Abstract
Background
Few studies have reported the safety and efficacy of hybrid surgery (HS), and some of the studies comparing HS with ACDF have reported conflicting results. We conducted this meta-analysis to clarify the advantages of HS in the treatment of multilevel cervical spondylosis.
Material/Methods
We performed a systematic literature search in PubMed, Medline, and CNKI to identify relevant controlled trials published up to October 2015. The standardized mean difference (SMD) and 95% confidence interval (95% CI) of the perioperative parameters, visual analogue scale pain score (VAS), neck disability index (NDI), and range of motion (ROM) of C2–C7 and adjacent segments were calculated. We also analyzed complications and Odom scale scores using risk difference (RD) and 95% CI.
Results
In total, 7 studies were included. The pooled data exhibited significant differences in blood loss between the 2 groups. However, there was no evidence indicating significant differences in operation time, complications, VAS, NDI, or Odom scale scores. Compared with the ACDF group, the HS group exhibited significantly protected C2-C7 ROM and reduced adjacent-segment ROM.
Conclusions
The safety of HS may be as good as that of ACDF. Furthermore, HS is superior to ACDF in conserving cervical spine ROM and decreasing adjacent-segment ROM. However, the results should be accepted cautiously due to the limitations of the study. Studies with larger sample sizes and longer follow-up periods are required to confirm and update the results of the present study.
MeSH Keywords: Cervicoplasty, Meta-Analysis, Spinal Fusion
Background
With successful fusion rates and satisfactory clinical results, anterior cervical discectomy and fusion (ACDF) is a standard technique for treating cervical disc disease [1,2]. Although ACDF is the most widely accepted procedure, with further study and extension of follow-up time, certain questions have arisen. The surgical procedure relieves symptoms but deprives patients of surgical-segment motor function, which may cause or accelerate adjacent segment degeneration (ASD). ASD is a common complication of ACDF, especially in long-term fusion, affecting approximately 25% of patients within 10 years after the initial surgery [3].
With advances in surgical techniques, artificial arthroplasty was developed and used for the treatment of cervical disc disease, gaining widespread popularity. Artificial disc replacement (ADR) is used in the surgery procedure, which largely retains the cervical spine range of motion. Although the results of artificial arthroplasty are less established, the technique is beneficial in terms of preserving the motion of the cervical spine and reducing degeneration of adjacent levels [4,5], especially in multilevel surgeries [6,7]. However, some studies reported that prosthesis implantation may require a longer procedure, which can lead to the possibility of increasing blood loss and wound complications [8–10]. Furthermore, compared with the broad indications of ACDF, use of ADR is limited to a more stringently selected group of patients.
Hybrid surgery (HS) incorporates ACDF and artificial arthroplasty by combining the advantages of these 2 technologies, thus retaining cervical spine motion as much as possible without prolonging the operation time or increasing complications. To obtain a reliable conclusion to the existing controversial situation, we performed a meta-analysis to compare the operation time, blood loss, evaluation of clinical outcomes, and radiographic evaluation between HS and ACDF.
Material and Methods
Literature search strategy
Electronic databases PubMed, MEDLINE, and CNKI (China National Knowledge Infrastructure, a widely used search engine in China) were searched for relevant reports published up to October 2015. The following keywords or phrases were used: “hybrid surgery” or “arthroplasty or prosthesis or (disc replacement) combine fusion or ACDF or (anterior discectomy and fusion)” and “cervical”. There was no restriction on language. We screened the reference lists of all eligible articles manually to find more papers.
Inclusion and exclusion criteria
Inclusion criteria were: (1) all patients were diagnosed as having multilevel cervical spondylosis and had undergone an anterior procedure; (2) studies involving the comparison between HS and ACDF; (3) a clear assessment of surgical results; and (4) available data could be obtained from the literature included, or obtained by calculation. Exclusion criteria were: (1) the study involved corpectomy; (2) the study was a review article, case report or conference article; (3) it was an experimental in vitro or biomechanical study; (4) the study reported on special populations (e.g., elderly, infants, pregnant women); or (5) the full text was not available.
Study selection
We reviewed the titles and abstracts to find papers that met the inclusion criteria. In the presence of uncertainty regarding the relevance of a paper, a full-text assessment was conducted. Because the data used for this study were retrieved from the literature, we did not need to obtain approval from our Ethics Committee.
Data extraction
Two authors independently extracted the following data from each included study: operation time, blood loss, complications, preoperative and postoperative visual analogue scale pain score (VAS), preoperative and postoperative neck disability index (NDI), preoperative and postoperative Japanese Orthopedic Association (JOA) score, preoperative and postoperative C2–C7 range of motion (C2–C7 ROM), preoperative and postoperative adjacent segment range of motion (superior adjacent segment ROM and inferior adjacent segment ROM), and Odom score. The following data were recorded: first author, publication date, mean age, sample size, length of follow-up, major evaluation index, and prosthesis type. These data were then compiled into a standard table. Any disagreement was resolved by consultation with an arbiter.
Validity assessment
We performed the quality assessment based on the Cochrane risk of bias assessment tools for randomized trial and the Newcastle-Ottawa quality assessment scale (NOS) for non-randomized trials [11]. Any disagreements were resolved by discussion.
Statistical analysis
Statistical analysis was performed with Review Manager 5.2 and Stata 12.0 software. Standard mean differences (SMDs) and corresponding 95% confidence intervals (CIs) were used to measure the major outcomes of the 2 surgical approaches. Homogeneity testing was performed using the I2 statistic. A fixed-effects model was used to combine the SMDs in the absence of heterogeneity (I2 ≤50%); otherwise, a random-effects model was used. Additionally, we performed a sensitivity analysis to assess the effect of a single study on the overall estimate by removing each study included, one at a time. For detecting potential publication bias, we performed Begg’s and Egger’s tests; in the present study, this result was considered as statistically significant if the p-value was less than 0.05.
