Abstract
Electronic cigarettes (e-cigs) were created to approximate the look, feel, and experience of using a cigarette. Since cigarette and alcohol use co-occur, we hypothesized that e-cig and alcohol use also co-occur, likely due to shared positive drug expectations. Using self-report data from two independent samples of community-dwelling alcohol using adults, the present study: (1) modified the Nicotine and Other Substance Interaction Expectancy Questionnaire (NOSIE) to assess expectancies of combined e-cig and alcohol use (i.e. the individuals perceived likelihood of using e-cigs and alcohol together; NOSIE-ER); and (2) examined the relationships among e-cig use, expectancies, and alcohol use across e-cig use status. In the first sample (N=692, mean age=32.6, SD = 9.74, 50.7% female, 82.2% Caucasian), exploratory factor analysis suggested the presence of two factors: (1) alcohol use leads to e-cig use (Scale 1; α=0.85); and (2) e-cig use leads to alcohol use (Scale 2; α=0.91). In the second sample (N=714, mean age=34.1, SD=10.89, 47.8% female, 75.6% Caucasian), confirmatory factor analysis supported this factor structure (χ2=47.00, p<0.01, df=19; RMSEA=0.08, 90% CI=0.05–0.11; TLI=0.99; CFI=0.99). Compared to non e-cig users, e-cig users had significantly higher problematic alcohol use in both samples (b’s=0.09 to 0.14, p’s<.05). Expectancies of combined e-cig and alcohol use were significantly related to problematic alcohol use (b’s=−0.92 to 0.26, p’s<.05). In sum, e-cig use is related to alcohol use and expectancies of combined e-cig and alcohol use; consequently, reshaping of beliefs about needs or desires to co-use could be a prime point of intervention.
Keywords: e-cigarette use, alcohol use, e-cigarette expectancies, alcohol expectancies
1. Introduction
Electronic cigarettes (e-cigs) are electronic nicotine delivery systems that were created to approximate the look and feel of a cigarette (1). Recent research has found similarities between e-cigs and cigarettes, particularly in increasing blood nicotine levels (2) nicotine absorption (3–5), and serum cotinine levels (6, 7). Recently, e-cig use prevalence rates have increased to 6.2% in the general population (8) and 17% in substance dependent populations (9), likely as a result of comprehensive smoking bans (10) and perceived health benefits of e-cigs (11–13). However, although research does not currently support the efficacy of e-cigs for smoking cessation or other health benefits (14–18), many users report using e-cigs to stop traditional cigarette use, to circumvent smoking bans, and because e-cigs are perceived as less harmful than cigarettes (8). This high prevalence of e-cig use is likely driven by positive expectations about the use of e-cigs. However, this high prevalence is problematic because e-cig liquids contain potentially harmful substances such as propylene glycol and contain nicotine, which can lead to addiction (19–22).
Although recent research has investigated e-cig perceptions and use in substance dependent populations (9), little research has examined how e-cigs influence other addictive behaviors in adults, particularly alcohol use. Traditional cigarettes have a well-established relationship with alcohol use (23–27) and cigarette smokers are at a higher risk for developing an alcohol use disorder (AUD; 28). Additionally, nicotine consumption has been linked to alcohol consumption in multiple ways. First, the mesolimbic dopamine system is responsible for the reinforcing effects of substances of abuse (29), and might subsequently contribute to the motivation to seek both alcohol and nicotine (30–32); in this way, the dopamine system serves as a plausible mechanism for the high rates of nicotine and alcohol co-use, and could generalize to concurrent alcohol and e-cig use. Second, Rohsenow and colleagues (33) propose a “priming hypothesis,” in which tobacco serves as a conditioned stimulus for alcohol consumption and vice versa. Such conditioned processes likely contribute to high rates of co-use between alcohol and cigarettes, and may generalize to e-cig and alcohol co-use. Third, nicotine has been found to mitigate the sedative effect of alcohol, as nicotine is alerting in small doses (34). These and other learned expectancies of combined cigarette and alcohol use (e.g., If I drink and smoke, I will be more sociable) are implicated in the relationship between cigarette and alcohol use (36–38). From such beliefs arise combined expectancies, which have previously been measured using the Nicotine and Other Substance Interaction Expectancy Questionnaire (NOSIE; 39), which assesses expectancies of combined smoking and substance use through 29 items that fall onto four scales: a) substance use increases tobacco use urges (e.g., I need a cigarette while I am drinking or using drugs); b) smoking increases substance use urges (e.g., Smoking gives me more desire for alcohol or drugs); c) smoking to cope with substance urges (e.g., I have smoked a cigarette in order to try and decrease my urge to drink or use drugs); and d) openness to quitting smoking during substance use treatment (e.g., I believe that I should try to quit smoking).
Given the similarities of e-cigs and cigarettes, expectancies of combined e-cig and alcohol use might also be similarly related to alcohol use behaviors; however, no studies have examined this. Elucidating whether such combined expectancies would lead to increased alcohol consumption can lead to a better understanding of the potential harm of using e-cigs, particularly for those at risk for developing alcohol use disorders and/or for those who are more likely to use e-cigs (9). The goals of the present studies were: a) to adapt the NOSIE to assess expectancies of combined e-cig and alcohol use (NOSIE-ER), and b) to examine and characterize the relationship between e-cig use, expectancies, and alcohol use across e-cig use status.
2. Methods
2.1. Participants
Two independent samples were collected using identical methods and measures. Participants who met study inclusion criteria (21 years or older, able to read and understand questions in English, live in the United States, and drink alcohol), signed up to participate online through Amazon’s Mechanical Turk (www.mturk.com; MTurk), which is an online web service that connects researchers with individuals willing to complete tasks for a wage. The MTurk subject pool has recently been used to research an array of psychological constructs, including addiction (40), personality (41), relationships (42), self-injury (43) and grief (44). MTurk samples have shown good test-retest reliability, with less than two percent showing inconsistent responses across one week (45).
2.2. Measures
2.2.1. E-cig Use Status
Participants responded to face valid e-cig use (“Do you use electronic-cigarettes currently” with 3 response options - “No”, “Yes, I use e-cigarettes regularly [daily]”, “Yes, I use e-cigarettes, in social contexts only”), and cigarette use (“Do you smoke cigarettes currently” with 3 response options - “No”, “Yes, I smoke cigarettes regularly [daily]”, “Yes, I smoke cigarettes, in social contexts only”) items. Those reporting daily e-cig use and no cigarette use were designated “regular,” those reporting e-cig use in social contexts and no cigarette use were designated “social,” those reporting daily e-cig use and any cigarette use were designated “regular dual,” and those reporting e-cig use in social contexts and any cigarette use were designated “social dual.”
