Abstract
New and emerging mobile technologies are providing unprecedented possibilities for understanding and intervening on obesity-related behaviors in real time. However, the mobile health (mHealth) field has yet to catch up with the fast-paced development of technology. Current mHealth efforts in weight management still tend to focus mainly on short message systems (SMS) interventions, rather than taking advantage of real-time sensing to develop Just-In-Time, Adaptive Interventions (JITAIs). This paper will give an overview of the current technology landscape for sensing and intervening on three behaviors that are central to weight management; diet, physical activity, and sleep. Then five studies that really dig into the possibilities that these new technologies afford will be showcased. We conclude with a discussion of hurdles that mHealth obesity research has yet to overcome, and a future-facing discussion.
Keywords: obesity, mHealth, sensors, real-time, Just-In-Time, adaptive interventions
Introduction
New mobile technologies, including wearable, deployable, and ingestible low-energy sensors, coupled with ever-improving, data-hungry and ubiquitous smart phones, are providing unprecedented opportunities for innovation in obesity prevention and treatment1–3. These mobile, digital, interactive (mHealth) technologies offer solutions that could significantly revolutionize current practice. For obesity research and interventions, mHealth offers new ways to track the three major obesity-related behaviors, i.e. diet, activity and sedentariness, and sleep4. Smartphone/watch interfaces provide avenues for acquiring ecologically valid, momentary information on participant experience directly from participants via Ecological Momentary Assessment (EMA)5. Through wearable and deployable sensors, often linked wirelessly to a smartphone/watch, behaviors can now be tracked ubiquitously and continuously, with little or no effort from the user. These behaviors can also be tracked in context, with sensors continually gleaning information on environmental and social surroundings. The combination of sensors linked wirelessly to mobile computers (smartphones, smart watches, tablets) provides the interactivity needed to deliver Just-in-Time, Adaptive Interventions (JITAIs). JITAIs are ecologically sound because at least some elements are delivered ‘in the wild’, i.e. as people go about their daily lives. Intervention elements are adapted over time to an individual’s changing status and contexts. Because JITAIs can be delivered remotely, they can be delivered at the moment and in the context that the person needs it most and is most likely to be receptive. Using incoming sensor and EMA data, intervention dose and content can be regularly adapted according to participant data6. However, most mHealth interventions to date have focused on short message systems (SMS) interventions that may not be responsive to changes in participant behaviors7–9, and few have taken advantage of the possibilities that mHealth technologies have to offer2.
This review will give a brief overview of cutting edge mHealth technologies for obesity sensing and intervention, and highlight some of the capabilities that a combination of these approaches can provide. The purpose is not to exhaustively review all interactive interventions for obesity prevention and treatment, as several excellent recent reviews are available2, 7, 9, 10. Rather, five innovative mHealth studies that have employed multiple interconnected mHealth technologies to achieve obesity-related behavior change will be showcased. We conclude with some of the hurdles that mHealth obesity research has yet to overcome, and a future-facing discussion.
Fast-paced development of mobile technologies for obesity prevention and treatment
Physical activity and sedentary behavior
Sensing for physical activity and sedentary behavior has become increasingly sophisticated. Some research grade accelerometers now provide streaming, blue-tooth enabled data, and researchers as well as industry are quickly developing mobile tools to facilitate their use11. These include combinations of smartphone applications (apps) that interact with a computer interface to allow researchers and health professionals to track accelerometer wear, check that it is providing good data, and receive and eventually react to the data in real time. These technologies and cut-points to determine energy expenditure have been rigorously validated in various populations12, 13. Pattern recognition techniques can be developed to recognize specific activities as they occur, such as sitting, standing or walking, using data from sensors and smartphones14–16. More recently, popular wearable devices and phone apps for capturing physical activity have also been tested for accuracy17, and depending upon the research question and main outcomes, these, too can be used to inform interventions. To intervene in the moment or ‘Just in Time’, researchers need to be able to obtain physical activity and sedentary data in real- or ‘near’-time. Many off-the-shelf accelerometers and activity trackers do not yet provide streaming data and/or an open application programming interface (API), which allows researchers to access data and harmonize software and hardware. Therefore, some researchers continue to develop and test their own accelerometers18, or their own applications that can derive momentary physical activity estimates from the raw accelerometer data obtained by smartphones14, 19.
Diet and eating behaviors
Accurate measurement of diet remains the ‘wicked problem’ in obesity research, as well as in mobile health. Currently, the two avenues most explored in mobile health are the detection of nutrient intake using pictures, and the detection of eating episodes and/or caloric intake using sensed wrist20 or jaw21 movements. Pictures are either taken by the participant on a smartphone and uploaded to a server manually22, or acquired and uploaded automatically by a wearable device that takes pictures continually, for instance every 2 seconds23. While the wearable device might be more likely to capture all eating events since it does not depend upon participants’ conscious effort to take and upload a picture, both technologies utilize image upload and analysis. The timespan between upload, analysis and report back to participant or health professional is not fully delineated, and the ongoing effort to validate pattern recognition for the major foods from various cultures is immense. One wrist-worn device can relatively accurately detect eating through wrist movements24, has shown some promise in assessing caloric intake ubiquitously25, and gives real-time feedback on amount eaten. A possible disadvantage of the wrist sensor discussed here is that it must be turned on by the participant prior to every eating event, and switched off afterwards.
Sleep
Sleep sensing and feedback has taken off in the last few years, using both wearable and deployable sensors. Sleep measures using wrist worn actigraphy have been validated using research-grade accelerometers26, 27, and some of these are beginning to provide streaming data that will allow for immediate data capture, analysis and real-time feedback. Several commercially available wrist- or chest-worn devices measure physical activity and sleep, provide some immediate feedback and some access to data through open APIs, although few have been validated for sleep measurement28. The Lullaby deployable bedroom sensor suite is an example of a research project that provided extensive sensing of the sleep environment (temperature, light, sound and motion) and immediate feedback29. There is a growing crop of commercially available bedroom sensors for placing under the mattress30, 31 or near/on the bedside table32, with varying degrees of real- or near-time feedback, validation, and open APIs. However, the field is progressing rapidly, with an increasing focus on open source coding33.
