Abstract
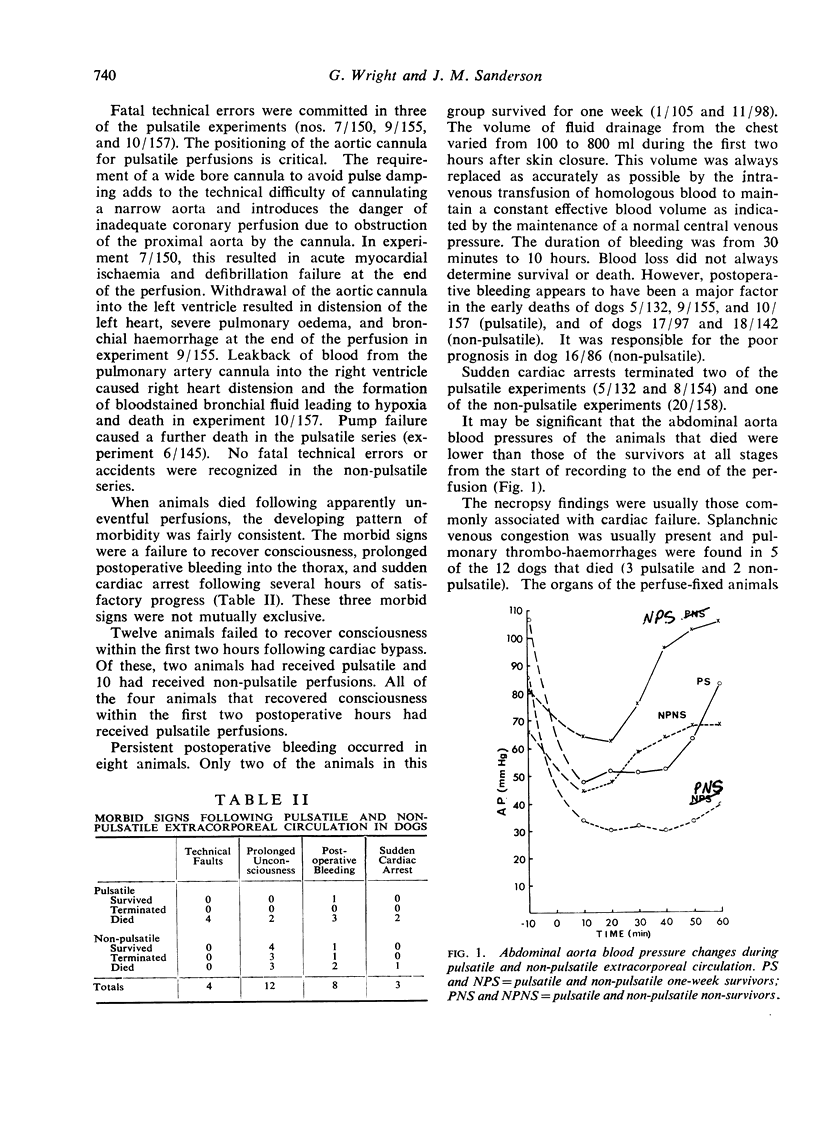
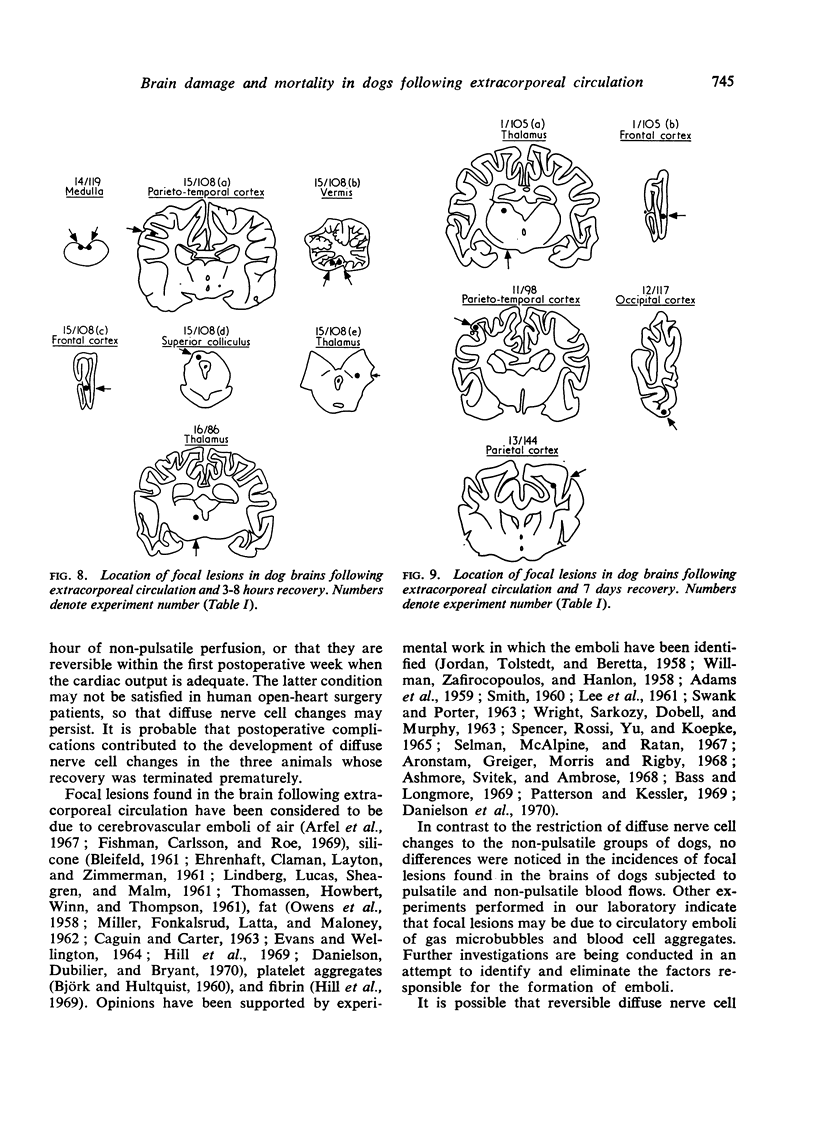
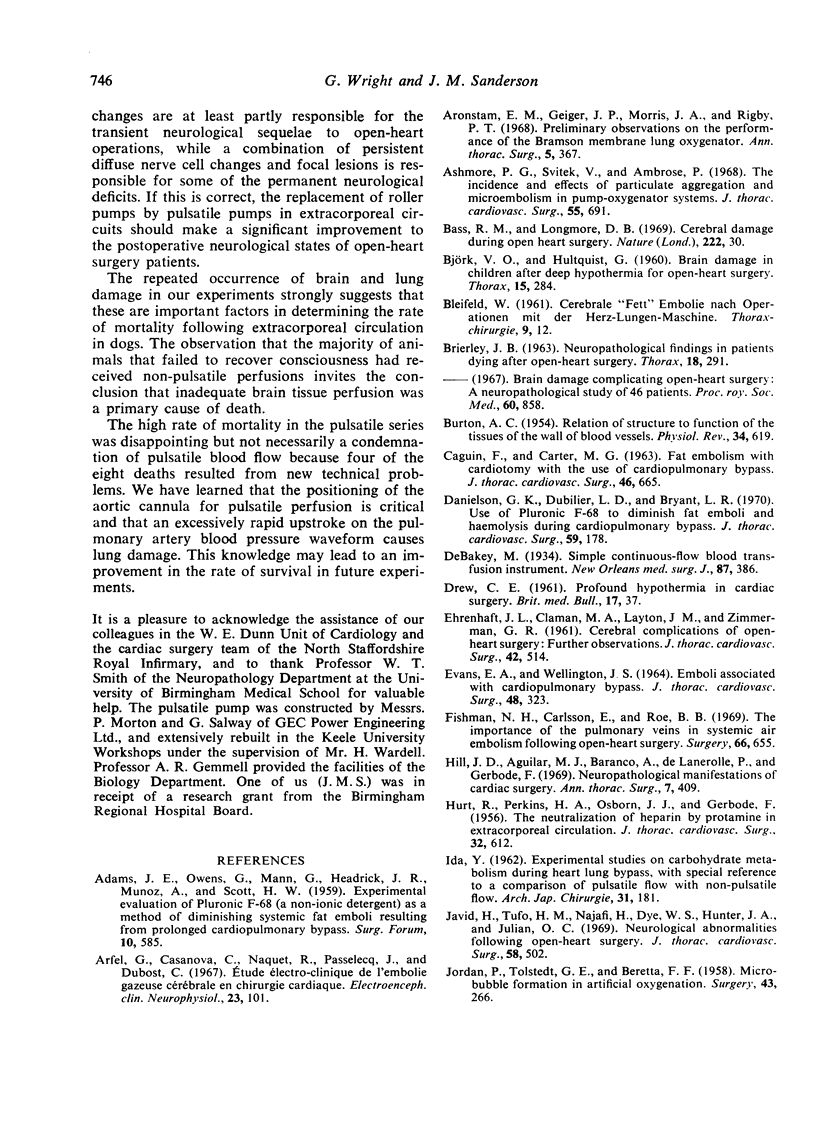
In a series of 20 dog experiments, total cardiac bypass was followed by a high rate of mortality during the first 12 postoperative hours. Only five dogs survived for one week, but a further three dogs were perfuse-fixed after shorter periods of survival. All dogs developed pulmonary alveolar haemorrhages and seven of the eight perfuse-fixed brains exhibited brain damage. Diffuse nerve cell changes were found in the brains of dogs subjected to non-pulsatile blood flow. Focal brain lesions were found following both pulsatile and non-pulsatile blood flows. The lesions varied from staining pallor and rarefaction of the neuropil to total nerve cell loss and glial infiltration depending upon the duration of survival. When considered in conjunction with a previous series of experiments, these results show that the diffuse nerve cell changes associated with roller pump perfusions can be avoided by using a new pulsatile pump, but focal brain damage was not eliminated, and lung damage and mortality were not reduced.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- ADAMS J. E., OWENS G., MANN G., HEADRICK J. R., MUNOZ A., SCOTT H. W., Jr Experimental evaluation of pluronic F68 (A non-ionic detergent) as a method of diminishing systemic fat emboli resulting from prolonged cardiopulmonary bypass. Surg Forum. 1960;10:585–589. [PubMed] [Google Scholar]
- Arfel G., Casanova C., Naquet R., Passelecq J., Dubost C. Etude électro-clinique de l'embolie gazeuse cérébrale en chirurgie cardiaque. Electroencephalogr Clin Neurophysiol. 1967 Aug;23(2):101–122. doi: 10.1016/0013-4694(67)90101-0. [DOI] [PubMed] [Google Scholar]
