Abstract
Background/Aims
Prokinetic drugs such as metoclopramide are frequently used as second-line therapy for patients with gastroesophageal reflux disease. However, their beneficial effects remain unclear. Esophageal motor activities and compliance of the esophagogastric junction (EGJ) are important for prevention of gastroesophageal reflux. Although metoclopramide has been reported to increase lower esophageal sphincter (LES) pressure, its effects on EGJ compliance have not been evaluated. In the present study, we investigated the effects of metoclopramide on esophageal motor activities and EGJ compliance.
Methods
Nine healthy male volunteers without abdominal symptoms were enrolled. Peristaltic esophageal contractions and LES pressure were examined using high-resolution esophageal manometry, while EGJ compliance was evaluated with an endoluminal functional lumen-imaging probe. After obtaining baseline values for esophageal motor activities and EGJ compliance, metoclopramide (10 mg) was intravenously administered, then all measurements were repeated at 15 minutes after administration in each subject.
Results
Following administration of metoclopramide, mean resting LES pressure was significantly increased as compared with the baseline (13.7 ± 9.2 vs 26.7 ± 8.8 mmHg, P < 0.05). In addition, metoclopramide significantly augmented peristaltic contractions, especially in the distal esophageal segment (P < 0.05). On the other hand, distensibility index did not change after administration (4.5 ± 0.5 vs 4.1 ± 0.5 mm2/mmHg), suggesting no significant effect of metoclopramide on EGJ compliance.
Conclusions
Metoclopramide augmented esophageal contractions without changing EGJ compliance in healthy adults.
Keywords: Esophageal sphincter, lower, Esophagogastric junction, Manometry, Metoclopramide, Motor Activity
Introduction
The patients with gastroesophageal reflux disease (GERD) suffer from heartburn and regurgitation, which are caused by reflux of stomach contents, leading to a significant impairment of quality of life. Proton pump inhibitor (PPI) administration is the current mainstay for first-line treatment of GERD because of the consistent inhibitory effect on acid secretion. However, use of a PPI alone is insufficient in approximately 30% of GERD patients.1 As second-line therapy, prokinetic drugs have been used in clinical settings, though their beneficial effects for GERD are not well elucidated.2,3
Metoclopramide, a prokinetic agent, has been widely used for treatment of gastrointestinal motility disorders. In addition to acting as a central dopamine D2 receptor antagonist, metoclopramide blocks the dopamine D2 receptor in peripheral nerve endings and promotes release of acetylcholine. As a result, metoclopramide augments gastrointestinal motility and enhances gastric emptying, and also increases lower esophageal sphincter (LES) tone.4–8
It has recently been reported that esophageal motor activities and compliance of the esophagogastric junction (EGJ) is important for prevention of gastroesophageal reflux, with the latter considered to cause greater volume reflux of gastric contents into the esophagus.9–11 Fundoplication surgery for repairing the EGJ has been consistently shown to prevent pathological gastroesophageal reflux by restoration of normal EGJ compliance.12,13
An endoluminal functional lumen imaging probe (EndoFLIP, Crospon Ltd, Galway, Ireland) has been developed as a novel device to determine cross-sectional area (CSA) and distensibility at the EGJ.9 We previously used this probe and high-resolution manometry (HRM) to show that high-dose mosapride (40 mg), a prokinetic agent that acts on the 5-hydroxytryptamine type 4-receptors, augments peristaltic contractions and mean resting LES pressure, which significantly reduced EGJ compliance, though the effects of mosapride on esophageal motor activity vary at lower doses.14,15
Although metoclopramide has been reported to increase LES pressure, its effects on EGJ compliance have not been evaluated.4–8 Therefore, the aim of the present study was to investigate the effects of metoclopramide on esophageal motor activities and EGJ compliance in healthy volunteers, for which we employed the EndoFLIP system and high-resolution 36-channel manometry.
Materials and Methods
Subjects and Study Protocol
Nine healthy male volunteers (mean age 25.4 ± 3.1 years) without chest or abdominal symptoms were enrolled in this study. None had a history of cardiac, respiratory, neurologic, or gastrointestinal disorders, or were taking any medications.
