Abstract
Objectives
The purpose of this study is to evaluate five-year radiographic follow-up results of the Korean sandblasting with large grit, and acid etching (SLA)-treated implant system.
Materials and Methods
The subjects of the study are 54 patients who have been followed-up to date, of the patients who underwent implant surgery from May 1, 2009 to April 30, 2011. In all, 176 implant placements were performed. Radiographs were taken before the first surgery, immediately after the first and second surgeries, immediately and six months after the final prosthesis installation, and every year after that. Bone loss was evaluated by the method suggested by Romanos and Nentwig.
Results
A total of 176 implant placements were performed-122 in men and 54 in women. These patients have been followed-up for an average of 4.9 years. In terms of prosthetic appliances, there were 156 bridges and 20 single prostheses. Nine implants installed in the maxillary molar area, three in the mandibular molar area and two in the maxillary premolar area were included in group M, with bone loss less than 2 mm at the crestal aspect of the implant. Of these, eight implants were single prostheses. In all, six implants failed-four in the mandible and two in the maxilla. All of these failures occurred in single-implant cases. The implant survival rate was 98.1% on the maxilla and 94.3% on the mandible, with an overall survival of 96.6%.
Conclusion
Within the limitations of this study, implants with the SLA surface have a very superior survival rate in relatively poor bone environments such as the maxilla.
Keywords: Dental implants, Survival rate
I. Introduction
The application of osseointegration, introduced by Branemark, was initially limited to edentulous patients but is now widely used in both edentulous patients and patients with missing individual teeth. Replacement of missing teeth by dental implant has become an integral part of modern dental health care1.
There has been much technological development to enhance the survival rates of implants, particularly with regard to implant surface treatment. Albrektsson et al.2 reported that, when an implant had a rough surface rather than a machined surface, more rapid bone growth and superior physical adhesion were observed, while osteoblasts were better attached to rough surface implants, thus influencing the maturation, differentiation, and bone-implant interface of attached cells. Wennerberg et al.3 reported that a rough surface implant had larger bone-implant contact (BIC) and higher removal torque compared with a machined surface implant.
Surface treatment methods, by which an implant surface is made rough to increase the bone-implant interface, include acid etching4, blasting5, hydroxyapatite coating6, titanium plasma spray7 and sandblasting with large grit, and acid etching (SLA)8.
Buser et al.9 reported that the 10-year survival rate of implants with the SLA surface was 98.8%, while the prevalence of peri-implantitis over 10 years was 1.8%.
In the present study, the authors evaluated the five-year survival rate and the surrounding bony change of dental implants with the SLA surface (Snucone Dental Implant, Daegu, Korea).
II. Materials and Methods
The subjects in the study are 54 patients who have been followed-up to date, of the patients who underwent implant surgery at Chungnam National University Hospital (Daejeon, Korea) from May 1, 2009 through April 30, 2011. Medically compromised patients were sent them to physicians to undergo medical treatment prior to implant surgery. In all, 176 implant placements were performed.
The implant surgeries were divided into first and the second surgeries and were carried out in two stages. The surgeries and prosthetic treatments were carried out by one skillful oral and maxillofacial surgeon.
The first surgeries were performed according to general surgery principles and a protocol provided by the manufacturer. In the case of lateral window opening cases, horizontal and vertical incisions were made on the alveolar ridge and the lateral surface of the maxillary sinus, respectively, for exposure of the lateral surface of the maxillary sinus. In all lateral window opening cases, the bone graft material and the membrane were xenograft (Bio-Oss; Geistlich Pharma AG, Wolhusen, Switzerland) and collagen membrane (Bio-Gide; Geistlich Pharma AG), respectively. After the first surgeries, antibiotics and analgesics were prescribed for all patients for seven to ten days. All the patients were instructed to not apply any stimuli to the surgical site until the removal of the stitches. They were also instructed to perform a 0.12% chlorhexidine mouth rinse three or four times a day. The removal of the stitches usually occurred after 10 days. In the mandible, the second surgery was performed an average of 2.5 months after the first surgery. In the maxilla, however, the second surgery was performed five months after the first. For lateral window opening cases, the second surgery was performed seven months after the first. Dental impressions were usually performed two weeks after the second surgery, and temporary prostheses were installed one week after the impressions were created. One month after temporary prosthesis setting, the final prostheses were manufactured and set. Panoramic radiographs were collected before and immediately after the first surgery, after the second surgery, immediately after the final prosthesis setting, three months after the final prosthesis setting, six months after the final prosthesis setting, and every year after that.
