Summary
Background
We aimed to report the image quality, relationship between heart rate and image quality, amount of contrast agent given to the patients and radiation doses in coronary CT angiography (CTA) obtained by using high-pitch prospectively ECG-gated “Flash Spiral” technique (method A) or retrospectively ECG-gated technique (method B) using 128×2-slice dual-source CT.
Material/Methods
A total of 110 patients who were evaluated with method A and method B technique with a 128×2-detector dual-source CT device were included in the study. Patients were divided into three groups based on their heart rates during the procedure, and a relationship between heart rate and image quality were evaluated. The relationship between heart rate, gender and radiation dose received by the patients was compared.
Results
A total of 1760 segments were evaluated in terms of image quality. Comparison of the relationship between heart rate and image quality revealed a significant difference between heart rate <60 beats/min group and >75 beats/min group whereas <60 beats/min and 60–75 beats/min groups did not differ significantly. The average effective dose for coronary CTA was calculated as 1.11 mSv (0.47–2.01 mSv) for method A and 8.22 mSv (2.19–12.88 mSv) for method B.
Conclusions
Method A provided high quality images with doses as low as <1 mSv in selected patients who have low heart rates with a high negative predictive value to rule out coronary artery disease. Although method B increases the amount of effective dose, it provides high diagnostic quality images for patients who have a high heart rate and arrhythmia which makes it is difficult to obtain images.
MeSH Keywords: Coronary Angiography, Heart Rate, Image Enhancement, Multidetector Computed Tomography, Radiation Dosage, Radiology
Background
Coronary artery disease (CAD) is currently an important cause of morbidity and mortality [1]. CAD is the clinical presentation of atherosclerosis which is a narrowing of coronary artery lumen due to lipid-rich fibrous or calcified plaques. It starts with inflammation due to injury of endothelial cells and lipid deposition on intimal surfaces. Atherosclerotic plaque continues to grow by accumulation of immunity and muscle cells and lipid. In advanced stages it consists of fibrous sheath and lipid plaque formed by extracellular lipid, fibrous plaque, calcified plaque and complex thrombotic lesions which are prone to rupture [2,3].
At present, conventional coronary angiography (CCA) is considered as a gold standard in the diagnostics of CAD. However, the invasive nature of the procedure that could lead to complications and hospitalization risk are some of its limitations. Also the level of the radiation dose and the amount of contrast media used are important [4]. The most important factors that make it difficult to assess the coronary arteries are the quite small diameters of coronary arteries and their constant mobility during the heartbeat. Developing multi-slice computed tomography (MSCT) technology of noninvasive evaluation of coronary arteries with CT had made it possible [5–7]. Dual-source CT technology became available in 2005 and has provided high temporal resolution for coronary CT angiography (CTA) [8]. High-pitch value and table speed have made it possible to obtain all volumetric data of the heart with radiation exposure as low as 1 mSv in a single cardiac cycle [9–11].
In our study, we aimed to report the image quality, relationship between heart rate and image quality, amount of contrast agent given to the patients and radiation doses in coronary CTA obtained by using high-pitch prospective or retrospective ECG-gated method via 128×2-slice dual-source CT angiography and comparative results of patients who underwent CCA when moderate-to-severe stenoses were detected with coronary CTA.
Material and Methods
Patient selection
After the approval of the ethics board, 126 patients who were known to have CAD or those who were referred to our clinic for reasons such as assessment of coronary artery stenosis and had underwent coronary CTA between February 2013 and December 2013 were retrospectively reviewed. None of the patients was excluded from the study because of uncontrolled arrhythmias, heart rate above 70 or morbid obesity which are considered as limitations of coronary CTA in the literature. However, 16 patients with a history of by-pass and stent were excluded from the study. Patients with allergy to contrast agent and nephropathy were not included. One hundred and ten patients who were evaluated with prospectively electrocardiography (ECG)-gated high pitch “Flash Spiral” technique (method A) and retrospectively ECG-gated spiral (method B) technique in dual-source CT were included in the study.
Patient preparation
All patients were asked to present for procedure after 6 hours of fasting (in order to prevent aspiration during vomiting that may develop due to contrast allergy). Arterial blood pressure was measured. Antecubital intravenous line was established preferably with a 16 Gauge (G) branule (gray color) or 18 G branule (green color) prior to entrance in the procedure room. Before the procedure, breath-holding exercises were done until patients were able to hold their breath approximately for 15–20 seconds.
