Abstract
Context
Health insurance benefits for mental health services typically have paid less than benefits for physical health services, resulting in potential underutilization or financial burden for people with mental health conditions. Mental health benefits legislation was introduced to improve financial protection (i.e., decrease financial burden) and to increase access to, and use of, mental health services. This systematic review was conducted to determine the effectiveness of mental health benefits legislation, including executive orders, in improving mental health.
Evidence acquisition
Methods developed for the Guide to Community Preventive Services were used to identify, evaluate, and analyze available evidence. The evidence included studies published or reported from 1965 to March 2011 with at least one of the following outcomes: access to care, financial protection, appropriate utilization, quality of care, diagnosis of mental illness, morbidity and mortality, and quality of life. Analyses were conducted in 2012.
Evidence synthesis
Thirty eligible studies were identified in 37 papers. Implementation of mental health benefits legislation was associated with financial protection (decreased out-of-pocket costs) and appropriate utilization of services. Among studies examining the impact of legislation strength, most found larger positive effects for comprehensive parity legislation or policies than for less-comprehensive ones. Few studies assessed other mental health outcomes.
Conclusions
Evidence indicates that mental health benefits legislation, particularly comprehensive parity legislation, is effective in improving financial protection and increasing appropriate utilization of mental health services for people with mental health conditions. Evidence is limited for other mental health outcomes.
Context
The domestic disease burden of mental health (MH) disorders (including substance use) is well established.1–4 Nearly 20% of U.S. adults reported a diagnosable mental illness in 2012,5 and nearly 50% will experience at least one during their lifetime.1–4 A 1999 U.S. Surgeon General’s report estimates that mental illness is the second largest contributor to disease burden in established market economies such as the U.S.6
Moreover, untreated and undertreated MH disorders contribute to the high domestic burden.7–9 In a 2012 national survey, only 62.9% of adults with a serious mental illness had received any MH services in the past year and only 10.8% of 23.1 million individuals with substance use disorders had been treated.10 Many affected people cite cost as a major factor preventing them from seeking health care.5,6,9,11 In 2009, more than half of American families reported limiting health care in the previous year because of cost, and nearly 20% indicated substantial financial concerns associated with medical bills.9,11
Mental health benefits legislation (MHBL) involves changing regulations for MH insurance coverage to improve financial protection (i.e., decrease financial burden) and to increase access to, and use of, MH services including substance abuse (SA) services. Such legislation can be enacted at the federal or state level and categorized as:
parity, which is on a continuum from limited (covering only a few mental illnesses) to comprehensive (covering all mental illness), with varying degrees of benefits; or
mandate laws, which: (1) provide some specified level of MH coverage; (2) offer option of MH coverage; or (3) require a minimum benefits level if providing MH coverage.
Thus, MHBL is intended to reduce out-of-pocket costs and increase access to care, creating the potential for increased utilization among those in need of MH services.
Legislative Context
Prior to enactment of comprehensive MH/SA parity legislation, health insurance plans generally offered less-extensive coverage for MH/SA services compared with physical health services.12 Three federal laws—the 1996 MH Parity Act13 (MHPA, Title VII), the 2008 Paul Wellstone and Pete Domenici MH Parity, Addiction Equity Act14 (MHPAEA, Subtitle B), and the Affordable Care Act (ACA)15—have addressed parity in MH and MH/SA benefits.16 As of January 2014, mandate legislation had been passed by 49 states and the District of Columbia.17
The first official MH/SA insurance parity action occurred in 1961 through an executive order requiring the Federal Employees Health Benefits (FEHB) Program to cover psychiatric illnesses at a level equivalent to general medical care.18 Parity was offered in two FEHB insurance plans from 1967 until 1975, when it was discontinued because of increases in cost and utilization associated with adverse selection and moral hazard.a,19,20 The uptake of managed care as a mechanism for reducing “inappropriate” utilization of services in the late 1980s and early 1990s provided economic feasibility and renewed the political viability of MH/SA parity legislation.21,22
The first federal parity law in 1996, the MHPA, required lifetime and annual limits for MH services to be no different than physical health services.16 The legislation was limited with no provisions for parity in SA services, treatment limitations, or cost-sharing mechanisms. Thus, the legislation had little impact, although it served as a catalyst for subsequent MHBL, particularly at the state level.23 In 1999, a second executive order was issued to implement full parity in the FEHB Program, extending MH/SA parity to approximately 8.5 million beneficiaries.24 The second federal legislation in 2008, the MHPAEA, was part of the Emergency Economic Stabilization Act.17,25 The MHPAEA was more comprehensive, requiring that financial requirements and treatment limitations beyond annual and lifetime dollar limits for MH/SA be no different than those for physical health.26 However, the MHPAEA retained exemptions for employers with ≤50 employees or demonstrating a 2% cost increase annually as a result of the legislation. The most recent federal legislation, the ACA in 2010, extended existing federal MH/SA parity requirements and differed from previous federal legislation by requiring: (1) qualified health plans to offer MH and SA coverage; and (2) coverage of specific MH/SA services for certain health plans.15 See Appendix A (available online) for more details.
The purpose of this systematic review was to summarize and assess evidence on the effectiveness of MHBL in improving MH and related outcomes.
Evidence Acquisition
The Community Guide systematic review process was used to assess the effectiveness of MHBL.27,28,29 The process involved forming a systematic review team to work with oversight from the independent, nonfederal, unpaid Community Preventive Services Task Force (Task Force), to develop evidence-based recommendations.
Conceptual Approach and Analytic Framework
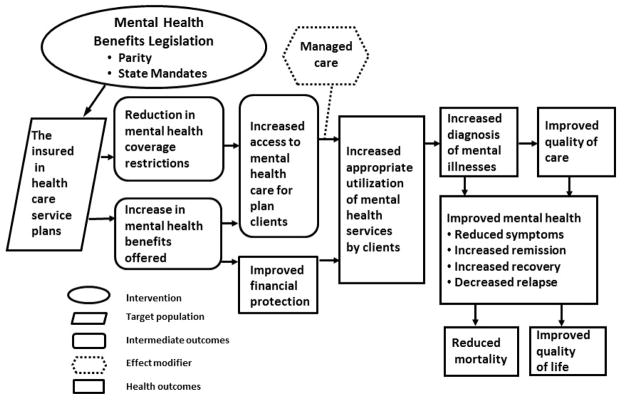
The conceptual approach depicting inter-relationships among interventions, populations, and outcomes is represented in the analytic framework (Figure 1). The team hypothesized that MHBL will affect the insured population through reductions in MH/SA coverage restrictions and through increases in MH/SA benefits offered. This will lead to improvements in access to care and financial protection, which may increase appropriate utilization, diagnosis, and quality of care. Subsequent reductions in morbidity and mortality and improvements in quality of life are expected. Managed care is included as an effect modifier implemented before, concurrent with, or after MHBL, and expected to offset anticipated increases in cost and utilization from MHBL.
Figure 1.
Analytic framework: hypothesized ways in which mental health benefits legislation improves mental health.
Research Questions
This review addressed a comprehensive research question: Is legislation for MH/SA benefits effective in improving MH in the community by increasing (1) access to care, (2) financial protection, (3) appropriate utilization of MH services, (4) diagnosis of mental illness, and (5) quality of care; by reducing (6) morbidity and (7) mortality; and by improving (8) quality of life?
Outcome Measures Used to Determine Effectiveness
Outcomes assessed in this review are defined briefly here. See Appendix B (available online) for full definitions and examples.
Access to care. The ability of those with public or private insurance to obtain MH/SA care including workforce coverage for MH/SA benefits.
Financial protection. The reduction in out-of-pocket costs paid by an individual for MH/SA services; includes measures of out-of-pocket spending.30,31
Appropriate utilization. Receiving the proper amount and quality of services when needed, including: (1) utilization of MH/SA services by people in need; (2) services rendered by MH specialists (e.g., psychiatrist, psychologist, social worker); or (3) receipt of services consistent with evidence-based guidelines for MH/SA care.
Diagnosis. The determination that a person meets established criteria for an MH condition.
Quality of care. Health services that are likely to result in the desired health outcomes and are consistent with current professional knowledge.32
Morbidity. The presence of any MH condition, such as depression.
Mortality. Any death associated with an MH condition, such as suicide.
Quality of life (health-related). Perception of physical and mental health over time.33
Search for Evidence
Eighteen bibliographic databases were searched from their inception through March 2011. Other sources included reference lists; suggestions from team members and other subject matter experts; and searches through Internet portals, Google, and the National Council on State Legislatures website.17 The search included terms related to parity, MH, SA, and insurance. Search terms and strategy are available at www.thecommunityguide.org/mentalhealth/SS-benefitslegis.html.
Inclusion criteria
Studies were included if they: (1) evaluated an intervention relating to MHBL, including executive orders at the federal or state level; (2) measured and reported at least one review outcome; and (3) were reported in English.
Exclusion criteria
Studies were excluded if they were: (1) based primarily on simulation data; (2) reforms to restructure care only, such as Medicaid waivers; (3) single-disease mandates, such as coverage mandate for autism only; and (4) implemented outside the U.S., because of differences in health systems and legislation.
Abstraction and Evaluation of Studies
Two reviewers evaluated each study using an adaptation of a standardized abstraction form, which included a quality assessment (www.thecommunityguide.org/methods/abstractionform.pdf).29 Disagreements were resolved by discussion and team consensus. DistillerSR, version 1 was used to manage references, screen citations, and abstract data. Microsoft Excel, 2010 was used for effect size calculation and other analyses. Papers based on the same study data set were linked; only the paper with the most complete data (e.g., longest follow-up) was included in analyses. See Appendix C (available online) for more details.
Summarizing the Body of Evidence on Effectiveness
Effect measurement and data synthesis
Effect estimates of absolute percentage point (pct pt) change or relative percentage change were calculated with corresponding 95% CIs and adjusted for baseline data when possible. Regression coefficients or ORs were used as the effect estimates when reported.
Summary effect estimates (medians), interquartile intervals (IQIs), and number of studies are reported when outcomes contained five or more data points. Results for most outcomes of interest were synthesized descriptively and p-values are reported when available. Tables illustrating the effect direction are used to display effects based on methods developed by Thomson and Thomas34 (see Appendix C, available online, for formulas and details on data synthesis). Analyses were conducted in 2012.
