Abstract
Objective
To examine the association between route of delivery and neonatal outcomes in a large, diverse cohort of preterm, appropriate for gestational age neonates
Methods
This is a retrospective cohort study examining New York City birth data for 1995 to 2003 linked to hospital discharge data. Data were limited to singleton, live born, cephalic neonates delivered between 24 and 34 weeks. Exclusion criteria included congenital anomalies, forceps or vacuum assistance, birth weight missing, less than 500 grams or not appropriate for gestational age. Any neonatal diagnosis of intraventricular hemorrhage, seizure, sepsis, subdural hemorrhage, respiratory distress, five minute Apgar less than 7, or neonatal death was considered significant. Associations between method of delivery and neonatal morbidities were estimated using logistic regression.
Results
Out of 20,231 neonates meeting study criteria, 69.3% were delivered vaginally and 30.7% were delivered by cesarean. After controlling for maternal age, ethnicity, education, primary payer, prepregnancy weight, gestational age, diabetes and hypertension, cesarean delivery compared with vaginal delivery was associated with increased odds of respiratory distress (39.2% compared with 25.6%, adjusted odds ratio [aOR] 1.74; 95% confidence interval [CI] 1.61–1.89) and five minute Apgar less than 7 (10.7% compared with 5.8%, aOR 2.04; 95% CI 1.77–2.35).
Conclusion
In this preterm cohort, cesarean delivery was not protective against poor outcomes and in fact was associated with increased risk of respiratory distress and low Apgar score compared with vaginal delivery.
Introduction
The cesarean delivery rate is significantly higher in preterm deliveries than in term deliveries (1). Undoubtedly many preterm cesareans are performed for necessary indications such as abruption or nonreassuring fetal status. However, it is uncertain how the route of delivery affects the outcome of the preterm neonate. Given the increased maternal morbidity and cost associated with preterm cesareans, it is vital that cesarean deliveries be reserved for instances in which they have clear benefit for the neonate or mother.
Previous studies have demonstrated mixed results. Deulofeut et al evaluated the smallest infants born before 34 weeks and suggested a reduction in mortality and intraventricular hemorrhage (IVH) with vaginal delivery (2). Additionally, Lee at al showed a decrease in mortality with vaginal delivery in appropriately grown preterm neonates (3). Other studies have found no significant difference between cesarean and vaginal deliveries with regard to neonatal outcomes in appropriately grown premature neonates (4,5,6). Even in small for gestational age neonates, a prior study by the authors of this paper found no difference in neonatal outcomes between cesarean and vaginal deliveries except with regard to neonatal respiratory distress, which was moderately decreased with vaginal delivery(7). This decrease has been hypothesized to result from active labor expelling excess fluid from the fetal lungs.
We sought to examine the association between route of delivery and neonatal outcomes in a large, diverse cohort of preterm, appropriate for gestational age neonates. We were particularly interested in examining the outcomes based on indication for delivery (maternal medical condition or obstetric complication) and gestational age (at or before 34 weeks and at or before 31 weeks).
Materials and Methods
Data on live births between 1995 and 2003 from the New York City Department of Health and Mental Hygiene were linked to the hospital discharge data from the Statewide Planning and Research Cooperative System (SPARC). Our study population was limited to deliveries in which birth certificates could be successfully linked to hospital discharge records utilizing a matching algorithm used in multiple other studies (n=1,025,903) (7,8,9). Our study population included women delivering cephalic-presenting, singleton neonates between 24 and 34 completed weeks of gestation (n=25,615). Infants with congenital anomalies, those with growth restriction or a neonatal weight less 500 grams, those who were large for gestational age and those with missing information on neonatal weight were excluded. Growth restriction was defined as a birth weight less than the 10th percentile based on gestational age, gender-specific U.S. standard birth weights and large for gestational age was defined as a birth weight greater than the 90th percentile based on the same norms (10,11, 12). Infants delivered by vacuum or forceps were also excluded from this analysis given the possibility that operative deliveries may independently increase morbidity or mortality for the preterm neonate. Mode of delivery was determined both by birth certificate information and procedural codes in the SPARCS database. Based on these inclusion and exclusion criteria, the study population in this analysis was 20,231 (see Figure 1).