Peristaltic esophageal contractions and LES pressure were examined by high-resolution esophageal manometry (ManoScan360; Sierra Scientific Instruments, Los Angeles, CA, USA), while EGJ compliance was investigated using the EndoFLIP system.9 Prior to each measurement, an intravenous access was obtained. After baseline measurements of esophageal motor activities and EGJ compliance, 10 mg of metoclopramide was administered as an intravenous single bolus. At 15 minutes after administration of metoclopramide, the measurements were repeated.
The study protocol was approved by the ethical committee of Shimane University Faculty of Medicine. Written informed consent was obtained from each subject before enrollment in the study, which was carried out in accordance with the Declaration of Helsinki. This study was registered with the University Hospital Medical Information Network clinical trials registry, number UMIN (000013521).
Determination of Esophageal Motor Activity
Esophageal motor activity was determined using high-resolution 36-channel manometry, according to a previously reported method.14–16 Based on the manufacturer’s instructions, the manometric catheter was inserted in a transnasal manner after local anesthesia (2% lidocaine jelly) and measurements were performed in a supine position starting 5 minutes after insertion. Initially, we determined resting LES pressure for at least 5 minutes. Then, esophageal body peristaltic contractions were evaluated after a wet swallow of drinking water (5 mL). That was repeated at intervals of 2 minutes until 5 complete contraction records were obtained. Esophageal body peristaltic contractions were observed in 3 segments (proximal, middle, distal, segments 1, 2, 3, respectively), based on a previous report.14–16 LES pressure and peak peristaltic contraction pressure in the 3 segments of the esophageal body were analyzed using ManoView analysis software (Sierra Scientific Instruments).
Determination of Esophagogastric Junction Compliance
EGJ compliance was determined by use of the EndoFLIP system. The probe was a 240-cm long catheter with a 3-mm outer diameter and equipped with a 14-cm long bag in the distal end, which is compliant to a maximal diameter of 25 mm. Inside the bag, 16 paired impedance electrodes were placed at 4-mm intervals along with a pressure sensor. As the bag was filled with a specially formulated conductive solution, impedance across each segment was inversely proportional to the CSA of the bag at that locus. This allows the diameter and CSA of the bag to be measured, along with intra-bag pressure. Data from the 16 paired electrodes and pressure sensor were sampled by a recording unit, which displayed them in real time on a monitor. The catheter was calibrated based on the manufacturer’s instructions, then inserted in a transnasal manner until the impedance electrodes straddled the EGJ at its mid-point. We ignored peristaltic waves, which were often visible. The bag was inflated to volumes of 20, 30, and 40 mL, with a 30-second recording obtained at each distension volume. We evaluated minimum diameter (Dmin), narrowest CSA, and distensibility index (DI [mm/mmHg]) at each distension volume, as previously reported. EGJ distensibility index was defined as the narrowest CSA in relation to the corresponding intra-bag pressure and calculated using the following equation: narrowest CSA/intra-bag pressure + intragastric pressure offset.
Statistical Methods
Data are expressed as the mean ± SE. Statistical comparisons between metoclopramide administration and the baseline period were performed used a Wilcoxon signed rank test. Differences at P < 0.05 were considered to be statistically significant. All analyses were performed using SPSS version 19.0 (IBM SPSS Japan Inc, Tokyo, Japan).
Results
All 9 subjects completed the study protocol without any adverse events. EndoFLIP data for 1 were not appropriately recorded due to technical problems, thus those obtained from 8 subjects were analyzed. In addition, data for esophageal motor activity obtained with HRM were successfully recorded in all cases.
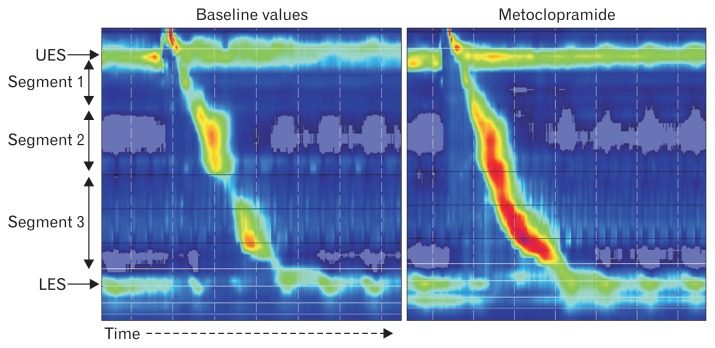
Consistent with previous reports, mean resting LES pressure in a supine position was significantly elevated after intravenous administration of metoclopramide (13.7 ± 9.2 vs 26.7 ± 8.8 mmHg, P < 0.05). In addition, metoclopramide significantly augmented maximal peristaltic contractions, especially in segment 3 (distal; 109.8 ± 45.4 vs 140.5 ± 51.7 mmHg, P < 0.05) (Fig. 1 and Table 1). Contraction pressure in segments 1 and 2 (proximal and middle, respectively) also tended to be elevated after administration, though the differences did not reach statistical significance.