The patients were laid on the table in the supine position. ECG electrodes were deliberately placed on bony prominences to avoid muscle artefacts. Calcium scoring was performed in patients over 40 years of age and to those who had a high risk of CAD before the procedure. At the final stage, 3 minutes prior to scanning, 5–10 mg of isosorbide dinitrate (Isordil®) was given in order to enlarge coronary arteries.
CT imaging
CTA examination was carried out with a dual-source CT scanner which has two X-ray tubes located with 95º angle and a 128-channel two-detector row (128×2-slice Somatom Definition Flash, Siemens Healthcare Forscheim, Germany) in our center. After obtaining a topogram image for determining the scanning area, a single cross-sectional image was taken based on the level of the left atrium over the topogram for a “bolus-tracking” program. The left atrium was marked manually.
Scanning area was determined as between the level of the carina and diaphragmatic surface of the heart. Non-ionic contrast medium containing 400 mg of iodine (Iomeron®, Bracco, Italy) was given at a speed of 4.5–6 mL/s with an automatic injector system by making synchronized ECG recording. After contrast was administered, shooting was carried out by giving 40 mL of NaCl at a speed of 6 mL/sec with the automatic injector. When the predicted contrast level was reached, scanning was started with a program (Sure Start®) which launched automatically and completed in a single breath-hold time while repetitive images were captured from the single section marked at the left atrial lumen with the “bolus-tracking” technique. Procedures were successfully completed without any complications in all of the patients.
Patients were divided into two groups according to gender as male and female and into 3 groups according to heart rate as <60, 60–75 and >75 determined by the CT device.
Coronary CTA data were obtained using method A and method B. In our study, the device automatically determined the most ideal kV values with the Care kV option from the received topogram images according to BMI of the patient. In addition, automatic mAs values were obtained with the CareDose 4D option. CT acquisition parameters were as follows: slice collimation 2×128×0.6 mm with a z-flying focal spot; gantry rotation time 270 ms; pitch 3.4 for method A, 0.17 for method B. Images were reconstructed with 0.75 mm slice thickness and 0.4 mm increment using a medium smooth tissue iteractive reconstruction kernel (I26f). Sinogram affirmed iterative reconstruction (SAFIRE) was used and strength was chosen as 3 in all patients.
The display was obtained starting from the 60% zone of the R-R interval in method A. Half-scan reconstruction algorithm which provides 75 ms temporal resolution in the center of the image was used for image reconstruction. In method B, heart rate and ECG tracings were recorded for segmental reconstruction. Small reconstruction images of the first several centimeters of the coronary arteries were created with increments of 10% between 40–90% to find the percentile where the movement is minimal. Then, some of the best images were selected and images to be reported were obtained by repeating the reconstruction for the whole heart at the same percentile of selected images.
Image analysis
Data of the patients were transferred to the workstation (syngo.Via, 2009, Siemens Erlangen, Germany) for evaluation. Workstation device automatically found the best diastolic phases itself. Coronary arteries were examined in detail based on the least artifacted axial images of each coronary artery and reconstruction images obtained by multiplanar recontruction, maximum intensity projection and 3D volume rendered techniques (Figures 1, 2).
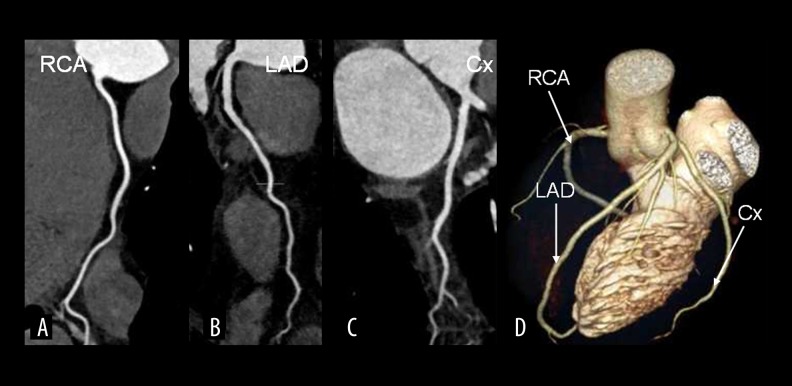
Figure 1.