- Aronstam E. M., Geiger J. P., Morris J. A., Jr, Rigby P. T. Preliminary observations on the performance of the Bramson membrane lung oxygenator. Ann Thorac Surg. 1968 Apr;5(4):367–370. doi: 10.1016/s0003-4975(10)66359-x. [DOI] [PubMed] [Google Scholar]
- Ashmore P. G., Svitek V., Ambrose P. The incidence and effects of particulate aggregation and microembolism in pump-oxygenator systems. J Thorac Cardiovasc Surg. 1968 May;55(5):691–697. [PubMed] [Google Scholar]
- BRIERLEY J. B. NEUROPATHOLOGICAL FINDINGS IN PATIENTS DYING AFTER OPEN-HEART SURGERY. Thorax. 1963 Dec;18:291–304. doi: 10.1136/thx.18.4.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BURTON A. C. Relation of structure to function of the tissues of the wall of blood vessels. Physiol Rev. 1954 Oct;34(4):619–642. doi: 10.1152/physrev.1954.34.4.619. [DOI] [PubMed] [Google Scholar]
- Bass R. M., Longmore D. B. Cerebral damage during open heart surgery. Nature. 1969 Apr 5;222(5188):30–33. doi: 10.1038/222030a0. [DOI] [PubMed] [Google Scholar]
- CAGUIN F., CARTER M. G. FAT EMBOLIZATION WITH CARDIOTOMY WITH THE USE OF CARDIOPULMONARY BYPASS. J Thorac Cardiovasc Surg. 1963 Nov;46:665–672. [PubMed] [Google Scholar]
- DREW C. E. Profound hypothermia in cardiac surgery. Br Med Bull. 1961 Jan;17:37–42. doi: 10.1093/oxfordjournals.bmb.a069861. [DOI] [PubMed] [Google Scholar]
- Danielson G. K., Dubilier L. D., Bryant L. R. Use of Pluronic F-68 to diminish fat emboli and hemolysis during cardiopulmonary bypass. A controlled clinical study. J Thorac Cardiovasc Surg. 1970 Feb;59(2):178–184. [PubMed] [Google Scholar]
- EVANS E. A., WELLINGTON J. S. EMBOLI ASSOCIATED WITH CARDIOPULMONARY BYPASS. J Thorac Cardiovasc Surg. 1964 Aug;48:323–330. [PubMed] [Google Scholar]
- Fishman N. H., Carlsson E., Roe B. B. The importance of the pulmonary veins in systemic air embolism following open-heart surgery. Surgery. 1969 Oct;66(4):655–662. [PubMed] [Google Scholar]