Figure 1.
Esophageal motor activity with and without metoclopramide. Examination of a representative subject using high-resolution manometry. Esophageal peristaltic contractions (segments 1–3) and resting lower esophageal sphincter (LES) pressure were augmented after intravenous administration of metoclopramide. UES, upper esophageal sphincter.
Table 1.
Esophageal Motor Activity
| Baseline | Metoclopramide | P-value | |
|---|---|---|---|
| Maximal peristaltic contraction (mmHg) | |||
| Segment 1 | 83.4 ± 28.3 | 86.9 ± 25.6 | |
| Segment 2 | 103.5 ± 45.3 | 114.3 ± 48.9 | |
| Segment 3 | 109.8 ± 45.4 | 140.5 ± 51.7 | < 0.05 |
| Resting LES pressure (mmHg) | 13.7 ± 9.2 | 26.7 ± 8.8 | < 0.05 |
LES, lower esophageal sphincter.
Values are expressed as the mean ± SE.
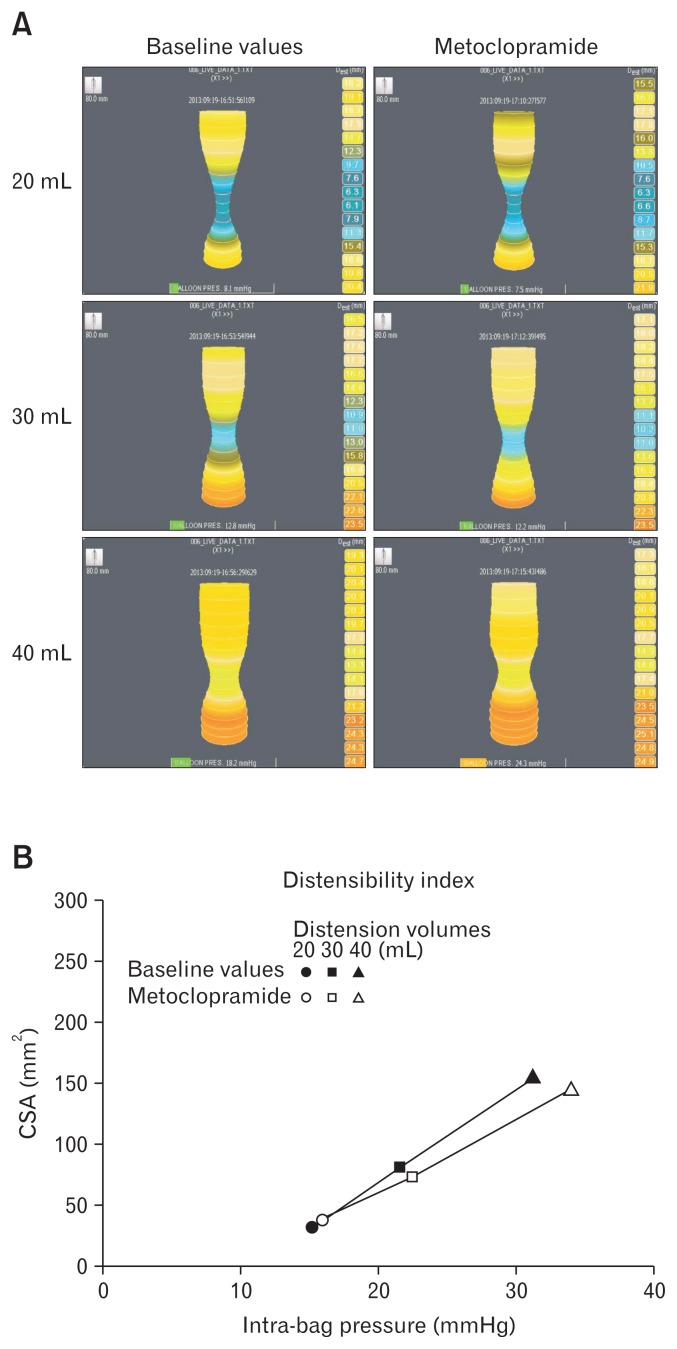
On the other hand, metoclopramide did not change EGJ compliance after intravenous administration. When the EndoFILP bag was distended to straddle the EGJ, the bag formed an hourglass shape by central contraction at the diaphragmatic hiatus during both metoclopramide administration and the baseline period (Fig. 2). There was no statistically significant differences in regard to hiatal minimum diameter (13.8 ± 1.5 vs 13.6 ± 0.7 mm, distention volume 40 mL), CSA (152.4 ± 34.2 vs 146.1 ± 15.3 mm2, distention volume 40 mL), or distensibility index (4.5 ± 0.5 vs 4.1 ± 0.5 mm2/mmHg, distention volume 40 mL) between the baseline period and following intravenous administration of metoclopramide (Table 2).
