Abstract
Objective
To test the efficacy of a weight loss intervention designed to appeal to men.
Design and methods
A randomized trial tested the efficacy of the REFIT (Rethinking Eating and FITness) weight loss program compared to a waitlist control. The six-month intervention was delivered via two face-to-face sessions followed by Internet contacts. REFIT encouraged participants to create calorie deficits by making six 100-calorie changes to their eating daily while increasing physical activity and the program encouraged customization through selection of specific diet strategies evaluated each week.
Results
Participants (N=107, 44.2 years, 31.4 kg/m2, 76.6% white) were randomized into the study and 90.6% provided data at six months. REFIT participants lost -5.0 kg (95% CI: -6.1, -3.9) at three months, which was maintained through six months (-5.3 kg, 95% CI: -6.5, -4.2); this was greater than the control group (p<0.001; 6-month: -0.6, 95% CI: -1.8, 0.5). More REFIT participants (49%) achieved a 5% weight loss than control participants (19%; OR 9.4; 95% CI: 3.2, 27.4). An average of 11.2 (±2.7) of 13 of the online intervention contacts were completed.
Conclusions
The novel REFIT intervention produced clinically significant weight losses. This approach holds promise as an alternative to traditional behavioral therapy for men.
Keywords: men, weight loss, behavioral therapy
Introduction
Recent estimates suggest that men and women have near equal rates of combined overweight and obesity [1]. Behavioral interventions for weight control have been developed that produce weight losses of approximately 5-10% of initial body weight and improve multiple health outcomes [2]. However, several reviews have shown that men represent only approximately 27% of study samples [3-6]. In order to help men reduce the negative consequences of obesity, it is important to better involve men in behavioral weight loss interventions.
A recent review suggests that men can lose weight when they participate in weight loss programs [7], indicating that men are not likely to be avoiding participation due to lack of success. Instead, it is hypothesized that a mismatch between men's preferences for weight loss programs and the programs that are currently available is contributing to the low participation rates. Men have indicated that they view weight loss as a feminine activity [8-10] and perceive weight loss programs as targeted at women [10]. Men report wanting individually focused programs that do not include strict meal plans and provide the ability to tailor the diet to their preferences. Additionally, they prefer programs that do not disrupt their daily routine and provide information in a clear and direct manner [8, 9, 11-13].
One approach that has been used to meet men's preferences for weight loss programs has been to use lower intensity, self-directed programs. While this approach has been efficacious in some studies [14-17], other studies did not observe weight losses greater than the control group [18]. Another approach that has been used has been to deliver programs via the Internet (e.g., [19]) in order to minimize the potential for lifestyle disruptions caused by programs delivered via face-to-face sessions.
The purpose of this study was to test a multicomponent weight loss program designed to appeal to men, featuring novel (modest caloric-restriction via 100-calorie reductions, self-tailored calorie-reduction strategy order, simplified self-monitoring,) and established (physical activity progression, tailored feedback) treatment components. The primarily Internet-delivered Rethinking Eating and FITness (REFIT) program was tested in a randomized controlled trial compared to a wait-list control group over six months. The primary outcome was change in weight with secondary outcomes of change in waist circumference, body fat, caloric intake, and leisure-time physical activity.
Methods
Participants and Recruitment
Participants were recruited via emails sent to the university community and local worksites, flyers distributed in surrounding communities, and word of mouth between July 2013 and March 2014. Men were required to be 18-65 years of age, have a body mass index (BMI) 25-40 kg/m2, have regular access to the Internet, and be able exercise safely [20]. Men were excluded if they reported high alcohol intake [21], major psychiatric conditions, weight loss > 10 pounds over the past six months, current treatment for cancer, or if they were unable/unwilling to attend group sessions. Participants who reported diagnoses of high blood pressure, high cholesterol, or diabetes, history of cancer, or any joint problems were required to obtain consent from their physician.
