Abstract
Objective
We sought to establish the prevalence and correlates of disability during the two years preceding hip fracture.
Design
Data from participants who experienced hip fracture in the Health and Retirement Study (HRS) with hip fracture identified by linked Medicare claims. Each participant was interviewed at varying time points in the two years prior to hip fracture. Disability was defined as self-report of the need for assistance in any activity of daily living (walking across the room, eating, bathing, dressing, using the toilet, and transferring). Based on the timing between the interview and the hip fracture, we calculated the prevalence of disability in the cohort as a whole over the two years prior to hip fracture and in subgroups defined by demographic and clinical characteristics.
Setting
The HRS is a nationally representative longitudinal study (1992-2010).
Participants
Adults age > 65.
Results
856 participants experienced hip fracture (mean age at fracture 84, 77% women). The adjusted prevalence of disability was 20% (95% CI 14% to 25%) two years prior to hip fracture, with little change until about 10 months before fracture when it started to rise, reaching 44% (95% CI 33% to 55%) in the month prior to hip fracture. The prevalence of disability was highest in the last month prior to fracture for persons age 85 and older (53%) and for those with dementia (60%).
Conclusion
Care models for hip fracture need to consider not only the acute medical and surgical needs, but also the very high level of need for supportive care and caregiver assistance required among chronically disabled patients.
Keywords: Hip fracture, Disability, Epidemiology
INTRODUCTION
In the US, 258,000 people over age 65 were admitted to the hospital for hip fracture in 2010 1. Worldwide, the annual incidence of hip fractures is estimated to reach 2.6 million in the year 2025 and 4.5 million in the year 2050.2 Approximately half of persons experiencing hip fracture will experience a new permanent disability.3-5 One quarter of women and one third of men experiencing hip fracture will die in the following year6 The estimated lifetime attributable cost for hip fracture is $81,300, or an estimated lifetime cost of $20 billion for all hip fractures in the US in a single year.7
Hip fracture is generally perceived to be an acute, catastrophic, sentinel event, and care protocols are often focused on the acute management needs and predicated on a desire to prevent disability and the many other adverse outcomes associated with hip fracture.8 But hip fracture patients are often of highly advanced age, are frail, and may have high care needs even before their hip fracture. The advanced age and frailty of persons who have hip fracture makes it plausible that many patients with hip fracture are seriously disabled even before their hip fracture, and that the disability acceleration we see in persons with hip fracture may sometimes start even before the hip fracture. This reframing can provide guidance for post hip fracture care.
We know little about the prevalence of disability in the months prior to hip fracture because most studies of hip fracture enroll patients at the time of hip fracture, and assess disability following the fracture.3,4 It is difficult to examine disability before a hip fracture since one does not know in advance who will have a hip fracture. To better understand the prevalence of disability before hip fracture, we leveraged the Health and Retirement Study (HRS), a population based study that has followed older persons for several decades. We identified HRS participants who had hip fracture, and utilizing the variable time points at which subjects were interviewed before the fracture, estimated rates of disability in the 2 years prior to fracture.
METHODS
Participants
The HRS was designed to examine changes in health and wealth as people age.9 The HRS is an ongoing nationally representative longitudinal study of participants age 50 and older. The study started in 1992 and interviews are scheduled every 2 years; to account for the slightly uneven spacing of interviews across waves, we used data from subjects who had an interview within 2.5 years of the fracture event. New community living participants are recruited every six years so that HRS remains nationally representative of the US population. Most HRS interviews are conducted by phone (80%), but in-person interviews are conducted for persons who are age 80 or older, as well as subjects too ill to be interviewed by phone or without access to a phone. If a participant is not able to complete an interview, the interview is conducted with a proxy respondent, generally the subject's next of kin.
