Abstract
HIV-positive adolescents who engage in unsafe sex are at heightened risk for transmitting or re-acquiring HIV. Disclosure of HIV-status to sexual partners may impact on condom use, but no study has explored the effects of (i) adolescent knowledge of one's HIV-status, (ii) knowledge of partner status and (iii) disclosure to partners, on safer sex behaviour. This study aimed to identify whether knowledge of HIV-status by HIV-positive adolescents and partners was associated with safer sex. Eight fifty eight HIV-positive adolescents (10–19 years old, 52% female, 68.1% vertically infected) who had ever initiated antiretroviral treatment in 41 health facilities in the Eastern Cape, South Africa, were interviewed using standardised questionnaires. Quantitative analyses used multivariate logistic regressions, controlling for confounders. Qualitative research included interviews, focus group discussions and observations with 43 HIV-positive teenagers and their healthcare workers. N = 128 (14.9%) of the total sample had ever had sex, while N = 109 (85.1%) of sexually active adolescents had boy/girlfriend. In total, 68.1% of the sample knew their status, 41.5% of those who were sexually active and in relationships knew their partner's status, and 35.5% had disclosed to their partners. For adolescents, knowing one's status was associated with safer sex (OR = 4.355, CI 1.085–17.474, p = .038). Neither knowing their partner's status, nor disclosing one's HIV-status to a partner, were associated with safer sex. HIV-positive adolescents feared rejection, stigma and public exposure if disclosing to sexual and romantic partners. Counselling by healthcare workers for HIV-positive adolescents focused on benefits of disclosure, but did not address the fears and risks associated with disclosure. These findings challenge assumptions that disclosure is automatically protective in sexual and romantic relationships for HIV-positive adolescents, who may be ill-equipped to negotiate safer sex. There is a pressing need for effective interventions that mitigate the risks of disclosure and provide HIV-positive adolescents with skills to engage in safe sex.
Keywords: HIV-status, disclosure, safe sex, HIV-positive adolescents, South Africa
Introduction
Sub-Saharan Africa is home to 90% of the world's HIV-positive adolescents: an estimated 1.3–2.2 million vertically and horizontally infected 10–19-year-olds (United Nations Children's Fund [UNICEF], 2013). Evidence shows high rates of unprotected sex with other adolescents (27–90%) (Cataldo et al., 2012), and low rates of disclosure of HIV-status to sexual partners (Birungi, Mugisha, Obare, & Nyombi, 2009; Dempsey, Macdonell, Naar-king, Lau, & The Adolescent Medicine Network for HIV/AIDS Interventions, 2012). Negotiating safe sexual practices is particularly challenging for HIV-positive adolescents, exacerbated by HIV-related factors: learning and accepting their status (Lam, Naar-king, & Wright, 2007), and withholding or disclosing their HIV-status to sexual partners (Dempsey et al., 2012; Hardon & Posel, 2012). World Health Organisation guidelines recommend disclosure to adolescents of their own status (World Health Organization [WHO], 2011), but recommend prior counselling on potential benefits and risks of disclosure to others (WHO, 2013).
The paucity of research on associations between disclosure and negotiating safe sexual practices was highlighted in a recent systematic review (Maccarthy, Rasanathan, Ferguson, & Gruskin, 2012). Studies from sub-Saharan Africa report inconsistent associations between knowing own HIV-status and safe sex (Beyeza-Kashesya et al., 2011; Obare & Birungi, 2010). Only two known studies worldwide test associations of disclosure of status to partners: one found lower, but not statistically significant, rates of condom use among adolescents who had disclosed to their partners (Birungi et al., 2009), while the second reported that disclosure of status to partners was not associated with safe sex (Dempsey et al., 2012). Both use samples recruited from adolescents attending healthcare facilities only.
Qualitative research from sub-Saharan Africa suggests that disclosure in sexual and romantic relationships is shaped by complex factors, including knowing one's partner's status (Alemayehu, Aregay, Kalayu, & Yebyo, 2014), stigma (Li et al., 2010), medication-taking (Marhefka, Elkington, Dolezal, & Mellins, 2010), desire for love and acceptance (Busza, Besana, Mapunda, & Oliveras, 2013; Zamudio-Haas, Mudekunye-Mahaka, Lambdin, & Dunbar, 2012), and progression of HIV disease (Cooper et al., 2007).
This study adds to the limited existing evidence on how disclosure to and by HIV-positive adolescents is associated with safer sex. It uses a large, community-traced adolescent sample of vertically and horizontally infected adolescents in South Africa, combining qualitative and quantitative methods.
Methods
This study integrated quantitative and qualitative methods in design and implementation, a recommended practice for research among young people on health-related topics (Pluye & Hong, 2014) (Figure 1 includes additional information on method integration). Iterative methods were applied: preliminary qualitative research findings guided quantitative measures, particularly items on disclosure, while emerging quantitative findings framed the thematic focus of qualitative research, with topics followed up through in-depth interviews (Creswell, 2013). Researchers trained in both forms of data collection worked with investigators to facilitate greater rapport with participants, helping to improve the quality and efficacy of data collection. The “workshopping” of research approaches also ensured the sharing of emerging methodological challenges and research themes, with which both qualitative and quantitative researchers could engage more substantively through participant research. Ethical approval for this study was provided by Research Ethics Committees at the Universities of Oxford (SSD/CUREC2/12–21) and Cape Town (CSSR 2013/4), Eastern Cape Departments of Health and Basic Education, and ethical review boards of participating hospitals.
Figure 1.
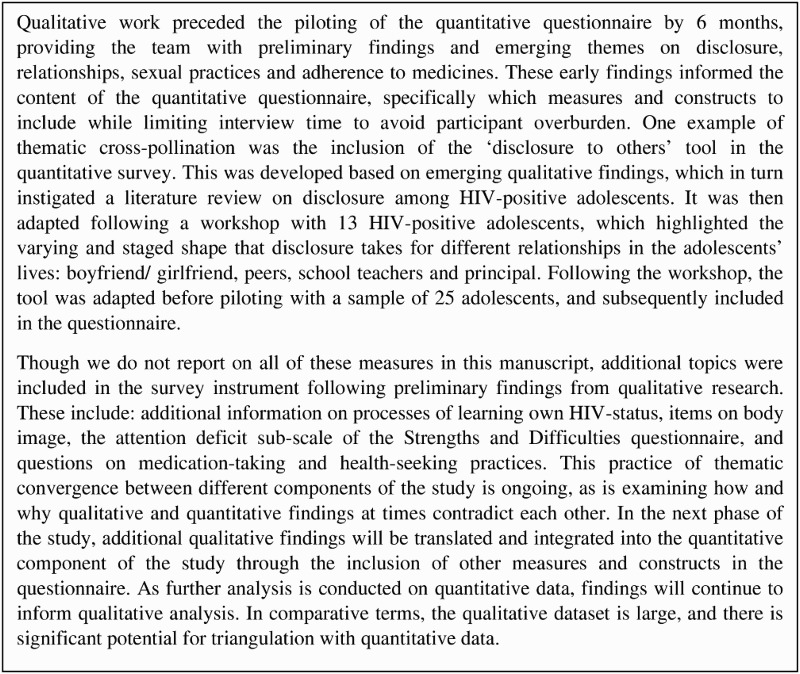
Approach to integrating qualitative and quantitative methods.