Figure 2.
Esophagogastric junction (EGJ) compliance with and without metoclopramide. (A) EGJ compliance with and without metoclopramide administration. The EndoFILP bag was distended to 20, 30, and 40 mL, which gave the bag an hourglass shape from the corresponding intra-bag pressure during both metoclopramide administration and the baseline period. There were no differences in bag shape following metoclopramide administration. (B) Distensibility index (DI) with and without metoclopramide. To determine the DI, intra-bag pressure (x-axis) and hiatal cross-sectional area (CSA; y-axis) were determined with the EndoFLIP bag distended to 20 mL (circles), 30 mL (squares), and 40 mL (triangles). There were no differences between the baseline period and the period following intravenous administration of metoclopramide.
Table 2.
Esophagogastric Junction Compliance
| Baseline | Metoclopramide | |
|---|---|---|
| Distention volume: 20 mL | ||
| Dmin (mm) | 6.4 ± 0.9 | 6.9 ± 1.6 |
| Hiatal CSA (mm2) | 32.9 ± 10.0 | 39.4 ± 18.5 |
| Intra-bag pressure (mmHg) | 15.5 ± 5.1 | 16.3 ± 6.8 |
| DI (mm2/mmHg) | 1.8 ± 0.2 | 1.9 ± 0.2 |
| Distention volume: 30 mL | ||
| Dmin (mm) | 10.2 ± 1.9 | 9.6 ± 1.4 |
| Hiatal CSA (mm2) | 84.5 ± 33.2 | 74.2 ± 19.8 |
| Intra-bag pressure (mmHg) | 22.0 ± 6.0 | 22.4 ± 7.1 |
| DI (mm2/mmHg) | 3.5 ± 0.6 | 3.0 ± 0.4 |
| Distention volume: 40 mL | ||
| Dmin (mm) | 13.8 ± 1.5 | 13.6 ± 0.7 |
| Hiatal CSA (mm2) | 152.4 ± 34.2 | 146.1 ± 15.3 |
| Intra-bag pressure (mmHg) | 31.2 ± 6.8 | 34.1 ± 8.0 |
| DI (mm2/mmHg) | 4.5 ± 0.5 | 4.1 ± 0.5 |
Dmin, minimum diameter; CSA, cross-sectional area; DI, distensibility index.
Values are expressed as the mean ± SE.
Discussion
GERD is defined as symptoms, such as heartburn and regurgitation, or esophageal mucosal injury produced by gastroesophageal reflux. A disorder of esophageal motor function is one of the important factors for occurrence of GERD.17 Notably, esophageal body motor function and LES pressure are considered to be the most relevant factors for preventing gastroesophageal reflux.18,19 High LES pressure prevents reflux of gastric contents. In previous studies, low LES pressure and impaired esophageal peristalsis were observed in GERD patients, and free and stress-induced gastroesophageal refluxes are known to frequently occur in those cases.20–23 Furthermore, in order to clear gastric contents that have refluxed into the esophagus, efficient esophageal body peristaltic contractions are important.24–27
EGJ distensibility, an additional factor that prevents large volume gastroesophageal reflux, has recently drawn interest from researchers. Limited EGJ distensibility reduces large volume fluid reflux from the stomach and that in GERD patients has been reported to be augmented to a greater degree than that seen in healthy controls.9–11 Prokinetic agents are expected to improve those anti-reflux functions and considered to be effective for treatment of GERD.28 We previously reported that high-dose mosapride (40 mg) not only augmented esophageal peristaltic contractions and mean resting LES pressure, but also reduced EGJ compliance, whereas a standard dosage did not consistently change esophageal motor activity.14,15
The present is the first study to show the effects of metoclopramide on esophageal motor activity and EGJ compliance in healthy adults using HRM and the EndoFLIP system. Metoclopramide is used as a prokinetic drug and has pharmacological actions similar to mosapride. Consistent with our previous study, metoclopramide was found to augment LES pressure to the same degree as mosapride. However, metoclopramide did not decrease EGJ distensibility, which was different from the effect of mosapride. Collectively, metoclopramide augmented esophageal motor activities, without affecting EGJ distensibility.