Images of excellent quality using prospective ECG-triggered (flash spiral technique) coronary CTA (pitch 3.4, 65 mL at 5.5 mL/s) in a 48-year-old male patient with an atypical chest pain, a mean heart rate of 67 beat/min. Curved reformation images show an excellent quality; (A) a normal right coronary artery (RCA), (B) left anterior descending artery (LAD), (C) circumflex artery and (D) 3D volume rendering reformation. The effective dose was 0.7 mSv.
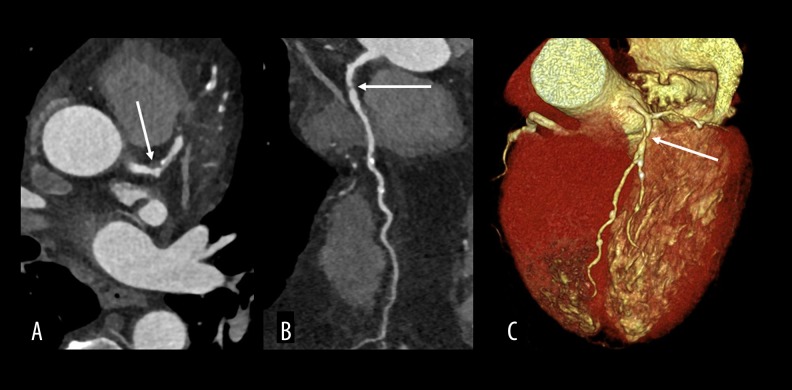
Figure 2.
(A–C) Images obtained using the prospective ECG-triggered (flash spiral technique) coronary CTA (pitch 3.4, 75 mL at 5.5 mL/s) in a 55-year-old male patient with an atypical chest pain, a mean heart rate of 72 beat/min. Axial, coronal multiplanar recontruction images and 3D volume rendered image show a discrete soft plaque causing a severe luminal stenosis (85%) in proximal LAD (arrows). The effective dose of 0.9 mSv.
A modified 17-segment American Heart Association (AHA) classification was used for segmental classification of coronary arteries. A total number of segments of the coronary arteries was calculated as the number and percentage at the end of procedure. Image quality of the coronary arteries was evaluated segment by segment. A 4-point scale was used:
1 = without artifact;
2 = mildly artifacted, but completely assessable;
3 = artifacted but assessable in terms of stenosis;
4 = cannot be assessed.
One image quality score was given per segment. In addition to these points, ‘0’ score was given to the segments without coronary artery. A difference in terms of coronary artery image quality between the groups of patients with different heart rates was evaluated.
Radiation dose
Radiation dose was determined based on the dose-length product (DLP) which takes place in CT scanning protocol. Effective dose (ED-mSv) was estimated using the DLP method with a conversion factor k=0.014 for adults. Then, differences of the radiation doses between the genders, association between heart rates and radiation dose and received radiation doses of method A–B were evaluated.
Statistical analysis
Categorical variables related with coronary risk factors such as age, gender, height, weight, and heart rate were given as numbers and percentages (%).
The One-Sample Kolmogrov Smirnov Test was used to evaluate whether the variables showed normal distribution or not. Variables were found to show normal distribution. Therefore, parametric tests were used for statistical analysis. Homogeneity was tested with the One-Sample Kolmogorov-Smirnov test and results revealed that data of all groups showed normal distribution. The Independent-Samples t-test was used to evaluate whether there were differences between the genders in terms of dose. The relationship between patient’s heart rates and image quality was assessed by one-way ANOVA test. Multiple comparisons were performed with a post hoc Tukey test. The Independent-Samples t-test was performed to assess the impact of the procedure protocol on ED and other parameters.
All images were evaluated and scored by 2 independent readers. To resolve any disagreement in the detection of stenosis and image qualty, a consensus reading was appended. The interobserver agreement of the image quality scoring and stenosis assessment was tested with Cohen’s κ value. The interobserver agreement for the image quality rating was interpreted as moderate for 0.4< κ ≤0.60, good for 0.6< κ ≤0.80, and excellent for κ >0.80 CCA. In the whole statistical analysis, p<0.05 was considered as significant.
In general, patients with negative coronary CTA in combination with a negative stress test and/or a good response to medical treatment were not referred to CCA. However, CCA was performed in patient discordance between symptoms and the results of diagnostic tests. Finally, coronary CTA and CCA results of 23 patients in whom moderate or severe stenosis was detected in at least one coronary artery segment as a result of CTA examination and who underwent CCA within two following weeks were compared with CCA taken as the gold standard. The same classification of stenosis was used for both coronary CTA and CCA. Accordingly, luminal stenosis was defined as minimal (1–24%), mild (25–49%), moderate (50–69%), severe (70–99%) and occluded (100%).
