Abstract
Objective
To compare the effects of Tai Chi (TC, n = 37) and Western exercise (WE, n = 39) with an attention-control group (C, n = 56) on physical and cognitive functioning in healthy adults age 69 ± 5.8 yr, in a 2-phase randomized trial.
Methods
TC and WE involved combined class and home-based protocols. Physical functioning included balance, strength, flexibility, and cardiorespiratory endurance. Cognitive functioning included semantic fluency and digit-span tests. Data were analyzed using intention-to-treat analysis.
Results
At 6 mo, WE had greater improvements in upper body flexibility (F = 4.67, p = .01) than TC and C. TC had greater improvements in balance (F = 3.36, p = .04) and a cognitive-function measure (F = 7.75, p < .001) than WE and C. The differential cognitive-function improvements observed in TC were maintained through 12 mo.
Conclusion
The TC and WE interventions resulted in differential improvements in physical functioning among generally healthy older adults. TC led to improvement in an indicator of cognitive functioning that was maintained through 12 mo.
Keywords: mind–body therapy, physical activity, executive function, aged adult
Healthy aging is an important public health issue, given the increasing number of older adults worldwide. They account for the greatest proportion of chronic-disease burden, which often contributes to impaired physical and cognitive functioning, loss of independent living, and increased disability (“Trends in Aging,” 2003). Conversely, regular physical activity is a critical element of an overall healthy lifestyle that can extend years of independent living, reduce disability, and improve physical and cognitive functioning among older adults (Colcombe & Kramer, 2003; Hogan, 2005; King et al., 2000; Mazzeo et al., 1998). Physical activity recommendations for older adults include moderate-intensity aerobics and muscle-strengthening and flexibility activities, along with balance exercises, to improve and maintain health (Nelson et al., 2007). Despite the widely reported benefits of regular physical activity (Colcombe & Kramer, 2003; Netz, Wu, Becker, & Tenenbaum, 2005; Whelton, Chin, Xin, & He, 2002), most older adults do not achieve recommended levels (Centers for Disease Control and Prevention, 2004, 2005). The challenge and opportunity are to make physical activity long lasting and more attractive to older adults of all ages, interests, and abilities (King, 2001).
Among older adults, research examining Western forms of exercise (WE) such as walking or calisthenics has reported improvements in cardiorespiratory endurance, muscle strength, flexibility, balance, and cognitive functioning (American College of Sports Medicine [ACSM], 2004; Colcombe & Kramer, 2003; Mazzeo et al., 1998; Nelson et al., 2007). Prior studies indicate that a 6-month moderate-intensity aerobic-exercise program is adequate for significant improvements in cognitive function, with the greatest benefit occurring in executive-control processes (Colcombe & Kramer, 2003). Improvements in cardiovascular-disease biomarkers, such as blood pressure, atherogenic lipid profiles, and heart-rate variability, resulting from participation in regular physical activity are thought to contribute to improvements in cognitive function (Physical Activity Guidelines Advisory Committee, 2008).
Tai Chi is an Eastern form of exercise that appeals to a growing number of older adults, with somewhat similar improvements in physical functioning reported when compared with WE (Hartman et al., 2000; Lan, Lai, Chen, & Wong, 1998, 2000; Wolf et al., 1996; Wong, Lin, Chou, Tang, & Wong, 2001). Tai Chi is a gentle, low-impact exercise that has been practiced in China for hundreds of years (Galante, 1981; Taylor-Piliae, 2003). “The Compendium of Physical Activities” (Ainsworth et al., 2000) classifies Tai Chi as a moderate-intensity exercise, at 4 metabolic equivalents similar in intensity to brisk walking. In addition, Tai Chi may provide benefits beyond traditional forms of WE (Galante, 1981; Lan, Lai, & Chen, 2002). During the performance of Tai Chi exercise, individuals are taught to be mindful of what their bodies are doing and how it feels. The goal is for the whole body to remain relaxed while practicing TC, integrating mental concentration and breathing control (Galante, 1981).
Most research on Tai Chi among older adults has focused on balance, flexibility, postural control, muscle strength, and fall-risk reduction, although various styles of Tai Chi were used in these studies (Hartman et al., 2000; Lan et al., 1998, 2000; Wolf et al., 1996; Wong et al., 2001) that can represent different exercise intensities and durations, making comparisons difficult. Anecdotal evidence suggests that Tai Chi may also improve cognitive function, but experimental evidence in this area is not well documented (Galante, 1981; Lan et al., 2002). Given this, the major objective of the Wellness Interventions for Self Enrichment (WISE) study was to evaluate the effects of Tai Chi versus a standard program of WE consisting of cardiorespiratory-endurance, strength, and flexibility training on physical and cognitive functioning in healthy, community-dwelling adults age 60 years and older.
Methods
Study Design
The WISE study was a randomized clinical trial with two phases: The first 6 months were designated as an adoption phase during which Tai Chi, WE, and attention-control groups were compared. During the second 6 months, designated as the maintenance phase, the two exercise groups (Tai Chi and WE) continued to be compared. Once volunteers completed the baseline evaluation and were deemed eligible for the study, they were randomized to one of the three groups. Because the programs were taught in classes, participants were entered in cohorts of 20–30 so that 8–10 participants could start a class together to help facilitate instruction. Over the course of the study, five cohorts were enrolled between April 2000 and September 2001. Major follow-up evaluations were completed at 6 and 12 months, with a limited evaluation performed at 3 months. Data were collected through October 2002. The WISE protocol was approved by the Panel on Human Subjects in Medical Research at Stanford University.
Study Sample
Men and women living at home or in a community residential setting in either Santa Clara County or San Mateo County in northern California were eligible to participate in WISE. Inclusion criteria were being age 60 years or older, living within a reasonable commute to Stanford University and the community exercise facilities, understanding the English language sufficiently to give study consent and follow intervention instructions, signed written consent, being sedentary (no regular exercise >60 min/week), and being able to walk without assistive devices. Exclusion criteria included major medical diagnoses that would interfere with participation in moderate-intensity exercise, for example, myocardial infarction, cardiac surgery, or stroke in past 3 months; congestive heart failure, angina pectoris, serious cardiac arrhythmias, or blood pressure >160/100 mm Hg; or active treatment for cancer, alcoholism, recreational drug abuse, or severe cognitive impairment (ACSM, 2005; King et al., 2005).
Participant Recruitment and Randomization
The recruitment plan included newspaper and radio advertisements, flyers, and brochures placed in senior centers, retirement residences and clubs, pharmacies, and primary-care offices. Presentations about the project were made to members of senior centers and senior residences. Interested individuals completed a telephone interview and, if still interested and apparently eligible, were invited to a group or individual orientation session. At the orientation session the study was described in detail, the requirements for participation were explained, and study-related questions were answered. Participants still interested and eligible were scheduled for baseline evaluations. After screening for eligibility and baseline measurements, participants were randomly assigned to Tai Chi, WE, or control. A decision was made to randomize participants in a disproportionate manner, with approximately 30% assigned to each of the two exercise groups and 40% to control. The larger number of participants randomized to control at baseline provided more participants for rerandomization after the adoption phase (first 6 months) of this study to interventions in a subsequent supplemental study. Data from the supplemental study are not reported in this article.
