Abstract
The relationship between patient and physician is in flux with the advent of electronic media that are advancing and enhancing communication. We perform a retrospective, current, and forward-looking examination of the technologies by which information is exchanged within the healthcare community. The evolution from email and listservs to blogs and the modern social networks is described, with emphasis on the advantages and pitfalls of each medium, especially in regard to maintaining the standards of privacy and professionalism to which doctors are held accountable. We support the use of contemporary platforms like Twitter and Facebook for physicians to establish themselves as trustworthy online sources of medical knowledge, and anticipate ongoing collaboration between researchers, patients, and their advocates in trial design and accrual.
Social media comprise electronic resources by which users can create content and share information in a virtual community setting. Membership in these communities is provided through specific Internet-based and/or mobile applications, which are widely available and most often either free or accessible at low cost1. The use of social media is far from exclusive to the healthcare setting; indeed, serious and understandable concerns about privacy and professionalism may have slowed the acceptance and adoption of social media by many members of the medical community. However, in spite of these issues, social media provide new opportunities for the dissemination of reliable, validated information pertaining to healthcare, as well as for the progress of science and treatment in a patient-centered manner. In this review article, we examine the past, present, and future means of electronic communication between physicians and patients, particularly as they relate to oncology and the cooperative groups tasked with advancing cancer care.
I. Past
Email is a method of patient-doctor communication that, ideally, eliminates the delays encountered with conventional mail; it has been described as an evolved hybrid between letter writing and the spoken word2, overcoming the slow pace of the former and the impermanence of the latter. However, it is also an almost unavoidably asynchronous exchange, which, as a putative benefit, allows the healthcare provider flexibility in the time and convenience of their response, but also does not guarantee receipt in a manner that is sufficiently timely to address appropriately the patient's concerns. For instance, and most worryingly, there are some complaints raised by the patient in an email that would best be addressed by immediate attention in the clinic or emergency room, but where the triage and management process is delayed as the medical issue awaits attention in an inbox. Here, there might be a hazardous gap between the passivity of the message's arrival and the action taken by the doctor once the message is received and read in the context of the patient's illness.
Especially at the time of email's introduction to the medical community, its proponents described it as an improvement over the traditional phone messaging systems that were (and are) omnipresent in doctors' offices, but patient preference for the convenience of email does not necessarily reflect equal or improved timeliness of response from the doctor or their clinical staff to telephone calls3. As the volume of electronic correspondence grows, it becomes proportionately more possible that such a clinically meaningful message could be overlooked or neglected when it might need to be addressed immediately. “Email metastasis” is a term that has been coined to describe the untenably voluminous amount of messages that this medium can generate, with the allegedly ‘free’ method of correspondence actually carrying substantial and hidden costs in terms of the time and otherwise hypothetically monetized physician effort devoted to reading each message and assessing its importance4.
Additionally, while emails can offer permanence, the inclusion of these messages in the medical record is by no means universal or guaranteed, meaning that important communication between patient and provider may, from a medicolegal perspective, go undocumented or even contravene previously written recommendations. Finally, the privacy of such dialogue is not always assured, at least not at a standard commensurate with the traditional notions of patient-doctor confidentiality5; in response to this last concern, secure, and usually intra-institutional, messaging systems have emerged6, by which the content of messages is protected behind the same firewall that guards all other personal health information, but these privacy measures still do not necessarily overcome the same pitfalls of timing by which a patient's concern may not reach the doctor's attention quickly enough. The duties of responding to patient-authored messaging may be shared with a larger healthcare team, e.g. nurse practitioners and physician assistants, which can accelerate the processing and reaction time but which the patient might perceive as an erosion of confidentiality or as only a facsimile of one-on-one communication with their doctor7.
A further criticism of these exchanges is that they are almost always individualized in the recommendations offered by the doctor. There is rare generalizability, even above and beyond justifiable concern about revelations of identifying details of the patient's presentation by which their confidentiality and anonymity could be compromised. Single-addressee email, or any other traditionally secure direct-to-patient messaging system, is far from an ideal forum in which to share insights that are applicable to multiple patients.
