Abstract
Objective
Researchers have identified significant limitations in some currently-used measures of health literacy. The purpose of this paper is to present data on the relation of health-related quality of life, health status, and health service utilization to performance on a new measure of health literacy in a nonpatient population.
Methods
The new measure was administered to 475 English- and Spanish-speaking community-dwelling volunteers along with existing measures of health literacy and assessments of health-related quality of life, health status, and healthcare service utilization. Relations among measures were assessed via correlations and health status and utilization was tested across levels of health literacy using ANCOVA models.
Results
The new health literacy measure is significantly related to existing measures of health literacy as well as to participants’ health-related quality of life. Persons with lower levels of health literacy reported more health conditions, more frequent physical symptoms, and greater healthcare service utilization.
Conclusion
The new measure of health literacy is valid and shows relations to measures of conceptually-related constructs such as quality of life and health behaviors. Practice Implications: FLIGHT/VIDAS may be useful to researchers and clinicians interested in a computer administered and scored measure of health literacy.
Keywords: Health literacy, quality of life, healthcare service utilization, FLIGHT/VIDAS
1. Introduction
Health literacy has been defined as a person’s ability to obtain and use health information to make decisions [1] Research shows that health literacy is related to health indicators that include self-reported health, daily functioning, risk for hospitalization and death, and use of healthcare services [2-5]. The observed relations between health literacy and important indicators of health status have led investigators to develop interventions to improve health literacy [6,7] in the hope that they may be effective in improving patient health and address race- and ethnicity related health disparities [8,9]. In order to evaluate intervention effectiveness and provide a means to evaluate health literacy as a construct it is necessary to measure it.
Several measures of health literacy have been developed, and each has strengths and weaknesses. Perhaps the most widely-used measure of health literacy is the Test of Functional Health Literacy in Adults [10]. The TOFHLA samples a person’s performance in reading comprehension as well as in performing simple tasks requiring number skills. The TOFHLA must be administered and scored by a clinician and in general takes 30 minutes. The time required thus limits the TOFHLA’s use. The Rapid Estimate of Adult Literacy in Medicine, or REALM [11], asks that patients read aloud a list of health-related words. It requires less time to complete than the TOFHLA, but doesn’t evaluate whether the patient understands what he or she reads or numeracy skills. The Newest Vital Sign [12], on the other hand, consists of brief questions about a food nutrition label. It is short and easy to administer and score, but assesses only a very small range of health literacy skills.
While measures are thus available, they have also been criticized for other reasons [13-16]. Most sample a very limited set of health literacy skills and were developed on small and homogeneous groups of clinic patients rather than the general population [15]. Spanish and English versions of several measures are available but it is not clear that they measure the same construct in both languages or are equivalent in difficulty so that their scores can be meaningfully compared. For example, the Spanish and English versions of the TOHFLA Reading subscale are based on the same text passages but require responses to different elements in those passages. Response format may also be an issue, as the cloze procedure used in the TOFHLA reading subtest may be differentially more difficult for older compared to younger persons [17]. A final problem with existing measures is that most show pronounced ceiling effects (many persons obtain perfect or near-perfect scores) when administered to groups in the general population. Perhaps reflecting that most were developed with convenience samples of persons at clinics, they function well as screening tools to detect persons with low health literacy. These measures may not work as well to evaluate health literacy in other groups.
A health literacy test that addresses these issues is clearly needed. In addition, a measure that is computer-administered and scored would make assessment of patient and research participant health literacy more easily accessible. Such a measure could be integrated into an electronic health record, automating the process of assessment and interpretation by providing data directly to providers and researchers. This information could in turn be used to provide automated tailoring of information to patients’ level of health literacy. This may be an effective strategy to reduce race- and ethnicity-related health disparities [18].
A key issue in the development of any new measure is its validity. Standard approaches to validity for new measures of a construct usually center on demonstrating a new measure’s relation to existing measures of the same construct (concurrent validity), its ability to predict something in the future (predictive validity), the extent to which the measure represents a coherent or logical concept (construct validity) and the extent to which the items making up the measure have a clear relation to the concept they are believed to measure (content validity). Demonstration of a relation to existing measures of the construct health literacy is a necessary first step in showing that a new test is at least measuring something previously demonstrated to be important. This demonstration is thus key in linking the new test to existing research. In this paper we argue that a useful measure of health literacy should also be related to things that are meaningful to health care consumers as well as in relation to the healthcare system itself. In the project described here, we assessed participants’ health-related quality of life, health status by self-report of symptoms and diagnoses, and use of healthcare services such as doctor visits and medications.