Results
Characteristics of selected studies
Initially, 404 records were retrieved according to the search strategy. Among these, 90 reports were excluded as duplicate studies. In total, 307 reports were excluded for not meeting the inclusion criteria after review of the title, abstract, or full text. After the review, 7 studies were included [12–18] (Figure 1). No additional study was obtained after review of reference lists. Seven eligible studies (1 RCT and 6 non-RCTs) consisting of 240 patients with cervical spondylosis (HS group, 114; ACDF group, 126) were published between 2009 and 2015. The average age of the patients was between 44.2 and 56.4 years. The general data of the included studies are summarized in Tables 1 and 2.
Figure 1.
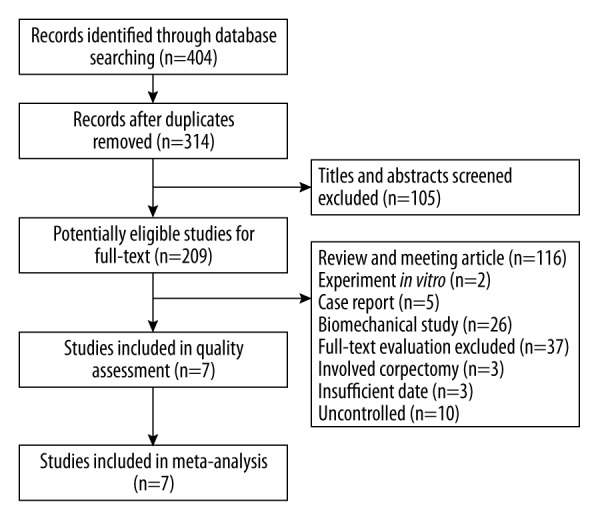
Flow diagram of literature screening.
Table 1.
Basic character of included studies.
| Author | Publication year | Country | Mean age (HS/ACDF) | Sample size (HS/ACDF) |
|---|---|---|---|---|
| Shin et al. | 2009 | Korea | 45.7/48 | 20/20 |
| Kang et al. | 2012 | China | 53.6/55.3 | 12/12 |
| Liu et al. | 2012 | China | 53.7/56.4 | 17/17 |
| Shen et al. | 2013 | China | 54.2/54.9 | 18/30 |
| Hey et al. | 2013 | Singapore | 51/48 | 7/7 |
| Grasso | 2015 | Italy | 44.2/47.3 | 20/20 |
| Ji et al. | 2015 | Korea | 45.7/48 | 20/20 |
HS – hybrid surgery of anterior cervical discectomy and fusion combine with artificial arthroplasty; ACDF – anterior cervical discectomy and fusion.
Table 2.
Surgery and follow-up character of included studies.
| Author | Follow-up time | No. of operative segment | Major evaluation index | Prosthesis type |
|---|---|---|---|---|
| Shin et al. | 2 year | 2 level | NDI VAS ROM | Mobi-C |
| Kang et al. | 2 year | 3 level | NDI VAS ROM | Prodisc-C |
| Liu et al. | 6 months | 2 level | NDI JOA ROM | Prodisc-C |
| Shen et al. | 24.1 months (18–24 months)* | 2 level | NDI JOA ROM | Bryan |
| Hey et al. | 2 year | 2 level and 3 leve | NDI VAS | Prodisc-C |
| Grasso | >2 year | 2 level | NDI VAS ROM | Prodisc-C |
| Ji et al. | 5 year | 2 level | NDI VAS ROM | Mobi-C |
NDI – Neck Disability Index; VAS – visual analogue scale pain score; JOA – Japanese Orthopedic Association; ROM – range of motion;
Mean time of follow-up (range).
Risk of bias assessment
Only 1 RCT was conducted using quality assessment based on Cochrane risk of bias assessment tools. Randomization was conducted using the odd or hospital number, which prompted a high risk; adequate concealment of allocation was hard to guarantee or was unclear (Figure 2). Six non-RCTs used NOS and all scores were greater than 7, showing higher quality (Table 3).
Figure 2.
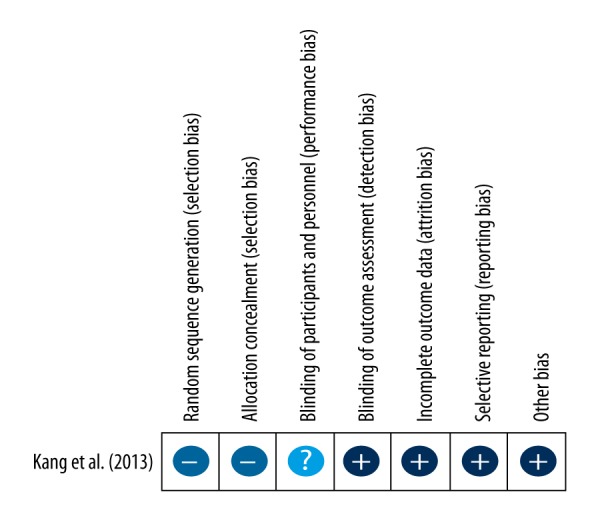
Summary of bias risk of randomized controlled trials.
Table 3.