Interventions
After randomization, initial individual counseling sessions were provided to participants by their respective class instructor, including program schedule, safety issues, and intervention procedures. The two exercise interventions involved a combined class- and home-based protocol to maximize long-term participation (King et al., 2000). A social-cognitive approach to the acquisition and maintenance of physical activity was employed that included personalized feedback, specific structuring of expectations, consciousness raising regarding the benefits of physical activity, realistic and individualized goal setting, encouragement from staff, reinforcement of successful change, and monitoring of adherence (Bandura, 1997; King, 2001; King et al., 2000). Classes lasted approximately 60 min and were no more than moderate in intensity. During the adoption phase, participants in the exercise groups were assigned two class-based and three home-based exercise sessions per week, and the attention-control group met once a week for approximately 90 min. During the maintenance phase, participants in the exercise groups were instructed to engage in one class-based and three home-based exercise sessions per week.
Tai Chi
The Tai Chi classes were held in the community room of a local church that provided privacy and a relaxing atmosphere. All Tai Chi classes were taught by a Tai Chi grand master. Participants were taught 12 postures of the Yang short-form style of Tai Chi (Lee, Lee, & Johnstone, 1989). A new posture was taught each week during the first 12 weeks, with the entire sequence of postures practiced together during the remainder of the adoption phase. During the maintenance phase 12 additional postures were taught, with participants learning a total of 24 postures during the study (Lee, Lee, Lee, & Lee, 2002). The postures were practiced with continuous movement from one to the next, in a slow and rhythmic motion. Each class consisted of 45 min of instruction including warm-up exercises, with chairs available for participants to rest as needed. Participants were provided with written instructions, illustrations of the postures, and a videotape (Lee & Lee, 1989) for use during practice on home-based exercise days. In addition to the Tai Chi postures, they were taught essential elements of performing Tai Chi, such as body orientation, relaxation, breathing, attention to feeling, inattention to thoughts, upright and relaxed posture, symmetry, weight shifting, and a slow and relaxed pace. Daily practice was encouraged.
Western Exercise
The WE program incorporated endurance, resistance/strength, and flexibility exercises. Participants attended supervised classes held at a YMCA exercise facility and led by certified exercise leaders. Each class started with 8–10 min of warm-up activities consisting of stretching, light calisthenics, and slow walking. This was followed by cardiorespiratory-endurance activities lasting for 15–25 min consisting of more vigorous walking and calisthenics performed to music and then a session of both resistance/strength and flexibility exercises lasting 15–20 min. The resistance exercises included selected calisthenics and the use of light hand weights and rubber exercise bands. Home-based exercise sessions included ≥30 min of walking and 10–25 min of resistance and flexibility exercises three times per week. The intensity of the exercise was gradually increased over time using heart-rate monitoring and ratings of perceived exertion. A 1-year YMCA senior membership was provided to all the WE participants.
Control Group
Throughout the 6-month adoption phase, participants in the attention-control group attended “healthy aging” classes to control for time, attention, support, or additional factors that could potentially influence the study outcomes, independent of the exercise interventions. Experienced professionals provided information on a number of topics, for example, healthy eating, elder hostels, forgiveness, elder law, and appropriate foot and eye care. Classes met once a week for approximately 90 min and included visits to markets to learn about reading food labels and selecting produce. Controls were provided with the opportunity to participate in one of the exercise interventions after completion of the study.
Measurements
Measurements were made at the outpatient clinical research facility operated by the Stanford Prevention Research Center. Trained and certified staff obtained baseline and all follow-up data and were blinded to participants’ group assignment. Adoption-phase data were collected at baseline, 3 months, and 6 months for all three groups. Maintenance-phase data were collected at 12 months for the two exercise groups. The full measurement battery was collected at baseline and at 6 and 12 months. At 3 months, a subset of these measures was collected. The data collected at 3 months are not included in this report.
Physical Functioning
Physical-functioning measures included balance, muscle strength and endurance, flexibility, and cardiorespiratory endurance. Balance measures included the single-leg-stance and functional-reach tests. The single-leg-stance test is frequently used in studies evaluating health-related fitness in older adults (Bohannon, 2006; Suni et al., 1996). Participants are timed on their ability to stand on a single leg with their eyes open, up to a 1-min maximum. The better of two trials for each leg is recorded. Functional reach assesses dynamic balance by measuring the maximal distance a participant can reach forward beyond arms’ length, while maintaining a fixed base of support in the standing position (Duncan, Weiner, Chandler, & Studenski, 1990). The better of two trials is recorded.
Upper and lower body muscle-strength and -endurance measures included 30-s timed arm-curl and chair-stand tests, respectively (Rikli & Jones, 1999a, 1999b). For the arm-curl test, participants perform a full range of motion using a hand weight (5 lb for women, 8 lb for men). The number of arm curls completed in 30 s is recorded. For the chair-stand test participants rise to a full standing position and then return to a seated position, with arms folded across their body, as many times as possible within the 30-s time limit. The number of stands completed within the time limit is recorded (Rikli & Jones, 1999a, 1999b).
Upper and lower body flexibility measures included the back-scratch (Rikli & Jones, 1999a, 1999b) and sit-and-reach tests (Minister of Supply and Services Canada, 1986; Jackson & Langford, 1989), respectively. For the back-scratch test, participants stand and then raise one arm above the head, bend the elbow, and reach down across the back as far as possible. Simultaneously, the opposite arm is extended up along the back as far as possible to meet or overlap the fingers of both hands. The distance of overlap (plus score) or the distance between (minus score) the tips of the middle fingers is measured in centimeters. The better of two trials is recorded. The sit-and-reach test was performed using the Accuflex I Sit and Reach Box (Novel Products, Rockton, IL) with the participant sitting on the floor, head and back against a wall, legs outstretched, and feet against the box. They were instructed to reach as far forward as possible with their arms stretched out in front and fingertips lightly sliding along a ruler. After a practice trial, participants perform the procedure three times and the best score is used.
Cardiorespiratory endurance was assessed by treadmill testing. At baseline, participants performed a clinical maximal treadmill exercise test using a Balke-type protocol (1- to 2-MET increase every 2 min) with continuous monitoring of a 12-lead ECG, with blood pressure and rating of perceived exertion recorded at the end of each stage and at peak exercise (ACSM, 2005). This test was used to provide medical clearance for the exercise programs and as a baseline measure of cardiorespiratory fitness. At 6 and 12 months a submaximal treadmill test was performed with an intensity target of 85% of estimated age-predicted maximal heart rate. Changes in heart rate, systolic blood pressure, and rating of perceived exertion at a set submaximal work rate (treadmill speed and grade) have been identified as reliable measures of changes in cardiorespiratory fitness (ACSM, 2005). The treadmill protocol (progression of workloads and measurements) remained the same, which enabled us to use changes in submaximal heart rate, systolic blood pressure, and rating of perceived exertion as indicators of changes in cardiorespiratory endurance.
Cognitive Functioning
Age-related cognitive changes are thought to be associated in part with a decline in executive functions (Lezak, 1995; Spreen & Strauss, 1998). Measures of executive function assessing specific processes, such as goal-directed behavior, information-processing speed, or working memory, have been reported to be sensitive to change after aerobic-exercise interventions (Colcombe & Kramer, 2003). In this study, a 60-s animal-naming test was used to assess semantic fluency (verbal retrieval and recall; Lezak, 1995; Tombaugh, Kozak, & Rees, 1999), and forward and backward digit-span tests were used to assess attention, concentration, and mental tracking (Bopp & Verhaeghen, 2005; Spreen & Strauss, 1998). There is no strong consensus as to what cognitive measures to use as outcomes of physical activity, but the measures selected have been reported to be sensitive to change after an exercise intervention and were easy to administer with only minor staff and participant burden (Colcombe & Kramer, 2003).