Bone loss surrounding an implant was evaluated in accordance with the method suggested by Romanos and Nentwig10. Evaluation of bone loss was graded as follows: group 0, no bone loss; group M, minimal bone loss (less than 2 mm at the crestal aspect of the implant); group 1, bone loss involving 1/4 of the implant length; group 2, progressive bone loss between 1/4 and 1/2 of the implant length.
Bone loss measurements were made on the mesial and distal sides of the fixture-abutment junction to the cortical bone. The values from the mesial and distal sides were averaged to be used in the evaluation. Bone loss was evaluated by calculation of the rates to the known length of the fixture. The radiographs taken right after the final setting of the prosthetic appliance were compared with the follow-up radiographs for evaluation.
As the number of implants placed was not large, no statistical analysis was performed.
III. Results
Of the 54 patients, 40 were male and 14 female. The age range of the men was 24 years to 70 years, with an average of 54.8 years. The age range of the women was 39 years to 75 years, with an average of 57.4 years. Among men, those in their 50s were the most common, at 20 patients. Among women, those in their 60s were the most common, at 6 patients. Of the 176 implants, 106 were placed in the maxilla, while 70 were placed in the mandible; 122 implants were performed in men and 54 in women.(Table 1)
Table 1. Location of implant.
| Gender | Mx. anterior | Mx. premolar | Mx. molar | Mn. anterior | Mn. premolar | Mn. molar | Total |
|---|---|---|---|---|---|---|---|
| Male | 6 | 18 | 42 | 4 | 12 | 40 | 122 |
| Female | 10 | 10 | 20 | 2 | 2 | 10 | 54 |
| Total | 16 | 28 | 62 | 6 | 14 | 50 | 176 |
(Mx.: maxilla, Mn.: mandible)
Values are presented as number of implants
Fixtures 4.3 mm in diameter and 10 mm in length were used most often. The number of the fixtures used is shown in Table 2.
Table 2. Fixture diameter and length.
| Length×diameter (mm) | Number of fixtures |
|---|---|
| 3.5×10 | 22 |
| 4.0×10 | 37 |
| 4.3×8 | 31 |
| 4.3×10 | 47 |
| 4.8×8 | 19 |
| 4.8×10 | 20 |
In lateral window opening cases, 30 implant placements were performed in 18 cases in 16 men, and 14 implant placements in eight cases in eight women. An osteotome technique with a crestal approach was used for 14 implant placements in 10 men, while no women were treated with an osteotome technique.
As for the kinds of prosthetic appliances, the number of the implants manufactured as a bridge was 156, while the number of single prostheses was 20.
In a total of 54 patients, 176 implants underwent follow-up. The range of the follow-up periods was four years to six years, with an average of 4.9 years. The bone loss evaluated by the method suggested by Romanos and Nentwig10 is shown in Table 3.
Table 3. Evaluation of bone loss surrounding an implant.
| Group | Prosthesis setting | 1 yr | 2 yr | Most recent follow-up |
|---|---|---|---|---|
| Group 0 | 176 | 164 | 162 | 162 |
| Group M | - | 12 | 14 | 14 |
| Group 1 | - | - | - | - |
| Group 2 | - | - | - | - |
(Group 0: no bone loss, Group M: bone loss less than 2 mm at the crestal aspect of the implant, Group 1: bone loss involving 1/4 of the implant length, Group 2: progressive bone loss between 1/4 and 1/2 of the implant length)
No implants were included in group 1 or 2.