Subgroup analyses
Two comparisons were assessed qualitatively: (1) stronger parity legislation versus no or weak parity legislation35–37; and (2) mutually exclusive categories of parity versus no or weak parity legislation.38–40 Categories of parity were based on primary author’s definitions.
Subgroup analyses were also planned to compare outcomes by settings (e.g., U.S. states), clients (e.g., age group, racial and ethnic group, type of mental illness), employer size, and health plan type (e.g., public versus private).
Economic Evaluation
The methods and findings of the economic evaluation of MHBL interventions are described elsewhere (www.thecommunityguide.org/mentalhealth/RRbenefitslegis.html).
Evidence Synthesis
Study Characteristics
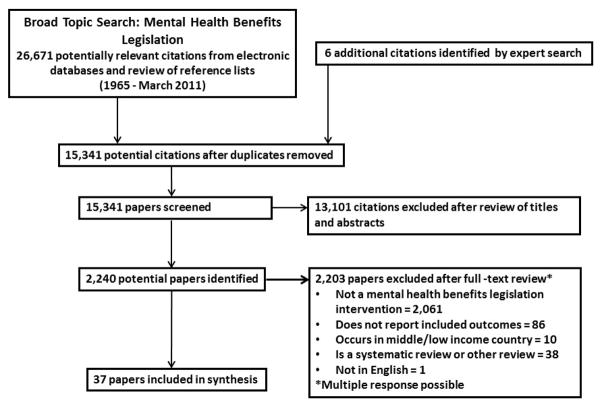
A total of 15,341 papers were identified from the literature search and screened by title and abstract (Figure 2). Further detailed review of full-text papers produced 30 quasi-experimental and observational studies from 37 papers that met inclusion criteria. Of these, 11 studies (reported in 16 papers12,24,38–51) were of greatest design suitability, nine (reported in ten papers20,35–37,52–55,56,57) were of moderate suitability, and ten (reported in 11 papers58–68) were least suitable. Twelve studies (reported in 18 papers20,24,37,41,43–47,49–52,55–57,61,62) were of good quality of execution and 18 (reported in 19 papers12,35,36,38–40,42,48,53,54,57–60,63–68) were fair. Twenty-eight studies (reported in 35 papers12,20,24,35–55,57–63,65–68) examined effects of state or federal MH/SA parity policies or legislation, and two56,64 examined effects of state-mandated coverage for MH and SA. Six studies35,37–40,42 examined effects of comprehensive parity legislation or policies. No studies evaluated the 2010 ACA. Most studies used a nationwide sample to examine effects of federal legislation or state mandates, and were conducted between 1990 and 2011.. Summary evidence tables that present further details of each study are provided at www.thecommunityguide.org/mentalhealth/SET-benefitslegis.pdf. No prior systematic reviews on the effectiveness of MHBL were found in the literature.
Figure 2.
Flow chart showing number of studies identified, reviewed in full text, excluded, and total number included.
Overall Results
Access to care
Seven studies in eight papers39,53,60,63–66,68 reported changes in access to care, and three studies in four papers60,63,64,68 (eight data points) reported percentage change of employees with coverage for MH/SA services. Median absolute pct pt increase for employees covered by MH/SA services was 13.6 (IQI= −3.8, 48.0). Four studies39,53,65,66 provided additional evidence. One of those65 reported that restrictions for MH/SA remained greater than restrictions for physical health services for 89% of plans after implementation of the 1996 MHPA. Another study66 reported the percentage of employers covering MH/SA benefits before and after MHPA implementation for specific services; overall results suggested no change in proportion of employers covering MH/SA benefits. Two studies39,53 found that more people with an MH need (including SA) perceived their access to MH/SA care to be easier after implementation of a state parity mandate, with increases of 8.1 and 3.3 pct pts (p>0.05), respectively.
Financial protection
Five studies in six papers assessed financial protection,36,44,47,51,52,67 and effectiveness was shown for all financial-protection outcomes. One study36 found the proportion of people reporting out-of-pocket spending of >$1,000 and people reporting a financial burden for children’s MH care in parity states was 7.1 and 9.4 pct pts less, respectively, than for people in non-parity states. Two studies with seven study arms52,67 reported that MHBL was associated with a median decline of 4.6 pct pts (IQI= −12.0, −4.0) in the percentage of overall out-of-pocket healthcare spending used to pay for MH services. Two studies reported in three papers44,47,51 found an overall decrease in MH out-of-pocket spending per user comparing those covered under FEHB versus those covered by self-insurance plans: one47 reported an annual median decline of $9 in adult-only plans (from baselines of $202–$257); similarly, another51 reported an annual median decline of $37 in child and adult plans (from baselines of $251–$418) and a subgroup analysis44 also reported an annual median decline of $51 in child-only plans (from baselines of $724–$1,131).
Appropriate utilization
Nine studies assessed appropriate utilization as an increase in the number of: (1) visits to MH specialists35,39,42,56; (2) evidence-based or guideline-concordant care visits24,40; or (3) MH visits for people with a MH need.12,35,38,39,46 In general, studies reported positive effect estimates following MHBL (specifically, state mandates, FEHB, or Medicare parity in cost sharing). Three studies35,39,42 reported greater MH specialist service use in those states with parity laws compared to those without (Table 1). Two studies24,40 reported increases in adoption of guideline-concordant care as a result of MH parity implementation (Table 2). Effects of MH parity on increasing service utilization among populations identified as having an MH need, reported in five studies,12,35,38,39,46 are shown in Table 3. All five studies reported increased service utilization among populations in need.
Table 1.
Results of Studies Evaluating Effect of Mental Health Parity Legislation on Utilization of Mental Health Specialists
| Author, year | Comparison | Population | Outcome | Conclusion |
|---|---|---|---|---|
| McGuire, 198256 | States with a mandate vs. states without a mandate | Adults with private insurance | Use of psychiatrists’ and psychologists’ services | ▲ |
| Pacula, 200035 | Parity states vs. non-parity states | Adults with private insurance | Number of specialty mental health visits | ▲ |
| Bao, 200439 | Strong parity states vs. weak parity states | Adults with private insurance | Number of specialty mental health visits | ▲ |
| Barry, 200542 | Parity states vs. non-parity states | Adults with private insurance | Number of specialty mental health visits (weighted mean) | ▲ |
▲ = favors parity; shape does not represent effect magnitude. All studies include adults aged ≥18 years with private insurance. See detailed data in Appendix Table D-1, available online.
Table 2.
Results of Studies Evaluating Effect of Mental Health Parity on Guideline-Concordant Care
| Author, year | Need indicator | Population | Outcome | Conclusion |
|---|---|---|---|---|
| Busch, 200624 | Diagnosis of major depressive disorder | Adults with private insurance | Receipt of any antidepressant and/or psychotherapy | ▲ |
| Duration of follow up (MH/SA visits and/or antidepressants) ≥4 months | ▲ | |||
| Intensity of follow-up (i.e. Any MH/SA visit) first 2 months, ≥ 2 per month | ○ | |||
| Intensity of follow-up (i.e. Any MH/SA visit) second 2 months, ≥1 per month | ○ | |||
| Trivedi, 200840 | Previous hospitalization for psychiatric disorder | Adults with public insurance | 7 day follow up for plans that continued full parity vs. plans that discontinued full parity (Adjusted* percentage point difference) | ▲ |
| 30 day follow up for plans that continued full parity vs. plans that discontinued full parity (Adjusted* percentage point difference) | ▲ |
Adjusted for sociodemographic and health plan characteristics, clustering by plan, and repeated measurements of enrollees.
▲ = favors parity; ○ = null. Shapes do not represent effect magnitude. See detailed data in Appendix Table D-2, available online.
Table 3.
Effects of Mental Health Parity on Increasing Service Utilization Among Populations With an Identified Mental Health Need
| Author, year | Need Indicator | Population | Outcome | Conclusion |
|---|---|---|---|---|
| Harris, 200612 | K6 Distress Scale >6a | Adults with employer-sponsored insurance | % Past year any MH service use | ▲ |
| Dave, 200938 | Privately referred | Adults with public or private insurance or uninsured | Substance abuse treatment admissions (DDD) | ▲ |
| Pacula, 200035 | MHI-5 <50b | Adults with private insurance | # MH specialty visits (OLS regression) | ▲ |
| Bao, 200439 | MHI-5 <50b | Adults with private insurance | # MH specialty visits (standard error) | ▲ |
| Busch, 200846 | MHI-5 <67b | Adults, employer-sponsored insurance | Any mental health service use (logistic regression) | ▲ |
▲ = favors parity; Shapes do not represent effect magnitude.
K6 Distress Scale, The Kessler 6 (a standardized and validated measure of nonspecific psychological distress). (Cited from www.cdc.gov/mentalhealth/data_stats/nspd.htm.)
MHI-5, Mental Health Inventory-5 (measures general psychological distress and well-being and used to assess mental health of consumers with a wide variety of conditions). (Cited from amhocn.org/static/files/assets/bae82f41/MHI_Manual.pdf.)
DDD, difference-in-difference-in-difference; MH, mental health; OLS, ordinary least squares See detailed data in Appendix Table D-3, available online.
Diagnosis of mental health conditions
One study in two papers20,24 reported relative increases of 13.0% in identification of major depressive disorders and 25.6% in SA disorders, and absolute increases of 0.3 pct pts (p<0.05) and 0.1 pct pts, respectively, following implementation of the FEHB parity policy.
Morbidity
One study46 assessed the effect of state parity mandates on MH-related morbidity. In five states that enacted state parity mandates during the study period, there was a 3.2-pct pt decrease in the prevalence of people reporting poor MH. Similarly, the prevalence of people reporting poor MH was 2.8 pct pts lower in states that had state mandated parity for the entire study period than for those without.
Mortality
Two studies37,41 reported evidence on reduced suicide rate using national data from the same source. Klick and Markowitz37 conducted a two-stage least squares regression, controlling for state-level variables, and reported regression coefficients of −0.145 for partial parity versus −0.212 for full parity states, indicating a reduced suicide rate. However, neither of these results was significant (p>0.05). In a similar study using updated classification of state parity status, Lang41 found, among states that enacted parity mandates, the suicide rate per 100,000 decreased significantly by a relative 5% (p<0.01) compared with states that enacted no or weak parity mandates.
