Abstract
Background and Objectives
Dental caries is an important healthcare challenge in adults over 65 years of age. Integration of oral health screening into non-dental primary care practice may improve access to preventive dental care for vulnerable populations such as the elderly. Such integration would require easy, fast, and accurate early caries detection tools. Primary goal of this study was to evaluate the diagnostic performance of optical coherence tomography (OCT) imaging for detecting very early caries in the elderly living in community-based settings. The International Caries Detection and Assessment System (ICDAS) served as gold standard. Secondary goal of this study was to provide baseline prevalence data of very early caries lesions in independent living adults aged 65+ years.
Materials and Methods
Seventy-two subjects were recruited from three sites in Southern California: a retirement community, a senior health fair, and a convalescent hospital. Clinical examination was performed using the ICDAS visual criteria and this was followed by OCT imaging. The two-dimensional OCT images (B-scan) were analyzed with simple software. Locations with a log of back-scattered light intensity (BSLI) below 2.9 were scored as sound, and areas equaling or exceeding 2.9 BSLI were considered carious. Diagnostic performance of OCT imaging was compared with ICDAS score.
Results
OCT-based diagnosis demonstrated very good sensitivity (95.1%) and good specificity (85.8%). 54.7% of dentate subjects had at least one tooth with very early coronal caries.
Conclusions
Early coronal decay is prevalent in the unrestored pits and fissures of coronal surfaces of teeth in independent living adults aged 65+ years. Though OCT imaging coupled with a simple diagnostic algorithm can accurately detect areas of very early caries in community-based settings, existing devices are expensive and not well-suited for use by non-dental health care providers. Simple, inexpensive, fast, and accurate tools for early caries detection by field health care providers working in non-traditional settings are urgently needed to support inter-professional dental health management. Lasers Surg.
Keywords: coronal caries, dental decay, diagnostic imaging, ICDAS, inter-professional health care, optical coherence tomography, oral diagnosis
INTRODUCTION
Although dental caries is largely preventable, it is responsible for considerable morbidity in the elderly. Dental decay leads to tooth loss, difficulty eating, increased risk of diabetes, and reduced quality of life [1]. The 2011 Institute of Medicine Reports [2,3] call for increased integration of oral health screening and prevention interventions with primary health care to ensure better health in vulnerable populations such as the elderly. However, primary health care providers often lack training in basic oral health screening. A simple, low-cost, rapid tool that enables non-dental health professionals to screen for and monitor early non-cavitated caries in the elderly is essential to preventing the many negative sequellae of progressive cavitated dental caries.
Dental caries is a clinical challenge in adults over age 65 years [1,2]. Although caries risk in older adults is influenced by lifelong attributes such as sociodemographics, economics, and health-related behavior and attitudes, overall, the risk of dental caries increases with aging, resulting from factors such as side effects of medications and changes in cognition and dexterity. The National Center for Health Statistics reports that one out of five (19.6%) US adults over the age of 65 years has untreated coronal caries, and, if root caries is included, the prevalence is considerably greater [3]. Older adults experience 0.47–1.31 new carious surfaces per year, compared with 0.8–1.4 in adolescents [4]. In non-frail older adults, an average of 2.4 coronal surfaces become carious in 3 years, as compared with 1.1 root surfaces over the same period of time, with the latter often resulting from partial denture wear [5,6]. The prevalence of very early caries is not known. National statistics exclude its manifestations, such as white spot lesions from demineralization [7].
Very early dental caries can be arrested or even reversed [8]. In one study, 96% of very early dental caries was effectively treated with non-invasive interventions [9]. However, older adults often do not access routine dental care, where simple preventive measures could be provided. Even older adults who consistently seek medical care do not engage in regular dental visits, nor do they typically receive dental caries-preventive services (NHANES 1999–2014) [10]. Integrating oral health into low-cost, community-based primary health care programs for older adults can provide an opportunity for basic oral exams to assess and monitor early caries. Such exams could provide the basis for prevention interventions, consequently reducing future need for expensive and often arduous dental treatment [11,12].
Detection of early lesions and monitoring early dental caries for signs of progression can be challenging, even for experienced dentists [13–15]. The limitations of radiographs and clinical visual-tactile exams hamper detection of the minimal enamel changes characteristic of early caries progression or remineralization [16]. Emergent dental caries assessment criteria such as the ICDAS can augment the ability of health care providers to assess and manage early caries [17,18]. However, its very finely nuanced visual diagnostic criteria are not well-suited for adoption by non-dental community health care providers, and they cannot differentiate between arrested and active stained lesions. Accurate ICDAS assessment requires a highly developed synthesis of subtle visual cues on natural teeth that are the result of changes in the refractive index of the enamel surface. Excellent diagnostic sensitivity and specificity are possible when used by highly trained and standardized experts. It is, however, arduous, time-consuming, and less accurate when utilized by non-experts [19]. Histologic examination such as the methodology proposed by Ekstrand is the gold standard [20]; however, in the clinical situation, histologic examination clearly is not possible.