Participants and procedures
The study took place in the Eastern Cape, South Africa's poorest province with antenatal HIV prevalence of 29.1% (95% CI 27.3–30.9; Department of Health, 2012). Every public health facility in the study area, a mixed rural–urban health sub-district, was mapped in 2013. Thirty two clinics were identified that provided antiretroviral treatment (ART) to >4 adolescents. Subsequent to the mapping, the national decentralisation of ART programmes resulted in an increase of the clinic sample to 41 facilities. Adolescent participants were recruited in health facilities, followed by tracing of adolescents in their home communities or schools (“community-tracing”) to ensure that adolescents not actively engaged in care were included in sample. Clinical registers were used to identify all patients aged 10–19 who had ever initiated ART, regardless of clinic attendance (n = 1339): 40 had died, 402 had missing or false information, so could not be traced.
The quantitative arm of the study recruited 858 HIV-positive adolescents. Voluntary informed consent was obtained from adolescents and caregivers to take part in a 90-minute quantitative interview (refusal rate 4.3%) and, for the qualitative sample, to audio-record qualitative interviews and focus group discussions (FGDs). No incentives were provided, but all participants received a small gift pack and a certificate of participation. To prevent the possibility of stigma from participation in HIV-related research, the study was presented publicly as focusing on adolescents who use public health services. HIV-negative adolescents in neighbouring homes were also interviewed (n = 375, not included in this analysis).
Participants for the qualitative study were purposively recruited from the quantitative sample based on (i) consent and availability to participate in extensive interviews, (ii) reported experience of romantic/sexual relationships and (iii) reported experience of disclosing or withholding information about HIV-status to sexual partners. Three qualitative methods were triangulated: 72 in-depth interviews were conducted with 43 HIV-positive teenagers, with 17 participants interviewed more than once; followed by three focus groups (i) adolescent girls, (ii) adolescent boys and (iii) adolescent girls and boys combined to create opportunities for both gender-specific and interactive feedback; and 18 months of direct observation at five public health facilities (three hospitals and two health centres).
Data collection tools
Questionnaires, interview schedules and consent forms were translated from English into Xhosa, reviewed after back-translation, and then piloted with 25 HIV-positive adolescents. Adolescents participated in the language of their choice. Interviewers were trained in conducting research with HIV-affected adolescents. Quantitative questionnaires were administered using tablets, known to improve reporting of stigmatised behaviours (Gorbach et al., 2013; Jaspan et al., 2007). Qualitative interviews and focus group guides (see Figure 2 for sample prompts) used probes to explore specific subjects.
Figure 2.
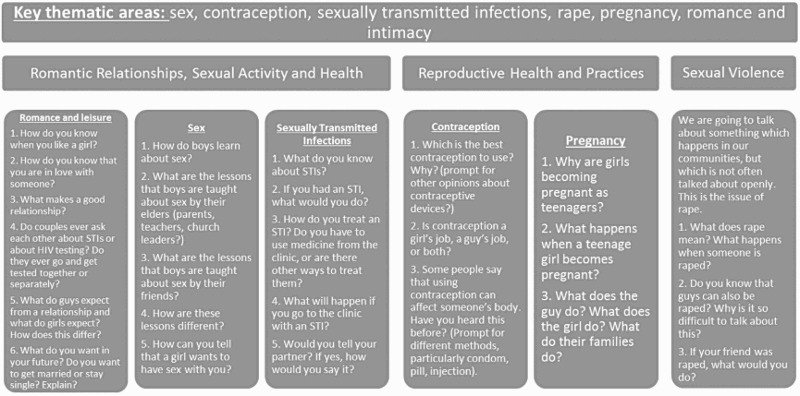
Themes and prompts of focus group discussion with adolescent boys.
Participants were assured that the information they shared would be kept anonymous, except in cases of significant harm or requested assistance. Where participants reported recent abuse, rape or risk of harm, referrals were made to child protection and health services, with follow-up support. When participants reported unprotected sex, ethical protocols required that interviewers provide counselling, and offer referral to local social workers.
Quantitative measures
Disclosure to and from adolescents
Adolescent knowledge of HIV-status was assessed in steps: first through healthcare worker report, then with primary caregivers during the consent process. Discrepancies between healthcare worker and caregiver reports required that interviewers check whether adolescents understood their status while obtaining consent, to prevent unintentional disclosure. Adolescents were screened on their recent history of illness and medication-taking. Those who did not to know their status were asked about “illness” and “medication” instead of “HIV” and “ART”, respectively. Disclosure to partners was measured by adolescent report using an 8-point gradient of disclosure depth/levels (Figure 3). Levels of disclosure were conceptualised as incremental, based on qualitative literature and piloting with HIV-positive youth (Lam et al., 2007; Michaud et al., 2009; Peele, D'Angelo, Chandwani, Abramowitz, & Koenig, 2012). The variable was dichotomised: 1 = partner knows adolescent is positive and/or taking ARVs, 0 = partner does not know.
Figure 3.