Quality of care and quality of life
In this review, no independent measures of quality of care or quality of life were reported.
Subgroup analyses
Overall, six studies35,37–40,42 examined the impact of strength and scope of legislation on the outcomes of utilization, appropriate utilization, and suicide rates (Table 4). The first group of studies had an indirect comparison of the effectiveness of comprehensive parity versus no/weak parity to the effectiveness of all types of parity versus no/weak parity (the categories of parity are not mutually exclusive; Table 4, top). The second set of studies (Table 4, bottom) had an indirect comparison of comprehensive parity to more limited forms of parity (i.e., weaker parity); these categories are mutually exclusive.
Table 4.
Results of Studies Evaluating Strength and Scope of Parity Legislation
| Comparative effectiveness of more comprehensive parity to all paritya | ||||
|---|---|---|---|---|
| Author, year | Population | Comparative effectiveness | Outcome | Conclusion |
| Pacula, 200035 | Adults with private insurance | Strict parity to all parity | No. of MH visits for general population (no differences) | ○ |
| No. of MH visits among those with MH need (MHI-5<50) | ▲ | |||
| Barry, 200542 | Adults with private insurance | Full parity to all parity | Mean % of MH/SA users | ○ |
| Mean % of specialty MH users | ○ | |||
| Mean number of specialty visits | ○ | |||
| Klick, 200637 | Adults with private or public insurance | Full parity to all parity | Adult suicide rate | ▲ |
| Comparative effectiveness of more comprehensive parity to more limited parityb | ||||
|---|---|---|---|---|
| Author, year | Population | Comparative effectiveness | Outcome | Conclusion |
| Dave, 200938 | Adults with public or private insurance, and adults without insurancec | Broad parity to limited parity | Total SA treatment admissions | ▲ |
| Bao, 200439 | Adults with private insurance | Strong parity to no/weak parity | Number of MH specialty visits | ▲ |
| Medium parity to no/weak parity | ||||
| Trivedi, 200840 | Adults with public insurance | Full parity versus intermediate parity | % received follow-up in 7 days | ▲ |
| % received follow-up in 30 days | ▲ | |||
▲ = differential effects favors comprehensive parity; ○ = no differential effects; shapes do not represent effect magnitude.
See detailed data in Appendix Table D-4, available online.
More comprehensive parity versus the reference group (no/weak parity) is indirectly compared to all parity vs. the reference group (weak/no parity). These groups are not mutually exclusive.
Mutually exclusive groups of more comprehensive parity are compared to more limited forms of parity (reference group in each comparison: no/weak parity).
Uninsured population not covered by parity legislation.
MH, mental health; MHI-5, Mental Health Inventory-5; SA, substance abuse
Additional evidence on utilization
Sixteen studies in 18 papers12,20,38,39,43,44,46–52,54,56,59,61,62,67 reported utilization of MH or SA services but did not provide sufficient information to meet the criteria for appropriate utilization. Results were mixed (see Appendix D, available online, for more details).
Applicability
All studies were conducted in the U.S., among people who were covered by private or public insurance. Analysis by age36,44 indicated that effects for financial protection were similar for children and adults. Analysis by region43,44,60,64,68 and employer size46,52,60,65,66 showed no difference in access to care. No studies reported outcomes by health plan type or racial/ethnic minority groups; however, the body of evidence includes national samples that should be representative of all health plan types and racial/ethnic groups.
One study40 reported evidence on effectiveness in low-SES populations for appropriate utilization among Medicare enrollees aged ≥65 years; MH benefit changes were most effective for people in the lowest income and education groups (p<0.05). Another study46 found that employees working for small employers (<100 employees) were more likely to use MH services after implementation of state parity mandates, regardless of income, and state parity mandates were most effective in increasing utilization of any MH service for people in the lowest income group (p<0.05). In summary, the body of evidence is applicable to the insured population across the U.S., with some evidence for specific outcomes on children, low-income and low-education groups, and employees of small employers. MHBL does not apply to the uninsured population.
Additional Benefits and Harms
One study56 in this review suggested that increased MH service use after implementation of MHBL might have an additional benefit of decreasing utilization of social or other health services, because of the association between mental and physical health.56,69 These authors56 and others70,71 have speculated that insurance coverage–related discrimination for MH could decrease as a result of legislation because insurance providers would no longer be able to refuse coverage for these conditions.
Two potential harms of MHBL described earlier are moral hazard and adverse selection. No studies in this review provided evidence on moral hazard. However, increased adverse selection was found in one study61 following implementation of a state parity law, but only in a subgroup that allowed beneficiaries to choose among health plans.
Some researchers have suggested that employers may drop MH/SA coverage to avoid being subject to MHBL.72,73 A national study conducted in 201073 found that although 5% of employers dropped MH/SA coverage that year, only 2% reported dropping coverage after passage of the 2008 MHPAEA. The U.S. General Accounting Office 2011 Mental Health and Substance Abuse Report72 found similar results, showing that approximately 2% of employers discontinued coverage in 2010 of either: (1) MH and substance use; or (2) only substance use disorders. Current provisions of the 2010 ACA will require state Medicaid programs and insurance plans in state health insurance exchanges to cover both MH and SA as one of ten categories of essential health benefits in 2014.74,75
Considerations for Implementation
Challenges to effective implementation of MHBL include underutilization, access to services, and exemptions. This legislation alone is not sufficient to address underutilization of MH/SA services in the U.S.10 Additionally, it is unclear to what extent MHBL reduces public stigma, a barrier to utilization of MH/SA services.76–78 Low awareness of legislative provisions also may hinder service utilization by beneficiaries.79
Conversely, limited numbers of MH providers80 and inpatient beds81 restrict access to services, especially in rural areas.81 In some cases, covered services and treatments are not clearly defined in the legislation, allowing individual health plans to limit benefits provided for certain conditions or illnesses.82 Further, investigational treatments typically are not covered by insurance plans, thus limiting access to care.82
Another implementation issue concerns exemptions that may decrease the potential reach of MHBL. Larger employers often self-insure, and are therefore exempt from MH insurance–related state mandate laws because of the 1974 Employee Retirement Income Security Act (ERISA).83 Both employers with <50 employees and group health plans that demonstrate an MH benefit–related cost increase of 1% (MHPA) and 2% (MHPAEA) are exempt from the respective federal legislation.16
Conclusions
Summary of Findings
Results of this review suggest that MHBL has favorable effects on financial protection and access to care. Evidence on increasing appropriate utilization of MH services and certain evidence on aspects of MH care (e.g., increased diagnosis of mental illness) is also favorable, with larger effects for comprehensive parity legislation. In addition, MHBL, and specifically comprehensive parity, is associated with favorable effects for health-related outcomes of reducing suicides and morbidity, although the small number of studies limits inferences.
Discussion
MHBL creates levels of financial protection and access to care that are no more restrictive for certain insured individuals seeking MH/SA services than for those seeking services for physical health conditions.26 Nonetheless, accurately interpreting these results requires consideration of two caveats:
Simultaneous implementation of MHBL and adoption of managed care have made isolating the effects of MHBL difficult. Overall, the interrelationship between managed care and MHBL is unclear; managed care might reduce moral hazard and ensure appropriateness of services rendered following improved financial protection84 or it might restrict access to services through excessive or inappropriate use of management tools.56 Further, some parity legislation applies only to managed care insurance plans, or explicitly authorizes and encourages the use of managed care.84
Of 37 included papers, 35 examined effects of state, federal, or executive-ordered MH/SA parity, whereas the remaining two papers56,64 investigated effects of mandating coverage for MH and SA for only the outcomes of access and utilization. Therefore, effects on most outcomes can be associated with some level of parity legislation.
The 2010 ACA affects MH/SA parity in two critical ways. First, the ACA extends the reach of the two previous federal parity laws to certain types of health plans not previously required to comply.17,74 Second, ACA contains provisions mandating that: (1) MH and SA services in general are covered by certain health insurance issuers; and (2) specific MH and SA disorder services are covered by specified plan types (i.e., qualified health plans, certain Medicaid plans, and plans offered through the individual market).17,74 Combined, these two new provisions extend the requirements and reach of MH/SA parity.
Limitations
A number of challenges in studying the effects of MHBL were limitations in the current review but do not threaten validity of findings substantially. First, there was difficulty isolating the effects of managed care from those of MHBL. Second, many studies did not report sufficient information to assess appropriate utilization. Third, there is potential for data dependency (i.e., same people or populations represented more than once in the body of evidence). Some studies in this review used the same national data sources, such as the Healthcare for Communities survey85 or MarketScan database,86 but the extent of overlap is unclear. Fourth, data sources might introduce bias either through survey data, which are based on self-reporting and potentially subject to recall bias or claims data, which might lead to spuriously low results for MH/SA service use because of under-reported diagnoses and underutilization of treatment.45 Fifth, classifications of strength of state parity mandates differed across studies. Although many authors relied on the National Conference of State Legislatures,17 others used alternative sources or their own classification. Sixth, few studies of private employer plans controlled for exemptions, such as the 1974 ERISA, which exempts self-insured employers (typically large employers with >500 employees) from state mandates.83 Additionally, no studies controlled for the small employer exemption (≤50 employees) or cost exemption (1%–2% cost increase following parity implementation) of the two federal laws.16 Failure to control for these exemptions could lead to underestimates of MHBL effects.
Evidence Gaps
Research evaluating effects of MHBL on MH outcomes is limited. Studies are needed to assess effects of legislation on morbidity (e.g., symptom reduction remission and recovery), mortality, quality of life, and aspects of quality of care (e.g. intensity and duration of treatment, and coordination of care). Most studies that reported utilization did not assess appropriateness of use as indicated by guideline-concordant care or patient need. In addition, researchers often reported outcomes that combined inpatient and outpatient utilization, but the desired direction (i.e., increase or decrease) differed with various patient conditions. Reporting types of utilization separately and including measures of appropriate utilization will allow for assessments of appropriate care.
Research is also needed to clarify the role of MHBL in reducing health-related disparities and improving MH outcomes among subgroups (e.g., low-SES groups, racial/ethnic minorities, and various MH conditions) that may experience greater issues with access to care and impairments. Moreover, evidence is limited for people covered by public health insurance (e.g., Medicaid and Medicare). Further, evaluations are needed to examine effects of the 2008 MHPAEA, which contains more requirements for parity than the 1996 MHPA and the 2010 ACA, which currently has provisions to establish parity for MH/SA in many insurance plans in 2014.74 Finally, studies that include a longer follow-up (>3 years) are necessary to assess long-term effects of MHBL.