Optical coherence tomography (OCT) is a non-ionizing tissue imaging modality based on reflectivity and phase retardation by tissue surfaces. It has been used widely in medicine and has demonstrated great promise in assessing early caries [9,21–31], typically employing the near-infrared wavelength of 1,310 nm. Dentists and non-dental health care providers alike would benefit from a quick, simple, precise, and accurate caries assessment method [14]. Previous papers describe the use of OCT for dental caries detection [32–40]; however, to the best of our knowledge, there exist no studies that describe the use of OCT imaging to screen for caries in adults over 65 years of age.
The primary goal of this study was to evaluate the use of OCT imaging to detect early coronal caries. As the latest version of ICDAS, the ICDAS-II, is the most accurate clinical visual method currently available for this purpose, it was used as the primary measure for early decay. The secondary goal of this study was to provide baseline prevalence data of very early coronal caries lesions in independent living older adults aged 65+ years.
MATERIALS AND METHODS
This project was performed in full compliance with UCI protocol HS# 2011-8471 and UCLA IRB Reliance #365.
Protocol
Seventy-two subjects were recruited from three sites in Southern California: a retirement community, a senior health fair, and a convalescent hospital. Examiners completed the online ICDAS training (available at www.icdas.org/icdas-e-learning-course). At the retirement community, advertisements describing the study were placed in the community newspaper. Clinical examination and data collection took place on portable dental chairs in a recreational room. In the second cohort of subjects, participants undergoing a dental screening at a senior health fair were invited to participate in this study. Clinical examination and data collection were conducted in dental cubicles at a local dental hygiene school. The third cohort consisted of subjects at a convalescent hospital. These were otherwise independently living adults who were temporarily recovering from a medical procedure. Subjects were expected to return to independent living within days of our survey. After description of the study, individuals interested in participating were consented and then examined in their rooms.
A secondary goal of this study was to determine the prevalence of very early coronal caries in a more generalized population of older adults. For this reason edentulous individuals were not excluded at any of the sites. ICDAS-II requires teeth to be dry and clean; therefore, teeth in dentate individuals were dry-brushed in a standardized fashion to loosen debris, wiped with moistened cotton-tipped swabs, dried with cotton gauze, and then examined. Tooth presence, visible decay, and size of cavitation were determined visually and recorded on a scale of 0–6 using the ICDAS-II system [41]. Teeth that showed no evidence of change in the enamel of the occlusal surface were considered sound and given an ICDAS-II score of 0. Minor white or brown discoloration at the entrance to occlusal pits/fissures that was visible only after drying the teeth was recorded as an ICDAS-II score of 1. Distinct white or brown discoloration at the entrance to occlusal pits/fissures that was visible prior to drying the teeth was given an ICDAS-II score of 2. Visible signs of enamel breakdown without dentinal involvement were given an ICDAS-II score of 3; signs of enamel breakdown with dentinal involvement including rank decay were given an ICDAS-II score of 4+. Procedures were performed by a dentist with a head mounted light but without magnification. When one or more teeth scored as an ICDAS score of “1” or greater, photographs of areas of interest were recorded using a wireless intraoral camera (Daryou Instrument Ltd, Ontario, Canada MD950AUW).
Next, OCT images were acquired of no more than four of the highest and two of the lowest ICDAS scored areas of interest. Imaging was performed with a NirisR OCT system (Imalux, Cleveland, OH), a portable time-domain OCT system that uses low-coherent broadband light in the near infrared range. The central wavelength is 1,310 nm with a bandwidth of 70 nm. This system provides real-time images of 200 × 200 pixels with a maximum frame rate of 0.7 HZ. The spatial depth resolution of the system is 10–20 µm, with a depth scanning range of 2–3 mm in tissues. The lateral resolution is 25 µm, with a lateral scanning range of 1.5–2.5 mm. The device uses a 2.7 mm flexible fiber optic probe with sterile disposable sheath for real-time imaging.
Photographs were immediately downloaded to a dedicated study computer, and OCT scan lines marked electronically using Photoshop software to provide an accurate record of imaging location. Between subjects, the intra-oral camera was decontaminated using hospital grade decontamination wipes and a new impermeable, sterile disposable sheath was fitted over the imaging probe.
OCT Image Analysis
The two-dimensional OCT images (B-scan) were analyzed using Image J software (http://imagej.nih.gov/ij/). Measurement parameter was back scattered light intensity, i.e., intensity of the light signal returning from the sample onto the probe detector. An upper intensity thresholding of 2.9 was used to create the desired mask. Locations with a log of back-scattered light intensity (BSLI) below 2.9 were scored as sound (S), and areas equaling or exceeding 2.9 were considered to be decayed (D). This cut-off point was chosen based on a previous study which had identified this cut-off point to differentiate between very early decay (ICDAS-1) and sound tooth substance (ICDAS 0) [29].
Data Analysis
Descriptive analyses were conducted using IBM SPSS (Version 22) to describe study population (gender, age, and race) and tooth characteristics (missing, decayed, restored tooth). Prevalence of decay, sensitivity, and specificity, by OCT versus Gold Standard (ICDAS-II) were determined.