Figure 1.
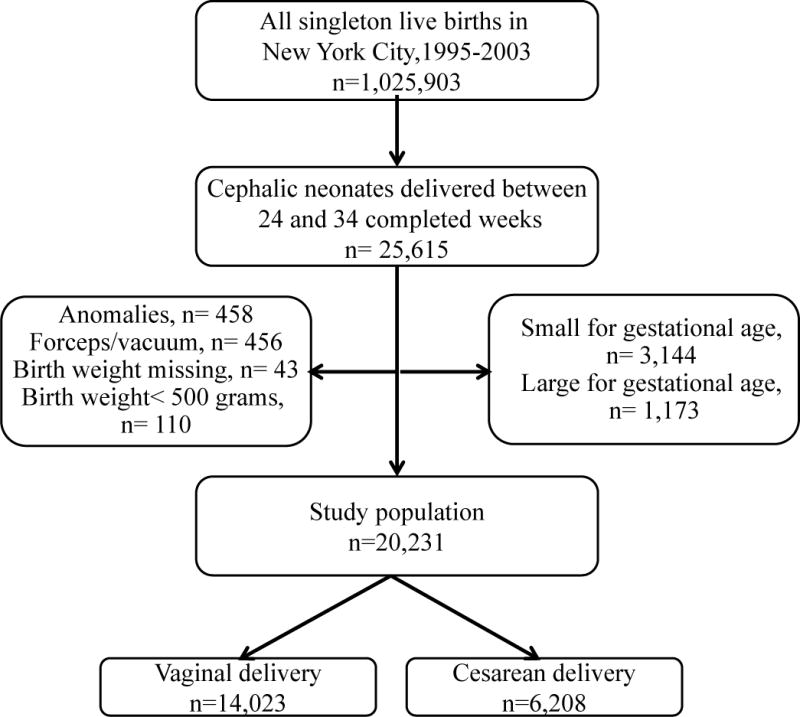
Study population flowchart
Several additional subanalyses were performed within this cohort. To investigate the effect that delivery indication could have on mode of delivery and outcome we subdivided the cohort based on A) deliveries for maternal medical indications (n=5,828), B) deliveries for obstetric complications (n=9,318), and C) deliveries with no medical or obstetric complications (n=7,511). The complete list of conditions composing each category is contained in Box 1 and is similar to the indications used in other studies (13). The maternal medical conditions and obstetric complications were not mutually exclusive; therefore, a given birth could be represented in both of these categories (n=2,426). Additionally to investigate the effect that early gestational age could have on mode of delivery and outcome, we performed a subgroup analysis in which we limited the study population to those with a gestational age less than or equal to 31 weeks (n=5,997).
Box 1. Indication Categories.
|
|
Category A: Maternal Medical Conditions (n=5,828)*
|
|
|
Category B: Obstetric Complications (n=9,318)*
|
|
|
Category C: Other (n=7,511)
|
|
|
* Category A and B are not mutually exclusive. Some deliveries had both obstetric and maternal complications.
The outcomes of interest in this study included neonatal death prior to discharge, neonatal respiratory distress, sepsis, intraventricular hemorrhage, seizure, subdural hemorrhage or five minute Apgar less than 7. Neonatal death was determined by discharge data included in the SPARCS dataset. Neonatal morbidities including respiratory distress, sepsis, intraventricular hemorrhage, seizure and subdural hemorrhage were ascertained using International Classification of Diseases, Ninth Revision (ICD-9) codes from the infant’s hospitalization record. Unfortunately, more detailed information on these diagnoses, such as the grade of intraventricular hemorrhage or how respiratory distress was diagnosed (clinically or radiographically), was not available. Neonatal seizure was defined by the presence of this complication in either the SPARCS or the birth certificate data since seizure is also identified on the birth certificate. Five minute Apgar scores were obtained from birth certificate data.
