Abstract
Purpose
No prismatic solution for peripheral field loss (PFL) has gained widespread acceptance. Field extended by prisms has a corresponding optical scotoma at the prism apices. True expansion can be achieved when each eye is given a different view (through visual confusion). We analyze the effects of apical scotomas and binocular visual confusion in different designs to identify constraints on any solution that is likely to meet acceptance.
Methods
Calculated perimetry diagrams were compared to perimetry with PFL patients wearing InWave channel prisms and Trifield spectacles. Percept diagrams illustrate the binocular visual confusion.
Results
Channel prisms provide no benefit at primary gaze. Inconsequential extension was provided by InWave prisms, although accessible with moderate gaze shifts. Higher-power prisms provide greater extension, with greater paracentral scotoma loss, but require uncomfortable gaze shifts. Head turns, not eye scans, are needed to see regions lost to the apical scotomas. Trifield prisms provide field expansion at all gaze positions, but acceptance was limited by disturbing effects of central binocular visual confusion.
Conclusions
Field expansion when at primary gaze (where most time is spent) is needed while still providing unobstructed central vision. Paracentral multiplexing prisms we are developing that superimpose shifted and see-through views may accomplish that.
Translational Relevance
Use of the analyses and diagramming techniques presented here will be of value when considering prismatic aids for PFL, and could have prevented many unsuccessful designs and the improbable reports we cited from the literature. New designs must likely address the challenges identified here.
Keywords: low vision rehabilitation, prism treatment, perimetry, visual field loss, tunnel vision, retinitis pigmentosa
Introduction
Conditions such as retinitis pigmentosa (RP), choroideremia, and glaucoma shrink the available visual field diameter. Mobility becomes a problem, as both orientation (way finding) and awareness of hazards (safety) become difficult. Many patients do not notice the loss until their central field diameter shrinks below about 40°, and the effects are severe below about 20°, which is commonly the criterion for legal blindness due to peripheral field loss (PFL). Nonprismatic minifying aids, like reversed telescopes and amorphic lenses, have limitations that have impacted their acceptance,1–6 principal among which is the loss of resolution (acuity). They are not considered in this article. A few styles of prism spectacles have been introduced to aid people with this loss, but there has been little long-term acceptance of these aids by patients, and we have found no reliable evidence that they improved (or did not negatively impact) patient safety. Using two very different, but representative, configurations as examples, InWave channel prisms7 and our Trifield design,8,9 we analyze the limitations that various prismatic effects represent in these devices that may largely account for their limited acceptance. We conclude by identifying constraints that any prismatic solution should likely overcome to gain better utility and wider acceptance. Prisms may be beneficial when searching for misplaced objects, which is also challenging for these patients, but here we deal only with mobility safety issues.
Diagramming techniques we developed for analyzing prism effects for hemianopic field loss (HFL)10 yield substantially different conclusions when applied here for PFL because of the enormous difference in the size of the residual field. While HFL is a loss of just 50% of the normal binocular visual field, a patient with a residual field of 20° diameter has only about 1.5% of the normal visual field, and one with 10° residual field has only about 0.4%. This severely limits the area that can be expanded with prisms. When reviewing reports of prior application of prisms for PFL, we found many with results that are unsupportable based on the optical configurations employed or the unrealistic eye movements they required. Use of analytical tools together with confirming perimetry, as applied here, could have provided insight into just how the world would look to the patient through the devices and what demands the devices placed on the patient's visual system. Such analyses could likely have avoided ineffective (and possibly dangerous) prescriptions.
The detailed analyses here of well-intentioned but largely unsuccessful prism glasses are not meant to aid clinicians in dispensing those devices, nor are the patients who wore the devices to validate our geometric results representative users or case studies for the configurations we used. Our purpose has been to gain insights into why these approaches did not succeed and help develop the criteria that future configuration will likely need to satisfy if they are to meet the challenge of PFL.
When the apex of a prism is placed within view, there is a discontinuity and a resulting unseen region in the available field of view, between the last undeviated ray at the apex and the first ray deflected within the prism. This “prism jump” is due to the apical scotoma. See figure 1 in Apfelbaum et al.10 for illustrations of the apical scotoma and its formation. This scotoma is a gap in the view of the scene, not a gap in retinal response. The gap is equal in size to the effective power of the prism at its apex. Thus a prism loses as much field of view at its apex as it gains at its base (if we ignore the gradual magnification distortion described in Jung and Peli11). We use the term field extension to describe this sort of field substitution, reserving the term field expansion for a true increase in the total field area in view. We only use the term awareness when citing its use in the literature, to describe the goal prisms are intended to achieve, even though this is an imprecise concept, generally not measurable, and certainly not predicted by perimetry.
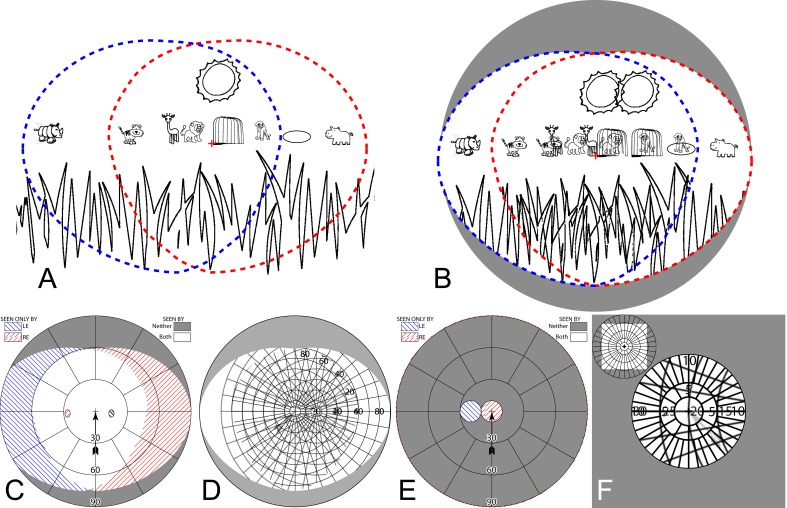
Figure 1.
