Abstract
An increasing body of literature indicates that discrimination has a negative impact on health; poor sleep may be an underlying mechanism. The primary objective of this review was to examine existing studies on the relationship between discrimination and sleep to clarify (a) the potential role of discrimination in shaping population patterns of sleep and sleep disparities, and (b) research needed to develop interventions at individual and institutional levels. We identified articles from English-language publications in Pubmed and Ebsco databases from inception through July 2014. We employed a broad definition of discrimination to include any form of unfair treatment and all self-reported and objectively-assessed sleep outcomes, including duration, difficulties, and sleep architecture. Seventeen studies were identified: four prospective, twelve cross-sectional, and one that utilized a daily-diary design. Fifteen of the 17 studies evaluated interpersonal discrimination as the exposure and the majority of studies included self-reported sleep as the outcome. Only four studies incorporated objective sleep assessments. All 17 studies identified at least one association between discrimination and a measure of poorer sleep, although studies with more detailed consideration of either discrimination or sleep architecture revealed some inconsistencies. Taken together, existing studies demonstrate consistent evidence that discrimination is associated with poorer sleep outcomes. This evidence base can be strengthened with additional prospective studies that incorporate objectively-measured aspects of sleep. We outline important extensions for this field of inquiry that can inform the development of interventions to improve sleep outcomes, and consequently promote wellbeing and reduce health inequities across the life course.
Keywords: sleep, discrimination, unfair treatment, racism, sexism, prejudice, systematic review
An estimated 50 to 70 million adults in the United States have disordered or insufficient sleep (1). Sleep disorders and sleep deprivation have been found to increase risk for a variety of adverse health outcomes including mood disorders (2), substance abuse disorders (3), central adiposity and obesity (4-6), immune function (7, 8), diabetes (9, 10), hypertension (11), heart disease (12, 13), and mortality (14-17). Sleep problems are also associated with increased functional impairment, including employee absenteeism, lower work productivity, and medical errors (18). The Institute of Medicine reports that hundreds of billions of dollars each year are spent on direct and indirect costs associated with sleep loss and sleep disorders (1, 18-20), and sleep health is a key goal of the U.S. Department of Health and Human Services’ Healthy People 2020 (21).
Nationally-representative and community-based studies in the US show that sleep characteristics vary by race and ethnicity (22-27), immigration history (28), and socioeconomic status (SES) (23, 25), with disadvantaged groups typically showing poorer sleep-related outcomes. For example, using objective assessments, the Coronary Artery Risk Development in Young Adults (CARDIA) study found that Black respondents had shorter sleep duration, poorer sleep efficiency, and greater sleep latency compared to White respondents (22). In order to address the national burden of sleep loss and disorders, and racial/ethnic and socioeconomic inequalities in sleep health, it is critical to identify potentially modifiable risk factors for sleep problems among disadvantaged groups.
Discrimination—defined as differential or unfair treatment based on actual or perceived membership in a group (29)—can occur based on race/ethnicity, national origin, religion, gender, sexual orientation, SES, or other social factors, and is increasingly recognized as a determinant of health across the life course (30-35). Discrimination can occur at multiple levels, including institutional discrimination, which refers to unfair institutional policies or practices, as well as interpersonal discrimination, which typically refers to perceived discriminatory interactions within social encounters (35-37). Building on initial discrimination and health research, there is now great interest in identifying the underlying mechanisms through which discrimination affects health. Insufficient or poor quality sleep may be one pathway that connects perceived discrimination to physical and mental health problems (38, 39), and a growing literature has documented sleep as a mediator of the relationship between stressors and health (40-43). Experiences of discrimination could impact sleep directly through a variety of mechanisms, such as activating feelings of threat, arousal, vigilance (44), psychological distress (e.g., depression, anxiety, cynical hostility, anger) (45-47), or physiological changes (e.g., hypothalamic pituitary adrenal axis dysfunction, sympathetic nervous system hyperactivation) (48) that impede high quality sleep.
The primary aim of this study is to review existing studies of the relationship between discrimination and sleep, and evaluate whether this association is maintained after adjusting for important confounders, as systematic consideration of this literature can elucidate the role of discrimination in shaping population-level patterns of sleep and sleep disparities. The secondary aim is to discuss important directions for research that can inform interventions.
METHODS
We conducted a systematic review of all English-language articles published in Pubmed, Web of Science, and Ebsco databases (PsychInfo, ERIC, CINAHL) from 1971 through July 2014. Our search strategy was informed by prior literature reviews on discrimination and health (30, 32, 49). Medical Subject Headings (MeSH) of the National Library of Medicine and keywords were used to search Pubmed, and a similar search was designed for the Ebsco databases (see Appendix 1 for sample search strategy). We also searched reference lists of selected articles and relevant review articles for applicable studies. Studies identified in the database searches were assessed for relevance based on title and abstract, and selected studies were obtained in full and assessed for inclusion criteria. Studies were included if they analyzed perceived discrimination, unfair treatment, prejudice, or organization injustice in relation to one or more characteristics of sleep such as insomnia, poor sleep quality, or sleep duration. For each selected article, we extracted data related to: study design, sample size, sample age, geographic location, measurement of discrimination, measurement of sleep, covariates, and results.
RESULTS
Description of Included Studies
Our database search identified 453 records; after excluding duplications (n=96), 17 articles were selected for further evaluation, and two additional studies were identified from reference sections. A total of 17 articles met inclusion criteria for this review (see Figure 1 for Flow Diagram). Characteristics of the selected studies are presented in Table 1. The earliest study on discrimination and sleep was published in 2003 (50). Twelve of the 17 studies were cross-sectional, three were observational prospective studies (50-52), one included a 9-day daily diary component (46), and one included a natural experiment with an intervention (53). The sample sizes ranged from 93 (54) to 10,039 (55), with a median of 1,523 participants. Eleven of the 16 studies took place in the United States; the others were conducted in Finland (50), Brazil (56), Korea (55, 57), Sweden (58), and the United Kingdom (51). Only two of the 17 studies used samples comprised of children or adolescents (56, 59). Across studies, three measured discrimination using a single item (39, 56, 60), while the majority used multiple-items scores. The majority of studies evaluated interpersonal discrimination, while one study assessed the impact of unfair treatment at the institutional level (a pay cut to all nurses) on sleep problems (53), and another study evaluated race-related vigilance (i.e., the extent to which participants anticipated and prepared for racial discrimination) (61). Some studies specifically evaluated racial/ethnic discrimination (54, 59-64), and others focused on unfair treatment in the workplace (50, 51, 53, 55, 57, 64) or in healthcare (60).
Figure 1.
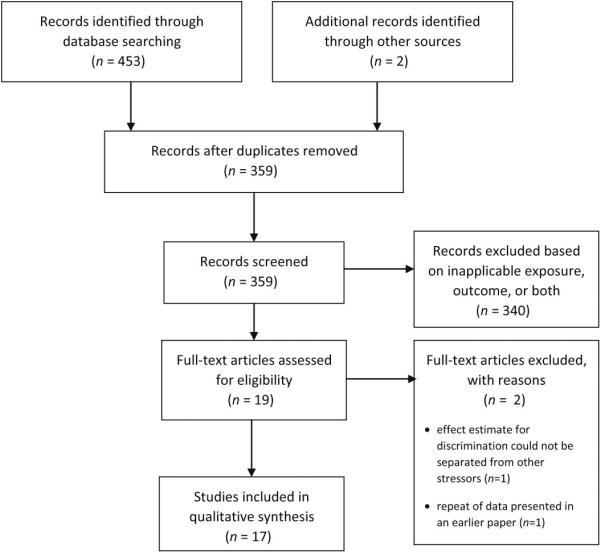
Flow Diagram
Table 1.