We examined participants age >65 who had a record of hip fracture while enrolled in the HRS. To ascertain hip fracture events, we linked the HRS survey data to Medicare claims. A participant was identified as having hip fracture event if one of the following two conditions was met: (1) the participant was admitted to a hospital with an admitting diagnosis ICD9 code for hip fracture “820.xx”; or (2) a surgeon's charge for operative hip repair (CPT code 27230 – 27248) supported with either (a) a second surgeon's charge within 2 days or (b) a supporting ICD9 procedure code for hip fracture surgery [3] (ICD9 7855, 7905, 7915, 7925).10-13 We excluded admissions which were considered late effects from a prior hip fracture, identified by ICD9 codes 733.81, 733.82, 905.3, V540-V549.10,14,15
Out of 25,146 HRS participants age 65 or older at any point between 1992 and 2010, 19,006 (76%) agreed to have their HRS surveys linked to the Medicare claims. We identified 1,124 hip fracture events among those participants. Since we used Medicare claims to identify the presence of comorbid conditions prior to the hip fracture event, we excluded hip fracture events that were not preceded with one continuous year of Medicare fee-for-service enrollment. Of the remaining 1,017 hip fracture events, 161 (16%) had no HRS interview within 2.5 years before the hip fracture event and were therefore excluded. Five hip fracture events were repeat events and were removed from our sample, resulting in the final sample of 857 participants with hip fracture.
Measures
The outcome of interest was disability in the two years before hip fracture. Because these individuals were evaluated only every two years, we were unable to track the individual trajectories of patients with hip fracture. We therefore evaluated the prevalence of disability in groups of patients interviewed at various times prior to the hip fracture event. Functional disability was determined by the need for assistance in six Activities of Daily Living (ADLs), which included walking across the room, eating, bathing, dressing, using the toilet, and transferring to/from bed. Subjects who reported requiring assistance with any ADL were defined as disabled. In addition to disability, we examined four measures of higher order functional impairment: difficulty with walking several blocks, climbing one flight of stairs, managing finances, or taking medications.
To characterize the study population, we used the HRS interviews to describe self-reported age, gender, race or ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, and other), education, wealth, a report of falls in the previous interview, nursing home residence, reported number of helpers, average number of days per month a helper provided assistance, and average number of hours in a day the helper provides assistance. We determined a history of dementia and a Charlson comorbidity score for each participant using Medicare claims.16 Mortality after hip fracture was determined using a linkage to the National Death Index.
Statistical Analysis
The relationship between the prevalence of disability might take many forms. For example, the prevalence might increase or decrease linearly over time (i.e. a linear relationship). Or the prevalence might increasingly increase over time (i.e. a quadratic relationship). Or, as we found, the prevalence might stay flat until some time period, then increase sharply over the last several months prior to hip fracture (i.e. a spline relationship). Spline models allow for linear segments that transition in slope around specific time points, called knots (e.g. a flat slope to an increasing slope). In this case, the spline model allowed us to account for the possibility that the degree of change in function was not steady over time, but could accelerate at certain time points.
We avoided making assumptions about the relationship between the prevalence of disability over the two years prior to hip fracture (e.g. assuming a linear relationship when the relationship is not linear). Instead, we modeled several functional forms of the relationship (linear, quadratic, and spline models) to determine which model was the best fit for the data. We examined splines with 1, 2, or 3 knots placed at varying time points prior to the occurrence of hip fracture. The formal tests for model fit we examined were the Akiake and Baysian Information Criterion for each model (AIC and BIC, respectively). The AIC and BIC measure the fit of the model, with a penalty for greater complexity of the model in order to penalize over-fitting of the data. Over-fitting is creating a model that fits the data at hand nearly perfectly, but is unlikely to generalize to a different dataset. The AIC and BIC suggested that the spline model with a single knot at 10 months prior to hip fracture was the best fit.
We then used the spline mode with a knot at 10 months prior to hip fracture to estimate a multivariate model adjusting for age and gender. To provide a comparison for the background prevalence of disability, we provide the prevalence of disability for age and gender matched participants who did not experience hip fracture.
Next we examined differences in the prevalence of disability among subgroups of interest. We calculated predicted probabilities of functional disability by level of each independent variable using the final multivariable model and fixing all other variables at population means. Predicted probabilities were calculated at 3 different time points (two years before hip fracture, 10 months prior to hip fracture, and the month before hip fracture).
All analyses were weighted to account for the differential probability of subject selection and complex design of the HRS. Statistical analysis were done using Stata software, version 12 (StataCorp, College Station, Texas) and SAS software, version 9.3 (SAS institute, Cary, North Carolina). The institutional review board at the University of California, San Francisco, approved this study.
RESULTS
Among 856 participants mean age at the pre-hip fracture interview was 82.1 and mean age at the time of the hip fracture was 83.7; 76.9% were women (see Table 1). Twenty percent of respondents were proxies. Twenty-six percent of participants experienced moderate to severe pain, 33% CES-D scores suggested clinical depression, 16% had dementia, and 43% had a Charlson comorbidity score of greater than two, suggesting a high severity of illness or multiple chronic conditions. Fifty-eight percent required assistance more than 14 days out of the month, and 10% resided in nursing homes. One-year mortality was 27% in the year following hip fracture.