Newcastle-Ottawa quality assessment scale (NOS) for non-randomized trials.
| Quality assessment for non-randomized trials | Shin et al. | Liu et al. | Hey et al. | Shen et al. | Grasso | Ji et al. |
|---|---|---|---|---|---|---|
| Selection | ||||||
| Is the case definition adequate | * | * | * | * | * | * |
| Representativeness of the cases | * | * | * | * | * | * |
| Selection of Controls | * | * | * | * | * | * |
| Definition of Controls | ||||||
| Comparability | ** | ** | ** | ** | ** | ** |
| Exposure | ||||||
| Ascertainment of exposure | * | * | * | * | * | * |
| Same method of ascertainment for cases and controls | * | * | * | |||
| Non-Response rate | * | * | * | * | * | * |
| Total score | 7 | 8 | 8 | 7 | 8 | 7 |
Meta-analysis
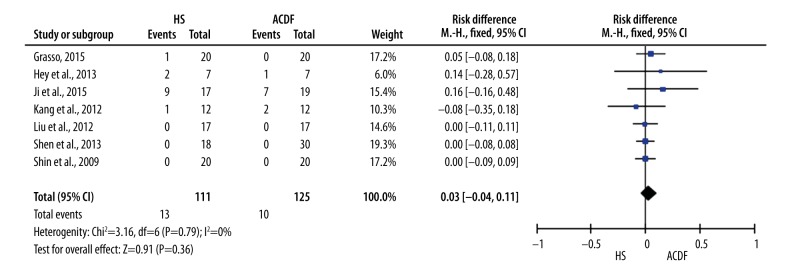
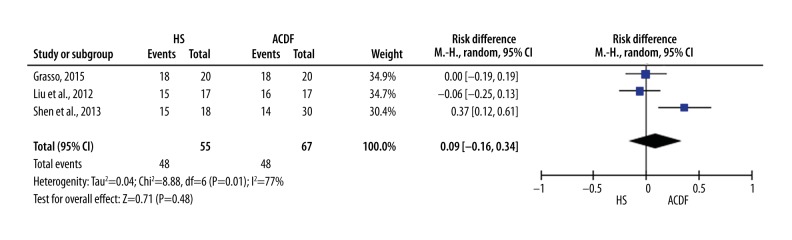
We analyzed differences between the 2 groups in operation times, blood loss, complications, NDI, VAS, JOA, C2-C7 ROM, adjacent-segment ROM, and Odom score. Pooled data from the 7 included studies revealed no significant differences in operation times (Table 4). However, pooled data from the 4 relevant studies revealed a significant difference in blood loss (Table 4). We compared the complications between the 2 groups, and the pooled data from the 7 included studies revealed no significant differences in complications (Figure 3).
Table 4.
Meta-analysis results (operation time, blood loss, VAS and NDI).
| Outcome | No. of studies | Pooled effect | p-value | Heterogeneity | ||
|---|---|---|---|---|---|---|
| SMD | 95%CI | I2 | p-value | |||
| Operation time | 6 | 1.54 | −0.08, 3.16 | 0.06 | 95% | <0.00001 |
| Blood loss | 4 | −0.72 | −1.38, −0.05 | 0.04 | 73% | 0.01 |
| VAS | ||||||
| Preoperative | 2 | 0.05 | −0.59, 0.69 | 0.88 | 0 | 0.61 |
| Postoperative | 2 | −0.52 | −1.19, 0.15 | 0.13 | 67% | 0.08 |
| NDI | ||||||
| Preoperative | 3 | −0.06 | −0.58, 0.45 | 0.81 | 0 | 0.36 |
| Postoperative | 3 | −0.24 | −0.75, 0.28 | 0.37 | 0 | 0.39 |
Figure 3.
Forest plot for comparison of complications between HS group and ACDF group.
Two studies reported differences in preoperative and postoperative VAS between the 2 groups. The pooled SMD of preoperative and postoperative VAS were 0.05 and −0.52, respectively (Table 4). Three studies reported differences in preoperative and postoperative NDI between the 2 groups. No significant differences in preoperative NDI or postoperative NDI were noted (Table 4).
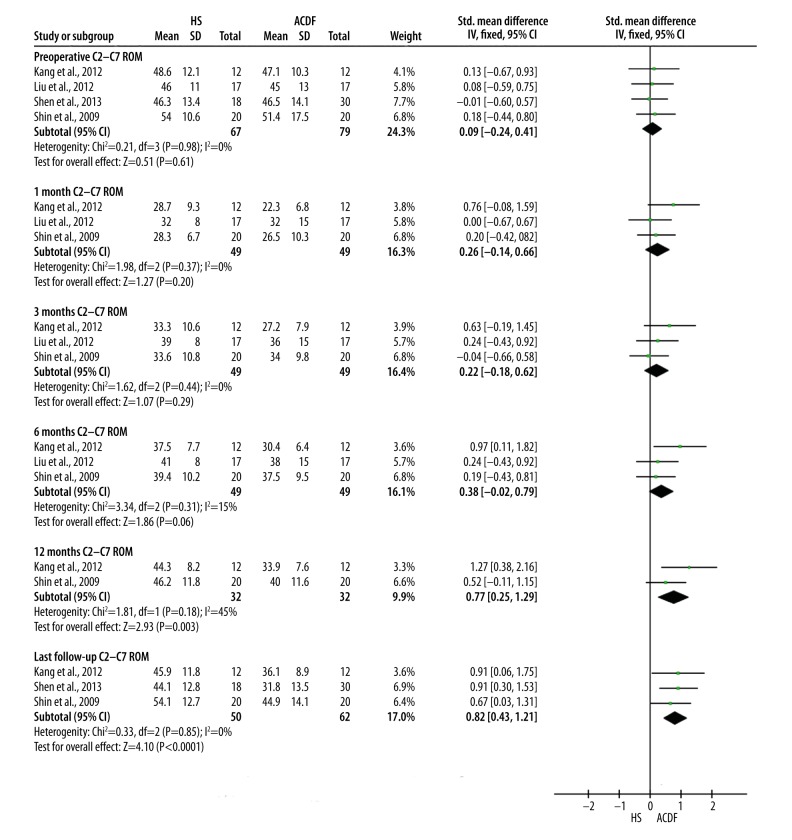
The pooled data revealed no significant differences in preoperative, postoperative 1-month, postoperative 3-month, or postoperative 6-month C2-C7 ROM (Figure 4). However, pooled data revealed a significant difference in postoperative 12-month and last follow-up C2–C7 ROM (Figure 4).