Physical environment and social context
All obesity-related behaviors take place in context, and context impacts behavior34. One of the great strengths of mobile technologies is the ability to capture data on behavioral environments and contexts in an ongoing fashion. King, Glanz, and Patrick recently outlined some of the major advances in environmental context-based sensing and intervention35. Built environmental sensing at the individual level is based on the use of global positioning systems (GPS) that can track personal location. Most smartphones can now track location quite adequately. To contextualize behavior, GPS data is often integrated with geographic information systems (GIS) data, i.e. layers of maps that provide information on various components of the physical environment. Other wearable and deployable sensors, such as cameras36, Radio Frequency Identification (RFID)-type tags, light and sound sensors (many integrated into smartphones) can gather data that can improve insight into obesity-related behaviors such as sleep (ambient noise), diet (food purchases) and physical activity (air quality, weather). Many of these have been integrated with smartphones.
Obesity-related behaviors are also influenced by social context. Important advances are being made in sensed social contexts that go beyond Facebook, Twitter and other rich sources of social network data. A combination of sensors and smartphone applications allow automated recognition, so that time spent in proximity to another specific person can be quantified and reciprocal influences on behavior can be observed and modified37. A great deal of progress has also been made in sensing length and quality of social interactions using ambient sounds via smartphones or other wearable technologies38. Research has repeatedly shown that sensed and perceived environments do not necessarily overlap, and both have impact upon behavior39. Furthermore, behaviors tend to cluster and mutually impact each other, suggesting that multiple behavior change models might be the most parsimonious. Therefore, integrated systems40 that take advantage of multiple sensors and analytic methods to understand obesity-related behaviors in context provide the most compelling tools data to support contextualized JITAIs.
The central role of the smartphone: Sensing and integration
At the center of this transformation in mHealth is the ever-evolving computer that we carry in our pockets and purses, i.e. the mobile phone. As of January 2014, 90% of American adults owned mobile phones, and as of October 2014, 64% owned smartphones41. African Americans (70%) and Hispanics (71%) are more likely than whites (60%) to own a smartphone. There are no differences in mobile phone ownership between these groups. Worldwide, in 2014 there was a 96% penetration of mobile cellular subscriptions, with 59% coverage in least developed countries (LDCs). Smartphone ownership is also increasing worldwide42. Smartphones provide a hub for the Internet of Things (IoT)43. Relatively low-cost Bluetooth enabled digital scales can provide fairly accurate weight, BMI and body fat data to smartphones and back-end servers44. Data from the phone and its sensors (calls, SMS, email, pictures, accelometry, GIS, ambient sound, apps, etc.) as well as data from connected wearable and deployable sensors can be gathered, stored, analyzed, and sent to the cloud or backend severs for storage and analysis. EMA responses and Ecological Momentary Interventions (EMI) can be delivered in text format on mobile phones as well as smartphones. The smartphone also has capacities for providing feedback using sounds, haptics and/or visualizations45. The smartphone is poised to assume an even more critical role in health research, promotion and care with the development of tools such as ResearchKit46. Research Kit was developed for the iPhone, and currently comprises 3 customizable modules: informed consent forms, surveys, and real-time active tasks (these include gait and motor activities, walk tests of fitness, spatial memory tests of cognition, and phonation voice tests). New modules will likely be developed and integrated with iPhone’s health and fitness data collection capabilities (such as step counts, data from incorporated apps, sleep-wake cycles, and more). Smart watches with embedded sensors, watch-to-phone connectivity, communication options and burgeoning capabilities are poised to augment smartphones as hubs for mHealth research, intervention and prevention.
Some interim conclusions regarding fast-paced mHealth technology development: Challenges and opportunities
Challenges
The previous section has provided an overview of some new technologies for sensing behavior and environment as they relate to obesity. The fast-paced development of mHealth-relevant technologies poses several challenges. Technology turnover is one such challenge. Technologies might become obsolete or be discontinued during a project that relies upon them, or they can be upgraded, rebranded or replaced with superior technologies. This technology turnover makes it difficult to identify and maintain mobile technologies for longitudinal intervention studies. Upgrades and new software can disrupt an intervention and require new programming. Therefore, the field is moving towards new, more agile research designs47, 48 that support ongoing personalization and optimization, as well as the adoption of new technologies where necessary or advisable. Other major challenges include privacy, security, confidentiality, and the problem of ‘secondary’ or ‘unintended’ participants, whose data might be collected unintentionally and without their consent by wearable or deployable sensors49.
Opportunities
Because the mobile phone is so ubiquitous, mHealth has the potential to improve access, understanding and services for hard-to-reach populations. Ubiquitous mHealth technologies are also providing unprecedented opportunities to understand behavior in place, time and context through ongoing access to temporally dense, highly contextualized data50. Interactive technologies for real-time, contextualized obesity monitoring and interventions provide a level of ecological validity only attainable through observation and intervention ‘in the wild’51. Methods that sample experiences in everyday environments and circumstances may be much more representative of people’s everyday lives than more traditional laboratory observations. Methods that intervene in everyday circumstances may provide more useful and effective ways of helping people to change their lives in the moment than more traditional interventions that occur outside daily, lived experience. mHealth technologies currently offer six different modalities for real-time data collection and JITAI intervention delivery: Signal-contingent, time-based, event-based, location-based and sensor-based. Data can be collected or people can receive interventions based on a certain time schedule, for instance at predicted mealtimes, or every two hours, or at random signals (signal-contingent). Event-based data collection is when a participant reports specific occurrences, for instance temptation to drink52. Using GPS, data collection and/or JITAIs can be contingent on sensed location53. Using streaming sensor data, interventions, EMAs or other data collection can be contingent on sensed behavior, such as a certain amount of time spent in sedentary behavior54. These modalities can be combined in many ways, for instance a sensor-based plus time-based intervention that only intervenes on sedentary behavior in children after school. Finally, interactive mHealth technologies provide streaming data that can be used to adapt the intervention to the needs of the participant, according, for instance, to momentary availability to be able to react to prompts55, or changes in participant behaviors56. For instance, if an intervention to reduce sugar intake focuses on reduction of sugar sweetened beverage intake, and one participant is quickly successful while another still struggles, intervention goals can be personalized and adjusted on a momentary basis to fit the needs of each individual participant according to available data in real- or near-time.
JITAI Case studies
As mentioned in the introduction, few mHealth obesity-related prevention or treatment programs have made creative use of the possibilities that fast-paced technology development has to offer. Several have pioneered developments of innovative technologies to intervene in real time57–59, (or see 2, 60), few have made it past the design stage into interventions. There are some notable exceptions. Five true Just-In-Time, Adaptive, obesity-related mHealth interventions are highlighted here.