The purpose of this paper is to report the relations of a newly-developed computer administered and scored measure of health literacy to existing measures as well as health-related quality of life, health status, and health service utilization. The new measure has been developed in both English and Spanish; the English project is named Fostering Literacy for Good Health Today (FLIGHT) and the Spanish is Vive Desarollando Amplia Salud (VIDAS).
2. Methods
2.1 Overview of initial development
This section provides an overview of the initial development of FLIGHT/VIDAS. Development procedures and analyses establishing the construct validity of FLIGHT/VIDAS have been described in detail in a previous publication [19] and are only summarized here. In Phase I of the project, items for the new measure were developed to assess a wide range of healthcare related content, based on the goals of health literacy outlined in the 2004 Institute of Medicine report on health literacy (Table 2-1, p. 42 [1]). By creating items related to these goals (promote health, understand information, use information, navigate the healthcare system, participate in encounters, give informed consent, and advocate for rights) in three literacy formats (prose, document, quantitative) an initial group of more than 225 questions was created. Items in the measure assess a wide variety of competencies, including information search, critical evaluation of information and strategies for health promotion in addition to content similar to that of existing measures, such as understanding how to take medications or diseases.
Table 2. Descriptive statistics for validity measures.
| Mean (SD) | T (df) | p | |||
|---|---|---|---|---|---|
|
| |||||
| English | Spanish | t | df | P | |
| TOFHLA Readinga | 45.7 (5.5) | 42.8 (9.5) | 5.45 | 472 | < .001 |
| TOFHLA Numeracya | 47.4 (3.7) | 42.6 (6.7) | 9.63 | 473 | < .001 |
| TOFHLA Total | 93.0 (8.0) | 84.4 (14.1) | 8.28 | 472 | < .001 |
| REALM | 62.1 (8.0) | N/Aa | |||
| SAHLSA | n/aa | 45.1 (4.5) | |||
| Hospitalb | .31 (.73) | .73 (1.04) | −4.97 | 459 | < .001 |
| Formsb | 2.5 (.93) | 2.0 (1.12) | 4.69 | 460 | < .001 |
| Infob | .48 (.85) | .79 (1.09) | −3.29 | 456 | < .001 |
| SF Phys Func | 77.3 (25.9) | 83.9 (21.3) | −2.98 | 450 | .003 |
| SF Limit Phys Func | 23.1 (37.3) | 13.3 (29.2) | 3.13 | 455 | .002 |
| SF Limit Emot Probs | 20.1 (34.3) | 16.6 (33.7) | 1.09 | 451 | .27 |
| SF Energy/Fatigue | 64.3 (21.2) | 72.7 (18.8) | −4.55 | 458 | < .001 |
| SF Emotional Wellbeing |
80.6 (16.6) | 77.0 (18.2) | 2.22 | 457 | .03 |
| SF Social Function | 84.4 (20.9) | 84.7 (19.3) | .11 | 456 | .91 |
| SF Pain | 72.9 (25.0) | 78.4 (22.0) | −2.52 | 459 | .01 |
| SF General Health | 70.9 (18.9) | 73.4 (17.5) | −1.42 | 451 | .16 |
| Physical Symptoms | 14.7 (9.4) | 11.7 (9.4) | 3.19 | 405 | .002 |
| Health Conditions | 3.3 (3.2) | 2.6 (3.1) | 2.48 | 456 | .01 |
| Medications | 1.4 (1.5) | 1.3 (1.5) | .80 | 462 | .42 |
| Doctor Visits | |||||
Table 1. Description of participants.
| English (N = 236) | Spanish (N = 239) | |
|---|---|---|
| Gender M/F | 94 (40%) / 142 (60%) | 94 (39%) / 145 (61%) |
| Hispanic | 24 | 239 |
| African American | 86 | 0 |
| Afro Caribbean | 26 | 0 |
| Asian/Pacific Islander | 2 | 0 |
| Mixed Race | 0 | 2 |
| White | 1 22 | 237 |
|
| ||
| Participants’ Age Group | ||
|
| ||
| Age Group (years) | N | N |
|
| ||
| 18 - 30 | 33 | 26 |
| 31 - 40 | 35 | 30 |
| 41 – 50 | 35 | 55 |
| 51 – 60 | 40 | 34 |
| 61 – 70 | 40 | 34 |
| 71 – 80 | 38 | 35 |
| Greater than 80 | 13 | 8 |
|
| ||
| Means (standard deviations) | ||
|
| ||
| Age | 51.9 (18.4) | 51.7 (16.5) |
| Education | 13.2 (2.4) | 11.7 (3.3) |
| Income | $31,894 ($24,471) | $26,088 ($21,752) |
These were then pilot tested with community-dwelling older and younger individuals in both English (n = 74) and Spanish (n = 72). The items were screened for equivalent functioning in older and younger persons and in both languages using nonparametric item response theory methods in order to screen items for equivalent function in both languages. A procedure was developed and implemented to evaluate Spanish speakers’ competence in both English and Spanish to determine in which language they would complete the study. This was done because other researchers have shown that Spanish speakers who state that they are fluent in English may be at a significant disadvantage compared to native English speakers on measures of health literacy [20].