Procedure
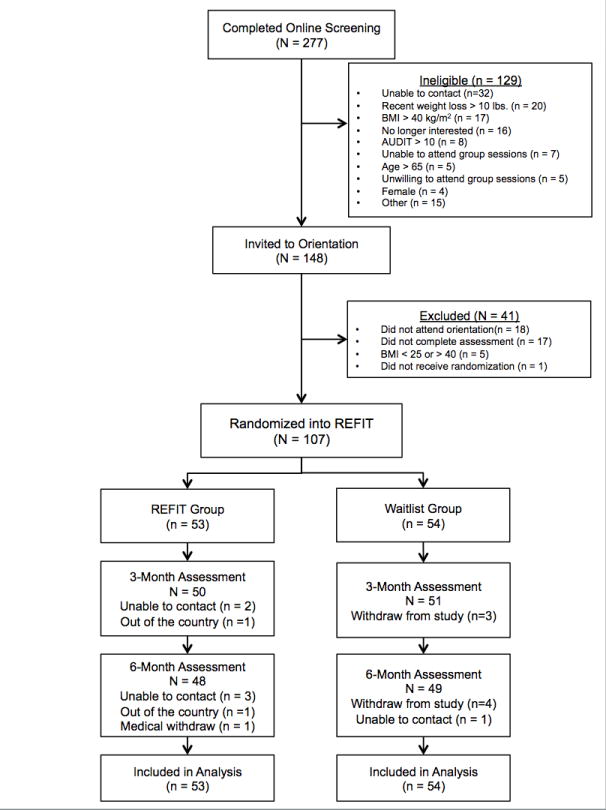
Two hundred seventy-seven individuals completed the online eligibility screener (Figure 1). Those who were initially eligible were contacted via telephone to complete the screening process and schedule an orientation session. At orientation, participants provided informed consent and scheduled their baseline assessment visit. Randomization occurred after baseline assessments and was revealed to participants during a face-to-face group session. Randomization was conducted using Excel's random number generator in a 1:1 ratio.
Figure 1. CONSORT Diagram.
Follow-up assessments were conducted at three and six months post-randomization. The first author, who was unblinded to participant randomization, conducted assessments. After completing each follow-up assessment, all participants received $20 and feedback reports including their anthropometric measurements and a summary of their diet. The University of North Carolina at Chapel Hill Institutional Review Board approved this study.
Intervention Description
The REFIT intervention targeted constructs from social cognitive theory [22] and self-determination theory [23] and focused on promoting autonomy to enhance its appeal to men. Table 1 describes the constructs targeted by the intervention. Recommendations were provided for changing diet, physical activity, and self-monitoring behaviors and was delivered via two one-hour, face-to-face group sessions followed by interactive online intervention contacts weekly for 10 weeks and monthly online contact for three months. Intervention materials were developed and delivered by a doctorate-level public health trainee.
Table 1. Intervention Components and Theory Constructs.
| Theory Construct | Intervention Component |
|---|---|
| Self-efficacy |
|
| Autonomous Motivation |
|
| Outcome Expectancies |
|
| Self-Regulation |
|
Diet recommendations and tailored lesson selection
The REFIT program utilized a novel approach to achieving a modest caloric deficit and allowed participants to self-tailor the order of calorie-reduction strategies and associated lessons. Participants were encouraged to create a modest calorie deficit by making a minimum of six 100-calorie changes from typical eating habits each day (approximately 4200 calories per week). Participants self-tailored the order of specific diet strategies to focus on each week and received a brief online lesson on how to implement the strategy. For example, reducing dietary fat was included as strategy which encouraged replacing high-fat/high-calorie foods with lower fat foods with fewer calories. Reducing portion size was a strategy presented as a way to choose the foods participants preferred while reducing typical consumption. The lessons integrated behavioral techniques included in traditional weight loss programs [e.g., problem solving; 24, 25]. Strategies and lessons later in the program focused on lifestyle changes that have demonstrated effects on weight loss [e.g., water to replace caloric beverages; 26] or weight loss maintenance [e.g., maintaining consistent eating patterns; 27].