JITAIs in adults
The Engaged Trial 61–63
The E-Networks Guiding Adherence to Goals in Exercise and Diet (ENGAGED) study was a randomized controlled trial (RCT) that used a theory-guided, technology-supported weight loss program. Engaged was based on lessons learned from the Diabetes Prevention Program64, social networks theory, and the control systems theory of self regulation65. This theory posits that self-regulation can be understood in terms of feedback loops, where people set a goal, self-monitor their behavior, and then modify their behavior to reduce perceived discrepancy between their behavior and their goals. Engaged was a 6-month, two-armed RCT. Sixty-nine adults (aged 28–86 years, 85.5% men, 30.4% minority) were randomized to Intervention or Intervention + mobile. Both groups attended biweekly 1.5-hour sessions led by dieticians, psychologists, or physicians. Intervention + mobile participants received a personal digital assistant (PDA) loaded with an interactive study app and a study accelerometer which they were asked to wear. The diet section of the Engaged app required self-entry of dietary intake. Fans were coded in traffic light colors that showed how many calories and how much fat participants had eaten during the day relative to the dietary allowances set up with interventionists. Green signified that the participant could still eat some calories or fat during the day, red indicated that the calorie or fat allowance had been exceeded. The app was also equipped with a physical activity thermometer that automatically accrued data from the study accelerometer but also allowed for manual entry. The green physical activity thermometer showed how may minutes of moderate intensity exercise the participant had reached towards their weekly goal. Participants were also put into teams, and teams competed against one another. Color-coded information was shown about team members weight loss and diet and activity behaviors. Team members could use a private message board to support one another, offer help and cheer each other on. Data were sent to an interventionist who monitored recording compliance and behavior, and then provided personalized coaching by telephone. The intervention + mobile group lost 3.9 kg more that the intervention only group (95% CI, 2.2–5.5 kg), representing 3.1% more weight loss.
Mobile Motivational Frame Testing 45
In this study, three different smartphone apps to promote regular physical activity and reduce sedentary behavior were developed. Each app was based on distinct motivational frameworks from behavioral science. One app was based on an “analytic” framework, using principles from the Social Cognitive Theory 66 and self-regulation theories67. The analytic app showed two dials that quantified amounts of time spent in moderate-to-vigorous physical activity and time spent sitting, and how close the person was to reaching their preset goals. The analytic app also provided some problem solving around barriers to behavior change, informational tips or advice for behavior change, text-based reinforcement when a participant reached their goals, and a graphic display of past physical activity and sitting time. The second app was based on a “social” framework. A second physical activity app applied a social influence framework68. The social app showed a live wallpaper display of individual avatars representing the user and other study participants randomized to use this app who had been assigned to the user’s “virtual group” as well as the members of a second “virtual group” that did not include the user. Each of the avatars was shown in activities (like lying down, or running) that reflected how active the person had been up to that moment in the day. Feedback on activity levels of the user was displayed along with cumulative feedback on the user’s group and feedback about the other virtual group. (i.e., social norm comparisons and contextualization). Similar to the analytic app, a history tab was available to show a visual summary of their overall activity history, but this history tab always referenced the group averages. A participant electronic “message board” was available for participants to post information or comments to their virtual group in real-time. The third app used an “affective” motivational framework based on operant conditioning principles69 and the idea of emotional transference to an avatar. The avatar appeared in the glanceable display as a bird was used to reflect how active/sedentary the user was throughout the day. The bird changed behavior, posture and position depending upon how active the user was up to that point in the day, and only appeared happy if the participant reached at least 30 minutes per day of moderate-to-vigorous physical activity or less that 8 hours of sitting. As the participant got more active, the bird might engage in other behaviors, like moving toward and following the person’s touch on the screen. There was also a screen where participants could play games with the bird. The three apps were further integrated with a fourth app that compiled and analyzed the built-in accelerometer data collected on a continuous basis from the project smartphones. This app was programmed to provide “just-in-time” feedback to users of all three of the behavior change apps using validated algorithms based on the national recommendations for physical activity (i.e., 150 minutes or more per week of moderate-intensity physical activities such as walking). Participants (68 adults aged 45–81 years, mean age 59.1 years, 69% white), were randomized to one of the three apps to participate in an 8-week trial. All but one participant used the smartphone and app for at least 5 weeks. All three groups increased weekly minutes of brisk walking (Mean minutes/week increase ± SD: Analytic=71.1 ± 147.3; Social=122.9 ± 153.3; Affect=105.7 ± 187.2). Self-reported minutes of television viewing decreased across all three apps on an average of 29.1 ± 84.5 minutes/day with no statistically significant differences across apps.
B-MOBILE 54
The B-MOBILE study was designed to intervene on sedentary behavior in real time. Participants received a study mobile phone loaded with the B-MOBILE app. The app used real-time accelerometry data from the smartphone and validated algorithms to estimate sedentary time. It included sedentary behavior goal-setting, prompting, and feedback using an automobile dashboard that was visible when the smartphone display was active. The dashboard included a fuel gage that showed the number of sedentary minutes remaining until the next activity break, two odometers that tracked total number of sedentary and active minutes accumulated during that day. If a participant reached the preset limit of minutes spent in sedentary behaviors, the app beeped and an on screen message appeared reminding the participant to take an activity break. Participants could respond to the prompt by being active, silencing the prompt, or delaying the prompt for 30 minutes. Real-time accelerometry from the phone was used to determine when a participant was compliant to the prompt. If a participant successfully complied by performing physical activity for the recommended duration, they received a praising message, a bright green light appeared on the dashboard and the fuel gauge on the screen was updated. Because so little is known about how best to intervene on sedentary behavior in real time, the B-MOBILE study compared 3 different conditions, each followed for a 7-day period and presented in a counterbalanced order: (1) 3-min break prompt after 30 continuous sedentary minutes; (2) 6-min break prompt after 60 continuous sedentary minutes; and (3) 12-min break prompt after 120 continuous sedentary minutes. Participants were 30 overweight/obese adults (mean age 47.5 ± 13.5, 83.3% female, 66.7% white). Percent time spent in sedentary behavior decreased significantly in all 3 conditions relative to baseline (p =.005). Pairwise comparisons showed that the 3-min physical activity break condition produced significantly greater reductions in percent time spent sedentary compared to the 12-min physical activity break condition (p=0.04).