Visual confusion and diplopia. (A) A savannah cartoon. The blue and red dashed outlines represent the field of view of the left eye (LE) and right eye (RE), respectively, when a 20° shift is provided by a full-lens base-out prism (∼36Δ) in front of the LE. The red cross (not part of the scene) marks the fixation location of the nonprism RE. (B) The way this scene appears in the binocular visual field of an observer with no visual field loss. Everything within the intersection of the blue and red outlines in (A) is seen diplopically (i.e., at two apparent locations), while everything within the intersection of the red and blue outlines in (b) is seen with visual confusion (superposition of different images at the same apparent direction). Thus the LE view of the lion overlaps the RE view of the cage, the LE view of the cage has captured the RE view of the cub, and the giraffe is now prey for the lion and tiger. The LE is bathing the cub in the RE's pond, but the hippo is no closer to bathing in the pond since both pond and hippo are only seen by the RE. Thus the pond is seen in confusion but not diplopia, while the hippo and rhino are seen without confusion or diplopia. Although the tiger is seen in a region with visual confusion, there happens to be no conflicting RE salient image at that location. Visual confusion is primarily a problem only when salient images appear in both eyes at corresponding retinal locations (directions), and is more disturbing centrally than in the periphery. Diplopia is always noticeable, but more disturbing centrally than in the periphery. (C) Calculated dichoptic perimetry for this configuration. By convention, the diagram is limited to a radius of 90°, as is a Goldmann perimeter, although the field of view in this case actually extends left to 110°. Note the direct relationship between (A) and (C), with everything in the central white area of (C) seen diplopically. (D) The corresponding percept diagram10 identifies visual confusion, as shown by the superimposed images representing the view of a perimetry grid seen by each eye. LE views are blurred slightly to distinguish them and represent the loss of optical quality through the prism, and the light gray arrow (not part of the patient's percept) points to fixation in these percept diagrams. Note the direct relationship between (B) and (D). (E) Calculated perimetry for a patient with 20° residual visual fields and the same prism configuration. Since entirely different portions of the scene are viewed by each eye, there is no diplopia. (F) The corresponding percept diagram10 (with just the central portion of interest shown). There is visual confusion everywhere. Thus with PFL, confusion without diplopia is possible, allowing for field of view expansion without diplopia. (Diplopia without visual confusion is a possibility in cases of bitemporal or binasal hemianopia with phorias.12)
When fitting prisms, the field lost at the prism apex should be considered, as it may affect the wearer's function and safety at least as much as the view gained by the prism shift. Fitting prisms over only one lens can allow the fellow eye to see regions lost to the apical scotomas, and thus provide true field expansion. However, this double vision causes binocular visual confusion (seeing two different objects in the same direction; Fig. 1). Improperly designed unilateral fitting can even cause diplopia (perceiving the same object in two different directions; Fig. 1), as can improper alignment of bilaterally fitted prisms.10 Diplopia can and should decidedly be avoided (at least centrally), as it represents a problem without any benefit, while confusion carries the benefit of field expansion. Thus the location of the prism apex and the effects of unilateral and bilateral fitting (as well as prism power) all figure into the results that can be expected for the patient at different positions of gaze. The effects of all these parameters can be calculated and diagrammed. Throughout, we distinguish the regions of the external scene (“the scene”) made available with these devices from the portions of the retina upon which the images fall and can be perceived, using the term “field of view” for the former and “visual field” for the latter. Thus, prisms may increase the field of view, but not the visual field. As shown in Figure 1, perimetry maps field of view, and only corresponds to visual field if the resulting images on both retinas are aligned. Goldmann perimetry does not detect visual confusion, since stimuli are only presented to one location in the field of view at a time. It can identify diplopia if the patient is asked to report it (as was done in Jung and Peli11). The percept diagrams introduced in Apfelbaum et al.,10 readily show visual confusion. See figure 2 in that article for a more detailed explanation of these diagrams.
The InWave channel prism design used three prism segments on each carrier lens, and was recommended to be used bilaterally.7 The full design was marketed in the late 1990s, using molded lenses, as the InWave (Janesville, WI) channel prism lens blanks. A patient's prescription was ground into the back surface of these lenses, making for a very attractive product cosmetically. The term “channel” refers to the nonprismatic area of the carrier lens that extends from just below the residual visual field at primary gaze to the top of the lens (Fig. 2B). 12Δ prisms to the left and right of the channel with apices tangent to the channel (temporal base out, nasal base in) were intended to provide lateral field “awareness,” while an 8Δ base-down prism with apex tangent to the bottom of the channel and flaring outward from there by about 60° was intended to provide awareness of floor-level obstacles along the patient's path. The channel prism configuration is still available from Chadwick Optical (Souderton, PA) with prism powers up to 25Δ. A compound lens is constructed from four separate ophthalmic prism lens segments glued together (Fig. 2A). Bifocal add can be applied to the lower prisms. Practitioners have also used Press-On™ Fresnel prisms (3M, Minneapolis, MN) to implement the channel design, with powers generally not exceeding 20Δ (but 40Δ illustrated for clarity in Fig. 2C). In all channel prism designs the prisms are not in view at primary gaze, so field extension is only provided when gaze is shifted into the prisms.
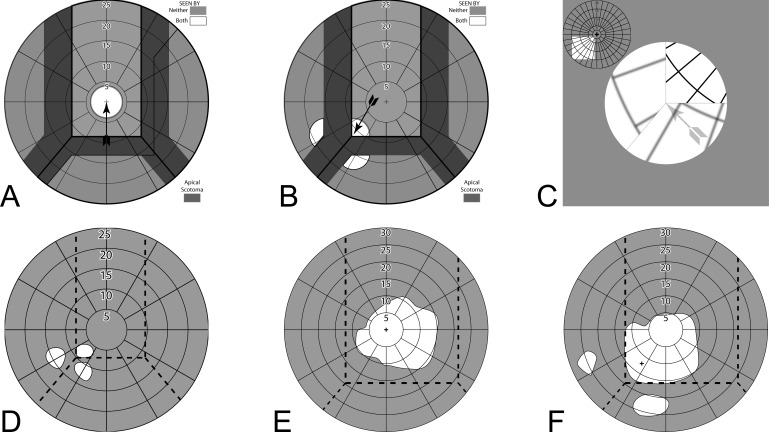
Figure 2.
Channel prisms. (A) Channel prism lens available from Chadwick Optical. There are three sector prisms per carrier lens, with the apices outside the borders of the patient's functional field when at primary gaze. In this case, the lateral prisms are 12Δ, base-in and base-out, on the nasal and temporal side, respectively, and the lower prisms are 8Δ, base-down, matching the configuration and prism powers that were used by InWave. Note the break in the visibility of the spectacles' temples due to the apical scotomas. (B) Photo through a molded InWave channel prism trial lens. A polar grid with 5° radius increments is seen through the lens. The channel width is 6 mm (17°), the smallest offered by InWave. Note that the central circle in the grid is 10° in diameter. Approximately 6° laterally are lost to each of the left and right prisms' apical scotomas to achieve a corresponding lateral field substitution (extension, not expansion), and 4° lost to the lower scotoma, hiding sections of the original grid from view. (C) 6 mm channel lens fabricated using 40Δ 3M Press-On™ Fresnel prisms. High-power prisms have correspondingly large apical scotomas. (The spectacles are just a few millimeters from the paper, yet the apical scotoma changes each fox into an ox.)