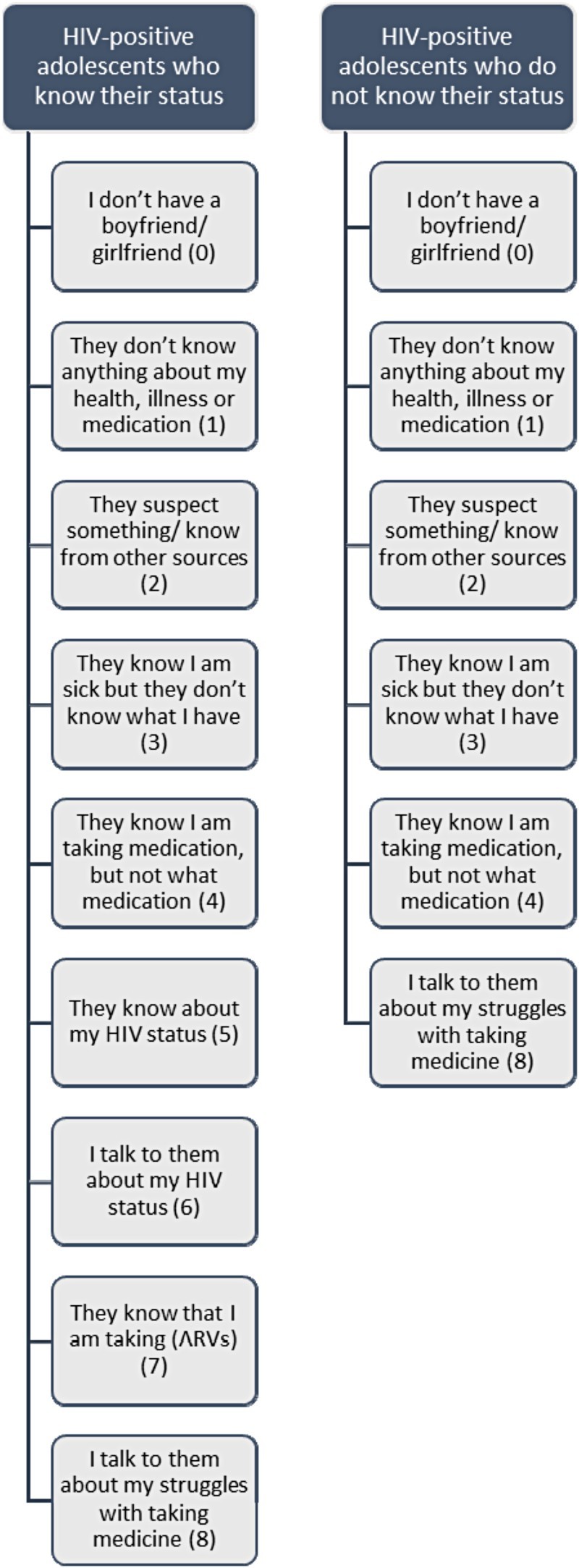
Levels of disclosure from HIV-positive adolescents to their partners (boyfriend or girlfriend).
Sex and relationship-related factors
Participants were asked if they had a boy/girlfriend and whether their partner's status was positive, negative, or unknown. Sexual experiences were measured through a series of questions using items adapted from other studies with HIV-positive youth (Bauermeister, Elkington, Robbins, Kang, & Mellins, 2012), including: age of sexual debut, and type of contraception at first and most recent sexual experience. Safe sex was dichotomised as 1 = abstinence or condom use, 0 = unprotected sex for two items: first or last sexual encounter. Reasons for safe sex were recorded through a multiple-choice question, adapted from the only other study among HIV-positive adolescents in Southern Africa to record these motivations quantitatively (Birungi et al., 2009). Experiences accessing contraception were measured through an item asking participants whether they felt comfortable talking to nurses about obtaining contraception, adapted from qualitative research (0 = no, 1 = yes).
Socio-demographic factors of adolescent age, gender, language, urban/rural location and formal/informal housing were measured using items adapted from the South African census. Household assets were measured using an index of the eight highest socially perceived necessities for children, corroborated by >80% of the population in the nationally representative Social Attitudes Survey (Pillay, Roberts, & Rule, 2006).
HIV-related factors included mode of infection, time on treatment, type of healthcare facility they receive treatment at (hospital vs. primary care clinic), engagement with health services (lost-to-follow-up or active in care) and self-reported sexually transmitted infections (STIs) or opportunistic infection symptoms. Following similar studies in Southern Africa (Evans et al., 2013; Ferrand et al., 2009), adolescents were coded as vertically infected if they had started ART before the age of 12 or if they had been on treatment for more than 5 years. Non-adherence was measured as any missed dose in the past week, based on a 95% adherence cut-off (Paterson et al., 2000). Symptoms of STIs and opportunistic infections were measured through an adapted version of the Verbal Autopsy scale (Lopman et al., 2006), adapted through qualitative research and an extensive literature review, asking adolescents to list symptoms from the last 6 months.
Data analyses
Qualitative interviews were audio-recorded, transcribed verbatim and coded. Thematic codes were developed from the data, based on the principles of grounded theory (Glaser & Strauss, 1967). These themes were cross checked with study participants to enhance validity. Qualitative findings informed the content of quantitative items and helped develop data collection methods that established trust and rapport with participants, important in light of the sensitive nature of research on sex, romance and risk-taking.
Quantitative analyses were conducted using SPSS 19.0. Analyses involved three stages:
Socio-demographic and health characteristics of HIV-positive adolescents, disaggregated by whether they knew their status.
Rates of romantic and sexual characteristics for both sub-groups were calculated using chi-square tests.
Relationship between knowing one's status, knowing one's partner status, disclosing to one's partner, and safe sex were explored using multivariate logistic regressions, controlling for age, gender, poverty, rural/urban residence, formal/informal housing type, mode of infection, time on treatment, sexual activity and relationship status, HIV-related factors and factors identified through qualitative research. Missing data were minimal (<1%), due to rigorous data checking and the use of mobile-assisted technology.
Results
Socio-demographic characteristics
Participant age ranged from 10 to 19 (mean = 13.53, SD = 2.69), 52% were female, 68.1% vertically infected. 96.4% spoke Xhosa at home, 20.3% lived in rural areas, while 16.6% lived in informal housing (Table 1). Two-thirds (66.2%) lived in homes that could not afford basic necessities, such as 3 meals a day, visit to the doctor, or warm clothes, while 15.4% had gone hungry for at least one day in the last week. Sixty eight point one percent of the sample knew their status, reporting an average of 3.94 years since disclosure (SD = 3.25). Those more likely to know their status were horizontally infected (p = .002), female (p = .049), older adolescents 15–19 years old (p ≤ .001), living in urban areas (p = .003), who were receiving care in the hospital setting (p = .011) and those on ART (p = .022) for a longer time.