Table 1.
Sample Characteristics
| Characteristic | Study Sample (n=856)* | |
|---|---|---|
| Demographic | ||
| Age at interview before fracture, % | ||
| 65-75 | 16.7% | |
| 75-85 | 43.0% | |
| 85-90 | 24.6% | |
| ≥90 | 15.7% | |
| Female, % | 76.9% | |
| Race, % | ||
| White | 91.8% | |
| Black | 3.7% | |
| Hispanic | 3.9% | |
| Other | 0.6% | |
| Socioeconomic | ||
| Less than high school diploma, % | 41.8% | |
| Net worth, median (IQR) | 84K (7K-273K) | |
| Married or partnered | 32.6% | |
| Proxy interview, % | 19.6% | |
| Nursing home resident | 9.5% | |
| Health | ||
| Charlson Comorbidity Score, % | ||
| ≤2 | 56.9% | |
| >2 | 43.1% | |
| Dementia | 16.2% | |
| Disability, % | ||
| Bathing | 20.8% | |
| Transferring bed to chair | 7.6% | |
| Dressing | 14.2% | |
| Eating | 6.7% | |
| Toileting | 5.3% | |
| Walking across room | 8.7% | |
| Difficulty managing finances, % | 35.7% | |
| Difficulty taking medications, % | 18.5% | |
| Difficulty walking several blocks, % | 63.5% | |
| Difficulty climbing one flight of stairs, % | 47.3% | |
| Fall in the past year, % | 48.2% | |
| Moderate or severe pain, % | 26.3% | |
| Depression (CES-D > 3) | 33.0% | |
| Caregiver support | ||
| Number of helpers | ||
| 0 | 58.9% | |
| 1 | 20.7% | |
| 2+ | 20.5% | |
| Average number of days in a month helper provided assistance | ||
| ≤7 | 26.9% | |
| 7-14 | 15.3% | |
| >14 | 57.8% | |
| Average number of hours in a day helper provided assistance | ||
| ≤2 | 51.2% | |
| 2-8 | 36.1% | |
| >8 | 12.8% | |
Reported values incorporate survey weights to account for the complex survey design
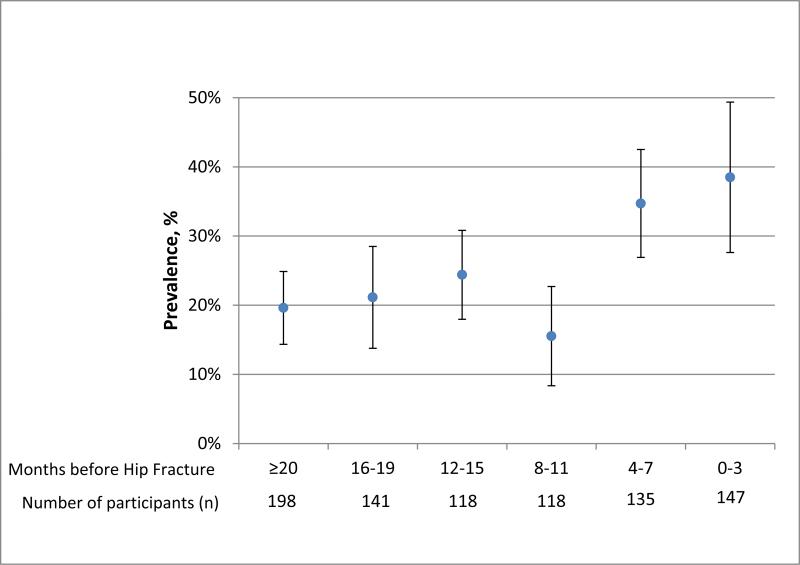
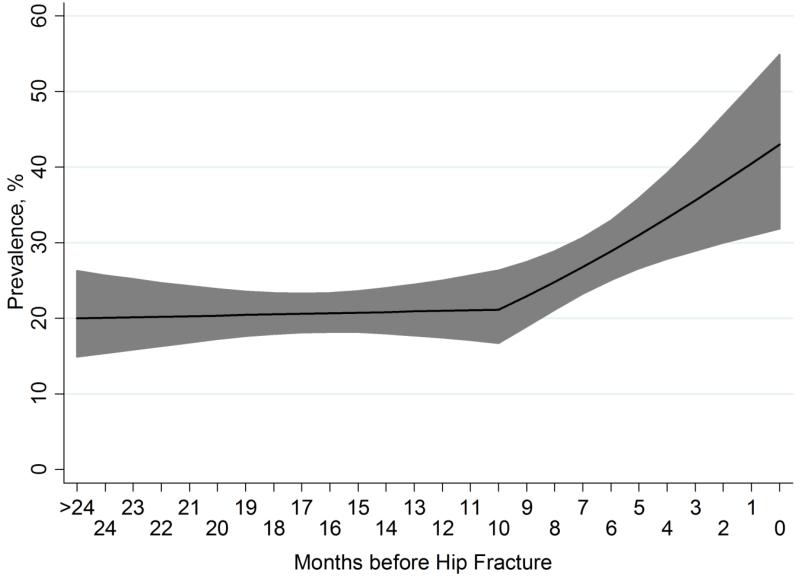
The raw prevalence of disability prior to hip fracture is depicted in Figure 1. For the remainder of the results, we refer to the best-fit spline model with a knot at 10 months prior to hip fracture (Figure 2). In the modeled results, the prevalence of disability was flat at 20% (95% CI 15 to 25) two years prior to hip fracture up until 10 months prior to hip fracture (20%, 95% CI 15 to 25) (slope differs from zero, p=0.55) (see Figure 1, Table 2). During the last 10 months prior to hip fracture, the prevalence increased an average of 2.4% per month, reaching 44% (95% CI 33% to 55%) in the month prior to hip fracture (slope differs from zero, p=.002). The increase in disability at 10 months prior to hip fracture was present for all ADL (all p<.05 for change in slope), though greatest for disability in walking, bathing, and dressing (see Online Appendix Figure 1). In comparison, the prevalence of disability in a sample of participants matched by age and gender who did not experience hip fracture (n=851) was 15% (95% CI 13% to 17%), which was less than the 26% (95% C: 22% to 29%) prevalence in the participants interviewed at any point within two years of hip fracture (p<.001).
Figure 1. Raw Prevalence of Disability During the Two Years Prior to Hip Fracture.