Listservs
In order to disseminate information more widely through email, listservs have been utilized, wherein there are many recipients automatically copied on the same message. The collective nature of this message distribution can instill a sense of community, to the point that listservs have been invoked as a means of psychosocial intervention to help cancer patients and their caregivers lessen their isolation through contact with their peers8,9.
The main disadvantage to this distribution method is the ‘closed loop’ by which only those individuals who sign up for message delivery will have access to the information, and even then with variable relevance to each subscriber. There is no way to ‘opt out’ of reading messages that lack interest, short of choosing not to open emails with unappealing titles or removing oneself from the entire distribution list. Here, logistically, the listserv requires some level of central management, often accomplished by a manual administrator who can add or subtract members and who also assumes responsibility for the conduct of members in the tenor of their exchange. The openness of content generation means that not all information that is distributed has been vetted or validated by a healthcare professional.
Many listservs are still in active existence, but the seminal concept of an online community where like-minded individuals share information provided a crucial stepping stone to non-email-based groups with potentially wider and more inclusive memberships: the modern social networks.
II. Present
If listservs were an early method by which physicians could choose to share health information with patients who were not necessarily “theirs”, i.e. not under their direct care, this broadened online exchange can now occur over a variety of contemporary platforms.
Blogs
Blog is a truncated but more commonly used term for web log. Partly evolving out of the conversational threads of the listservs, blogging has traditionally consisted of an individual sharing their own writing with a passive audience, who access the content by visiting the author's website. Each blog post is static once it is shared, but the blog as a whole is dynamic, typically being refreshed in reverse chronological order as a series of observations. Unless the blog is set up with the interactive capability to record reader comments, this medium does not encourage conversation, but rather represents a more unidirectional way of communicating. Another pitfall is that the blog can be seen as overly personal or even self-centered, as the medium was embraced early on by online diarists.
That said, it can still foster relationships and mutual understanding between the blogger and their readers. Authorship can also be shared in a rotating fashion, e.g. the ASCO Connection (connection.asco.org/commentary.aspx), or even assumed by a cooperative group (http://swog.org/media/frontline/).
Twitter is the quintessential microblog. The service deliberately constrains each message, or Tweet, to a maximum of 140 characters. Unregistered users can read Tweets, which by default are publicly visible, but registration allows a user to post as well, encouraging a call-and-response to the extent that up to 40% of all Twitter activity is conversational in nature (https://www.pearanalytics.com/wp-content/uploads/2012/12/Twitter-Study-August-2009.pdf). A Twitter user can curate the information streamed to their own account by choosing the other users they wish to ‘follow’, and a follower can then choose simply to receive content or to react. The asymmetry of Twitter is often appealing to novices, as “following another user does not require reciprocation, and this may be reassuring to new users who are uncomfortable with the ‘familiarity’ of [social media] connections”10. Whether unidirectional or bidirectional, it is these links between people that establish the network of Twitter's information exchange, and “the growth of a new user's Twitter following is directly correlated with [their] level of engagement with the Twitter ecosystem; such engagement includes contributing meaningful content through link-sharing and commentary, rebroadcasting others' tweets (“retweeting”), and engaging in online dialogue”10.
Retweeting in particular is a way to amplify information that merits repeating, such that the most useful content can be shared with a progressively wider audience. In this manner, health professionals can curate the data stream for one another and their followers, selecting for replication the items they deem newsworthy and helpful. The authenticity of a physician's voice within the Twitter conversation can attract new followers, even if that doctor is not necessarily generating their own novel content (the abbreviation RT denotes a retweet and credits the original author via their Twitter handle, e.g. RT@marklewismd). Hashtags, by which a Tweet is tagged with a pound sign (#) to create a searchable keyword, make items visible to non-followers; for instance, the hashtag #cancer would render a Tweet discoverable to any Twitter user looking for that word, although the lack of specificity could return Tweets about both the disease and the astrological sign (http://www.aacr.org/Documents/Best%20Practices%20for%20Tweeting%20at%20a%20Meeting%20Advocates.docx). Nonetheless, retweets and hashtags can both expand the audience of a Twitter user.