Figure 4.
Forest plot for comparison of C2–C7 ROM between HS group and ACDF group.
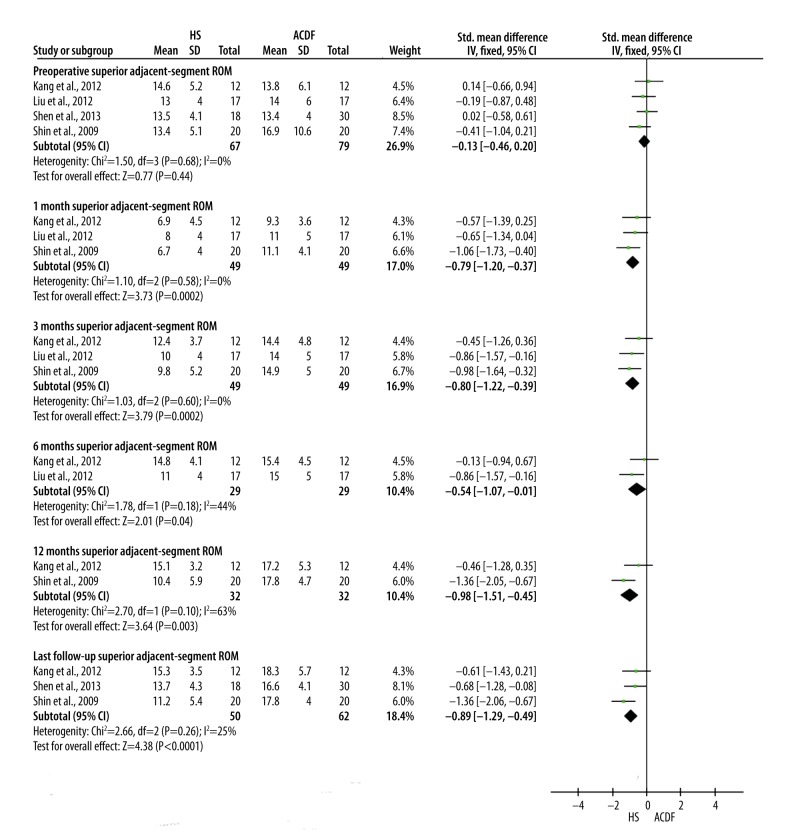
No significant differences in preoperative superior adjacent segment ROM were noted (Figure 5). However, the pooled data revealed a significant difference in postoperative superior adjacent-segment ROM at 1 month, 3 months, 6 months, 12 months, and the last follow-up superior adjacent-segment ROM (Figure 5).
Figure 5.
Forest plot for comparison of superior adjacent-segment ROM between HS group and ACDF group.
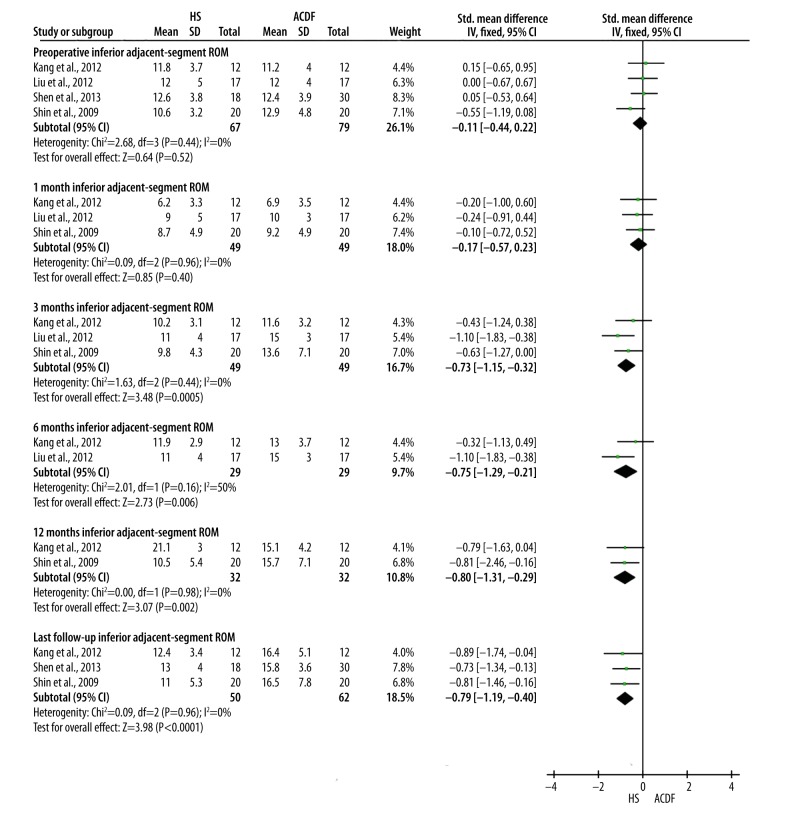
No significant differences in preoperative or postoperative 1-month inferior adjacent-segment ROM were noted (Figure 6). However, compared with the ACDF group, the pooled data revealed significant differences in postoperative inferior adjacent-segment ROM at 3 months, 6 months, 12 months, and the last follow-up in the HS group (Figure 6). Three studies reported Odom score and the pooled date revealed no significant differences in “good” scores between the groups (Figure 7).