Participants with hip fracture were interviewed once approximately every two years. Therefore, these subjects were interviewed once within the two years preceding hip fracture. We used these reports to determine the prevalence of disability at varying time points prior to hip fracture. Depicted are the point prevalence of disability (solid circle) in 4 month intervals with 95% CI's (hash marks). The number of participants interviewed at each time interval prior to hip fracture is noted on the x-axis.
Figure 2. Modeled Prevalence of Any Disability in Activities of Daily Living During the Two Years Prior to Hip Fracture.
Predicted prevalence of disability modeled as a spline with a single knot at 10 months prior to the occurrence of hip fracture. Solid line represents the average prevalence; shaded areas indicate the 95% confidence boundary. The P value for the increase in disability prevalence during the months before the knot was 0.55, and the P value for the increase in disability prevalence during the 10 months between the knot and the occurrence of hip fracture was 0.002.
Table 2.
Prevalence of Disability at 3 Time Points Before Hip Fracture for Various Subgroups
| Prevalence of ADL disability | ||||
|---|---|---|---|---|
| 2 yr | 10 mo | 1 mo | p-value | |
| Total Population | 20 (15-25) | 20 (15-25) | 44 (33-55) | |
| Age | ||||
| <85 | 15 (10-20) | 15 (10-20) | 36 (24-47) | 0.001 |
| ≥85 | 26 (19-33) | 27 (20-33) | 53 (41-66) | |
| Gender | ||||
| Men | 19 (13-26) | 20 (12-28) | 43 (30-56) | 0.863 |
| Women | 20 (14-26) | 20 (15-26) | 44 (32-56) | |
| Race or ethnicity | ||||
| White | 19 (13-24) | 20 (15-25) | 43 (32-55) | - |
| Black | 24 (13-34) | 25 (13-38) | 51 (34-68) | 0.273 |
| Latino | 26 (13-39) | 27 (14-41) | 54 (36-72) | 0.177 |
| Charlson comorbidity score | ||||
| ≤2 | 18 (13-24) | 19 (13-25) | 42 (30-53) | 0.297 |
| >2 | 22 (15-28) | 22 (16-28) | 47 (33-60) | |
| Falls reported in interview before fracture | ||||
| No | 14 (9-18) | 13 (9-18) | 31 (22-40) | <0.001 |
| Yes | 28 (21-35) | 27 (20-34) | 52 (40-65) | |
| Education less than high school diploma | ||||
| No | 15 (9-21) | 17 (11-22) | 37 (25-48) | 0.004 |
| Yes | 25 (18-31) | 27 (20-34) | 52 (39-65) | |
| Wealth less than median | ||||
| No | 14 (10-18) | 15 (10-20) | 35 (23-46) | <0.001 |
| Yes | 25 (17-32) | 26 (20-33) | 52 (40-64) | |
| Nursing home resident | ||||
| No | 17 (12-22) | 17 (12-21) | 34 (22-45) | <0.001 |
| Yes | 69 (59-80) | 68 (56-81) | 85 (78-92) | |
| Dementia | ||||
| No | 17 (12-22) | 18 (13-23) | 40 (29-52) | <0.001 |
| Yes | 31 (23-40) | 33 (23-43) | 60 (45-75) | |
*Predicted prevalence values are the predicted probabilities from the spline model with a single interior knot at 10 months prior to hip fracture, adjusted for age and gender. p-values represent the differences between groups of patients across time points (e.g. men vs. women).