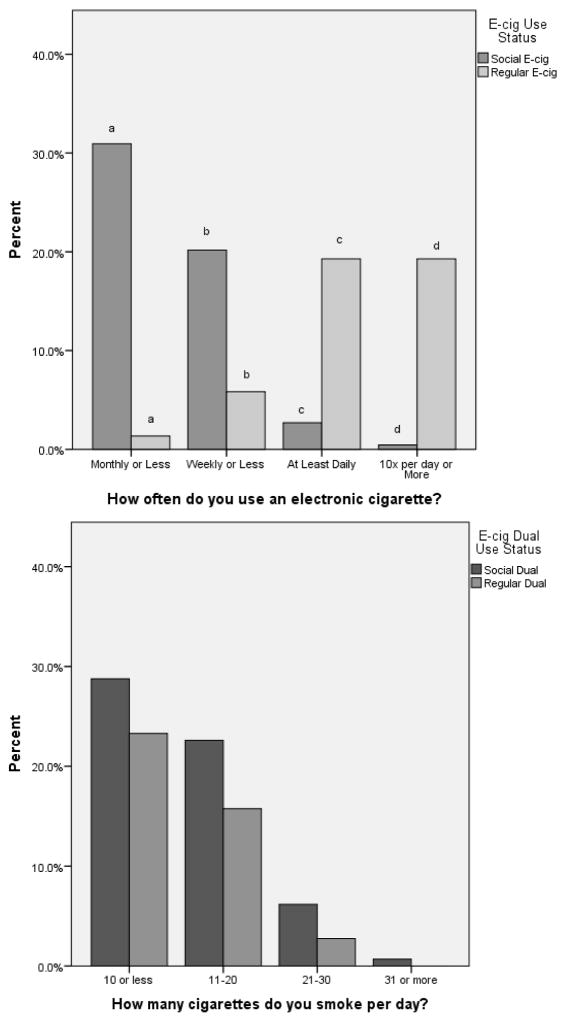
E-cig use frequency was assessed in Sample 1 with one item created for this study (“How often do you use an e-cig?” with 4 response options – “Monthly or less,” “Weekly or less,” “At least daily,” and “10x a day or more”). The purpose of the item was to validate the measure of social versus daily e-cig use. More social users, compared to regular users, reported using e-cigs monthly or less, χ2=80.78, p<.001, and weekly or less, χ2=16.28, p<.001, while more regular users, compared to social users, reported using e-cigs at least daily, χ2=46.10, p<.001, and at least 10 times per day, χ2=19.96, p<.001 (Figure 1). Amount of cigarettes smoked per day was examined using one item created for the study (“How many cigarettes do you smoke per day?” with 4 response options – “10 or less,” “11–20”, “21 to 30,” and “31 or more”). Social dual and regular dual e-cig users did not vary on the amount of cigarettes smoked per day (Figure 1).
Figure 1.
E-cig Use Frequency for Social and Regular E-cig Users and Smokers
Sample 1 e-cig use frequency by e-cig use status (left). Chi-square tests of independence were conducted to examine the difference between social and regular e-cig users on e-cig use frequency. a χ2=80.78, p<.001 b χ2=16.28, p<.001 c χ2=46.10, p<.001 d χ2=19.96, p<.001. Sample 1 cigarettes smoked per day for social and regular dual e-cig users (right). Users did not differ in smoking 10 or less cigarettes, χ2=0.842, p=.36, 11–20 cigarettes, χ2=1.78, p=.18, or 21–30 cigarettes, χ2=1.92, p=.17. Comparisons were not computed for 31 or more cigarettes, as there were not enough participants per category.
2.2.2. E-cigs and Alcohol Use Expectancies
E-cig using participants completed the Nicotine and Other Substance Interaction Expectancies-E-cig Revised version (NOSIE-ER), which was adapted from the NOSIE to reflect combined expectancies of e-cig use and alcohol consumption (39). The original NOSIE contains 29 items; only the 8 items on Scale 1 and Scale 2 of the NOSIE were modified for use in the NOSIER-ER as they were the most relevant to measuring combined expectancies. Scores on the NOSIE have shown acceptable to good reliability (α=0.69 to 0.81), and are related to level of nicotine dependence (r=0.13, p<.05), number of heavy drinking days (r=0.13, p<.05), and drug use (r=0.14, p<.05; 39). The adapted NOSIE-ER consists of eight true/false items that assess expectations about e-cig use increasing alcohol consumption and alcohol consumption increasing e-cig use (see Table 1). Total data from the NOSIE-ER had good reliability in both samples (α=0.88 and α=0.84) and data were approximately normally distributed in Sample 1 (mean=3.24, SD=2.65, skewness=0.30, kurtosis=−1.06) and Sample 2 (mean=3.06, SD=2.50, skewness=0.322, kurtosis=−0.90). The NOSIE-ER was related measures of alcohol consumption in the present studies (see Section 3.2 and 4.2).
Table 1.
Exploratory Factor Analysis of the NOSIE-ER.
| NOSIE-ER Items | Scale 1 Alcohol Use Leads to E-cig Use | Scale 2 E-cig Use Leads to Alcohol Use |
|---|---|---|
|
| ||
| 1. It is second nature for me to pick up a e-cigarette while I am drinking | 0.646 | 0.131 |
| 2. Drinking results in me wanting to smoke a e-cigarette more | 0.932 | −0.113 |
| 3. I need to smoke a e-cigarette while I am drinking | 0.561 | 0.258 |
| 4. I smoke more e-cigarettes while I am having a drink than while I am not actually drinking | 0.675 | 0.048 |
| 5. I enjoy smoking an e-cigarette more after I have had a drink | 0.702 | −0.079 |
| 6. Smoking e-cigarettes gives me more desire for alcohol | 0.007 | 0.907 |
| 7. I tend to drink more after I smoke an e-cigarette | 0.039 | 0.834 |
| 8. If I could smoke e-cigarettes, my urge to drink would increase | −0.063 | 0.884 |
Note. PAF using promax rotation; factors determined using eigenvalue>1, scree plot, and parallel analysis.
2.2.3 Alcohol Use
The Alcohol Use Disorders Identification Test (AUDIT; 46) is a ten-item scale that assesses hazardous alcohol consumption, abnormal alcohol consumption behavior, and alcohol related problems. Data obtained by the AUDIT allows for discriminating between hazardous and non-hazardous drinkers (46), with AUDIT responses showing concurrent validity with other measures of alcohol use (47). The AUDIT demonstrated good reliability in both samples (α=0.85 and α=0.81).
The Timeline Follow-Back (TLFB; 48) aids participants in estimating daily alcohol consumption. Participants were asked to indicate the number of drinks they consumed each day over a two-week period. Total number of drinks was calculated by summing the total number of drinks each individual consumed over the two-week period. Average number of drinks per drinking day was calculated by dividing the sum of the total number of drinks consumed over the two-week period by the total number of alcohol consumption days. Responses on the TLFB have adequate test-retest reliability for days abstinent from alcohol, days with alcohol consumption and without a binge episode, and days with binge episodes in social drinkers (48). The TLFB also demonstrated high convergent validity with the Addiction Severity Index (49).
2.2.4 Careless Responding
As suggested by Meade & Craig (2012; 50), careless responding was assessed by the use of four “bogus items” placed randomly throughout the test (“I have never brushed my teeth,” “I do not understand a word of English,” I sleep less than one hour per night,” and “I have been to every country in the world”), with one proceeding the TLFB, one preceding the AUDIT, and two proceeding a measure unrelated to the present study. Participants responded to items on a 1 (agree strongly) to 7 (disagree strongly) scale. It was determined a priori that answering a 1 or 2 on two or more bogus items would result in that participant’s data being removed for study analyses.
2.3 Procedure
Workers on Amazon’s Mechanical Turk self-selected to take part in this online study, which was listed as “E-cig, Cigarette, and Alcohol Use Study.” Participants were given a link to the survey location, where inclusion criteria were reassessed and those who met inclusion completed study measures. Participants who completed the study received $0.75 in compensation, which is in line with the average MTurk hourly wage of $1.40 (51). Participants who failed two or more bogus items were removed from all analyses (N=51 and 88, across both samples). Less than 0.01% of the data were missing at random; therefore, were imputed through linear interpolation, which produces less biased results compared to other imputation techniques (52).