Results
Among 110 patients enrolled in the study 61 were male and 49 were female. The mean age of the patients was 53.75, the mean systolic blood pressure of patients before procedure was 127.9 mm Hg (range: 90–200 mm Hg) and diastolic pressure was 81.6 mm Hg (60–120 mmHg). The mean heart rate of patients was 79.63 (range: 47–117). Patients were divided into three groups according to their heart rate. Accordingly, 13 patients had a heart rate lower than 60 beats/min (group 1), 29 patients had a heart rate of 60–75 beats/min (group 2) and 68 patients had a heart rate of more than 75 beats/min (group 3).
Forty patients were examined with method A while 70 were examined with method B. When selecting the procedure technique, method A was used to those whose heart rate was equal to or lower than 75 and heart rhythm was regular, and method B was used to those whose heart rate was over 75 or arrhythmic. Patients evaluated with method A had a mean DLP value of 79.37 mGy-cm (range: 34–144 mGy-cm) and a mean effective dose of 1.11 mSv (range: 0.47–2.01 mSv). Patients evaluated with method B had a mean value of DLP of 587.82 mGy-cm (range: 157–920 mGy-cm) and the corresponding mean of effective dose of 8.22 mSv (range: 2.19–12.88 mSv).
In 110 patients included in the study, 1760 coronary artery segments were evaluated. A total of 1444 of them (82%) received image quality score of 1, 248 (14%) received 2, 53 (3%) received 3 and 15 (1%) received 4 points. Distribution of 15 segments which took 4 points is presented in Table 1. Distribution of the mean score of image quality of each segment is shown in Table 2, as the average score of the given segment calculated. The interobserver agreement for image quality score and stenosis was good (κ=0.80) for all segments.
Table 1.
Distribution of segments with 4 points.
| RCA-p | RCA-m-d | RCA-PDA | RCA-PL | Dİ | D2 | LCX-PL | CX-d | OM1 | OM2 |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 3 | 1 | 1 | 2 | 1 | 2 | 1 | 1 | 2 |
RCA – right coronary artery; PDA – posterior descending artery; PL – posterolateral branch; D –: diagonal; LCx – left circumflex artery; OM – obtus marginalis; p – proximal; m – middle; d – distal; 4 points – segments that cannot be assessed.
Table 2.
Mean image quality scores of the segments.
| Segment | RCA (p) | RCA (m) | RCA (d) | RCA (PDA) | RCA (PL) | LMCA |
|---|---|---|---|---|---|---|
| Score | 1.25 | 1.29 | 1.44 | 1.37 | 1.35 | 1.01 |
| Segment | LAD (p) | LAD (m) | LAD (d) | D1 | D2 | |
| Score | 1.03 | 1.07 | 1.27 | 1.19 | 1.25 | |
| SEGMENT | LCX(p) | OMİ | LCX(d) | OM2 | LCX(PL) | RI |
| Score | 1.12 | 1.19 | 1.32 | 1.39 | 1.19 | 1.01 |
RCA – right coronary artery; PDA – posterior descending artery; PL – posterolateral branch; D – diagonal; LCx – left circumflex artery; OM – obtus marginalis; LMCA – left main coronary artery; RI – ramus intermedius; p – proximal; m – middle; d – distal.
According to the assessment, the highest image quality scores were recorded for segments of LMCA and RI (1.01), followed by proximal (1.03) and middle (1.07) segments of LAD. The lowest image quality was for the distal branches of RCA (1.44). The OM2 branch of LCX (1.39) and the PDA branch of RCA in the right dominant systems had the lowest image quality scores.
Image quality score per patient was calculated by taking the mean value of scores per segment. Six (5%) of 110 patients obtained image quality score higher than 2, while the remaining 104 patients (95%) a score of ≤2; all of the examinations were diagnostic.
Variables according to gender, especially ED and DLP, were evaluated by independent samples t-test. Comparison of variables according to gender is shown in Table 3. Mean DLP value was 368.57 mGy-cm and ED was 5.16 mSv for all men regardless of the procedure technique while for women mean DLP value was 453.83 mGy-cm and ED was 6.35 mSv, also regardless of the procedure technique. P value was found to be 0.117 and 0.120 for men and women respectively and there was no statistically significant difference.