Table 1. Socio-demographic and health characteristics of HIV-positive adolescents by knowledge of HIV-status.
| Category | Factor | Knows HIV-status (n = 584)a | Does not know HIV-status (n = 274)a | Total HIV-positive sample (n = 858)a |
|---|---|---|---|---|
| Gender | Female | 317 (54.3)* | 129 (45.7)* | 446 (52.0) |
| Male | 267 (47.1)* | 145 (52.9)* | 412 (48.0) | |
| Age | Age in yearsa | 14.28 (2.66)*** | 11.95 (2.00)*** | 13.53 (2.69) |
| 10–14 years old | 328 (56.2)*** | 241 (88)*** | 569 (66.3) | |
| 15–19 years old | 256 (43.8)*** | 33 (12)*** | 289 (33.7) | |
| Residence | Urban | 475 (82.5)** | 195 (73.6)** | 670 (79.7) |
| Rural | 101 (17.5)** | 70 (26.4)** | 171 (20.3) | |
| Ethnicity | Xhosa | 562 (96.2) | 265 (96.7) | 827 (96.4) |
| Other | 22 (3.8) | 9 (3.3) | 31 (3.6) | |
| Housing type | Informal | 96 (16.4) | 46 (16.8) | 142 (16.6) |
| Formal | 488 (83.6) | 228 (83.2) | 716 (83.4) | |
| Poverty | Missing any of the basic eight necessities | 400 (68.5)** | 168 (61.3)* | 568 (66.2) |
| Hunger in the last week | 91 (15.6) | 41 (15.0) | 132 (15.4) | |
| Caregiving arrangement | Living with biological parent | 240 (41.4)* | 139 (50.7)* | 379 (44.4) |
| Maternal orphan | 291 (49.8)*** | 97 (35.4)*** | 388 (45.2) | |
| Paternal orphan | 194 (33.2)** | 65 (23.7)** | 259 (30.2) | |
| Double orphan | 106 (18.2)** | 30 (10.9)** | 136 (15.9) | |
| Mode of infection | Vertically | 420 (71.9)** | 164 (28.1)** | 584 (68.1) |
| Horizontally | 224 (81.8)** | 50 (18.2)** | 274 (31.9) | |
| Treatment-related factors | Years on ARTa | 6.45 (4.68)* | 5.83 (4.15)* | 6.26 (4.53) |
| Non adherent in the last week | 196 (33.6) | 100 (36.5) | 296 (34.5) | |
| Access to healthcare services | Hospital | 256 (43.8)* | 95 (34.7)* | 351 (40.9) |
| Clinic or community healthcare centre | 328 (56.2)* | 179 (65.3)* | 507 (59.1) | |
| Health | At least 2 STI symptoms | 78 (13.4) | 40 (14.6) | 118 (13.8) |
| At least one opportunistic infection | 348 (59.6) | 172 (62.8) | 520 (60.6) |
Notes: This table includes the results of a series of chi-square tests with knowing one's status as an outcome and the noted factor as the independent variable. The first two columns display numbers and proportional percentages within groups, the third column displays numbers and shares between groups. Bold typeface indicates determinants that were significant: ***p ≤ .001, **p ≤ .01, *p ≤ .05.
aAll values displayed are numbers (%) except for age in years, and years on treatment. These display mean (SD).
Sexual and relationships characteristics
N = 178 (20.8%) reported having a boy/girlfriend, with N = 128 (14.9%) ever having had sex. Of those who had a boy/girlfriend, n = 107 (60.1%) had ever had sex (Table 2). Among the latter sub-group, n = 44 (41.5%) knew their partner's status, with n = 38 (35.5%) of them having disclosed their status to their partner. Among sexually active adolescents, those who knew their status were more likely to report safe sex (p = .050), while among sexually active adolescents in relationships, those who knew their partner's status and those who had not disclosed were more likely to report safe sex (n.s.) (Figure 4), with 65% of adolescents using contraception to prevent pregnancy (Table 2). Girls were more likely to have ever had sex (p ≤ .001), less likely to report safe sex (p = .037), and more likely to report disclosing to their partners (p ≤ .001). Gender-disaggregated relationship and sexual practices are reported in Table 3.
Table 2. Sexual and relationship characteristics of HIV-positive adolescents by knowledge of HIV-status.
| Factors | Categories | Knows HIV-status (n = 584) N (%) |
Does not know HIV-status (n = 274) N (%) |
Total HIV-positive sample (n = 858) N (%) |
|---|---|---|---|---|
| Relationship status | Has a boyfriend or girlfriend | 146 (25)*** | 32 (11.7)*** | 178 (20.8) |
| Sexual Debut | Ever had intercourse (vaginal or anal) | 117 (20)*** | 11 (4.0)*** | 128 (14.9) |
| Among sexually active adolescents in a relationship | ||||
| Factors |
Categories |
Knows HIV-status (n = 99) N (%) |
Does not know HIV-status (n = 8) N (%) |
Total HIV-positive sample (n = 107) N (%) |
| Knowledge of partner status | Unknown | 57 (58.2) | 5 (62.5) | 62 (58.5) |
| HIV-negative | 28 (28.6) | 3 (37.5) | 31 (29.2) | |
| HIV-positive | 13 (13.3) | 0 (0) | 13 (12.3) | |
| Disclosure to partner | Partner knows adolescents is HIV-positive and/or taking ARVs for HIVb | 34 (34.3) | 4 (50.0) | 38 (35.5) |
| Among sexually active adolescents | ||||
| Factors |
Categories |
Knows HIV-status (n = 117) N (%) |
Does not know HIV-status (n = 11) N (%) |
Total HIV-positive sample (n = 128) N (%) |
| First sexual experience | Age in yearsa | 15.55 (1.86)*** | 13.27 (5.39)*** | 15.35 (2.42) |
| Abstinent or male condom use | 88 (75.2) | 7 (63.6) | 95 (74.2) | |
| Unprotected sex | 29 (24.8) | 4 (36.4) | 33 (25.8) | |
| Most recent sexual experience | Abstinent or male condom use | 86 (73.5) | 5 (45.5)* | 91 (71.1) |
| Unprotected sex | 31 (26.5)* | 6 (55.5)* | 37 (28.9) | |
| Reasons for safe sex | Prevent pregnancy | 73 (65.2) | 7 (63.6) | 80 (65.0) |
| Passing HIV to my partner | 70 (62.5) | N/A | 70 (54.7) | |
| Prevent STI infection | 52 (46.4) | 4 (36.4) | 56 (45.5) | |
Notes: This table includes the results of a series of chi-square tests with sexual practices or relationship-related factors as an outcome and knowing one's status as the independent variable. Percentages report rates within each sub-group, that is, among adolescents who knew their status and those who did not. Bold typeface indicates determinants that were significant: ***p ≤ .001, **p ≤ .01, *p ≤ .05.
aAll values displayed are numbers (%) except for age of sexual debut in yearsa. These display mean (SD).
bHIV-positive adolescents who did not know their status were asked if they had told their boyfriend/girlfriend that they were taking medication.
Figure 4.