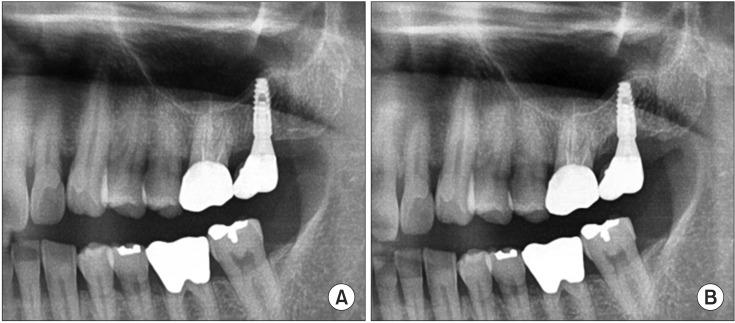
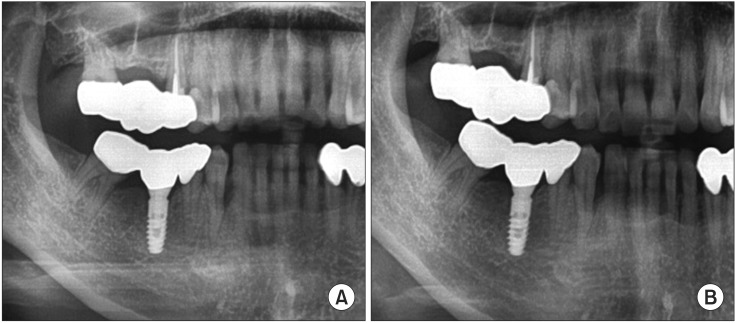
The numbers of implants included in group M were nine for molar teeth in the maxilla, three for molar teeth in a mandible, and two for premolar teeth in the maxilla.(Fig. 1) Of these, five teeth in molar areas in the maxilla and three teeth in molar areas in the mandible were single prostheses. The horizontal positions of the alveolar bone were maintained in a relatively stable state in the rest of the implants.(Fig. 2)
Fig. 1. A. One dental implant was placed at the maxillary left second molar site with an osteotome sinus elevation technique in 2010. B. Marginal bone loss surrounding an implant was observed in group M (bone loss less than 2 mm at the crestal aspect of the implant) in 2015.
Fig. 2. A. One dental implant was placed at the mandibular right first molar in 2011. B. A 4-year follow-up radiograph demonstrated excellent maintenance of marginal bone surrounding an implant.
A total of six implants failed-four in the mandible and two in the maxilla; all of these were single-implant cases. In one case, a fixture placed in the mandible of a male patient experienced fracture. In three cases, the patients were receiving chemotherapy, while two patients were suffering from diabetes or chronic renal failure. In all five cases, except for the patient with the fractured fixture, no abnormalities were found in the radiograph tests performed right before the implant failures occurred. When the implants were removed, there was little bleeding. All the failed implants belonged to group 0, and no failed implants belonged to group M.
The implant survival rate was 98.1% in the maxilla and 94.3% in the mandible, resulting in an overall survival of 96.6%.
IV. Discussion
Treatment using dental implants has become an integral part of modern dental health care. Studies are continually being performed to improve the survival rate of implants and to shorten the healing period through development of bone graft material and improvement of surgical methods, implant design, and surface treatment methods. Fast healing of peri-implant bone after implant placement and continuous and stable maintenance of osseointegration are important factors. The implant surface itself is very important for long-term success. Several studies have shown that a rough surface implant has more merits than a machined surface implant2,11,12,13,14.
Osteoblasts have greater binding affinity with a rough surface than with a machined surface, while a rough surface influences the maturation, differentiation, and bone-implant interface of attached cells. Deposition of an inorganic component in bone tissues and the bone cell alkaline phosphatase activity have been found to be higher on a rough implant surface. Thus, a rough surface implant shows larger BIC than a machined surface implant5,15,16.
The surface treatment method, which is widely used lately, uses either resorbable blasting media (RBM) or SLA. The RBM method uses resorbable particles, such as calcium phosphate, in order to supplement the shortfall of blasted particles left on the implant surface5.
Im et al.17 reported higher BIC in SLA implants (82.7%) than in RBM implants (78.3%) 12 weeks after implant placement in adult mutts. Elkhaweldi et al.18, who compared the survival rate of RBM surface implants with that of SLA surface implants, reported that the former was 95.2% and the latter 99.1%, with a higher survival rate observed in SLA surface implants. They reported that SLA surface implants produced better results in the posterior maxilla with poor bone.
For long-term success of an implant, stable maintenance of the peri-implant bone is an important indicator. In this study, we evaluated the bone loss in accordance with the method suggested by Romanos and Nentwig10.
The implants included in group M were placed in areas experiencing high occlusal force, while they occurred between two and three years after the final placement of the prosthetic appliances, and many of them were in the maxilla.
Considering that most of the failed implants occurred within one year after placement, a somewhat longer follow-up period is thought to be needed. The reason for the higher number of failures in the maxilla is thought to be similar to the reason for the lower implant survival rate in the upper jaw than in the mandible18,19.
After about one year, peri-implant bone had become stable, and little subsequent change was observed. The use of panoramic radiographs, which have lower resolution than periapical radiographs, might have resulted in a somewhat low accuracy; however, it is believed that there were no major errors because we performed the measurements in consideration of the rates to the known length of the fixtures.