Maternal characteristics were examined as covariates and potential confounders based on previous literature. Maternal information derived from birth certificates included age, parity, race/ethnicity, level of education, insurance status, pre-pregnancy weight and tobacco use. Pre-pregnancy weight was used as a surrogate for body mass index because mother’s height was not available (9,14). We used categorical variables for maternal age based on the fields defined in New York State birth certificates (aged younger than 20 years, aged 20–34 years, and aged 35 years or older). These categories were used as advanced maternal age (aged 35 years and older) and teenage pregnancy (aged less than 20 years) are associated with increased risk for some complications.
Pregnancy and medical complications used as covariates include diabetes, hypertension and gestational age of delivery based on the clinical estimate reported on the birth certificate. We adjusted for gestational age using the clinical estimate in weeks reported on the birth certificate. This represents the delivering physician’s best estimate of gestation. Pregnancies complicated by diabetes and gestational diabetes were determined by a previously described algorithm that used information from both the hospital discharge and birth data (15). We combined diabetes and gestational diabetes as both are associated with fetal weight abnormalities and neonatal morbidity (16). Presence of maternal hypertension included preeclampsia, hypertension with onset during pregnancy and pre-existing hypertension as all can be associated with impaired fetal growth (17,18,19).
Statistical analysis
We estimated univariable associations between delivery mode and neonatal outcomes using the chi-square statistic. Logistic regression was used to determine the odds of each neonatal morbidity and neonatal mortality for cesarean delivery compared to vaginal delivery adjusting for potential confounders as described above. Covariates were considered for inclusion in the multivariable model if the univariable chi-square P values were less than 0.01.
All potential confounders were found to be significant based on this criterion and thus included. Analyses were conducted using the SAS System version 9.2 (SAS Institute, Cary NC). This study was approved by the Yale University Human Investigations Committee.
Results
Of the 20,321 neonates meeting the study criteria, 14,023 (69.3%) were delivered vaginally and 6,208 (30.7%) were delivered by cesarean. Baseline characteristics for those delivered vaginally and by cesarean are presented in Table 1. Given the large study population, all maternal and pregnancy characteristics differed significantly between comparison groups (p<0.05). Women who underwent cesarean delivery were older, heavier, more educated and more likely to have private insurance. They also were more likely to have diabetes and much more likely to have hypertensive disorders. Interestingly, women who had cesareans were also more likely to be parous compared to those who had vaginal deliveries.
Table 1.
Sociodemographic Characteristics by Delivery Mode
| Appropriate for Gestational Age | |||
|---|---|---|---|
| Vaginal Delivery (n=14,023) | Cesarean Delivery (n=6,208) | P | |
| Maternal age (years) | <0.001 | ||
| ■Younger than 20 | 12.8 | 5.5 | |
| ■20–34 | 68.6 | 63.8 | |
| ■35 and older | 18.6 | 30.8 | |
| Parity | <0.001 | ||
| ■Nulliparous | 46.5 | 41.4 | |
| ■1 | 26.9 | 27.1 | |
| ■2 | 13.6 | 16.2 | |
| ■3 or more | 13.1 | 15.3 | |
| Mother’s ethnicity | <0.001 | ||
| ■White, non-Hispanic | 15.2 | 17.5 | |
| ■Black, non-Hispanic | 40.4 | 41.5 | |
| ■Hispanic | 37.5 | 34.6 | |
| ■Asian or Pacific Islander | 6.3 | 6.3 | |
| ■Other | 0.6 | 0.2 | |
| Maternal education | <0.001 | ||
| ■High school or less | 67.4 | 58.3 | |
| ■More than high school | 32.6 | 41.7 | |
| Primary payer | <0.001 | ||
| ■Medicaid | 61.2 | 52.4 | |
| ■HMO | 9.6 | 12.4 | |
| ■3rd party | 22.9 | 30.2 | |
| ■Self-pay | 6.3 | 5.1 | |
| Prepregnancy weight (pounds) | <0.001 | ||
| ■99 or less | 3.4 | 2.2 | |
| ■100–149 | 62.0 | 55.6 | |
| ■150–199 | 28.0 | 32.5 | |
| ■200 or more | 6.6 | 9.7 | |
| Gestational age at delivery (weeks) | <0.001 | ||
| ■Less than 26 | 5.9 | 4.1 | |
| ■26–28 | 6.1 | 8.9 | |
| ■28–30 | 8.3 | 14.2 | |
| ■30–32 | 14.5 | 18.1 | |
| ■Greater than 32 | 65.2 | 54.6 | |
| Diabetes* | 6.7 | 9.8 | <0.001 |
| Hypertensive disorders† | 9.7 | 36.8 | <0.001 |
| Tobacco | 9.1 | 6.0 | <0.001 |
Data are percent unless otherwise specified.