The Peli Trifield prism spectacles9,13 were developed to provide field expansion at all gaze positions. Prisms are fit monocularly, leaving the fellow eye with its natural views and able to compensate for the apical scotomas. Two horizontal sector prisms are used on the nondominant eye, apex-to-apex, with the apices at the pupil position in primary gaze (Fig. 3). Thus, at primary gaze there are three (hence “Trifield”) views; the unaided view of the dominant eye plus left and right views shifted through the prisms.
Figure 3.

Trifield prism spectacles. (A) Front view. (B) View from above. Tinted prisms aid in determining veridical direction of objects seen through them.
The impact of the apical scotoma has not been mentioned or addressed in much of the literature.1,6,14,15 Though “prism jump” is sometimes mentioned, it is generally in the context of its startle effect or to call attention to the nonveridical direction of the view through the prisms, not to raise awareness of the associated field loss.16,17 Some authors have addressed the apical scotoma; Cohen's18 illustrations show a field loss at the apex equal to the gain at the base. Tallman et al.19 advocate teaching the patient “to avoid the blind area” at the leading edge of the prism and “look through the central […] area of the carrier lens or […] look further into the Fresnel prism to avoid the leading edge.” However, eye movements shifting gaze farther into the prism do not provide a view of the field lost in the apical scotoma; only a head turn to move the prism and its apical scotoma position can do that (with the shifted scotoma then obscuring another part of the scene).
Finn et al.20 described training to familiarize the patient with the location and extent of the scotoma, and the need for head turns, not eye scans, to see in that area. Gadbaw et al.21 call attention to the “blind spot” at the apex but do not indicate its magnitude or mention the need for awareness of hazards that may lurk in that region of the scene. Bailey's22 analysis is an exception, with a clear discussion of the apical scotoma (as well as visual confusion and diplopia), primarily in the context of prisms for homonymous hemianopia, but equally applicable for PFL. Perlin and Dziadul23 call attention to the “blind area” during training and the need for a head turn to avoid it. Reports of problems with the apical scotomas are rare, but Hoppe and Perlin24 describe a 23-month prism user who discontinued prism use after “an episode in which he missed the handrail on a stair case due to the blind spot […] and almost tumbled down the stairs. In the same day, he hit his head on a pole in his pathway, again blaming the incident on the blind spot.”
Conventional perimetry is typically used to identify and monitor visual field loss due to pathological processes. Here, we use perimetry primarily to identify gaps (or gains) in the field of view caused by prisms (in addition to any loss of retinal or cortical function), as well as to identify diplopia. While a perimetry diagram identifies the actual direction of a stimulus that is seen, it does not indicate where it is perceived by the patient, nor can it identify visual confusion. Percept diagrams identify visual confusion and more directly represent the view the patient experiences. Diplopia and binocular confusion can materially affect the experience of wearing prismatic aids. Diplopia and confusion are particularly disturbing foveally or paracentrally, while they are well tolerated (indeed natural) farther in the periphery.25 Used together, as illustrated here, perimetry and percept diagrams provide a better insight into the value and challenges the prism aids create for the patient.
Methods
Synthesized perimetry and percept diagrams are scaled in degrees of visual angle (from the nodal point) and assume a cornea to nodal point distance (NPD) of 7.1 mm (per Gullstrand's Schematic Eye26) and spectacles with a back vertex distance (BVD) of 13 mm. Ocular rotation calculations assume a center of rotation 13.5 mm from the cornea. Prismatic secondary effects such as vignetting at the edges and optical spatial distortions are ignored. (For more on the distortions that are significant primarily for prisms with higher powers than used in the aids discussed here, see Jung and Peli.11) Informed consent was obtained from the two patients with PFL who wore prism glasses for the measured field diagrams. The patients were used to confirm the validity of our diagrams and predictions. Patient 1 had ∼8° binocular residual field diameter due to RP, and best corrected visual acuity 20/25. Patient 2, with optic nerve atrophy, was functionally monocular, with an asymmetric monocular residual field ∼30° horizontally and acuity of 20/500 in the better right eye. We note that since the patients were essentially instruments to confirm the predicted optical effects (which are independent of patient variables), testing with additional patients was unnecessary. All procedures were conducted in accordance with the tenets of the Declaration of Helsinki, and the protocol was approved by the Massachusetts Eye and Ear Human Studies Committee. Our computerized Dichoptic (central) Visual Field perimeter27 was used for these measurements, with a recent enhancement to support fixation locations offset from primary gaze (not readily achievable with a Goldmann perimeter, and needed for the measurements with averted gaze in the figures below). The screen distance from the subjects was 1 m. Bright (140 cd/m2) square stimuli presented over a dark background (0.2 cd/m2) were used in a standard kinetic perimetry procedure (moving from not seen to seen). The stimulus was 4.2 × 4.2 mm (0.25°) for patient 1 and 8.4 × 8.4 mm (0.5°) for patient 2. Due to the small angular differences of interest, to achieve finer resolution we used higher contrast and smaller stimuli than normal.
Whereas clinical perimetry is normally fairly insensitive to head position, when prisms or other devices are worn on the head or spectacles, slight shifts in head position can have large impacts on the resulting fields.28 Simply having the patient's head in a chin rest and brow bar allowed far too much movement and generally did not position the prisms at the needed alignment, nor ensure that head alignment (and thus prism location) would be maintained across trials with fixation at primary and shifted gaze positions. We added a tight head strap to aid the patient in maintaining position. This was not effortless for the patients, especially since the position involved turning and tilting somewhat away from the position the original restraints were designed to maintain.
To locate the trial channel prism edges (Fig. 2), the operator moved the stimulus laterally to the expected apex position of the left prism and the patient turned his head to split the stimulus at the edge. The operator then moved the stimulus to the expected apex position of the right prism, repeating this process until the patient's residual field was centered between the apices when gazing at the central fixation target. Then, the stimulus was moved to the expected edge position of the lower prism (a couple of degrees below the lower edge of the patient's residual field), and the patient adjusted head tilt to split the stimulus image, taking care to maintain the achieved rotation or tilt with the support of the head strap. Free eye movements (not fixation) were necessary and permitted during this process. This was repeated until the channel was appropriately centered symmetrically around the residual field (not necessarily the fovea) when at central fixation, and then confirmed by a “wiggle test” in which the stimulus was placed at a lower channel corner and the patient wiggled slightly in the restraints to confirm that slight lateral or vertical movements caused the stimulus to go in and out of view. Note that the center of the trial lens is thus not necessarily at the position of pupil center in primary gaze; rather it is centered on the residual field at central fixation. Due to the limited accuracy with which the trial lens and trial frames could be fitted on the patient and the resulting need for small head rotations and tilts in the apparatus to align the channel, central fixation was not necessarily precisely at the position of primary gaze.