Acknowledgments
The authors would like to acknowledge Kate W. Harris for the thorough editing of this paper and advice given during the revision process; Cristian Dumitru for contributing in multiple phases of this project; Gail Bang and Onnalee Gomez for conducting the literature searches; Sierra Baker, Guthrie Byard, Su Su, and Elena Watzke for their work as fellows at the beginning of this project; and Farifteh F. Duffy, Jane Pearson, and Samantha Williams for their work as Mental Health Coordination Team members.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of CDC or the National Institute of Mental Health.
The work of Ramona K.C. Finnie, John A. Knopf, Shuli Qu, Jeffrey A. Reynolds, Cristian Dumitru, Sierra Baker, Guthrie Byard, Su Su, and Elena Watzke was supported with funds from the Oak Ridge Institute for Scientific Education (ORISE).
Appendix A: Affordable Care Act
PART I—ESTABLISHMENT OF QUALIFIED HEALTH PLANS
SEC. 1301. QUALIFIED HEALTH PLAN DEFINED
(a) Qualified Health Plan.—In this title: (1) In general.—The term “qualified health plan” means a health plan that—(A) has in effect a certification (which may include a seal or other indication of approval) that such plan meets the criteria for certification described in section 1311(c) issued or recognized by each Exchange through which such plan is offered; (B) provides the essential health benefits package described in section 1302(a); and (C) is offered by a health insurance issuer that— (i) is licensed and in good standing to offer health insurance coverage in each State in which such issuer offers health insurance coverage under this title (ii) agrees to offer at least one qualified health plan in the silver level and at least one plan in the gold level in each such Exchange; (iii) agrees to charge the same premium rate for each qualified health plan of the issuer without regard to whether the plan is offered through an Exchange or whether the plan is offered directly from the issuer or through an agent; and (iv) complies with the regulations developed by the Secretary under section 1311(d) and such other requirements as an applicable Exchange may establish.
(Source: Patient Protection and Affordable Care Act (H.R. 3590) Public Law 111-148; 2009. pp. 44–45)
Appendix B: Mental Health Outcome Definitions and Examples
Access to care
The ability of those with public or private insurance to obtain MH/SA care. Examples include workforce coverage for mental health/substance abuse (MH/SA) benefits and insured’s perception of that coverage.
Financial protection
The reduction in out-of-pocket costs paid by an individual for MH/SA services.1,2 Examples include measures of decreased financial burden, dollar amount, and percentage of out-of-pocket spending.
Appropriate utilization
Receiving the proper amount and quality of services when needed, including utilization of MH/SA services by people with a MH/SA need, services rendered by MH specialists (e.g., psychiatrist, psychologist, social worker), or receipt of services conforming to evidence-based guidelines for MH/SA care.
Diagnosis
The determination that a person meets established criteria for a MH condition. Examples include recognition of newly identified mental health–related conditions, such as depression or substance abuse.
Quality of care
“The degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge.” Examples include; appropriateness of treatment; type, intensity, and duration of treatment; patient satisfaction; and coordination of care.3
Morbidity
The presence of any type of MH condition. Examples include measures of MH status; reduced morbidity includes reduction in symptoms as measured by standardized and validated instruments such as Mental Health Inventory Scale (MHI-5; amhocn.org/static/files/assets/bae82f41/MHI_Manual.pdf), Kessler 6 distress scale (K6; www.cdc.gov/mentalhealth/data_stats/nspd.htm), increased remission, increased recovery, and decreased relapse. In this review, the team accepted cutoff scores used by primary study authors.
Mortality
Any death associated with a MH condition Examples include suicides, deaths related to eating disorders, and alcohol and drug (i.e., substance) abuse.
Quality of life
Health-related quality of life, “an individual’s or group’s perceived physical and mental health over time.”4 Outcome measures that report health-related quality of life include the Medical Outcomes Study Short Forms 125 and 36,6 the Sickness Impact Profile,7 and Quality of Life Index for Mental Health.8
Appendix C: Data Abstraction and Synthesis
Abstraction and Evaluation of Studies
Two reviewers read and evaluated each study that met inclusion criteria using an adaptation of a standardized abstraction form (www.thecommunityguide.org/methods/abstractionform.pdf)9 that included data describing elements of mental health benefits legislation, population characteristics, study characteristics, study results, applicability, potential harms, additional benefits, and considerations for implementation. Assessment of study quality included study design and execution, which were evaluated using these criteria: studies with greatest design suitability were those with prospective data on exposed/comparison populations; studies with moderate design suitability were those with retrospective data on exposed/comparison populations or with data collected at multiple pre and post-intervention time points; studies with least-suitable designs were cross-sectional studies with no comparison population (including one-group single pre- and post-measurement). Studies were assigned limitations for quality of study execution based on seven categories of threats to validity identified in studies, up to a total of nine limitations across six categories: (1) description of study population and intervention to include at least year of intervention, study location and population characteristics (one limitation); (2) sampling to include representation, selection bias, and appropriate control group (one limitation); (3) measurement of exposure to include reliability of outcome and exposure variables (two limitations); (4) data analysis to include appropriate statistical tests and controls (e.g., time, intensity, secular trends, plan types, condition of patient, etc.) and adjustment for multi-year data (one limitation); (5) interpretation of results/sources of potential bias to include attrition < 80%, comparability of comparison group, recall bias for surveys, accounting for overlapping laws and adequate controls for confounding (three limitations), and (6) other issues such as missing data (one limitation). Study quality of execution was characterized as good (0–1 limitation), fair (2–4 limitations), or limited (≥5 limitations). Studies with good or fair quality of execution and any level of design suitability were included in the analyses. Papers based on the same study dataset were linked; only the paper with the most complete data (e.g., longest follow-up) for each outcome was included in each analysis.
Studies were stratified by five subgroups when data were available: strength and scope of legislation, setting, clients, employer size, and health plan type.
Effect Measurement and Formulas
Effect estimates for absolute percentage point change and relative percentage change were calculated using the following formulas:
For studies with pre- and post-measurements and concurrent comparison groups:
where:
Ipost = last reported outcome rate or count in the intervention group after the intervention;
Ipre = reported outcome rate or count in the intervention group before the intervention;
Cpost = last reported outcome rate or count in the comparison group after the intervention;
Cpre = reported outcome rate or count in the comparison group before the intervention.
Effect estimates for studies with pre- and post-measurements but no concurrent comparison:
Outcome data were reported as proportions when possible and were converted to effect estimates of absolute percentage point change or relative percent change.
Summarizing and Synthesizing the Body of Evidence on Effectiveness
The rules of evidence under which the Community Preventive Services Task Force makes its determination address several aspects of the body of evidence, including the number of studies of different levels of design suitability and execution, consistency of the findings among studies, public health importance of the overall effect estimate, and balance of benefits and harms of the intervention.9–11
Appendix D: Detailed Tables of Results and Additional Evidence
Table D-1.
Results of Studies Evaluating the Effect of Mental Health Parity Legislation on Utilization of Specialty Mental Health Provider Services
| Author, year | Comparison | Outcome | Effect estimate | Direction |
|---|---|---|---|---|
| McGuire, 198212 | States with a mandate vs. states without a mandate | Use of psychiatrists’ services | Absolute pct pt change: 9.2 | Favorable |
| Use of psychologists’ services | Absolute pct pt change: 18.0 | |||
| Pacula, 200013 | Parity states vs. non-parity states | Number of specialty MH visits | Ordinary least squares regression coefficient: 0.827, p<0.01 | Favorable |
| Bao, 200414 | Strong parity states vs. weak parity states | Number of specialty MH visits | Difference-in-Difference-in Difference (DDD): 8.9, SE=4.9, p<0.10 | Favorable |
| Barry, 200515 | Parity states vs. non-parity states | Number of specialty MH visits | Difference-in-means (weighted means): 4.71, p<0.001 | Favorable |
Note: All studies include adults aged ≥ 18 years with private insurance.
MH, mental health; pct pt, percentage point
Table D-2.
Results of Studies Evaluating the Effect of Mental Health Parity on Guideline-Concordant Care
| Author, year | Need indicator | Comparison | Outcome | Effect estimate | Direction |
|---|---|---|---|---|---|
| Busch, 200616 | Diagnosis of Major Depressive Disorder | Post-FEHB vs. pre-FEHB | Receipt of any antidepressant and/or psychotherapy | OR=1.26 95% CI= 1.18, 1.34; p<0.0001 |
Favorable |
| Duration of follow-up (MH/SA visits and/or antidepressants) ≥ 4 months | OR=1.37 95% CI= 1.20, 1.56; p<0.0001 |
Favorable | |||
| Intensity of follow-up (i.e., any MH/SA visit) first 2 months, ≥ 2 per month | OR=1.09 95% CI= 0.95, 1.25; p>0.05 |
Null | |||
| Intensity of follow-up (i.e., any MH/SA visit) second 2 months, ≥ 1 per month | OR=1.05 95% CI= 0.92, 1.20; p>0.05 |
Null | |||
| Trivedi, 200817 | Previous hospitalization for psychiatric disorder | Full parity Medicare plans vs. discontinued parity Medicare plans | 7-day follow-up (Adjusteda percentage point difference) | Percentage point difference=19.0 95% CI= 6.6, 31.3; p=0.003 |
Favorable |
| 30-day follow-up (Adjusteda percentage point difference) | Percentage point difference=14.2 95% CI= 4.5, 23.9; p=0.007 |
Favorable |
Adjusted for socio-demographic and health plan characteristics, clustering by plan, and repeated measurements of enrollees; both studies include adults aged ≥ 18 years.
FEHB, Federal Employees Health Benefits Program; MH, mental health; SA, substance abuse
Table D-3.