Includes pregestational and gestational diabetes.
Includes chronic hypertension and preeclampsia
Table 2 presents the proportions, unadjusted and adjusted odds of neonatal complications including in-hospital neonatal mortality with cesarean delivery compared with vaginal delivery. Neonates born by cesarean had a higher risk of respiratory distress syndrome, 5 minute Apgar less than 7, sepsis, seizure and death compared to those delivered vaginally. After adjusting for maternal age, race, parity, education, insurance status, prepregnancy weight, diabetes, hypertension, smoking and gestational age at delivery, cesarean delivery continued to be associated with increased odds of respiratory distress syndrome, five minute Apgar less than 7 and death compared to vaginal delivery. To prevent one case of neonatal respiratory distress, 7.35 vaginal deliveries compared to cesarean deliveries were needed.
Table 2.
Proportion, Unadjusted and Adjusted Risk of Adverse Neonatal Outcomes by Mode of Delivery For Appropriate-For-Gestational-Age Infants*
| Vaginal Delivery (%) | Cesarean Delivery (%) | Odds Ratio (95% CI) | Adjusted Odds Ratio† (95% CI) | |
|---|---|---|---|---|
| Respiratory distress | 25.6 | 39.2 | 1.88 (1.76–2.00) |
1.74 (1.61–1.89) |
| Sepsis | 3.1 | 3.9 | 1.28 (1.09–1.50) |
1.128 (0.94–1.35) |
| Intraventricular hemorrhage | 5.0 | 5.5 | 1.10 (0.96–1.26) |
0.99 (0.84–1.17) |
| Seizures | 0.7 | 1.1 | 1.53 (1.12–2.09) |
1.25 (0.84–1.85) |
| Subdural hemorrhage | 0.9 | 0.9 | 1.01 (0.74–1.38) |
0.90 (0.61–1.31) |
| Five minute Apgar less than 7 | 5.8 | 10.7 | 1.94 (1.74–2.15) |
2.04 (1.77–2.35) |
| Death | 2.8 | 3.4 | 1.24 (1.04–1.48) |
1.30 (1.02–1.66) |
CI, confidence interval.
Appropriate for gestational age defined as greater than the 10th percentile and less than 90th percentile.
Adjusted for age, parity, ethnicity, education, insurance, prepregnancy weight, gestational age at delivery, smoking, diabetes and hypertension.
When the study population was examined based on indication, cesarean delivery was more common than vaginal delivery if a maternal medical condition was identified (2,995 or 51.4% by cesarean delivery and 2,833 or 48.6% by vaginal delivery). Vaginal delivery was more frequent when the indication for delivery was obstetric complication (5,343 or 57.3% by vaginal delivery and 3,975 or 42.7% by cesarean delivery). Vaginal delivery was also far more common if the delivery did not involve a maternal or obstetric complication (6,816 or 90.8% by vaginal delivery and 695 or 9.2% by cesarean delivery). Regardless of indication for delivery, cesarean delivery was associated with increased odds of respiratory distress compared to vaginal delivery (see Table 3).
Table 3.