Studies on perceived unfair treatment and sleep outcomes (n = 17)
| Study | Sample a | Design | Exposure | Outcome(s) | Covariates | Findings |
|---|---|---|---|---|---|---|
| Elovainio et al. (50) | Male and female hospital employees in 10 Finnish hospitals (N=3,773, mean age=44.4 years) | Prospective | Procedural Justice Scale (8 items) Relational Justice Scale (7 items) |
Self-reported sleep difficulties (4 items) | Age, sex, income, smoking, alcohol, physical activity | • Positive associations for both |
| Greenberg (53) | Male and female nurses in 4 US hospitals (N=467) | Prospective, natural experiment with an intervention | Organizational injustice (pay cut) | Self-reported insomnia (4 items) | None/NA (demographics balanced between groups) | • Positive association; conditional on supervisor training in interactional justice |
| Steffen et al. (62) | Community-based sample of Hispanic-American male and female immigrants in Provo, UT (N=168, mean age=33 years) | Cross-sectional | Perceived Racism Scale (51 items) | Self-reported sleep disturbance (PSQI, 19 items) | Gender, income, education | • Positive association |
| Taloyan et al. (58) | Swedish and Kurdish immigrant men in the 1996 Swedish National Survey of Immigrants and Swedish Level-of-Living Survey (N=1,523, age range=27 to 60 years) | Cross-sectional | Perceptions of equal treatment, relative to Swedish citizens (9 items) | Self-reported sleep difficulties (1 item) | Age, marital status, education, home ownership, employment, number of children | • Positive association |
| Thomas et al. (54) | Community sample of employed African American (mean age=38.1 years) and White (mean age=35.6 years) males and females in California (N=93) | Cross-sectional | Perceived Discrimination subscale of the Scale of Ethnic Experience (9 items) | Self-reported fatigue (MSFI-SF, 30 items) PSG-assessed TST, sleep latency, sleep efficiency, WASO, REM sleep, and slow-wave sleep (Stages 3 and 4) |
Age, BMI, hypertension status, cigarette smoking, CES-D score | • Positive association with fatigue (not significant after control for depressive symptoms) • Negative association with Stage 4 sleep (significant after control for depressive symptoms) |
| Bittencourt et al.(56) | Representative sample of 7th grade male and female students in Gravatai, South Brazil (N=1,170, age range=12 to 18 years) | Cross-sectional | Discrimination in past 30 days (1 item) | Self-reported sleep difficulty (1 item) | Sex, ethnicity, SES, school absenteeism, peer relationships, use of alcohol, tobacco, and other drugs, parental empathy, # of friends, body image concerns, loneliness, sadness, suicidal ideation, fear of going to school, fights, insults | • Positive association |
| Elovainio et al. (51) | Male and females in the Whitehall II study of white-collar British civil servants (N=5,209, mean age=44.2 years) | Prospective | Justice scale (10 items) | Self-reported sleep problems (sleep onset: 1 item; unrefreshing sleep: 1 item; sleep maintenance: 2 items) | Age, employment grade, BMI, alcohol consumption, smoking, job strain, baseline sleeping problems, baseline depressive symptoms | • Men: positive association with overall sleep problem score and all 3 components • Women: positive association with overall sleep problem score and non-refreshing sleep |
| Beatty et al. (65) | Middle-aged males and females in the Pittsburgh, PA metropolitan area, recruited as part of HeartSCORE, a larger study (N=210, mean age=59.9 years) | Cross-sectional and daily diary (10 days) | Detroit Area Study Everyday Unfair Treatment Scale (9 items) plus one additional item (10 items total) | Self-report: diary sleep quality (2 items), sleep quality (PSQI, 18 items), daytime sleepiness (Epworth Sleepiness Scale, 8 items) Objective measures: actigraphy (duration, efficiency), PSG (duration, efficiency, WASO, Stage 3-4 sleep, REM sleep, Apnea-Hypopnea Index) |
Age, gender, race/ethnicity, BMI, hypertensive status and/or related medication use, composite SES, and other psychosocial characteristics (anger, anxiety, hostility, and depressive symptoms, analyzed separately) | • In models with basic demographic covariates: positive associations with poorer self-reported sleep quality and greater daytime sleepiness; negative association with actigraphy- and PSG-assessed sleep duration and efficiency and PSG-assessed proportion of REM sleep. • All sig. associations remained after adjustment for depression and hostility; for models adjusting for trait anger and anxiety, there were some exceptions. • Conditional association: unfair treatment associated with > WASO in Whites but not in African Americans. |
| Kim et al. (57) | Korean male and female employees recruited as part of a nationwide random sample (N=8,155) | Cross-sectional | Organizational injustice (4 items) | Self-reported insomnia (3 items) | Age, marital status, education, industrial type, company size, employment status, work schedule, job type, working hours, alcohol, smoking, exercise, BMI, and treated diseases | • Positive association |
| Grandner et al. (60) | Male and female adults from the Michigan and Wisconsin 2006 Behavioral Risk Factor Surveillance System (N=7,148, mean age=50.9 years) | Cross-sectional | Racism in health care setting (1 item) | Self-reported sleep disturbance (1 item) and daytime fatigue (1 item) | Age, gender, race/ethnicity, education, income, marital status, employment | • Positive associations |
| Tomfohr et al. (63) | African American (mean age=38.2 years) and White (mean age=33.4 years) male and female San Diego residents participating in larger study on vascular health disparities (N=164) | Cross-sectional | Perceived Discrimination subscale from the Scale of Ethnic Experience (9 items) | Objectively measured sleep via PSG (TST, sleep efficiency, sleep latency, WASO, Stages 1 and 2, slow wave sleep (composed of Stages 3 and 4), REM) | Age, BMI, SES, smoking, race/ethnicity | • Positive association with proportion of Stage 2 sleep (light sleep) • Inverse association with proportion of slow-wave sleep (deep sleep) |
| Huynh et al. (59) | Latino and Asian American 11th and 12th grade male and female students recruited from 2 Southern California high schools (N=360, mean age=17.2 years) | Cross-sectional | Overt discrimination by peers and adults (14 items) Ethnic Microaggressions Scale (“subtle discrimination”; 12 items) |
Self-reported sleep quality (2 items) Self-reported average hours of night time sleep |
Sex, race/ethnicity, perceived stress, socioeconomic status | • Positive associations between overt and subtle discrimination and sleep quality; association between overt discrimination and sleep quality conditional on school belonging • Negative association between subtle discrimination and sleep duration |
| Lewis et al. (52) | African American, White, and Chinese women from Study of Women's Health Across the Nation Sleep Study (N=368, mean age=51 years) | Prospective | Everyday Discrimination Scale (10 items) | Self-reported subjective sleep complaints (PSQI, 19 items) Objectively measured sleep via PSG (sleep latency, WASO, total sleep time, Stages 3 and 4, and REM) |
Age, race/ethnicity, financial strain, BMI, menopausal status, depressive symptoms, uses of medication that impact sleep, education | • Positive association with subjective sleep complaints and PSG-assessed WASO |
| Park et al. (55) | Representative sample of working male and female adults in the First Korean Working Conditions Survey (N=10,039, mean age=42 years) | Cross-sectional | Discrimination by age (1 item) and sex (1 item) | Self-reported sleep problems (1 item) | Sex, age, education, income, smoking status, alcohol consumption, presence of illness, employment status, job type, employment contract, working hours, work schedule | • Positive associations for sex discrimination and age discrimination |
| Chen et al. (39) | Male and female respondents in the Public Health Management Corporation's 2008 Southeastern Pennsylvania Household Health Survey (N=9,880, mean age=52.3 years) |
Cross-sectional | Single item | Self-report sleep quality (1 item) | Age, sex, marital status, income, education, race/ethnicity | • Positive association |
| Hicken et al. (61) | White, Black, and Hispanic males and females in the Chicago Community Adult Health Study (N=3,094, mean age=42.4 years) | Cross-sectional | Racism-related vigilance (3 items) | Self-reported sleep difficulty (3 items) | Age, gender, education, income, | • Positive association |
| Slopen et al. (64) | White, Black, and Hispanic males and females in the Chicago Community Adult Health Study (N=2,983, mean age=42.3 years) | Cross-sectional | Everyday discrimination (5 items) Major experiences of discrimination (4 items) Workplace harassment and incivilities (2 items) |
Self-reported sleep difficulty (3 items) Self-reported sleep duration |
Age, sex, race/ethnicity, income, education, acute events, childhood adversity, and financial, community, employment, and relationship stressors | • Positive associations between racial and non-racial everyday discrimination and sleep difficulties • Inverse association between major experiences of discrimination attributed to race/ethnicity and sleep duration |
Mean age provided when available.
