS outcome framework 2009–2011. 2010 Available at: http://www.unaids.org/en/media/unaids/contentassets/dataimport/pub/basedocument/2010/jc1713_joint_action_en.pdf.
- 3.Schwartländer B, Stover J, Hallett T, et al. on behalf of the Investment Framework Study Group. Towards an improved investment approach for an effective response to HIV/AIDS. Lancet. 2011;377:2031–2041. doi: 10.1016/S0140-6736(11)60702-2. [DOI] [PubMed] [Google Scholar]
- 4.Miller E, Samson M. HIV-sensitive social Protection: state of the evidence 2012 in sub-Saharan africa. Cape Town, South Africa: Commissioned by UNICEF and produced by the Economic Policy Research Institute; 2012. [Accessed August 1, 2014]. Available at: http://www.unicef-irc.org/files/documents/d-3826-HIV-Sensitive-Social-Prot.pdf. [Google Scholar]
- 5.PEPFAR. [Accessed July 29, 2014];The U.S. President’s emergency plan for AIDS relief: technical considerations provided by PEPFAR technical working groups for FY 2014 COPS and ROPS. 2013 Available at: http://www.pepfar.gov/documents/organization/217761.pdf.
- 6.Miller C, Tsoka MG. ARVs and cash too: caring and supporting people living with HIV/AIDS with the Malawi Social Cash Transfer. Trop Med Int Health. 2012;17:204–210. doi: 10.1111/j.1365-3156.2011.02898.x. [DOI] [PubMed] [Google Scholar]
- 7.Baird SJ, Garfein RS, McIntosh CT, et al. Effect of a cash transfer programme for schooling on prevalence of HIV and herpes simplex type 2 in Malawi: a cluster randomized trial. Lancet. 2012;379:1320–1329. doi: 10.1016/S0140-6736(11)61709-1. [DOI] [PubMed] [Google Scholar]
- 8.Kennedy C, Fonner V, O’Reilly K, et al. A systematic review of income generation interventions, including microfinance and vocational skills training, for HIV prevention. AIDS Care. 2014;26:659–673. doi: 10.1080/09540121.2013.845287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kaplan J, Hamm T, Forhan S, et al. The impact of HIV care and support interventions on key outcomes in low and middle-income countries: a literature review. Introduction. J Acquir Immune Defic Syndr. 2015;68(suppl 3):S253–S256. doi: 10.1097/QAI.0000000000000495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.James-Wilson D, Torres V, van Bastelaer T, et al. Field Report 2: Economic Strengthening for Vulnerable Children: Principles of Program Design and Technical Recommendations for Effective Field Interventions. [Accessed July 29, 2014];USAID, Academy for Educational Development, Save the Children. Available at: https://www.microlinks.org/sites/microlinks/files/resource/files/FIELD%20Report%20No%202_2012.pdf.
- 11.Daly J, Willis K, Small R, et al. A hierarchy of evidence for assessing qualitative health research. J Clin Epidemiol. 2007;60:43–49. doi: 10.1016/j.jclinepi.2006.03.014. [DOI] [PubMed] [Google Scholar]
- 12.Okello F, Stuer F, Kidanel A, et al. Saving the sick and improving the Socio-economic conditions of people living with HIV in Ethiopia through traditional burial groups. Health Policy Plan. 2013;28:549–557. doi: 10.1093/heapol/czs097. [DOI] [PubMed] [Google Scholar]
- 13.Muñoz M, Bayona J, Sanchez E, et al. Matching social support to individual needs: a community-based intervention to improve HIV treatment adherence in a resource-poor setting. AIDS Behav. 2011;15:1454–1464. doi: 10.1007/s10461-010-9697-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pandit JA, Sirotin N, Tittle R, et al. Shamba Maisha: a pilot study assessing impacts of a micro-irrigation intervention on the health and economic wellbeing of HIV patients. BMC Public Health. 2010;10:245. doi: 10.1186/1471-2458-10-245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Holmes K, Winskell K, Hennink M, et al. Microfinance and HIV mitigation among people living with HIV in the era of anti-retroviral therapy: emerging lessons from Cote d’Ivoire. Glob Public Health. 2011;6:447–461. doi: 10.1080/17441692.2010.515235. [DOI] [PubMed] [Google Scholar]
- 16.Datta D, Njuguna J. Microcredit for people affected by HIV and AIDS: insights from Kenya. SAHARA J. 2008;5:94–102. doi: 10.1080/17290376.2008.9724906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Viravaidya M, Wolf RC, Guest P. An assessment of the positive partnership project in Thailand: key considerations for scaling-up microcredit loans for HIV-positive and negative pairs in other settings. Glob Public Health. 2008;3:115–136. doi: 10.1080/17441690801903070. [DOI] [PubMed] [Google Scholar]
- 18.Wagner G, Rana Y, Linnemayr S, et al. A qualitative Exploration of the economic and social effects of microcredit among people living with HIV/AIDS in Uganda. AIDS Res Treat. 2012;2012:318957. doi: 10.1155/2012/318957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lagarde M, Haines A, Palmer N. The impact of conditional cash transfers on health outcomes and use of health services in low and middle income countries. Cochrane Database of Systematic Reviews. 2009;(4) doi: 10.1002/14651858.CD008137. Art. No.: CD008137. [DOI] [PMC free article] [PubMed] [Google Scholar]