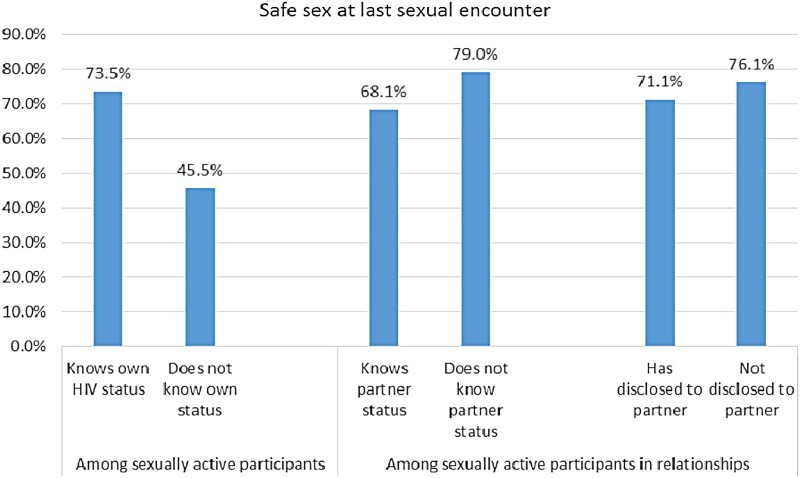
Rates of safe sex by type of disclosure.
Table 3. Sexual and relationship characteristics of HIV-positive adolescents by sex.
| Factors | Categories | Female (n = 446) N (%) |
Male (n = 412) N (%) |
Total sample (n = 858) N (%) |
|---|---|---|---|---|
| Relationship status | Has a boyfriend or girlfriend | 99 (22.1) | 82 (19.9) | 181 (21.0) |
| Sexual Debut | Ever had intercourse (vaginal or anal) | 88 (19.2)*** | 44 (10.7)*** | 130 (15.1) |
| Among sexually active adolescents in relationships | Female (n = 70) | Male (n = 37) | Total sample (n = 107) | |
| Disclosure | Knows own status | 64 (91.4) | 35 (94.6) | 99 (92.5) |
| Knowledge of partner status | Unknown | 36 (50.7) | 26 (70.3) | 62 (57.4) |
| HIV-negative | 24 (33.8) | 9 (27.3) | 33 (30.6) | |
| HIV-positive | 11 (15.5) | 2 (5.4) | 13 (12.0) | |
| Disclosure to partner | Partner knows adolescents is HIV-positive and/or taking ARVs for HIVa | 33 (45.8)*** | 5 (13.5)*** | 38 (34.9) |
| First sexual experience | Age of sexual debutb | 16.19 (1.21)*** | 14.27 (2.75)*** | 15.54 (2.08) |
| Abstinent or male condom use | 55 (76.4) | 31 (83.8) | 86 (78.9) | |
| Unprotected sex | 17 (23.6) | 6 (16.2) | 23 (21.1) | |
| Most recent sexual experience | Abstinent or male condom use | 49 (68.1)* | 32 (86.5)* | 81 (74.3) |
| Unprotected sex | 23 (31.9)* | 5 (13.5)* | 28 (25.7) | |
Note: This table includes the results of a series of chi-square tests with sexual practices or relationship-related factors as an outcome and sex (male/female) as the independent variable. The first two columns display numbers and proportional percentages within groups, the third column displays numbers and shares between groups, that is, among girls and boys. Bold typeface indicates determinants that were significant: ***p ≤ .001, **p ≤ .01, *p ≤ .05.
aHIV-positive adolescents who did not know their status were asked if they had told their boyfriend/girlfriend that they were taking medication.
bAll values displayed are numbers (%) except for age of sexual debut in years. These display mean (SD).
Linkages between knowledge of status, disclosure to partners and safe sex
In Model 1 (Table 4), knowing one's status was associated with safer sex (OR = 4.355, CI 1.085–17.474, p = .038). In Model 2, knowing one's partner status was not associated with safe sex, though knowing one's own status remained associated with safer sex (OR = 4.335, CI 1.081–17.389, p = .039). In Model 3, disclosing to one's partner and knowing one's partner status were not associated with safer sex, while knowing one's HIV-status remained associated with safe sex (OR = 4.356, CI 1.084–17.500, p = .038). Of potential covariates: age, gender, poverty, rural/urban residence, formal/informal housing type, HIV-related factors, health and relationship factors, only mode of infection remained significantly associated with lower likelihood of safe sex in all regression analyses.
Table 4. Regression models to test associations between types of disclosure and safe sex.
| Factors | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| OR | CI | OR | CI | OR | CI | |
| Knowledge of adolescent's own status | 4.355 | 1.085–17.474* | 4.335 | 1.081–17.389* | 4.356 | 1.084–17.500* |
| Knowledge of partner's status | 0.870 | 0.283–2.669 | 0.824 | 0.198–3.426 | ||
| Disclosure of own status to partner | 1.091 | 0.262–4.536 | ||||
Notes: All regression models were run with safe sex as the dependent variable, controlling for age, gender, poverty, rural/urban residence, ethnicity, housing type, caregiving arrangements and treatment and health-related covariates. Bold typeface indicates determinants that were significant: ***p ≤ .001, **p ≤ .01, *p ≤ .05.
Qualitative findings suggest possible explanations for these associations. Among the sexually active adolescents in the qualitative sample, a basic understanding of living with HIV, modes of infection and transmission, was widespread. Yet this understanding did not always ensure safe sex, nor mutual disclosure of HIV-status between adolescents and partners (see Figure 5 for Thanda's case, which elucidates this complex negotiation of knowledge and action). Adolescents who knew their status attempted to use condom with their partners, but as the quantitative data suggest, though higher than among those who did not know their status, condom use was still inconsistent and subject to difficult negotiations: As 17-year-old Mandi explained:
We use a condom sometimes. At times my boyfriend would complain that the condom tightens his penis. He would forget to get them before I come to visit him and when I get there he would not have condoms. And sometimes I would insist on having sex with a condom and if he does not have one, we will not have sex.
Figure 5.
Thanda's story.
Disclosure of HIV-positive status to partners rendered adolescents vulnerable to abandonment and exposure. In return for sustained sexual and romantic intimacy, and to compensate for the loss of innocence, inviolability and desirability associated with being HIV-positive, adolescents were less able or willing to insist on condom use.
Disclosure of HIV-status to partners is not a priority: The prevention of pregnancy and the avoidance of HIV-related stigma and rejection were prioritised above HIV disclosure, particularly within casual relationships. Disclosure of HIV-status to sexual partners did not support HIV-positive adolescents in negotiating condom use or safer sex: participants postponed disclosure until the relationship was stable, concealing their status to maintain sexual desirability, which they feared would be lost through HIV disclosure. Prior to full disclosure, a common approach was to “test the waters” with partners with hypothetical questions: “What would you do if I told you I was HIV-positive?” [Siphe, 18-year-old female, to her partner]. For many of these adolescents, the disclosure of HIV-status to a partner did not further enable or enhance safe sex negotiation.