Considering our observations, it is important to note that the pharmacological characteristics of mosapride and metoclopramide are different, though both are used for gastrointestinal motility disorders as prokinetic agents. Mosapride mainly stimulates presynaptic 5-HT4 receptors in the peripheral autonomic motor nervous system and augments acetylcholine release at the neuromuscular junction with augmented gastrointestinal motility. On the other hand, metoclopramide mainly inhibits presynaptic dopamine D2 receptors and increases acetylcholine release during neuromuscular reactions. These differences between the drugs may result in different effects on EGJ distensibility. In addition, mosapride has few effects on the central nervous system, as it has difficulty crossing the blood brain barrier.29 In contrast, metoclopramide can easily cross the blood brain barrier and blocks dopamine D2 receptors in the brain, including the brain stem.30,31 Therefore, the combined central and peripheral activities of metoclopramide may have different effects on EGJ distensibility as compared to mosapride.
The relationship between EGJ compliance and LES pressure remains controversial. Pandolfino et al32 reported a weak negative relationship and concluded that basal LES pressure likely plays only a small role in determining EGJ distensibility. The EGJ is a complex structure that exists along with the LES, crural diaphragm, and clasp and sling fibers at the angle of His. Although, individual influences of prokinetic agents on factors such as those investigated in the present study are difficult to evaluate by EndoFLIP measurements alone, metoclopramide, and mosapride may have different effects.33
There are some limitations to our study. First, we administrated metoclopramide to healthy young volunteers and not GERD patients with impaired esophageal motor functions. In addition, we have intravenously administrated metoclopramide in this study. For evaluating the therapeutic value of metoclopramide for the treatment of GERD, the effect of oral administration need to be studied. Furthermore, the number of subjects enrolled was small and an additional larger study that includes GERD patients may be necessary in the future.
In conclusion, intravenous administration of metoclopramide augmented esophageal body peristalsis and resting LES pressure, without changing EGJ compliance.
Footnotes
Financial support: None.
Conflicts of interest: None.
Author contributions: Yoshikazu Kinoshita: study concept and design; Masahito Aimi and Hironobu Mikami: acquisition, analysis, and interpretation of data; Hironobu Mikami: drafting of the manuscript; Norihisa Ishimura and Yoshikazu Kinoshita: critical revision of the manuscript for important intellectual content; Masahito Aimi and Hironobu Mikami: statistical analysis; and Yoshikazu Kinoshita: study supervision.
References
- 1.Adachi K, Furuta K, Miwa H, et al. A study on the efficacy of rebamipide for patients with proton pump inhibitor-refractory non-erosive reflux disease. Dig Dis Sci. 2012;57:1609–1617. doi: 10.1007/s10620-012-2087-6. [DOI] [PubMed] [Google Scholar]
- 2.Miwa H, Inoue K, Ashida K, et al. Randomised clinical trial: efficacy of the addition of a prokinetic, mosapride citrate, to omeprazole in the treatment of patients with non-erosive reflux disease – a double-blind, placebo-controlled study. Aliment Pharmacol Ther. 2011;33:323–332. doi: 10.1111/j.1365-2036.2010.04517.x. [DOI] [PubMed] [Google Scholar]