Table 3.
Comparison of the variable parameters according to gender.
| Parameters | Male | Female | P value | ||
|---|---|---|---|---|---|
| Mean | Standard deviation | Mean | Standard deviation | ||
| Age (year) | 52.46 | 11.57 | 55.21 | 10.19 | .197 |
| Heart rate (beats/min) | 74.52 | 11.85 | 80.31 | 13.93 | .021* |
| DLP | 368.57 | 272.58 | 453.83 | 288.43 | .117 |
| ED-mSv | 5.16 | 3.82 | 6.35 | 4.04 | .120 |
| Contrast (mL) | 78.87 | 7.88 | 81.73 | 8.16 | .068 |
| Average image quality score | 1.17 | 0.26 | 1.31 | 0.41 | .043* |
DLP – dose-length product; ED-mSv – effective dose- millisievert.
Among 61 male patients, 24 were evaluated with method A and 37 were evaluated with method B. The mean value of ED was 0.967 mSv in method A and 7.879 mSv in method B. Among 49 female patients, 16 were evaluated with method A and 33 were evaluated with method B. The mean value of ED was 1.327 mSv in method A and 8.621 mSv in method B among females. Comparison of ED values with Student’s t-test for males and females resulted in a p-value equal to 0.03 (p<0.05) which showed that the difference was statistically significant. However, p-value was 0.10 in patients of method B and there was no significant difference between male and female doses.
The mean value of contrast media used during the procedure was 80.15 mL (range: 65–98 mL). ED and amount of contrast media given were compared between procedure protocols in method A and method B by independent samples t-test. The mean value of ED was 1.11 mSv in method A and 8.23 mSv in method B. The difference was statistically significant (p=0.000).
The mean amount of contrast media in method A was 72.65 mL and 84.43 mL in method B, which represents a significant difference (p=0.000). Mean score of image quality was 1.03 in method A while it was 1.35 in method B. When compared, this showed a strong significant difference (p=0.000).
Mean values of DLP, ED, amount of contrast given and image quality scores were evaluated with one-way ANOVA test initially, and multiple comparisons were performed with post hoc Tukey’s test between 3 groups divided according to the heart rate of patients. The results are displayed in Table 4.
Table 4.
Comparison with post hoc Tukey’s test of DLP, ED, amount of contrast agent and average image quality score with heart rate.
| Heart rate (<60) Group 1 | Heart rate (60–75) Group 2 | Heart rate (>75) Group 3 | ||||
|---|---|---|---|---|---|---|
| Mean | Standard deviation | Mean | Standard deviation | Mean | Standard deviation | |
| DLP | 80.85 | 36.64 | 140.55 | 192.74 | 576.41 | 182.72 |
| ED-mSv | 1.13 | 0.51 | 1.97 | 2.70 | 8.07 | 2.56 |
| Contrast (mL) | 73.69 | 3.25 | 73.03 | 7.05 | 84.41 | 5.87 |
| Average image quality score | 1.02 | 0.04 | 1.04 | 0.08 | 1.36 | 0.38 |
| Post-Hoc Tukey Test p value | ||||||
| Group 1–2 | Group 1–3 | Group 2–3 | ||||
| DLP | .566 | .000 | .000*** | |||
| ED-mSv | .566 | .000 | .000*** | |||
| Contrast | .942 | .000 | .000*** | |||
| Average image quality score | .986 | .001 | .000*** | |||
DLP – dose-length product; ED-mSv – effective dose- millisievert.
ED values were under 1 mSv in 20 patients and 1–2 mSv in 20 patients with method A. ED value was 10 mSv or higher in 14 patients with method B. All of those patients belonged to high heart rate group.
Coronary CTA and CCA results of 23 patients who had showed moderate to severe stenosis during coronary CTA and underwent CCA in the following 2 weeks were calculated based on specificity, sensitivity, positive and negative predictive values of 95% confidence interval with CCA results considered as a standard for reference. The sensitivity of our study was 100%, specificity 90%, positive predictive value 92.85%, negative predictive value 100% and test validity 95.65%.
Discussion
Conventional coronary angiography is the gold standard in the diagnostics of CAD which is an important cause of morbidity and mortality all over the world. However, radiation exposure of the patients and health-care personnel during the procedure, possible complications during and after the procedure, costs of hospitalization of patients, and, most importantly, invasiveness of the procedure are some of the most important limitations. Moreover, only 30% of CCA were performed to rule out the diagnosis of CAD [4]. To overcome this limitation, researchers have investigated different methods.