3. Sample 1 Results
3.1. Exploratory Factor Analysis
The final sample size was N=692 (n=225 e-cig users, mean age=32.6, SD=9.74, 50.7% female, 82.2% Caucasian; Table 2). Principal Axis Factoring (PAF) using exploratory factor analysis with promax rotation was conducted, which revealed two factors in the NOSIE-ER (determined by eigenvalue>1, scree plot, parallel analysis) replicating previous work with the original NOSIE (39) (Table 1): alcohol use leads to e-cig use (Scale 1, e.g., It is second nature for me to pick up an e-cig while I am drinking; 5 items.) and e-cig use leads to alcohol use (Scale 2, e.g., I tend to drink more after I use my e-cigarette; 3 items). Scale 1 (α=0.85) was approximately normally distributed (mean=2.62, SD=1.95, skewness=−0.15, kurtosis=−1.53), with scores ranging from 0 to 5. Scale 2 (α=0.91) was approximately normally distributed (mean=0.61, SD=1.11, skewness=1.45, kurtosis=0.37), with scores ranging from 0 to 3. The two scales were significantly correlated (r=0.45, p<.001).
Table 2.
Comparison of Demographic Characteristics across E-cig User Type.
| Age | Gender | |||
|---|---|---|---|---|
|
| ||||
| N | Mean(SD) | Male | Female | |
| Sample 1 | ||||
| Non | 366 | 33.36(10.96) | 189 | 230b |
| Social | 33 | 32.35(10.80) | 19 | 37c |
| Regular | 36 | 32.93(9.84) | 28 | 31 |
| Social Dual | 90 | 34.85(11.03)a | 36 | 54d |
| Regular Dual | 66 | 31.42(8.35)a | 47 | 19b, c, d |
|
| ||||
| Sample 2 | ||||
| Non | 494 | 34.12(11.08) | 255 | 237 |
| Social | 29 | 32.52(10.27) | 19 | 10 |
| Regular | 46 | 33.87(8.98) | 25 | 21 |
| Social Dual | 90 | 32.96(9.64) | 45 | 45 |
| Regular Dual | 56 | 36.14(12.71) | 28 | 28 |
Note. Independent samples t-tests were conducted on all age relationships. Chi-square difference tests were conducted on all ethnicity and gender relationships. There were no significant differences by ethnicity. Relationships marked with a superscript were significant at p<.05 and are described below. All other relationships were not significant at p<.05.
Sample 1:
t(155)=2.12, p=.03;
χ2= 15.55, p<.01;
χ2= 16.96, p<.01;
χ2= 14.90, p<.01
3.2. Relationships with variables of interest
Hierarchal linear regressions (Table 3), controlling for age, gender and ethnicity, indicated significant differences in alcohol use variables across e-cig use status (dummy coded 0-no e-cig use, 1-e-cig use). E-cig users reported significantly higher a) AUDIT scores, b=1.29, p=.001, b) Total drinks, b=2.12, p=.05, and c) Average number of drinks per drinking day, b=0.33, p=.02 (see Table 4 for mean scores on drinking measures by e-cig use status).
Table 3.
Sample 1 Hierarchical Linear Regression for E-cig Use on Alcohol Consumption Measures.
| Dependent Variable | b | B | t | p | ΔR2 | p | R2 | p | |
|---|---|---|---|---|---|---|---|---|---|
| AUDIT | Step1: Age | −0.07 | −0.16 | −3.9 | <.001 | 0.11 | <.001 | ||
| Gender | −2.4 | −0.26 | −6.4 | <.001 | |||||
| African American | 0.51 | 0.03 | 0.72 | .472 | |||||
| Hispanic | −1.16 | −0.06 | −1.1 | .27 | |||||
| Asian/Pacific Islander | −2.29 | −0.1 | −2.41 | .02 | |||||
| American Indian | −3.4 | −0.03 | −0.79 | .43 | |||||
| Other | 2.31 | 0.12 | 2 | .04 | |||||
| Step 2: E-cig user | 1.29 | 0.14 | 3.4 | .001 | 0.02 | 0.13 | <.001 | ||
| Total Drinking Days | Step 1: Age | 0 | 0 | 0.003 | .99 | 0.07 | <.001 | ||
| Gender | −6.58 | −0.25 | −6.04 | <.001 | |||||
| African American | 0.36 | 0.007 | 0.17 | .86 | |||||
| Hispanic | −5.83 | −0.119 | −1.83 | .06 | |||||
| Asian/Pacific Islander | −5.82 | −0.09 | −2.08 | .04 | |||||
| American Indian | −8.26 | −0.03 | −6.48 | .09 | |||||
| Other | 5.63 | 0.1 | −6.04 | .52 | |||||
| Step 2: E-cig User | 2.12 | 0.08 | 1.9 | .05 | 0.01 | 0.08 | <.001 | ||
| Average Drinks | Step 1: Age | −0.02 | −0.13 | −3.14 | <.01 | 0.07 | <.001 | ||
| Gender | −0.74 | −0.22 | −5.23 | <.001 | |||||
| African American | −0.24 | −0.04 | −0.88 | .38 | |||||
| Hispanic | −0.08 | −0.01 | −0.21 | .84 | |||||
| Asian/Pacific Islander | −0.26 | −0.03 | −0.63 | .48 | |||||
| American Indian | −1.04 | −0.03 | −0.7 | .40 | |||||
| Other | 0.37 | 0.05 | 0.84 | .53 | |||||
| Step 2: E-cig User | 0.33 | 0.09 | 2.26 | 0.02 | 0.01 | 0.08 | <.001 |
Note. Hierarchical regression results with gender, age, and ethnicity entered at step 1 and e-cig use at step 2, ethnicity dummy coded (0,1) with Caucasian as reference group, e-cig status dummy coded 1-e-cig user, 0-non e-cig user.
Table 4.
Comparison of Alcohol Use Measure by E-cig Status
| AUDIT | Total Drinks | Avg. Drinks Per Drinking Day | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
| N | Mean(SD) | F | p | Mean(SD) | F | p | Mean(SD) | F | p | |
| Sample 1 | ||||||||||
| Non | 366 | 6.52(5.14)a | 16.18(19.54) | 2.96(2.12) | ||||||
| Social | 33 | 6.82(4.67) | 19.18(15.09) | 3.36(2.05) | ||||||
| Regular | 36 | 7.31(5.80) | 17.51(17.27) | 3.24(2.18) | ||||||
| Social Dual | 90 | 7.81(6.00) | 21.75(17.48) | 3.52(2.48) | ||||||
| Regular Dual | 66 | 9.37(5.39)a | 9.36(5.40) | 3.27(1.80) | ||||||
| ANOVA | 4.51 | <.01 | 1.41 | .23 | 1.47 | .21 | ||||
|
| ||||||||||
| Sample 2 | ||||||||||
| Non | 494 | 6.42(4.73)f | 13.13(12.90) | 2.80(2.32) | ||||||
| Social | 29 | 6.31(4.30) | 12.28(8.75) | 3.00(1.40) | ||||||
| Regular | 46 | 6.70(4.14) | 11.43(9.64) | 2.85(2.21) | ||||||
| Social Dual | 90 | 7.60(5.30) | 16.05(12.79) | 3.43(1.94)j | ||||||
| Regular Dual | 56 | 7.80(5.80) | 16.17(13.42) | 2.87(2.22) | ||||||
| ANOVA | 2.14 | .07 | 2.02 | 0.08 | 1.52 | .19 | ||||
Note. Tukey’s HSD was calculated for significant and trending ANOVA’s. Relationship marked with a superscript was significant at p<.001. All other relationships were not significant.