Participants selected one strategy and associated lesson per week, which allowed them to independently evaluate the effect of the strategy on their weight loss. If the participant was successful (i.e., participant lost ≥ 1 lb), they had the option to continue using the successful strategy. Participants were presented with three strategies to choose from during their first selection and one new strategy was presented each week; therefore participants had at least three strategies to select from during each online contact. Strategy introduction order was based on potential for impact on calorie balance where higher impact strategies were presented earlier. All lessons focused on diet because during weight loss programs, men have more difficulty implementing changes to their diet than to their physical activity [28].
Physical activity
The REFIT program provided progressive exercise plans with weekly exercise goals increasing to 225 minutes of moderate-to-vigorous physical activity per week [29]. Behavioral strategies for increasing activity were included in the tailored feedback.
Self-monitoring
Participants were encouraged to monitor their diet through tracking the number of 100-calorie changes they made to their eating each day using a checklist paper tracking form recording only the number of changes they made each day. The form included areas to record their minutes of exercise and daily weight. Using detailed self-monitoring was a suggested strategy provided to participants who were consistently not meeting the weight loss goal. Daily self-weighing was presented as a form of self-regulation where participants could use the daily weights as objective feedback on their behaviors [30-32].
Intervention Procedure
Prior to making changes, participants completed a one-week self-evaluation, which occurred between two face-to-face group sessions. Participants used detailed self-monitoring (i.e., recording all calories and grams of fat eaten and all physical activity) and daily self-weighing to identify behaviors they were interested in changing. Participants could choose to monitor using provided paper diaries or a mobile application or website. After the self-evaluation, participants were provided personalized estimates for calorie needs to lose approximately one and two pounds per week (1,200 to 3,308 calories) [33]. The estimates were provided for reference only and participants were not instructed to continue tracking their daily calories.
After the two face-to-face sessions, intervention contact was delivered online through asynchronous interactive online contacts (Qualtrics survey). Participants reported their weight, physical activity, number of daily changes to diet, and days of self-weighing. Automated, tailored feedback was provided based on meeting or not meeting their physical activity goal, days of daily weighing (5 or more), their weight loss (≥1 pound) and the number of changes made to eating (≥ 42 changes per week). Participants selected their next strategy and created a SMART goal related to diet or exercise to accomplish over the next week. This process was completed in approximately 15-30 minutes. A reminder to complete the contact was sent midweek and a new strategy lesson was emailed if a participant did not complete the contact by week's end. If a participant did not complete online contact for two consecutive weeks, they were contacted via telephone.
Wait-list condition
Participants randomized to the waitlist condition attended one group session to receive their randomization assignment. They received a feedback report, which included a summary of their baseline measures, but no treatment recommendations were provided. After the six-month assessments, participants were offered one group session and 10 weeks of the online program.
Outcome measures
Demographic information
Demographic information including race, age, employment status, and marital status were obtained at baseline.
Anthropometrics
Weight was measured to the nearest 0.1 kg on a calibrated digital scale (Tanita BWB 800). Waist circumference was measured at the iliac crest using a flexible tape measure (Gulick II) to the nearest 0.1 cm. Height was measured to the nearest 0.1 cm using a wall-mounted stadiometer (baseline only). Measures were assessed twice for consistency. Body composition was assessed using air displacement plethysmography (Bod Pod, Cosmed).
Dietary Intake
Dietary intake was measured using the National Cancer Institute's Automated Self-Administered 24-hour Recall (version 2011). Participants completed two recalls at each assessment (weekday and weekend). Recalls outside the probable range for a single day intake for an adult man (650-5,700 calories) were removed (Baseline: n = 2, 3M: n = 3, 6M: n = 0).
Physical activity
Physical activity was measured using the Paffenbarger Activity Questionnaire [34]. This questionnaire assesses walking for exercise and transportation, flights of stairs climbed, and leisure-time physical activity (classified using the metabolic equivalents from the Compendium of Physical Activities [35]).