Additional Measures
At the study orientation session, participants were provided questionnaires to record demographics, medical history, health behaviors, and psychosocial status. These questionnaires were brought to the baseline visit and reviewed for completeness by study staff.
Physical Activity Assessment
Class attendance was recorded by the instructors to track adherence to the Tai Chi and WE interventions. In addition, to assess overall participation in physical activity during the study, participants completed the Community Healthy Activities Model Program for Seniors (CHAMPS) physical activity questionnaire (Stewart et al., 2001) at baseline and 6 and 12 months. Time spent and calories expended during moderate- and vigorous-intensity physical activity were determined from the CHAMPS. The CHAMPS has been shown to detect changes in physical activity among older adults in response to an intervention (Stewart et al., 2001).
Data Analysis
Frequency distributions were run on every variable to check for extreme values. Data were analyzed using the Statistical Analysis System (Version 9.1, SAS Institute Inc., Cary, NC). Descriptive statistics were calculated for all variables. Intention-to-treat analysis was performed, with all participants randomized to the study included in the analysis (Kraemer, 2003; Newell, 1992). Missing data were replaced using the last observation carried forward (Nich & Carroll, 2002; Streiner & Geddes, 2001). For the adoption-phase data, analysis of variance was performed on baseline to 6-month change data to determine which group had significantly better outcomes in physical and cognitive functioning after 6 months. If the overall ANOVA was significant, Tukey’s pairwise comparisons were performed to determine where the mean difference was. For the maintenance-phase data, independent-sample t tests were performed comparing change scores to determine which exercise group had significantly better outcomes in physical and cognitive functioning, by subtracting baseline from 12-month scores, using intention-to-treat analysis. In addition, because declines in physical and cognitive functioning are associated with aging, we calculated dependent-sample t tests to determine whether there were statistically significant changes in physical and cognitive functioning in each exercise group after 12 months.
Results
The recruitment, randomization, and retention flowchart for the study is shown in Figure 1. A total of 383 people were screened by phone for eligibility, 243 attended an orientation session, and 196 were invited for a baseline assessment. Approximately 34% (132) of the 383 people assessed for eligibility enrolled in the study. Major reasons for loss of participants between initial identification and randomization included scheduling conflicts (97), medical ineligibility (88), transportation issues (22), randomization refusal (21), and other reasons (23). A total of 115 (87%) participants completed the adoption phase of the study. The number of early dropouts in this study was not significantly different between groups (Fisher’s exact test, p = .08). Six-month study completers were more likely to be married and have fewer chronic health problems than those dropping out of the study earlier (Fisher’s exact test, p ≤ .01).
Figure 1.
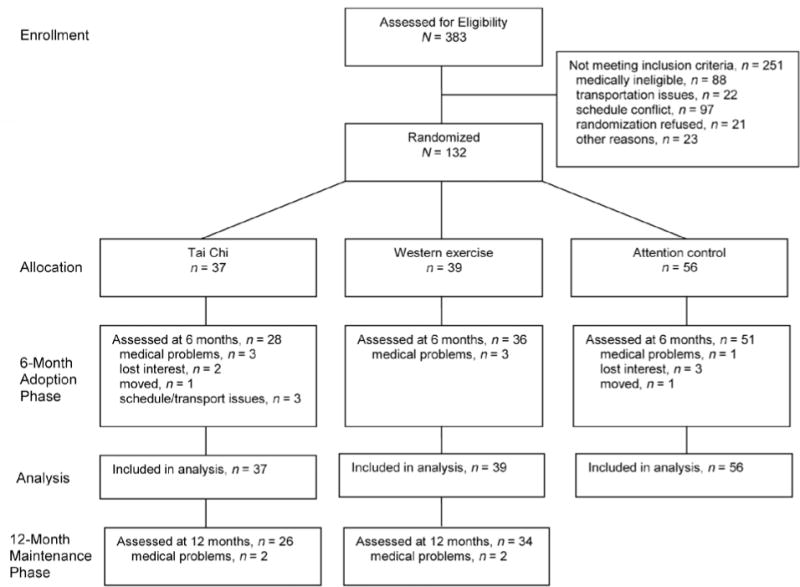
Flowchart of participants throughout the study. Recruitment and enrollment took place between April 2000 and September 2001. Data were collected through October 2002.
Baseline Characteristics
Baseline characteristics of participants are presented in Table 1. Participants were on average 69 (± 5.8) years old (range = 60–84 years), college educated, with good perceived health. Most were married (56%), White (85%), and women (70%). Hypertension (42.5%) was the most commonly self-reported medical problem, followed by chronic back pain (17.4%) and an irregular heartbeat (14.2%). There were no statistically significant differences between the groups at baseline, except for self-reported history of angina (p = .01; Table 1).
Table 1.
Baseline Characteristics of Participants in the Wellness Interventions for Self Enrichment
| Tai Chi | Western exercise | Control | Group comparisons, pa | |
|---|---|---|---|---|
| % (n) | 28% (37) | 30% (39) | 42% (56) | .19 |
| Age in years, M (SD) | 70.6 (5.9) | 68.5 (5.0) | 68.2 (6.2) | .14 |
| Education in years, M (SD) | 15.9 (2.7) | 16.1 (1.9) | 16.3 (1.6) | .61 |
| Perceived health,b M (SD) | 1.9 (0.8) | 2.0 (0.8) | 2.3 (0.7) | .11 |
| Women, % | 65 | 72 | 73 | .69 |
| Regular physical activity, % | 19 | 26 | 27 | .69 |
| Previous Tai Chi experience, % | 19 | 26 | 25 | .80 |
| Married or living together, % | 42 | 62 | 60 | .16 |
| White, % | 81 | 89 | 85 | .81 |
| Self-reported medical history, % | ||||
| hypertension | 47 | 35 | 45 | .55 |
| irregular heartbeat | 13 | 22 | 10 | .26 |
| angina | 13 | 3 | 0 | .01 |
| previous myocardial infarction | 6 | 0 | 0 | .07 |
| circulation problem in legs | 6 | 6 | 8 | 1.00 |
| ever smoked | 20 | 14 | 10 | .46 |
| current smoker | 0 | 2 | 2 | 1.00 |
| asthma | 6 | 16 | 6 | .26 |
| diabetes | 0 | 3 | 4 | .79 |
| chronic back pain | 13 | 19 | 19 | .75 |
| arthritis | 3 | 0 | 2 | .74 |
| major depression | 3 | 3 | 6 | .86 |
Analysis of variance or Fisher’s exact test group comparisons.
Possible range 1 = excellent to 5 = poor.
Intervention Adherence
Adoption Phase
The median adherence rate was highest in the Tai Chi group (77%), with slightly lower rates for the WE (68%) and control (67%) groups (between-groups differences, p > .05). In the Tai Chi group 75% of participants attended more than 66% of the class sessions, and 56% of WE participants attended 66% of prescribed classes (between-groups differences, p = .007). CHAMPS 6-month data indicated that WE participants significantly increased the number of moderate-intensity exercise sessions per week (4.6 ± 5.1) relative to baseline compared with the Tai Chi (1.6 ± 3.6, p < .05) and control groups (0.9 ± 3.3, p < .05).