RESULTS
Sample Description
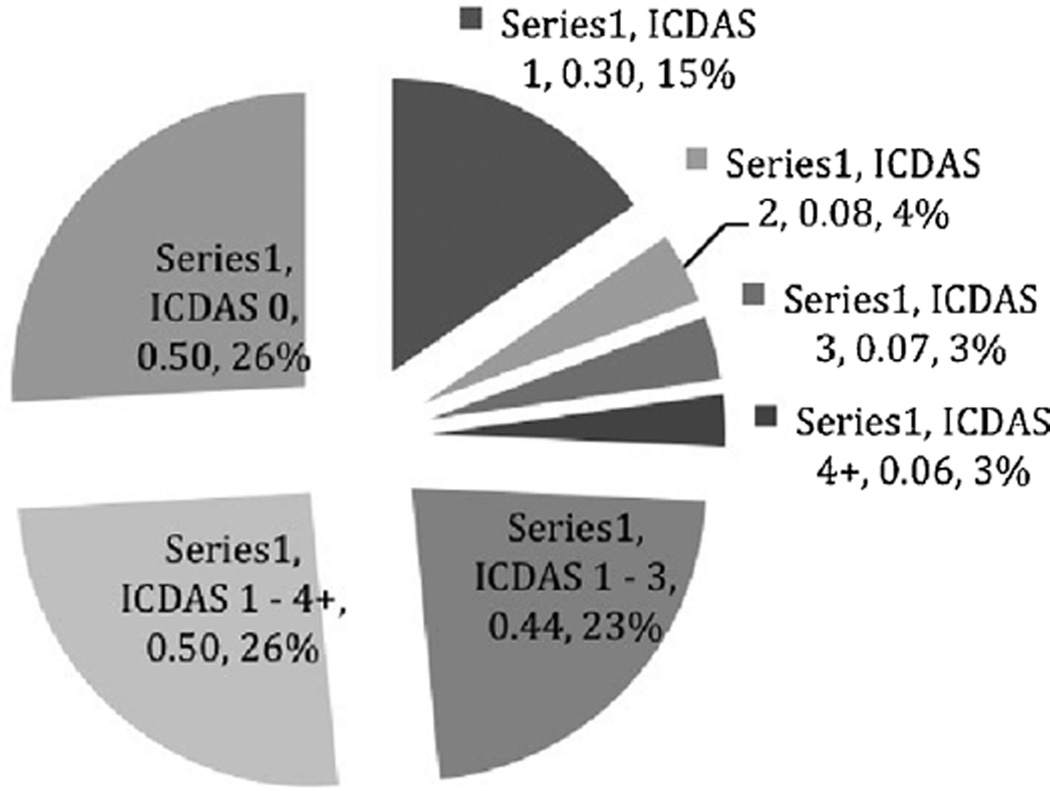
A total of 72 subjects were recruited. The sample was 63.9% female; 55.6% of subjects were between the ages of 65–74 years (the remainder were older), and 75.0% were white (Table 1). In 25% of subjects (n = 18) no teeth were scored by ICDAS or OCT as subjects were edentulous (11.1%, n = 8) or had no unrestored coronal pits/fissures (13.9%) and, therefore, no areas suitable for imaging. Almost half (44%) of unrestored posterior teeth in our population demonstrated signs of early dental caries (ICDAS 1–3), most of which were ICDAS 1 (Fig. 1).
TABLE 1.
Description of Subject Population
| Site 1 | Site 2 | Site 3 | Total | |||||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | |
| Gender | ||||||||
| F | 15 | 62.5 | 31 | 73.8 | 0 | 0.0 | 46 | 63.9 |
| M | 9 | 37.5 | 11 | 26.2 | 6 | 100.0 | 26 | 36.1 |
| Total | 24 | 100.0 | 42 | 100.0 | 6 | 100.0 | 72 | 100.0 |
| Age | ||||||||
| 65–74 | 24 | 100.0 | 11 | 26.2 | 5 | 83.3 | 40 | 55.6 |
| 75+ | 0 | 0.0 | 31 | 73.8 | 1 | 16.7 | 32 | 44.4 |
| Total | 24 | 100.0 | 42 | 100.0 | 6 | 100.0 | 72 | 100.0 |
| Race/ethnicity | ||||||||
| Asian | 1 | 4.2 | 1 | 2.4 | 3 | 50.0 | 5 | 6.9 |
| Black | 0 | 0.0 | 3 | 7.1 | 0 | 0.0 | 3 | 4.2 |
| Hispanic | 0 | 0.0 | 0 | 0.0 | 1 | 16.7 | 1 | 1.4 |
| Other | 0 | 0.0 | 9 | 21.4 | 0 | 0.0 | 9 | 12.5 |
| White | 23 | 95.8 | 29 | 69.0 | 2 | 33.3 | 54 | 75.0 |
| Total | 24 | 100.0 | 42 | 100.0 | 6 | 100.0 | 72 | 100.0 |
Site 1: a retirement community, Site 2: a convalescent hospital, Site 3: a senior health fair.
Fig. 1.
Mean proportion of decayed teeth per subject, adjusted to number of teeth scored.