An Analysis of Covariance (ANCOVA; Table 5), controlling for age, gender and ethnicity, indicated that NOSIE-ER Scale 1 scores differed across e-cig status (regular user, social user, regular dual user, social dual user), F(6,218)=3.50, p<.01, but Scale 2 scores did not F(6, 218)=0.58, p=.67 . Follow-up tests using Tukey’s HSD revealed that, on Scale 1, regular e-cig users (mean=3.15, SD=1.89) scored significantly higher than social-dual users (mean=2.08, SD=1.97). Non-users were not included in analysis, as they did not complete the NOSIE-ER.
Table 5.
Comparison of NOSIE-ER Scores across Type of E-cig User Type.
| Alcohol Use Leads to E-cig Use (5-items) | E-cig Use Leads to Alcohol Use (3 items) | ||||||
|---|---|---|---|---|---|---|---|
| N | Mean(SD) | F | p | Mean(SD) | F | p | |
| Sample 1 | |||||||
| Social | 33 | 3.30(1.72) | 0.76(1.30) | ||||
| Regular | 36 | 3.15(1.89)a | 0.31(0.71) | ||||
| Social Dual | 90 | 2.08(1.97)a | 0.58(1.11) | ||||
| Regular Dual | 60 | 2.72(1.91) | 0.76(1.17) | ||||
| ANOVA | 3.50 | <.01 | 0.58 | .67 | |||
|
| |||||||
| Sample 2 | |||||||
| Social | 29 | 2.48(1.64) | 0.72(1.22) | ||||
| Regular | 46 | 3.35(1.91) | 0.41(0.98) | ||||
| Social Dual | 89 | 2.13(1.92) | 0.48(1.07) | ||||
| Regular Dual | 56 | 2.68(2.01) | 0.45(0.99) | ||||
| ANOVA | 1.54 | .18 | 1.80 | .15 | |||
Note. Tukeys HSD was calculated for significant ANOVA’s. Relationships marked with a superscript were significant at p<.01. All other relationships were not significant.
Hierarchical linear regressions found that, after controlling for age, gender and ethnicity, total NOSIE-ER scores were significantly associated with a) AUDIT scores, ΔR2=0.04, p=.01, and b) Total drinks, ΔR2=0.03, p=.03, above and beyond demographic variables, but Average drinks per drinking day was not, ΔR2=0.01, p=.32. Hierarchical linear regressions were then conducted with the NOSIE-ER scales entered separately (Table 6). Scale 1 was significantly associated with a) AUDIT scores, b=0.39, p=.03, b) Total drinks, b=1.01, p=.02, and showed a trend for Average number of drinks per drinking day, b=0.11, p=0.13. Scale 2 was not significantly correlated with AUDIT scores, b=0.37, p=.25, Total drinks, b=.07, p=0.94, or Average number of drinks per drinking day, b=-.07, p=.56.
Table 6.
Sample 1 Hierarchical Linear Regression for NOSIE-ER Scores on Alcohol Consumption Measures.
| Dependent Variable | b | B | t | p | ΔR2 | p | R2 | p | |
|---|---|---|---|---|---|---|---|---|---|
| AUDIT | Step1: Age | −0.07 | −0.14 | −2.11 | .03 | 0.136 | <.001 | ||
| Gender | −2.77 | −0.28 | −4.31 | <.001 | |||||
| African American | 0.39 | 0.02 | 0.36 | .72 | |||||
| Hispanic | −1.97 | −0.11 | −1.11 | .27 | |||||
| Asian/Pacific Islander | 1.34 | −0.05 | −0.81 | .42 | |||||
| Other | 2.08 | 1.07 | 1.07 | .28 | |||||
| Step 2: Scale 1 | 0.39 | 0.15 | 2.14 | .03 | 0.04 | 0.01 | 0.14 | <.001 | |
| Scale 2 | 0.37 | 0.08 | 1.15 | .25 | |||||
| Total Drinking Days | Step 1: Age | 0.07 | 0.06 | 0.81 | .42 | 0.06 | 0.01 | ||
| Gender | −6.17 | −0.25 | −3.63 | <.001 | |||||
| African American | 2.13 | 0.05 | 0.75 | .46 | |||||
| Hispanic | −7.5 | −0.17 | −1.6 | .11 | |||||
| Asian/Pacific Islander | 1.57 | 0.02 | 0.36 | .72 | |||||
| Other | 5.79 | 0.12 | 1.13 | .26 | |||||
| Step 2: Scale 1 | 1.01 | 0.17 | 2.3 | .02 | 0.03 | 0.03 | 0.09 | 0.01 | |
| Scale 2 | 0.07 | 0.01 | 0.08 | .94 | |||||
| Average Drinks | Step 1: Age | −0.02 | −0.11 | −1.5 | .14 | 0.04 | 0.29 | ||
| Gender | −0.42 | −0.12 | −1.66 | .09 | |||||
| African American | −0.2 | −0.03 | 0.47 | .64 | |||||
| Hispanic | 0.07 | 0.01 | 0.1 | .92 | |||||
| Asian/Pacific Islander | −0.2 | −0.02 | −0.31 | .76 | |||||
| Other | 0.19 | 0.03 | 0.25 | .81 | |||||
| Step 2: Scale 1 | 0.11 | 0.12 | 1.5 | .13 | 0.01 | 0.32 | 0.05 | 0.30 | |
| Scale 2 | −0.07 | −0.05 | −0.58 | .56 |
Note. Hierarchical regression results with gender, age, and ethnicity entered at step 1 and NOSIE-ER scales at step 2, ethnicity dummy coded (0,1) with Caucasian as reference group.
4. Sample 2 Results
4.1. Confirmatory Factor Analysis
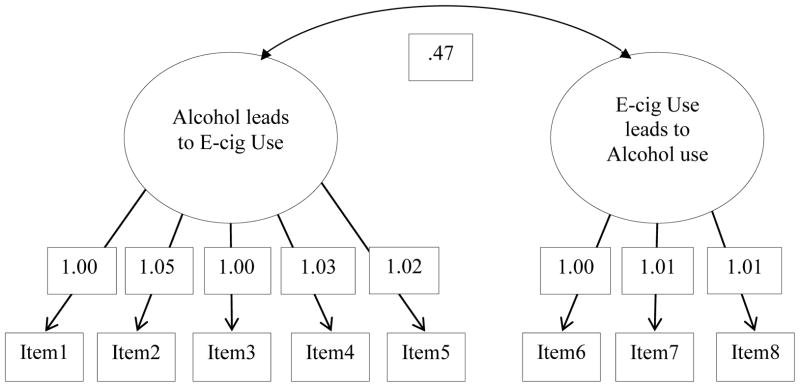
Nineteen individuals were removed from the analyses because their alcohol consumption measures were >3.13 SD from the sample mean. The final sample size was N=714 (n=221 e-cig users, mean age=34.1, SD=10.89, 47.8% female, 75.6% Caucasian; see Table 2). We conducted confirmatory factor analyses using weighted least squares method of variance with the Lavaan package in R3.0.1 (53), the following fit indices (54): χ2 (p>.05); Root Mean Square Error of Approximation (RMSEA<0.10); Tucker Lewis Index (TLI>0.95); and Comparative Fit Index (CFI>0.95). We tested a model (see Figure 2) supported by the initial exploratory factor analysis, with items 1–5 loading on the alcohol use leads to e-cig use (Scale 1) and items 6–8 loading onto the e-cig use leads to alcohol use (Scale 2). Fit indices for this model were good, suggesting adequate fit for the model: χ2=47.00, p<.01, df=19; RMSEA=0.08, 90% CI=0.05–0.11; TLI=0.99; CFI=0.99. Scale 1 (α=0.85) was approximately normally distributed (mean=2.57, SD=1.95, skewness=−0.09, kurtosis=−1.53), with scores ranging from 0 to 5. Scale 2 (α=0.94) was approximately normally distributed (mean=0.49, SD=1.05, skewness=1.83, kurtosis=1.576), with scores ranging from 0 to 3. The two scales were significantly correlated (r=0.33, p<.001).