During phase II of the project a reduced group of 98 items was administered to community-dwelling individuals from a wide range of ages, educational backgrounds, and across genders and race/ethnicity groups. Participants also completed a battery of measures intended to allow the measure’s validation not only in relation to other tests of health literacy but also to variables judged clinically meaningful. This battery thus included existing measures of health literacy and measures of health-related quality of life, health status and health service utilization.
In a previous publication we reported on the preliminary evaluation of the measure’s reliability and validity with an interim sample of 198 participants [19]. We concluded that, given the material assessed by the items of FLIGHT/VIDAS, the measure has clear content validity. In the previous publication we also described exploratory and confirmatory factor analyses that established the construct validity of the measure as representing four scales, general health literacy, numeracy, literacy, and conceptual knowledge. Data presented here are for the final sample of 475 participants.
2.2 Sample
Participants were recruited via flyers, presentations at community organizations, and by recruitment from previous studies. Purposive sampling focused on recruiting groups of Spanish- and English-speaking participants in the age ranges 18-30; 31-40; 41-50; 51-60; 61-70; 71-80; and 81 years and older. Recruitment was targeted to various socioeconomic, occupational, and educational backgrounds (e.g., ranging from grade school to doctoral-level graduate education) and, in the case of Spanish-speaking participants, to a range of national origins (Central and South America as well as Mexico and the US). This strategy allowed the recruitment of a diverse group of nonpatients so that preliminary norms for the new measure can be created. Participants were compensated for their participation. Participants complete study procedures in two sessions on one entire day or two separate half days; all persons have completed both sessions and thus no participants have dropped out.
2.3 Measures
As well as the new health literacy scale, participants completed a battery of existing measures (TOFHLA in English or Spanish; REALM or SAHLSA, and the self-report questions developed by Chew et al.[22]). Using a procedure modified from the MIDUS study [23], they provided information on their health status as the number and frequency of common physical symptoms they experienced (e.g., how often they had a headache) and the number of conditions they reported (e.g., heart disease, lung disease, cancer). Health-related quality of life was assessed with the Rand Medical Outcomes Study Short Form-36, or SF-36 [24], and mood with the Center for Epidemiological Studies Depression Scale or CES-D [25]. The EQ-5D is a widely-used health utility index that can be derived from SF-36 scales [26]. It provides a single general measure of health status that can be used in economic analyses and to track the impact of healthcare interventions, and has been shown to be useful in a number of conditions [27-32].
We asked participants how often they saw a physician or other provider and whether they took medications for health conditions such as hypertension or pain. When participants reported that they took medications, they were asked about how frequently they took them (e.g., every day for antihypertensives vs. occasional use of medication for headache). These measures were selected to allow the evaluation of the relation of the new measure to existing tests of health literacy to establish its concurrent validity with standard and widely-accepted measures. Other assessments (quality of life, health status, and health service utilization) were included to establish the new measure’s relation to clinically relevant variables that are not directly related to reading or education.
2.4 Data Analyses
Previous analyses [19] showed that FLIGHT/VIDAS has four scales: general health literacy (HL), numeracy (NUM), conceptual knowledge (FACT) and listening (LIS). Cronbach’s alpha was calculated for the scales of FLIGHT/VIDAS. Correlations of the FLIGHT/VIDAS scales with the TOFHLA, REALM, SAHLSA, and self-report questions were calculated to assess concurrent validity. We evaluated the relation of various levels of health literacy for health status, physician visits and medication use by defining groups with low, medium, and high levels of health literacy on the FLIGHT/VIDAS HL scale. Between-group differences were then assessed via analysis of variance (ANOVA).
All study procedures were completed under a protocol approved by the Institutional Review Board of Nova Southeastern University.
3. RESULTS
3.1 Descriptive data
Demographic data for participants (236 English- and 239 Spanish-speaking participants) are presented in Table 1. Spanish-speaking participants described their racial background as white or mixed race, consistent with findings from the US Census [33] while English-speaking participants were African American, Afro Caribbean, white, and Asian. Consistent with our sampling strategy, the average age of our participants is approximately 50, and the average level of education was equivalent to having completed high school. Our actual recruitment by target age groups is also included in this table. Table 2 presents descriptive statistics for the measures used to establish the concurrent validity of FLIGHT/VIDAS.