Figure 6.
Forest plot for comparison of inferior adjacent-segment ROM between HS group and ACDF group.
Figure 7.
Forest plot for comparison of “good” rate between HS group and ACDF group.
Sensitivity analysis
We conducted a sensitivity analysis of operation time and blood loss between the 2 groups by eliminating each study sequentially from the relevant data. Stata 12.0 software was used to pool SMD for the remaining studies. The consistent results suggested that no single study significantly altered the combined results (Figures 8, 9).
Figure 8.
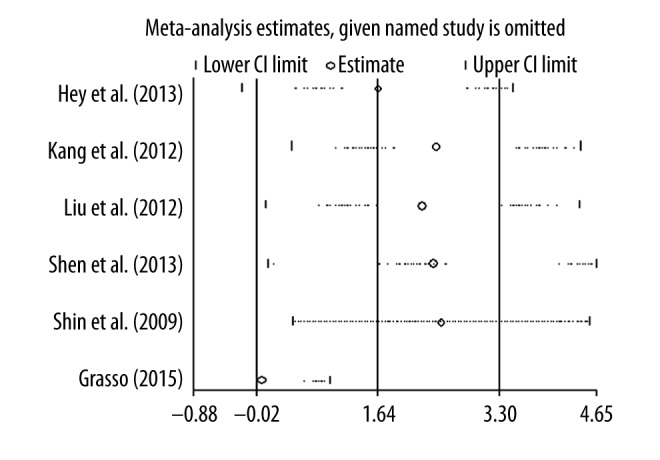
Plot of sensitivity analysis of operation time between HS group and ACDF group.
Figure 9.
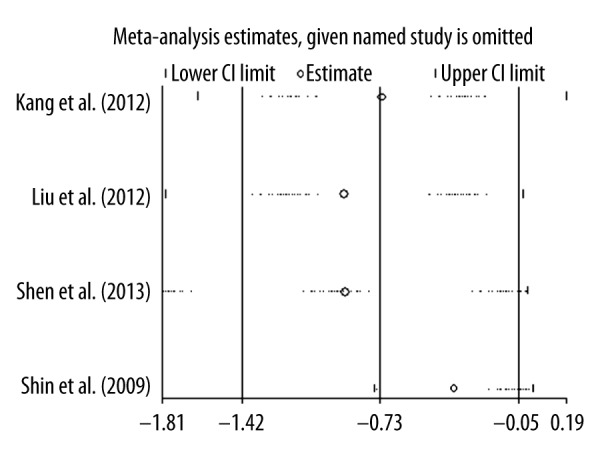
Plot of sensitivity analysis of blood loss between HS group and ACDF group.
Publication bias
We used Stata 12.0 software to detect publication bias for operation time and blood loss by using Egger’s and Begg’s tests. No substantial asymmetry was observed in Begg’s funnel plot (Figures 10, 11). Minimal evidence of publication bias was noted in Egger’s regression test (p=0.064 and 0.452, respectively).
Figure 10.
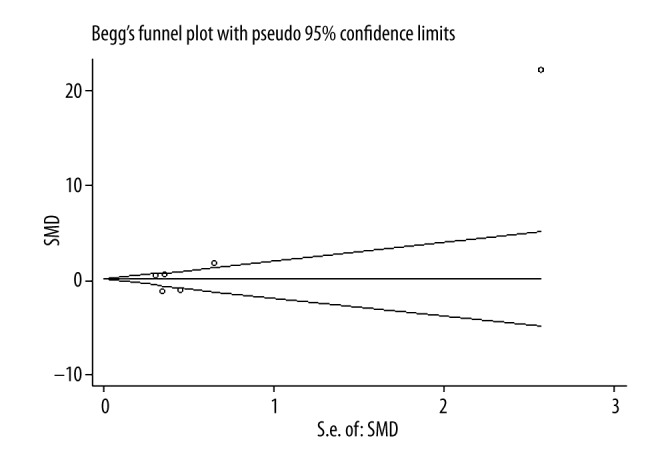
Funnel plot for publication bias of operation time.
Figure 11.
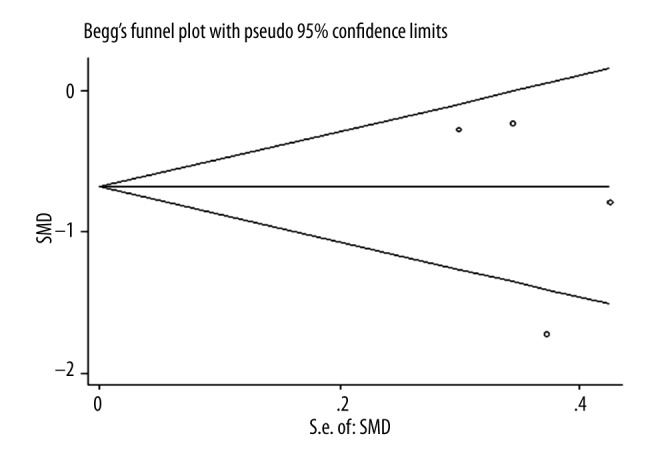
Funnel plot for publication bias of blood loss.
Discussion
In the treatment of cervical spondylosis, ACDF has been widely used [19]. With the use of spinal implants, this surgical procedure has enhanced the fusion rates, reduced postoperative immobilization, and improved clinical therapeutic effects [3,20]. Although ACDF benefits the target level, it may harm the adjacent segments. This feature is particularly prevalent in the case of multiple segments [21–23].