Maintenance Phase
Class adherence was higher in participants assigned to Tai Chi than those in WE (65% vs. 53%, respectively; between-groups differences, p > .05). During the maintenance phase, 50% and 28% of participants attended more than 66% of assigned classes in Tai Chi and WE, respectively. CHAMPS 12-month data showed a significant increase in the number of moderate-intensity exercise sessions per week for both WE (4.6 ± 4.5, p = .006) and Tai Chi (2.2 ± 5.0, p = .003) groups compared with baseline. There were no statistically significant between-groups differences (t = 1.99, p = .051).
Physical and Cognitive Functioning
Participants in this study had generally good baseline physical- and cognitive-functioning scores (Table 2). Reported age-specific normative physical-functioning data indicate that they were higher than the 50th percentile for functional reach and upper and lower body strength (Duncan et al., 1990; Rikli & Jones, 1999a, 1999b). Similarly, reported age-specific cognitive-functioning data indicate that participants in this study were higher than the 50th percentile for semantic fluency (Tombaugh et al., 1999) and the digit-span tests (Bopp & Verhaeghen, 2005).
Table 2.
Baseline Physical- and Cognitive-Functioning Measures of Central Tendency and Normative Data
| Baseline
|
Normative Data at 50th Percentile, 69 Years
|
Reference | ||||||
|---|---|---|---|---|---|---|---|---|
| M ± SD | Median | Observed range | Skewness | Kurtosis | Women | Men | ||
| Physical Functioning | ||||||||
| Balance | ||||||||
| single-leg stance (s) | 30.7 ± 20.7 | 25.7 | 1–60 | 0.23 | −1.42 | 27 | 27 | Bohannon, 2006 |
| functional reach (n = 103; in.) | 16.8 ± 2.8 | 17.0 | 8.5–27.5 | 0.19 | 2.43 | 14 | 14 | Duncan et al., 1990 |
| Strength | ||||||||
| arm curls (no. in 30 s) | 16.1 ± 5.1 | 15.0 | 8–38 | 0.97 | 1.55 | 15 | 18 | Rikli & Jones, 1999a, 1999b |
| chair stands (no. in 30 s) | 14.2 ± 4.9 | 14.0 | 4–33 | 1.15 | 2.6 | 14 | 15 | Rikli & Jones, 1999a, 1999b |
| Flexibility (n = 130) | ||||||||
| back-scratch test (cm) | −3.6 ± 9.7 | −1.0 | −30–20 | −0.58 | −0.11 | −1.0 | −4.0 | Rikli & Jones, 1999a, 1999b |
| sit-and-reach test (cm) | 19.3 ± 9.6 | 19.0 | 0–17 | −0.14 | 0.11 | 24 | 17 | Minister of Supply and Services Canada, 1986 |
| Cognitive Functioning | ||||||||
| Animal-naming test (n = 131; no. in 60 s) | 20.7 ± 5.3 | 20.0 | 11–38 | 0.42 | −0.12 | 19 | 19 | Tombaugh et al., 1999 |
| Digits forward (sequence length) | 9.7 ± 2.1 | 10.0 | 4–15 | 0.09 | −0.18 | 7 | 7 | Bopp & Verhaeghen, 2005 |
| Digits backward (sequence length) | 6.3 ± 2.1 | 6.0 | 2–11 | 0.41 | −0.39 | 5 | 5 | Bopp & Verhaeghen, 2005 |
Adoption Phase
Physical Functioning
At baseline, participants were able to stand on one leg on average for 30 s before losing their balance (single-leg stance, Tables 2 and 3), which is below the 50th percentile for reported age-specific normative data. Tai Chi participants had greater improvements than WE and control participants after the 6-month adoption phase, F(df 3, 129) = 3.36, p = .038. Tukey’s pairwise comparisons of the mean differences revealed that Tai Chi participants had significantly more improvement in balance than controls (mean difference = 5.5 s, p < .05).
Table 3.
Adoption-Phase (Baseline to 6 Months) Comparisons Between Groupsa
| Change, M ± SD
|
ANOVA
|
Group Comparisons, ES, Mean Difference [CI] if p ≤ .05
|
||||||
|---|---|---|---|---|---|---|---|---|
| TC, n = 37 | WE, n = 39 | C, n = 56 | F | p | TC vs. C | WE vs. C | TC vs. WE | |
| Physical Functioning | ||||||||
| Balance | ||||||||
| single-leg stance (s) | 6.5 ± 9.4 | 3.9 ± 13.9 | 0.9 ± 7.3 | 3.36 | .038 | 0.54, 5.5 [0.4, 10.7] |
0.29 | 0.25 |
| functional reach (n = 103; in.) | −0.02 ± 1.4 | 0.4 ± 1.8 | 0.3 ± 2.9 | 0.29 | .745 | −0.15 | 0.04 | −0.19 |
| Strength | ||||||||
| arm curls (no. in 30 s) | 3.7 ± 4.5 | 3.6 ± 4.6 | 3.5 ± 3.7 | 0.01 | .991 | 0.03 | 0.02 | 0.01 |
| chair stands (no. in 30 s) | 3.5 ± 3.8 | 3.4 ± 3.6 | 2.0 ± 3.2 | 3.05 | .051 | 0.46 | 0.41 | 0.05 |
| Flexibility (n = 130) | ||||||||
| back-scratch test (cm) | 0.8 ± 3.4 | 3.7 ± 6.7 | 1.1 ± 3.3 | 4.67 | .011 | −0.07 | 0.55, 2.5 [0.3, 4.8] |
−0.62, 2.9 [0.4, 5.4] |
| sit-and-reach test (cm) | 1.4 ± 5.1 | 2.3 ± 3.5 | 1.7 ± 3.3 | 0.49 | .613 | −0.06 | 0.16 | −0.22 |
| Cardiorespiratory endurance (n = 129)b | ||||||||
| heart rate (beats/min) | −3.2 ± 6.3 | −4.8 ± 5.6 | −3.8 ± 8.5 | 0.51 | .600 | 0.08 | −0.15 | 0.23 |
| systolic blood pressure, mm Hg | −3.2 ± 15.8 | −2.9 ± 15.1 | −3.3 ± 17.5 | 0.01 | .993 | 0.01 | 0.03 | −0.02 |
| rating of perceived exertion | −0.1 ± 1.5 | −0.4 ± 1.4 | −0.4 ± 1.3 | 0.80 | .454 | 0.26 | 0.06 | 0.20 |
| Cognitive Functioning | ||||||||
| Animal-naming test (n = 131; no. in 60 s) | 0.8 ± 4.1 | 2.0 ± 4.7 | 0.6 ± 4.1 | 1.18 | .311 | 0.04 | 0.31 | −0.27 |
| Digits forward (sequence length) | 0.03 ± 1.8 | −0.5 ± 1.6 | −0.05 ± 1.6 | 1.33 | .268 | 0.05 | −0.29 | 0.34 |
| Digits backward (sequence length) | 0.8 ± 1.7 | −0.7 ± 1.9 | −0.1 ± 1.6 | 7.75 | <.001 | 0.55, 0.9 [0.1, 1.8] |
−0.34 | 0.90, 1.5 [0.6, 2.5] |
Note. ES = effect size; CI = confidence interval; TC = Tai Chi; WE = Western exercise; C = control.