For the 25Δ Trifield prisms, the stimulus was placed at the expected lateral offsets and the patient confirmed that the jump in and out of prism view occurred at that location. This was repeated until the left and right offsets were the same distance from central fixation, indicating that the apices were at the line of sight when the fellow eye was fixating.
Results
Channel Prisms
InWave provided trial lens sets with channel widths from 6 to 14 mm, in 2-mm increments (17°–38°, for our assumed NPD + BVD). They recommended close fitting of the prism apices to the patient's residual field, using a channel size of 8 mm or less for patients with residual field diameter 20° or less, and their 14-mm channel for patients with fields greater than 40° (which exceeds the 38° we calculate for the 14-mm channel).
Fresnel channel prisms have been used before, during, and after the availability of InWave prisms. Patients with 10° to 15° diameter visual fields or less, without residual peripheral islands, were usually considered good candidates for these prisms.20,23,29,30 Clinicians have opted for wider channels than recommended by InWave,20,23,29–31 generally using only temporal and nasal prism segments, primarily 20Δ. Some recommended placing the prism apices 2 to 5 mm outside of the patient's functional field (∼8–14° of ocular rotation with a residual field diameter of 10°),15,29–31 while others advocated placing the prism apices at a position such that as much as 20° of ocular rotation is required in order to gaze through the sector prisms (almost 10 mm from primary gaze).23 Channel prisms fabricated as in Figures 2A and 2C could accommodate these widely divergent fitting recommendations, but as noted below, the results would be questionable, either for the large eye rotations needed or the impracticality of keeping very narrow channels in view.
In all cases, the prisms have no effect at primary gaze (Fig. 4A), so the design is intended to provide an effect only when scanning into the prisms, requiring smaller scan angles to reach larger eccentricities. It does this, however, with a loss of paracentral field due to the apical prism scotomas (Fig. 4B). That loss was not mentioned in any of the InWave literature we reviewed.
Figure 4.
InWave channel prism fields. (A) Calculated perimetry with 8° residual visual field at primary gaze in a 6-mm channel. The prisms have no effect. Field of view shaded darker is lost to the apical scotomas. (B) With gaze shifted 8.5° (of visual field) left and down to the channel corner (9° of diagonal ocular rotation), the field is split into three parts, giving a 6° extension left and 4° down, with corresponding gaps in between at the apical scotomas. (C) The percept diagram corresponding to (B) for this bilateral fitting shows the larger grid spacing of the shifted fields and perceived discontinuity (jump) in the field of view caused by the scotomas. Thin gray lines, not part of the patient's percept, are shown to identify the prism apices. There is no visual confusion or diplopia, nor field expansion. (D) Measured LE field of patient 1 at this gaze position (RE patched). The total area seen is slightly larger than the 8° residual field due to vignetting at the prism edges. Dashed lines indicate the apparent location of the prism apices, a bit to the right of the intended location. (E) The asymmetric monocular field of patient 2 required shifting the 12 mm (33°) channel to the right, so that the residual field at primary gaze lies entirely within the channel. (F) With fixation shifted 7° left and 9° degrees down, the channel corner splits the field. Even though the channel and residual field sizes differ greatly for these two patients, the extension provided is the same. The apparent difference in scotoma sizes is an artifact of the imprecision of these difficult measurements, also seen as the differences in field size and shape between (E) and (F) for the 20/500 acuity of this subject.
Unilateral fitting (never dispensed or promoted, to our knowledge) could compensate for the apical scotomas, but would introduce central visual confusion when gazing into the prisms (Fig. 5). The conventional bilateral fitting, therefore, provides only field substitution (extension), not field expansion, while unilateral fitting could provide expansion with paracentral confusion, but still no benefit at primary gaze. With bilateral fitting, any misalignment of the channels can cause visual confusion, though likely only over a small region. Even monocular positioning of channel prisms is quite difficult, given the small fields and angles involved, as evidenced by the apparent errors of a degree or two in Figures 4D–4F likely due to imperfect centering of the residual field in the channels when fixating, despite the great care we took. This was further complicated by vignetting effects that produce a monocular diplopic image of the perimetry stimulus, which made it hard to precisely identify the channel edges.
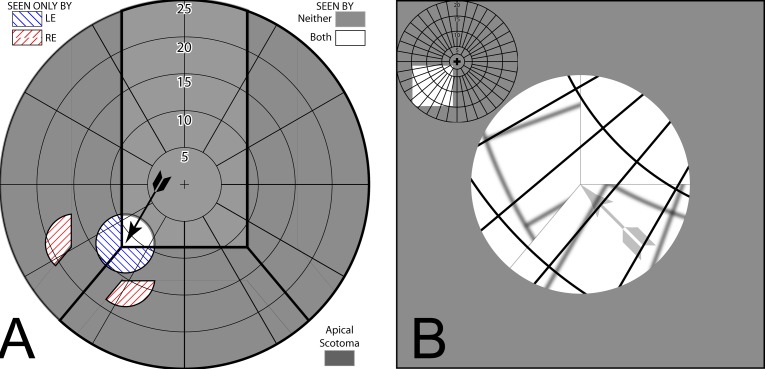
Figure 5.
Unilateral fitting. (A) With a channel prism lens fit only on the right eye (RE), the RE prism views provide true field expansion, as the LE sees the regions lost to the RE apical scotomas. (B) The percept diagram shows that the expansion comes at the expense of visual confusion.
While a base-down inferior prism segment has been somewhat helpful to patients during tasks such as eating, it has proved less successful and even hazardous for detecting steps and curbs.14 The low power used did not provide a view sufficiently close to the feet for this task. All InWave trial lenses placed the lower edge of the channel about 4 mm below center. At that position, the view of the floor through the lower lens (for a person with eyes 1.5 m above the path and spectacle rims 1.5 cm below primary) would extend from 2.2 to 6.4 m away, not likely much help in detecting arrival at a tripping hazard, and an apical scotoma extending from 6.4 to 9.9 m (when gazing at the prisms' lower and upper edges, respectively). Gadbaw et al.21 placed the edge of 20Δ lower prisms 25° of ocular rotation below primary, for a still-distant view of the floor from 1.7 to 2 m, and an apical scotoma to 3.2 m.