PSG=polysomnography; WASO=wakefulness after sleep onset; REM=rapid eye movement; BMI=body mass index; TST=total sleep time; PSQI=Pittsburgh Sleep Quality Index; MFSI-SF=Multidimensional Fatigue Symptom Inventory-Short Form; CES-D=Center for Epidemiologic Studies-Depression scale; SES=socioeconomic status.
Sixteen of the 17 studies evaluated self-reported sleep difficulties and/or daytime fatigue, and 12 of these studies exclusively relied on self-reported sleep outcomes. There was large variation in the self-report measures of sleep difficulties, ranging from single-item measures of sleep problems or daytime fatigue (39, 55, 56, 58, 60), self-reported sleep duration (59, 64), to extensively validated scales such as the Pittsburgh Sleep Quality Index (46, 52, 62), the Epworth Sleepiness Scale (46), and the Multidimensional Fatigue Symptom Inventory-Short Form (54). One study used actigraphy to measure sleep duration and efficiency (46), and four studies evaluated polysomnography- (PSG) assessed sleep outcomes (46, 52, 54, 63), including duration, efficiency, sleep latency, wake after sleep onset (WASO), rapid eye movement (REM) sleep, light sleep, and Stages 3 and 4 sleep. All studies controlled for basic demographic characteristics, including age, sex, and race (if appropriate based on the sample), and nearly all studies adjusted for SES. Roughly half of the studies adjusted for mental or physical health or health behavior covariates (e.g., BMI, depression, cigarette smoking, alcohol use, physical activity) (46, 50-52, 54, 55, 57, 63), and five studies adjusted for other psychosocial stressors in addition to discrimination (51, 52, 56, 59, 64).
Associations between discrimination and sleep outcomes
Self-reported sleep difficulties
All sixteen studies that included a measure of self-reported sleep problems reported positive associations between discrimination and outcomes including sleep difficulties or insomnia (39, 50-53, 55-62, 64, 65) and fatigue (54, 60, 65). The strongest evidence comes from the three prospective cohort studies (50-52) and the natural experiment (53). For example, a study of 368 African American, White, and Chinese women from the Study of Women's Health Across the Nation (SWAN) Sleep Study found that chronic everyday discrimination (collected annually for four years and averaged) was associated with more sleep complaints, independent of financial strain and a variety of health characteristics, including depressive symptoms (52). Similarly, among 5,209 males and females in the Whitehall II study of white collar British civil servants, organizational injustice (defined as perceived unfairness to employees by the system or its agents (51)) was associated with poorer sleep, even after controlling for baseline sleeping problems, depressive symptoms, health behaviors, and employment grade (51). In a natural experiment of 467 nurses, organizational injustice (resulting from a change in payment policy in two of four study hospitals) was associated with greater insomnia among nurses who experienced organizational injustice relative to nurses who did not (53). Notably, this study also found that degree of insomnia was moderated by supervisor training in interactional justice, whereby insomnia ratings were lower among nurses whose supervisors had received this training.
Sleep duration (self-reported and objectively measured)
Two of the six studies that evaluated discrimination in relation to sleep duration used self-reported duration (59, 64), and these studies had partially consistent findings. A study of 360 high school students found an inverse association between subtle ethnic discrimination (but not overt discrimination) and sleep duration (59). A probability sample of 2,983 adults in Chicago found an inverse association between major experiences of discrimination attributed to race/ethnicity (but not everyday discrimination attributed to race/ethnicity) and sleep duration in models adjusted for other forms of discrimination and multiple other types of psychosocial stress (64). The four studies that used PSG and/or actigraphy to assess sleep duration had mixed results (52, 54, 63, 65): one study of 210 adults in Pittsburgh found that everyday discrimination was associated with shorter actigraphy and PSG-assessed sleep duration (46), while significant associations were not observed in the three other studies (52, 54, 63).
Other Objectively-measured sleep quality characteristics
All four studies that assessed sleep using objective measures (52, 54, 63, 65) reported at least one association in the expected direction, however these studies did not include identical outcomes for comparison and there was variation across associations that were observed. For example, all four studies examined discrimination in relation to WASO, but associations were observed in only 2 of the 4 studies (52): the SWAN Sleep Study found a positive association between everyday discrimination and PSG-assessed WASO (52), and a study of adults in Pittsburgh (N=210) found that a conditional association by race whereby everyday discrimination was associated with greater WASO among Whites, but not among African Americans (46). All four studies also evaluated discrimination in relation to REM sleep, but only one study found that discrimination was associated with a smaller proportion of REM sleep (46). Two of the four studies documented an inverse association between discrimination and proportion of slow wave sleep (Stages 3 and 4) (54, 63). One study examined discrimination in relation to light sleep (Stage 2) and found a positive association (63). Of the three studies that examined discrimination in relation to sleep efficiency, two reported null associations (54, 63) and one documented an inverse association (46).
Control for Depressive Symptoms
Three cross-sectional (46, 54, 56) and two longitudinal (51, 52) studies controlled for depressive symptoms either prior to (51) or concurrent with (46, 52, 54, 56) sleep outcomes. Across studies, associations were generally attenuated (to varying extents) by inclusion of depressive symptoms, yet in 17 of 20 tests of associations (given multiple outcomes in several of these studies) the significant associations were maintained.