Figure 2.
Confirmatory Factor Analysis.
Note. We tested a model supported by the initial exploratory factor analysis; with items 1–5 loading on the alcohol use leads to e-cig use (Scale 1) and items 6–8 loading onto the e-cig use leads to alcohol use (Scale 2). For simplicity, error terms are not shown. Fit indices for this model were good, suggesting adequate fit for the model: χ2=47.00, p<0.01, df=19; RMSEA=0.08, 90% CI=0.05–0.11; TLI=0.99; CFI=0.99.
4.2. Relationships with variables of interest
As in sample 1, hierarchical regression analyses (Table 7), controlling for age, gender and ethnicity, indicated that e-cig users reported significantly higher AUDIT scores than non e-cig users, b=0.91, p=.01, and Average drinks per drinking day, b=0.29, p=.10 (see Table 4), but not for Total drinks, b=1.4, p=.17.
Table 7.
Sample 2 Hierarchical Linear Regressions for E-cig Use Status on Alcohol Consumption Measures.
| Dependent Variable | b | B | t | p | ΔR2 | p | R2 | p | |
|---|---|---|---|---|---|---|---|---|---|
| AUDIT | Step1: Age | −0.08 | −0.17 | −4.6 | <.001 | 0.06 | <.001 | ||
| Gender | −1.34 | −1.4 | −3.7 | <.001 | |||||
| African American | −1.45 | −0.07 | −1.8 | .07 | |||||
| Hispanic | 0.52 | 0.02 | 0.54 | .55 | |||||
| Asian/Pacific Islander | −0.09 | −0 | −0.1 | .92 | |||||
| American Indian | 1.62 | 0.02 | 0.48 | .60 | |||||
| Other | −0.73 | −0.02 | −0.61 | .54 | |||||
| Step 2: E-cig user | 0.91 | 0.09 | 2.37 | .01 | 0.01 | 0.07 | <.001 | ||
| Total Drinking Days | Step 1: Age | −0.03 | −0.02 | −0.93 | .53 | 0.03 | <.001 | ||
| Gender | −4.67 | −0.18 | 4.96 | <.001 | |||||
| African American | −1.6 | −0.03 | −0.76 | .45 | |||||
| Hispanic | 1.3 | 0.02 | 0.56 | .57 | |||||
| Asian/Pacific Islander | −0.36 | −0.01 | −0.15 | .88 | |||||
| American Indian | −4.13 | −0.02 | −0.47 | .64 | |||||
| Other | −1.16 | −0.01 | −0.37 | .71 | |||||
| Step 2: E-cig User | 1.4 | 0.05 | 1.4 | .17 | 0.01 | 0.04 | <.001 | ||
| Average Drinks | Step 1: Age | −0.02 | −0.09 | −2.45 | .02 | 0.04 | <.001 | ||
| Gender | −0.76 | −0.17 | −4.66 | <.001 | |||||
| African American | −0.42 | −0.04 | −1.09 | .27 | |||||
| Hispanic | 0.37 | 0.03 | 0.91 | .36 | |||||
| Asian/Pacific Islander | 0.4 | 0.04 | 1.07 | .29 | |||||
| American Indian | −1.23 | −0.03 | −0.78 | .43 | |||||
| Other | −0.28 | −0.02 | −0.51 | .61 | |||||
| Step 2: E-cig User | 0.29 | 0.06 | 1.64 | .10 | 0.01 | 0.05 | <.001 |
Note. Hierarchical regression results with gender, age, and ethnicity entered at step 1 and e-cig use at step 2, ethnicity dummy coded (0,1) with Caucasian as reference group, e-cig status dummy coded 1-e-cig user, 0-non e-cig user.
An ANCOVA (Table 5), controlling for age, gender and ethnicity, indicated that NOSIE-ER Scale 1 scores did not differ significantly by e-cig smoking status (regular user, social user, regular dual user, social dual user), F(5,215)=1.54, p=.18, nor did Scale 2 scores, F(3,216)=1.80, p=.15. Non-users were not included in analysis, as they did not complete the NOSIE-ER
Hierarchical linear regression, controlling for age, gender, and ethnicity, found that, similar to Study 1, total NOSIE-ER scores were significantly associated with AUDIT scores, ΔR2=0.07, p<.001, above and beyond demographics. Average drinks per drinking day, ΔR2=0.01, p=0.20 and Total Drinks, ΔR2=0.01, p=.37, were not significantly associated with total NOSIE-ER scores. Hierarchical linear regressions were then conducted with the NOSIE-ER scales entered separately (Table 8). In contrast to findings in Sample 1, Scale 1 was not significantly associated with AUDIT scores, b=0.04, p=.82, or Total drinks, b=.19, p=.67, and there was a trend towards significance for Average number of drinks per drinking day, b=0.14, p=.07. Scale 2 NOSIE-ER scores were significantly associated with AUDIT scores, b=1.20, p<.001, but not Total drinks, b=0.92, p=.26, or Average number of drinks per drinking day, b=-.08, p=.55.
Table 8.
Sample 2 Hierarchical Linear Regression for NOSIE-ER Scores on Alcohol Consumption Measures
| Dependent Variable | b | B | t | p | ΔR2 | p | R2 | p | |
|---|---|---|---|---|---|---|---|---|---|
| AUDIT | Step1: Age | −0.07 | −0.14 | −2.1 | .30 | 0.07 | 0.02 | ||
| Gender | −0.68 | −0.07 | −1.06 | .30 | |||||
| African American | −3.1 | −0.15 | −2.37 | .02 | |||||
| Hispanic | 1.34 | 0.06 | 1.02 | .31 | |||||
| Asian/Pacific Islander | 0.93 | 0.06 | 0.513 | .61 | |||||
| Other | 0.04 | 0.003 | 0.05 | .95 | |||||
| Step 2: Scale 1 | 0.04 | 0.02 | 0.23 | .82 | 0.07 | <.001 | 0.14 | <.001 | |
| Scale 2 | 1.2 | 0.26 | 3.8 | <.001 | |||||
| Total Drinking Days | Step 1: Age | 0.06 | 0.05 | 0.79 | .43 | 0.04 | 0.13 | ||
| Gender | −4.12 | −0.17 | −2.6 | .01 | |||||
| African American | −3.27 | −0.07 | −1 | .32 | |||||
| Hispanic | 2.97 | 0.06 | 0.91 | .37 | |||||
| Asian/Pacific Islander | 2.81 | 0.04 | 0.62 | .54 | |||||
| Other | −3.31 | −0.04 | −0.62 | .54 | |||||
| Step 2: Scale 1 | 0.19 | 0.03 | 0.43 | .67 | 0.01 | 0.37 | 0.05 | <.001 | |
| Scale 2 | 0.92 | 0.08 | 1.14 | .26 | |||||
| Average Drinks | Step 1: Age | 0.003 | 0.02 | 0.24 | .71 | 0.03 | 0.46 | ||
| Gender | −0.5 | −0.12 | −1.8 | .07 | |||||
| African American | −0.4 | −0.05 | −0.72 | .47 | |||||
| Hispanic | 0.76 | 0.09 | 1.34 | .18 | |||||
| Asian/Pacific Islander | 0.16 | 0.01 | 0.2 | .84 | |||||
| Other | 0.35 | −0.03 | −0.38 | .71 | |||||
| Step 2: Scale 1 | 0.14 | 0.13 | 1.8 | .07 | 0.01 | 0.19 | 0.04 | .34 | |
| Scale 2 | −0.08 | −0.04 | −0.61 | .55 |
Note. Hierarchical regression results with gender, age, and ethnicity entered at step 1 and NOSIE-ER scales at step 2, ethnicity dummy coded (0,1) with Caucasian as reference group
5. General Discussion
Overall, the data from these two independent samples suggest that e-cigs have a similar relationship to alcohol use as do traditional cigarettes. As assessed with our newly created scale, the NOSIE-ER, e-cig users report combined expectancies of e-cig use and alcohol use that are associated with alcohol use. These findings are consistent with previous findings indicating that combined expectancies for alcohol and tobacco use contribute to increased tobacco and alcohol use and AUDs (36–38). E-cig users report higher levels of alcohol use than non e-cig users, suggesting either that e-cig users are at a higher risk for more problematic alcohol use or problematic alcohol users are more likely to use e-cigs. Previous literature has found high e-cig use prevalence rates among substance using populations (9); however, no causal direction has been established to date. Considering that the relationship between cigarettes and alcohol consumption is likely bidirectional (25, 27, 55–57), a similar bidirectional relationship between e-cig and alcohol use would not be surprising.