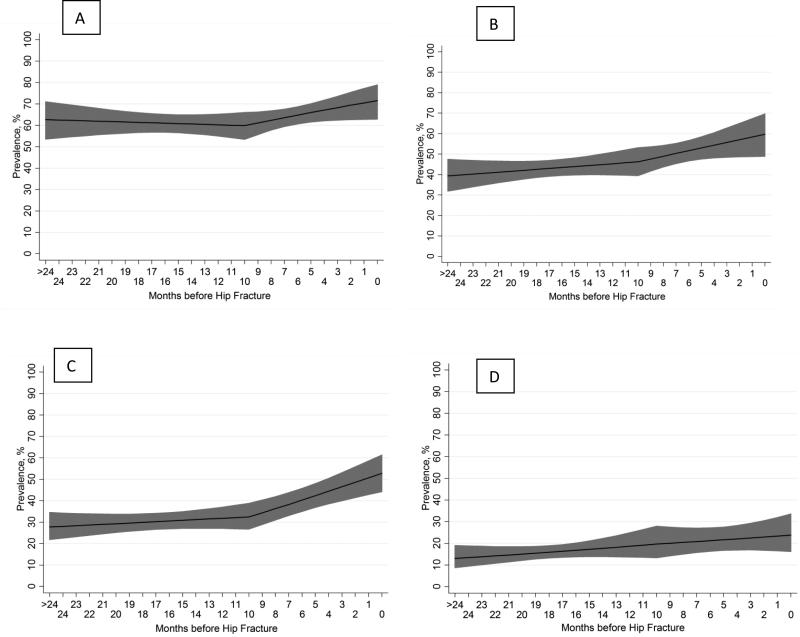
The prevalence of difficulty walking several blocks and climbing stairs was high even two years prior to hip fracture (Figure 3). Sixty three percent (95% CI 55% to 71%) of subjects had difficulty walking several blocks two years prior to hip fracture, and 40% (95% CI 33%-48%) had difficulty climbing one flight of stairs, rising to 72% (95% CI 65%-80%) and 61% (95% CI 51%-71%) during the last month prior to fracture, respectively. The prevalence of difficulty managing finances rose from 27% (95% CI 21%-33%) two years prior to hip fracture to 55% (95% CI 46%-63%) during the last month prior to hip fracture, and the prevalence of difficulty managing medications rose from 13% (9%-18%) two years prior to hip fracture to 24% (95% CI 15%-32%) during the last month prior to hip fracture (Figure 2).
Figure 3. Modeled Prevalence of Difficulty Ambulating, Climbing Stairs, Managing Finances, and Taking Medications During the Two Years Prior to Hip Fracture.
Predicted prevalence of functional difficulties modeled as a spline with a single knot at 10 months prior to the occurrence of hip fracture. Panel A: Difficulty walking several blocks. Panel B: Difficulty climbing one flight of stairs. Panel C: Difficulty managing finances. Panel D: Difficulty taking medications.