Comparison of OCT-Based Diagnosis and ICDAS
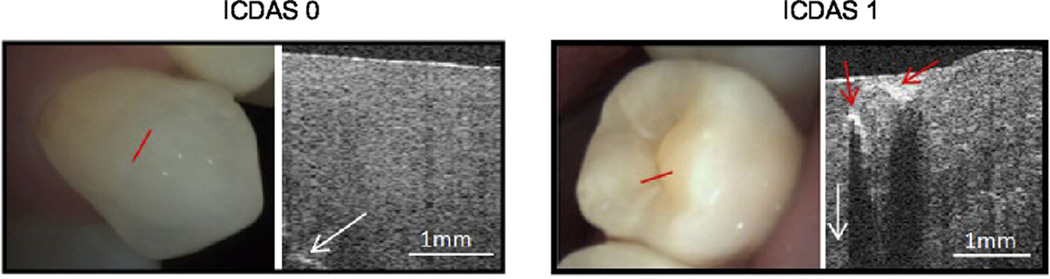
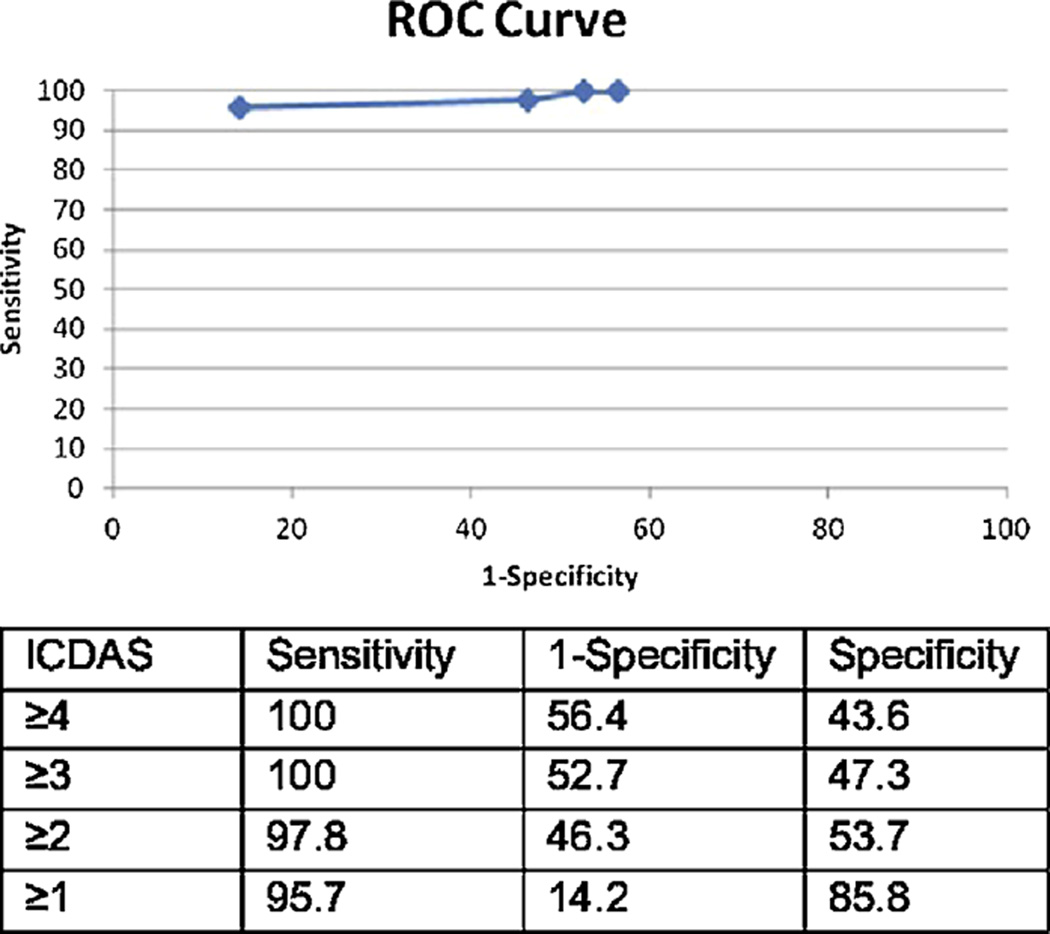
OCT-based diagnosis demonstrated very good sensitivity (97/102 = 95.1%) for correctly identifying early decayed teeth (ICDAS 1+ICDAS 2) and good specificity (91/106 = 85.8%) for correctly identifying sound teeth (Table 2). A total of 106 teeth that were clinically scored as sound (ICDAS 0) were imaged using OCT. Eighty-six percent (n = 91) were correctly classified as healthy by OCT imaging, and 15 teeth were classified as decayed using OCT data (Fig. 3). A total of 71 teeth were scored as very early caries (ICDAS 1). Ninety-four percent (n = 67) were correctly classified by OCT evaluation as decayed and four were classified as sound based on OCT data. An ROC curve (Fig. 2) demonstrates that OCT assessment demonstrated good sensitivity, but specificity varied depending on how tooth decay was defined. This is consistent with a cut-off point separating sound and decayed teeth (Fig. 3).
TABLE 2.
OCT Diagnosis Versus ICDAS-II Score by Individual Teeth (Includes Only OCT-Imaged Teeth)
| ICDAS Score | ||||||
|---|---|---|---|---|---|---|
| 0 (Sound) | 1 (Very early decay) | 2 (Early decay) | 3 (Enamel decay) | 4+ (Dentinal decay) | Total | |
| OCT | % (n) | % (n) | % (n) | % (n) | % (n) | % (n) |
| Healthy | 85.8 (91) | 5.6 (4) | 3.8 (1) | 0 (0) | 0 (0) | 43.0 (96) |
| Decayed | 14.2 (15) | 94.4 (67) | 96.2 (25) | 100.0 (17) | 100.0 (3) | 57.0 (127) |
| Total | 100.0 (106) | 100.0 (71) | 100.0 (26) | 100.0 (17) | 100.0 (3) | 100.0 (223) |
Fig. 3.