The finding that regular e-cig users are endorsing significantly higher problematic alcohol consumption is concerning, despite the unknown causal direction. First, e-cigs can be used where traditional cigarettes have been banned and where alcohol is consumed, such as bars and restaurants. Smoking bans inadvertently decreased public alcohol consumption among hazardous drinkers (49–50) perhaps through the extinction of classical conditioning associations between cigarettes and public alcohol consumption. However, given that e-cigs can be used in these locations, e-cig users are able to consume alcohol and use their e-cig together in time and place, which could undo the protective effects of smoking bans on problematic drinking. Also, smokers frequently endorse e-cig use as a smoking cessation device (15–18). If e-cigs are introduced as a smoking cessation device, interventions may perpetuate alcohol consumption or extend the nicotine addiction, especially among those at risk for alcohol and/or nicotine use disorders. This risk could be especially heightened among adolescents given their increased prevalence of e-cig use (58–59).
Many individuals endorse using e-cigs because they believe they are healthier than cigarettes, to circumvent smoking bans, and to quit smoking (10). Despite these endorsements, there is minimal empirical knowledge about the health effects of e-cigs. Results from the current study may suggest that e-cig use might cause inadvertent harm in adults at risk for AUDs, which is a novel finding that warrants further investigations. Expectancies about combined alcohol and e-cig use could serve as an intervention point for individuals at risk for developing an AUD who wish to or are currently using e-cigs. For example, interventions could challenge these expectancies of a need or desire to co-use e-cigs and alcohol. Indeed, previous literature has shown that: (1) expectancies play a causal role in nicotine use (60); (2) expectancy interventions are efficacious in reducing alcohol consumption (61); and (3) targeting both nicotine and alcohol use are an important part of substance treatment (26). Clinicians could challenge these perceived desires or expectancies to co-use e-cigs and alcohol (62).
Despite being cross-sectional in design and utilizing self-report measures, findings of the present studies suggest initial evidence supporting viability for future work examining the theory that alcohol consumption and e-cig use are related and may influence each other. This theory can be improved and expanded upon by future experimental, longitudinal, and clinical studies. Expectancies, craving, and dopaminergic processes should be examined as viable mechanisms underlying combined e-cig and alcohol use. These future studies should examine bidirectional causality. In particular, the NOSIE-ER may serve as a first step at examining this bidirectional effect between e-cig use and alcohol use, given that Scale 1 assesses alcohol leading to e-cig use and Scale 2 assesses e-cig use leading to alcohol use; however, the cross-sectional design of the current study limits such conclusions.
There are some limitations to the current study. First, although “bogus items” were included in the survey, validity of online survey data can be questionable. “Bogus items” were included between the scales and used a different response scale, which may have drawn participant’s attention to them, thus underestimating the amount of random responders. However, 100% of those failing the random responding checks were missing more than 75% of their data, which appeared to occur systematically at the end of the survey; as such, it was likely these individuals began the study and did not complete the study rather than responding randomly. Second, because participants self-selected for the study, individuals who used e-cigs, cigarettes, and alcohol were more likely to participate, which might have biased study findings. However, it is important to note that MTurk has recently been used to research an array of psychological constructs (40–44) and MTurk data has shown good test-retest reliability (45). Third, e-cig and cigarette use were assessed through single face-valid items, which asked participants to choose between social or regular use. The relationships of e-cig status with alcohol use outcomes might differ if cigarette and e-cig use was measured as a continuum (e.g., amount used in a week) rather than a dichotomy. Past studies have characterized e-cig use based on past 30-day use (63). Despite this possible limitation, recent literature has highlighted the importance of examining dual e-cig and cigarette users (64), as assessed in the present study. Overall this study was unique in assessing e-cig use by social use, regular use, regular dual use, and social dual use. It necessitates that future studies use these distinctions in examining e-cig use behavior such as motivations for e-cig use (e.g., to circumvent smoking bans, for smoking cessation). Though more research is needed on the relationship between e-cig use and alcohol consumption, these findings suggest that clinicians should make careful consideration when discussing e-cig use with individuals, particularly with those at risk for an AUD, as there are likely unintended consequences associated with e-cig use.
Highlights.
Development of the NOSIE-ER (ones perceived likelihood of using e-cigs and alcohol together)
NOSIE-ER scores related to problematic alcohol use
E-cig use, compared to no use, related to problematic alcohol use
Acknowledgments
Role of Funding Sources
This research was supported by an NIAAA training grant fellowship, T32 AA07462, awarded to Kenny A. Karyadi and an IUPUI Department of Psychology research grant awarded to Alexandra R. Hershberger. NIAAA and the IUPUI Department of psychology had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or decision to submit the paper for publication.
Footnotes
Contributors
Authors Alexandra Hershberger and Melissa A. Cyders designed the study. Alexandra Hershberger collected and analyzed data, and compiled the manuscript. Author Kenny Karyadi contributed to study design, editing, formatting, citations and data analysis. Author Davis VanderVeen contributed to editing and data analysis, and results write-up. Melissa A. Cyders facilitated the production of the manuscript, providing guidance, assistance, and extensive editing. All authors contributed to and have approved the final manuscript.