The enforced brevity of Tweets has already raised concern about the extent to which patients can truly and fully become informed through such messaging. The Food & Drug Administration was sufficiently alarmed that they released guidelines governing the behavior of pharmaceutical companies on social media, because “character space limitations may pose challenges for firms in providing a balanced presentation of both risks and benefits of medical products” (http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM401087.pdf).
The oncology community has embraced the service as a tool for discussion among patients and doctors. An analysis of ‘cancer talk’ among patients suggests that dense clusters have formed around disease-specific topics, e.g. prostate cancer, and that the diffuse, multi-connected Twitter web enables relationship-forming in a way that “traditional one-to-many communication technologies cannot support”11. Interestingly, these information nodes tend to reflect grass-roots interest and are seldom centered around the formal accounts of healthcare organizations or the news media.
Meanwhile, oncologists also use Twitter to converse with one another on a professional level, with notable spikes in traffic around the time of national meetings, where attendees proficient and active in social media can share exciting developments with a larger audience, enabling the virtual participation of colleagues who are not physically co-present12. This graphic captures the key physician Tweeters involved in the 2014 ASCO meeting and the specific hashtags they used to aggregate content by cancer type (http://am.asco.org/2014-asco-annual-meeting-tweeters), e.g. #bcsm = breast cancer social media (Figure 1):
Figure 1.
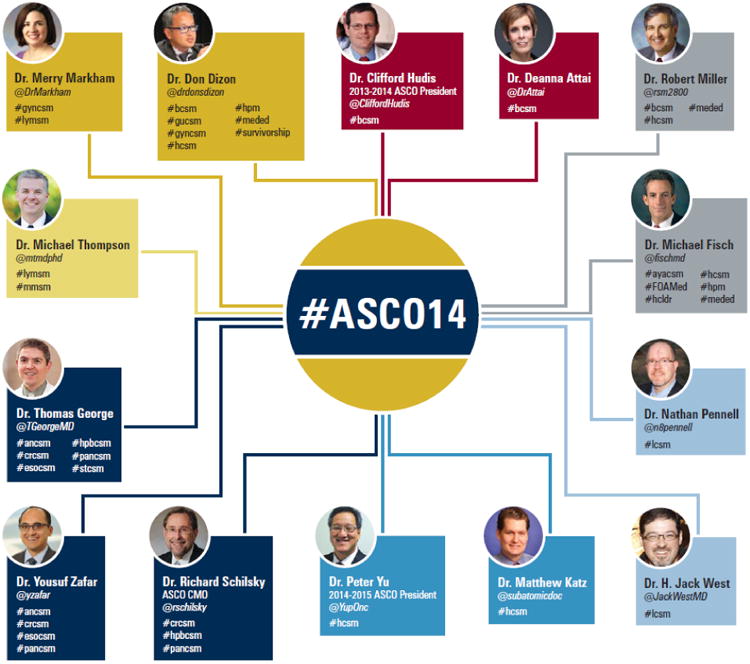
Key Physician Tweeters at 2014 ASCO National Meeting.
Even though Twitter lends itself toward more general observations about healthcare, privacy concerns persist. A Swedish study of doctors and medical students found a 2% rate of “unprofessional” Tweets, most worryingly related to the release of information that could violate patient confidentiality, even when no names or identification numbers were disclosed; other examples of Tweets deemed unprofessional included “[narrating] off-label self-medication with prescription drugs” and “lamenting patient behavior”13.
Facebook is the largest online social network in the world as of this writing. Launched in 2004, it is a platform for user-generated content that, for the most part, requires consent for its connectivity. It relies on users declaring ‘friendships’ with one another, to the extent that the act of agreement to exchange information with another person on the site has turned “friending” into a verb. Each post created by a Facebook user can, at their own discretion, be shared with friends, friends of friends, or everyone, meaning that it is discoverable by search engines outside Facebook.
The very notion of ‘friending’ a patient implies a relationship that might challenge appropriate boundaries and stray beyond the strictly businesslike14. Social networking can mean that “there is no longer a professional remove between many clinicians and their patients”15. Despite all these risks, there are also tremendous theoretical benefits to social media16, particularly in engaging the e-patients who cultivate an interest in their own care.