Within-Person Variance-Based Adaptive Intervention 56
This adaptive intervention harnessed within-person variance in physical activity to adjust individuals’ goals and feedback over time. The intervention was based on principles from Behavioral Economics70 and Operant Shaping71. Participants received a pedometer and were instructed on how to upload their pedometer data on a daily basis. They participated in a 10-day run-in phase to allow participant reactivity to the pedometer to subside, collect of baseline physical activity data, and determine whether participants were willing and able to upload their pedometer data to the Microsoft’s HealthVault. Those who successfully uploaded their data (n=20 inactive overweight adults, 85% women, mean age= 36.9±9.2 years, 35% non-white) were randomized to one of two conditions: 1) Static Intervention (SI), or 2) Adaptive Intervention (AI) intervention. Participants in both groups received health information and one brief message prompt (#160 characters) every 9 days to encourage physical activity. On the first day of the interventions, the Static Intervention group received the goal of 10, 000 steps per day at least 5 days a week. They were reminded of this goal on a monthly basis. The adaptive intervention group was prescribed new, personalized goals every day that adapted to their physical activity levels. To calculate these goals, the participants needed to send their cumulative pedometer step count to the research team every evening or early morning. Once the data was sent, the new goal, good for only one day, was sent back. The personalized, adaptive goal was calculated by taking the 60th percentile of that person’s physical activity data from the previous 9 days, using a moving window. SI participants received encouraging social feedback. AI participants received differential feedback messages depending on whether or not they met their daily goal. AI Participants who did not meet the goal received a simple confirmation that steps were entered correctly and were provided their next day’s goal. AI participants who met their goals received positive feedback in the form of encouragement and praise messages. SI participants received encouraging escalating financial incentives in the form of gift cards each month for uploading their pedometer steps to Microsoft HealthVault. AI participants received encouraging feedback and one point worth $1 for accomplishing each step goal. Points were not lost for missing a daily goal or failing to report step counts. Points were exchanged for e-gift cards to non-food retailers. Cumulative award amounts for both groups were similar. After adjusting for covariates, significant increases in physical activity were shown relative to baseline (p<.001), with a significant group interaction (p = .017). The SI group increased steps by an average of 1,598 steps/day between baseline and end of treatment. The AI group increased steps by an average of 2,728 steps/day between baseline and end of treatment, with a significant difference between groups of 1,130 steps/day.
JITAIs in children
Utilization of interactive technologies in mHealth studies in children and adolescent is limited despite reported acceptability and efficacy2. Aside from some very innovative early developmental work72, to our knowledge KNOWME Networks is the first JITAI to be delivered in children. The KNOWME Networks system integrates off-the-shelf sensors with a mobile phone and a secured website to reduce sedentary behavior (lying down, sitting, standing) and promote physical activity in overweight Hispanic adolescents. Development of the system was conducted using a three-session iterative user-centered design approach, which yielded a suite of interactive technologies that consisted of:
a wearable body area network (WBAN) with 2 Alive Technologies73 Bluetooth-enabled wireless combined heart rate/activity monitors,
a mobile phone app developed in-house74 that collected, analyzed, and displayed visualizations of participants’ physical activity and sedentary behavior based on personalized algorithms,
and a secure server and web-based dashboard that received & analyzed data transmitted from the mobile phone app every 10 minutes (near-time).
The development of the KNOWME system and the personalized physical activity algorithms that were used to detect specific activities has been detailed earlier14, 74, 75.
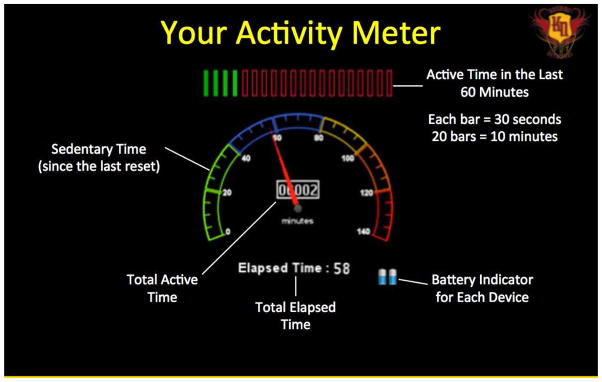
The KNOWME Networks pilot study aimed to decrease minutes spent in sedentary behaviors in overweight Hispanic youth. Ten Hispanic adolescents (mean age 16.3 ± 1.7, mean BMI percentile 97.2 ± 4.4, 50% female) completed a comprehensive intake interview and wore an Actigraph accelerometer from Friday after school to Sunday bedtime in order to collect baseline physical activity data. Within two weeks of baseline measurement, participants wore the KNOWME sensors, an Actigraph accelerometer, and carried a study phone equipped with the KNOWME ‘sedentary analyzer’ app (Figure 1) from Friday after school to Sunday bedtime for this pilot study. The KNOWME app transmitted the data from the heart rate/activity monitors to a secure backend server and website display that allowed researchers to monitor sensor status (wear and function) and cumulative minutes of physical activity and sedentary behavior throughout the day. Minutes of time spent in sedentary activities were also displayed to the participants in near-time on the KNOWME smartphone app (Figure 1). If a participant reached two hours of consecutive sedentary behavior, the phone automatically ‘beeped’ them with a ‘MOVE’ message and alerted researchers on the back end. If participants did not respond to the ‘MOVE’ message within 10 minutes, researchers initiated an SMS conversation aimed at immediately motivating the child to get some minutes of physical activity. Researchers were trained to provide timely feedback based on MI principles, and tailored precisely to the participant through use of the intake data about their home and neighborhood environments. Participants were able to reset the sedentary analyzer and avoid being alerted by being physically active for 10 consecutive minutes. Participants could also alert the researchers that they were unavailable to respond (for instance “I am having dinner at my grandmother’s”).
Figure 1.
Display of ‘sedentary analyzer’ KNOWME app that appears on the study phone. The app collects data from KNOWME’s Bluetooth enabled wearable sensors, analyses the data on the fly, and sends it to the secure KNOWME website and dashboard.