Submaximal treadmill test unadjusted for antihypertensive medication, age, or gender.
Intention-to-treat analysis, missing data = last observation carried forward.
The back-scratch test was used to assess upper body flexibility. At baseline, participants were below the 50th percentile for reported age-specific normative data (Tables 2 and 3). WE participants had greater improvements than Tai Chi and control participants after the 6-month adoption phase, F(df 3, 129) = 4.67, p = .011. Tukey’s pairwise comparisons of the mean differences revealed that WE participants had significantly more improvement in upper body flexibility than the other two groups (mean difference WE vs. control = 2.5 cm, p < .05; mean difference WE vs. Tai Chi = 2.9 cm, p < .05).
Cognitive Functioning
An indicator of cognitive functioning, the backward digit-span test, is thought to assess attention, concentration, and mental tracking (Lezak, 1995). At baseline, participants were below the 50th percentile for reported age-specific normative data (Bopp & Verhaeghen, 2005; Table 2). Tai Chi participants had greater improvements than WE and control participants after the 6-month adoption phase, F(df 3, 129) = 7.75, p < .001. Tukey’s pairwise comparisons of the mean differences revealed that Tai Chi participants had significantly more improvement in cognitive functioning than the other 2 groups (mean difference Tai Chi vs. control = 0.9 digits, p < .05; mean difference Tai Chi vs. WE = 1.5 digits, p < .05; Table 3).
Maintenance Phase
Physical Functioning
After the 6-month maintenance phase (i.e., Months 7–12), participants in the Tai Chi and WE groups had statistically significant within-group improvements in several measures of physical functioning compared with their baseline values (Table 4). However, there were no longer significant physical-functioning differences between the two exercise groups by Month 12 (p > .05).
Table 4.
Maintenance-Phase (Baseline to 12 Months) Comparisons Within and Between Exercise Groupsa
| Within-Group Comparisons
|
||||||||
|---|---|---|---|---|---|---|---|---|
| Tai Chi, n = 37
|
Western Exercise, n = 39
|
|||||||
| TCΔ
|
Baseline vs. 12 Mo
|
WE Δ
|
Baseline vs. 12 Mo
|
Between-G roups Comparisons, vs. 12 Mo
|
||||
| M ± SD | t | p | M ± SD | t | p | t | p | |
| Physical Functioning | ||||||||
| Balance | ||||||||
| single-leg stance (s) | 7.5 ± 11.3 | 3.51 | .002 | 1.0 ± 17.5 | 0.35 | .731 | 1.79 | .078 |
| functional reach (n = 103; in.) | −0.3 ± 1.4 | −0.83 | .419 | 0.4 ± 2.0 | 0.95 | .352 | −1.18 | .243 |
| Strength | ||||||||
| arm curls (no. in 30 s) | 6.0 ± 4.3 | 7.30 | <.001 | 5.2 ± 4.0 | 7.82 | <.001 | 0.71 | .481 |
| chair stands (no. in 30 s) | 5.0 ± 3.3 | 7.87 | <.001 | 4.0 ± 3.4 | 7.14 | <.001 | 1.10 | .274 |
| Flexibility (n = 130) | ||||||||
| back-scratch test (cm) | 2.0 ± 4.3 | 2.51 | .018 | 1.6 ± 4.0 | 2.35 | .025 | 0.46 | .645 |
| sit-and-reach test (cm) | 1.6 ± 4.5 | 1.92 | .065 | 1.7 ± 3.4 | 2.96 | .006 | −0.07 | .944 |
| Cardiorespiratory endurance (n = 129)b | ||||||||
| heart rate (beats/min) | −9.3 ± 8.0 | −5.94 | <.001 | −4.5 ± 10.7 | −2.38 | .024 | −1.89 | .065 |
| systolic blood pressure, mm Hg | −6.5 ± 18.1 | −1.82 | .080 | −1.8 ± 22.4 | −0.46 | .650 | −0.86 | .396 |
| rating of perceived exertion | −0.8 ± 1.9 | −2.12 | .044 | −0.3 ± 1.7 | −1.03 | .310 | −1.03 | .306 |
| Cognitive Functioning | ||||||||
| Animal-naming test (n = 131; no. in 60 s) | 3.7 ± 5.9 | 3.27 | .003 | 2.3 ± 4.8 | 2.81 | .008 | 1.03 | .308 |
| Digits forward (sequence length) | 0.4 ± 2.2 | 0.09 | .932 | −0.3 ± 2.1 | −0.80 | .428 | 0.59 | .561 |
| Digits backward (sequence length) | 0.8 ± 1.3 | 3.26 | .003 | −0.3 ± 2.1 | −0.78 | .440 | 2.52 | .014 |
Note. TC = Tai Chi; WE = Western exercise; Δ = change score.
Intention-to-treat analysis, missing data = last observation carried forward.
Submaximal treadmill test unadjusted for antihypertensive medication, age, or gender.
Cognitive Functioning
Similar to the results after the adoption phase, Tai Chi participants maintained their improvements in backward digit span compared with WE participants (Table 4). Tai Chi participants also had a statistically significant within-group improvement in the backward digit-span test (Table 4). An independent-sample t test examining the 12-month change in cognitive functioning was statistically significant between groups, with Tai Chi participants performing better than those in WE, t(df 2, 74) =2.52, p = .014. Participants in both Tai Chi and WE had statistically significant within-group improvements in semantic fluency after the maintenance phase, although between-groups differences did not reach statistical significance.
Discussion
This was a two-phase randomized clinical trial and, to our knowledge, the first to examine the effect of Tai Chi on cognitive functioning. The major objective of the WISE study was to evaluate the effects of Tai Chi versus a standard program of Western exercise consisting of endurance, strength, and flexibility training on physical and cognitive functioning in healthy, community-dwelling adults age 60 years and older. Participants in this study were on average healthy, college-educated White women, which is fairly representative of older adults living in San Mateo and Santa Clara counties in northern California (San Francisco Bay Area Census, 2002) with only minimal medical exclusions, so findings in this study mainly apply to healthy, college-educated White women. Despite the general age-associated declines in physical and cognitive functioning, WISE participants had baseline values greater than the 50th percentile on many of the physical- and cognitive-function variables measured, making it difficult to elicit statistically significant improvements and thus decreasing the likelihood that participation in either of the exercise programs would lead to significant improvements in these variables (i.e., a ceiling effect could have occurred; King, Haskell, Young, Oka, & Stefanick, 1995).
Class instruction was provided by highly trained instructors, and there were conveniently located community-based facilities willing to accommodate the exercise groups. Adherence to the two exercise interventions was good (adoption-phase median = 71%, maintenance-phase median = 59%) and similar to that of previous community-based exercise trials among older adults (King et al., 1995). Tai Chi participants on average attended more exercise classes than those assigned to WE, which may have affected the results. Exercise preference may partly explain the difference in intervention adherence rates; some previous research has indicated that some groups of women may prefer group-based exercise programs like Tai Chi (Kutner, Barnhart, Wolf, McNeely, & Xu, 1997; Taylor-Piliae & Froelicher, 2007) rather than exercising in a traditional gym-type setting (Moore, 1996; Ruland & Moore, 2001).