Potential and Pitfalls
There is a vibrant online community of such advocates, but also of patient-centric healthcare professionals, whose knowledge and experience can counteract the proliferation of unvalidated information and the “Dr. Google” phenomenon17. Within the last decades, the Internet has represented a disruptive technology in the dissemination of medical information, making it searchable to nearly everyone, while at the same time medicine, and oncology especially, has become complex to the point of sub-sub-specialization, requiring true expertise and attention to interpret properly the clinical significance of new findings. Directing patients to the Internet as a source of health information is fraught with issues concerning access (as many peer-reviewed articles remain behind paywalls) and variable quality18, whereas physicians engaged in social media can provide a more trustworthy online route to existing and emerging health information. An even larger inequity in access – the so-called digital divide, wherein members of lower income groups in the U.S. and other countries have less reliable availability of electronic communication – does create an ethical quandary in relying exclusively or predominantly on Internet-driven doctor-patient dialogue19. Older patients are also less like to seek health information online20.
ASCO's current #1 tip for use of social media is to “get involved”, urging oncologists to “take advantage of the greatest opportunity to disseminate credible information and influence both our peers and our patients” (http://www.asco.org/sites/www.asco.org/files/asco_socialmedia_card.pdf). However, to minimize the medicolegal pitfalls of social media engagement, Dizon et al. stress cognizance of policies that determine the appropriateness of online interaction1 (Table 1):
Table 1. Social Media Policies and Guidelines: 10 Common Concepts.
| 1 | Establish ownership of activity. |
| 2 | Establish patient–research subject authorization and consent. |
| 3 | Respect confidentiality of individuals and institutions and compliance with state and federal privacy laws. |
| 4 | Respect copyright. |
| 5 | Separate personal from professional. |
| 6 | Disclose role, relationships, and conflict of interest. |
| 7 | Review state professional licensure requirements. |
| 8 | Review medical records policies and laws. |
| 9 | Review malpractice insurance coverage. |
| 10 | Use disclosures to reinforce the following messages:
|
III. Future
The ideal intersection of interests may then be found in a considerate exchange between engaged patients and clinicians online. Sites such as PatientsLikeMe, described as “a patient-powered research network that improves lives and a real-time research platform that advances medicine”, aggregate similarly affected patients in a manner that affords them strength in numbers but whom are also ripe for study, “generat[ing] data about the real-world nature of disease that help researchers, pharmaceutical companies, regulators, providers and nonprofits develop more effective products, services, and care” (http://www.patientslikeme.com/). Patient-reported outcomes are increasingly recognized as valid endpoints for clinical significance and efficacy. In fact, PatientsLikeMe is already being mined for “quantitative outcome data [that] have the potential to provide an observational environment to monitor [medication] usage and its consequences”21; when such analyses reach similar conclusions as randomized clinical trials it reinforces the notion that “data reported by patients over the Internet may be useful for accelerating clinical discovery”21.
Thus, beyond today's embrace of social media by physicians to promote public health education and to share information with other healthcare professionals, there exists an opportunity to advance the medical field through research. One essential element of any successful clinical trial is the ability to accrue a sufficient number of patients to satisfy the statistical design ensuring that its results are credible and robust. Such recruitment has traditionally occurred through in-person encounters at academic medical centers as well as at well-connected community practices, but is now widening to encompass a less geographically restrictive patient population on the Internet.
This ‘crowdsourcing’ has several supposed advantages, including better congruence of patient to study. In the conventional model of ‘study matching’ the onus was entirely upon the clinician to be aware of available protocols for which a given patient was eligible. Of course, it should still ultimately remain the responsibility of the physician to adjudicate the appropriateness of study enrollment, but now patients, in a full manifestation of their autonomy, can be more involved and educated in the process of trial entry. CureLauncher (http://www.curelauncher.com), as an example, is a patient-facing website that urges individuals affected with serious diseases (not restricted to cancer) to “take control” and “know [their] options” while helping them navigate the thousands of clinical trials active at any one time in the U.S. In a more disease-specific effort, the website Army of Women (http://www.armyofwomen.org) is aiming to recruit up to a million volunteers, comprised of “women and men of every age and ethnicity, including breast cancer survivors, women and men at high-risk for disease, and healthy women and men, to partner with breast cancer researchers”, who can then recruit the enrollees on the website for study; the commitment for patients varies from completion of online questionnaires to the provision of tissue samples, but the website design allows participants to self-select from a range of investigations spanning prevention through treatment. The site also requires investigators to agree to follow the “Common Rule” (45CFR46) federal human subjects regulations and to obtain approval from an Institutional Review Board (IRB) before receiving access to the Army of Women for research purposes (http://researchers.armyofwomen.org/irbapproval).