Previous studies have demonstrated that a segment fusion increases biomechanical stress and motion at adjacent levels, which may activate or facilitate degeneration at those levels [21,23–28]. Theoretically, when fewer segments are fused, there is less compensatory activity in the adjacent segments. Thus, the likelihood of ASD decreases. Brodke and Zdeblick reported that fusion rate in 1-level ACDF is as high as 97% [29], whereas the fusion rate in 3-level ACDF decreased to 83%. Swank et al. reported that the likelihood of pseudoarthrosis was 10% in 1-level surgery, but in 2-level and 3-level surgeries the rates increased to 44% and 54%, respectively [30].
If the segment where the surgery was performed maintains mobility, compensatory hyperkinesia is less likely to occur in adjacent segments [3]. Artificial disc replacement (ADR) is reported to diminish ASD [10,21,31–37]. The therapeutic effect of this non-fusion of arthroplasty for retaining motion and reducing hyperkinesia of the adjacent segment has been reported in patients with Klippel-Feil syndrome [36,38]. However, the biomechanical effect of artificial arthroplasty involving multiple segments, especially 3 or more segments, remains poorly understood. In addition, the clinical effect of this technique has not yet been examined in prospective controlled trials. Arthroplasty is associated with several problems, including high health-care costs, difficult implantation, and prosthesis-related complications [39]. In addition, ambiguous surgical indications and select patients may restrict its use.
HS incorporates ACDF and artificial arthroplasty. This technique reduces possible complications from multilevel ADR, while preserving cervical motion and largely avoiding the drawbacks of multilevel fusion [40]. Although surgical indication protocols of the North American Spine Society (NASS) and the International Society for the Advancement of Spine Surgery (ISASS) do not approve of ADR adjacent to pre-existing fusion in the USA, several studies have demonstrated that HS currently has a better therapeutic effect than ACDF. Nevertheless, minimal information is available comparing efficacy and safety between HS and ACDF for the treatment of multilevel cervical disc disease and the effect of the combination procedure on adjacent segments. The superiority of HS is not sufficiently demonstrated by the few small-sample studies done to date. Therefore, we conducted a meta-analysis to determine which surgical procedure is optimal for use in multilevel cervical fusion.
Safety
The pooled data of intraoperative and postoperative parameters suggested that the safety of HS is as good as that of ACDF for multilevel cervical spondylosis. Blood loss in the HS group was lower (p=0.04) compared to the ACDF group. However, no statistically significant difference in operation times (p=0.06) or complications (p=0.75) was found. Of note, the heterogeneity was extremely high. The source of heterogeneity may be the small sample size, differences in follow-up time, unclear assignment of different types (radiculopathy or myelopathy) of cervical spondylosis in the 2 groups, difference in the surgery section, and the presence or absence of iliac bone harvest. We investigated the reliability of these results with a subsequent sensitivity analysis. No single study significantly altered the combined results. We evaluated publication bias by Egger’s and Begg’s tests and the results revealed little evidence of publication bias.
The efficiency of clinical outcome
An increased postoperative Japanese Orthopaedic Association (JOA) score suggested better clinical outcome, whereas NDI and VAS suggested the opposite. The pooled data revealed no significant difference in the preoperative NDI and VAS. No significant difference in the postoperative NDI and VAS was noted. Although Liu et al. and Shen et al. reported increased JOA scores in HS [14,16], it is difficult to compare the JOA score between the 2 groups using the existing data. To date, we have no evidence indicating that HS exhibits a better clinical outcome than ACDF. There were no extremely high heterogeneities noted in the comparison of NDI and VAS between groups.
The efficiency of radiological outcome
Compared with ACDF, HS has the advantages of protecting cervical ROM and reducing the adjacent-segment ROM. The HS group exhibited significantly greater postoperative C2–C7 ROM. After 12 months, C2–C7 ROM was better retained in the HS group. The forest plot revealed that HS had better C2–C7 ROM with the extended follow-up period. Furthermore, the superior adjacent-segment ROM was reduced in the HS group at 1 month after surgery, whereas the inferior adjacent-segment ROM was increased at 3 months postoperatively. Similarly, forest plots also revealed that HS had lower superior and inferior adjacent-segment ROM with time progression. No extreme heterogeneity was noted.
Limitations
We must acknowledge the limitations of this study. First, although we have attempted to identify all studies that compared HS and ACDF, the sample size of our study was relatively small. Second, only 1 randomized control trial (RCT) and 6 non-RCTs were included in our study. Biases for randomization and unclear allocation in the RCT were found. Although NOS score of non-RCTs ranged from 7 to 8 and can be considered to be of higher quality, no estimate sample size was described. These defects reduced the level of evidence. Third, 6 of the 7 included studies were from Asia, and geographical limitations may impact the results of our study [12–16]. Fourth, in 1 report the follow-up time was only 6 months [14], and 3 reports [12,14,16] claimed that there were no complications, which may lead to underestimate of complications. Fifth, the various numbers or levels of surgical segments may affect the results. Sixth, there was unclear assignment of different types (radiculopathy or myelopathy) of cervical spondylosis in the 2 groups and no statistical analysis explained this shortcoming. This situation may lead to inaccurate estimation of certain evaluations. Seventh, we could not complete the statistical analysis of the JOA scores. Eighth, although a 5-year follow-up study stated that no difference was found in fusion rate between the 2 groups [18] (p=0.551), we cannot complete the overall effect statistical analysis because the other studies did not mention this indicator. Finally, the different research centers and surgical teams may have affected the results.