- 3.Hsu YC, Yang TH, Hsu WL, et al. Mosapride as an adjunct to lansoprazole for symptom relief of reflux oesophagitis. Br J Clin Pharmacol. 2010;70:171–179. doi: 10.1111/j.1365-2125.2010.03696.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dilawari JB, Misiewicz JJ. Action of oral metoclopramide on the gastrooesophageal junction in man. Gut. 1973;14:380–382. doi: 10.1136/gut.14.5.380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Howard FA, Sharp DS. Effect of metoclopramide on gastric emptying during labour. Br Med J. 1973;1:446–448. doi: 10.1136/bmj.1.5851.446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brock-Utne JG, Rubin J, Welman S, Dimopoulos GE, Moshal MG, Downing JW. The action of commonly used antiemetics on the lower esophageal sphincter. Br J Anaesth. 1978;50:295–298. doi: 10.1093/bja/50.3.295. [DOI] [PubMed] [Google Scholar]
- 7.Baumann HW, Sturdevant AL, McCallum RW. L-Dopa inhibits metoclopramide stimulation of the lower esophageal sphincter in man. Dig Dis Sci. 1979;24:289–295. doi: 10.1007/BF01296543. [DOI] [PubMed] [Google Scholar]
- 8.Salem MR, Bruninga KW, Dodlapatii J, Joseph NJ. Metoclopramide does not attenuate cricoid pressure-induced relaxation of the lower esophageal sphincter in awake volunteers. Anesthesiology. 2008;109:806–810. doi: 10.1097/ALN.0b013e31818a37dc. [DOI] [PubMed] [Google Scholar]
- 9.Kwiatek MA, Pandolfino JE, Hirano I, Kahrilas PJ. Esophagogastric junction distensibility assessed with an endoscopic functional luminal imaging probe (EndoFLIP) Gastrointest Endosc. 2010;72:272–278. doi: 10.1016/j.gie.2010.01.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ghosh SK, Kahrilas PJ, Brasseur JG. Liquid in the gastroesophageal segment promotes reflux, but compliance does not: a mathematical modeling study. Am J physiol Gastrointest Liver Physiol. 2008;295:G920–G933. doi: 10.1152/ajpgi.90310.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kahrilas PJ, Shi G, Manka M, Joehl RJ. Increased frequency of transient lower esophageal sphincter relaxation induced by gastric distention in reflux patients with hiatal hernia. Gatroenterology. 2000;118:688–695. doi: 10.1016/S0016-5085(00)70138-7. [DOI] [PubMed] [Google Scholar]
- 12.Pandolfino JE, Curry J, Shi G, joehl RJ, Brasseur JG, Kahrilas PJ. Restoration of normal distensive characteristics of the esophagogastric junction after fundoplication. Ann Surg. 2005;242:43–48. doi: 10.1097/01.sla.0000167868.44211.f0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hoppo T, McMahon BP, Witteman BP, et al. Functional lumen imaging probe to assess geometric changes in the esophagogastric junction following endolumenal fundoplication. J Gastrointest Surg. 2011;15:1112–1120. doi: 10.1007/s11605-011-1562-2. [DOI] [PubMed] [Google Scholar]
- 14.Fukazawa K, Furuta K, Adachi K, et al. Effects of mosapride on esophageal motor activity and esophagogastric junction compliance in healthy volunteers. J Gastroenterol. 2014;49:1307–1313. doi: 10.1007/s00535-013-0876-0. [DOI] [PubMed] [Google Scholar]
- 15.Koshino K, Adachi K, Furuta K, et al. Effects of mosapride on esophageal functions and gastroesophageal reflux. J Gastroenterol Hepatol. 2010;25:1066–1071. doi: 10.1111/j.1440-1746.2010.06280.x. [DOI] [PubMed] [Google Scholar]
- 16.Morita T, Furuta K, Adachi K, et al. Effects of rikkunshito (TJ-43) on esophageal motor function and gastroesophageal reflux. J Neurogastroenterol Motil. 2012;18:181–186. doi: 10.5056/jnm.2012.18.2.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dodds WJ, Hogan WJ, Helm JF, Dent J. Pathogenesis of reflux esophagitis. Gastroenterology. 1981;81:376–394. [PubMed] [Google Scholar]
- 18.Castell DO, Murray JA, Tutuian R, Orlando RC, Arnold R. Review article: the pathophysiology of gastrooesophageal reflux disease - oesophageal manifestations. Aliment Pharmacol Ther. 2004;20(suppl 9):14–25. doi: 10.1111/j.1365-2036.2004.02238.x. [DOI] [PubMed] [Google Scholar]