Indeed, as IRBs govern all contact with study subjects, their jurisdiction extends to communication via social media. While the exact policies vary among research centers, in the U.S. they are all necessarily compliant with the Federal Policy for the Protection of Human Subjects22. These provisions for oversight require IRBs to prospectively review recruitment materials, such that any “advertising that is intended to be seen or heard by prospective subjects to solicit their participation in a study”23 requires pre-approval, regardless of the platform(s) used to invite patients to consider a given trial. Spontaneous communication via social media, e.g. Twitter, is permissible provided it falls within the bounds of general education about a disease, or contains only practical, non-solicitous information about a trial, i.e. study locations where the protocol has been activated22. For investigators seeking to maximize their accruals, a higher likelihood of recruitment has been demonstrably associated with the use of interactive computer programs and the provision of videos educating the public about the condition under study1,24, methods that lend themselves to exactly this non-coercive form of social media outreach.
Thompson et al. describe the enhancement of clinical trial recruitment via social media as the capacity for reaching more people, albeit in an appealingly targeted fashion:
“With hundreds of millions of individuals using [social media] outlets such as Facebook and Twitter, there is an unprecedented opportunity for physicians, healthcare professionals, caregivers, and patients to connect and share critical information in real time. In the past, we used to rely on mass emails and flyers that were mailed out to oncologists nationwide. However, these methods were inefficient and sometimes costly. They mainly targeted oncologists, who were bombarded by so many other flyers and mass emails that notices about important clinical trials wound up in their spam folder--or the wastebasket. In contrast, using [social media] allows the dissemination of the same information to a larger number of individuals, which may include patients and caregivers who have a vested interest in receiving this information. One does not need to know a recipient's street or email address to reach out and communicate. Patients can then ask simple questions about a trial to determine whether they are suitable candidates before they travel to a referring center to participate. They can choose to identify themselves as patients or they can inquire anonymously. Creating an awareness of a clinical trial should follow institutional rules but can be as simple as providing a link to the trial on Clinicaltrials.gov. Providing any additional information may require Institutional Review Board approval (quote with publisher permission)10.”
Some physician-scientists have even been receptive to soliciting patient input during protocol design, so as to overcome or circumvent methodologies that might later prove obstructive to adequate accrual or study maturation.
An important caveat is that, although social media can be used to attract patients to clinical trials, those same individuals' use of the networks may have to be policed during study enrollment to minimize the confounding exchange of information among participants, which could undermine, for instance, attempts at blinding. The lack of anonymity on social media obviously poses “informational risks” and also presents challenges to maintaining in an online forum the confidentiality that is associated with traditional patient care. Principal investigators should thus pursue a partial waiver of the Healthcare Information Portability and Accountability Act (HIPAA) privacy rule, which prohibits collection of personal health information without written authorization; before making initial contact with potential subjects, the researcher seeking to advertise via social media must explain the impracticality of collecting real-world signatures while also detailing the intended use and safeguards for the trial-related information. While recruitment efforts can be routed through third parties like Facebook and Twitter, any personal health information solicited for a study would then ideally be collected via a clinical trial website and firewalled with at least the same level of protection that would be afforded to patient data generated through conventional care22.
As in all other research efforts guided by the Common Rule, any advertisement of payment to study subjects should be preceded by IRB review of “both the amount of payment and the proposed method and timing of disbursement to assure that neither are coercive or present undue influence” [21 CFR 50.20]25.
Overall though, these disadvantages and caveats are likely outweighed by the beckoning promise of “team science”: the advancement of medicine in a manner which is both patient-centric and consistent with the ethos of shared enterprise for the common good that defines the mission of the oncology cooperative groups.