3.2 Reliability
Cronbach’s alphas for the scales of FLIGHT/VIDAS were 0.87 for HL for the combined sample (0.85 for English and 0.87 for Spanish speakers), 0.88 for NUM (0.87 for English and 0.85 for Spanish), 0.69 for FACT (0.74 for English and 0.60 for Spanish), and 0.55 for LIS (0.63 for English and 0.51 for Spanish). Consistent with our previous report on the reliabilities of the FACT and LIS scales,[19] we suggest that they be used for research purposes only.
3.3 Concurrent validity
Correlations of the FLIGHT/VIDAS scales with other measures of health literacy are presented in Table 3. It can be seen that even though FLIGHT/VIDAS was developed with a much broader range of content and uses a different response format, its scales are still significantly correlated with other tests of health literacy. Correlations of the FLIGHT/VIDAS scales with established measures of health literacy are similar to those among the established measures themselves.
Table 3. Scale intercorrelations and correlations of the new measure with other measures of health literacy.
| HL | NUMa | FACTa | LISa | TOFHLA Reading |
TOFHLA Numeracy |
REALMb | SAHLSAb | Hospitalc | Formsc | Infoc | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| HL | 1.00 | .82** | .77** | .65** | .69** | .50** | .59** | .52** | −.31** | .37** | −.34** |
| NUM | 1.00 | .53** | .57** | .59** | .49** | .50** | .33** | −.29** | .30** | −.28** | |
| FACT | 1.00 | .42** | .44** | .36** | .47** | .50** | −.24** | .26** | −.27** | ||
| LIS | 1.00 | .55** | .34** | .36** | .62** | −.05 | .32** | −.17* | |||
| TOFHLA Reading |
1.00 | .53** | .72** | .51** | −.31** | .39** | −.32** | ||||
| TOFHLA Numeracy |
1.00 | .47** | .31** | −.25** | .25** | −.31** | |||||
| REALMb | 1.00 | n/ab | −.34** | .22** | −.30** | ||||||
| SAHLSAb | 1.00 | .20* | .19* | −.30* | |||||||
| Hospitalc | 1.00 | −.33** | .52** | ||||||||
| Formsc | 1.00 | −.32** | |||||||||
| Infoc | 1.00 |
Correlation p < 0.01;
Correlation p < 0.001.
Five items on the FACT scale are also included in the HL scale, increasing scale intercorrelations.
The REALM was only administered to English speakers (n = 236), and the SAHLSA was only administered to Spanish speakers (n = 239).
Hospital = Need help reading hospital materials; Forms = Confident in filling out medical forms; Info= Difficulty in understanding written medical information
Correlations of FLIGHT/VIDAS with a measure of health-related quality of life and health utility (SF-36 scales and the EQ-5D) are presented in Table 4. This table includes participants’ total TOFHLA score to allow comparisons. The FLIGHT/VIDAS scales were correlated at low to moderate[34] levels with several SF-36 scales, including General Health, Physical Functioning, Social Functioning, and Emotional Wellbeing. All scales of FLIGHT/VIDAS were significantly correlated with the health utility index, the EQ-5D.
Table 4. Correlations of health literacy measures with SF-36 and EQ-5D.
| HL | NUM | FACT | LIS | TOFHLA Total |
SF Phys Funca |
SF Limit Phys Funca |
SF Limit Emot Probsa |
SF Energy/ Fatigue |
SF Emotional Wellbeing |
SF Social Function |
SF Pain |
SF General Health |
EQ-5D | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HL | 1.00 | .82** | .72** | .65** | .69** | .27** | −0.08 | −.11* | 0.07 | .22** | .17** | .12** | .14** | .26** |
| NUM | 1.00 | .53** | .57** | .63** | .24** | −0.07 | −0.08 | 0.01 | .15** | .18** | .13** | .10* | .23** | |
| FACT | 1.00 | .42** | .46** | 0.08 | 0.01 | −0.09 | 0.06 | .18** | .13** | 0.05 | .11* | .11* | ||
| LIS | 1.00 | .53** | .21** | −0.07 | −.11* | 0.03 | .14** | .13** | 0.09 | 0.04 | .18** | |||
| TOFHLA Total | 1.00 | .25** | −0.09 | −0.07 | 0.02 | .14** | .10* | 0.05 | .13** | .19** | ||||