In the external type of implant, where the abutment and the fixture are connected with a butt joint connection system, sealing was not secured between the abutment and the fixture, allowing the possibility of microleakage of bacteria. In addition, most of the stress caused by occlusal force is concentrated on the fixture top, causing marginal bone loss20.
Therefore, in the external type of implant, bone loss of 1.5 mm or less, with exposure of one or two threads, one year after loading and bone loss of 0.2 mm of less per year after that have generally been accepted as normal21.
Lazzara and Porter22 introduced a platform switching concept and demonstrated the maintenance of healthy soft tissue around an implant, with little marginal bone loss.
An internal type of implant was used in this study, where the abutment and the fixture were connected onto a slip joint connection system, similar to the platform switching concept, and where, it is believed, the fixture and the abutment were so closely connected that no microleakage occurred and healthy biologic width was maintained, maintaining the marginal bone.
Except for the one fractured implant, all five failed implants occurred in patients suffering from serious systemic diseases. There were no abnormalities found in the panoramic view examinations of these patients, and clinical examinations were performed right before the failures. Unless demineralization of bone exceeds 30% or more, it is difficult to evaluate the bony lesion; therefore, we used panorama radiographs, whose resolution is slightly lower than that of periapical radiographs. This might be one reason why we did not note bony change. For this reason, we think radiographs, which are more accurate, are necessary in implant follow-up. There were no failed implants in the group M.
The survival rate of SLA-treated implants was 98.1% in the maxilla and 94.3% in the mandible, with an overall survival rate of 96.6%. The reported 10-year survival rate ranges from 90% to 98.8% in recent article23. Another article reported a 12-year survival rate of 100%9.
V. Conclusion
Within the limitations of this study, implants with the SLA surface have a very superior survival rate. In particular, implants with the SLA surface seem to be superior in areas of relatively poor bone such as the maxilla. It is necessary to evaluate marginal bone loss using more accurate radiographs, such as periapical radiographs or cone-beam computed tomography, throughout the treatment periods.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Brånemark PI, Adell R, Albrektsson T, Lekholm U, Lundkvist S, Rockler B. Osseointegrated titanium fixtures in the treatment of edentulousness. Biomaterials. 1983;4:25–28. doi: 10.1016/0142-9612(83)90065-0. [DOI] [PubMed] [Google Scholar]
- 2.Albrektsson T, Brånemark PI, Hansson HA, Lindström J. Osseointegrated titanium implants. Requirements for ensuring a longlasting, direct bone-to-implant anchorage in man. Acta Orthop Scand. 1981;52:155–170. doi: 10.3109/17453678108991776. [DOI] [PubMed] [Google Scholar]
- 3.Wennerberg A, Ektessabi A, Albrektsson T, Johansson C, Andersson B. A 1-year follow-up of implants of differing surface roughness placed in rabbit bone. Int J Oral Maxillofac Implants. 1997;12:486–494. [PubMed] [Google Scholar]
- 4.Trisi P, Lazzara R, Rao W, Rebaudi A. Bone-implant contact and bone quality: evaluation of expected and actual bone contact on machined and osseotite implant surfaces. Int J Periodontics Restorative Dent. 2002;22:535–545. [PubMed] [Google Scholar]
- 5.Piattelli M, Scarano A, Paolantonio M, Iezzi G, Petrone G, Piattelli A. Bone response to machined and resorbable blast material titanium implants: an experimental study in rabbits. J Oral Implantol. 2002;28:2–8. doi: 10.1563/1548-1336(2002)028<0002:BRTMAR>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.Block MS, Kent JN, Kay JF. Evaluation of hydroxylapatite-coated titanium dental implants in dogs. J Oral Maxillofac Surg. 1987;45:601–607. doi: 10.1016/0278-2391(87)90270-9. [DOI] [PubMed] [Google Scholar]