Results of Studies Evaluating the Effect of Mental Health Parity on Increasing Service Utilization Among Populations With an Identified Mental Health Need
| Author, year | Need Indicator | Comparison | Outcome | Effect Estimate | Direction |
|---|---|---|---|---|---|
| Harris, 200618 | K6 Distress Scale >6 | Parity states vs. weak/non-parity states | % any MH service use in past year | Absolute percentage point change=0.99 | Favorable |
| Dave, 200919 | Privately referred | Parity states vs. weak parity states | Substance abuse treatment admissions | Privately referred: DDD coeff=0.207, p<0.01 Total population: DDD coeff=0.128, p<0.05 |
Favorable |
| Pacula, 200013 | MHI-5 <50 | Parity states vs. non-parity states | Number of MH specialty visits | OLS coeff=0.827 p<0.01 | Favorable |
| Bao, 200414 | MHI-5 <50 | Parity states vs. weak/non-parity states | Number of MH specialty visits | Absolute difference=2.4 | Favorable |
| Busch, 200820 | MHI-5 <67 | Parity states vs. non-parity states | Any MH service use | Parity: OR=1.032; SE=0.071 Parity*MHI-5<67: OR=1.212; SE=0.207 |
Favorable |
Notes:
All studies include adults ≥ 18 years of age with private or public insurance.
K6 Distress Scale: The Kessler 6 (K6) is a standardized and validated measure of nonspecific psychological distress.
Coeff, Coefficient; DDD, Difference-in-difference-in-difference; MH, mental health; MHI-5, Mental Health Inventory-5; OLS, ordinary least squares regression
Table D-4: Detailed Description
Subgroup analyses on strength and scope of legislation
Overall, six studies13–15,17,19,21 examined the impact of strength and scope of legislation on the outcomes of utilization, appropriate utilization, and suicide rates. The first group of studies had an indirect comparison of the effectiveness of comprehensive parity versus no/weak parity to the effectiveness of all types of parity versus no/weak parity (these categories of parity are not mutually exclusive; Table D-4, top). Pacula and Sturm13 found differential effects for MH service visits among those identified with an MH need when analyzing comparisons of states with a strict parity mandate and states with all levels of parity (reference group: non-parity states). There were no such differences for the general population. Barry15 found no differential effects for more visits for MH specialty visits in full parity states comparisons than all levels of parity comparisons (reference group: no/weak parity states). There were no differential effects for outcomes of proportion of mental health/substance abuse (MH/SA) users and specialty users. Klick and Markowitz21 found differential effects for greater reductions in adult suicide rates in states with full parity compared to states with more loosely defined parity mandates.
The second set of studies (Table D-4, bottom) had an indirect comparison of comprehensive parity to more limited forms of parity (i.e., weaker parity); these categories are mutually exclusive. Dave and Mukerjee19 reported a greater effect for broad parity legislation on increasing SA treatment admissions, compared to limited parity legislation (reference group: weak/no parity states). Bao and Sturm14 reported a greater increase in the number of MH visits in states with strong parity mandates compared to states with medium parity mandates (reference group: weak/no parity). Trivedi and colleagues17 reported a larger improvement in follow-up (appropriate utilization) of previously hospitalized psychiatric patients, comparing those with a full parity Medicare plan to those with an intermediate parity Medicare plan.
Table D-4.
Results of Studies Evaluating Strength and Scope of Parity Legislation
| Comparative effectiveness of more comprehensive parity to all parity | |||||
|---|---|---|---|---|---|
| Study (Years) | Population | Analysis: Outcome(s) | Comparative effectivenessa,b | Results | Direction |
| Pacula 200013 (1997 / 1998) | Adults with private insurance |
|
Strict parity vs. Non-parity |
|
Null |
| Parity vs. Non-parity |
|
Favorable | |||
| Barry 200515 (2001) | Adults with private insurance |
|
Full parity vs. Non-parity |
|
Mixed |
| Parity vs. Non- parity |
|
Mixed | |||
| Klick 200621 (1981–2000) | Adults with private or public insurance |
|
Full Parity vs. No/weak parity |
|
Favorable |
| Parity vs. No/weak parity |
|
Favorable | |||
| Comparative effectiveness of more comprehensive parity versus more limited parity | |||||
| Study (Years) | Population | Analysis: Outcome(s) | Comparative effectivenessa,b | Results | Direction |
| Dave 200919 (1992–2007) | Adults with private or public insurance, or uninsuredc |
|
Broad vs. Non- parity |
|
Favorable |
| Limited vs. non-parity |
|
Favorable | |||
| Bao 200414 (1998, 2000/ 2001) | Adults with private insurance |
|
Strong vs. No/weak parity |
|
Favorable |
| Medium vs. no/weak parity |
|
Favorable | |||
| Trivedi 200817 (2002–2006) | Adults with public insurance |
|
Full vs. non- parity |
|
Favorable |
| Intermediate vs. non-parity |
|
Favorable | |||
To assess effectiveness of more comprehensive legislation relative to more limited legislation, the results for the top box should be compared to those in the bottom box for the corresponding study.
- Broad parity: coverage of a broad range of mental conditions
- Full parity: insurers must provide mental health benefits at exactly the same terms applying to physical health benefits
- Intermediate parity: mental health care greater than primary care cost sharing but less than or equal to specialist cost sharing
- Limited parity: mental health benefits that apply to certain groups only e.g., those with severe biologically based mental illness, require parity for certain diagnoses (mandated offering), or require parity only if the plan already offers any type of mental health service (mandated if offered)
- Medium parity: allow exemptions for small employers and employers that experience cost increase due to the law, may contain “if offered” provisions
- No parity: no parity law or passed legislation matching the federal MHPA
- Strict parity: laws that are more generous than the federal legislation
- Strong parity: require equality in all cost-sharing and no exemptions
- Weak parity: mandated offering
Uninsured not covered by parity legislation.
MH, mental health
Additional Evidence
Sixteen studies in 18 papers12,14,18–20,22–34 reported utilization of MH or SA services but did not provide sufficient information to meet the criteria for appropriate utilization. Results were mixed, with eight studies14,18–20,24,27,33,35 indicating that implementation of MHBL was associated with increased utilization of any type of MH care, and three studies22,23,29 reporting decreased utilization after implementation of either state mandates or FEHB (median 0.6 pct pts; IQI= −0.34, 1.83; 10 studies, 11 papers). Outpatient visits per 100 members per year increased by a median of 5.4 following implementation of state parity mandates (IQI= −3.37, 34.77; 13 data points, 4 studies26,31,33,36); three additional studies18,25,34 that used different metrics for outpatient utilization had mixed results. Inpatient days per 1,000 members per year tended to decrease by a median of 13.47 following implementation of state parity mandates (IQI= −74.05, −3.24; 9 data points, 4 studies26,31,33,36); one additional study30 found a minimal decrease of 0.3 pct pts in MH/SA inpatient use.
Although not included in this review, there is also some evidence of favorable effects when employers voluntarily expanded MH/SA benefits to achieve parity. One study37 reported that a reduction in copayments resulted in increased utilization of substance use services. Two studies38,39 reported the combination of de-stigmatization and lower copayments was associated with a significant increase in the probability of initiating MH treatment by 1.2% and 0.74%, respectively (p<0.01 for each). And one study40 reported that benefit changes and de-stigmatization increased the likelihood of outpatient, pharmaceutical, or any MH treatment among intervention employers compared to control employers.
Appendix References
- 1.Wagstaff A. Measuring financial protection in health. The World Bank; 2008. http://dx.doi.org/10.1596/1813-9450-4554. [Google Scholar]
- 2.Moreno-Serra R, Millett C, Smith P. Towards improved measurement of financial protection in health. PLOS Med. 2011;8(9):e10001087. doi: 10.1371/journal.pmed.1001087. http://dx.doi.org/10.1371/journal.pmed.1001087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.IOM, Committee on Quality of Health Care in America. Crossing the quality chasm: A new health sytem for the 21st century. Washington, DC: National Academy Press; 2001. [Google Scholar]
- 4.Agency for Healthcare Research and Quality. Total Expenditure Panel Survey Household Component Data. 2011 meps.ahrq.gov/data_stats/quick_tables_search.jsp?component=1&subcomponent=0.