- GERBODE F., HURT R., OSBORN J. J., PERKINS H. A. The neutralization of heparin by protamine in extracorporeal circulation. J Thorac Surg. 1956 Nov;32(5):612–619. [PubMed] [Google Scholar]
- Hill J. D., Aguilar M. J., Baranco A., de Lanerolle P., Gerbode F. Neuropathological manifestations of cardiac surgery. Ann Thorac Surg. 1969 May;7(5):409–419. doi: 10.1016/s0003-4975(10)66203-0. [DOI] [PubMed] [Google Scholar]
- JORDAN P., Jr, TOLSTEDT G. E., BERETTA F. F. Microbubble formation in artificial oxygenation. Surgery. 1958 Feb;43(2):266–269. [PubMed] [Google Scholar]
- Javid H., Tufo H. M., Najafi H., Dye W. S., Hunter J. A., Julian O. C. Neurological abnormalities following open-heart surgery. J Thorac Cardiovasc Surg. 1969 Oct;58(4):502–509. [PubMed] [Google Scholar]
- LEE W. H., Jr, KRUMHAAR D., FONKALSRUD E. W., SCHJEIDE O. A., MALONEY J. V., Jr Denaturation of plasma proteins as a cause of morbidity and death after intracardiac operations. Surgery. 1961 Jul;50:29–39. [PubMed] [Google Scholar]
- LINDBERG D. A., LUCAS F. V., SHEAGREN J., MALM J. R. Silicone embolization during clinical and experimental heart surgery employing a bubble oxygenator. Am J Pathol. 1961 Aug;39:129–144. [PMC free article] [PubMed] [Google Scholar]
- OWENS G., ADAMS J. E., DAWSON R. E., LANCE E. M., SAWYERS J. L., SCOTT H. W., Jr Observed central nervous system responses during experimental employment of various pump-oxygenators. Surgery. 1958 Jul;44(1):240–254. [PubMed] [Google Scholar]
- Patterson R. H., Jr, Kessler J. Microemboli during cardiopulmonary bypass detected by ultrasound. Surg Gynecol Obstet. 1969 Sep;129(3):505–510. [PubMed] [Google Scholar]
- SMITH W. T. Cerebral lesions due to emboli of silicone anti-foam in dogs subjected to cardiopulmonary bypass. J Pathol Bacteriol. 1960 Jul;80:9–18. doi: 10.1002/path.1700800103. [DOI] [PubMed] [Google Scholar]