Adjusted Risk of Adverse Neonatal Outcomes by Mode of Delivery (Cesarean Delivery Compared With Vaginal Delivery) For Appropriate-for-Gestational-Age Infants* Based on Indication
| Maternal Medical Condition | Obstetric Complication | No Maternal or Obstetric Complication | |
|---|---|---|---|
| aOR† (95% CI) | aOR† (95% CI) | aOR† (95% CI) | |
| Respiratory distress | 1.96 (1.71–2.26) |
1.75 (1.58–1.95) |
1.47 (1.20–1.81) |
| Sepsis | 1.19 (0.89–1.58) |
0.92 (0.73–1.18) |
1.33 (0.87–2.04) |
| Intraventricular hemorrhage | 0.82 (0.62–1.08) |
1.14 (0.93–1.40) |
0.85 (0.53–1.36) |
| Seizures | 0.63 (0.34–1.17) |
1.27 (0.80–2.01) |
1.76 (0.66–4.69) |
| Subdural hemorrhage | 0.91 (0.47–1.76) |
0.83 (0.51–1.35) |
1.71 (0.86–3.44) |
| Five minute Apgar less than 7 | 1.73 (1.35–2.22) |
2.11 (1.78–2.49) |
1.47 (0.97–2.23) |
| Death | 0.91 (0.59–1.41) |
1.17 (0.89–1.54) |
1.49 (0.75–2.98) |
OR, odds ratio; CI, confidence interval.
Appropriate for gestational age defined as greater than the 10th percentile and less than the 90th percentile.
Adjusted for age, parity, ethnicity, education, insurance, prepregnancy weight, gestational age at delivery and smoking.
When the cohort was limited to the population delivered at or prior to 30 weeks, the association between cesarean and increased risk of respiratory distress (aOR 1.41; 95% CI 1.24–1.59) and Apgar less than 7 at 5 minute (aOR 1.43; 95% CI 1.22–1.68) persisted.
Discussion
Cesarean deliveries have been increasing steadily for the past two decades. Very preterm neonates (less than 34 weeks) have the highest rate of cesarean delivery, approaching 50% according to the National Vital Statistics (1). A few studies have found an association between cesarean delivery and increased odds of respiratory distress (7,20,21), but others have found no increased neonatal risk with cesarean delivery (4). Our study, like Lee et al., challenges the notion that cesareans are equivalent to vaginal deliveries for preterm neonates (3). For appropriately grown neonates, especially between 31weeks and 34 weeks, vaginal delivery is associated with decreased odds of neonatal death, respiratory distress and low Apgar scores. This suggests that when medically safe, vaginal delivery may be advantageous for the neonate, or at minimum, that it does no harm and avoids the potentially negative effect of cesarean delivery.
Interestingly, the indication for delivery, maternal or obstetric, did not significantly alter the odds ratios for respiratory distress. Even in the low risk population with no known maternal or obstetric complications, respiratory distress remained associated with cesarean compared with vaginal delivery. This suggests that the birthing process itself may provide early neonatal benefits above cesarean delivery.
This study has several strengths. Birth prior to 34 weeks is relatively uncommon and, given improved neonatal care, morbidity and mortality especially after 31 weeks is less common, requiring a large cohort. New York City provides an ideal study population for such a study as it is large and socially, racially and economically diverse. Additionally the database used combines birth certificate data and hospital discharge information. This pairing of analyzed variables has been shown to significantly improve the quality of the data (22).
While the population size and scope of this study would be difficult to obtain in a prospective fashion, using a retrospective, nonrandomized cohort has significant limitations. Misclassification of gestational age and mode of delivery as well as under-reporting of neonatal poor outcomes may have occurred in some cases (23). Additionally some desired data was unavailable. We were not able to differentiate those patients who were induced from those patients who labored spontaneously. We also were unable to identify patients who underwent cesarean deliveries without labor from those who labored and then had a cesarean. Finally, we could not adequately access the urgency of the delivery. For example, while nonreassuring fetal status was recorded as an indication, there was no distinction between a prolonged bradycardia and recurrent variables. The urgency of the delivery is particularly important as pregnancies complicated by emergent cesareans may not have benefited from steroids. Unfortunately, steroid administration data was not available for this cohort. Thus, despite extensive efforts to control for baseline differences in risks when comparing vaginal deliveries with cesarean deliveries, confounding by indication remains a possible explanation for our results.