- 19.Boeckxstaens GE. Review article: the pathophysiology of gastrooesophageal reflux disease. Aliment Pharmacol Ther. 2007;26:149–160. doi: 10.1111/j.1365-2036.2007.03372.x. [DOI] [PubMed] [Google Scholar]
- 20.Scheurer U, Halter F. Lower esophageal sphincter in reflux esophagitis. Scand J Gastroenterol. 1976;11:629–634. [PubMed] [Google Scholar]
- 21.Kahrilas PJ, Dodds WJ, Hogan WJ, Kern M, Arndorfer RC, Reece A. Esophageal peristaltic dysfunction in peptic esophagitis. Gastroenterology. 1986;91:897–904. doi: 10.1016/0016-5085(86)90692-x. [DOI] [PubMed] [Google Scholar]
- 22.Dodds WJ, Dent J, Hogan WJ, et al. Mechanism of gastroesophageal reflux in patients with reflux esophagitis. N Engl J Med. 1982;307:1547–1552. doi: 10.1056/NEJM198212163072503. [DOI] [PubMed] [Google Scholar]
- 23.Dodds WJ. The pathogenesis of gastroesophageal reflux disease. AJR Am J Roentgenol. 1988;151:49–56. doi: 10.2214/ajr.151.1.49. [DOI] [PubMed] [Google Scholar]
- 24.Ho SC, Chang CS, Wu CY, Chen GH. Ineffective esophageal motility is a primary motility disorder in gastroesophageal reflux disease. Dig Dis Sci. 2002;47:652–656. doi: 10.1023/A:1017992808762. [DOI] [PubMed] [Google Scholar]
- 25.Wong WM, Lai KC, Hui WM, et al. Pathophysiology of gastroesophageal reflux diseases in Chinese - role of transient lower esophageal sphincter relaxation and esophageal motor dysfunction. Am J Gastroenterol. 2004;99:2088–2093. doi: 10.1111/j.1572-0241.2004.30417.x. [DOI] [PubMed] [Google Scholar]
- 26.Chitkara DK, Fortunato C, Nurko S. Esophageal motor activity in children with gastroesophageal reflex disease and esophagitis. J Pediatr Gastroenterol Nutr. 2005;40:70–75. doi: 10.1097/00005176-200501000-00013. [DOI] [PubMed] [Google Scholar]
- 27.Iwakiri K, Kawami N, Sano H, et al. Mechanism of excessive esophageal acid exporsure in patients with reflux esophagitis. Dig Dis Sci. 2009;54:1686–1692. doi: 10.1007/s10620-008-0542-1. [DOI] [PubMed] [Google Scholar]
- 28.Furukawa N, Iwakiri R, Koyama T, et al. Proportion of reflux esophagitis in 6010 Japanese adults: prospective evaluation by endoscopy. J Gastroenterol. 1993;34:441–444. doi: 10.1007/s005350050293. [DOI] [PubMed] [Google Scholar]
- 29.Matsumoto S, Tagawa M, Amejima H, et al. Absorption, distribution and excretion of [carbonyl-14C] mosapride citrate after a single oral administration in rats, dogs and monkeys. Arzneimittelforschung. 1993;43:1084–1094. [PubMed] [Google Scholar]
- 30.Herberg LJ, Wishart TB. Selective permeation of the blood-brain barrier as a cause of the anomalous properties of ‘atypical’ neuroleptics. Pharmacol Biochem Behav. 1980;12:871–873. doi: 10.1016/0091-3057(80)90447-5. [DOI] [PubMed] [Google Scholar]
- 31.Brouwers JR, Assies J, Wiersinga WM, Huizing G, Tytgat GN. Plasma prolactin levels after acute and subchronic oral administration of domperidone and of metoclopramide: a cross-over study in healthy volunteers. Clin Endocrinol. 1980;12:435–440. doi: 10.1111/j.1365-2265.1980.tb02733.x. [DOI] [PubMed] [Google Scholar]
- 32.Pandolfino JE, Shi G, Trueworthy B, Kahrilas PJ. Esophagogastric junction opening during relaxation distinguishes nonhernia reflux patients, hernia patients, and normal subjects. Gastroenterology. 2003;125:1018–1024. doi: 10.1016/S0016-5085(03)01210-1. [DOI] [PubMed] [Google Scholar]
- 33.Tucker E, Sweis R, Anggiansah A, et al. Measurement of esophagogastric junction cross-sectional area and distensibility by an endoluminal functional lumen imaging probe for the diagnosis of gastroesophageal reflux disease. Neurogastroenterol Motil. 2013;25:904–910. doi: 10.1111/nmo.12218. [DOI] [PubMed] [Google Scholar]