Conclusions
This meta-analysis suggests that the safety of HS is as good as that of ACDF, with similar operation time, similar complication rate, and reduced blood loss. Although HS has a similar VAS and NDI compared with ACDF, this surgery is an effective procedure for protecting cervical ROM and decreasing adjacent-segment ROM. However, there are limitations to our study. Further evaluation and large-sample multi-center RCTs are required to confirm and update the results of this study.
Footnotes
Source of support: Departmental sources
References
- 1.Bohlman HH, Emery SE, Goodfellow DB, Jones PK. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am. 1993;75(9):1298–307. doi: 10.2106/00004623-199309000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Bose B. Anterior cervical fusion using Caspar plating: analysis of results and review of the literature. Surg Neurol. 1998;49(1):25–31. doi: 10.1016/s0090-3019(97)00306-6. [DOI] [PubMed] [Google Scholar]
- 3.Hilibrand AS, Carlson GD, Palumbo MA, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am. 1998;81(4):519–28. doi: 10.2106/00004623-199904000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Pimenta L, McAfee PC, Cappuccino A, et al. Superiority of multilevel cervical arthroplasty outcomes versus single-level outcomes: 229 consecutive PCM prostheses. Spine (Phila Pa 1976) 2007;32(12):1337–44. doi: 10.1097/BRS.0b013e318059af12. [DOI] [PubMed] [Google Scholar]
- 5.Phillips FM, Tzermiadianos MN, Voronov LI, et al. Effect of two-level total disc replacement on cervical spine kinematics. Spine(Phila Pa 1976) 2009;34( 22):E794–99. doi: 10.1097/BRS.0b013e3181afe4bb. [DOI] [PubMed] [Google Scholar]
- 6.Cardoso MJ, Rosner MK. Multilevel cervical arthroplasty with artificial disc replacement. Neurosurg Focus. 2010;28(5):E19. doi: 10.3171/2010.1.FOCUS1031. [DOI] [PubMed] [Google Scholar]
- 7.Huppert J, Beaurain J, Steib JP, et al. Comparison between single- and multi-level patients: clinical and radiological outcomes 2 years after cervical disc replacement. Eur Spine J. 2011;20(9):1417–26. doi: 10.1007/s00586-011-1722-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murrey D, Janssen M, Delamarter R, et al. Results of theprospective, randomized, controlled multicenter Food and Drug Administration investigational device exemption study of the ProDisc-C total disc replacement versus anterior discectomy and fusion for the treatment of 1-level symptomatic cervical disc disease. Spine J. 2009;9(4):275–86. doi: 10.1016/j.spinee.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 9.Sasso RC, Anderson PA, Riew KD, Heller JG. Results of cervical arthroplasty compared with anterior discectomy and fusion: four-year clinical outcomes in a prospective, randomized controlled trial. J Bone Joint Surg Am. 2011;93(18):1684–92. doi: 10.2106/JBJS.J.00476. [DOI] [PubMed] [Google Scholar]
- 10.Sasso RC, Smucker JD, Hacker RJ, Heller JG. Artificial discversus fusion: a prospective, randomized study with 2-year follow-up on 99 patients. Spine (Phila Pa 1976) 2007;32(26):2933–40. doi: 10.1097/BRS.0b013e31815d0034. [DOI] [PubMed] [Google Scholar]
- 11.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of non-randomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 12.Shin DA, Yi S, Yoon DH, et al. Artificial disc replacement combined with fusion versus two-level fusion in cervical two-level disc disease. Spine. 2009;34(11):1153–59. doi: 10.1097/BRS.0b013e31819c9d39. [DOI] [PubMed] [Google Scholar]
- 13.Kang LQ, Lin DS, Ding ZQ, et al. Artificial disk replacement combined with midlevel ACDF versus multilevel fusion for cervical disk disease involving 3 levels. Orthopedics. 2013;36(1):E88–94. doi: 10.3928/01477447-20121217-24. [DOI] [PubMed] [Google Scholar]
- 14.Liu HY, Xu XN, Wang B, et al. Clinical outcomes of hybrid-surgery to treat the two-level cervical disease. Chin J Surg. 2012;50(3):238–43. [PubMed] [Google Scholar]
- 15.Hey HW, Hong CC, Long AS, Hee HT. Is hybrid surgery of the cervicalspine a good balance between fusion and arthroplasty? Pilot results from a single surgeon series. Eur Spine J. 2013;22(1):116–22. doi: 10.1007/s00586-012-2486-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shen CH, Shen Y, Ding WY, et al. [Contrastive analysis of neck axial symptoms after hubrid surgery or traditionalanterior cervical discectomy and fusion for treatment of two-level cervical disease]. Chinese Journal of Reparative and Reconstructive Surgery. 2013;27(1):58–61. [in Chinese] [PubMed] [Google Scholar]
- 17.Grasso G. Clinical and radiological features of hybrid surgery in multilevel cervical degenerative disc disease. Eur Spine J. 2015 doi: 10.1007/s00586-015-4281-7. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 18.Ji GY, Oh CH, Shin DA, et al. Artificial disk replacement combined with fusion versus 2-level fusion in cervical 2-level disk disease with a 5-year follow-up. J Spinal Disord Tech. 2015 doi: 10.1097/BSD.0000000000000316. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 19.Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958;40-a(3):607–24. [PubMed] [Google Scholar]