Despite the limitations of this study, it underscores the lack of benefit to preterm neonates from the increasing cesarean delivery rate. There may be significant benefit to labor and vaginal delivery that is untapped when preterm neonates undergo a cesarean delivery. This benefit seems most pronounced in those deliveries that are preterm but not extremely premature. Prospective studies are needed to explore this association more completely. However, while awaiting future studies, the findings of this study suggest that it is most prudent to attempt a vaginal delivery in all preterm neonates needing to be delivered if it is medically safe to do so.
Footnotes
Financial Disclosure: None
Presented at the Society for Maternal-Fetal Medicine meeting, Dallas, Texas, February 9, 2012.
References
- 1.Menacker F, Hamilton BE. Recent trends in cesarean delivery in the United States. NCHS Data Brief. 2010:1–8. [PubMed] [Google Scholar]
- 2.Deulofeut R, Sola A, Lee B, Buchter S, Rahman M, Rogido M. The impact of vaginal delivery in premature infants weighing less than 1,251 grams. Obstet Gynecol. 2005;105:525–31. doi: 10.1097/01.AOG.0000154156.51578.50. [DOI] [PubMed] [Google Scholar]
- 3.Lee HC, Gould JB. Survival rates and mode of delivery for vertex preterm neonates according to small- or appropriate-for-gestational-age status. Pediatrics. 2006;118:e1836–44. doi: 10.1542/peds.2006-1327. [DOI] [PubMed] [Google Scholar]
- 4.Wylie BJ, Davidson LL, Batra M, Reed SD. Method of delivery and neonatal outcome in very low-birthweight vertex-presenting fetuses. Am J Obstet Gynecol. 2008;198:1–8. doi: 10.1016/j.ajog.2007.12.038. [DOI] [PubMed] [Google Scholar]
- 5.Riskin A, Riskin-Mashiah S, Lusky A, Reichman B, Israel Neonatal Network The relationship between delivery mode and mortality in very low birthweight singleton vertex-presenting infants. BJOG. 2004;111:1365–71. doi: 10.1111/j.1471-0528.2004.00268.x. [DOI] [PubMed] [Google Scholar]
- 6.Jonas HA, Lumley JM. The effect of mode of delivery on neonatal mortality in very low birthweight infants born in victoria, australia: Caesarean section is associated with increased survival in breech-presenting, but not vertex-presenting, infants. Paediatr Perinat Epidemiol. 1997;11:181–99. doi: 10.1046/j.1365-3016.1997.d01-19.x. [DOI] [PubMed] [Google Scholar]
- 7.Werner EF, Savitz DA, Janevic TM, Ehsanipoor RM, Thung SF, Funai EF, et al. Mode of delivery and neonatal outcomes in preterm, small-for-gestational-age newborns. Obstet Gynecol. 2012;120:560–4. doi: 10.1097/AOG.0b013e318265b16c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Werner EF, Janevic TM, Illuzzi J, Funai EF, Savitz DA, Lipkind HS. Mode of delivery in nulliparous women and neonatal intracranial injury. Obstet Gynecol. 2011;118:1239–46. doi: 10.1097/AOG.0b013e31823835d3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosenberg TJ, Garbers S, Lipkind H, Chiasson MA. Maternal obesity and diabetes as risk factors for adverse pregnancy outcomes: Differences among 4 racial/ethnic groups. Am J Public Health. 2005;95:1545–51. doi: 10.2105/AJPH.2005.065680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oken E, Kleinman KP, Belfort MB, Hammitt JK, Gillman MW. Associations of gestational weight gain with short- and longer-term maternal and child health outcomes. Am J Epidemiol. 2009;170:173–80. doi: 10.1093/aje/kwp101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oken E, Kleinman KP, Rich-Edwards J, Gillman MW. A nearly continuous measure of birth weight for gestational age using a united states national reference. BMC Pediatr. 2003;3:6. doi: 10.1186/1471-2431-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peleg D, Kennedy CM, Hunter SK. Intrauterine growth restriction: Identification and management. Am Fam Physician. 1998;58:453, 60, 466–7. [PubMed] [Google Scholar]