Results of the pilot study showed that participants accrued 170.8 minutes (p<0.1) less sedentary minutes using KNOWME as compared to baseline data, which is highly clinically significant. During the 2.5 day KNOWME wear weekend, an average of 43.1 ± 15.9 SMS were sent to participants by the research team. Lagged mixed regression analysis was completed using a subset of data (consisting of ten-minute time intervals from a mean of 10 hours of data per day) to determine if texts sent to participants were associated with an increase in physical activity in the following ten-minute period. Physical activity as measured by accelerometer counts was significantly higher (β=1046.44, p<0.01) after SMS messages from the research team were received compared to when no SMS messages were received.
We hypothesized that only MI-adherent message content would be related to changes in activity behaviors. SMS messages sent to participants were coded post-hoc using a scheme adopted from Motivational Interviewing framework (MI) 76. Messages sent by the researchers were categorized as 1) prompts (MI adherent): questions that asked participants think about what they could do to be physically active, 2) affirmations (MI adherent): commending participants for engaging in physical activity, 3) suggestions (non MI-adherent): suggesting specific activities, or 4) housekeeping (unrelated to MI): logistic messages about KNOWME wear, messages such as ‘good morning’, informal conversations about what the participant’s day was like, etc. Lagged mixed regression analyses showed that accelerometer counts were 2411.18 higher in the 10-minute period (p<0.001) after a prompt was sent, and 3183.61 counts higher in the 10-minute period (p<0.001) after an affirmation was sent relative to when no messages or other types of messages were sent.
Conclusion
Each of the studies showcased here has strengths and weaknesses. Most importantly, as technology moves forward, one can imagine each study adapting to incorporate these advances. For instance, in the Engaged Trial, data from the apps had to be manually uploaded in order for the interventionists to access. Now, that upload could be automated and continuous, allowing for the interventionists to give more personalized real-time feedback and adapting goals in a more agile fashion. In the Mobile Motivational Frame Testing study, a combination of an updated interface that collected, transmitted and analyzed participant progress in an ongoing fashion with a SMART research design77 could be used to determine which of the apps works best for which person, and adapt their group assignment accordingly. For the B-MOBILE and Within-Person Variance-Based Adaptive Intervention studies, more sophisticated wearable sensors and a study dashboard that showed ongoing physical activity status could enable combination of the two approaches. In combination with a MOST study design77 an adaptive study could be developed that did not rely on participant data upload and could test the various conditions for different participants. For the KNOWME study, advances in Natural Language Processing78 might be used to help automate some of the intervention, rather than relying on constant humans-in-the-loop. As to other possibilities, for instance, while these studies were all innovative, none took advantage of GPS, GIS, microphone or other types of data to understand and intervene on behavior taking social and environmental context into account.
Two recent articles have outlined hurdles facing the mHealth community50, 79. The fact that the field changes so quickly is one of the major challenges. Technical innovation and clinical discoveries can make new interventions outdated before they are published. The rush to market of untested apps and gadgets can lead consumers and providers to use interventions that do not have proven efficacy. The transdisciplinary teams have yet to overcome the Tower of Babel problem and learn to understand each other’s jargon and basic assumptions. Behavioral theories or models that can guide JITAIs have yet to be developed, and we have yet to develop best practices to utilize (in real time) the vast amount of real-time data that we are receiving from sensors and EMA. These two articles also provide some strategies for increasing the speed and usefulness of mHealth research. These involve (but are not limited to) using efficient study designs, enhancing transdisciplinary communications, and the development of new gold standard measures and new behavioral models. Future mHealth obesity-related research and interventions will have increasingly sophisticated technologies to work with, and hopefully they will take full advantage of these fast-paced developments.
Acknowledgments
Dr. Spruijt-Metz reports grants from National Institutes of Health (NIMHD 3P60MD002254-02S1).
Footnotes
Conflict of Interest
D. Spruijt-Metz, C.K.F. Wen, G. O’Reilly, M. Li, S Lee, B.A. Emken, U. Mitra, M. Annavaram, G. Ragusa, and S. Narayanan declare that they have no conflict of interest.
Compliance with Ethics Guidelines
Human and Animal Rights and Informed Consent
Contributor Information
C.K.F. Wen, Email: chengkuw@usc.edu.
G. O’Reilly, Email: goreilly@usc.edu.
M. Li, Email: mingli1@cmu.edu.
S Lee, Email: itools@gmail.com.
B.A. Emken, Email: adarandjeremy@gmail.com.