- 5.Ware J, Kosinski M, Keller S. A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. http://dx.doi.org/10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 6.McHorney C, Ware JJ, Lu J, et al. The MOS 36-item Short Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994;32:40–66. doi: 10.1097/00005650-199401000-00004. http://dx.doi.org/10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Bergner M, Bobbit R, Kressel S, Pollard W, et al. The Sickness Impact Profile. conceptual formulation and methodology for the development of a health status measure. Int J Health Services. 1976;6(3):393–415. doi: 10.2190/RHE0-GGH4-410W-LA17. http://dx.doi.org/10.2190/RHE0-GGH4-410W-LA17. [DOI] [PubMed] [Google Scholar]
- 8.Becker M, Diamond R, Sainfort F. A new patient focused index for measuring quality of life in persons with severe and persistent mental illness. Qual Life Res. 1993;2(4):239–251. doi: 10.1007/BF00434796. http://dx.doi.org/10.1007/BF00434796. [DOI] [PubMed] [Google Scholar]
- 9.Zaza S, Wright-de Aguero L, Briss P, et al. Data collection instrument and procedure for systematic reviews in the Guide to Community Preventive Services. Am J Prev Med. 2000;18(1S):44–74. doi: 10.1016/s0749-3797(99)00122-1. http://dx.doi.org/10.1016/S0749-3797(99)00122-1. [DOI] [PubMed] [Google Scholar]
- 10.Briss PA, Zaza S, Pappaioanou M, et al. Developing an evidence-based Guide to Community Preventive Services--methods. Am J Prev Med. 2000;18(1S):35–43. doi: 10.1016/s0749-3797(99)00119-1. http://dx.doi.org/10.1016/S0749-3797(99)00119-1. [DOI] [PubMed] [Google Scholar]
- 11.Sipe T, Chin H, Elder R, et al. Methods for conducting Community Guide systematic reviews of evidence on effectiveness and economic efficiency of group-based behavioral interventions to prevent adolescent pregnancy, HIV, and other sexually transmitted infections: Comprehensive risk reduction and abstinence education. Am J Prev Med. 2012;42(3):295–303. doi: 10.1016/j.amepre.2011.11.002. http://dx.doi.org/10.1016/j.amepre.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 12.McGuire TG, Montgomery JT. Mandated mental health benefits in private health insurance. J Health Polit Polic. 1982;7(2):380–406. doi: 10.1215/03616878-7-2-380. http://dx.doi.org/10.1215/03616878-7-2-380. [DOI] [PubMed] [Google Scholar]
- 13.Pacula RL, Sturm R. Mental health parity legislation: much ado about nothing? Health Services Research. 2000;(1 Pt 2):263–275. [PMC free article] [PubMed] [Google Scholar]
- 14.Bao Y, Sturm R. The effects of state mental health parity legislation on perceived quality of insurance coverage, perceived access to care, and use of mental health specialty care. Health Serv Res. 2004;(5):1361–1377. doi: 10.1111/j.1475-6773.2004.00294.x. http://dx.doi.org/10.1111/j.1475-6773.2004.00294.x. [DOI] [PMC free article] [PubMed]
- 15.Barry CL. Thesis. Harvard University; 2005. The political economy of mental health parity. [Google Scholar]
- 16.Busch AB, Huskamp HA, Normand SLT, Young AS, Goldman H, Frank RG. The impact of parity on major depression treatment quality in the Federal Employees’ Health Benefits Program after parity implementation. Med Care. 2006;(6):506–512. doi: 10.1097/01.mlr.0000215890.30756.b2. http://dx.doi.org/10.1097/01.mlr.0000215890.30756.b2. [DOI] [PMC free article] [PubMed]
- 17.Trivedi AN, Swaminathan S, Mor V. Insurance parity and the use of outpatient mental health care following a psychiatric hospitalization. JAMA. 2008;300(24):2879–2885. doi: 10.1001/jama.2008.888. http://dx.doi.org/10.1001/jama.2008.888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harris KM, Carpenter C, Bao Y. The effects of state parity laws on the use of mental health care. Med Care. 2006;44(6):499–505. doi: 10.1097/01.mlr.0000215813.16211.00. http://dx.doi.org/10.1097/01.mlr.0000215813.16211.00. [DOI] [PubMed] [Google Scholar]
- 19.Dave DP, Mukerjee SP. Mental health parity legislation, cost-sharing and substance-abuse treatment admissions. Health Econ. 2009;20(2):161–183. doi: 10.1002/hec.1577. http://dx.doi.org/10.1002/hec.1577. [DOI] [PubMed] [Google Scholar]
- 20.Busch SH, Barry CL. New evidence on the effects of state mental health mandates. Inquiry. 2008;45(3):308–322. doi: 10.5034/inquiryjrnl_45.03.308. http://dx.doi.org/10.5034/inquiryjrnl_45.03.308. [DOI] [PubMed] [Google Scholar]
- 21.Klick J, Markowitz S. Are mental health insurance mandates effective? Evidence from suicides. Health Econ. 2006;(1):83–97. doi: 10.1002/hec.1023. http://dx.doi.org/10.1002/hec.1023. [DOI] [PubMed]
- 22.An R, Sturm R. Self-reported unmet need for mental health care after California’s parity legislation. Psychiatric Serv. 2010;61(9):861–862. doi: 10.1176/appi.ps.61.9.861. http://dx.doi.org/10.1176/ps.2010.61.9.861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Azrin ST, Huskamp HA, Azzone V, et al. Impact of full mental health and substance abuse parity for children in the Federal Employees Health Benefits Program. Pediatrics. 2007;119(2):e452–459. doi: 10.1542/peds.2006-0673. http://dx.doi.org/10.1542/peds.2006-0673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Azzone V, Frank RG, Normand SLT, Burnam MA. Effect of insurance parity on substance abuse treatment. Psychiatric Serv. 2011;62(2):129–134. doi: 10.1176/appi.ps.62.2.129. http://dx.doi.org/10.1176/ps.62.2.pss6202_0129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barry CL, Busch SH. Caring for children with mental disorders: do state parity laws increase access to treatment? J Ment Health Policy Econ. 2008;11(2):57–66. [PubMed] [Google Scholar]
- 26.Branstrom RB, Sturm R. An early case study of the effects of California’s mental health parity legislation. Psychiatric Serv. 2002;53(10):1215–1216. doi: 10.1176/appi.ps.53.10.1215. http://dx.doi.org/10.1176/appi.ps.53.10.1215. [DOI] [PubMed] [Google Scholar]
- 27.Branstrom RB, Cuffel B. Economic grand rounds: policy implications of adverse selection in a preferred-provider organization carve-out after parity. Psychiatric Serv. 2004;55(4):357–359. doi: 10.1176/appi.ps.55.4.357. http://dx.doi.org/10.1176/appi.ps.55.4.357. [DOI] [PubMed] [Google Scholar]
- 28.Ciemens EL. Thesis. University of California; Berkley: 2003. The effect of mental health parity on children’s mental health and substance abuse service utilization in Massachusetts. [Google Scholar]
- 29.McConnell J, Gast S, Ridgely S, et al. Behavioral health insurance parity: Does Oregon’s experience presage the national experience with the mental health parity and addiction. Am J Psychiatry. 2011;169(1):31–38. doi: 10.1176/appi.ajp.2011.11020320. http://dx.doi.org/10.1176/appi.ajp.2011.11020320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Parity Evaluation Research Team, for DHHS, Assistant Secretary for Planning and Evaluation. Evaluation of parity in the Federal Employees Health Benefits (FEHB) Program: Final Report. 2004 aspe.hhs.gov/daltcp/reports/parity.htm.
- 31.Rosenbach M, Lake T, Young C, et al. Effects of the Vermont Mental Health and Substance Abuse Parity Law. Rockville, MD: Center for Mental Health Services, Substance Abuse & Mental Health Services Administration; 2003. DHHS Pub. No. (SMA) 03-3822. [Google Scholar]
- 32.Sturm R, McCulloch J. Mental health and substance abuse benefits in carve-out plans and the Mental Health Parity Act of 1996. J Health Care Finance. 1998;(3):82–92. [PubMed] [Google Scholar]
- 33.Zuvekas SH, Regier DA, Rae DS, Rupp A, Narrow WE. The impacts of mental health parity and managed care in one large employer group. Health Affairs. 2002;21(3):148. doi: 10.1377/hlthaff.21.3.148. http://dx.doi.org/10.1377/hlthaff.21.3.148. [DOI] [PubMed] [Google Scholar]
- 34.Zuvekas SH, Meyerhoefer CD. Coverage for mental health treatment: do the gaps still persist? J Ment Health Policy Econ. 2006;9(3):155–163. [PubMed] [Google Scholar]
- 35.McGuire TG, Montgomery JT. Mandated mental health benefits in private insurance. J Health Polit Polic. 1982;7(2):380–406. doi: 10.1215/03616878-7-2-380. http://dx.doi.org/10.1215/03616878-7-2-380. [DOI] [PubMed] [Google Scholar]
- 36.Sturm R, Goldman W, McCulloch J. Mental health and substance abuse parity: a case study of Ohio’s state employee program. J Ment Health Policy Econ. 1998;1(3):129–134. doi: 10.1002/(sici)1099-176x(1998100)1:3<129::aid-mhp16>3.0.co;2-u. http://dx.doi.org/10.1002/(SICI)1099-176X(1998100)1:3<129::AID-MHP16>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 37.Ciemins EL. The effect of parity-induced copayment reductions on adolescent utilization of substance use services. J Stud Alcohol. 2004;65(6):731–735. doi: 10.15288/jsa.2004.65.731. [DOI] [PubMed] [Google Scholar]
- 38.Lindrooth RC, Sasso ATL, Lurie IZ. The effect of expanded mental health benefits on treatment initiation and specialist utilization. Health Serv Res. 2005;40(4):1092–1107. doi: 10.1111/j.1475-6773.2005.00406.x. http://dx.doi.org/10.1111/j.1475-6773.2005.00406.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sasso ATL, Lindrooth RC, Lurie IZ, Lyons JS. Expanded mental health benefits and outpatient depression treatment intensity. Med Care. 2006;44(4):366–372. doi: 10.1097/01.mlr.0000204083.55544.f8. http://dx.doi.org/10.1097/01.mlr.0000204083.55544.f8. [DOI] [PubMed] [Google Scholar]
- 40.Sasso ATL, Lurie IZ, Lee JU, Lindrooth RC. The effects of expanded mental health benefits on treatment costs. J Ment Health Policy Econ. 2006;9(1):25–33. [PubMed] [Google Scholar]
Footnotes
Adverse selection occurs when people in poor health enroll in insurance plans that offer more-extensive benefits, resulting in a higher risk pool in those health plans. Moral hazard occurs when people in healthcare plans with reduced out-of-pocket costs use services at higher rates than people in plans with greater costs. (Frank RG, Koyanagi C, McGuire TG. The politics and economics of mental health “parity” laws. Health Affairs. 1994;(4):108–119.)
No financial disclosures were reported by the authors of this paper.
The names and affiliations of the Task Force members are listed at www.thecommunityguide.org/about/task-force-members.html
References
- 1.CDC. Mental illness surveillance among adults in the United States. MMWR Morb Mortal Wkly Rep. 2011;60(Suppl):1–29. [PubMed] [Google Scholar]
- 2.Kessler R, Berglund P, Demler O, Jin R, Walters E. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R) Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. http://dx.doi.org/10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 3.Kessler R, Chiu W, Demler O, Walter E. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psych. 2005;62:617–709. doi: 10.1001/archpsyc.62.6.617. http://dx.doi.org/10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kessler R, Chiu W, Colpe L, et al. The prevalence and correlates of serious mental illness (SMI) in the National Comorbidity Survey Replication (NCS-R) In: Manderscheid R, Berry J, editors. Mental Helath, United States. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2004. pp. 134–148. [Google Scholar]
- 5.Administration SAaMHS. Results from the 2012 National Survey on Drug Use and Health: Mental Health Findings, NSDUH Series H-47, HHS Publication No. (SMA) 13-4805. Rockville, MD: Substance Abuse and Mental Helath Services Administration; 2013. [Google Scholar]
- 6.Services USDoHaH. Mental Health: A Report of the Surgeon General. Rockville, MD: U.S. DHHS, Substance Abuse and Mental Health Services Adminsitration, Center for Mental Health Services, NIH, National Institute of Mental Health; 1999. [Google Scholar]
- 7.Hirschfeld RA, Keller MB, Panico S, et al. THe national depressive and manic-depressive association consensus statement on the undertreatment of depression. JAMA. 1997;277(4):333–340. http://dx.doi.org/10.1001/jama.1997.03540280071036. [PubMed] [Google Scholar]
- 8.National Council for Community Behavioral Healthcare. State spending on untreated mental illnesses and substance use disorders. Washington, DC: National Council for Behavioral Health; 2012. [Google Scholar]
- 9.IOM. The healthcare imperative: Lowering costs and improving outcomes: Workshop series summary. Washington, DC: National Academies Press; 2010. [PubMed] [Google Scholar]
- 10.Substance Abuse and Mental Health Services Administration. Results from the 2008 National Survey on Drug Use and Health: National findings. Rockville, MD: Office of Applied Studies; 2009. NSDUH Series H-36, HHS Publication No. SMA 09-4434. [Google Scholar]
- 11.Henry J Kaiser Family Foundation. Kaiser Health Tracking Poll: Public Opinion on Healthcare Issues. 2009 Feb; kff.org/health-costs/poll-finding/kaiser-health-tracking-poll-february-2009/
- 12.Harris KM, Carpenter C, Bao Y. The effects of state parity laws on the use of mental health care. Med Care. 2006;44(6):499–505. doi: 10.1097/01.mlr.0000215813.16211.00. http://dx.doi.org/10.1097/01.mlr.0000215813.16211.00. [DOI] [PubMed] [Google Scholar]
- 13.Public Law 104–204—Sept. 26, 1996. Departments of Veterans Affairs and Housing and Urban Development and Independent Agencies Appropriations Act; 1996
- 14.H. R. 1424—117 Subtitle B—Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act of 2008; 2008.