DISCUSSION
This systematic review displays consistent evidence that experiences of discrimination are associated with disordered sleep and objectively-assessed sleep characteristics, although clarification is needed for nuanced aspects of this association. Although the majority of studies presented cross-sectional associations, three prospective studies and a natural experiment provide supporting evidence for the hypothesized temporal ordering (50-53). Among the studies using PSG- or actigraphy-assessed sleep measures, there was variation across studies with regard to the specific sleep components that were associated with discrimination; however, each study reported at least one association between discrimination and a sleep parameter that is suggestive of poorer sleep quality. Importantly, five of the included studies adjusted for depressive symptoms (46, 51, 52, 54, 56). These studies suggest the relationship between discrimination and poorer sleep is independent of depression. Given the well-documented associations between discrimination and depression (35) and sleep difficulties and depression (66)—so much so that disrupted sleep is one of the diagnostic criteria for depression on almost every scale—it is notable that the relationship between discrimination and sleep problems is not fully confounded or mediated by depressive symptoms.
Our review has identified several gaps and important extensions for this field of inquiry that can inform the development of interventions. First, identifying mediators of the association between discrimination and sleep problems is an important goal for future research. By examining underlying mechanisms within prospective observational studies, we can identify promising targets for future interventions. Several cross-sectional studies have explored potential mediators of the association between discrimination and sleep outcome (46, 59). For example, in a study of Latino and Asian American adolescents, Huynh and Gillen-O'Neel (59) found that the association between discrimination and sleep quality is partially explained by perceived stress (59). In another study, Beatty and colleagues (46) report that nightly worry partially mediate the associations of unfair treatment with sleep quality, daytime sleepiness, sleep efficiency, and proportion of REM sleep. Mediation studies with prospective data are needed in order to evaluate temporality and improve causal inference.
Second, little is known about whether discrimination impacts sleep differently across different demographic groups. In future studies, it will be valuable to explore potential subgroup differences (i.e., effect modification) by age and sex, given that both sleep problems (26) and self-reported experiences of discrimination (67) vary based on these characteristics. Further, only two studies examined discrimination in relation to sleep outcomes in children or adolescents (34, 68). Studies indicate that racial/ethnic disparities in sleep are evident before the age of 2 (69), discriminatory experiences are common among children (70, 71), and that sleep is associated with children's emotional and behavioral difficulties (72) and academic outcomes (73); therefore, this represents an important area of further inquiry.
Third, further research is needed to evaluate sleep as a mechanism linking discrimination to poorer health. Two cross-sectional studies in this review provide evidence that sleep may mediate associations between discrimination and depressive symptoms (62) and self-rated health (39); however, prospective studies, and studies with non-self-report outcomes are needed. For example, poor sleep is a known risk factor for metabolic syndrome and incident hypertension, and self-reported discrimination has been linked to metabolic indices (e.g. visceral fat (4) and blood pressure dysregulation (74)); studies have yet to examine whether the association between self-reported discrimination and these outcomes is partially or fully explained by poor sleep. If sleep does in fact function as a mediating mechanism, it suggests a potentially modifiable target for interventions to address health disparities resulting from discrimination. A meta-analysis (75) of 23 randomized controlled trials documented that behavioral interventions (e.g., relaxation and exercise (76), cognitive-behavioral treatment (77)) can lead to improvements in sleep quality, sleep latency, and wakening after sleep onset. More recent research suggests that web-based interventions to address sleep problems are also effective (78, 79). It is possible that implementing these types of interventions in individuals with high levels of self-reported discrimination might ultimately reduce the negative impact of discriminatory stressors on health. However, the initial, prospective studies establishing sleep as an important mechanism between discrimination and objective health outcomes have yet to be done.
Fourth, identifying individual- and contextual-level modifiers of the relationship between discrimination and sleep problems is also important for intervention development. For example, Huynh and Gillen-O'Neel's (59) study found that feelings of school belonging buffered against the negative impact of overt discrimination on sleep quality and duration reported by Latino and Asian American adolescents. Related, several studies examining other health outcomes suggest that multiple forms of discrimination could interact synergistically to influence sleep (80-82). One study of sexual minority men found an interaction between interpersonal and structural forms of discrimination in predicting tobacco and alcohol use (80); other studies identified interactions between interpersonal discrimination and internalized negative racial group bias in predicting cellular aging (81) and cardiovascular disease (82) among African American men. Fifth, recent research shows that occupation significantly modifies the association between sleep duration and race, whereby racial disparities for Blacks and Asians compared to Whites are widest among those holding professional occupations (83, 84). In future research, it will be valuable to examine the extent to which discrimination contributes to this pattern so that effective interventions can be developed.
Finally, nearly all of the identified studies evaluated experiences of interpersonal discrimination, with the exception of one study that used a direct measure of organizational injustice (rather than perceptions) (53) and one study on racism-related vigilance (61). Future research on discrimination and health (including sleep outcomes) will benefit from more extensive consideration of other forms of discrimination that co-occur with interpersonal discrimination (35, 37, 85), such as institutional or structural forms of discrimination (36, 86, 87), internalized discrimination (68, 88, 89), and culturally-salient events that evoke prejudice or race-related stress (i.e., “macro-racial stressors” (68)) which have been shown to predict a variety of health outcomes (90-92)). There could also be sleep-related consequences of state-level discriminatory policies shown to negatively impact other health outcomes among sexual minorities (93, 94) and immigrants (95). Experiences of discrimination could also impact sleep via circumstantial sequela or downstream consequences of discrimination, such as shift work, multiple jobs, crowded housing, unsafe neighborhood conditions, or financial strain. The threat of exposure to discrimination (or, racism-related vigilance) has also received limited attention to date (68, 88). An emerging field of research that includes both observational (61, 96-99) and experimental (100) studies suggests that anticipation of prejudice may be a significant and unique source of stress that has a detrimental influence on sleep (61), self-reported psychological and physical health (98, 99), and adverse cardiovascular traits, such as lower larger arterial elasticity among males (96), hypertension among Blacks (97), and greater blood pressure reactivity in a threat paradigm (100).
There are several limitations of the present review including the potential for under-representation of studies with null results due to publication bias (101). General limitations of the summarized studies include the cross-sectional design of many of the included studies which limits causal inference and also our ability to understand the potential role of depressive symptoms for observed associations (in studies where depression was included a potential confounder or mediator (46, 51, 52, 54, 56)). Only a few studies (54, 63, 64) evaluated the contribution of discrimination to racial/ethnic disparities in sleep duration or difficulties, thus we have a poor understanding of the role of discrimination for sleep disparities by race/ethnicity (22-27) or SES (23, 25) in the US. Despite these limitations, the existing literature has notable strengths, including many studies with multi-item measures of exposures and outcomes, several studies with PSG- or actigraphy-assessed outcomes, and a subset of studies with large and diverse samples representing a variety of racial/ethnic and socioeconomic groups.
In conclusion, the existing literature indicates that discrimination is associated with sleep problems and shorter sleep duration. Findings are fairly consistent across a range of study designs and populations. Scientific evidence for this association can be strengthened with additional prospective studies that incorporate objectively-measured aspects of sleep (102). This review also shows that there are many unanswered questions with regard to (1) the mediators of the association between discrimination and sleep problems, (2) how discrimination influences sleep in children or adolescents, (3) sleep as a mechanism linking discrimination to poorer health, (4) modifiers of the relationship between discrimination and sleep problems, including interactions between multiple forms of discrimination, (5) the extent to which discrimination contributes to disparities in sleep, and (6) the contributions of threat of discrimination, internalized discrimination, and structural or institutional forms of discrimination to sleep outcomes. Further research in these directions will advance our capacity to develop interventions at the individual and institutional levels to improve sleep-related outcomes, and consequently to promote wellbeing and reduce health inequities across the life course.