Program utilization and evaluation
Completion of online contacts and selection of strategies were collected automatically through the online system. At each assessment, participants were asked how frequently they weighed themselves on a seven point scale [31, 36].
During the six-month assessment, REFIT group participants were asked how frequently they used strategies recommended including: made 100-calorie changes to their diet, used the study tracking sheet, tracked their intake using an application/website, or recorded their exercise. These were reported on a five-point scale ranging from 1 “Never or hardly ever” to 5 “always or almost always.” They rated their satisfaction with the program and how likely they were to recommend the program to other men on a four-point scale. Finally, they rated their confidence they were that they would be able to continue using the approach recommended by the program on an eight-point scale [37].
Statistical analyses
An a priori power analysis estimated that 104 participants were needed to detect a 2.0 kg difference between treatment groups [15, 16, 18], assuming a 15% attrition rate (80% power and p = 0.025, adjusting for multiple comparisons at three and six months).
Data were analyzed using SAS 9.3. Differences between groups at baseline and between study completers and non-completers were tested using t-test and chi-square analyses. Changes in primary and secondary outcomes were tested in intent-to-treat analyses (N = 107) using linear mixed model analyses with multiple imputations to account for missing data. PROC MI was used to develop five datasets with data imputed for missing values using the Markov chain Monte Carlo procedure. Mean centered values for marital status and full-time employment were included as covariates in all models. Predictors of weight loss were assessed using Spearman's correlations.
Results
Baseline demographic characteristics are presented in Table 2. There were no differences between treatment groups (p's > 0.05). The majority of participants returned for the three-month (94.4%) and six-month (90.7%) assessments, with no difference in completion rates by treatment group (p's = 0.98). While not significant, participants who did not return for the follow-up assessment at three months were less likely to be married than those who returned (50.0% vs. 81.2%, p = .07). At six-month assessments, dropouts were less likely to be employed fulltime (70.0% vs. 90.1%, p = 0.05). Dropouts did not otherwise differ from those who participated in the assessments (p's ≥ 0.13).
Table 2. Baseline Sample Characteristics: mean ± SD or N (%).
| REFIT | Waitlist | p-value (between groups) | |
|---|---|---|---|
| N | 53 | 54 | |
| Age | 44.7 ± 11.3 | 43.7 ± 11.6 | 0.63 |
| Race/ethnicity | 0.19 | ||
| White | 44 (83%) | 38 (70%) | |
| Black | 5 (9%) | 12 (22%) | |
| Other | 4 (8%) | 4 (7%) | |
| Marital Status | 0.67 | ||
| Married, living with partner | 43 (81%) | 42 (78%) | |
| Not married | 10 (19%) | 12 (22%) | |
| Education | 0.64 | ||
| High school, vocational training, or partial college | 8 (15%) | 10 (19%) | |
| College graduate or more | 45 (85%) | 44 (81%) | |
| Employed full-time | 48 (91%) | 47 (87%) | 0.56 |
| Weight (kg) | 99.6 ± 14.3 | 99.9 ± 14.8 | 0.91 |
| BMI (kg/m2) | 31.4 ± 3.9 | 31.5 ± 4.0 | 0.96 |
| Waist (cm) | 109.0 ±10.2 | 108.5 ± 10.4 | 0.80 |
| Percent body fat | 34.5 ± 6.1 | 34.1 ±6.3 | 0.74 |
Weight loss and secondary outcomes
Table 3 shows changes between baseline and three or six months for anthropomorphic values, intake, and exercise. Weight loss was significantly greater in the REFIT group as compared to the waitlist group at both three and six months (p's < 0.001; see Figure 2). There were greater reductions in the REFIT group in waist circumference and percent body fat at both time points (p's < 0.001). More REFIT participants achieved a 5% weight loss (49.1%) than the waitlist group (9.3%, Odds ratio 9.4; 95% CI: 3.2, 27.4).