Cross-sectional OCT images of healthy (ICDAS 0) and demineralized (ICDAS 1) tooth. Imaging scan line shown in red. Dentin enamel junction (DEJ) is indicated by the white arrow. Area of increased reflectivity (brightness) indicates demineralization. Underlying dark shadow is due to increased light reflection from the lesion above, causing reduced light access to underlying area.
Fig. 2.
ROC curve comparing ICDAS and OCT-based diagnosis.
DISCUSSION
Integration of dental caries management into non-dental primary care practice requires easy, fast, and accurate early caries detection tools as an alternative to the current standard visual-tactile exam. It is particularly important to be able to identify areas of early caries (ICDAS 1 and 2) that may benefit from caries prevention strategies (e.g., fluoride application and dental sealants) to arrest or reverse caries progression; and to detect the non-visible changes indicate caries progression. Caries detection methods such as radiographs, fiber-optic transillumination (FOTI), fluorescence-based methods (DIAGNOdent), and electrical conductivity lack adequate specificity for enamel lesions [16] and can lead to false positives as well as over treatment [13]. Cone-beam computer tomograms offer good sensitivity for early occlusal and interproximal lesions [42] but expose patients to ionizing radiation and are expensive [43]. In this study, an OCT-imaging approach demonstrated good accuracy with very good sensitivity and good specificity for demineralization (early caries), even in non-traditional dental settings (a recreational room at a community center and patient rooms at a convalescent center) when ICDAS-II was used as the gold standard.
Simple diagnostic modalities that provide direct guidance with regard to triage and follow-up needs would greatly enhance the potential for successful community-based dental caries screening and prevention interventions in the elderly. Moreover, they would permit evaluation and comparison of the preventive efficacy of diverse approaches. This is particularly important as effective dental caries preventive strategies for older adults have not yet been definitively established [1,14,15,44–51]. Such modalities could then be integrated into eHealth systems to monitor at risk areas for changes, identify the effectiveness of non-invasive dental caries preventive interventions, and support collaborative efforts between non-dental and dental health professionals to facilitate dental decay management
Early decay is highly prevalent on the coronal surfaces of teeth in independent living adults aged 65+ years. Our sample had a higher prevalence of edentulousness (11.1%) than the national average (5%) and a higher prevalence of untreated tooth decay [52]. More than 48.6% of our sample population evidenced at least one posterior tooth surface with early decay (ICDAS 1–3). Nationally, 17.07% of adults 65–74 years are reported to have untreated tooth decay and 19.52% of adults 75+ years [52]. This disparity likely reflects the fact that the national survey (NHANES) does not record very early caries, whereas this parameter was the primary target of our study. In our sample, 54.7% of dentate subjects had at least one tooth with very early caries (ICDAS 1), though many of these lesions were stained, leaving the lesion activity status undefined. A limitation of this study was the lack of air-drying of subjects’ teeth, which might affect the ability of ICDAS criteria to detect early white (and thus likely active) ICDAS 1 lesions. Stained and brown occlusal ICDAS 1 lesions may be arrested. Stained lesions may become active if the oral environment changes associated with aging (e.g., medication-induced xerostomia, reduced manual dexterity, difficulty chewing, and swallowing). If these lesions are detected early, integration of non-invasive caries management strategies such as dietary and behavioral counseling (avoidance of cariogenic beverages and foods), topical fluoride (fluoridated water, toothpaste, mouthrinse, gels, and varnish), and/or dental sealants may be able to prevent these very early lesions from progressing to the stage where surgical excision and tissue replacement are necessary. Such early interventions can greatly reduce health care trauma, time, and cost. Moreover, the provision of invasive dental treatment such as restorations, crowns, endodontic therapy, and extractions for older adults can be particularly difficult due to diminished function, financial limitations, psychological and biological status, and transportation or access barriers [53].
In this study, an OCT -imaging based approach was evaluated for its potential usefulness in screening for early caries in non-traditional dental settings. Diagnostic accuracy was very good. However, currently available OCT devices tend to be too costly and cumbersome for routine use in a community-based setting, and specific caries-diagnostic software remains unavailable to the best of our knowledge. Additionally, the OCT probe sheath’s length and inflexibility make it difficult to examine all the dental surfaces that clinicians may need to assess. Thus, although this study has demonstrated an urgent need for effective community-based caries screening in the elderly, the good performance of the OCT modality tested is offset by the lack of clinic-ready instrumentation. Hopefully, technological advances will serve to overcome these barriers in the near future. Improved identification of early caries lesions should not result in over treatment any more than any other form of diagnosis when it is used correctly. Rather, it should provide clinicians with a means of implementing non-invasive preventive interventions before permanent damage has occurred and permit monitoring of measures to arrest caries.