U. Mitra, Email: ubli@usc.edu.
M. Annavaram, Email: annavara@usc.edu.
G. Ragusa, Email: ragusa@usc.edu.
S. Narayanan, Email: shri@sipi.usc.edu.
References
Papers of particular interest, published recently, have been
highlighted as:
• Of importance
•• Of major importance
- 1.Kaplan RM, Stone AA. Bringing the Laboratory and Clinic to the Community: Mobile Technologies for Health Promotion and Disease Prevention a. Annu Rev Psychol. 2013;64:471–98. doi: 10.1146/annurev-psych-113011-143736. [DOI] [PubMed] [Google Scholar]
- 2.Turner T, Spruijt-Metz D, Wen C, Hingle M. Prevention and treatment of pediatric obesity using mobile and wireless technologies: a systematic review. Pediatric Obesity. 2015 doi: 10.1111/ijpo.12002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thomas JG, Bond DS. Review of innovations in digital health technology to promote weight control. Curr Diab Rep. 2014;14(5):485. doi: 10.1007/s11892-014-0485-1. [DOI] [PubMed] [Google Scholar]
- 4.Spruijt-Metz D. Etiology, Treatment, and Prevention of Obesity in Childhood and Adolescence: A Decade in Review. Journal of Research on Adolescence. 2011;21(1):129–52. doi: 10.1111/j.1532-7795.2010.00719.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- 6.Nahum-Shani I, Hekler E, Spruijt-Metz D. Building health behavior models to guide the development of just-in-time adaptive interventions: A pragmatic framework. doi: 10.1037/hea0000306. Under Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu F, Kong X, Cao J, Chen S, Li C, Huang J, Gu D, Kelly TN. Mobile Phone Intervention and Weight Loss Among Overweight and Obese Adults: A Meta-Analysis of Randomized Controlled Trials. Am J Epidemiol. 2015;181(5):337–48. doi: 10.1093/aje/kwu260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hutchesson M, Rollo M, Krukowski R, Ells L, Harvey J, Morgan P, Callister R, Plotnikoff R, Collins C. eHealth interventions for the prevention and treatment of overweight and obesity in adults: a systematic review with meta-analysis. Obesity Reviews. 2015;16(5):376–92. doi: 10.1111/obr.12268. [DOI] [PubMed] [Google Scholar]
- 9.Wickham CA, Carbone ET. Who’s calling for weight loss? A systematic review of mobile phone weight loss programs for adolescents. Nutr Rev. 2015;73(6):386–98. doi: 10.1093/nutrit/nuu018. [DOI] [PubMed] [Google Scholar]
- 10.Bacigalupo R, Cudd P, Littlewood C, Bissell P, Hawley MS, Buckley Woods H. Interventions employing mobile technology for overweight and obesity: an early systematic review of randomized controlled trials. Obesity Reviews. 2013;14(4):279–91. doi: 10.1111/obr.12006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Actigraph. 2015 cited 2015 July 6; Available from: http://www.actigraphcorp.com/solutions-and-products/activity-monitors/actigraph-link/
- 12.Johansson E, Ekelund U, Nero H, Marcus C, Hagstromer M. Calibration and cross-validation of a wrist-worn Actigraph in young preschoolers. Pediatric Obesity. 2015;10(1):1–6. doi: 10.1111/j.2047-6310.2013.00213.x. [DOI] [PubMed] [Google Scholar]
- 13.Trost SG, Loprinzi PD, Moore R, Pfeiffer KA. Comparison of accelerometer cut points for predicting activity intensity in youth. Med Sci Sports Exerc. 2011;43(7):1360–8. doi: 10.1249/MSS.0b013e318206476e. [DOI] [PubMed] [Google Scholar]
- 14.Li M, Rozgica V, Thatte G, Lee S, Emken A, Annavaram M, Mitra U, Spruijt-Metz D, Narayanan S. Multimodal physical activity recognition by fusing temporal and cepstral information. IEEE Trans Neural Syst Rehabil Eng. 2010;18(4):369–80. doi: 10.1109/TNSRE.2010.2053217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Incel OD, Kose M, Ersoy C. A review and taxonomy of activity recognition on mobile phones. Bio Nano Science. 2013;3(2):145–71. [Google Scholar]
- 16.Mannini A, Intille SS, Rosenberger M, Sabatini AM, Haskell W. Activity recognition using a single accelerometer placed at the wrist or ankle. Med Sci Sports Exerc. 2013 doi: 10.1249/MSS.0b013e31829736d6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Case MA, Burwick HA, Volpp KG, Patel MS. Accuracy of Smartphone Applications and Wearable Devices for Tracking Physical Activity Data. JAMA. 2015;313(6):625–6. doi: 10.1001/jama.2014.17841. [DOI] [PubMed] [Google Scholar]
- 18.Intille SS, Albinali F, Mota S, Kuris B, Botana P, Haskell WL. Design of a wearable physical activity monitoring system using mobile phones and accelerometers. Conf Proc IEEE Eng Med Biol Soc. 2011;2011:3636–9. doi: 10.1109/IEMBS.2011.6090611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hekler EB, Buman MP, Grieco L, Rosenberger M, Winter SJ, Haskell W, King AC. Validation of Physical Activity Tracking via Android Smartphones Compared to ActiGraph Accelerometer: Laboratory-Based and Free-Living Validation Studies. JMIR mHealth and uHealth. 2015;3(2):e36. doi: 10.2196/mhealth.3505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Scisco JL, Muth ER, Dong Y, Hoover AW, O’Neil P, Fishel-Brown SR. Usability and Acceptability of the “Bite Counter” Device. Proceedings of the Human Factors and Ergonomics Society Annual Meeting; 2011; SAGE Publications; 2011. pp. 1967–9. [Google Scholar]
- 21.Sazonov ES, Fontana JM. A sensor system for automatic detection of food intake through non-invasive monitoring of chewing. Sensors Journal, IEEE. 2012;12(5):1340–8. doi: 10.1109/JSEN.2011.2172411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Boushey CJ, Harray AJ, Kerr DA, Schap TE, Paterson S, Aflague T, Ruiz MB, Ahmad Z, Delp EJ. How Willing Are Adolescents to Record Their Dietary Intake? The Mobile Food Record. JMIR mHealth and uHealth. 2015;3(2):e47. doi: 10.2196/mhealth.4087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sun M, Burke LE, Mao ZH, Chen Y, Chen HC, Bai Y, Li Y, Li C, Jia W. eButton: A Wearable Computer for Health Monitoring and Personal Assistance. Proceedings/Design Automation Conference Design Automation Conference. 2014;2014:1–6. doi: 10.1145/2593069.2596678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Desendorf J, Bassett DR, Raynor HA, Coe DP. Validity of the Bite Counter device in a controlled laboratory setting. Eating behaviors. 2014;15(3):502–4. doi: 10.1016/j.eatbeh.2014.06.013. [DOI] [PubMed] [Google Scholar]
- 25.Dong Y, Hoover A, Scisco J, Muth E. A new method for measuring meal intake in humans via automated wrist motion tracking. Appl Psychophysiol Biofeedback. 2012;37(3):205–15. doi: 10.1007/s10484-012-9194-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Johnson NL, Kirchner HL, Rosen CL, Storfer-lsser A, Cartar LN, Ancoli-Israel S, Emancipator JL, Kibler AM, Redline S. Sleep estimation using wrist actigraphy in adolescents with and without sleep disordered breathing: a comparison of three data modes. Sleep. 2007;30(7):899. doi: 10.1093/sleep/30.7.899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Blackwell T, Yaffe K, Laffan A, Ancoli-Israel S, Redline S, Ensrud KE, Song Y, Stone KL. Associations of objectively and subjectively measured sleep quality with subsequent cognitive decline in older community-dwelling men: the MrOS sleep study. Sleep. 2013;37(4):655–63. doi: 10.5665/sleep.3562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jeon L, FINKELSTEIN J. Consumer Sleep Tracking Devices: A Critical Review. 2015. [PubMed] [Google Scholar]
- 29.Kay M, Choe EK, Shepherd J, Greenstein B, Watson N, Consolvo S, Kientz JA. Lullaby: a capture & access system for understanding the sleep environment. Proceedings of the 2012 ACM Conference on Ubiquitous Computing; 2012; ACM; 2012. pp. 226–34. [Google Scholar]
- 30.Paalasmaa J, Waris M, Toivonen H, Leppakorpi L, Partinen M. Unobtrusive online monitoring of sleep at home. Engineering in Medicine and Biology Society (EMBC), 2012 Annual International Conference of the IEEE; 2012; IEEE; 2012. pp. 3784–8. [DOI] [PubMed] [Google Scholar]
- 31.Beddit. Beddit. 2015 cited 2015 July 7; Available from: http://www.beddit.com.