- 20.Bose B. Anterior cervical instrumentation enhances fusion rates in multilevel reconstruction in smokers. J Spinal Disord. 2001;14(1):3–9. doi: 10.1097/00002517-200102000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Robertson JT, Papadopoulos SM, Traynelis VC. Assessment of adjacent segment disease in patients treated with cervical fusion or arthroplasty: a prospective 2-year study. J Neurosurg Spine. 2005;3(6):417–23. doi: 10.3171/spi.2005.3.6.0417. [DOI] [PubMed] [Google Scholar]
- 22.Goffin J, Geusens E, Vantomme N, et al. Long-term follow-up after inter-body fusion of the cervical spine. J Spinal Disord Tech. 2004;17(2):79–85. doi: 10.1097/00024720-200404000-00001. [DOI] [PubMed] [Google Scholar]
- 23.Goffin J, van Loon J, Van Calenbergh F, Plets C. Long-term results after anterior cervical fusion and osteosynthetic stabilization for fractures and/or dislocations of the cervical spine. J Spinal Disord. 1995;8(6):500–8. [PubMed] [Google Scholar]
- 24.Eck JC, Humphreys SC, Lim TH, et al. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine. 2002;27(22):2431–34. doi: 10.1097/00007632-200211150-00003. [DOI] [PubMed] [Google Scholar]
- 25.Fuller DA, Kirkpatrick JS, Emery SE, et al. A kinematic study of the cervical spine before and after segmental arthrodesis. Spine. 1998;23(15):1649–56. doi: 10.1097/00007632-199808010-00006. [DOI] [PubMed] [Google Scholar]
- 26.Matsunaga S, Kabayama S, Yamamoto T, et al. Strain on intervertebral discs after anterior cervical decompression and fusion. Spine. 1999;24(7):670–75. doi: 10.1097/00007632-199904010-00011. [DOI] [PubMed] [Google Scholar]
- 27.Schwab JS, Diangelo DJ, Foley KT. Motion compensation associated with single-level cervical fusion: where does the lost motion go? Spine. 2006;31(21):2439–48. doi: 10.1097/01.brs.0000239125.54761.23. [DOI] [PubMed] [Google Scholar]
- 28.Park DH, Ramakrishnan P, Cho TH, et al. Effect of lower two-level anterior cervical fusion on the superior adjacent level. J Neurosurg Spine. 2007;7(3):336–40. doi: 10.3171/SPI-07/09/336. [DOI] [PubMed] [Google Scholar]
- 29.Brodke DS, Zdeblick TA. Modified Smith-Robinson procedure for anterior cervical diskectomy and fusion. Spine (Phila Pa 1976) 1992;17(Suppl 10):S427–30. doi: 10.1097/00007632-199210001-00014. [DOI] [PubMed] [Google Scholar]
- 30.Swank ML, Lowery GL, Bhat AL, McDonough RF. Anterior cervical allograft arthrodesis and instrumentation: Multilevel interbody grafting or strut graft reconstruction. Eur Spine J. 1997;6(2):138–43. doi: 10.1007/BF01358747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Duggal N, Pickett GE, Mitsis DK, Keller JL. Early clinical and biomechanical results following cervical arthroplasty. Neurosurg Focus. 2004;17(3):E9. doi: 10.3171/foc.2004.17.3.9. [DOI] [PubMed] [Google Scholar]
- 32.Emery SE, Bohlman HH, Bolesta MJ, Jones PK. Anterior cervical decompression and arthrodesis for the treatment of cervical spondylotic myelopathy. Two to seventeen-year follow-up. J Bone Joint Surg Am. 1998;80(7):941–51. doi: 10.2106/00004623-199807000-00002. [DOI] [PubMed] [Google Scholar]
- 33.Liu F, Cheng J, Komistek RD, et al. In vivo evaluation of dynamic characteristics of the normal, fused, and disc replacement cervical spines. Spine. 2007;32(23):2578–84. doi: 10.1097/BRS.0b013e318158cdf8. [DOI] [PubMed] [Google Scholar]
- 34.Pickett GE, Rouleau JP, Duggal N. Kinematic analysis of the cervical spine following implantation of an artficial cervical disc. Spine. 2005;30(17):1949–54. doi: 10.1097/01.brs.0000176320.82079.ce. [DOI] [PubMed] [Google Scholar]
- 35.Yi S, Kim SH, Shin HC, et al. Cervical arthroplasty in a patient with KlippelFeil syndrome. Acta Neurochir (Wien) 2007;149(8):805–9. doi: 10.1007/s00701-007-1115-7. [DOI] [PubMed] [Google Scholar]
- 36.Yi S, Shin HC, Kim KN, et al. Modified techniques to prevent sagittal imbalance after cervical arthroplasty. Spine. 2007;32(18):1986–91. doi: 10.1097/BRS.0b013e318133fb99. [DOI] [PubMed] [Google Scholar]
- 37.Yoon DH, Yi S, Shin HC, et al. Clinical and radiological results following cervical arthroplasty. Acta Neurochir (Wien) 2006;148(9):943–50. doi: 10.1007/s00701-006-0805-6. [DOI] [PubMed] [Google Scholar]
- 38.Leung CH, Ma WK, Poon WS. Bryan artificial cervical disc arthroplasty in a patient with Klippel-Feil syndrome. Hong Kong Med J. 2007;13(5):399–402. [PubMed] [Google Scholar]
- 39.Auerbach JD, Jones KJ, Fras CI, et al. The prevalence of indications and contraindications to cervical total disc replacement. Spine J. 2008;8(5):711–16. doi: 10.1016/j.spinee.2007.06.018. [DOI] [PubMed] [Google Scholar]
- 40.Barbagallo GM, Assietti R, Corbino L, et al. Early results and review of the literature of a novel hybrid surgical technique combining cervical arthrodesis and disc arthroplasty for treating multilevel degenerative disc disease: opposite or complementary techniques? Eur Spine J. 2009;18(Suppl 1):29–39. doi: 10.1007/s00586-009-0978-9. [DOI] [PMC free article] [PubMed] [Google Scholar]