Disclosure is an anxiety-provoking experience: Both genders reported anxiety around HIV disclosure to sexual partners, due to the fear of “outing”. Kwakza had dated four girls, had sex with three of them, but had not disclosed his status to any of them. The decision to conceal his status was based both on the brevity and changeable nature of adolescent relationships, and on fear of exposure: “Well, you never know if this person will publicise it when we break up.” [17-year-old male]. HIV disclosure to partners was fraught with fears of abandonment, despoliation and rejection:
Once you have told that guy [that you are HIV-positive], he will sleep with you, and when he is finished with you he will just dump you like nothing has happened. His friend will want you as well, but that boy will tell him, “No, I'm finished everything there, so there's nothing left for you.” [16-year-old female, FGD iii, Mdantsane]
Disclosure counselling and support: As recommended by clinical guidelines, healthcare providers observed in this study counselled HIV-positive adolescents to disclose to their partners. However, adolescents' fears of rejection often overshadowed this advice:
When I had the test, they counselled me, and the sister told me that I must disclose to my sexual partners. But no-one is going to do that, no one can. Maybe some can, but they are scared that their partners will blame them. Because if the boy didn't go to test, he is going to say to you, “You are the one who has brought this to me”, even though he doesn't know his status. [Siphe, 18-year-old female]
Healthcare workers conveyed anger towards the perceived recklessness of their adolescent patients, which manifested in the embarrassment and harsh treatment of HIV-positive adolescent patients. In observations of engagements between healthcare providers and adolescents, adolescents were silenced into shame by the treatment they received. After a brief account of her symptoms, 18-year-old Siphe was asked to undress behind the screen and given a vaginal examination. The nurse, familiar with her HIV-status and her clinical presentation with successive cases of STIs, berated Siphe for her reckless behaviour. From behind the screen, she instructed Siphe to open her legs, then stated with disgust: “Yoh, I can already smell it. It's a smelly discharge here. Are you condomising?” Siphe remained silent. This nurses' statements were clearly audible to the 3–4 other people in the room.
Sexual risk-taking among HIV-positive adolescents was widely acknowledged and censured by healthcare workers, who treated successive cases of STIs among their HIV-positive adolescent patients with frustration and bewilderment. As one of them explained of her HIV-positive adolescent patients who concealed their status and did not use condoms: “They are more committed to a secret than survival.” [Female nurse, day hospital.]
Aware of adolescents' fears of exposure, healthcare workers used them strategically to both threaten and motivate patients into changing risky behaviours. Secrecy and exposure were thus wielded as tools, both means of health promotion, and of punishment for risk-taking. Allegations of recklessness, and the spectre of purposeful HIV transmission, were both discernible in nurses' admonishments of their adolescent patients, which often took place in the presence of other healthcare workers and patients. As the sister-in-charge of a large and busy family planning clinic explained: ‘These teenagers struggle … To us, they come when they are already having a baby. They do not use contraceptives. They do not use a condom. Some of them want to give their partners HIV. Some of their partners want to give it to them [Female nurse, hospital]. Another nurse echoed these claims: ‘They [HIV-positive adolescents] don't really take care of themselves. They don't know the status of the partner … They still engage without condoms.’ [Female nurse, day hospital.]
Numerous studies have documented the punitive attitudes of healthcare workers towards women seeking sexual health services in South Africa's public health sector (Hodes, 2013; Wood & Jewkes, 2006). However, while this research revealed punitive practices, it also demonstrated that healthcare workers used blame and humiliation strategically to instruct patients to desist from risky behaviours. In clinic observations, nurses humiliated HIV-positive adolescents who presented with STIs, while seeking simultaneously to motivate them to practice safer sex. After examining an HIV-positive adolescent girl, one nurse switched from humiliation to motivation, encouragement and material support for safer sex: “As a woman, you need to be kind to your body. Here are condoms, take as many as you want so that, [ … ] you will always have it. You are such a beautiful girl, a right girl”. [Female nurse, day hospital]
Discussion
Our findings contribute to whether HIV-status knowledge (of self and partner) and disclosure to partners shapes safe sex among HIV-positive adolescents. Among HIV-positive adolescents, knowledge of HIV-status was strongly associated with safer sex, while knowing one's partner's status or disclosing one's status were not.
These quantitative associations were elucidated by qualitative findings: fear of rejection, exposure and stigma discouraged HIV-positive adolescents from disclosing to their partners as a strategy for negotiating safer sex, while disclosure counselling and support from healthcare workers did not address these challenges. The qualitative findings confirm that being HIV-positive is strongly associated with a sense of shame and contamination (Rohleder & Gibson, 2006; Simbayi et al., 2007). Guidelines on counselling HIV-positive adolescents should focus on promoting safe sex with all sexual partners as the first priority, rather than promoting disclosure to sexual partners. Focusing on adolescents' motivation to prevent pregnancy and STIs may enable healthcare providers to support adolescent efforts to negotiate safe sex with all partners.
Female participants were more likely to be sexually active and to report unprotected sex. Qualitative accounts of adolescent girls reveal gendered power imbalances within sexual relationships. Blaming attitudes towards girls for perceived moral and sexual indiscretions, including HIV infection, were widely reported by adolescents and healthcare workers.
Current WHO guidelines recommend that HIV-positive adolescents are counselled on the risks and benefits of disclosure to their partners. However, our qualitative findings suggest that current counselling practices did not address these fears, but rather exacerbated them through shaming and cajoling strategies. Clinical exposure and humiliation exacerbated adolescents' fears of being “outed” beyond the clinic, through their social networks, in turn related to broader socio-cultural beliefs regarding HIV as a manifestation of moral and physical pollution (Delius & Glaser, 2005). Aware of adolescents' fears of exposure, healthcare workers used them strategically to both threaten and motivate patients into changing risky behaviours. Secrecy and exposure were thus wielded as tools, both means of health promotion, and of punishment for risk-taking. Allegations of recklessness, and the spectre of purposeful HIV transmission, were both discernible in nurses' admonishments of their adolescent patients, which often took place in the presence of other healthcare workers and patients. Disclosure counselling for HIV-positive adolescents could be enhanced by improving patient confidentiality, by addressing adolescent fears on the dangers of disclosure, and by giving HIV-positive adolescents skills to negotiate safer sex.
This study has a number of limitations. First, although our outcome – last sexual experience – took place after or during disclosure, the cross-sectional nature of our data limits our ability to reach conclusions beyond associations. Second, some of our measures, namely knowledge of partner status, were based on adolescent self-reports and could not be verified. Third, the rates of disclosure of HIV-status to partners in our sample were low, and so this sub-group may require larger scale studies to test generalizability of findings.