CONCLUSION
Early decay is prevalent in the unrestored pits and fissures of coronal surfaces of teeth in independent living adults aged 65+ years. Integration of oral health screening and prevention interventions with health care is key to improving oral health in the elderly. OCT imaging coupled with a simple diagnostic algorithm can accurately detect areas of very early caries. This ability could provide a means of identifying prevention intervention needs, facilitating the provision of successful preventive care (fluoride gels and varnishes) in the elderly. Effective prevention would combat lesion progression and reduce the need for invasive restorative measures. Only evidence of lesion progression during subsequent follow-up events would indicate the need for a dental referral. Thus, OCT technologies have the potential for improving screening and prevention capabilities for dental decay. However, existing OCT devices are expensive, bulky, and not well suited for use by non-dental health care providers. Simple, inexpensive, fast, and accurate tools for early caries detection by field health care providers working in nontraditional settings are urgently needed to improve dental health management in independent, non-frail elderly.
Acknowledgments
Contract grant sponsor: LAMMP; Contract grant number: NIH P41EB015890; Contract grant sponsor: ASLMS; Contract grant sponsor: The Beckman Foundation; Contract grant number: NIH R03EB014852.
Footnotes
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
REFERENCES
- 1.Saunders RH, Jr, Meyerowitz C. Dental caries in older adults. Dent Clin North Am. 2005;49(2):293–308. doi: 10.1016/j.cden.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 2.Ettinger RL. The unique oral health needs of an aging population. Dent Clin North Am. 1997;41(4):633–649. [PubMed] [Google Scholar]
- 3.Health, United States, 2012: With Special Feature on Emergency Care. Hyattsville, MD: National Center for Health Statistics; 2013. [PubMed] [Google Scholar]
- 4.Griffin SO, Griffin PM, Swann JL, Zlobin N. Estimating rates of new root caries in older adults. J Dent Res. 2004;83(8):634–638. doi: 10.1177/154405910408300810. [DOI] [PubMed] [Google Scholar]
- 5.Hand JS, Hunt RJ, Beck JD. Coronal and root caries in older Iowans: 36-month incidence. Gerodontics. 1988;4(3):136–139. [PubMed] [Google Scholar]
- 6.Thomson WM. Dental caries experience in older people over time: What can the large cohort studies tell us? Br Dent J. 2004;196(2):89–92. doi: 10.1038/sj.bdj.4810900. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS) Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 1992. National Health and Nutrition Examination Survey III Oral Examination Protocol. http://www.cdc.gov/nchs/data/nhanes/nhanes3/cdrom/nchs/manuals/dental.pdf. section 5.6.3. [Google Scholar]
- 8.Ekstrand KR, Ricketts DN, Kidd EA, Qvist V, Schou S. Detection. Diagnosing, monitoring and logical treatment of occlusal caries in relation to lesion activity and severity: An in vivo examination with histological validation. Caries Res. 1998;32(4):247–254. doi: 10.1159/000016460. [DOI] [PubMed] [Google Scholar]
- 9.Makhija SK, Gilbert GH, Funkhouser E, Bader JD, Gordan VV, Rindal DB, Qvist V, Nørrisgaard P National Dental PBRN Collaborative Group. Twenty-month follow-up of occlusal caries lesions deemed questionable at baseline: Findings from The National Dental Practice-Based Research Network. J Am Dent Assoc. 2014;145(11):1112–1118. doi: 10.14219/jada.2014.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vujicic M. Health care reform brings new opportunities. J Am Dent Assoc. 2014;145(4):381–382. doi: 10.14219/jada.2014.16. [DOI] [PubMed] [Google Scholar]
- 11.Institute of Medicine (U.S.) Advancing oral health in America. Washington, DC: National Academies Press; 2011. Committee on an Oral Health Initiative. [Google Scholar]
- 12.Integration of Oral Health and Primary Care Practice: Health Resources and Services Administration. 2014 [Google Scholar]
- 13.Holtzman JS, Ballantine J, Fontana M, et al. Assessment of early occlusal caries pre- and post- sealant application-An imaging approach. Lasers Surg Med. 2014 doi: 10.1002/lsm.22249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Twetman S, Fontana M. Patient caries risk assessment. Monogr Oral Sci. 2009;21:91–101. doi: 10.1159/000224214. [DOI] [PubMed] [Google Scholar]
- 15.Rodrigues JA, Lussi A, Seemann R, Neuhaus KW. Prevention of crown and root caries in adults. Periodontol 2000. 2011;55(1):231–249. doi: 10.1111/j.1600-0757.2010.00381.x. [DOI] [PubMed] [Google Scholar]
- 16.Caries Management - Science and Clinical Practice. Stuttgart: Thieme Medical Publishers; 2013. [Google Scholar]