The observed improvements in physical functioning in this study are consistent with previous studies that showed that participants assigned to WE had greater improvements in upper body flexibility than the other two groups, and participants assigned to Tai Chi had greater improvements in static balance (Wolf et al., 1996). In addition, the statistically significant 12-month improvements in both exercise groups for measures taken during the submaximal treadmill testing, an indicator of cardiorespiratory endurance (Table 4), support the adequacy of intervention exercise dose for each group. Furthermore, data from the CHAMPS indicated that, on average, participants in both the Tai Chi and WE groups increased their frequency of moderate-intensity activities between baseline and 6 and 12 months, with greater increases reported in the WE group.
On the other hand, cognitive functioning in WE participants was not significantly better than in the other two groups. This finding is in contrast with previous reported research among older adults examining the effect of WE on cognitive functioning compared with controls (Fabre, Chamari, Mucci, Masse-Biron, & Prefaut, 2002; Molloy, Beerschoten, Borrie, Crilly, & Cape, 1988; Weuve et al., 2004). Executive functions are high-level skills (e.g., planning) that influence more basic skills such as attention, memory, and motor skills. A person may perform well on a simple task, such as naming as many animals as possible in 1 min, but struggle with more complex tasks such as repeating a sequence of numbers in reverse order (Angevaren, Aufdemkampe, Verhaar, Aleman, & Vanhees, 2008). In addition, the relationship between regular physical activity and cognitive function could potentially be modified by factors other than improvements in cardiovascular biomarkers, such as genetic predispositions or various comorbidities, which may in part explain the results obtained in this study.
Animal models have shown possible underlying mechanisms for an exercise effect on cognition in older adults. Specifically, exercise decreases amyloid load (Adlard, Perreau, Pop, & Cotman, 2005), positively affects hippocampal neuronal function (Fordyce, Starnes, & Farrar, 1991) and hippocampal and parietal cortical cholinergic function and spatial learning (Fordyce & Farrar, 1991), increases levels of brain-derived neurotrophic factors, and may protect against antioxidant and other forms of neuronal damage (Stummer, Weber, Tranmer, Baethmann, & Kempski, 1994).
Tai Chi participants had a statistically significant improvement in one measure of cognitive functioning, the backward digit-span test, when compared with the other two groups, which is a novel finding. The digit-span tests are considered indicators of attention, concentration, and mental tracking (Lezak, 1995; Spreen & Strauss, 1998). In addition, mental tracking in the backward digit-span test is thought to involve double tracking (Dore, Elias, Robbins, Elias, & Brennan, 2007; Robbins, Elias, Elias, & Budge, 2005). When practicing Tai Chi, participants were taught to be mindful of their movements. During the performance of Tai Chi, paying careful attention to what the body is doing and how it feels is important, for example, relaxation and correct foot placement. Concentration was enhanced during Tai Chi, as participants were instructed to perform at a slow and relaxed pace with inattention to thoughts. Mental tracking during Tai Chi is important so that participants remain relaxed and remember the sequence of postures and the correct arm and leg movements. Double tracking is plausible during Tai Chi when both the mental and physical aspects are performed simultaneously (Lee et al., 2002; Spreen & Strauss, 1998). In contrast, WE groups in the current study were not specifically instructed to mentally focus on exactly how they were moving. However, further Tai Chi research is needed to determine whether this type of improvement in cognitive functioning can be replicated in other populations and why the backward digit-span test in particular may be sensitive to change with this type of activity.
To help achieve “healthy aging,” a major goal of exercise conditioning programs, as well as other life-style interventions, is to prevent age-related declines that occur with various aspects of physical- and cognitive-functioning domains (Fries, 1996). In WISE, many participants scored well on a number of tests evaluating physical and cognitive functioning. Thus, for an exercise regimen to be “successful” for this population, it may not need to produce significant increases in functioning but simply prevent or slow its decline so that independence and quality of life are maintained (Fries, 1996). To test such hypotheses, specific interventions will need to be tested for years, not just weeks or months.
We conclude that both Western and Tai Chi exercises can have positive, though somewhat different, impacts on a variety of functional domains, including physical and cognitive function. The potential impact of Tai Chi on cognitive function, in particular, deserves further investigation.
Acknowledgments
The authors would like to thank all the participants and study staff—Kathy Berra, Laurie Ausserer, Lisa Hagerty, and Jeff Myll—for their enthusiasm and support. Special thanks to Emily Lee, our Tai Chi grand master; the Western-exercise instructors—Janet Schumacher, Toni Toledo, Joyce Russum, Robert Tognoli, Dina Amsterdam, and Becky Meldrum—and the YMCA for use of the facility to conduct the study.
This study was funded by Grant # NIH/NIA AG 16337 (W. Haskell, PI) from the U.S. Department of Health and Human Services. Dr. Taylor-Piliae was supported by Public Health Service Training Grant T32 HL007034-31 from the National Heart, Lung and Blood Institute (S. Fortmann, PI) while working on this study. She is currently employed at the University of Arizona. Ms. Newell and Ms. Cherin have no financial support or interests to report. Dr. Lee is currently funded by the Department of Energy and has an ownership interest in the Tai Chi Cultural Center, Los Altos, CA. Dr. King has research funding from NIH/NIA and NHLBI and is an NIH scientific consultant. Dr. Haskell has research funding from NIH/NIA and NHLBI and is chairman of the Cooper Institute Scientific Advisory Board.
Footnotes
Author contributions: Dr. Taylor-Piliae: Acquisition of data, analysis and interpretation of data, and manuscript preparation. Ms. Newell: Study concept and design, acquisition of participants, and manuscript preparation. Ms. Cherin: Acquisition of participants and manuscript preparation. Dr. Lee: Study concept and design and manuscript preparation. Dr. King: Study concept and design, analysis and interpretation of data, and manuscript preparation. Dr. Haskell: Study concept and design, analysis and interpretation of data, and manuscript preparation.
Sponsor’s role: The funding agency had no role in the design, methods, recruitment, data collection, analyses, or manuscript preparation.
Contributor Information
Ruth E. Taylor-Piliae, College of Nursing, University of Arizona, Tucson, AZ.
Kathryn A. Newell, School of Medicine
Rise Cherin, School of Medicine.
Martin J. Lee, The Stanford Linear Accelerator Center, Stanford University, Stanford, CA
Abby C. King, School of Medicine
William L. Haskell, School of Medicine
References
- Adlard PA, Perreau VM, Pop V, Cotman CW. Voluntary exercise decreases amyloid load in a transgenic model of Alzheimer’s disease. The Journal of Neuroscience. 2005;25(17):4217–4221. doi: 10.1523/JNEUROSCI.0496-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, Leon AS. Compendium of physical activities: An update of activity codes and MET intensities. Medicine and Science in Sports and Exercise. 2000;32(9, Suppl):S498–S504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- American College of Sports Medicine. American College of Sports Medicine practice guideline: Physical activity programs and behavior counseling in older adult populations. Medicine and Science in Sports and Exercise. 2004;36(11):1997–2003. doi: 10.1249/01.mss.0000145451.08166.97. [DOI] [PubMed] [Google Scholar]
- American College of Sports Medicine. American College of Sports Medicine’s guidelines for exercise testing and prescription. 7th. Philadelphia, PA: Lippincott Williams & Wilkins; 2005. [Google Scholar]
- Angevaren M, Aufdemkampe G, Verhaar HJ, Aleman A, Vanhees L. Physical activity and enhanced fitness to improve cognitive function in older people without known cognitive impairment. Cochrane Database of Systematic Reviews (Online: Update Software) 2008;3:CD005381. doi: 10.1002/14651858.CD005381.pub3. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. New York, NY: W. H. Freeman; 1997. [Google Scholar]
- Bohannon RW. Single limb stance times: A descriptive meta-analysis of data from individuals at least 60 years of age. Topics in Geriatric Rehabilitation. 2006;22(1):70–77. [Google Scholar]
- Bopp KL, Verhaeghen P. Aging and verbal memory span: A meta-analysis. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 2005;60(5):223–233. doi: 10.1093/geronb/60.5.p223. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. The state of aging and health in America 2004. Washington, DC: Author, Merck Institute of Aging & Health, & Gerontological Society of America; 2004. [Google Scholar]
- Centers for Disease Control and Prevention. US physical activity statistics: 2003 state demographic data comparison. 2005 Sep 13; Retrieved from http://apps.nccd.cdc.gov/PASurveillance/DemoCompareResultV.asp#result.