- 15.Patient Protection and Affordable Care Act (H.R. 3590) Public Law 111–148; 2009.
- 16.Secretary Solis, U.S. Department of Labor. Report to Congress. Compliance of group health plans (and health insurance coverage offered in connection with such plans) with the requirements of the Mental Health Parity and Addiction Equity Act of 2008. www.dol.gov/ebsa/publications/mhpaeareporttocongress2012.html.
- 17.Cauchi R, Landless S, Thangasamy A. State laws mandating or regulating mental health benefits. www.ncsl.org/issues-research/health/mental-health-benefits-state-laws-mandating-or-re.aspx.
- 18.Goldman H, Lichtenstein C, Frank RG, et al. Evaluation of parity in the Federal Employees Health Benefits (FEHB) program: Final report. Washington, DC: U.S. DHHS; 2005. [Google Scholar]
- 19.Sharfstein SS, Magnas HL. Insuring intensive psychotherapy. Am J Psychiatry. 1975;132(2):1252–1256. doi: 10.1176/ajp.132.12.1252. [DOI] [PubMed] [Google Scholar]
- 20.Azzone V, Frank RG, Normand SLT, Burnam MA. Effect of insurance parity on substance abuse treatment. Psychiatric Serv. 2011;62(2):129–134. doi: 10.1176/appi.ps.62.2.129. http://dx.doi.org/10.1176/ps.62.2.pss6202_0129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gitterman D. Why mental health parity in the U.S.? Political and economic determinants of policy change. Paper presented at the Tenth NIMH Biennial Research Conference on the Economics of Mental Health; Bethesda, MD. 2000. [Google Scholar]
- 22.Frank RG, Goldman HH, McGuire TG. Will parity in coverage result in better mental health care? New Engl J Med. 2001;(23):1701–1704. doi: 10.1056/NEJM200112063452311. http://dx.doi.org/10.1056/NEJM200112063452311. [DOI] [PubMed]
- 23.Gitterman DP, Sturm R, Pacula RL, Scheffler RM. Does the sunset of mental health parity really matter? Adm Policy Ment Health. 2001;28(5):353–369. doi: 10.1023/a:1011113932599. http://dx.doi.org/10.1023/A:1011113932599. [DOI] [PubMed] [Google Scholar]
- 24.Busch AB, Huskamp HA, Normand SLT, Young AS, Goldman H, Frank RG. The impact of parity on major depression treatment quality in the Federal Employees’ Health Benefits Program after parity implementation. Med Care. 2006;(6):506–512. doi: 10.1097/01.mlr.0000215890.30756.b2. http://dx.doi.org/10.1097/01.mlr.0000215890.30756.b2. [DOI] [PMC free article] [PubMed]
- 25.Mental Health Parity and Addiction Equity Act of 2008 (HR 1424). www.ncsl.org/issues-research/health/archive-federal-mental-health-parity-2008.aspx
- 26.U.S. Department of Labor, Employee Benefits Security Administration. Fact sheet: The Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA) 2010 www.dol.gov/ebsa/newsroom/fsmhpaea.html.
- 27.Briss PA, Zaza S, Pappaioanou M, et al. Developing an evidence-based Guide to Community Preventive Services—methods. Am J Prev Med. 2000;18(1S):35–43. doi: 10.1016/s0749-3797(99)00119-1. http://dx.doi.org/10.1016/S0749-3797(99)00119-1. [DOI] [PubMed] [Google Scholar]
- 28.Sipe T, Chin H, Elder R, et al. Methods for conducting Community Guide systematic reviews of evidence on effectiveness and economic efficiency of group-based behavioral interventions to prevent adolescent pregnancy, HIV, and other sexually transmitted infections: Comprehensive risk reduction and abstinence education. Am J Prev Med. 2012;42(3):295–303. doi: 10.1016/j.amepre.2011.11.002. http://dx.doi.org/10.1016/j.amepre.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 29.Zaza S, Wright-de Aguero L, Briss P, et al. Data collection instrument and procedure for systematic reviews in the Guide to Community Preventive Services. Am J Prev Med. 2000;18(1S):44–74. doi: 10.1016/s0749-3797(99)00122-1. http://dx.doi.org/10.1016/S0749-3797(99)00122-1. [DOI] [PubMed] [Google Scholar]
- 30.Wagstaff A. Measuring financial protection in health. The World Bank; 2008. http://dx.doi.org/10.1596/1813-9450-4554. [Google Scholar]
- 31.Moreno-Serra R, Millett C, Smith P. Towards improved measurement of financial protection in health. PLOS Med. 2011;8(9):e10001087. doi: 10.1371/journal.pmed.1001087. http://dx.doi.org/10.1371/journal.pmed.1001087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.IOM, Committee on Quality of Health Care in America. Crossing the quality chasm: A new health sytem for the 21st century. Washington, DC: National Academy Press; 2001. [Google Scholar]
- 33.Health Related Quality of Life. CDC work group; www.cdc.gov/hrqol/concept.htm. [Google Scholar]
- 34.Thomson HJ, Thomas S. The effect direction plot: visual display of non-standardised effects across multiple outcome domains. Res Synth Methods. 2013;4(1):95–101. doi: 10.1002/jrsm.1060. http://dx.doi.org/10.1002/jrsm.1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pacula RL, Sturm R. Mental health parity legislation: much ado about nothing? Health Serv Res. 2000;(1 Pt 2):263–275. [PMC free article] [PubMed]
- 36.Barry CL, Busch SH. Do state parity laws reduce the financial burden on families of children with mental health care needs? Health Serv Res. 2007;(3 Pt 1):1061–1084. doi: 10.1111/j.1475-6773.2006.00650.x. http://dx.doi.org/10.1111/j.1475-6773.2006.00650.x. [DOI] [PMC free article] [PubMed]
- 37.Klick J, Markowitz S. Are mental health insurance mandates effective? Evidence from suicides. Health Econ. 2006;(1):83–97. doi: 10.1002/hec.1023. http://dx.doi.org/10.1002/hec.1023. [DOI] [PubMed]
- 38.Dave DP, Mukerjee SP. Mental health parity legislation, cost-sharing and substance-abuse treatment admissions. Health Econ. 2009;20(2):161–183. doi: 10.1002/hec.1577. http://dx.doi.org/10.1002/hec.1577. [DOI] [PubMed] [Google Scholar]
- 39.Bao Y, Sturm R. The effects of state mental health parity legislation on perceived quality of insurance coverage, perceived access to care, and use of mental health specialty care. Health Serv Res. 2004;(5):1361–1377. doi: 10.1111/j.1475-6773.2004.00294.x. http://dx.doi.org/10.1111/j.1475-6773.2004.00294.x. [DOI] [PMC free article] [PubMed]
- 40.Trivedi AN, Swaminathan S, Mor V. Insurance parity and the use of outpatient mental health care following a psychiatric hospitalization. JAMA. 2008;300(24):2879–2885. doi: 10.1001/jama.2008.888. http://dx.doi.org/10.1001/jama.2008.888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lang M. The impact of mental health insurance laws on state suicide rates. Health Econ. 2011;21(10) doi: 10.1002/hec.1816. [DOI] [PubMed] [Google Scholar]
- 42.Barry CL. Thesis. Harvard University; 2005. The political economy of mental health parity. [Google Scholar]
- 43.Barry CL, Busch SH. Caring for children with mental disorders: do state parity laws increase access to treatment? J Ment Health Policy Econ. 2008;11(2):57–66. [PubMed] [Google Scholar]
- 44.Azrin ST, Huskamp HA, Azzone V, et al. Impact of full mental health and substance abuse parity for children in the Federal Employees Health Benefits Program. Pediatrics. 2007;119(2):e452–459. doi: 10.1542/peds.2006-0673. http://dx.doi.org/10.1542/peds.2006-0673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Goldman HH, Frank RG, Burnam MA, et al. Behavioral health insurance parity for federal employees. New Engl J Med. 2006;354(13):1378–1386. doi: 10.1056/NEJMsa053737. http://dx.doi.org/10.1056/NEJMsa053737. [DOI] [PubMed] [Google Scholar]
- 46.Busch SH, Barry CL. New evidence on the effects of state mental health mandates. Inquiry. 2008;45(3):308–322. doi: 10.5034/inquiryjrnl_45.03.308. http://dx.doi.org/10.5034/inquiryjrnl_45.03.308. [DOI] [PubMed] [Google Scholar]
- 47.McConnell J, Gast S, Ridgely S, et al. Behavioral health insurance parity: Does Oregon’s experience presage the national experience with the mental health parity and addiction. Am J Psychiatry. 2011;169(1):31–38. doi: 10.1176/appi.ajp.2011.11020320. http://dx.doi.org/10.1176/appi.ajp.2011.11020320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zuvekas SH, Regier DA, Rae DS, Rupp A, Narrow WE. The impacts of mental health parity and managed care in one large employer group. Health Aff. 2002;21(3):148. doi: 10.1377/hlthaff.21.3.148. http://dx.doi.org/10.1377/hlthaff.21.3.148. [DOI] [PubMed] [Google Scholar]
- 49.Zuvekas SH, Rupp A, Norquist GS. The impacts of mental health parity and managed care in one large employer group: A reexamination. Health Aff (Millwood) 2005;24(6):1668–1671. doi: 10.1377/hlthaff.24.6.1668. http://dx.doi.org/10.1377/hlthaff.24.6.1668. [DOI] [PubMed] [Google Scholar]
- 50.Zuvekas SH, Rupp AE, Norquist GS. Spillover effects of benefit expansions and carve-outs on psychotropic medication use and costs. Inquiry. 2005;(1):86–97. doi: 10.5034/inquiryjrnl_42.1.86. http://dx.doi.org/10.5034/inquiryjrnl_42.1.86. [DOI] [PubMed]
- 51.Parity Evaluation Research Team, for DHHS, Assistant Secretary for Planning and Evaluation. Evaluation of parity in the Federal Employees Health Benefits (FEHB) Program: Final Report. 2004 aspe.hhs.gov/daltcp/reports/parity.htm.