- SPENCER F. C., ROSSI N. P., YU S. C., KOEPKE J. A. THE SIGNIFICANCE OF AIR EMBOLISM DURING CARDIOPULMONARY BYPASS. J Thorac Cardiovasc Surg. 1965 Apr;49:615–634. [PubMed] [Google Scholar]
- SWANK R. L., PORTER G. A. Disappearance of micro-emboli transfused into patients during cardiopulmonary bypass. Transfusion. 1963 May-Jun;3:192–197. doi: 10.1111/j.1537-2995.1963.tb04619.x. [DOI] [PubMed] [Google Scholar]
- Sanderson J. M., Wright G., Sims F. W. Brain damage in dogs immediately following pulsatile and non-pulsatile blood flows in extracorporeal circulation. Thorax. 1972 May;27(3):275–286. doi: 10.1136/thx.27.3.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selman M. W., McAlpine W. A., Ratan R. S. The effectiveness of various heart-lung machines in the elimination of microbubbles from the circulation. J Thorac Cardiovasc Surg. 1967 May;53(5):613–617. [PubMed] [Google Scholar]
- Shepard R. B., Kirklin J. W. Relation of pulsatile flow to oxygen consumption and other variables during cardiopulmonary bypass. J Thorac Cardiovasc Surg. 1969 Nov;58(5):694–passim. [PubMed] [Google Scholar]
- Shepard R. B., Simpson D. C., Sharp J. F. Energy equivalent pressure. Arch Surg. 1966 Nov;93(5):730–740. doi: 10.1001/archsurg.1966.01330050034005. [DOI] [PubMed] [Google Scholar]
- Trinkle J. K., Helton N. E., Wood R. E., Bryant L. R. Metabolic comparison of a new pulsatile pump and a roller pump for cardiopulmonary bypass. J Thorac Cardiovasc Surg. 1969 Oct;58(4):562–569. [PubMed] [Google Scholar]
- WRIGHT E. S., SARKOZY E., DOBELL A. R., MURPHY D. R. Fat globulemia in extracorporeal circulation. Surgery. 1963 Apr;53:500–504. [PubMed] [Google Scholar]
- Wright G., Sanderson J. M. Improved method for fixation of dog brain by vascular perfusion. J Pathol. 1970 Apr;100(4):295–305. doi: 10.1002/path.1711000409. [DOI] [PubMed] [Google Scholar]