Table 3. Weight, Body Composition, and Behavior Outcomes by Treatment Group.
| Assessment Perioda | Time | p-valueb | Group × Time | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline | 3 month | 6 month | |||||||
| 3 mo. vs. BL | 6 mo. vs. BL | Group | 3 mo. | 6 mo. | |||||
| Weight (kg) | |||||||||
| REFIT | 99.5 (95.7, 103.3) | 94.5 (90.7, 98.3) | 94.2 (90.3, 98.0) | <.001 | <.001 | 0.85 | <.001 | <.001 | |
| Waitlist | 100.0 (96.2, 103.8) | 99.4 (95.6, 103.2) | 99.4 (95.6, 103.3) | 0.28 | 0.30 | ||||
| Percent weight loss | |||||||||
| REFIT | Ref | -4.9 (-5.9, -4.0) | -5.2 (-6.2, -4.2) | <.001 | <.001 | 0.96 | <.001 | <.001 | |
| Waitlist | Ref | -0.6 (-1.5, 0.4) | -0.6 (-1.6, 0.4) | 0.31 | 0.28 | ||||
| Waist Circumference (cm) | |||||||||
| REFIT | 108.7 (106.1, 111.8) | 104.7 (101.0, 108.3) | 103.8 (100.1, 107.6) | <.001 | <.001 | 0.92 | <.001 | <.001 | |
| Waitlist | 108.5 (105.0, 112.0) | 107.7 (104.1, 111.2) | 107.4 (103.8, 110.9) | 0.09 | 0.02 | ||||
| Percent Body Fat | |||||||||
| REFIT | 34.5 (32.7, 36.2) | 31.4 (29.7, 33.2) | 30.3 (28.5, 32.1) | <.001 | <.001 | 0.80 | <.001 | <.001 | |
| Waitlist | 34.1 (32.4, 35.9) | 33.7 (32.0, 35.5) | 33.1 (31.9, 34.8) | 0.32 | 0.02 | ||||
| Caloric Intake (kcal) | |||||||||
| REFIT | 2334 (2169, 2499) | 1899 (1720, 2078) | 1915 (1740, 2090) | <.001 | <.001 | 0.29 | 0.28 | 0.08 | |
| Waitlist | 2460 (2296, 2623) | 2184 (2013, 2355) | 2291 (2121, 2462) | 0.007 | 0.10 | ||||
| % Calories from Fat | |||||||||
| REFIT | 35.9 (34.1, 37.8) | 35.6 (33.6, 37.7) | 36.5 (34.5, 38.5) | 0.82 | 0.62 | 0.31 | 0.51 | 0.43 | |
| Waitlist | 37.3 (35.4, 39.1) | 35.9 (34.0, 37.9) | 36.6 (34.6, 38.5) | 0.24 | 0.55 | ||||
| Caloric Expenditure (kcal)* | |||||||||
| REFIT | 717.1 (492.5, 983.9) | 1437.6 (1104.8, 1814.1) | 1305.7 (984.9, 1671.7) | <.001 | <.001 | 0.75 | <.001 | .001 | |
| Waitlist | 774.1 (541.8, 1047.7) | 723.6 (495.8, 994.3) | 756 (529.5, 1045.0) | 0.65 | 0.94 | ||||
Note.
Values are model estimated means and 95% confidence intervals
Linear mixed model analysis using five imputed datasets adjusting for marital status and education.
Analysis performed on square root transformed values.
Figure 2.