Clinical application of CTA was introduced with electron-beam tomography in 1984 by Boyd et al. [12] and continued by Flohr et al. [13] with the first four-slice retrospective gated CT in 1998 which reduced temporal resolution to 250 ms. In their study, 88% of coronary artery segments could be displayed in a patient population with an average heart rate of 71.8±13 beats/min before the application of beta-blockers. They also showed that 16-slice CT did not require heart rate to be lower than 65 beats/min (with the help of beta-blockers) for optimum viewing, which was required by 4-section CT, and so diagnostic quality imaging could be carried out even with heart rates of up to 80 beats/min [14].
With advances in multidetector technology, Leschka et al., in their studies including 54 patients, performed with the use of 64-slice CT which started to be used in 2004, showed that all significant stenoses of the coronary arteries could be demonstrated with high diagnostic accuracy by multisegment reconstruction algorithms without the use of beta-blockers [15–17]. Despite this fact, many studies have suggested the use of beta-blockers and the authors used them. In 2007, in the study by Brodoefel et al. [18] which included 102 patients and applied 64-slice CT with administration of beta-blockes, the image quality was lower but the diagnostic accuracy was not affected when patients with a heart rate of 75 beats/min were compared with those under 65 beats/min.
In our study, patients’ heart rates ranged from 46 to 117 (mean 76.9 beats/min). Coronary artery segments which could not be diagnostically displayed constituted only 1%. We found similar results to the studies mentioned in the literature, and high diagnostic accuracy was obtained even in high heart rates. Paul et al. [19] demonstrated that high diagnostic image quality could be obtained without movement or breathing artifact at a low radiation dose with 128×2-slice dual source prospective triggering CT, accepting 70 beats/min as the limit heart rate value in 96 patients without the use of beta-blockers. In our study, method A accepting 75 beats/min as the limit value was able to scan with 75 ms temporal resolution and reconstruct the whole heart in one heart beat in 40 patients. We obtained higher quality images with method A. We also used method B to image patients with heart rates higher than 75 beats/min or with irregular rhythm.
If we compare the number of patients in our study with the literature, we find the following: Tsilifkas et al. [20] 170 patients in 2010, Achenbach et al. [21] 50 patients in 2010, Lell et al. [22] 25 patients in 2009, Yi-ning et al. [23] 75 patients in 2010. When compared with other studies, 110 patients included in our study is an adequate number.
In 2009, Smith-Bindman et al. [24], in their study investigated the radiation doses of 1119 patients in CT at different centers according to the values of DLP and ED. In this study, the mean value of ED in cardiac CT was 22 mSv (7–39) which was a dose equivalent to 309 chest X-rays. The risk of developing cancer in women was reported to be 1/270 and in men 1/600 if they had coronary CTA in their 40sbased on the knowledge that radiation exposure to younger patients and women would increase the incidence of cancer in later years.
In our study, ED values were under 1 mSv in 20 of 110 patients. The mean ED value of 40 patients was 1.11 mSv with method A; the mean ED value of 70 patients was 8.22 mSv with method B. When 110 patients were evaluated together, the mean radiation dose was 5.64 mSv which indicated a decline of 74.3% according to the report of 2009.
Another result of our study is the the statistically significant difference between the amounts of contrast used; it was 72.65 mL in method A and 84.43 mL in method B. It is is also necessary to avoid unnecessary use of contrast agents like avoiding unnecessary radiation. In 2013, Layritz et al. [25] in their dual-source cardiac CT study carried out in 100 patients reconstructed images by FBP (filtered back projection) technique in half of the patients with a high-concentration contrast agent (Iopromide 370) using either the standard 100 kVp or 120 kVp if the patient’s BMI was greater than 25, while reconstructing images by IR (iterative reconstruction) technique in other half of the patients with low-concentration contrast agent (iodixanol 270) using either 800 kVp or 100 kVp if the patient’s BMI was greater than 25. There was no significant difference between the 2 groups with regard to attenuation values, image quality and noise ratio but there was a decrease of 56.4% in the radiation dose. Although we did not aim to reduce the dose by displaying with 80 kVp or reducing the amount of constrast medium, we observed that method A reduced the radiation dose and the amount of contrast agent when compared with method B.