Conflict of Interest
All authors declare that they have no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.American Cancer Society. Electronic cigarettes (e-cigarettes) CA: A Cancer Journal for Clinicians. 2014;64:169–170. doi: 10.3322/caac.21228. [DOI] [PubMed] [Google Scholar]
- 2.Dawkins L, Corcoran O. Acute electronic cigarette use: nicotine delivery and subjective effects in regular users. Psychopharmacology. 2013;231(2):401–407. doi: 10.1007/s00213-013-3249-8. [DOI] [PubMed] [Google Scholar]
- 3.Etter JF, Bullen C. Saliva continine levels in users of electronic cigarettes. European Respiratory Journal. 2011;38:1219–1220. doi: 10.1183/09031936.00066011. [DOI] [PubMed] [Google Scholar]
- 4.Dawkins L, Turner J, Hasna S, Soar K. The electronic-cigarette: effects on desire to smoke, withdrawal symptoms, and cognition. Addictive Behaviors. 2012;37:970–973. doi: 10.1016/j.addbeh.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 5.Nides MA, Leisschow SJ, Bhatter M, Simmons M. Nicotine blood levels and short-term smoking reducation with an electronic nicotine delivery system. American Journal of Health Behaviors. 2014;38:265–274. doi: 10.5993/AJHB.38.2.12. [DOI] [PubMed] [Google Scholar]
- 6.Flouris AD, Chorti MS, Poulianti KP, Jamurtas AZ, Kostikas K, Tzatzarakis MN, Wallace Hayes A, Tsatsakis AA, Koutedakis Y. Acute impact of active and passive electronic cigarette smoking on serum cotinine and lung function. Inhalation Toxicology. 2013;25:91–101. doi: 10.3109/08958378.2012.758197. [DOI] [PubMed] [Google Scholar]
- 7.Grana R, Benowitz N, Stant A, Glantz A. Contemporary Reviews in Cardiovascular Medicine: E-cigarettes. Circulation. 2014;129:1972–1986. doi: 10.1161/CIRCULATIONAHA.114.007667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.King BA, Alam S, Promoff G, Arrazola R, Dube SR. Awareness and ever-use of electronic cigarettes among U.S. Adults, 2010–2011. Nicotine and Tobacco Research. 2013;15:1623–1627. doi: 10.1093/ntr/ntt013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peters EN, Harrell PT, Hendricks PS, O’Grady KE, Pickworth WB, Vocci FJ. Electronic cigarettes in adults in outpatient substance use treatment: Awareness perceptions, use, and reasons for use. American Journal on Addictions. doi: 10.1111/ajad.12206. in press. [DOI] [PubMed] [Google Scholar]
- 10.Etter JF, Bullen C. Electronic cigarette: Users profile, utilization, satisfaction and perceived efficacy. Addiction. 2011;106:2017–2028. doi: 10.1111/j.1360-0443.2011.03505.x. [DOI] [PubMed] [Google Scholar]
- 11.Grana RA, Ling PM. ‘Smoking revolution’: A content analysis of electronic cigarette retail websites. American Journal of Preventive Medicine. 2014;46:395–403. doi: 10.1016/j.amepre.2013.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huang J, Kornfield R, Szczypka G, Emery SL. A cross-sectional examination of marketing of electronic cigarettes on Twitter. Tobacco Control: An International Journal. 2014;23(Supp 3):26–30. doi: 10.1136/tobaccocontrol-2014-051551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paek H, Kim S, Hove T, Huh JY. Reduced harm or another gateway to smoking? Source, message, and information characteristics of E-cigarette videos on YouTube. Journal of Health Communication. 2014;19:545–560. doi: 10.1080/10810730.2013.821560. [DOI] [PubMed] [Google Scholar]
- 14.Brown J, Beard E, Kotz D, Michie S, West R. Real-world effectiveness of e-cigarettes when used to aid smoking cessation: a cross sectional population study. Addiction. 2014;109:1531–1540. doi: 10.1111/add.12623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bullen C, Howe C, Laugesen M, McRobbie H, Parag V, Williman J, Walker N. Electronic cigarettes for smoking cessation: A randomized controlled trial. Lancet. 2013;382:1629–1637. doi: 10.1016/S0140-6736(13)61842-5. [DOI] [PubMed] [Google Scholar]
- 16.Caponnetto P, Campagna D, Cibella F, Morjaria JB, Caruso M, Russo C, Polosa R. Efficiency and safety of an eLectronic cigAreTte (ECLAT) as tobacco cigarettes substitute: A prospective 12-Month randomized control design study. Plos ONE. 2013;8:1–12. doi: 10.1371/journal.pone.0066317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Popova L, Ling PM. Alternative tobacco product use and smoking cessation: A national study. American Journal of Public Health. 2013;103:923–930. doi: 10.2105/AJPH.2012.301070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Siegel MB, Tanwar KL, Wood KS. Electronic cigarettes as a smoking-cessation tool: Results from an online survey. American Journal of Preventive Medicine. 2011;40:472–475. doi: 10.1016/j.amepre.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 19.Czogala J, Goniewicz ML, Fidelus B, Zielinska-Danch W, Travers MJ, Sobczak A. Secondhand exposure to vapors from electronic cigarettes. Nicotine & Tobacco Research. 2014;16:655–662. doi: 10.1093/ntr/ntt203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Etter J, Zäther E, Svensson S. Analysis of refill liquids for electronic cigarettes. Addiction. 2013;108:1671–1679. doi: 10.1111/add.12235. [DOI] [PubMed] [Google Scholar]
- 21.Food and Drug and Administration. Summary of results: Laboratory analysis of electronic cigarettes conducted by FDA. 2014 Retrieved from: http://www.fda.gov/NewsEvents/PublicHealthFocus/ucm173146.htm.
- 22.Benoqitze NL. Nicotine addiction. New England Journal of Medicine. 2010;362:2295–2303. doi: 10.1056/NEJMra0809890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grant BF, Hasin DS, Chou SP. Nicotine dependence and psychiatric disorders in the United States, results from the national epidemiologic survey on alcohol and related conditions. Archives of General Psychiatry. 2004;61:1108–1115. doi: 10.1001/archpsyc.61.11.1107. [DOI] [PubMed] [Google Scholar]
- 24.Little HJ. Behavioral mechanisms underlying the link between smoking and drinking. Alcohol Research & Health. 2000;24:215–224. [PMC free article] [PubMed] [Google Scholar]
- 25.McKee SA, Falba T, O’Malley SS, Sindelar J, O’Connor PG. Smoking status as a clinical indicator for alcohol misuse in adults. Archives of Internal Medicine. 2007;167:716–721. doi: 10.1001/archinte.167.7.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kahler CW, Metrik J, LaChance HR, Ramsey SE, Abrams DB, Monti PM, Brown RA. Addressing heavy drinking in smoking cessation treatment: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 2008;76:852–862. doi: 10.1037/a0012717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wilson N, Weerasekera D, Kahler CW, Borland R, Edwards R. Hazardous patterns of alcohol use are relatively common in smokers: ITC Project (New Zealand) The New Zealand medical journal. 2012;125:34–41. [PubMed] [Google Scholar]
- 28.Grucza RA, Bierut LJ. Smoking and the risk for alcohol use disorders among adolescent drinkers. Alcoholism: Clinical and Experimental Research. 2006;30:2046–2054. doi: 10.1111/j.1530-0277.2006.00255.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Funk D, Marinelli PW, Lê A. Biological processes underlying co-use of alcohol and nicotine: Neuronal mechanisms, cross-tolerance, and genetic factors. Alcohol Research & Health. 2006;29:186–192. [PMC free article] [PubMed] [Google Scholar]
- 30.Soderpalm B, Ericson M, Olausson P. Nicotinic mechanisms involved in the dopamine activating and reinforcing properties of ethanol. Behavior and Brain Research. 2000;113:85–96. doi: 10.1016/s0166-4328(00)00203-5. [DOI] [PubMed] [Google Scholar]
- 31.Ericson M, Molander A, Lof E, Engel JA, Soderpalm B. Ethanol elevates accumbal dopamine levels via indirect activation of ventral tegmental nicotinic acetylcholine receptors. European Journal of Pharmacology. 2003;467:85–93. doi: 10.1016/s0014-2999(03)01564-4. [DOI] [PubMed] [Google Scholar]