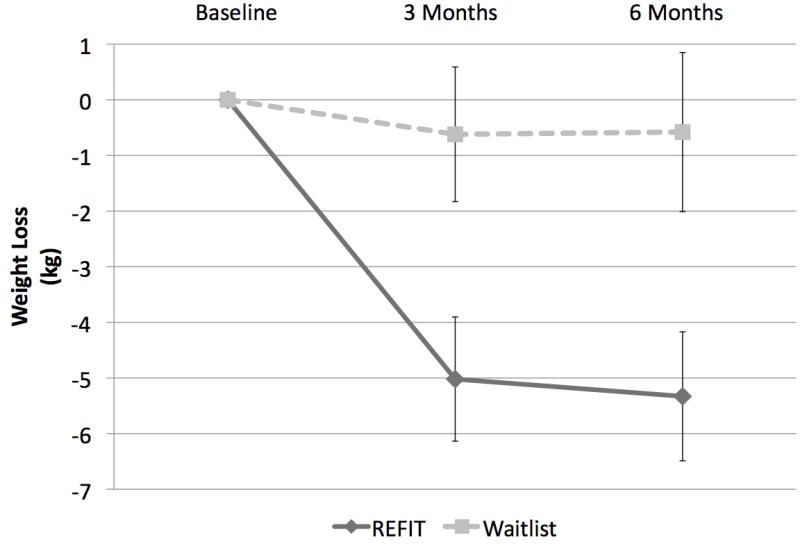
Weight loss by group and time
There were significant increases in physical activity reported by the REFIT group compared to the waitlist group at both follow-up time points (p's ≤ 0.001). There was a significant reduction in caloric intake reported by both groups at three months (group by time difference: p = 0.28). At six months, the difference between groups had increased; however, this between group difference did not reach significance (p = 0.08). Changes in diet between baseline and three and six months were associated with weight loss in the REFIT group (Spearman's r = 0.40, p = 0.01, r = 0.33, p = 0.02; respectively) whereas change in intake was only associated with weight change at six months in the waitlist group (3m: r = 0.01, p = 0.94; 6m: r = 0.33, p = 0.02). Change in physical activity was only associated with weight loss at 6-months in the REFIT group (3m: r = -0.24, p = 0.09; 6m: r = -0.36, p = 0.01; Waitlist 3m: r = 0.10, p = 0.48; 6m: r = -0.17, p = 0.23).
Program utilization
All participants randomized to the REFIT group completed the two face-to-face sessions and completed 11.2 ± 2.7 of the 13 online intervention contacts. Participants reported making 28 ± 16 of the 42 recommended 100-calorie reductions per week during the first 12 weeks of the intervention and reported 224 ± 143 minutes of physical activity during intervention week 12. Table 4 shows the completion rates of each of the contacts and participants' strategy selections. Across all weeks, participants selected the new strategy 50.8% of the time while they self-tailored strategy order by selecting a previously introduced strategy during 30.9% of contacts and reviewing a successful strategy 18.4% of the time. Participants selected an average of 13 (± 3) strategies during the program.
Table 4. Online Intervention Contact Completion Rates and Participant Strategy Selections.
| Program Week | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 15 | 19 | 22 | |
| Complete intervention online contact (n) | -- | 48 | 48 | 48 | 48 | 48 | 51 | 45 | 48 | 47 | 42 | 40 | 39 | 42 |
| Complete intervention online contact (%) | -- | 90.6 | 90.6 | 90.6 | 90.6 | 90.6 | 96.2 | 84.9 | 90.6 | 88.7 | 79.2 | 73.6 | 75.5 | 79.2 |
| Percent eligible to review strategy based on successful weight loss (≥1lb/week) | 81.3 | 81.3 | 87.5 | 72.9 | 85.4 | 72.5 | 68.9 | 75.0 | 68.1 | 66.7 | 77.5 | 76.9 | 57.1 | |
| Participant Strategy Selection (%) | ||||||||||||||
| Review strategy after weight loss | n/a | 27.1 | 12.5 | 18.8 | 18.8 | 29.2 | 21.6 | 11.1 | 29.2 | 17.0 | 11.9 | 17.5 | 10.3 | 14.3 |
| Select previously introduced strategy (self-tailored order) | n/a | 33.3 | 62.5 | 27.1 | 47.9 | 29.2 | 27.5 | 35.6 | 31.3 | 40.4 | 4.8 | 25.0 | 10.3 | 26.2 |
| Select newly introduced strategy (program order) | 100% | 39.6 | 25.0 | 54.2 | 33.3 | 41.7 | 51.0 | 53.3 | 39.6 | 42.6 | 83.3 | 57.5 | 79.5 | 59.5 |
Note. Strategy options in order of introduction fat reduction, reducing calories from beverages, reduce portion sizes (week 2), calories from snacks, calories from meats, using meal-replacements, fast-food, reducing added sugar, restaurant eating, calorie-density, eating during sedentary behavior, meal patterns, water as beverage replacement, eating in social situations, relapse prevention, and maintaining motivation.