| SF Phys Funca | 1.00 | −.63** | −.31** | .45** | .25** | .39** | .61** | .45** | .87** | |||||
| SF Limit Phys Funca | 1.00 | .31** | −.46** | −.29** | −.49** | −.62** | −.43** | −.71** | ||||||
| SF Limit Emot Probsa | 1.00 | −.48** | −.61** | −.61** | −.34** | −.37** | −.49** | |||||||
| SF Energy/Fatigue | 1.00 | .64** | .59** | .53** | .63** | .64** | ||||||||
| SF Emotional Wellbeing |
1.00 | .65** | .34** | .47** | .56** | |||||||||
| SF Social Function |
1.00 | .50** | .51** | .67** | ||||||||||
| SF Pain | 1.00 | .49** | .86** | |||||||||||
| SF General Health |
1.00 | .62** | ||||||||||||
| EQ 5D | 1.00 |
HL = FLIGHT/VIDAS General Health Literacy; NUM = FLIGHT/VIDAS Numeracy; FACT = FLIGHT/VIDAS Conceptual Knowledge; LIS = FLIGHT/VIDAS Listening; SF Phys Func = SF-36 Physical Function; SF Limit Phys Func = SF-36 Role limitations due to physical health; SF Limit Emot Probs = SF-36 Role limitations due to emotional problems
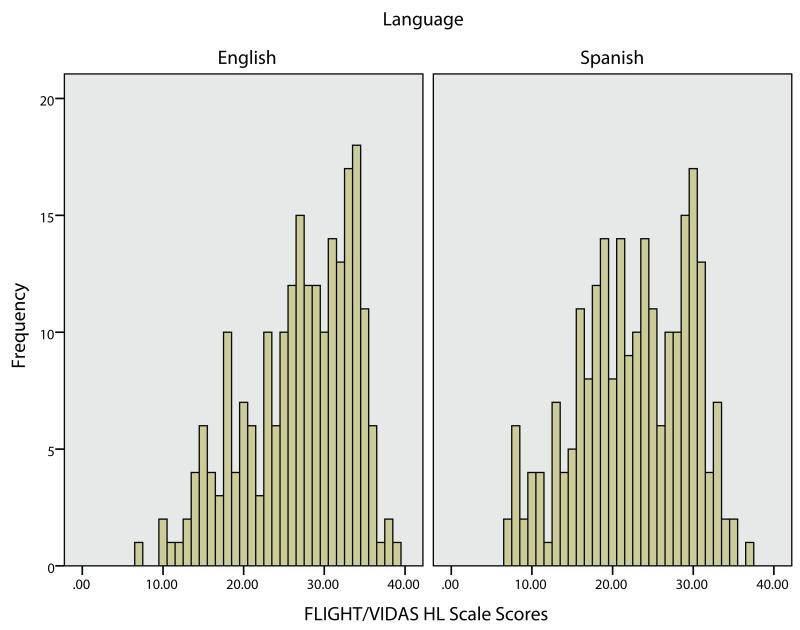
3.4 Range of scores
Most available measures of health literacy show pronounced ceiling effects when used in the general population, limiting their use in evaluating health literacy in nonpatients groups. A specific focus of FLIGHT/VIDAS development was to ensure that items with difficulties of sufficient difficulty were created that would be challenging even for well-educated participants. Figure 1 presents a histogram of HL scale scores for English and Spanish-speaking participants. It can be seen that the range of scores on HL is substantial and includes a number of cases at the lower and higher ends of the range. Scores on HL ranged from 7 to 39 (of 40), on NUM from 0 to 24 (of 24), FACT from 0 to 14 (of 14), and LIS from 3 to 12 (of 12). Ranges for the two language groups were similar.
Figure 1.
Distribution of FLIGHT/VIDAS HL scale scores
3.5 Levels of health literacy, health status, and service utilization
Analysis of covariance (ANCOVA) models assessed differences health status and utilization variables across groups defined by scores on the HL scale of FLIGHT/VIDAS. Models included age, gender, race, education, and language as covariates in order to take these possible confounders into account. Groups were established at the cut points for the 33rd and 66th percentile of scores, resulting in a group with low (n = 131), intermediate (n = 134), and high (n = 157) levels of health literacy. ANCOVA models are presented in Table 5. Those with the highest levels of health literacy reported fewer conditions and symptoms, less frequent use of medications and fewer doctor visits.
Table 5. Health status and healthcare utilization for health literacy groups.
| Mean (SD) for Tertile of Health Literacy | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| Variable | Low | Intermediate | High | df | F | P |
| Conditions | 3.6 (3.4) | 2.8 (2.9) | 2.4 (2.4) | 2,414 | 3.01 | 0.050 |
| Symptoms | 15.5 (10.3) | 13.4 (9.6) | 10.1 (8.0) | 2,370 | 6.64 | 0.001 |
| Medications | 1.7 (1.7) | 1.3 (1.6) | 1.0 (1.2) | 2,420 | 3.78 | 0.02 |
| Doctor Visits |
11.5 (17.9) | 10.8 (19.6) | 7.0 (7.3) | 2,381 | 3.32 | 0.04 |
4. Discussion and Conclusion
4.1 Discussion
This paper reports on the relation of a new measure of health literacy, FLIGHT/VIDAS, to other measures of health literacy and to a measure of health-related quality of life. We also evaluated the relation of level of health literacy as assessed by the scale to health status and health care service utilization. Analyses show that FLIGHT/VIDAS scales are correlated significantly with established measures of health literacy and a well-known measure of health-related quality of life. Persons with varying levels of health literacy as assessed by the FLIGHT/VIDAS show significant differences in health status and health service utilization.