Supplementary Material
Research Highlights.
We identified 17 studies on the relationship between discrimination and sleep.
All 17 studies found at least one association between discrimination and worse sleep.
Studies with more detailed exposures and outcomes revealed some inconsistencies.
Longitudinal designs and studies using objective sleep assessments are needed.
Acknowledgments
Funding: N Slopen and DR Williams received support from grant RO1 AG038492. TT Lewis received support from grant K01HL092591.
Appendix 1. Pubmed Search Strategy
(“Sleep”[Mesh] OR “Sleep Disorders”[Mesh] OR “Polysomnography”[Mesh] or “sleep”[tiab] OR “sleep disorders”[tiab] OR “polysomnography”[tiab] OR “insomnia”[tiab]) AND (racism[Mesh] OR sexism[Mesh] OR ageism[Mesh] OR “Discrimination (Psychology)”[Mesh] OR “Social Discrimination”[Mesh] OR “Prejudice”[Mesh] OR “racial discrimination”[tiab] OR “perceived discrimination”[tiab] OR prejudice[tiab] OR “race discrimination”[tiab] OR “ethnic discrimination”[tiab] OR “social discrimination”[tiab] OR racialized[tiab] OR racialization[tiab] OR “Racism”[tiab] OR “sexism”[tiab] OR ageism[tiab] OR “unfair treatment”[tiab] OR “organizational injustice”[tiab]) AND English[lang] NOT (Editorial[ptyp] OR Letter[ptyp] OR Practice Guideline[ptyp] OR Case Reports[ptyp])
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Institute of Medicine . Sleep disorders and sleep deprivation: an unmet public health problem. The National Academies Press; Washington, DC: 2006. [PubMed] [Google Scholar]
- 2.Ford DE, Cooper-Patrick L. Sleep disturbances and mood disorders: An epidemiologic perspective. Depress Anxiety. 2001;14(1):3–6. doi: 10.1002/da.1041. [DOI] [PubMed] [Google Scholar]
- 3.Crum RM, Storr CL, Chan YF, Ford DE. Sleep disturbance and risk for alcohol-related problems. Am J Psychiat. 2004;161(7):1197–203. doi: 10.1176/appi.ajp.161.7.1197. [DOI] [PubMed] [Google Scholar]
- 4.Lewis TT, Kravitz HM, Janssen I, Powell LH. Self-reported Experiences of Discrimination and Visceral Fat in Middle-aged African-American and Caucasian Women. American Journal of Epidemiology. 2011;173(11):1223–31. doi: 10.1093/aje/kwq466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hunte HER. Association Between Perceived Interpersonal Everyday Discrimination and Waist Circumference Over a 9-Year Period in the Midlife Development in the United States Cohort Study. American Journal of Epidemiology. 2011;173(11):1232–9. doi: 10.1093/aje/kwq463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc Sci Med. 2010;71(5):1027–36. doi: 10.1016/j.socscimed.2010.05.041. [DOI] [PubMed] [Google Scholar]
- 7.Everson CA. Sustained sleep-deprivation impairs host-defense. Am J Physiol. 1993;265(5):R1148–R54. doi: 10.1152/ajpregu.1993.265.5.R1148. [DOI] [PubMed] [Google Scholar]
- 8.Ackermann K, Revell VL, Lao O, Rombouts EJ, Skene DJ, Kayser M. Diurnal rhythms in blood cell populations and the effect of acute sleep deprivation in healthy young men. Sleep. 2012;35(7):933–40. doi: 10.5665/sleep.1954. Epub 2012/07/04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ayas NT, White DP, Al-Delaimy WK, Manson JE, Stampfer MJ, Speizer FE, et al. A prospective study of self-reported sleep duration and incident diabetes in women. Diabetes Care. 2003;26(2):380–4. doi: 10.2337/diacare.26.2.380. [DOI] [PubMed] [Google Scholar]
- 10.Van Cauter E, Holmback U, Knutson K, Leproult R, Miller A, Nedeltcheva A, et al. Impact of sleep and sleep loss on neuroendocrine and metabolic function. Horm Res. 2007;67:2–9. doi: 10.1159/000097543. [DOI] [PubMed] [Google Scholar]
- 11.Gottlieb DJ, Redline S, Nieto FJ, Baldwin CM, Newman AB, Resnick HE, et al. Association of usual sleep duration with hypertension: The sleep heart health study. Sleep. 2006;29(8):1009–14. doi: 10.1093/sleep/29.8.1009. [DOI] [PubMed] [Google Scholar]
- 12.Ayas NT, White DP, Manson JE, Stampfer MJ, Speizer FE, Malhotra A, et al. A prospective study of sleep duration and coronary heart disease in women. Archives of Internal Medicine. 2003;163(2):205–9. doi: 10.1001/archinte.163.2.205. [DOI] [PubMed] [Google Scholar]
- 13.Qureshi AI, Giles WH, Croft JB, Bliwise DL. Habitual sleep patterns and risk for stroke and coronary heart disease: A 10-year follow-up from NHANES I. Neurology. 1997;48(4):904–11. doi: 10.1212/wnl.48.4.904. [DOI] [PubMed] [Google Scholar]
- 14.Cappuccio FP, D'Elia L, Strazzullo P, Miller MA. Sleep Duration and All-Cause Mortality: A Systematic Review and Meta-Analysis of Prospective Studies. Sleep. 2010;33(5):585–92. doi: 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Patel SR, Ayas NT, Malhotra MR, White DP, Schernhammer ES, Speizer FE, et al. A prospective study of sleep duration and mortality risk in women. Sleep. 2004;27(3):440–4. doi: 10.1093/sleep/27.3.440. [DOI] [PubMed] [Google Scholar]
- 16.Gallicchio L, Kalesan B. Sleep duration and mortality: a systematic review and meta- analysis. J Sleep Res. 2009;18(2):148–58. doi: 10.1111/j.1365-2869.2008.00732.x. [DOI] [PubMed] [Google Scholar]
- 17.Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Archives of General Psychiatry. 2002;59(2):131–6. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 18.Roth T. Comorbid Insomnia: Current Directions and Future Challenges. Am J Manag Care. 2009;15(1):S6–S13. [PubMed] [Google Scholar]
- 19.Hossain JL, Shapiro CM. The Prevalence, Cost Implications, and Management of Sleep Disorders: An Overview. Sleep Breath. 2002;6(2):85–102. doi: 10.1007/s11325-002-0085-1. [DOI] [PubMed] [Google Scholar]
- 20.Ozminkowski RJ, Wang SH, Walsh JK. The direct and indirect costs of untreated insomnia in adults in the United States. Sleep. 2007;30(3):263–73. doi: 10.1093/sleep/30.3.263. [DOI] [PubMed] [Google Scholar]
- 21.U.S. Department of Health and Human Services. Office of Disease Prevention and Health Promotion . Healthy People 2020. Washington, DC: 2012. [2012 August 30]. http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=38. [Google Scholar]
- 22.Lauderdale DS, Knutson KL, Yan LJL, Rathouz PJ, Hulley SB, Sidney S, et al. Objectively measured sleep characteristics among early-middle-aged adults - The CARDIA study. American Journal of Epidemiology. 2006;164(1):5–16. doi: 10.1093/aje/kwj199. [DOI] [PubMed] [Google Scholar]
- 23.Hall MH, Matthews KA, Kravitz HM, Gold EB, Buysse DJ, Bromberger JT, et al. Race and Financial Strain are Independent Correlates of Sleep in Midlife Women: The SWAN Sleep Study. Sleep. 2009;32(1):73–82. [PMC free article] [PubMed] [Google Scholar]