- 7.Wennerberg A, Albrektsson T. On implant surfaces: a review of current knowledge and opinions. Int J Oral Maxillofac Implants. 2010;25:63–74. [PubMed] [Google Scholar]
- 8.Cochran DL, Buser D, ten Bruggenkate CM, Weingart D, Taylor TM, Bernard JP, et al. The use of reduced healing times on ITI implants with a sandblasted and acid-etched (SLA) surface: early results from clinical trials on ITI SLA implants. Clin Oral Implants Res. 2002;13:144–153. doi: 10.1034/j.1600-0501.2002.130204.x. [DOI] [PubMed] [Google Scholar]
- 9.Buser D, Janner SF, Wittneben JG, Brägger U, Ramseier CA, Salvi GE. 10-year survival and success rates of 511 titanium implants with a sandblasted and acid-etched surface: a retrospective study in 303 partially edentulous patients. Clin Implant Dent Relat Res. 2012;14:839–851. doi: 10.1111/j.1708-8208.2012.00456.x. [DOI] [PubMed] [Google Scholar]
- 10.Romanos GE, Nentwig GH. Single molar replacement with a progressive thread design implant system: a retrospective clinical report. Int J Oral Maxillofac Implants. 2000;15:831–836. [PubMed] [Google Scholar]
- 11.Bowers KT, Keller JC, Randolph BA, Wick DG, Michaels CM. Optimization of surface micromorphology for enhanced osteoblast responses in vitro. Int J Oral Maxillofac Implants. 1992;7:302–310. [PubMed] [Google Scholar]
- 12.Rich A, Harris AK. Anomalous preferences of cultured macrophages for hydrophobic and roughened substrata. J Cell Sci. 1981;50:1–7. doi: 10.1242/jcs.50.1.1. [DOI] [PubMed] [Google Scholar]
- 13.Martin JY, Schwartz Z, Hummert TW, Schraub DM, Simpson J, Lankford J, Jr, et al. Effect of titanium surface roughness on proliferation, differentiation, and protein synthesis of human osteoblastlike cells (MG63) J Biomed Mater Res. 1995;29:389–401. doi: 10.1002/jbm.820290314. [DOI] [PubMed] [Google Scholar]
- 14.den Braber ET, de Ruijter JE, Smits HT, Ginsel LA, von Recum AF, Jansen JA. Effect of parallel surface microgrooves and surface energy on cell growth. J Biomed Mater Res. 1995;29:511–518. doi: 10.1002/jbm.820290411. [DOI] [PubMed] [Google Scholar]
- 15.Wennerberg A, Albrektsson T, Andersson B, Krol JJ. A histomorphometric and removal torque study of screw-shaped titanium implants with three different surface topographies. Clin Oral Implants Res. 1995;6:24–30. doi: 10.1034/j.1600-0501.1995.060103.x. [DOI] [PubMed] [Google Scholar]
- 16.Wennerberg A, Albrektsson T, Lausmaa J. Torque and histomorphometric evaluation of c.p. titanium screws blasted with 25- and 75-microns-sized particles of Al2O3. J Biomed Mater Res. 1996;30:251–260. doi: 10.1002/(SICI)1097-4636(199602)30:2<251::AID-JBM16>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 17.Im JH, Kim SG, Oh JS, Lim SC. A comparative study of stability after the installation of 2 different surface types of implants in the maxillae of dogs. Implant Dent. 2015;24:586–591. doi: 10.1097/ID.0000000000000292. [DOI] [PubMed] [Google Scholar]
- 18.Elkhaweldi A, Lee DH, Wang W, Cho SC. The survial rate of RBM surface versus SLA surface in geometrically identical implant design. J Oral Bio. 2014;1:1–8. [Google Scholar]
- 19.Higuchi KW, Folmer T, Kultje C. Implant survival rates in partially edentulous patients: a 3-year prospective multicenter study. J Oral Maxillofac Surg. 1995;53:264–268. doi: 10.1016/0278-2391(95)90222-8. [DOI] [PubMed] [Google Scholar]
- 20.Quirynen M, Bollen CM, Eyssen H, van Steenberghe D. Microbial penetration along the implant components of the Brånemark system. An in vitro study. Clin Oral Implants Res. 1994;5:239–244. doi: 10.1034/j.1600-0501.1994.050407.x. [DOI] [PubMed] [Google Scholar]
- 21.Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986;1:11–25. [PubMed] [Google Scholar]
- 22.Lazzara RJ, Porter SS. Platform switching: a new concept in implant dentistry for controlling postrestorative crestal bone levels. Int J Periodontics Restorative Dent. 2006;26:9–17. [PubMed] [Google Scholar]
- 23.Östman PO, Hellman M, Sennerby L. Ten years later. Results from a prospective single-centre clinical study on 121 oxidized (TiUnite™) Brånemark implants in 46 patients. Clin Implant Dent Relat Res. 2012;14:852–860. doi: 10.1111/j.1708-8208.2012.00453.x. [DOI] [PubMed] [Google Scholar]