- 32.Hello. Sense. 2015 cited 2015 July 8; Available from: https://hello.is.
- 33.Estrin D, Sim I. Open mHealth Architecture: An Engine for Health Care Innovation. Science. 2010;330(6005):759. doi: 10.1126/science.1196187. [DOI] [PubMed] [Google Scholar]
- 34.Volpp K, Loewenstein G, Asch D. BEHAVIORAL ECONOMICS AND HEALTH. Health Behavior: Theory, Research, and Practice. 2015:389. [Google Scholar]
- 35.King AC, Glanz K, Patrick K. Technologies to measure and modify physical activity and eating environments. Am J Prev Med. 2015;48(5):630–8. doi: 10.1016/j.amepre.2014.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kerr J, Marshall SJ, Godbole S, Chen J, Legge A, Doherty AR, Kelly P, Oliver M, Badland HM, Foster C. Using the SenseCam to Improve Classifications of Sedentary Behavior in Free-Living Settings. Am J Prev Med. 2013;44(3):290–6. doi: 10.1016/j.amepre.2012.11.004. [DOI] [PubMed] [Google Scholar]
- 37.Madan A, Moturu ST, Lazer D, Pentland AS. Social sensing: obesity, unhealthy eating and exercise in face-to-face networks. Wireless Health 2010; 2010; ACM; 2010. pp. 104–10. [Google Scholar]
- 38.Lane ND, Lin M, Mohammod M, Yang X, Lu H, Cardone G, Ali S, Doryab A, Berke E, Campbell AT. Bewell: Sensing sleep, physical activities and social interactions to promote wellbeing. Mobile Networks and Applications. 2014;19(3):345–59. [Google Scholar]
- 39.Spruijt-Metz D, Berrigan D, Kelly LA, McConnell R, Dueker D, Lindsey G, Atienza AA, Nguyen-Michel ST, Irwin ML, JW, MJ, Tatalovic Z, Redline S. Measures of Physical Activity and Exercise. In: Allison DB, Baskin ML, editors. Handbook of Assessment Methods for Eating Behaviors and Weight-Related Problems: Measures, Theory, and Research. 2. Los Angeles, London, New Delhi: Sage; 2009. pp. 187–254. [Google Scholar]
- 40.Ko J, Lu C, Srivastava MB, Stankovic J, Terzis A, Welsh M. Wireless sensor networks for healthcare. Proceedings of the IEEE. 2010;98(11):1947–60. [Google Scholar]
- 41.Pew Research Center. The Smartphone Difference: US Smartphone Ownership 2015. 2015. [Google Scholar]
- 42.International Telecommunication Union. Measuring the Information Society Report 2014. Geneva, Switzerland: 2014. [Google Scholar]
- 43.Kim H, Jin Z, Oh S, Lee M. An Information Provider for Exercise Data using IoT techniques. International Journal. 2015;4(2) [Google Scholar]
- 44.Smith JM. The doctor will see you ALWAYS. Spectrum, IEEE. 2011;48(10):56–62. [Google Scholar]
- 45.King AC, Hekler EB, Grieco LA, Winter SJ, Sheats JL, Buman MP, Banerjee B, Robinson TN, Cirimele J. Harnessing different motivational frames via mobile phones to promote daily physical activity and reduce sedentary behavior in aging adults. PLoS One. 2013;8(4):e62613. doi: 10.1371/journal.pone.0062613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ritter S. Apple’s Research Kit Development Framework for Iphone Apps Enables Innovative Approaches to Medical Research Data Collection. J Clin Trials. 2015;5:e120. [Google Scholar]
- 47.Hekler E, Klasnja P, Riley WT, Buman MP, Huberty J. Agile Science: Creating useful products for sustained behavior change in the real-world. doi: 10.1007/s13142-016-0395-7. under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Almirall D, Nahum-Shani I, Sherwood NE, Murphy SA. Introduction to SMART designs for the development of adaptive interventions: with application to weight loss research. Translational behavioral medicine. 2014;4(3):260–74. doi: 10.1007/s13142-014-0265-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nebeker C. Examining the ethical dimensions of wearable and sensing technologies in mHealth research. 142nd APHA Annual Meeting and Exposition; November 15–November 19, 2014; APHA; 2014. [Google Scholar]
- 50.Spruijt-Metz D, Hekler E, Saranummi N, Intille S, Korhonen I, Nilsen W, Rivera D, Spring B, Michie S, Asch D, Sanna A, Salcedo V, Kukakfa R, Pavel M. Building new computational models to support health behavior change and maintenance: new opportunities in behavioral research. Translational Behavioral Medicine. 2015:1–12. doi: 10.1007/s13142-015-0324-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kaplan RM, Stone AA. Bringing the laboratory and clinic to the community: mobile technologies for health promotion and disease prevention. Annu Rev Psychol. 2013;64:471–98. doi: 10.1146/annurev-psych-113011-143736. [DOI] [PubMed] [Google Scholar]
- 52.Hufford MR, Shields AL, Shiffman S, Paty J, Balabanis M. Reactivity to ecological momentary assessment: an example using undergraduate problem drinkers. Psychology of addictive behaviors. 2002;16(3):205. [PubMed] [Google Scholar]
- 53.Intille SS, Lester J, Sallis JF, Duncan G. New horizons in sensor development. Med Sci Sports Exerc. 2012;44(1 Suppl 1):S24–31. doi: 10.1249/MSS.0b013e3182399c7d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bond DS, Thomas JG, Raynor HA, Moon J, Sieling J, Trautvetter J, Leblond T, Wing RR. B-mobile-a smartphone-based intervention to reduce sedentary time in overweight/obese individuals: A within-subjects experimental trial. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sarker H, Sharmin M, Ali AA, Rahman MM, Bari R, Hossain SM, Kumar S. Assessing the availability of users to engage in just-in-time intervention in the natural environment. Proceedings of the 2014 ACM International Joint Conference on Pervasive and Ubiquitous Computing; 2014; ACM; 2014. pp. 909–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56*.Adams MA, Sallis JF, Norman GJ, Hovell MF, Hekler EB, Perata E. An adaptive physical activity intervention for overweight adults: a randomized controlled trial. PloS one. 2013;8(12):e82901. doi: 10.1371/journal.pone.0082901. This paper gives an excellent example of a Just-in-Time, Adaptive Intervention. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Consolvo S, McDonald DW, Toscos T, Chen MY, Froehlich J, Harrison B, Klasnja P, LaMarca A, LeGrand L, Libby R. Activity sensing in the wild: a field trial of ubifit garden. Vol. 2008. ACM; 2008. pp. 1797–806. [Google Scholar]