Despite the above limitations, the study has several strengths. This large study is the first to include adolescents who are both actively retained and not retained in clinical care. It is the only study to include both vertically and horizontally infected adolescents. And it is the first to test associations of both disclosure to and disclosure by adolescents with safer sex practices. Applying mixed-methods allowed for the development of more rigorous and adaptive research tools and more reflexive analysis.
A deeper understanding of the challenges that adolescents face in learning about their status, in disclosing their status to sexual and romantic partners, and in negotiating safe sex, is crucial. Further research is needed to aid the design and implementation of programmes responsive to the unique psychosocial and sexual health needs of this population group. Future research should elucidate how we can support the current and future generations of HIV-positive adolescents to use knowledge of their HIV-status to negotiate safer sexual practices.
Acknowledgements
This study is a collaboration of the Universities of Oxford and Cape Town, UNICEF, the South African National Departments of Health, Basic Education and Social Development and Paediatric AIDS Treatment for Africa, and local CBOs: the Keiskamma Trust, the Raphael Centre and Small Projects Foundation. Research was conducted by a dedicated research team. We acknowledge and thank all research participants, particularly adolescents, families and healthcare providers. The authors would also like to thank Julia Rosenfeld, Maya Isaacsohn, Marija Pantelic, Janina Steinart, Craig Carty, Gerry Boon, Luntu Galo, Cheree Goldswain, Justus Hofmeyr, Sibongile Mandondo, Lulama Sidloyi and Nicoli Nattrass. Statement of co-authorship: ET led the quantitative study design, data analysis and writing. RH led the qualitative study design, data analysis and writing. LC conceptualised the study, and contributed to data analysis and writing. KK contributed to the literature review and analysis. All authors have read and approved the final text.
Funding Statement
This work was supported by the Nuffield Foundation under Grant CPF/41513, the International AIDS Society through the CIPHER grant (155-Hod), and the Clarendon-Green Templeton College Scholarship (Elona Toska). Additional support for Lucie Cluver was provided by the European Research Council (ERC) under the European Union's Seventh Framework Programme (FP7/2007–2013)/ERC grant agreement n°313421. Additional support for Rebecca Hodes was provided by South Africa's National Research Foundation and the University of Cape Town's Humanities Faculty. The study was supported by the Pediatric AIDS Management Programme of the Eastern Cape provincial Department of Health, and by 41 health facilities in the Buffalo City sub-district and Amathole district, Eastern Cape, South Africa. Open Access publication funded by Evidence for HIV Prevention in Southern Africa (EHPSA), a DFID programme managed by Mott MacDonald.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Alemayehu M., Aregay A., Kalayu A., Yebyo H. HIV disclosure to sexual partner and associated factors among women attending ART clinic at Mekelle hospital, Northern Ethiopia. BMC Public Health. 2014:746. doi: 10.1186/1471-2458-14-746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauermeister J. A., Elkington K. S., Robbins R. N., Kang E., Mellins C. A. A prospective study of the onset of sexual behavior and sexual risk in youth perinatally infected with HIV. Journal of Sex Research. 2012;(5):413–422. doi: 10.1080/00224499.2011.598248.A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beyeza-Kashesya J., Kaharuza F., Ekström A. M., Neema S., Kulane A., Mirembe F. To use or not to use a condom: A prospective cohort study comparing contraceptive practices among HIV-infected and HIV-negative youth in Uganda. BMC Infectious Diseases. 2011;(1):144. doi: 10.1186/1471-2334-11-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birungi H., Mugisha J. F., Obare F., Nyombi J. K. Sexual behavior and desires among adolescents perinatally infected with human immunodeficiency virus in Uganda: Implications for programming. Journal of Adolescent Health. 2009;(2):184–187. doi: 10.1016/j.jadohealth.2008.06.004. [DOI] [PubMed] [Google Scholar]
- Busza J., Besana G. V. R., Mapunda P., Oliveras E. “I have grown up controlling myself a lot.” Fear and misconceptions about sex among adolescents vertically-infected with HIV in Tanzania. Reproductive Health Matters. 2013;(41):87–96. doi: 10.1016/S0968-8080(13)41689-0. [DOI] [PubMed] [Google Scholar]
- Cataldo F., Malunga A., Rusakaniko S., Umar E., Zulu J., Teles N., Musandu H. 2012, July Experiences and challenges in sexual and reproductive health for adolescents living with HIV in Malawi, Mozambique, Zambia and Zimbabwe. In XIX International AIDS Conference, Washington, DC, USA.
- Cooper D., Harries J., Myer L., Orner P., Bracken H., Zweigenthal V. “Life is still going on”: Reproductive intentions among HIV-positive women and men in South Africa. Social Science & Medicine (1982) 2007;(2):274–283. doi: 10.1016/j.socscimed.2007.03.019. [DOI] [PubMed] [Google Scholar]
- Creswell J. Research design: Qualitative, quantitative, and mixed methods approaches. Thousand Oaks, CA: Sage; 2013. [Google Scholar]
- Delius P., Glaser C. Sex, disease and stigma in South Africa: Historical perspectives. African Journal of AIDS Research. 2005;(1):29–36. doi: 10.2989/16085900509490339. [DOI] [PubMed] [Google Scholar]
- Dempsey A. G., Macdonell K. E., Naar-king S., Lau C.-Y. The Adolescent Medicine Network for HIV/AIDS Interventions Patterns of disclosure among youth who are HIV positive: A multisite study. Journal of Adolescent Health. 2012;(3):315–317. doi: 10.1016/j.jadohealth.2011.06.003.Patterns. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Health . The 2011 National Antenatal Sentinel HIV & syphilis prevalence survey in South Africa. Pretoria: Author; 2012. [Google Scholar]
- Evans D., Menezes C., Mahomed K., Macdonald P., Untiedt S., Levin L., Maskew M. Treatment outcomes of HIV-infected adolescents attending public-sector HIV clinics across Gauteng and Mpumalanga, South Africa. AIDS Research and Human Retroviruses. 2013:1–13. doi: 10.1089/aid.2012.0215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrand R. A., Corbett E. L., Wood R., Hargrove J., Ndhlovu C. E., Cowan F. M., Wiliams B. G. AIDS among older children and adolescents in Southern Africa: Projecting the time course and magnitude of the epidemic. AIDS. 2009;(15):2039–2046. doi: 10.1097/QAD.0b013e32833016ce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glaser B. G., Strauss A. L. The discovery of grounded theory. International journal of qualitative methods. Vol. 5. Chicago, IL: Aldine; 1967. [Google Scholar]