We had previously provided a preliminary report of the relations of the FLIGHT/VIDAS scales to other measures with analyses based on a much smaller interim sample.[19] This paper supplements this earlier report with analyses using the final full sample of participants. The core scales (HL and NUM) of FLIGHT/VIDAS have excellent reliability and significant correlations with established tests of health literacy and with participant self-report of difficulties in reading health-related materials, showing that it is likely to be a valid measure of health literacy. Their range of scores shows that the scales may be useful across a number of ability levels, potentially making FLIGHT/VIDAS more useful for research on health literacy in the general population than other measure that show marked ceiling effects.
Two other FLIGHT/VIDAS scales, FACT (general health knowledge) and LIS (listening comprehension) are face valid based on their content (basic health facts for the FACT scale) or administration format (responses to questions about the content presented in several audiovisual vignettes for the LIS scale). They also are correlated significantly with other health literacy measures (Table 3) and health status variables (Table 4). Their internal consistency reliabilities (Cronbach’s alpha), however, are lower than generally considered desirable for psychometric measures. We believe that this may be the result of the diverse content included in each scale. Because of their potential usefulness, we include them in this presentation but caution that they should be considered experimental scales. We plan to continue their development in order to improve their psychometric characteristics.
The purpose of this paper has also been to go beyond solely demonstrating the new measure’s relation to established scales and to relate performance on it to meaningful clinical status and utilization variables such as health-related quality of life, use of healthcare services, and health utility. Results show that performance on FLIGHT/VIDAS is related in small to moderately large ways to multiple aspects of health related quality of life. Results show that participants with the highest levels of health literacy report fewer health conditions, fewer and less frequent symptoms, less medication use and fewer doctor visits.
The guiding principles in creating FLIGHT/VIDAS were to create a new measure that addressed limitations of existing measures and was computer administered and scored. One important limitation has been that some measures have not been demonstrated to have relations to variables in addition to other measures of health literacy. Exceptions include the TOFHLA, which has been related to cognitive function, quality of life, and health utilization. The TOFHLA, however, focuses on a narrow range of content, relies on the cloze procedure to assess reading comprehension, and must be hand administered and scored. While it is effective for detecting persons with low health literacy it suffers from substantial ceiling effects when used in other populations. FLIGHT/VIDAS addresses these issues. It includes diverse content ranging from reading pill bottle labels to understanding health promotion messages. It does not rely on the cloze procedure which may be more difficult for older compared to younger persons [17]. It can be administered and scored with little or no clinician intervention, and has a wide range of scores in a normal population.
Data presented here demonstrate that FLIGHT/VIDAS performance is related to meaningful variables such as health-related quality of life and use of health services suggesting that it may be a useful addition to current measures in clinical practice and in research. Given its range of health-related content and wide range of scores in the general population, FLIGHT/VIDAS may be useful in research studies examining the impact of individuals’ health literacy on the interactions with organizations that themselves have varying levels of health literacy [35,36] and in better understanding health literacy as a social construct [16,37].
4.2 Conclusion
The new measure of health literacy, FLIGHT/VIDAS, is computer-administered and scored and shows evidence of excellent reliability and significant relations to better-established measures of health literacy. It includes content not only related to tasks such as taking medications or understanding disease but also to information search, health promotion activities, and critical evaluation of health information. Given its potential broader use in nonclinical populations, it may be a useful addition to research on health literacy. As it is computer administered and scored, it may also be a useful addition to clinical practice, making information on patients’ health literacy more readily available for use by clinicians. We plan to support its dissemination by making it available for use online and by providing a standard manual for administration that will include preliminary norms.
4.3 Practice Implications
FLIGHT/VIDAS may be a useful addition to existing measures of health literacy. It addresses several limitations of other tests of health literacy and can be administered in an automated fashion. A disadvantage of the measure is that it requires computer equipment for use. Advantages include the broad content assessed, the wide range of scores in the general population, its clear relation not only to existing measures but also to clinically meaningful health status and utilization, and its availability in English and Spanish. FLIGHT/VIDAS may thus be useful for research and clinical practice in contexts in which its can be administered and its length is not prohibitive. It may be especially advantageous for research on health literacy in the general population and among persons with average to above average educational backgrounds where existing tests show ceiling effects.
Acknowledgments
The study described in this paper was supported by grant R01HL096578 to Dr. Ownby from the National Heart, Lung, and Blood Institute.