The retrospective nature of our study might be perceived as a limitation. Sometimes patients with the same BMI values were evaluated with different tube voltage and current values and different results were obtained because of the lack of protocols which would adjust the standardized kVp-mAs values according to the patient’s weight or BMI. Studies using standardized protocols according to BMI values, with a higher sample size are needed. In addition, our study had one major limitation, i.e. a small number of patients compared with CCA.
Conclusions
In conclusion, awareness of radiation led to new dual-source systems of CT technologies which can display high-quality imaging in selected patients with ED values of ≤1 mSv. With the limit of the heart rate of 75 beats/min, high-quality images were obtained with method A in patients who did not use beta-blockers. Coronary CTA may be helpful to rule out CAD in low-to-moderate risk patients without premedication because of its high negative predictive value and low radiation doses.
References
- 1.American Heart Association. Heart disease and stroke statistics – 2006 update. Dallas, Texas: American Heart Association; 2007. [Google Scholar]
- 2.Stary HC, Chandler AB, Dinsmore RE, et al. A definition of advanced types of atherosclerotic lesions and a histologic classification of atherosclerosis. Circulation. 1995;92:1355–74. doi: 10.1161/01.cir.92.5.1355. [DOI] [PubMed] [Google Scholar]
- 3.Pasterkamp G, Falk E, Woutman H, et al. Techniques characterizing the coronary atherosclerotic plaque: influence on clinical decision making. J Am Coll Cardiol. 2000;36:13–21. doi: 10.1016/s0735-1097(00)00677-x. [DOI] [PubMed] [Google Scholar]
- 4.Scanlon PJ, Faxon DP, Audet AM, et al. ACC/AHA guidelines for coronary angiography. A report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (Committee on Coronary Angiography). Developed in collaboration with the Society for Cardiac Angiography and Interventions. J Am Coll Cardiol. 1999;33:1756–824. doi: 10.1016/s0735-1097(99)00126-6. [DOI] [PubMed] [Google Scholar]
- 5.Windecker S, Maier-Rudolph W, Bonzel T, et al. Interventional cardiology in Europe in 1995: working group coronary circulation of the European Society of Cardiology. Eur Heart J. 1999;20:484–95. doi: 10.1053/euhj.1998.1356. [DOI] [PubMed] [Google Scholar]
- 6.Kalender WA, Seissler W, Klotz E, Vock P. Spiral volumetric CT with single breathhold technique, continous transport, and continous scanner rotation. Radiology. 1990;176:181–83. doi: 10.1148/radiology.176.1.2353088. [DOI] [PubMed] [Google Scholar]
- 7.Yang X, Yang J, Tian F, et al. High-pitch dual-source CT in prospectively electrocardiogram-trigerred spiral double scanning mode for diagnosing coronary artery patency. Nan Fang Yi Ke Da Xue Xue Bao. 2013;33:1605–10. [PubMed] [Google Scholar]
- 8.Sun K, Han RJ, Ma LJ, et al. Prospectively electrocardiogram-gated high-pitch spiral acquisition mode dual-source CT coronary angiography in patients with high heart rates: comparison with retrospective electrocardiogram-gated spiral acquisition mode. Korean J Radiol. 2012;13:684–93. doi: 10.3348/kjr.2012.13.6.684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang X, Fang J, Tong H, et al. High-pitch dual-source CT coronary angiography: analysis of the impact on image quality of altered electrocardiography waves during data acquisition. Int J Cardiovasc Imaging. 2012;28:15–20. doi: 10.1007/s10554-012-0078-5. [DOI] [PubMed] [Google Scholar]
- 10.Achenbach S, Marwan M, Schepis T, et al. High-pitch spiral acquisition: a new scan mode for coronary CT angiography. J Cardiovasc Comput Tomogr. 2009;3:117–21. doi: 10.1016/j.jcct.2009.02.008. [DOI] [PubMed] [Google Scholar]
- 11.Yuceler Z, Kantarci M, Yuce I, et al. Follow-up of coronary artery bypass graft patency: diagnostic efficiency of high-pitch dual-source 256-slice MDCT findings. J Comput Assist Tomogr. 2014;38:61–66. doi: 10.1097/RCT.0b013e3182a58a8c. [DOI] [PubMed] [Google Scholar]