Peli Trifield Prisms
Trifield prism powers were selected to be somewhat larger in power than the patient's residual field width and adjusted for the patient's phoria posture. Here, we assume orthophoria, but when, as in this design, single central binocular vision is not maintained, determining prism power and placement is complicated by the patient's natural, and possibly variable, phoria.9 At primary gaze, monocular paracentral apical scotomas occur between the prism views (Fig. 6A). The field of view is expanded, but not contiguous. The corresponding percept diagram (Fig. 6B) shows the three-field two-way visual confusion at primary gaze. To aid the patient in interpreting the reversals in shift direction that can accompany small shifts in central gaze, the prisms are tinted red and green. If gaze is shifted more than half the patient's visual field width, the field is placed entirely within one prism, and there is relatively little scotoma between the prism and nonprism views (Fig. 6C), and only two-view confusion, as shown in the corresponding percept diagram (Fig. 6D). Lower prism powers would have induced diplopia (Figs. 6E, 6F). Thus the Trifield configuration provides a full (sometimes split) residual-field-width of true field expansion at all gaze positions, but through visual confusion. This central confusion is almost always annoying and disturbing, as it gives rise to rivalry (as well as warranting the term confusion). The Trifield spectacles were particularly difficult to use when walking at night on a sidewalk next to oncoming cars on a busy street, as a prism brought the bright car headlights into central view, impacting dark adaptation and the ability to see the sidewalk. A reflexive head turn away from the cars (while maintaining gaze ahead) would not change the view of the headlights. A counterintuitive head turn toward the cars would be needed to shift the headlight glare to a blind portion of the retina and recover the view of the sidewalk with the nonprism eye.
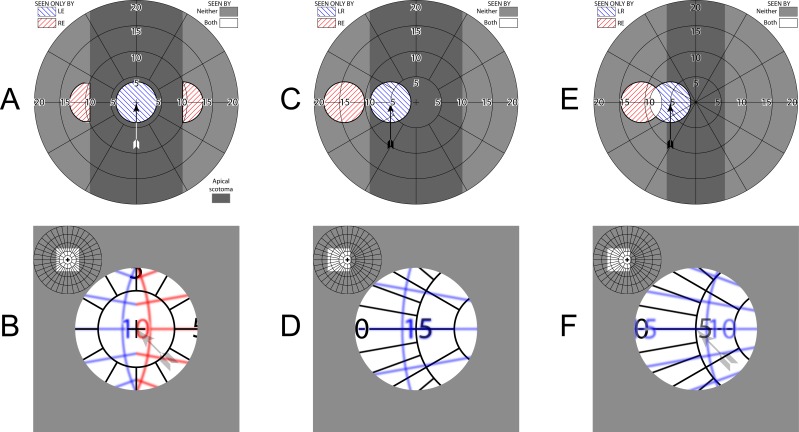
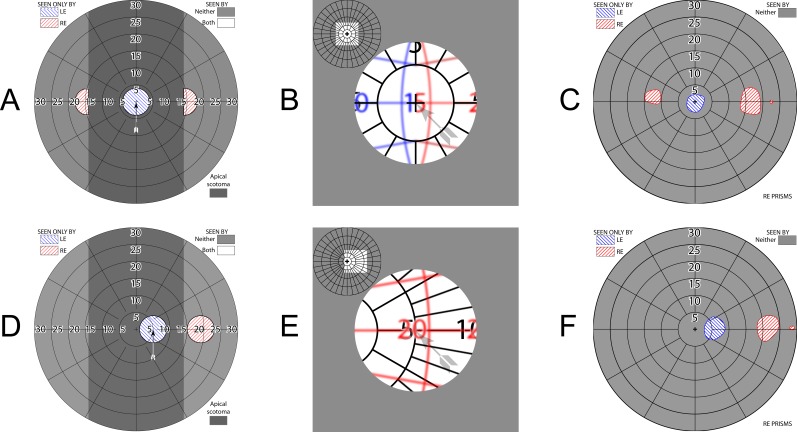
Figure 6.
Trifield prisms. (A) Simulated perimetry at primary gaze. The two 16Δ prisms add two peripheral islands of visibility. Two adjoining (but only monocular) apical scotomas, each larger than the patient's 8° field width, are evident (darker gray shading). (B) Corresponding percept diagram. Blue and red tints in the percept diagrams identify field viewed through the tinted right eye (RE) left (green) and right (red) prisms, respectively. (Although the prisms are tinted red and green, we diagram with red and blue in deference to dichromats.) Left eye (LE) maintains a direct, nonprismatic view at all gaze positions. True field expansion comes at the expense of central visual confusion. (C) With a left gaze shift of about half the residual field width, the RE view is entirely within the left green prism and a relatively continuous expanded view is afforded, without diplopia. (D) The corresponding percept diagram shows that there is still central confusion, but only from two views, not three. The digit 5 is coincidentally overlaid. (E) With 10Δ prisms, the power is not sufficient to avoid undesirable diplopia. (F) A region including the zero of the 10° eccentricity marking is thus perceived diplopically.
Figure 7 illustrates Trifield perimetry results for patient 1, using spectacles dispensed more than a decade ago,9 when his residual fields were larger. His use of Trifield spectacles ended after the pilot phase of the Trifield study and they were reused for this test. This illustrates the trade-off possible between apical scotoma size and the location of the expanded field areas available at primary gaze and on gaze shift.
Figure 7.
Patient 1 Trifield results. The patient's fields have shrunk in the decade since the 25Δ prisms were fitted, resulting in larger field of view gaps than illustrated in Figure 6A (and the diagram scale has changed to accommodate the higher-power prisms). Unlike channel prisms, which provide no access to the scotoma areas even with gaze shifts, the fellow nonprism eye can see into the apical scotoma regions, so the loss (without head turning) is not as problematic. Having access at primary gaze to the region at eccentricities larger than the scotomas may be desirable, although that has not been studied. (A) Simulated perimetry at primary gaze. (B) Corresponding percept diagram shows the “Trifield” binocular central visual confusion. (C) Corresponding perimetry. The asymmetry is indicative of the difficulty of positioning the prism apices exactly at primary gaze, as the perimeter's fixation target is invisible at that location in the prisms, and the eyes readily dissociate into the phoria posture, without any clue for the directional shift needed to align the eyes to assess veridical direction. (However, since the prisms are intended to provide hazard detection followed by a gaze turn to foveate the hazard with the nonprism eye, precise angular perception may not be needed.) (D) With a 5° gaze shift toward the right, the right eye (RE) view is entirely through the right prism. (E) The corresponding percept diagram again illustrates that there is still central confusion showing, but only from two views, not three. (F) Corresponding perimetry. We use the symbology of our dichoptic perimeter, but dichoptic shutter goggles were not needed to identify each eye's obvious and separate contribution.