Supported by grant R01HL096578 from the National Heart, Lung, and Blood Institute to Dr. Ownby.
Footnotes
Conflict of interest
All authors state that they have no conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- [1].Nielsen-Bohlman L, Panzer AM, Kindig DA. Health literacy: A prescription to end confusion. National Academies Press; Washington DC: 2004. [PubMed] [Google Scholar]
- [2].Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011 Jul 19;155(2):97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- [3].Bostock S, Steptoe A. Association between low functional health literacy and mortality in older adults: longitudinal cohort study. BMJ. 2012;344:e1602. doi: 10.1136/bmj.e1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Dewalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes: a systematic review of the literature. J Gen Intern Med. 2004 Dec;19(12):1228–39. doi: 10.1111/j.1525-1497.2004.40153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Sudore RL, Yaffe K, Satterfield S, Harris TB, Mehta KM, Simonsick EM, et al. Limited literacy and mortality in the elderly: the health, aging, and body composition study. J Gen Intern Med. 2006 Aug;21(8):806–12. doi: 10.1111/j.1525-1497.2006.00539.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Ownby RL, Waldrop-Valverde D, Jacobs RJ, Caballero J. Baseline medication adherence and response to an electronically-delivered health literacy intervention targeting adherence. Neurobehavioral HIV Medicine. 2012;4:113–21. doi: 10.2147/NBHIV.S36549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Sheridan SL, Halpern DJ, Viera AJ, Berkman ND, Donahue KE, Crotty K. Interventions for individuals with low health literacy: a systematic review. J Health Commun. 2011 Sep 27;16(Suppl 3):30–54. doi: 10.1080/10810730.2011.604391. [DOI] [PubMed] [Google Scholar]
- [8].Osborn CY, Cavanaugh K, Wallston KA, Kripalani S, Elasy TA, Rothman RL, et al. Health literacy explains racial disparities in diabetes medication adherence. J Health Commun. 2011;16(Suppl 3):268–78. doi: 10.1080/10810730.2011.604388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Waldrop-Valverde D, Osborn CY, Rodriguez A, Rothman RL, Kumar M, Jones DL. Numeracy skills explain racial differences in HIV medication management. AIDS Behav. 2010 Aug;14(4):799–806. doi: 10.1007/s10461-009-9604-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Parker RM, Baker DW, Williams MV, Nurss JR. The Test of Functional Health Literacy in Adults: A new instrument for measuring patients’ literacy skills. J Gen Intern Med. 1995 Oct;10(10):537–41. doi: 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- [11].Murphy PW, Davis TC, Long SW, Jackson RH, Decker BC. Rapid Estimate of Adult Literacy in Medicine (REALM): A quick reading test for patients. Journal of Reading. 1993;37:124–30. [Google Scholar]
- [12].Weiss BD, Mays MZ, Martz W, Castro KM, Dewalt DA, Pignone MP, et al. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. 2005 Nov;3(6):514–22. doi: 10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Baker DW. The meaning and the measure of health literacy. J Gen Intern Med. 2006 Aug;21(8):878–83. doi: 10.1111/j.1525-1497.2006.00540.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Pleasant A, McKinney J. Coming to consensus on health literacy measurement: an online discussion and consensus-gauging process. Nurs Outlook. 2011 Mar;59(2):95–106. doi: 10.1016/j.outlook.2010.12.006. [DOI] [PubMed] [Google Scholar]
- [15].Jordan JE, Osborne RH, Buchbinder R. Critical appraisal of health literacy indices revealed variable underlying constructs, narrow content and psychometric weaknesses. J Clin Epidemiol. 2011 Apr;64(4):366–79. doi: 10.1016/j.jclinepi.2010.04.005. [DOI] [PubMed] [Google Scholar]
- [16].Pleasant A. Health literacy. In: Horning-Priest S, editor. Encyclopedia of Science and Technology Communication. Sage; Thousand Oaks, CA: 2010. pp. 353–60. [Google Scholar]