- 24.Mezick EJ, Matthews KA, Hall M, Strollo PJ, Buysse DJ, Kamarck TW, et al. Influence of race and socioeconomic status on sleep: Pittsburgh SleepSCORE project. Psychosomatic Medicine. 2008;70(4):410–6. doi: 10.1097/PSY.0b013e31816fdf21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Krueger PM, Friedman EM. Sleep Duration in the United States: A Cross-sectional Population-based Study. American Journal of Epidemiology. 2009;169(9):1052–63. doi: 10.1093/aje/kwp023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ram S, Seirawan H, Kumar SKS, Clark GT. Prevalence and impact of sleep disorders and sleep habits in the United States. Sleep Breath. 2010;14(1):63–70. doi: 10.1007/s11325-009-0281-3. [DOI] [PubMed] [Google Scholar]
- 27.Nunes J, Jean-Louis G, Zizi F, Casimir GJ, von Gizycki H, Brown CD, et al. Sleep duration among black and white Americans: Results of the National Health Interview Survey. Journal of the National Medical Association. 2008;100(3):317–22. doi: 10.1016/s0027-9684(15)31244-x. [DOI] [PubMed] [Google Scholar]
- 28.Hale L, Rivero-Fuentes E. Negative Acculturation in Sleep Duration Among Mexican Immigrants and Mexican Americans. J Immigr Minor Health. 2011;13(2):402–7. doi: 10.1007/s10903-009-9284-1. [DOI] [PubMed] [Google Scholar]
- 29.Williams DR, Lavizzo-Mourey R, Warren RC. The concept of race and health status in America. Public Health Reports. 1994;109(1):26. [PMC free article] [PubMed] [Google Scholar]
- 30.Priest N, Paradies Y, Trenerry B, Truong M, Karlsen S, Kelly Y. A systematic review of studies examining the relationship between reported racism and health and wellbeing for children and young people. Social Science & Medicine. 2013;95(0):115–27. doi: 10.1016/j.socscimed.2012.11.031. [DOI] [PubMed] [Google Scholar]
- 31.Pachter LM, Coll CG. Racism and child health: A review of the literature and future directions. Journal of Developmental and Behavioral Pediatrics. 2009;30(3):255–63. doi: 10.1097/DBP.0b013e3181a7ed5a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pascoe EA, Richman LS. Perceived Discrimination and Health: A Meta-Analytic Review. Psychol Bull. 2009;135(4):531–54. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Paradies Y. A systematic review of empirical research on self-reported racism and health. International Journal of Epidemiology. 2006;35(4):888–901. doi: 10.1093/ije/dyl056. [DOI] [PubMed] [Google Scholar]
- 34.Gee GC, Walsemann KM, Brondolo E. A Life Course Perspective on How Racism May Be Related to Health Inequities. American Journal of Public Health. 2012;102(5):967–74. doi: 10.2105/AJPH.2012.300666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32(1):20–47. doi: 10.1007/s10865-008-9185-0. Epub 2008/11/26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Acevedo-Garcia D, Rosenfeld LE, Hardy E, McArdle N, Osypuk TL. Future Directions in Research on Institutional and Interpersonal Discrimination and Children's Health. American Journal of Public Health. 2013;103(10):1754–63. doi: 10.2105/AJPH.2012.300986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Krieger N. Discrimination and health inequities. In: Berkman LF, Kawachi I, Glymour M, editors. Social Epidemiology. 2 ed Oxford University Press; 2014. [Google Scholar]
- 38.Hale L, Do P. Racial differences in self-reports of sleep duration in a population-based study. Sleep. 2007;30(9):1096–103. doi: 10.1093/sleep/30.9.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chen D, Yang TC. The pathways from perceived discrimination to self-rated health: an investigation of the roles of distrust, social capital, and health behaviors. Soc Sci Med. 2014;104:64–73. doi: 10.1016/j.socscimed.2013.12.021. Epub 2014/03/04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Moore PJ, Adler NE, Williams DR, Jackson JS. Socioeconomic status and health: The role of sleep. Psychosomatic Medicine. 2002;64(2):337–44. doi: 10.1097/00006842-200203000-00018. [DOI] [PubMed] [Google Scholar]
- 41.Mohr D, Vedantham K, Neylan T, Metzler TJ, Best S, Marmar CR. The mediating effects of sleep in the relationship between traumatic stress and health symptoms in urban police officers. Psychosomatic Medicine. 2003;65(3):485–9. doi: 10.1097/01.psy.0000041404.96597.38. [DOI] [PubMed] [Google Scholar]
- 42.Pereira D, Elfering A. Social Stressors at Work, Sleep Quality and Psychosomatic Health Complaints—A Longitudinal Ambulatory Field Study. Stress and Health. 2014;30(1):43–52. doi: 10.1002/smi.2494. [DOI] [PubMed] [Google Scholar]
- 43.Hale L, Hill TD, Friedman E, Javier Nieto F, Galvao LW, Engelman CD, et al. Perceived neighborhood quality, sleep quality, and health status: Evidence from the Survey of the Health of Wisconsin. Soc Sci Med. 2013;79(0):16–22. doi: 10.1016/j.socscimed.2012.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Harrell JP, Hall S, Taliaferro J. Physiological Responses to Racism and Discrimination: An Assessment of the Evidence. American Journal of Public Health. 2003;93(2):243–8. doi: 10.2105/ajph.93.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Brondolo E, Hausmann LM, Jhalani J, Pencille M, Atencio-Bacayon J, Kumar A, et al. Dimensions of Perceived Racism and Self-Reported Health: Examination of Racial/Ethnic Differences and Potential Mediators. Annals of Behavioral Medicine. 2011;42(1):14–28. doi: 10.1007/s12160-011-9265-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Beatty DL, Hall MH, Kamarck TA, Buysse DJ, Owens JF, Reis SE, et al. Unfair treatment is associated with poor sleep in African American and Caucasian adults: Pittsburgh SleepSCORE project. Health Psychol. 2011;30(3):351–9. doi: 10.1037/a0022976. Epub 2011/05/11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Huynh V. Ethnic Microaggressions and the Depressive and Somatic Symptoms of Latino and Asian American Adolescents. J Youth Adolescence. 2012;41(7):831–46. doi: 10.1007/s10964-012-9756-9. [DOI] [PubMed] [Google Scholar]
- 48.Buckley TM, Schatzberg AF. On the Interactions of the Hypothalamic-Pituitary-Adrenal (HPA) Axis and Sleep: Normal HPA Axis Activity and Circadian Rhythm, Exemplary Sleep Disorders. The Journal of Clinical Endocrinology & Metabolism. 2005;90(5):3106–14. doi: 10.1210/jc.2004-1056. [DOI] [PubMed] [Google Scholar]
- 49.Paradies Y, Priest N, Ben J, Truong M, Gupta A, Pieterse A, et al. Racism as a determinant of health: a protocol for conducting a systematic review and meta-analysis. Systematic Reviews. 2013;2(1):85. doi: 10.1186/2046-4053-2-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Elovainio M, Kivimäki M, Vahtera J, Keltikangas-Järvinen L, Virtanen M. Sleeping problems and health behaviors as mediators between organizational justice and health. Health Psychol. 2003;22(3):287–93. doi: 10.1037/0278-6133.22.3.287. [DOI] [PubMed] [Google Scholar]