- 32.Tizabi Y, Copeland RL, Jr, Louis VA, Taylor RE. Effects of combined systemic alcohol and central nicotine administration into ventral tegmental area on dopamine release in the nucleus accumbens. Alcoholism: Clinical and Experimental Research. 2002;26:394–399. [PubMed] [Google Scholar]
- 33.Rohsenow DJ, Monti PM, Colby SM, Gulliver SB, Sirota AD, Niaura RS, Abrams DB. Effects of alcohol cues on smoking urges and topography among alcoholic men. Alcoholism: Clinical and Experimental Research. 1997;21:101–107. [PubMed] [Google Scholar]
- 34.Perkins KA, Sanders M, D’Amico D, Wilson A. Nicotine discrimination and self-administration in humans as a function of smoking status. Psychopharmacology. 1997;131(4):361–370. doi: 10.1007/s002130050304. [DOI] [PubMed] [Google Scholar]
- 35.Drobes DJ. Concurrent alcohol and tobacco dependence: Mechanisms and treatment. Alcohol Research & Health. 2002;26:136–142. [Google Scholar]
- 36.Fearnow-Kenny MD, Wyrick DL, Hansen WB, Dyreg D, Beau DB. Normative beliefs, expectancies, and alcohol-related problems among college students: Implications for theory and practice. Journal Of Alcohol And Drug Education. 2001;47:31–44. [Google Scholar]
- 37.Fromme K, D’Amico EJ. Measuring adolescent alcohol outcome expectancies. Psychology of Addictive Behaviors. 2000;14:206–212. doi: 10.1037//0893-164x.14.2.206. [DOI] [PubMed] [Google Scholar]
- 38.Pabst A, Kraus L, Piontek D, Mueller S, Demmel R. Direct and indirect effects of alcohol expectancies on alcohol-related problems. Psychology Of Addictive Behaviors. 2014;28:20–30. doi: 10.1037/a0031984. [DOI] [PubMed] [Google Scholar]
- 39.Rohsenow DJ, Colby SM, Martin RA, Monti PM. Nicotine and other substance interaction expectancies questionnaire: Relationship of expectancies to substance use. Addictive Behaviors. 2005;30:629–641. doi: 10.1016/j.addbeh.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 40.Boynton MH, Richman LS. An online daily diary study of alcohol using Amazon’s Mechanical Turk. Drug and Alcohol Review. 2014;33:456–461. doi: 10.1111/dar.12163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Holden CJ, Dennie T, Hicks AD. Assessing the reliability of the M5-120 on Amazon’s Mechanical Turk. Computers In Human Behavior. 2013;29(4):1749–1754. [Google Scholar]
- 42.Adams HM, Luevano VX, Jonason PK. Risky business: Willingness to be caught in an extra-pair relationship, relationship experience, and the Dark Triad. Personality and Individual Differences. 2014;66:204–207. [Google Scholar]
- 43.Andover MS. Non-suicidal self-injury disorder in a community sample of adults. Psychiatry Research. 2014;219(2):305–310. doi: 10.1016/j.psychres.2014.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Papa A, Lancaster NG, Kahler J. Commonalities in grief responding across bereavement and non-bereavement losses. Journal Of Affective Disorders. 2014;161:136–143. doi: 10.1016/j.jad.2014.03.018. [DOI] [PubMed] [Google Scholar]
- 45.Shapiro DN, Chandler J, Mueller PA. Inside the Turk: Understanding Mechanical Turk as a participant pool. Clinical Psychological Science. 2013;1(2):213–220. [Google Scholar]
- 46.Saunders JB, Aasland OG, Babor TF, De la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption I. Addiction. 1993;88:349–362. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 47.Donovan DM, Kivlahan DR, Doyle SR, Longabaugh R, Greenfield SF. Concurrent validity of the Alcohol Use Disorders Identification Test (AUDIT) and AUDIT zones in defining levels of severity among out-patients with alcohol dependence in the COMBINE study. Addiction. 2006;101:1696–1704. doi: 10.1111/j.1360-0443.2006.01606.x. [DOI] [PubMed] [Google Scholar]
- 48.Sobell LC, Sobell MB. Timeline followback: A technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen J, editors. Measuring alcohol consumption: Psychosocial and biological methods. New Jersey: Humana Press; 1992. pp. 41–72. [Google Scholar]
- 49.DeMarce JM, Burden JL, Lash SJ, Stephens RS, Grambow SC. Convergent validity of the Timeline Followback for persons with comorbid psychiatric disorders engaged in residential substance use treatment. Addictive Behaviors. 2007;32:1582–1592. doi: 10.1016/j.addbeh.2006.11.015. [DOI] [PubMed] [Google Scholar]
- 50.Meade AW, Craig SB. Identifying careless responses in survey data. Psychological Methods. 2012;17(3):437–455. doi: 10.1037/a0028085. [DOI] [PubMed] [Google Scholar]
- 51.Horton JJ, Rand DG, Zeckhauser RJ. The online laboratory: Conducting experiments in a real labor market. Experimental Economics. 2011;14:399–425. [Google Scholar]
- 52.Little RJA, Rubin DB. Statistical analyses with missing data. 2. Princeton, NJ: Wiley; 2002. [Google Scholar]
- 53.Beaujean AA. Latent variable modeling using R: A step-by-step guide. New York, NY: Routledge/Taylor & Francis Group; 2014. [Google Scholar]
- 54.Hu L, Bentler PM. Fit indicies in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods. 1998;3(4):424–453. [Google Scholar]
- 55.Harrison EL, Hinson RE, McKee SA. Experimenting and daily smokers: episodic patterns of alcohol and cigarette use. Addictive behaviors. 2009;34:484–486. doi: 10.1016/j.addbeh.2008.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mathers M, Toumbourou JW, Catalano RF, Williams J, Patton GC. Consequences of youth tobacco use: A review of prospective behavioural studies. Addiction. 2006;101:948–958. doi: 10.1111/j.1360-0443.2006.01438.x. [DOI] [PubMed] [Google Scholar]
- 57.Sayette MA, Martin CS, Wertz JM, Perrott MA, Peters AR. The effects of alcohol on cigarette craving in heavy smokers and tobacco chippers. Psychology of Addictive Behaviors. 2005;19(3):263–270. doi: 10.1037/0893-164X.19.3.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.King BA, Alam S, Promoff G, Arrazola R, Dube SR. Awareness and ever-use of electronic cigarettes among US adults, 2010–2011. Nicotine & Tobacco Research. 2013;15(9):1623–1627. doi: 10.1093/ntr/ntt013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Centers for Disease Control and Prevention. Tobacco use among middle school and high school students-United States 2013. MMWR Morbidity and Mortality Weekly Report. 2013;63:1021–1026. http://origin.glb.cdc.gov/mmwr/preview/mmwrhtml/mm6345a2.htm. [PMC free article] [PubMed] [Google Scholar]
- 60.Copeland AL, Brandon TH. Testing the causal role of expectancies in smoking motivation and behavior. Addictive Behaviors. 2000;25(3):445–449. doi: 10.1016/s0306-4603(99)00003-9. [DOI] [PubMed] [Google Scholar]
- 61.Lau-Barraco C, Dunn ME. Evaluation of a single-session expectancy challenge intervention to reduce alcohol use among college students. Psychology Of Addictive Behaviors. 2008;22(2):168–175. doi: 10.1037/0893-164X.22.2.168. [DOI] [PubMed] [Google Scholar]
- 62.Scott-Sheldon LJ, Terry DL, Carey KB, Garey L, Carey MP. Efficacy of expectancy challenge interventions to reduce college student drinking: A meta-analytic review. Psychology Of Addictive Behaviors. 2012;26(3):393–405. doi: 10.1037/a0027565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Pokhrel P, Little MA, Fagan P, Muranaka N, Herzog TA. Electronic cigarette use outcome expectancies among college students. Addictive behaviors. 2014;39:1062–1065. doi: 10.1016/j.addbeh.2014.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Farsalinos KE, Romagna G, Voudris V. Factors associated with dual use of tobacco and electronic cigarettes: A case control study. International Journal of Drug Policy. doi: 10.1016/j.drugpo.2015.01.006. in press. [DOI] [PubMed] [Google Scholar]