The SWOG and NRG oncology groups are already harnessing the power of electronic messaging in a platform-agnostic manner for digital engagement of physicians and patients alike. For instance, the SWOG trial S1105 (http://www.clinicaltrials.gov/ct2/show/NCT01515800) is an examination of the effectiveness of text-messaging in promoting compliance with aromatase inhibitors (AIs) as adjuvant therapy for women with early-stage hormone receptor-positive breast cancer; messages are sent twice-weekly to patients' mobile phones as a reminder to take their AIs, intermixed with messages offering emotional support and reinforcing the effectiveness of hormone therapy. Urine levels of the drugs and patient-reported adherence are then compared to those of women receiving standard follow-up care. Over 700 patients were enrolled to this trial over a 15-month period, with patients to be followed for 3 years, and, to date, more than 35,000 text messages have been delivered to patients in the text-messaging arm, at a minimal cost.
Far from frivolous, social media initiatives recognize that people are the most important asset within any information platform, and should allow the cooperative groups to preserve and expand their reputations as delivery mechanisms for personalized cancer solutions. At each assembly of SWOG and NRG, educational programs and working groups are held to encourage clinicians and researchers to adopt the professional use of social media, and to overcome knowledge and attitudinal barriers to embracing these tools. In this manner, the sense of community fostered at face-to-face semiannual meetings can be extended online for the remainder of the year, allowing real-time exchange of information at the actual pace of discovery and potentially increasing productivity at the physical conferences. Furthermore, both groups have made a conscious effort to involve patient advocacy groups and oncology research foundations in these events, cultivating their sense of ownership in the process as they can give early input on trial design, assist in crowdfunding efforts for under-resourced projects, and use their influence to encourage trial awareness, patient activation & engagement, and ultimately enhance accrual.
Acknowledgments
The authors wish to acknowledge the valuable contributions of Dr. Michael Fisch and Dr. Dawn Hershman to the review and revision of this manuscript
Grant Support: None
Footnotes
Disclosures: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Mark A. Lewis, Gastrointestinal Medical Oncology and General Oncology, MD Anderson Cancer Center, Houston, Texas.
Adam P. Dicker, Radiation Oncology, Kimmel Cancer Center, Thomas Jefferson University, Philadelphia, Pennsylvania.
References
- 1.Dizon DS, Graham D, Thompson MA, et al. Practical guidance: the use of social media in oncology practice. Journal of oncology practice / American Society of Clinical Oncology. 2012;8:e114–24. doi: 10.1200/JOP.2012.000610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kane B, Sands DZ. Guidelines for the clinical use of electronic mail with patients. The AMIA Internet Working Group, Task Force on Guidelines for the Use of Clinic-Patient Electronic Mail. Journal of the American Medical Informatics Association : JAMIA. 1998;5:104–11. doi: 10.1136/jamia.1998.0050104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fridsma DB, Ford P, Altman RA. Survey of Patient Access to Electronic Mail -Attitudes, Barriers, and Opportunities. J Am Med Inform Assn. 1994:15–9. [PMC free article] [PubMed] [Google Scholar]
- 4.Paul IM, Levi BH. Metastasis of e-mail at an academic medical center. JAMA pediatrics. 2014;168:290–1. doi: 10.1001/jamapediatrics.2013.3934. [DOI] [PubMed] [Google Scholar]
- 5.Katzen C, Solan MJ, Dicker AP. E-mail and oncology: a survey of radiation oncology patients and their attitudes to a new generation of health communication. Prostate cancer and prostatic diseases. 2005;8:189–93. doi: 10.1038/sj.pcan.4500797. [DOI] [PubMed] [Google Scholar]
- 6.Slack WV. A 67-year-old man who e-mails his physician. JAMA : the journal of the American Medical Association. 2004;292:2255–61. doi: 10.1001/jama.292.18.2255. [DOI] [PubMed] [Google Scholar]
- 7.Goodyear-Smith F, Wearn A, Everts H, Huggard P, Halliwell J. Pandora's electronic box: GPs reflect upon email communication with their patients. Informatics in primary care. 2005;13:195–202. doi: 10.14236/jhi.v13i3.597. [DOI] [PubMed] [Google Scholar]