- 51.Elovainio M, Ferrie JE, Gimeno D, De Vogli R, Shipley M, Brunner EJ, et al. Organizational justice and sleeping problems: The Whitehall II study. Psychosom Med. 2009;71(3):334–40. doi: 10.1097/PSY.0b013e3181960665. Epub 2009/03/03. [DOI] [PubMed] [Google Scholar]
- 52.Lewis TT, Troxel WM, Kravitz HM, Bromberger JT, Matthews KA, Hall MH. Chronic exposure to everyday discrimination and sleep in a multiethnic sample of middle-aged women. Health Psychol. 2013;32(7):810–9. doi: 10.1037/a0029938. Epub 2012/10/24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Greenberg J. Losing sleep over organizational injustice: attenuating insomniac reactions to underpayment inequity with supervisory training in interactional justice. The Journal of applied psychology. 2006;91(1):58–69. doi: 10.1037/0021-9010.91.1.58. Epub 2006/01/27. [DOI] [PubMed] [Google Scholar]
- 54.Thomas KS, Bardwell WA, Ancoli-Israel S, Dimsdale JE. The toll of ethnic discrimination on sleep architecture and fatigue. Health Psychol. 2006;25(5):635–42. doi: 10.1037/0278-6133.25.5.635. Epub 2006/10/04. [DOI] [PubMed] [Google Scholar]
- 55.Park JB, Nakata A, Swanson NG, Chun H. Organizational factors associated with work- related sleep problems in a nationally representative sample of Korean workers. Int Arch Occup Environ Health. 2013;86(2):211–22. doi: 10.1007/s00420-012-0759-3. Epub 2012/03/20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bittencourt AA, Aerts D, Alves GG, Palazzo L, Monteiro L, Vieira PC, et al. Feelings of discrimination among students: prevalence and associated factors. Revista De Saude Publica. 2009;43(2):236–45. doi: 10.1590/s0034-89102009005000008. [DOI] [PubMed] [Google Scholar]
- 57.Kim HC, Kim BK, Min KB, Min JY, Hwang SH, Park SG. Association between job stress and insomnia in Korean workers. J Occup Health. 2011;53(3):164–74. doi: 10.1539/joh.10-0032-oa. Epub 2011/03/23. [DOI] [PubMed] [Google Scholar]
- 58.Taloyan M, Johansson LM, Johansson SE, Sundquist J, Kocturk TO. Poor self-reported health and sleeping difficulties among Kurdish immigrant men in Sweden. Transcult Psychiatry. 2006;43(3):445–61. doi: 10.1177/1363461506066988. Epub 2006/11/09. [DOI] [PubMed] [Google Scholar]
- 59.Huynh VW, Gillen-O'Neel C. Discrimination and Sleep: The Protective Role of School Belonging. Youth & Society. 2013 [Google Scholar]
- 60.Grandner MA, Hale L, Jackson N, Patel NP, Gooneratne NS, Troxel WM. Perceived racial discrimination as an independent predictor of sleep disturbance and daytime fatigue. Behav Sleep Med. 2012;10(4):235–49. doi: 10.1080/15402002.2012.654548. Epub 2012/09/06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hicken MT, Lee H, Ailshire J, Burgard SA, Williams DR. “Every shut eye, ain't sleep”: The role of racism-related vigilance in racial/ethnic disparities in sleep difficulty. Race and social problems. 2013;5(2):100–12. doi: 10.1007/s12552-013-9095-9. Epub 2013/07/31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Steffen PR, Bowden M. Sleep disturbance mediates the relationship between perceived racism and depressive symptoms. Ethn Dis. 2006;16(1):16–21. Epub 2006/04/08. [PubMed] [Google Scholar]
- 63.Tomfohr L, Pung MA, Edwards KM, Dimsdale JE. Racial differences in sleep architecture: the role of ethnic discrimination. Biol Psychol. 2012;89(1):34–8. doi: 10.1016/j.biopsycho.2011.09.002. Epub 2011/09/20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Slopen N, Williams DR. Discrimination, Other Psychosocial Stressors, and Self- Reported Sleep Duration and Difficulties. Sleep. 2014;37(1):147–U365. doi: 10.5665/sleep.3326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Beatty DL, Matthews KA. Unfair Treatment and Trait Anger in Relation to Nighttime Ambulatory Blood Pressure in African American and White Adolescents. Psychosomatic Medicine. 2009;71(8):813–20. doi: 10.1097/PSY.0b013e3181b3b6f8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Harvey AG. Sleep and Circadian Functioning: Critical Mechanisms in the Mood Disorders? Annual Review of Clinical Psychology. 2011;7(1):297–319. doi: 10.1146/annurev-clinpsy-032210-104550. [DOI] [PubMed] [Google Scholar]
- 67.Kessler RC, Mickelson KD, Williams DR. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. J Health Soc Behav. 1999;40(3):208–30. [PubMed] [Google Scholar]
- 68.Williams DR, Mohammed SA. Racism and Health I: Pathways and Scientific Evidence. American Behavioral Scientist. 2013;57(8):1152–73. doi: 10.1177/0002764213487340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Taveras EM, Gillman MW, Kleinman KP, Rich-Edwards JW, Rifas-Shiman SL. Reducing racial/ethnic disparities in childhood obesity: The role of early life risk factors. JAMA Pediatrics. 2013;167(8):731–8. doi: 10.1001/jamapediatrics.2013.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Seaton EK, Caldwell CH, Sellers RM, Jackson JS. The prevalence of perceived discrimination among African American and Caribbean Black youth. Developmental Psychology. 2008;44(5):1288–97. doi: 10.1037/a0012747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Coker TR, Elliott MN, Kanouse DE, Grunbaum JA, Schwebel DC, Gilliland MJ, et al. Perceived Racial/Ethnic Discrimination Among Fifth-Grade Students and Its Association With Mental Health. American Journal of Public Health. 2009;99(5):878–84. doi: 10.2105/AJPH.2008.144329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gregory AM, Sadeh A. Sleep, emotional and behavioral difficulties in children and adolescents. Sleep Medicine Reviews. 2012;16(2):129–36. doi: 10.1016/j.smrv.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 73.Dewald JF, Meijer AM, Oort FJ, Kerkhof GA, Bögels SM. The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: A meta-analytic review. Sleep Medicine Reviews. 2010;14(3):179–89. doi: 10.1016/j.smrv.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 74.Brondolo E, Love EE, Pencille M, Schoenthaler A, Ogedegbe G. Racism and Hypertension: A Review of the Empirical Evidence and Implications for Clinical Practice. American Journal of Hypertension. 2011;24(5):518–29. doi: 10.1038/ajh.2011.9. [DOI] [PubMed] [Google Scholar]
- 75.Irwin MR, Cole JC, Nicassio PM. Comparative meta-analysis of behavioral interventions for insomnia and their efficacy in middle-aged adults and in older adults 55+ years of age. Health Psychology. 2006;25(1):3–14. doi: 10.1037/0278-6133.25.1.3. [DOI] [PubMed] [Google Scholar]
- 76.Li F, Fisher KJ, Harmer P, Irbe D, Tearse RG, Weimer C. Tai Chi and Self-Rated Quality of Sleep and Daytime Sleepiness in Older Adults: A Randomized Controlled Trial. Journal of the American Geriatrics Society. 2004;52(6):892–900. doi: 10.1111/j.1532-5415.2004.52255.x. [DOI] [PubMed] [Google Scholar]
- 77.Edinger JD, Sampson WS. A primary care “friendly” cognitive behavioral insomnia therapy. Sleep. 2003;26(2):177–82. doi: 10.1093/sleep/26.2.177. Epub 2003/04/10. [DOI] [PubMed] [Google Scholar]