- 58.Anderson I, Maitland J, Sherwood S, Barkhuus L, Chalmers M, Hall M, Brown B, Muller H. Shakra: Tracking and sharing daily activity levels with unaugmented mobile phones. Mobile Networks and Applications. 2007;12(2):185–99. [Google Scholar]
- 59.Lin J, Mamykina L, Lindtner S, Delajoux G, Strub H. Fish’n’Steps: Encouraging physical activity with an interactive computer game. UbiComp 2006: Ubiquitous Computing. 2006:261–78. [Google Scholar]
- 60.O’Reilly GA, Spruijt-Metz D. Current mHealth Technologies for Physical Activity Assessment and Promotion. Am J Prev Med. 2013;45(4):501–7. doi: 10.1016/j.amepre.2013.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61*.Pellegrini CA, Duncan JM, Moller AC, Buscemi J, Sularz A, DeMott A, Pictor A, Pagoto S, Siddique J, Spring B. A smartphone-supported weight loss program: design of the ENGAGED randomized controlled trial. BMC Public Health. 2012;12(1):1041. doi: 10.1186/1471-2458-12-1041. Nice overview of how to design a Just-in-Time, Adaptive Intervention. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Spring B, Duncan JM, Janke EA, Kozak AT, McFadden HG, DeMott A, Pictor A, Epstein LH, Siddique J, Pellegrini CA, Buscemi J, Hedeker D. Integrating technology into standard weight loss treatment: a randomized controlled trial. JAMA Intern Med. 2013;173(2):105–11. doi: 10.1001/jamainternmed.2013.1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gotsis BM, Paiva A, Spruijt-Metz D. Healthy Apps: Mobile Devices for Continuous Monitoring and Intervention. IEEE PULSE. 2013;4(6):34–40. doi: 10.1109/MPUL.2013.2279620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Knowler WC, Fowler SE, Hamman RF, Christophi CA, Hoffman HJ, Brenneman AT, Brown-Friday JO, Goldberg R, Venditti E, Nathan DM. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet. 2009;374(9702):1677–86. doi: 10.1016/S0140-6736(09)61457-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Carver CS, Scheier MF. On the self-regulation of behavior. Cambridge University Press; 2001. [Google Scholar]
- 66.Bandura A. Toward a psychology of human agency. Perspectives on psychological science. 2006;1(2):164–80. doi: 10.1111/j.1745-6916.2006.00011.x. [DOI] [PubMed] [Google Scholar]
- 67.Umstattd MR, Wilcox S, Saunders R, Watkins K, Dowda M. Self-regulation and physical activity: The relationship in older adults. American journal of health behavior. 2008;32(2):115–24. doi: 10.5555/ajhb.2008.32.2.115. [DOI] [PubMed] [Google Scholar]
- 68.Basic Behavioral Science Task Force of the National Advisory Mental Health Council. Basic behavioral science research for mental health: Social influence and social cognition. Am Psychol. 1996;51(5):478–84. [PubMed] [Google Scholar]
- 69.Skinner BF. Science and human behavior. Simon and Schuster; 1953. [Google Scholar]
- 70.Sallis JF, Owen N, Fisher EB. Ecological models of health behavior. Health behavior and health education: Theory, research, and practice. 2008;4:465–86. [Google Scholar]
- 71.Epstein LH. Integrating Theoretical Approaches to Promote Physical Activity. Am J Prev Med. 1998;15(4):257–65. doi: 10.1016/s0749-3797(98)00083-x. [DOI] [PubMed] [Google Scholar]
- 72.Toscos T, Faber A, An S, Gandhi MP. Chick clique: persuasive technology to motivate teenage girls to exercise. Vol. 2006. ACM; 2006. pp. 1873–8. [Google Scholar]
- 73.Alive technologies. Alive heart and activity monitor. 2015 cited 2015 July 10; Available from: http://www.alivetec.com/alive-bluetooth-heart-activity-monitor/
- 74.Lee S, Annavaram M, Thatte G, Rozgic V, Li M, Mitra U, Narayanan S, Spruijt-Metz D. Sensing for Obesity: KNOWME Implementation and Lessons for an Architect. Proceedings of the Workshop on Biomedicine in Computing: Systems, Architectures, and Circuits (BiC2009); Austin, TX. 2009. [Google Scholar]
- 75.Emken BA, Li M, Thatte G, Lee S, Annavaram M, Mitra U, Narayanan S, Spruijt-Metz D. Recognition of physical activities in overweight Hispanic youth using KNOWME Networks. J Phys Act Health. 2012;9(3):432–41. doi: 10.1123/jpah.9.3.432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Rubak S, Sandbaek A, Lauritzen T, Christensen B. Motivational interviewing: a systematic review and meta-analysis. Br J Gen Pract. 2005;55(513):305–12. [PMC free article] [PubMed] [Google Scholar]
- 77**.Collins LM, Murphy SA, Strecher V. The multiphase optimization strategy (MOST) and the sequential multiple assignment randomized trial (SMART): new methods for more potent eHealth interventions. Am J Prev Med. 2007;32(5 Suppl):S112–8. doi: 10.1016/j.amepre.2007.01.022. This is a key paper on new agile research designs. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Baron NS. Shall we talk? Conversing with humans and robots. The Information Society. 2015;31(3):257–64. [Google Scholar]
- 79.Baker TB, Gustafson DH, Shah D. How can research keep up with eHealth? Ten strategies for increasing the timeliness and usefulness of eHealth research. Journal of Medical Internet Research. 2014;16(2) doi: 10.2196/jmir.2925. [DOI] [PMC free article] [PubMed] [Google Scholar]