- 12.Boyd DP. Transmission computed tomography. In: Newton Th, Potts DG., editors. Radiology of the skull and brain Technical aspects of computed tomography. Vol. 5. C.V. Mosby Company; St. Louis: 1981. pp. 4357–71. [Google Scholar]
- 13.Flohr T, Ohnesorge B. Heart-rate adaptive optimization of spatial and temporal resolution for ECG-gated multi-slice spiral CT of the heart. J Comp Assist Tomogr. 2001;25:907–23. doi: 10.1097/00004728-200111000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Hoffmann MH, Shi H, Schmitz BL, et al. Noninvasive coronary angiography with multislice computed tomography. JAMA. 2005;293:2471–78. doi: 10.1001/jama.293.20.2471. [DOI] [PubMed] [Google Scholar]
- 15.Leschka S, Alkadhi H, Plass A, et al. Accuracy of MSCT coronary angiography with 64-slice technology: first experience. Eur Heart J. 2005;26:1482–87. doi: 10.1093/eurheartj/ehi261. [DOI] [PubMed] [Google Scholar]
- 16.Leschka S, Scheffel H, Desbiolles L, et al. Image quality and reconstruction intervals of dual-source CT coronary angiography: recommendations for ECG-pulsing windowing. Invest Radiol. 2007;42:543–49. doi: 10.1097/RLI.0b013e31803b93cf. [DOI] [PubMed] [Google Scholar]
- 17.Leschka S, Stolzmann P, Desbiolles L, et al. Diagnostic accuracy of high-pitch dual-source CT for the assessment of coronary stenoses: first experience. Eur Radiol. 2009;19:2896–903. doi: 10.1007/s00330-009-1618-9. [DOI] [PubMed] [Google Scholar]
- 18.Brodoefel H, Reimann A, Burgstahler C, et al. Noninvasive coronary angiography using 64-slice spiral computed tomography in an unselected patient collective: Effect of heart rate, heart rate variability and coronary calcifications on image quality and diagnostic accuracy. Eur J Radiol. 2008;66:134–41. doi: 10.1016/j.ejrad.2007.05.013. [DOI] [PubMed] [Google Scholar]
- 19.Paul JF, Amato A, Rohnean A. Low-dose coronary-CT angiography using step and shoot at any heart rate: comparison of image quality at systole for high heart rate and diastole for low heart rate with a 128-slice dual-source machine. Int J Cardiovasc Imaging. 2013;29:651–57. doi: 10.1007/s10554-012-0110-9. [DOI] [PubMed] [Google Scholar]
- 20.Tsiflikas I, Brodoefel H, Reimann A, et al. Coronary CT angiography with dual source computed tomography in 170 patients. Eur J Radiol. 2010;74:161–65. doi: 10.1016/j.ejrad.2009.01.039. [DOI] [PubMed] [Google Scholar]
- 21.Achenbach S, Marwan M, Ropers D, et al. Coronary computed tomography angigraphy with a consistent dose below 1 mSv using prospectively electrocardiogram-triggered high-pitch spiral acquisition. Eur Heart J. 2010;31:340–46. doi: 10.1093/eurheartj/ehp470. [DOI] [PubMed] [Google Scholar]
- 22.Lell M, Marwan M, Schepis T, et al. Prospectively ECG-triggered high-pitch spiral acquisition for coronary CT angiography using dual-source CT: technique and initial experience. Eur Radiol. 2009;19:2576–83. doi: 10.1007/s00330-009-1558-4. [DOI] [PubMed] [Google Scholar]
- 23.Yi-ning W, Shuo L, Ling-yan K, et al. Coronary computed tomographic angiography using low-dose prospectively electrocardiographic triggered high-pitch spiral acquisition by dual-source computed tomography: Image quality and radiation dose. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2010;32:597–600. doi: 10.3881/j.issn.1000.503X.2010.06.001. [DOI] [PubMed] [Google Scholar]
- 24.Smith-Bindman R, Lipson J, Marcus R, et al. Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern Med. 2009;169:2078–86. doi: 10.1001/archinternmed.2009.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Layritz C, Muschiola G, Flohr T, et al. Automated attenuation-based selection of tube voltage and tube current for coronary CT angiography: Reduction of radiation exposure versus a BMI-based strategy with an expert investigator. J Cardiovasc Comput Tomogr. 2013;7:303–10. doi: 10.1016/j.jcct.2013.08.010. [DOI] [PubMed] [Google Scholar]