- Colcombe S, Kramer AF. Fitness effects on the cognitive function of older adults: A meta-analytic study. Psychological Science. 2003;14(2):125–130. doi: 10.1111/1467-9280.t01-1-01430. [DOI] [PubMed] [Google Scholar]
- Dore GA, Elias MF, Robbins MA, Elias PK, Brennan SL. Cognitive performance and age: Norms from the Maine–Syracuse Study. Experimental Aging Research. 2007;33(3):205–271. doi: 10.1080/03610730701319087. [DOI] [PubMed] [Google Scholar]
- Duncan PW, Weiner DK, Chandler J, Studenski S. Functional reach: A new clinical measure of balance. Journal of Gerontology. 1990;45(6):M192–M197. doi: 10.1093/geronj/45.6.m192. [DOI] [PubMed] [Google Scholar]
- Fabre C, Chamari K, Mucci P, Masse-Biron J, Prefaut C. Improvement of cognitive function by mental and/or individualized aerobic training in healthy elderly subjects. International Journal of Sports Medicine. 2002;23(6):415–421. doi: 10.1055/s-2002-33735. [DOI] [PubMed] [Google Scholar]
- Fordyce DE, Farrar RP. Physical activity effects on hippocampal and parietal cortical cholinergic function and spatial learning in F344 rats. Behavioural Brain Research. 1991;43(2):115–123. doi: 10.1016/s0166-4328(05)80061-0. [DOI] [PubMed] [Google Scholar]
- Fordyce DE, Starnes JW, Farrar RP. Compensation of the age-related decline in hippocampal muscarinic receptor density through daily exercise or underfeeding. Journal of Gerontology. 1991;46(6):B245–B248. doi: 10.1093/geronj/46.6.b245. [DOI] [PubMed] [Google Scholar]
- Fries JF. Physical activity, the compression of morbidity, and the health of the elderly. Journal of the Royal Society of Medicine. 1996;89(2):64–68. doi: 10.1177/014107689608900202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galante L. Tai Chi: The supreme ultimate. York Beach, ME: Samuel Weiser; 1981. [Google Scholar]
- Hartman CA, Manos TM, Winter C, Hartman DM, Li B, Smith JC. Effects of T’ai Chi training on function and quality of life indicators in older adults with osteoarthritis. Journal of the American Geriatrics Society. 2000;48(12):1553–1559. doi: 10.1111/j.1532-5415.2000.tb03863.x. [DOI] [PubMed] [Google Scholar]
- Hogan M. Physical and cognitive activity and exercise for older adults: A review. International Journal of Aging & Human Development. 2005;60(2):95–126. doi: 10.2190/PTG9-XDVM-YETA-MKXA. [DOI] [PubMed] [Google Scholar]
- Jackson A, Langford NJ. The criterion-related validity of the sit and reach test: Replication and extension of previous findings. Research Quarterly for Exercise and Sport. 1989;60(4):384–387. doi: 10.1080/02701367.1989.10607468. [DOI] [PubMed] [Google Scholar]
- King AC. Interventions to promote physical activity by older adults. Journals of Gerontology, Series A. Biological Sciences and Medical Sciences. 2001;56(Spec. No. 2):36–46. doi: 10.1093/gerona/56.suppl_2.36. [DOI] [PubMed] [Google Scholar]
- King AC, Haskell WL, Young DR, Oka RK, Stefanick ML. Long-term effects of varying intensities and formats of physical activity on participation rates, fitness, and lipoproteins in men and women aged 50 to 65 years. Circulation. 1995;91(10):2596–2604. doi: 10.1161/01.cir.91.10.2596. [DOI] [PubMed] [Google Scholar]
- King AC, Pruitt LA, Phillips W, Oka R, Rodenburg A, Haskell WL. Comparative effects of two physical activity programs on measured and perceived physical functioning and other health-related quality of life outcomes in older adults. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 2000;55(2):M74–M83. doi: 10.1093/gerona/55.2.m74. [DOI] [PubMed] [Google Scholar]
- King ML, Williams MA, Fletcher GF, Gordon NF, Gulanick M, King CN American Association for Cardiovascular and Pulmonary Rehabilitation. Medical director responsibilities for outpatient cardiac rehabilitation/secondary prevention programs: A scientific statement from the American Heart Association/American Association for Cardiovascular and Pulmonary Rehabilitation. Circulation. 2005;112(21):3354–3360. doi: 10.1161/CIRCULATIONAHA.105.170333. [DOI] [PubMed] [Google Scholar]
- Kraemer HC. “Rules” of evidence in assessing the efficacy and effectiveness of treatments. Developmental Neuropsychology. 2003;24(2–3):705–718. doi: 10.1080/87565641.2003.9651916. [DOI] [PubMed] [Google Scholar]
- Kutner NG, Barnhart H, Wolf SL, McNeely E, Xu T. Self-report benefits of Tai Chi practice by older adults. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 1997;52(5):242–246. doi: 10.1093/geronb/52b.5.p242. [DOI] [PubMed] [Google Scholar]
- Lan C, Lai JS, Chen SY. Tai Chi Chuan: An ancient wisdom on exercise and health promotion. Sports Medicine (Auckland, NZ) 2002;32(4):217–224. doi: 10.2165/00007256-200232040-00001. [DOI] [PubMed] [Google Scholar]
- Lan C, Lai JS, Chen SY, Wong MK. 12-month Tai Chi training in the elderly: Its effect on health fitness. Medicine and Science in Sports and Exercise. 1998;30(3):345–351. doi: 10.1097/00005768-199803000-00003. [DOI] [PubMed] [Google Scholar]
- Lan C, Lai JS, Chen SY, Wong MK. Tai Chi Chuan to improve muscular strength and endurance in elderly individuals: A pilot study. Archives of Physical Medicine and Rehabilitation. 2000;81(5):604–607. doi: 10.1016/s0003-9993(00)90042-x. [DOI] [PubMed] [Google Scholar]
- Lee MJ, Lee E. Mind–body fitness: Ch’i-Kung Tai Chi. Los Altos, CA: Tai Chi Cultural Center; 1989. [Google Scholar]
- Lee MJ, Lee E, Johnstone J. Ride the tiger to the mountain: Tai Chi for health. Reading, MA: Perseus Books; 1989. [Google Scholar]
- Lee MJ, Lee E, Lee MT, Lee J. Becoming one with nature: Restore yourself with Tai Chi. New York, NY: Sterling; 2002. [Google Scholar]
- Lezak MD. Neuropsychological assessment. 3rd. New York, NY: Oxford University Press; 1995. [Google Scholar]
- Mazzeo RS, Cavanagh P, Evans WJ, Fiatarone M, Hagberg J, McAuley E, Startzell J. American College of Sports Medicine position stand. Exercise and physical activity for older adults. Medicine and Science in Sports and Exercise. 1998;30(6):992–1008. [PubMed] [Google Scholar]