Disability in Subgroups
After adjustment for age and gender, disability rates prior to fracture were considerably higher for those over the age of 85, a history of falls, less than high school education, wealth less than the median, residing in nursing homes, and a history of dementia (Table 2). The prevalence of disability by age was 11% points higher for those 85 and older than patients 65 to 84 two years prior to hip fracture. This difference widened during the last 10 months, reaching a difference of 17% points in the month prior to hip fracture. Sixty percent of participants with dementia (95% CI, 45-75%) and 85% of participants residing in nursing homes (95% CI, 78-92%) experienced disability in the month prior to hip fracture.
DISCUSSION
In a nationally representative cohort of older adults, we examined the prevalence of disability in cohorts of patients who experienced hip fracture over the following two years. We found the prevalence of disability was essential flat at 20% until almost a year prior to the hip fracture event. Beginning around ten months prior to hip fracture, the prevalence of disability increased, topping forty percent in the last month prior to hip fracture. A majority of the very elderly, participants with dementia, and nursing home residents were already disabled pre-fracture. Mobility is central to quality of life for older adults, and one of the major goals of acute hip fracture management is to restore mobility.17,18 Yet about half of older adults had difficulty walking several blocks or climbing stairs two years prior to the occurrence of hip fracture.
The surgical, “There is a fracture, I need to fix it” mentality has been caricatured with over a million views on YouTube.19 This video has traction because, as evidence suggests,20 there is an element of truth to the notion that the clinical and functional circumstances of the patient matter little to a subset of surgeons narrowly focused on “fixing” the broken bone. However, models of care focused on acute surgical management and restoration of independence may not be sufficient for older persons, many of whom are dependent on others for basic ADL even before the fracture, and have large needs for supportive care which will only accelerate after the fracture. Clinicians who see patients with hip fracture need to consider the bigger picture. We observed that for four out of ten older adults, hip fracture is an event that occurs in a patient that has already experienced disability. Over a quarter of subjects in our study experienced clinically significant pain or depression. Nearly 60% required assistance more than 14 days out of the month. Sixteen percent had dementia. Ten percent lived in a nursing home. Over one quarter of participants died during the year following hip fracture.
These data suggest that an aggressive surgical/palliative approach that addresses symptom burden while attending to treatment burden and mitigation of disability may be optimal for many patients experiencing hip fracture. Because palliative care grew first out of the hospice movement and for patients with cancer, older conceptions of palliative care were tied closely with end-of-life care and a short-term prognosis. In the new conception, palliative care is appropriate throughout the course of serious illness, should ideally be introduced early, and delivered concurrently with all other medical treatments, including surgical and restorative care. Hip fracture fits well with the new conception of palliative care. Goals of care conversations will be critical for those with acute on chronic disability, or dementia. Assessment and treatment of pre-existing pain from chronic conditions is essential in addition to the pain caused by the fracture and its related surgery,21 The need for assistance with caregiving will accelerate after the hip fracture, requiring extensive planning and support for caregivers. Further, while surgery for hip fracture is almost always indicated, in rare cases it is not.8,22 It is reasonable to consider a non-operative approach for patients who are severely disabled, are immobile at baseline, have a high operative risk, and/or have a non-displaced femoral neck fracture that is conducive to non-surgical management and responsive to pain medications.
Hip fracture is often viewed as a catastrophic cause of disability, similar to stroke. The bulk of clinical efforts are on returning the patient to independent function. This is clearly the correct focus for a large number of patients, particularly those who were independent before the hip fracture. However, our results strongly suggest that a large number of patients were on a clinical trajectory of functional decline before their hip fracture. In these patients, the hip fracture may be as much a manifestation of the disablement process as the cause of the disablement process. From a clinical perspective, it is important to carefully consider the functional and health trajectory of patients before the hip fracture. Others have demonstrated that disability can be relapsing and remitting.23 Identifying persons with a likely reversible disability is crucial. For these persons there is still often a place for a focus on traditional rehabilitation. However, it is also important for clinicians to recognize that in patients who were developing disability before the hip fracture, it is likely that both the disability trajectory, and the resulting palliative and supportive needs will markedly increase after the hip fracture. For this reason, in patients who were disabled before the hip fracture, care plans need to consider both rehabilitative and palliative needs.
The disparities in disability during the two years prior to hip fracture by socioeconomic position are concerning. We observed that patients who had less than a high school education or were poor were more likely to experience disability during the two years prior to hip fracture. While the reasons for these disparities are not clear from our data, they indicate that social vulnerability, function, and fracture risk interact in complex ways that belie a simple biomedical conception of illness.24,25 Whatever the underlying mechanism, the clinical reality is there is a substantial group of patients who have limited financial resources, who were doing much worse functionally before the occurrence of hip fracture, and have now experienced a condition leading to further deterioration. Other than the acute and brief post-acute period following fracture repair, the longer term needs for assistance of these patients are not funded by Medicare.