- 78.Ritterband LM, Thorndike FP, Gonder-Frederick LA, Magee JC, Bailey ET, Saylor DK, et al. Efficacy of an Internet-based behavioral intervention for adults with insomnia. Arch Gen Psychiatry. 2009;66(7):692–8. doi: 10.1001/archgenpsychiatry.2009.66. Epub 2009/07/08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Espie CA, Kyle SD, Williams C, Ong JC, Douglas NJ, Hames P, et al. A randomized, placebo-controlled trial of online cognitive behavioral therapy for chronic insomnia disorder delivered via an automated media-rich web application. Sleep. 2012;35(6):769–81. doi: 10.5665/sleep.1872. Epub 2012/06/02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Pachankis JE, Hatzenbuehler ML, Starks TJ. The influence of structural stigma and rejection sensitivity on young sexual minority men's daily tobacco and alcohol use. Social Science & Medicine. 2014;103(0):67–75. doi: 10.1016/j.socscimed.2013.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Chae DH, Nuru-Jeter AM, Adler NE, Brody GH, Lin J, Blackburn EH, et al. Discrimination, Racial Bias, and Telomere Length in African-American Men. Am J Prev Med. 2014;46(2):103–11. doi: 10.1016/j.amepre.2013.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Chae DH, Lincoln KD, Adler NE, Syme SL. Do experiences of racial discrimination predict cardiovascular disease among African American men? The moderating role of internalized negative racial group attitudes. Social Science & Medicine. 2010;71(6):1182–8. doi: 10.1016/j.socscimed.2010.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Jackson C, Kawachi I, Redline S, Juon H-S, Hu F. Asian-White disparities in short sleep duration by industry of employment and occupation in the US: a cross-sectional study. BMC Public Health. 2014;14(1):552. doi: 10.1186/1471-2458-14-552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Jackson CL, Redline S, Kawachi I, Williams MA, Hu FB. Racial Disparities in Short Sleep Duration by Occupation and Industry. American Journal of Epidemiology. 2013;178(9):1442–51. doi: 10.1093/aje/kwt159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Smedley BD. The Lived Experience of Race and Its Health Consequences. American Journal of Public Health. 2012;102(5):933–5. doi: 10.2105/AJPH.2011.300643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116(5):404–16. doi: 10.1093/phr/116.5.404. Epub 2002/06/04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lukachko A, Hatzenbuehler ML, Keyes KM. Structural racism and myocardial infarction in the United States. Social Science & Medicine. 2014;103(0):42–50. doi: 10.1016/j.socscimed.2013.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Harrell CJP, Burford TI, Cage BN, Nelson TM, Shearon S, Thompson A, et al. Multiple pathways linking racism to health outcomes. Du Bois Review: Social Science Research on Race. 2011;8(01):143–57. doi: 10.1017/S1742058X11000178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Jones CP. Levels of racism: a theoretic framework and a gardener's tale. American Journal of Public Health. 2000;90(8):1212–5. doi: 10.2105/ajph.90.8.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Lauderdale D. Birth outcomes for Arabic-named women in California before and after September 11. Demography. 2006;43(1):185–201. doi: 10.1353/dem.2006.0008. [DOI] [PubMed] [Google Scholar]
- 91.Padela AI, Heisler M. The Association of Perceived Abuse and Discrimination After September 11, 2001, With Psychological Distress, Level of Happiness, and Health Status Among Arab Americans. American Journal of Public Health. 2010;100(2):284–91. doi: 10.2105/AJPH.2009.164954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Richman L, Jonassaint C. The Effects of Race-related Stress on Cortisol Reactivity in the Laboratory: Implications of the Duke Lacrosse Scandal. Annals of Behavioral Medicine. 2008;35(1):105–10. doi: 10.1007/s12160-007-9013-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Hatzenbuehler ML, Bellatorre A, Lee Y, Finch BK, Muennig P, Fiscella K. Structural stigma and all-cause mortality in sexual minority populations. Social Science & Medicine. 2014;103(0):33–41. doi: 10.1016/j.socscimed.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hatzenbuehler ML, Keyes KM, Hasin DS. State-Level Policies and Psychiatric Morbidity In Lesbian, Gay, and Bisexual Populations. American Journal of Public Health. 2009;99(12):2275–81. doi: 10.2105/AJPH.2008.153510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Toomey RB, Umaña-Taylor AJ, Williams DR, Harvey-Mendoza E, Jahromi LB, Updegraff KA. Impact of Arizona's SB 1070 Immigration Law on Utilization of Health Care and Public Assistance Among Mexican-Origin Adolescent Mothers and Their Mother Figures. American Journal of Public Health. 2013;104(S1):S28–S34. doi: 10.2105/AJPH.2013.301655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Clark R, Benkert RA, Flack JM. Large Arterial Elasticity Varies as a Function of Gender and Racism-Related Vigilance in Black Youth. J Adolesc Health. 2006;39(4):562–9. doi: 10.1016/j.jadohealth.2006.02.012. [DOI] [PubMed] [Google Scholar]
- 97.Hicken MT, Lee H, Morenoff J, House JS, Williams DR. Racial/Ethnic Disparities in Hypertension Prevalence: Reconsidering the Role of Chronic Stress. American Journal of Public Health. 2013;104(1):117–23. doi: 10.2105/AJPH.2013.301395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Lindström M. Social capital, anticipated ethnic discrimination and self-reported psychological health: A population-based study. Social Science & Medicine. 2008;66(1):1–13. doi: 10.1016/j.socscimed.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 99.Mohseni M, Lindström M. Ethnic differences in anticipated discrimination, generalised trust in other people and self-rated health: a population-based study in Sweden. Ethnicity & Health. 2008;13(5):417–34. doi: 10.1080/13557850802009603. [DOI] [PubMed] [Google Scholar]
- 100.Sawyer PJ, Major B, Casad BJ, Townsend SSM, Mendes WB. Discrimination and the Stress Response: Psychological and Physiological Consequences of Anticipating Prejudice in Interethnic Interactions. American Journal of Public Health. 2012;102(5):1020–6. doi: 10.2105/AJPH.2011.300620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Dickersin K. THe existence of publication bias and risk factors for its occurrence. JAMA. 1990;263(10):1385–9. [PubMed] [Google Scholar]
- 102.Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self-Reported and Measured Sleep Duration How Similar Are They? Epidemiology. 2008;19(6):838–45. doi: 10.1097/EDE.0b013e318187a7b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