Discussion
As peripheral field diameters continue to shrink, residual field becomes a precious commodity. Any application of prisms to improve detection of peripheral hazards must add more value than is lost to the intervention. Channel prisms avoid impacting the central field, but have no effect at primary gaze, where most time is spent. With the recommended bilateral fitting, field substitution, not expansion, is achieved when gaze is shifted into the prisms, and thus paracentral field is completely lost to the apical scotomas. The low power of the molded ophthalmic prisms from InWave limited the amount of field shift (and the scotoma sizes). Achieving an additional 6° laterally at the expense of that amount of paracentral field loss does not seem to be worthwhile, especially since there is no cue available to alert the patient to a need to scan into the prisms. Similarly, shifting the lower field up by a mere 4° (and losing 4° in between) is also not likely to provide a valuable benefit, as floor-level obstacles close to tripping require a much steeper angular shift relative to primary position of gaze.
Practitioners have used higher-power Press-On Fresnel prisms in channel configurations to achieve larger field relocations.6,14,15,17,19–24,29–33 All reports of improvements in patient satisfaction and mobility in the studies we found were subjective.14,15,21,24,29,30 However, those subjective reports may be unreliable and liable to placebo effects, as an appropriate control condition was not included, nor were there properly executed objective measures that could corroborate the results. In a randomized controlled cross-over trial comparing real and sham peripheral prism glasses for homonymous hemianopia,34 a significant placebo effect was indicated wherein 26% of subjects chose the sham prisms. A mobility questionnaire also showed this effect, as scores improved when using the shams. Thus, patient-reported gains in mobility in the channel prism trials cited must be viewed with caution, and might not represent true gains in mobility or safety.
A reviewer commented that we seem to have an axe to grind, and indeed we do. Many (and perhaps most) reports of prism use for PFL in the literature would not stand up to the scrutiny we have proposed, often describing impossible or improbable results. Perimetry conducted at primary gaze with properly aligned channel prisms should show no effect from the prisms (Figs. 4A, 4E). Yet Bohlman32 reported substantial field expansion with InWave channel prisms in Goldmann perimetry. It is hard to imagine how that result could be achieved. Perhaps the prisms were both misaligned and viewed centrally, and the reported kinetic perimetry stopped at the edge of the detected field, without continuing inward to detect both channel misalignment and residual apical scotomas. It is harder to rationalize how Somani et al.15 found field expansion using the Humphrey Field Analyzer 10-2 program. Patients were screened at the outset without prisms, and included only if their residual field diameter was 10° or less. After prism fitting and training in their use, they were measured with the prisms, and an increase in field area was found. Misaligned prisms in one eye could expand the binocular field, but the results were presented separately for each eye, not taken binocularly. The best explanation we can conjecture is that a misaligned, centrally placed, prism projected paracentral stimuli onto the central field, while spurious reflections35 in the prism from central stimuli were also detected. Both studies attributed the field gains to improved scanning, but of course scanning is not permitted during perimetry, and if it occurred the results would be meaningless.
Reported choices of prism placement are also quite variable. There does seem to be agreement among practitioners that the close fitting of the channel edges to the residual field, as recommended by InWave, is not tolerated by patients. There is not agreement on how far the prisms should be placed, and it is the rationale for that placement that adds to the uncertainty. Some reports30,31,33 argue that the channel should be widened as the patients learn to scan, apparently to avoid the prisms during “normal” scanning. There is a belief expressed that encountering the prisms trains the patient to scan and may eventually make the prisms unnecessary.33 After continually moving the prism apices temporally for a patient with 5° residual fields, Ferraro et al.30 said “He began seeing objects in almost a 180° range during the training activities.” They did acknowledge that this was unexpected. (The prisms were initially only fit temporally, and nasal prisms were added later.) No information was provided on the test conditions, such as measures of head versus eye movement or time allowed to detect the objects. They had noted before the training that the patient did an unusual amount of head scanning. We surmise that prisms had nothing to do with the outcome, except that the patient insisted on always being tested with them. Conversely, others suggest that as the patients become comfortable with the prisms, the apices can be moved closer to the residual field edge.19,23
Since channel prisms have no effect at the primary gaze position, it is necessary to scan into the prisms to get any advantage of wider field access with relatively smaller eye movements. Although some authors clearly believe that patients can be trained to scan widely with eye movements,20,21,30 we have not found any objective evidence to support a persistent effect of that training, especially when walking. Patients certainly do not seem to learn that skill on their own. Our studies have found that patients with PFL simply do not compensate for their loss by using eye scans farther than those with normal sight,36 and saccades as wide or wider than 15° are rare.37 A study with hemianopes reported that hemianopic patients adopted an effective scan strategy enabling them to detect virtual basketballs thrown at them in a head-mounted display when seated, but when the same task was attempted while walking in the same simulated environment, trained performance dramatically declined.38
While the close placement of the prism apices to the residual field, as recommended by InWave, made the prisms accessible during normal saccades (but would not overcome the apical scotoma losses), we found only two reports of use of the InWave prisms.32,39 The Fresnel prisms used in all other reports seem to have been placed far enough from the primary gaze position to avoid encountering them with normal saccades, as patients reported that encroachments were uncomfortable or disturbing.21,30,31 The training procedure designed by Jose29 is best described as familiarizing the patient with the effects of the prisms and familiarizing them with the need to interpret the nonveridical views through them. There is no mention of training to use wide eye scans to reduce the need for head scanning in that oft-cited1,6,15,17,18,22,23,30,31,40 article.29 Yet, later reports stress the belief, not supported by actual measurement, that training for wider eye scans and less head motion has been effective and improves mobility.20,21,30,31
There is simply no reliable support for the notion that this training results in unconsciously directed eye scans that effortlessly increase the effective field. Some authors, however, make the more realistic assumption that intermittent, conscious, scanning into the prisms, followed by head turns to view detected objects of interest through the prism-free channel, can be accomplished, much as one uses a rear-view mirror when driving.19,23 However, a rear-view mirror is used infrequently and primarily when the driver plans a maneuver such as a lane change that requires monitoring cars behind, while a walking pedestrian constantly needs the peripheral field to detect unexpected stationary or moving obstacles.
We found no reports of satisfactory use of Fresnel prisms greater than 20Δ. Channel prisms seem an unlikely formula for improved safety when walking. Head scans are needed to avoid the dangers of apical scotomas. Normal saccades fall largely within the clear channel, providing no cue to trigger a scan into the prisms, while uncomfortable larger scans provide only a 10° prism shift.
We encourage practitioners to use field simulation diagrams to predict the effects of prism interventions, including various positions of gaze and head turns. Then any discrepancy between predicted and measured results should trigger investigation into the causes of the discrepancies and thus avoid prescribing ineffective solutions or erroneous publications. Had we followed this advice for all, and not just some, of the configurations presented in Apfelbaum et al.,10 we would not have had, in Jung and Peli,35 to acknowledge and correct the oversimplifications of our earlier high-power (57Δ) prism simulations.