- 17.Shimada Y, Sadr A, Burrow MF, Tagami J, Ozawa N, Sumi Y. Validation of swept-source optical coherence tomography (SS-OCT) for the diagnosis of occlusal caries. J Dent. 2010;38(8):655–665. doi: 10.1016/j.jdent.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 18.Kang H, Jiao JJ, Lee C, Le MH, Darling CL, Fried D. Nondestructive assessment of early tooth demineralization using cross-polarization optical coherence tomography. IEEE J Sel Top Quantum Electron. 2010;16(4):870–876. doi: 10.1109/JSTQE.2009.2033610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mendes FM, Novaes TF, Matos R, Bittar DG, Piovesan C, Gimenez T, Imparato JC, Raggio DP, Braga MM. Radiographic and laser fluorescence methods have no benefits for detecting caries in primary teeth. Caries Res. 2012;46(6):536–543. doi: 10.1159/000341189. [DOI] [PubMed] [Google Scholar]
- 20.Ekstrand KR, Ricketts DN, Kidd EA. Reproducibility and accuracy of three methods for assessment of demineralization depth of the occlusal surface: An in vitro examination. Caries Res. 1997;31(3):224–231. doi: 10.1159/000262404. [DOI] [PubMed] [Google Scholar]
- 21.Ferreira Zandoná A, Santiago E, Eckert GJ, Katz BP, Pereira de Oliveira S, Capin OR, Mau M, Zero DT. The natural history of dental caries lesions: A 4-year observational study. J Dent Res. 2012;91(9):841–846. doi: 10.1177/0022034512455030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rodrigues JA, Hug I, Diniz MB, Lussi A. Performance of fluorescence methods, radiographic examination and ICDAS II on occlusal surfaces in vitro. Caries Res. 2008;42(4):297–304. doi: 10.1159/000148162. [DOI] [PubMed] [Google Scholar]
- 23.Gomez J, Zakian C, Salsone S, Pinto SC, Taylor A, Pretty IA, Ellwood R. In vitro performance of different methods in detecting occlusal caries lesions. J Dent. 2013;41(2):180–186. doi: 10.1016/j.jdent.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 24.Le MH, Darling CL, Fried D. Automated analysis of lesion depth and integrated reflectivity in PS-OCT scans of tooth demineralization. Lasers Surg Med. 2010;42(1):62–68. doi: 10.1002/lsm.20862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Louie T, Lee C, Hsu D, Hirasuna K, Manesh S, Staninec M, Darling CL, Fried D. Clinical assessment of early tooth demineralization using polarization sensitive optical coherence tomography. Lasers Surg Med. 2010;42(10):738–745. doi: 10.1002/lsm.21013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Baumgartner A, Dichtl S, Hitzenberger CK, Sattmann H, Robl B, Moritz A, Fercher AF, Sperr W. Polarization-sensitive optical coherence tomography of dental structures. Caries Res. 2000;34(1):59–69. doi: 10.1159/000016571. [DOI] [PubMed] [Google Scholar]
- 27.Douglas SM, Fried D, Darling CL. Imaging natural occlusal caries lesions with optical coherence tomography. Proc Soc Photo Opt Instrum Eng. 2010;7549:75490N. doi: 10.1117/12.849344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kang H, Jiao JJ, Lee C, Darling CL, Fried D. Imaging early demineralization with PS-OCT. Proc Soc Photo Opt Instrum Eng. 2010:75490M. doi: 10.1117/12.849343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Holtzman JS, Osann K, Pharar J, Lee K, Ahn YC, Tucker T, Sabet S, Chen Z, Gukasyan R, Wilder-Smith P. Ability of optical coherence tomography to detect caries beneath commonly used dental sealants. Lasers Surg Med. 2010;42(8):752–759. doi: 10.1002/lsm.20963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kühnisch J, Berger S, Goddon I, Senkel H, Pitts N, Heinrich-Weltzien R. Occlusal caries detection in permanent molars according to WHO basic methods, ICDAS II and laser fluorescence measurements. Community Dent Oral Epidemiol. 2008;36(6):475–484. doi: 10.1111/j.1600-0528.2008.00436.x. [DOI] [PubMed] [Google Scholar]
- 31.Jones RS, Fried D. Remineralization of enamel caries can decrease optical reflectivity. J Dent Res. 2006;85(9):804–808. doi: 10.1177/154405910608500905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ibusuki T, Kitasako Y, Sadr A, Shimada Y, Sumi Y, Tagami J. Observation of white spot lesions using swept source optical coherence tomography (SS-OCT): In vitro and in vivo study. Dent Mater J. 2015;34(4):545–552. doi: 10.4012/dmj.2015-058. [DOI] [PubMed] [Google Scholar]
- 33.Wada I, Shimada Y, Ikeda M, Sadr A, Nakashima S, Tagami J, Sumi Y. Clinical assessment of non carious cervical lesion using swept-source optical coherence tomography. J Biophotonics. 2014;9999(9999) doi: 10.1002/jbio.201400113. [DOI] [PubMed] [Google Scholar]