- 52.Rosenbach M, Lake T, Young C, et al. Effects of the Vermont Mental Health and Substance Abuse Parity Law. Rockville, MD: Center for Mental Health Services, Substance Abuse & Mental Health Services Administration; 2003. DHHS Pub. No. (SMA) 03-3822. [Google Scholar]
- 53.Sturm R. State parity legislation and changes in health insurance and perceived access to care among individuals with mental illness: 1996–1998. J Ment Health Policy Econ. 2000;3(4):209–213. doi: 10.1002/mhp.97. http://dx.doi.org/10.1002/mhp.97. [DOI] [PubMed] [Google Scholar]
- 54.Sturm R, Goldman W, McCulloch J. Mental health and substance abuse parity: a case study of Ohio’s state employee program. J Ment Health Policy Econ. 1998;1(3):129–134. doi: 10.1002/(sici)1099-176x(1998100)1:3<129::aid-mhp16>3.0.co;2-u. http://dx.doi.org/10.1002/(SICI)1099-176X(1998100)1:3<129::AID-MHP16>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 55.Sturm R, Pacula RL. State mental health parity laws: cause or consequence of differences in use? Health Aff. 1999;18(5):182–192. doi: 10.1377/hlthaff.18.5.182. http://dx.doi.org/10.1377/hlthaff.18.5.182. [DOI] [PubMed] [Google Scholar]
- 56.McGuire TG, Montgomery JT. Mandated mental health benefits in private health insurance. J Health Polit Polic. 1982;7(2):380–406. doi: 10.1215/03616878-7-2-380. http://dx.doi.org/10.1215/03616878-7-2-380. [DOI] [PubMed] [Google Scholar]
- 57.Ciemens EL. Thesis. University of California; Berkley: 2003. The effect of mental health parity on children’s mental health and substance abuse service utilization in Massachusetts. [Google Scholar]
- 58.Rosenbach ML, Ammering CJ. Trends in Medicare Part B mental health utilization and expenditures: 1987–92. Health Care Financ Rev. 1997;18(3):19–42. [PMC free article] [PubMed] [Google Scholar]
- 59.An R, Sturm R. Self-reported unmet need for mental health care after California’s parity legislation. Psychiatric Serv. 2010;61(9):861–862. doi: 10.1176/appi.ps.61.9.861. http://dx.doi.org/10.1176/ps.2010.61.9.861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Barry CL, Gabel JR, Frank RG, Hawkins S, Whitmore HH, Pickreign JD. Design of mental health benefits: Still unequal after all these years. Health Aff. 2003;22(5):127–137. doi: 10.1377/hlthaff.22.5.127. http://dx.doi.org/10.1377/hlthaff.22.5.127. [DOI] [PubMed] [Google Scholar]
- 61.Branstrom RB, Cuffel B. Economic grand rounds: policy implications of adverse selection in a preferred-provider organization carve-out after parity. Psychiatric Serv. 2004;55(4):357–359. doi: 10.1176/appi.ps.55.4.357. http://dx.doi.org/10.1176/appi.ps.55.4.357. [DOI] [PubMed] [Google Scholar]
- 62.Branstrom RB, Sturm R. An early case study of the effects of California’s mental health parity legislation. Psychiatric Serv. 2002;53(10):1215–1216. doi: 10.1176/appi.ps.53.10.1215. http://dx.doi.org/10.1176/appi.ps.53.10.1215. [DOI] [PubMed] [Google Scholar]
- 63.Dinallo E. Report by the Superintendent of Insurance on the cost and effectiveness of New York’s 2006 Mental Health Parity Legislation (Timothy’s Law) Albany, NY: New York State Insurance Department; 2009. [Google Scholar]
- 64.Morrisey MA, Jensen GA. Employer-sponsored insurance coverage for alcoholism and drug-abuse treatments. J Stud Alcohol. 1988;49(5):456–461. doi: 10.15288/jsa.1988.49.456. [DOI] [PubMed] [Google Scholar]
- 65.Morton JD, Aleman P. Trends in employer-provided mental health and substance abuse benefits. Monthly Labor Rev. 2005;128(4):25–35. [Google Scholar]
- 66.Teich JL, Buck JA. Mental health benefits in employer-sponsored health plans. J Behav Health Serv Res. 2007;34(3):343–348. doi: 10.1007/s11414-006-9050-2. http://dx.doi.org/10.1007/s11414-006-9050-2. [DOI] [PubMed] [Google Scholar]
- 67.Zuvekas SH, Meyerhoefer CD. Coverage for mental health treatment: do the gaps still persist? J Ment Health Policy Econ. 2006;9(3):155–163. [PubMed] [Google Scholar]
- 68.Jensen G, Rost K, Burton R, Bulycheva M. Mental health insurance in the 1990s: are employers offering less to more? Health Aff. 1998;17(3):201–208. doi: 10.1377/hlthaff.17.3.201. http://dx.doi.org/10.1377/hlthaff.17.3.201. [DOI] [PubMed] [Google Scholar]
- 69.Mechanic D. Considerations in the design of mental health benefits under national health insurance. Am J Public Health. 1978;68(5):482–488. doi: 10.2105/ajph.68.5.482. http://dx.doi.org/10.2105/AJPH.68.5.482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Shannon BD. Paving the path to parity in health insurance coverage for mental illness: new law or merely good intentions. Univ Colo Law Rev. 1997;68:63–106. [Google Scholar]
- 71.Lee D, Foster G. Mental health and universal coverage. Los Angeles, CA: California Endowment; 2008. [Google Scholar]
- 72.Mental health and substance use: Employers’ insurance coverage maintained or enhanced since Parity Act, but effect of coverage on enrollees varied. Washington, DC: U.S. Government Accountability Office; 2011. GAO-12-63. [Google Scholar]
- 73.Claxton G, DiJulio B, Finder B, Lundy J. Employer health benefits: 2010 annual survey. Kaiser Family Foundation and Health Research and Educational Trust: The Henry J. Kaiser Family Foundation; 2010. [Google Scholar]
- 74.Sarata AK. Mental health parity and the Patient Protection and Affordable Care Act of 2010. Washington, DC: Congressional Research Service; 2011. [Google Scholar]
- 75.Krisberg K. Health law raising U.S. mental health parity to the next level: Access will widen. thenationshealth.aphapublications.org/content/42/7/1.1.full. The Nation’s Health. 2012;42(7):1–14. [Google Scholar]
- 76.Sartorius N. Stigma and mental health. Lancet. 2007;370(9590):810–811. doi: 10.1016/S0140-6736(07)61245-8. http://dx.doi.org/10.1016/S0140-6736(07)61245-8. [DOI] [PubMed] [Google Scholar]
- 77.Witwer S. The patient experience with the mental health system: A focus on integrated care solutions. J Manag Care Pharm. 2006;12(2 Suppl):21–23. doi: 10.18553/jmcp.2006.12.S2-A.S21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Fink PJ, Tasman A. Stigma and mental illness. Washington, DC: American Psychiatric Press; 1992. [Google Scholar]
- 79.Lake T, Sasser A, Young C, Quinn BA. snapshot of the implementation of California’s mental health parity law. Princeton, NJ: Mathmatica Policy Research, Inc; 2002. [Google Scholar]
- 80.Torrey E, Entsminger K, Geller J, Stanley J, Jaffe D. The shortage of public hospital beds for mentally ill persons: A report of the Treatment Advocacy Center. Arlington, VA: Treatment Advocacy Center; 2008. [Google Scholar]
- 81.Thomas K, Ellis A, Konrad T, Holzer C, Morrissey J. County-level estimates of mental health professional shortage in the United States. Psychiatric Serv. 2009;60(10):1323–1328. doi: 10.1176/ps.2009.60.10.1323. http://dx.doi.org/10.1176/ps.2009.60.10.1323. [DOI] [PubMed] [Google Scholar]
- 82.Mental health parity: Barriers and recommendations. California Department of Mental Health; 2005. A report to the Legislature. [Google Scholar]
- 83.Buchmueller TC, Cooper PF, Jacobson M, Zuvekas SH. Parity for whom? Exemptions and the extent of state mental health parity legislation. Health Aff (Millwood) 2007;26(4):w483–487. doi: 10.1377/hlthaff.26.4.w483. http://dx.doi.org/10.1377/hlthaff.26.4.w483. [DOI] [PubMed] [Google Scholar]
- 84.Barry CL. The political evolution of mental health parity. Harv Rev Psychiatry. 2006;14(4):185–194. doi: 10.1080/10673220600883168. http://dx.doi.org/10.1080/10673220600883168. [DOI] [PubMed] [Google Scholar]
- 85.Sturm R, Gresenz C, Sherbourne C, Minnium K. The design of Healthcare for Communities: A study of health care delivery for alcohol, drug abuse, and mental health conditions. Inquiry. 1999;36(2):221–233. [PubMed] [Google Scholar]
- 86.Truven Health Analytics. Better understand health economics and treatment outcomes. www.truvenhealth.com/your_healthcare_focus/pharmaceutical_and_medical_device/data_databases_and_online_tools.aspx.