- 13.Reddy UM, Zhang J, Sun L, Chen Z, Raju TN, Laughon SK. Neonatal mortality by attempted route of delivery in early preterm birth. Am J Obstet Gynecol. 2012;207:117.e1–117.e8. doi: 10.1016/j.ajog.2012.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rosenberg TJ, Garbers S, Chavkin W, Chiasson MA. Prepregnancy weight and adverse perinatal outcomes in an ethnically diverse population. Obstet Gynecol. 2003;102:1022–7. doi: 10.1016/j.obstetgynecol.2003.07.005. [DOI] [PubMed] [Google Scholar]
- 15.Savitz DA, Janevic TM, Engel SM, Kaufman JS, Herring AH. Ethnicity and gestational diabetes in new york city, 1995–2003. BJOG. 2008;115:969–78. doi: 10.1111/j.1471-0528.2008.01763.x. [DOI] [PubMed] [Google Scholar]
- 16.Aljohani N, Rempel BM, Ludwig S, Morris M, Cheang M, Murray R, et al. Impact of diabetes on maternal-fetal outcomes in manitoba: Relationship with ethnic and environmental factors. Clin Invest Med. 2008;31:E338–45. doi: 10.25011/cim.v31i6.4919. [DOI] [PubMed] [Google Scholar]
- 17.Sibai BM, Koch MA, Freire S, Pinto e Silva JL, Rudge MV, Martins-Costa S, et al. The impact of prior preeclampsia on the risk of superimposed preeclampsia and other adverse pregnancy outcomes in patients with chronic hypertension. Am J Obstet Gynecol. 2011;204:345.e1–345.e6. doi: 10.1016/j.ajog.2010.11.027. [DOI] [PubMed] [Google Scholar]
- 18.Gilbert WM, Young AL, Danielsen B. Pregnancy outcomes in women with chronic hypertension: A population-based study. J Reprod Med. 2007;52:1046–51. [PubMed] [Google Scholar]
- 19.Tuuli MG, Rampersad R, Stamilio D, Macones G, Odibo AO. Perinatal outcomes in women with preeclampsia and superimposed preeclampsia: Do they differ? Am J Obstet Gynecol. 2011;204:508.e1–508.e7. doi: 10.1016/j.ajog.2011.01.065. [DOI] [PubMed] [Google Scholar]
- 20.Malloy MH. Impact of cesarean section on intermediate and late preterm births: United states, 2000–2003. Birth. 2009;36:26–33. doi: 10.1111/j.1523-536X.2008.00292.x. [DOI] [PubMed] [Google Scholar]
- 21.Hansen AK, Wisborg K, Uldbjerg N, Henriksen TB. Risk of respiratory morbidity in term infants delivered by elective caesarean section: Cohort study. BMJ. 2008;336:85–7. doi: 10.1136/bmj.39405.539282.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lydon-Rochelle M, Holt VL, Cárdenas V, Nelson JC, Easterling TR, Gardella C, et al. The reporting of pre-existing maternal medical conditions and complications of pregnancy on birth certificates and in hospital discharge data. Am J Obstet Gynecol. 2005;193:125–34. doi: 10.1016/j.ajog.2005.02.096. [DOI] [PubMed] [Google Scholar]
- 23.Vinikoor LC, Messer LC, Laraia BA, Kaufman JS. Reliability of variables on the north carolina birth certificate: A comparison with directly queried values from a cohort study. Paediatr Perinat Epidemiol. 2010;24:102–12. doi: 10.1111/j.1365-3016.2009.01087.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