- Minister of Supply and Services Canada. Canadian Standardized Test of Fitness operations manual. 3rd. Ottawa: Author; 1986. [Google Scholar]
- Molloy DW, Beerschoten DA, Borrie MJ, Crilly RG, Cape RD. Acute effects of exercise on neuropsychological function in elderly subjects. Journal of the American Geriatrics Society. 1988;36(1):29–33. doi: 10.1111/j.1532-5415.1988.tb03430.x. [DOI] [PubMed] [Google Scholar]
- Moore SM. Women’s views of cardiac rehabilitation programs. Journal of Cardiopulmonary Rehabilitation. 1996;16(2):123–129. doi: 10.1097/00008483-199603000-00007. [DOI] [PubMed] [Google Scholar]
- Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC American Heart Association. Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116(9):1094–1105. doi: 10.1161/CIRCULATIONAHA.107.185650. [DOI] [PubMed] [Google Scholar]
- Netz Y, Wu MJ, Becker BJ, Tenenbaum G. Physical activity and psychological well-being in advanced age: A meta-analysis of intervention studies. Psychology and Aging. 2005;20(2):272–284. doi: 10.1037/0882-7974.20.2.272. [DOI] [PubMed] [Google Scholar]
- Newell DJ. Intention-to-treat analysis: Implications for quantitative and qualitative research. International Journal of Epidemiology. 1992;21(5):837–841. doi: 10.1093/ije/21.5.837. [DOI] [PubMed] [Google Scholar]
- Nich C, Carroll KM. Intention-to-treat meets missing data: Implications of alternate strategies for analyzing clinical trials data. Drug and Alcohol Dependence. 2002;68(2):121–130. doi: 10.1016/s0376-8716(02)00111-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee report. 2008 Retrieved from http://www.health.gov/PAGuidelines/committeereport.aspx.
- Rikli RE, Jones CJ. Development and validation of a functional fitness test for community-residing older adults. Journal of Aging and Physical Activity. 1999a;7:129–161. [Google Scholar]
- Rikli RE, Jones CJ. Functional fitness normative scores for community-residing older adults, ages 60–94. Journal of Aging and Physical Activity. 1999b;7:162–181. [Google Scholar]
- Robbins MA, Elias MF, Elias PK, Budge MM. Blood pressure and cognitive function in an African-American and a Caucasian-American sample: The Maine–Syracuse Study. Psychosomatic Medicine. 2005;67(5):707–714. doi: 10.1097/01.psy.0000171164.50990.80. [DOI] [PubMed] [Google Scholar]
- Ruland CM, Moore SM. Eliciting exercise preferences in cardiac rehabilitation: Initial evaluation of a new strategy. Patient Education and Counseling. 2001;44(3):283–291. doi: 10.1016/s0738-3991(00)00189-0. [DOI] [PubMed] [Google Scholar]
- San Francisco Bay Area Census. San Francisco Bay Area census data. 2002 Retrieved from http://www.bayareacensus.ca.gov/bayarea.htm.
- Spreen O, Strauss E. A compendium of neuropsychological tests: Administration, norms, and commentary. 2nd. New York, NY: Oxford University Press; 1998. [Google Scholar]
- Stewart AL, Mills KM, King AC, Haskell WL, Gillis D, Ritter PL. CHAMPS physical activity questionnaire for older adults: Outcomes for interventions. Medicine and Science in Sports and Exercise. 2001;33(7):1126–1141. doi: 10.1097/00005768-200107000-00010. [DOI] [PubMed] [Google Scholar]
- Streiner D, Geddes J. Intention to treat analysis in clinical trials when there are missing data. Evidence-Based Mental Health. 2001;4(3):70–71. doi: 10.1136/ebmh.4.3.70. [DOI] [PubMed] [Google Scholar]
- Stummer W, Weber K, Tranmer B, Baethmann A, Kempski O. Reduced mortality and brain damage after locomotor activity in gerbil forebrain ischemia. Stroke. 1994;25(9):1862–1869. doi: 10.1161/01.str.25.9.1862. [DOI] [PubMed] [Google Scholar]
- Suni JH, Oja P, Laukkanen RT, Miilunpalo SI, Pasanen ME, Vuori IM, Bös K. Health-related fitness test battery for adults: Aspects of reliability. Archives of Physical Medicine and Rehabilitation. 1996;77(4):399–405. doi: 10.1016/s0003-9993(96)90092-1. [DOI] [PubMed] [Google Scholar]
- Taylor-Piliae RE. Tai Chi as an adjunct to cardiac rehabilitation exercise training. Journal of Cardiopulmonary Rehabilitation. 2003;23(2):90–96. doi: 10.1097/00008483-200303000-00004. [DOI] [PubMed] [Google Scholar]
- Taylor-Piliae RE, Froelicher ES. Methods to optimize recruitment and retention to an exercise study in Chinese immigrants. Nursing Research. 2007;56(2):132–136. doi: 10.1097/01.NNR.0000263971.46996.14. [DOI] [PubMed] [Google Scholar]
- Tombaugh TN, Kozak J, Rees L. Normative data stratified by age and education for two measures of verbal fluency: FAS and animal naming. Archives of Clinical Neuropsychology. 1999;14(2):167–177. [PubMed] [Google Scholar]
- Trends in aging—United States and worldwide. Morbidity & Mortality Weekly Report. 2003;52(6):101–104. 106. [PubMed] [Google Scholar]
- Weuve J, Kang JH, Manson JE, Breteler MM, Ware JH, Grodstein F. Physical activity, including walking, and cognitive function in older women. Journal of the American Medical Association. 2004;292(12):1454–1461. doi: 10.1001/jama.292.12.1454. [DOI] [PubMed] [Google Scholar]
- Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure: A meta-analysis of randomized, controlled trials. Annals of Internal Medicine. 2002;136(7):493–503. doi: 10.7326/0003-4819-136-7-200204020-00006. [DOI] [PubMed] [Google Scholar]
- Wolf SL, Barnhart HX, Kutner NG, McNeely E, Coogler C, Xu T. Reducing frailty and falls in older persons: An investigation of Tai Chi and computerized balance training. Atlanta FICSIT Group. Frailty and Injuries: Cooperative Studies of Intervention Techniques. Journal of the American Geriatrics Society. 1996;44(5):489–497. doi: 10.1111/j.1532-5415.1996.tb01432.x. [DOI] [PubMed] [Google Scholar]
- Wong AM, Lin YC, Chou SW, Tang FT, Wong PY. Coordination exercise and postural stability in elderly people: Effect of Tai Chi Chuan. Archives of Physical Medicine and Rehabilitation. 2001;82(5):608–612. doi: 10.1053/apmr.2001.22615. [DOI] [PubMed] [Google Scholar]