In 1975, Finn et al.20 said “It is hoped that standards for the placement of prism lenses can be developed, along with techniques for training.” Apparently the ensuing four decades have done little to fulfill that hope. The literature has been devoid of objective evaluations of channel prisms. However, given our analyses of their inability to provide aid at primary gaze and the gaze shifts needed to gain a bit of field-of-view substitution, not expansion, with the corresponding loss of paracentral field, we doubt that refined fitting and training methods would be able to overcome the fundamental limitations of this design. Gadbaw et al.21 reported that five of 15 patients with RP in their study who accepted Fresnel channel prisms continued to wear them after a year. In a study by Lindsay,39 three of five patients offered InWave channel prisms chose to try them, and only one of those three reported wearing them at a long-term follow-up. The Trifield prism glasses developed in our lab provide true lateral field expansion at all positions of gaze. Yet, just three of 12 participants in a clinical trial continued to wear them approximately a year later.9 Constant central visual confusion likely contributed to this limited success. The clear central views with channel prisms and the availability of bifocal add make continuous wear possible, while Trifield spectacles were only intended for mobility, and not for reading.
Peli prisms developed for hemianopia8 have gained wide acceptance because they provide significant field expansion, while their placement in the upper and lower periphery avoids central visual confusion.34 We conclude that a prismatic solution for PFL must also provide meaningful expansion at primary gaze while avoiding central visual confusion.
Brilliant et al.6 also identified the need to avoid central placement in the design of their Trioptical lenses, which had a horizontally minifying telescope in the bioptic upper central position and a temporally placed base-out Fresnel sector prism on each carrier lens, leaving the lower center and nasal portions clear. However, the Fresnel placement was too far in the periphery to provide any benefit without very large scans (> 26° of ocular rotation). Since the prisms were only fitted on the temporal side of the carrier lens, if the patient did scan into the prism on either side, the effect of the prism was unilateral, resulting in true field expansion (with central confusion, though neither effect was mentioned in the report). Only gazes through the clear lower central portion of the lenses provided unmodified binocular views. The power of the prisms was not specified, but the pictures suggest that it was not more than 20Δ, providing an expansion of at most 10° and resulting in diplopia for users with residual field diameter larger than 10°. Continued use after 1 year by four of six patients in their trial was more likely due to benefits when searching while stationary (most likely using the bioptic amorphic minifier), not to prism-increased field during mobility. Since the system did not impact primary gaze, continued wearing was possible without the central visual confusion of our Trifield prisms. However, we know of no additional application of this prism design beyond that one study, and the Amorphic telescope it used was discontinued some years ago.
Achieving 25% retention with Trifield prisms despite the central confusion is likely a testament to the great need these patients have for a field expansion solution, as compared to 50% retention of Peli prisms by hemianopes,34,41 who are not nearly as handicapped by their field loss, and 100% retention in an independent study.42 Visual confusion, however, is the main mechanism by which true prismatic expansion is achieved. (With high power prisms some additional expansion is provided by prism minification due to the change in effective power with change in angle of incidence.11) We are investigating the use of our newly invented multiplexing prisms.43,44 These prisms provide simultaneous shifted and straight-through views, thus eliminating apical scotomas. If placed in the residual (upper and lower) near periphery, they are expected to provide expansion at primary gaze without apical scotomas, albeit with near peripheral (not central) visual confusion and decreased contrast. Thus they address the drawbacks of prior approaches we have noted, and potentially meet the requirements we have identified for this highly constrained application. It remains to be seen if sufficient functional near peripheral field is available for prismatic expansion while maintaining a sufficiently clear central area to sustain single central binocular vision. The balance of costs and benefits has yet to be determined experimentally.
Acknowledgments
We thank Amy Doherty for her perseverance and patience conducting the challenging perimetry sessions, and Nicole Ross, OD, MS for the initial literature search.
Supported in part by NIH grants R01EY12890 (EP) R01EY023385 (EP) and P30EY003790, and by gifts from Chadwick Optical, Souderton, PA, and Multilens AB, Mölnlycke, Sweden.
Aspects of this study have been presented in abstract form as: Apfelbaum HL, Peli E. Considering optical scotomas when prescribing prisms for peripheral visual field loss (abstract). Optom Vis Sci. 2011;88:E-abstract 115073.
Disclosure: H. Apfelbaum, None; E. Peli, (P). E. Peli has a patent assigned to Schepens Eye Research Institute and licensed to Chadwick Optical for the use of peripheral prism for hemianopia, and has applied for a patent for the multiplexing prism and its use in expanding visual fields.
References
- 1. Geruschat DR,, Turano KA. Connecting research on retinitis pigmentosa to the practice of orientation and mobility. J Vis Impair Blind. 2002; 96; 69–85. [Google Scholar]
- 2. Drasdo N. Techniques instruments, cases; visual field expanders. Am J Optom Physiol Opt. 1976; 53 (9 pt 1): 464–467. [DOI] [PubMed] [Google Scholar]
- 3. Krefman RA. Reversed telescopes on visual efficiency scores in field-restricted patients. Am J Optom Physiol Opt. 1981; 58; 159–162. [DOI] [PubMed] [Google Scholar]
- 4. Hoeft WW,, Feinbloom W,, Brilliant R,, et al. Amorphic lenses: a mobility aid for patients with retinitis pigmentosa. Am J Optom Physiol Opt. 1985; 62: 142–148. [PubMed] [Google Scholar]
- 5. Szlyk JP,, Seiple W,, Laderman DJ,, Kelsch R,, Ho K,, McMahon T. Use of bioptic amorphic lenses to expand the visual field in patients with peripheral loss. Optom Vis Sci. 1998; 75; 518–524. [DOI] [PubMed] [Google Scholar]
- 6. Brilliant RL,, Appel SD,, Ruggiero RJ. The amorphic Fresnel Prism trioptical system. : Woo GC. Low Vision. New York: Springer; 1987: 209–215. [Google Scholar]