- 8.Lucas MR. A private caregiver ListServ: maximum benefit for minimum cost. Journal of psychosocial oncology. 2011;29:168–74. doi: 10.1080/07347332.2010.548442. [DOI] [PubMed] [Google Scholar]
- 9.Klemm P, Wheeler E. Cancer caregivers online: hope, emotional roller coaster, and physical/emotional/psychological responses. Computers, informatics, nursing : CIN. 2005;23:38–45. doi: 10.1097/00024665-200501000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Thompson MA, Younes A, Miller RS. Using Social Media in Oncology for Education and Patient Engagement. Oncology (Williston Park, NY) 2012;26(9):782–91. [PubMed] [Google Scholar]
- 11.Himelboim I, Han JY. Cancer talk on twitter: community structure and information sources in breast and prostate cancer social networks. Journal of health communication. 2014;19:210–25. doi: 10.1080/10810730.2013.811321. [DOI] [PubMed] [Google Scholar]
- 12.Chaudhry A, Glode LM, Gillman M, Miller RS. Trends in twitter use by physicians at the american society of clinical oncology annual meeting, 2010 and 2011. Journal of oncology practice / American Society of Clinical Oncology. 2012;8:173–8. doi: 10.1200/JOP.2011.000483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brynolf A, Johansson S, Appelgren E, Lynoe N, Edstedt Bonamy AK. Virtual colleagues, virtually colleagues--physicians' use of Twitter: a population-based observational study. Bmj Open. 2013;3 doi: 10.1136/bmjopen-2013-002988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wiener L, Crum C, Grady C, Merchant M. To friend or not to friend: the use of social media in clinical oncology. Journal of oncology practice / American Society of Clinical Oncology. 2012;8:103–6. doi: 10.1200/JOP.2011.000357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jain SH. Practicing medicine in the age of Facebook. The New England journal of medicine. 2009;361:649–51. doi: 10.1056/NEJMp0901277. [DOI] [PubMed] [Google Scholar]
- 16.George DR. “Friending Facebook?” A minicourse on the use of social media by health professionals. The Journal of continuing education in the health professions. 2011;31:215–9. doi: 10.1002/chp.20129. [DOI] [PubMed] [Google Scholar]
- 17.West HJ. Practicing in partnership with Dr. Google: the growing effect of social media in oncology practice and research. The oncologist. 2013;18:780–2. doi: 10.1634/theoncologist.2012-0453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Anderson AS, Klemm P. The Internet: friend or foe when providing patient education? Clinical journal of oncology nursing. 2008;12:55–63. doi: 10.1188/08.CJON.55-63. [DOI] [PubMed] [Google Scholar]
- 19.Virji A, Yarnall KS, Krause KM, et al. Use of email in a family practice setting: opportunities and challenges in patient- and physician-initiated communication. BMC medicine. 2006;4:18. doi: 10.1186/1741-7015-4-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kontos E, Blake KD, Chou WY, Prestin A. Predictors of eHealth Usage: Insights on The Digital Divide From the Health Information National Trends Survey 2012. Journal of medical Internet research. 2014;16:e172. doi: 10.2196/jmir.3117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wicks P, Vaughan TE, Massagli MP, Heywood J. Accelerated clinical discovery using self-reported patient data collected online and a patient-matching algorithm. Nature biotechnology. 2011;29:411–U230. doi: 10.1038/nbt.1837. [DOI] [PubMed] [Google Scholar]
- 22.Gearhart CA. IRB Review of the Use of Social Media in Research. Quorum Review Monitor. 2012 [Google Scholar]
- 23.Guidance for Institutional Review Boards and Clinical Investigators; Recruiting Study Subjects - Information Sheet. Accessed at http://www.fda.gov/RegulatoryInformation/Guidances/ucm126428.htm. [Google Scholar]
- 24.Caldwell PHY, Hamilton S, Tan A, Craig JC. Strategies for Increasing Recruitment to Randomised Controlled Trials: Systematic Review. Plos Med. 2010;7 doi: 10.1371/journal.pmed.1000368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Guidance for Institutional Review Boards and Clinical Investigators; Recruiting Study Subjects - Information Sheet. Accessed at http://www.fda.gov/RegulatoryInformation/Guidances/ucm126429.htm. [Google Scholar]