- [17].Ownby RL, Waldrop-Valverde D. Differential item functioning related to age in the Reading subtest of the Test of Functional Health Literacy in Adults. Journal of Aging Research. 2013;2013:1–6. doi: 10.1155/2013/654589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Jerant A, Sohler N, Fiscella K, Franks B, Franks P. Tailored interactive multimedia computer programs to reduce health disparities: opportunities and challenges. Patient Educ Couns. 2011 Nov;85(2):323–30. doi: 10.1016/j.pec.2010.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Ownby RL, Acevedo A, Waldrop-Valverde D, Jacobs RJ, Homs AM, Czaja SJ, et al. Development and initial validation of a computer-administered health literacy assessment in Spanish and English: FLIGHT/VIDAS. Patient Related Outcome Measures. 2013 Aug 19;4:1–15. doi: 10.2147/PROM.S48384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Aguirre AC, Ebrahim N, Shea JA. Performance of the English and Spanish S-TOFHLA among publicly insured Medicaid and Medicare patients. Patient Educ Couns. 2005 Mar;56(3):332–9. doi: 10.1016/j.pec.2004.03.007. [DOI] [PubMed] [Google Scholar]
- [21].Ownby RL, Acevedo A, Waldrop-Valverde D, Jacobs RJ, Caballero J. A new computer-administered measure of health literacy: Validity and relation to quality of life in Spanish and English speakers; Paper presented at the International Conference on Communication in Healthcare; Montreal. October. 2013. [Google Scholar]
- [22].Chew LD, Griffin JM, Partin MR, Noorbaloochi S, Grill JP, Snyder A, et al. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med. 2008 May;23(5):561–6. doi: 10.1007/s11606-008-0520-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Ryff C, Almeida DM, Ayanian JS, Carr DS, Cleary PD, Coe C, et al. National Survey of Midlife Development in the United States (MIDUS II), 2004-2006. Inter-university Consortium for Political and Social Research (ICPSR); Ann Arbor, MI: 2012. [Google Scholar]
- [24].Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):478–83. [PubMed] [Google Scholar]
- [25].Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- [26].Ara R, Brazier J. Deriving an algorithm to convert the eight mean SF-36 dimension scores into a mean EQ-5D preference-based score from published studies (where patient level data are not available) Value Health. 2008 Dec;11(7):1131–43. doi: 10.1111/j.1524-4733.2008.00352.x. [DOI] [PubMed] [Google Scholar]
- [27].Aggarwal R, Wilke CT, Pickard AS, Vats V, Mikolaitis R, Fogg L, et al. Psychometric properties of the EuroQol-5D and Short Form-6D in patients with systemic lupus erythematosus. J Rheumatol. 2009 Jun;36(6):1209–16. doi: 10.3899/jrheum.081022. [DOI] [PubMed] [Google Scholar]
- [28].Pickard AS, Wilke CT, Lin HW, Lloyd A. Health utilities using the EQ-5D in studies of cancer. Pharmacoeconomics. 2007;25(5):365–84. doi: 10.2165/00019053-200725050-00002. [DOI] [PubMed] [Google Scholar]
- [29].Pickard AS, Wilke C, Jung E, Patel S, Stavem K, Lee TA. Use of a preference-based measure of health (EQ-5D) in COPD and asthma. Respir Med. 2008 Apr;102(4):519–36. doi: 10.1016/j.rmed.2007.11.016. [DOI] [PubMed] [Google Scholar]
- [30].Brazier J, Roberts J, Tsuchiya A, Busschbach J. A comparison of the EQ-5D and SF-6D across seven patient groups. Health Econ. 2004 Sep;13(9):873–84. doi: 10.1002/hec.866. [DOI] [PubMed] [Google Scholar]
- [31].Luo N, Johnson JA, Shaw JW, Coons SJ. Relative efficiency of the EQ-5D, HUI2, and HUI3 index scores in measuring health burden of chronic medical conditions in a population health survey in the United States. Med Care. 2009 Jan;47(1):53–60. doi: 10.1097/MLR.0b013e31817d92f8. [DOI] [PubMed] [Google Scholar]
- [32].Luo N, Johnson JA, Shaw JW, Feeny D, Coons SJ. Self-reported health status of the general adult U.S. population as assessed by the EQ-5D and Health Utilities Index. Med Care. 2005 Nov;43(11):1078–86. doi: 10.1097/01.mlr.0000182493.57090.c1. [DOI] [PubMed] [Google Scholar]
- [33].Ennis SR, Rios-Vargas M, Albert NG. The Hispanic population: 2010. US Department of Commerce, US Census Bureau; Washington, DC: 2011. [Google Scholar]
- [34].Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Routledge; New York: 1988. [Google Scholar]
- [35].Baur C. New directions in research on public health and health literacy. J Health Commun. 2010;15(Suppl 2):42–50. doi: 10.1080/10810730.2010.499989. [DOI] [PubMed] [Google Scholar]
- [36].Brach C, Dreyer B, Schyve P, Hernandez LM, Baur C, Lemerise AJ, et al. Attributes of a health literate organization [Discussion paper] Institute of Medicine; Washington DC: 2012. [Google Scholar]
- [37].Pleasant A, McKinney J, Rikard RV. Health literacy measurement: a proposed research agenda. J Health Commun. 2011;16(Suppl 3):11–21. doi: 10.1080/10810730.2011.604392. [DOI] [PubMed] [Google Scholar]