- 7. InWave. InWave Optics. Prescribing Guide. Janesville, WI: InWave; 1998. [Google Scholar]
- 8. Peli E. Vision multiplexing: an engineering approach to vision rehabilitation device development. Optom Vis Sci. 2001; 78: 304–315. [DOI] [PubMed] [Google Scholar]
- 9. Woods RL,, Giorgi RG,, Berson EL,, Peli E. Extended wearing trial of Trifield lens device for “tunnel vision.” Ophthalmic Physiol Opt. 2010; 30: 240–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Apfelbaum HL,, Ross NC,, Bowers AB,, Peli E. Considering apical scotomas, confusion, and diplopia when prescribing prisms for homonymous hemianopia. Transl Vis Sci Technol. 2013; 2: 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jung J-H,, Peli E. Impact of high power and angle of incidence on prism corrections for visual field loss. Opt Eng. 2014; 53: 061707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Peli E,, Satgunam P. Bitemporal hemianopia: its unique binocular complexities and a novel remedy. Ophthalmic Physiol Opt. 2014; 34: 233–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Peli E. Treating with spectacle lenses: a novel idea!? Optom Vis Sci. 2002; 79: 569–580. [DOI] [PubMed] [Google Scholar]
- 14. Hoeft WW. The management of visual field defects through low vision aids. J Am Optom Assoc. 1980; 51: 863–864. [PubMed] [Google Scholar]
- 15. Somani S,, Brent MH,, Markowitz SN. Visual field expansion in patients with retinitis pigmentosa. Can J Opthalmol. 2006; 41: 27–33. [DOI] [PubMed] [Google Scholar]
- 16. Weiss NJ. An application of cemented prisms with severe field loss. Am J Optom Arch Am Acad Optom. 1972; 49: 261–264. [DOI] [PubMed] [Google Scholar]
- 17. Fox CR. Low vision rehabilitation for patients with severe glaucoma. : Albert DM,, Jakobiec FA,, Azar DT,, Gragoudas ES,, Power SM,, Robinson NL, Principles and Practice of Ophthalmology. 2nd ed. Philadelphia, PA: W. B. Saunders; 1999: 3031–3043. [Google Scholar]
- 18. Cohen JM. An overview of enhancement techniques for peripheral field loss. J Am Optom Assoc. 1993; 64: 60–70. [PubMed] [Google Scholar]
- 19. Tallman KB,, Haskes C,, Perlin RR. A case study of choroideremia highlighting differential diagnosis and management with Fresnel prism therapy. J Am Optom Assoc. 1996; 67: 421–429. [PubMed] [Google Scholar]
- 20. Finn WA,, Gadbaw PD,, Kevorkian GA,, De L'Aune WR. Increasing field accessibility through prismatically displaced images. The New Outlook. 1975; 69: 465–467. [Google Scholar]
- 21. Gadbaw PD,, Finn WA,, Dolan MT. De l'Aune WR. Parameters of success in the use of Fresnel prisms. Opt J Rev Optom. 1976; 113: 41–43. [Google Scholar]
- 22. Bailey IL. Prismatic treatment for field defects. Optom Monthly. 1978; 69: 99–107. [Google Scholar]
- 23. Perlin RR,, Dziadul J. Fresnel prisms for field enhancement of patients with constricted or hemianopic visual fields. J Am Optom Assoc. 1991; 62 (1); 58–64. [PubMed] [Google Scholar]
- 24. Hoppe E,, Perlin RR. The effectivity of Fresnel prisms for visual field enhancement. J Am Optom Assoc. 1993; 64: 46–53. [PubMed] [Google Scholar]
- 25. Bishop PO. Binocular vision. : Moses RA. Adler's Physiology of the Eye: Clinical Applications. St. Louis, MO: C.V. Mosby; 1981: 575–649. [Google Scholar]
- 26. Fannin TE,, Grosvenor T. The correction of ametropia. : Clinical Optics. 2nd ed. Boston: Butterworth-Heinemann; 1996: 109–126. [Google Scholar]
- 27. Woods RL,, Apfelbaum HL,, Peli E. DLP-based dichoptic vision test system. J Biomed Optics. 2010; 016011: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Woods RL,, Fetchenheuer I,, Vargas-Martin F,, Peli E. The impact of non-immersive head-mounted displays (HMD) on the visual field. J Soc Inf Disp. 2003; 11: 191–198. [Google Scholar]
- 29. Jose RT,, Smith AJ. Increasing peripheral field awareness with Fresnel prisms. Opt J Rev Optom. 1976; 113: 33–37. [Google Scholar]
- 30. Ferraro J,, Jose RT, Olsen McClain LM. Fresnel prisms as a treatment option for retinitis pigmentosa. Texas Optometry. 1982; 38: 18–20. [Google Scholar]
- 31. Schmeidecke S,, Jose R. Prism therapy in low vision rehabilitation. Int Congress Series, Excerpta Medica. 2005; 1282: 709–713. [Google Scholar]
- 32. Bohlman H. Field expanding lenses in a patient with choroideremia (Abstract). : AAO Annual Meeting Abstracts: American Academy of Optometry. Austin TX: American Academy of Optometry; 1997: p. Poster 19. [Google Scholar]
- 33. Ferraro J,, Jose RT. Training programs for individuals with restricted fields. : Jose RT, Understanding Low Vision. New York: American Foundation for the Blind; 1983: 363–376. [Google Scholar]
- 34. Bowers A,, Keeney K,, Peli E. Randomized crossover clinical trial of real and sham peripheral prism glasses for hemianopia. JAMA Ophthalmol. 2014; 132: 214–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Jung JH,, Peli E. Spurious reflection effects in Fresnel prisms used for visual field expansion (abstract). Optom Vis Sci. 2013; 90:E-abstract 135000.
- 36. Vargas-Martin F,, Peli E. Eye movements of patients with tunnel vision while walking. Invest Ophthalmol Vis Sci. 2006; 47: 5295–5302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Luo G,, Peli E. Patients with tunnel vision frequently saccade to outside their visual fields in visual search (abstract). J Vis. 2006; 6: 505. [Google Scholar]
- 38. Iorizzo DB,, Riley ME,, Hayhoe M,, Huxlin KR. Differential impact of partial cortical blindness on gaze strategies when sitting and walking - an immersive virtual reality study. Vision Res. 2011; 51: 1173–1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Lindsay DM. Long-term outcomes regarding patient acceptance and use of the InWave field expanding lens (Abstract). : Vision '99 International Conference on Low Vison Abstract Book. New York: Lighthouse International; 1999: 216–217. [Google Scholar]
- 40. Herse P. Retinitis pigmentosa: visual function and multidisciplinary management. Clin Exp Optom. 2005; 88: 335–350. [DOI] [PubMed] [Google Scholar]
- 41. Bowers AR,, Keeney K,, Peli E. Community-based trial of a peripheral prism visual field expansion device for hemianopia. Arch Ophthalmol. 2008; 126: 657–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. O'Neill EC,, Connell PP,, O'Connor JC,, Brady J,, Reid I,, Logan P. Prism therapy and visual rehabilitation in homonymous visual field loss. Optom Vis Sci. 2011; 88: 263–268. [DOI] [PubMed] [Google Scholar]
- 43. Jung J-H,, Peli E. Multiplexing prism for field expansion of acquired monocular vision & normal sight (abstract). 2014: Poster presentation at VISION 2014, the 2011th International Conference on Low Vision (P2134).
- 44. Peli E. inventor. Vision modification based on a multiplexing prism. United States patent application PCT/US14/17351, 2014.