- Gorbach P. M., Mensch B. S., Husnik M., Coly A., Masse B., Makanani B., Forsyth A. Effect of computer-assisted interviewing on self-reported sexual behavior data in a microbicide clinical trial. AIDS Behaviour. 2013:790–800. doi: 10.1007/s10461-012-0302-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardon A., Posel D. Secrecy as embodied practice: Beyond the confessional imperative. Culture, Health & Sexuality: An International Journal for Research, Intervention and Care. 2012;(S1):S1–S13. doi: 10.1080/13691058.2012.726376. [DOI] [PubMed] [Google Scholar]
- Hodes R. ‘You know what a bad person you are?’ HIV, abortion, and reproductive health care for women in South Africa. In: Smith R. A., editor. Global HIV/AIDS politics, policy and activism: Persistent challenges and emerging issues. Santa Barbara, CA: Praeger; 2013. pp. 233–252.pp. 239–241. [Google Scholar]
- Jaspan H. B., Flisher A. J., Myer L., Mathews C., Seebregts C., Berwick J. R., Bekker L. Brief report: Methods for collecting sexual behaviour information from South African adolescents – A comparison of paper versus personal digital assistant questionnaires. Journal of Adolescence. 2007:353–359. doi: 10.1016/j.adolescence.2006.11.002. [DOI] [PubMed] [Google Scholar]
- Lam P. K., Naar-king S., Wright K. Social support and disclosure as predictors of mental health in HIV-positive youth. AIDS Patient Care and STDs. 2007;(1):20–29. doi: 10.1089/apc.2006.005. [DOI] [PubMed] [Google Scholar]
- Li R. J., Jaspan H. B., O'Brief V., Rabie H., Cotton M. F., Nattrass N. Positive futures: A qualitative study on the needs of adolescents on antiretroviral therapy in South Africa. AIDS Care: Psychological and Socio-Medical Aspects of AIDS/HIV. 2010;(6):751–758. doi: 10.1080/09540120903431363. [DOI] [PubMed] [Google Scholar]
- Lopman B. A., Barnabas R. V., Boerma J. T., Chawira G., Gaitskell K., Harrop T., Gregson S. Creating and validating an algorithm to measure AIDS mortality in the adult population using verbal autopsy. PLoS Medicine. 2006;(8):1273–1281. doi: 10.1371/journal.pmed.0030312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maccarthy S., Rasanathan J. J. K., Ferguson L., Gruskin S. The pregnancy decisions of HIV-positive women: The state of knowledge and way forward. Reproductive Health Matters. 2012;(39S):119–140. doi: 10.1016/S0968-8080(12)39641-9. [DOI] [PubMed] [Google Scholar]
- Marhefka S. L., Elkington K. S., Dolezal C., Mellins C. A. Society for adolescent medicine annual meeting program issue: Adolescent clinical care: Integrating art & science. Vol. 46. Elsevier; 2010. Transmission risk behaviour among youth living with perinatally acquired HIV: Are nonadherent youth more likely to engage in sexual behavior? p. S29. Retrieved from http://www.jahonline.org/issues?issue_key=S1054--139X%2809%29X0015--7. [Google Scholar]
- Michaud P.-A., Suris J.-C., Thomas L. R., Kahlert C., Rudin C., Cheseaux J.-J. The Swiss Mother and Child HIV Cohort Study To say or not to say: A qualitative study on the disclosure of their condition by human immunodeficiency virus – Positive adolescents. Journal of Adolescent Health. 2009;(4):356–362. doi: 10.1016/j.jadohealth.2008.08.004. [DOI] [PubMed] [Google Scholar]
- Obare F., Birungi H. The limited effect of knowing they are HIV-positive on the sexual and reproductive experiences and intentions of infected adolescents in Uganda. Population Studies: A Journal of Demography. 2010;(1):97–104. doi: 10.1080/00324720903427575. [DOI] [PubMed] [Google Scholar]
- Paterson D. L., Swindells S., Mohr J., Brester M., Vergis E. N., Squier C., Singh N. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Annals of Internal Medicine. 2000;(1):21–30. doi: 10.7326/0003-4819-133-1-200007040-00004. [DOI] [PubMed] [Google Scholar]
- Peele Y. L., D'Angelo L. J., Chandwani S., Abramowitz S., Koenig L. 2012 Determinants of HIV serostatus self-disclosureamong adolescents participants in the adolescent impact study. Society for adolescent health and medicine 2012 annual meeting, New Orleans, Louisiana, USA – Poster session II: HIV, p. 164.
- Pillay U., Roberts B., Rule S. P. South African social attitudes: Changing times, diverse voices. Cape Town: HSRC Press; 2006. (U. Pillay, B. Roberts, & S. P. Rule, Eds.) Retrieved from http://books.google.com/books?hl=en&lr=&id=ag9kMWd4IWkC&pgis=1. [Google Scholar]
- Pluye P., Hong Q. N. Combining the power of stories and the power of numbers: mixed methods research and mixed studies reviews. Annual Review of Public Health. 2014:29–45. doi: 10.1146/annurev-publhealth-032013-182440. [DOI] [PubMed] [Google Scholar]
- Rohleder P., Gibson K. “We are not fresh”: HIV-positive women talk of their experience of living with their ‘spoiled identity’. South African Journal of Psychology. 2006:25–44. doi: 10.1177/008124630603600103. Retrieved from http://www.cssr.uct.ac.za/sites/cssr.uct.ac.za/files/pubs/wp110.pdf. [DOI] [Google Scholar]
- Simbayi L. C., Kalichman S., Strebel A., Cloete A., Henda N., Mqeketo A. Internalized stigma, discrimination, and depression among men and women living with HIV/AIDS in Cape Town, South Africa. Social Science & Medicine (1982) 2007:1823–1831. doi: 10.1016/j.socscimed.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations Children's Fund . Towards an AIDS-free generation – Children and AIDS: Sixth stocktaking report, 2013. New York: Author; 2013. [Google Scholar]
- Wood K., Jewkes R. K. Blood blockages and scolding nurses: Barriers to adolescent contraceptive use in South Africa. Reproductive Health Matters. 2006;(27):109–118. doi: 10.1016/S0968-8080(06)27231-8. [DOI] [PubMed] [Google Scholar]
- World Health Organization . Guideline on HIV disclosure counselling for children up to 12 years of age. Geneva: Author; 2011. [PubMed] [Google Scholar]
- World Health Organization . HIV and adolescents: HIV testing and counselling, treatment and care for adolescents living with HIV (Policy brief) Geneva: Author; 2013. [Google Scholar]
- Zamudio-Haas S., Mudekunye-Mahaka I., Lambdin B. H., Dunbar M. S. If, when and how to tell: A qualitative study of HIV disclosure among young women in Zimbabwe. Reproductive Health Matters. 2012:18–26. doi: 10.1016/S0968-8080(12)39637-7. [DOI] [PubMed] [Google Scholar]