Our findings must be understood within the limitations of our study design. Because Medicare claims are not captured for patients with Medicare Managed Care, our findings may not generalize to the approximately 15% of patients with Medicare Managed Care during this time period. Twenty percent of interviews were conducted with proxy respondents. However, in contrast to subjective health states such as depression, proxy reports of disability are highly concordant with participant responses.26 We were unable to track the individual trajectories of patients with hip fracture, instead presenting the prevalence of disability in groups of patients interviewed at varying times prior to the hip fracture event. Other research suggests that individuals often transition between independence and disability over short time periods, such as months.23 Despite these individual fluctuations, however, on a population level our work suggests an overall increase in disability prevalence in the final months prior to hip fracture. Furthermore, a study of trajectories of individual patients who will experience hip fracture during the next two years would be prohibitively expensive as huge numbers of patients would need to be followed regularly in order to capture the small proportion who experience hip fracture.
In conclusion, disability during the two years prior to hip fracture is common, occuring in over 40% of patients during the months immediately preceding the fracture event, and 20% two years prior to fracture. Clinicians should consider functional histories as they consider how to manage patients with hip fracture. A combined surgical/rehabilitative and palliative approach may be optimal for some patients.
Supplementary Material
ACKNOWLEDGMENT
Funding Source: This project was funded by the National Institute for Nursing Research (R01NR013347). Dr. Smith was funded by a K23 Beeson award from the National Institute on Aging (1K23AG040772) and the American Federation for Aging Research.
Sponsor's Role: The NIA and American Federation for Aging Research had no role in the design, methods, subject recruitment, data collections, analysis and preparation of paper.
Footnotes
Author Contributions: Study concept and design: All authors
Acquisition of subjects and/or data: Smith, Cenzer, Boscardin, Covinsky
Analysis and interpretation of data: All authors
Preparation of manuscript: All authors
References
- 1. [March 28, 2014];Hospital discharges by first- and any-listed diagnosis: US, 1990-2010 (Source: NHDS) 2010 http://205.207.175.93/HDI/TableViewer/tableView.aspx. 2014.
- 2.Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 1997;7(5):407–413. doi: 10.1007/pl00004148. [DOI] [PubMed] [Google Scholar]
- 3.Magaziner J, Hawkes W, Hebel JR, et al. Recovery from hip fracture in eight areas of function. The journals of gerontology. Series A, Biological sciences and medical sciences. 2000 Sep;55(9):M498–507. doi: 10.1093/gerona/55.9.m498. [DOI] [PubMed] [Google Scholar]
- 4.Magaziner J, Simonsick EM, Kashner TM, Hebel JR, Kenzora JE. Predictors of functional recovery one year following hospital discharge for hip fracture: a prospective study. Journal of gerontology. 1990 May;45(3):M101–107. doi: 10.1093/geronj/45.3.m101. [DOI] [PubMed] [Google Scholar]
- 5.Magaziner J, Fredman L, Hawkes W, et al. Changes in functional status attributable to hip fracture: a comparison of hip fracture patients to community-dwelling aged. American journal of epidemiology. 2003 Jun 1;157(11):1023–1031. doi: 10.1093/aje/kwg081. [DOI] [PubMed] [Google Scholar]
- 6.Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB. Incidence and mortality of hip fractures in the United States. JAMA : the journal of the American Medical Association. 2009 Oct 14;302(14):1573–1579. doi: 10.1001/jama.2009.1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Braithwaite RS, Col NF, Wong JB. Estimating hip fracture morbidity, mortality and costs. Journal of the American Geriatrics Society. 2003 Mar;51(3):364–370. doi: 10.1046/j.1532-5415.2003.51110.x. [DOI] [PubMed] [Google Scholar]
- 8.Parker M, Johansen A. Hip fracture. Bmj. 2006 Jul 1;333(7557):27–30. doi: 10.1136/bmj.333.7557.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. [3/17/2014];The Health and Retirement Study. 2014 http://hrsonline.isr.umich.edu/. 2014.