- 34.Lenton P, Rudney J, Fok A, Jones RS. Clinical cross-polarization optical coherence tomography assessment of subsurface enamel below dental resin composite restorations. J Med Imaging (Bellingham) 2014;1(1):016001. doi: 10.1117/1.JMI.1.1.016001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fried D, Staninec M, Darling CL, Chan KH, Pelzner RB. Clinical monitoring of early caries lesions using cross polarization optical coherence tomography. Proc SPIE Int Soc Opt Eng. 2013;8566 doi: 10.1117/12.2011014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nee A, Chan K, Kang H, Staninec M, Darling CL, Fried D. Longitudinal monitoring of demineralization peripheral to orthodontic brackets using cross polarization optical coherence tomography. J Dent. 2014;42(5):547–555. doi: 10.1016/j.jdent.2014.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shimada Y, Nakagawa H, Sadr A, Wada I, Nakajima M, Nikaido T, Otsuki M, Tagami J, Sumi Y. Noninvasive cross-sectional imaging of proximal caries using swept-source optical coherence tomography (SS-OCT) in vivo. J Biophotonics. 2014;7(7):506–513. doi: 10.1002/jbio.201200210. [DOI] [PubMed] [Google Scholar]
- 38.Lenton P, Rudney J, Chen R, Fok A, Aparicio C, Jones RS. Imaging in vivo secondary caries and ex vivo dental biofilms using cross-polarization optical coherence tomography. Dent Mater. 2012;28(7):792–800. doi: 10.1016/j.dental.2012.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fried D, Staninec M, Darling CL, Lee C, Kang H, Chan KH. In vivo Near-IR Imaging of Occlusal Lesions at 1310-nm. Proc SPIE Int Soc Opt Eng. 2011;7884(78840B) doi: 10.1117/12.878888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Feldchtein F, Gelikonov V, Iksanov R, Gelikonov G, Kuranov R, Sergeev A, Gladkova N, Ourutina M, Reitze D, Warren J. In vivo OCT imaging of hard and soft tissue of the oral cavity. Opt Express. 1998;3(6):239–250. doi: 10.1364/oe.3.000239. [DOI] [PubMed] [Google Scholar]
- 41.International Caries Detection and Assessment System (ICDAS) Coordinating Committee. Rational and Evidence for the International Caries Detection and Assessment System (ICDASII). In: Stookey GK, editor. Early detection of dental caries: proceedings of the 2005 Indiana conference; Indiana University; Indianapolis. 2007. [Google Scholar]
- 42.Krzyzostaniak J, Surdacka A, Kulczyk T, Dyszkiewicz-Konwinska M, Owecka M. Diagnostic accuracy of cone beam computed tomography compared with intraoral radiography for the detection of noncavitated occlusal carious lesions. Caries Res. 2014;48(5):461–466. doi: 10.1159/000358101. [DOI] [PubMed] [Google Scholar]
- 43.Sansare K, Singh D, Sontakke S, Karjodkar F, Saxena V, Frydenberg M, Wenzel A. Should cavitation in proximal surfaces be reported in cone beam computed tomography examination? Caries Res. 2014;48(3):208–213. doi: 10.1159/000354838. [DOI] [PubMed] [Google Scholar]
- 44.Axelsson S, Söder B, Nordenram G, Petersson LG, Dahlgren H, Norlund A, Källestål C, Mejàre I, Lingström P, Lagerlöf F, Holm AK, Twetman S. Effect of combined caries-preventive methods: Asystematic review of controlled clinical trials. Acta Odontol Scand. 2004;62(3):163–169. doi: 10.1080/00016350410006842. [DOI] [PubMed] [Google Scholar]
- 45.Hujoel PP, Cunha-Cruz J, Banting DW, Loesche WJ. Dental flossing and interproximal caries:A systematic review. J Dent Res. 2006;85(4):298–305. doi: 10.1177/154405910608500404. [DOI] [PubMed] [Google Scholar]
- 46.Mjor IA, Holst D, Eriksen HM. Caries and restoration prevention. J Am Dent Assoc. 2008;139(5):565–570. doi: 10.14219/jada.archive.2008.0216. quiz 626. [DOI] [PubMed] [Google Scholar]
- 47.Gore DR. The use of dental sealants in adults: A long-neglected preventive measure. Int J Dent Hyg. 2010;8(3):198–203. doi: 10.1111/j.1601-5037.2009.00425.x. [DOI] [PubMed] [Google Scholar]
- 48.Sambunjak D, Nickerson JW, Poklepovic T, Johnson TM, Imai P, Tugwell P, Worthington HV. Flossing for the management of periodontal diseases and dental caries in adults. Cochrane Database Syst Rev. 2011;(12):CD008829. doi: 10.1002/14651858.CD008829.pub2. [DOI] [PubMed] [Google Scholar]
- 49.Chalmers JM, Ettinger RL. Public health issues in geriatric dentistry in the United States. Dent Clin North Am. 2008;52(2):423–446. vii–viii. doi: 10.1016/j.cden.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 50.Griffin SO, Regnier E, Griffin PM, Huntley V. Effectiveness of fluoride in preventing caries in adults. J Dent Res. 2007;86(5):410–415. doi: 10.1177/154405910708600504. [DOI] [PubMed] [Google Scholar]
- 51.Longbottom C, Ekstrand K, Zero D. Traditional preventive treatment options. Monogr Oral Sci. 2009;21:149–155. doi: 10.1159/000224219. [DOI] [PubMed] [Google Scholar]
- 52.Dye BA, Tan S, Smith V, Lewis BG, Barker LK, Thornton-Evans G, Eke PI, Beltrán-Aguilar ED, Horowitz AM, Li CH. Trends in oral health status: United States, 1998–1994 and 1999–2004. National Center for Health Statistics. Vital Health Stat. 2007;11(248) [PubMed] [Google Scholar]
- 53.Daniel SJ, Kumar S. Teledentistry: A key component in access to care. J Evid Based Dent Pract. 2014;14:201–218. doi: 10.1016/j.jebdp.2014.02.008. [DOI] [PubMed] [Google Scholar]