- 10.Fisher ES, Baron JA, Malenka DJ, et al. Hip fracture incidence and mortality in New England. Epidemiology. 1991 Mar;2(2):116–122. doi: 10.1097/00001648-199103000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Karagas MR, Baron JA, Barrett JA, Jacobsen SJ. Patterns of fracture among the United States elderly: geographic and fluoride effects. Annals of epidemiology. 1996 May;6(3):209–216. doi: 10.1016/1047-2797(96)00006-3. [DOI] [PubMed] [Google Scholar]
- 12.Karagas MR, Lu-Yao GL, Barrett JA, Beach ML, Baron JA. Heterogeneity of hip fracture: age, race, sex, and geographic patterns of femoral neck and trochanteric fractures among the US elderly. American journal of epidemiology. 1996 Apr 1;143(7):677–682. doi: 10.1093/oxfordjournals.aje.a008800. [DOI] [PubMed] [Google Scholar]
- 13.Rigler SK, Ellerbeck E, Whittle J, Mahnken J, Cook-Wiens G, Shireman TI. Comparing methods to identify hip fracture in a nursing home population using Medicare claims. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2011 Jan;22(1):57–61. doi: 10.1007/s00198-010-1264-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jacobsen SJ, Goldberg J, Miles TP, Brody JA, Stiers W, Rimm AA. Seasonal variation in the incidence of hip fracture among white persons aged 65 years and older in the United States, 1984-1987. American journal of epidemiology. 1991 May 15;133(10):996–1004. doi: 10.1093/oxfordjournals.aje.a115819. [DOI] [PubMed] [Google Scholar]
- 15.Lauderdale DS, Jacobsen SJ, Furner SE, Levy PS, Brody JA, Goldberg J. Hip fracture incidence among elderly Asian-American populations. American journal of epidemiology. 1997 Sep 15;146(6):502–509. doi: 10.1093/oxfordjournals.aje.a009304. [DOI] [PubMed] [Google Scholar]
- 16.Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. Journal of clinical epidemiology. 1994 Nov;47(11):1245–1251. doi: 10.1016/0895-4356(94)90129-5. [DOI] [PubMed] [Google Scholar]
- 17.Yeom HA, Fleury J, Keller C. Risk factors for mobility limitation in community-dwelling older adults: a social ecological perspective. Geriatric nursing. 2008 Mar-Apr;29(2):133–140. doi: 10.1016/j.gerinurse.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 18.Webber SC, Porter MM, Menec VH. Mobility in older adults: a comprehensive framework. The Gerontologist. 2010 Aug;50(4):443–450. doi: 10.1093/geront/gnq013. [DOI] [PubMed] [Google Scholar]
- 19.tazobactar. [June 20, 2014];orthopedia vs anesthesia. 2010 http://youtu.be/3rTsvb2ef5k.
- 20.Kruser JM, Cecanac KE, Brasel KJ, et al. “And I Think That We Can Fix It”: Mental Models Used in High-Risk Surgical Decision Making. Annals of Surgery. 2014 doi: 10.1097/SLA.0000000000000714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smith AK, Cenzer IS, Knight SJ, et al. The epidemiology of pain during the last 2 years of life. Annals of internal medicine. 2010 Nov 2;153(9):563–569. doi: 10.1059/0003-4819-153-9-201011020-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smith AK, Lo B, Sudore R. When previously expressed wishes conflict with best interests. JAMA internal medicine. 2013 Jul 8;173(13):1241–1245. doi: 10.1001/jamainternmed.2013.6053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hardy SE, Dubin JA, Holford TR, Gill TM. Transitions between states of disability and independence among older persons. American journal of epidemiology. 2005 Mar 15;161(6):575–584. doi: 10.1093/aje/kwi083. [DOI] [PubMed] [Google Scholar]
- 24.Shaw BA, McGeever K, Vasquez E, Agahi N, Fors S. Socioeconomic inequalities in health after age 50: are health risk behaviors to blame? Social science & medicine. 2014 Jan;101:52–60. doi: 10.1016/j.socscimed.2013.10.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stringhini S, Sabia S, Shipley M, et al. Association of socioeconomic position with health behaviors and mortality. JAMA : the journal of the American Medical Association. 2010 Mar 24;303(12):1159–1166. doi: 10.1001/jama.2010.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gill TM, Hardy SE, Williams CS. Underestimation of disability in community-living older persons. J Am Geriatr Soc. 2002 Sep;50(9):1492–1497. doi: 10.1046/j.1532-5415.2002.50403.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.