During the six-month assessment, REFIT participants (n = 47) were asked how frequently they used the recommended strategies. Sixty-two percent reported that they made 100-calorie changes to their diet “much of the time” or “always or almost always.” Few participants (23.4%) reported tracking these changes using the checklist form while 44.7% reported routinely self-monitoring their diet using a mobile application or website. A greater percentage of participants reported self-weighing daily during the six-month assessment (62.5%) than at baseline (16.7%; p < 0.001).
The number of online contacts completed was associated with weight loss at six months (Spearman's r = -0.37, p = 0.01). Similarly, self-reported frequency of making100-calorie changes to diet (r = -0.54, p < 0.001), using the study-created tracking sheet (r = -0.35, p = 0.02) or a mobile application to track diet (r = -0.37, p = 0.01), and self-weighing (r = -0.36, p = 0.01) were associated with weight loss. Total strategies selected and total strategies reviewed were not associated with weight loss (r = -0.13, p = 0.36; r = -0.05, p = 0.71, respectively). Predictors of achieving a 5% weight loss successful were similar to those of overall weight loss except that both modes of self-monitoring were non-significantly related to weight loss success (tracking sheet p = 0.06; application p = 0.05).
Program satisfaction
REFIT participants positively evaluated the intervention: 91.5% reported that they were satisfied or very satisfied with the program and 95.7% reported they would recommend the program to a friend. On a scale of 1 “not confident” to 8 “very confident,” participants reported feeling confident that they would be able to maintain the changes they made to their eating habits (6.2 ± 1.9) and physical activity (6.3 ± 1.7).
Discussion
This study tested the efficacy of a multicomponent, mainly Internet-delivered weight loss intervention for men with overweight and obesity. This program produced weight losses of approximately 5 kg (5%) at three months, which was maintained during the reduced-contact period through the six-month assessment as compared to a nonsignficant 0.6 kg (0.6%) weight loss in the waitlist comparison group. Nearly 50% of REFIT participants lost 5% of their initial body weight, an amount associated with significant health improvements. In addition to weight losses, there were improvements in waist circumference, percent body fat, and physical activity among REFIT recipients. Moreover, the REFIT program was well utilized and was positively reviewed by recipients.
This study contributes to the limited literature on creating behavioral weight loss programs targeting men. It builds on prior studies where participants were encouraged to change their eating and exercise through following recommendations related to a limited number of diet and physical activity behaviors [14-18]. The focus on a smaller number of behaviors was designed to streamline communication and minimize the time participants spent interacting with the intervention, thus making it appealing to men. Prior studies have differed on the emphasis placed on reducing intake ranging from reducing caloric density of the diet [18] to using traditional monitoring to stay below a calorie goal [14-17]. Given that men in REFIT and in the studies utilizing traditional calorie-reduction strategies achieved clinically meaningful weight losses, continuing to emphasize calorie reduction during weight loss programs with men appears important.
The REFIT program encouraged making changes related to one strategy each week, which was selected because it was hypothesized to be more appealing to men than traditional approaches. Similar approaches have been developed for general populations [e.g., 38, 39, 40]. In these earlier studies, participants selected a single eating and physical activity goal and worked towards meeting this goal until it was achieved. By contrast, the REFIT program encouraged participants to work towards a study-developed goal (i.e., six 100-calorie changes) but allowed the participants to personalize their approach towards reaching this goal via selection of strategies to focus on each week. This unique approach to choice within a weight loss program may be appealing to men and other populations underrepresented in weight loss programs.
Interestingly, and unexpectedly, more participants in the REFIT study reported using a mobile application or website to self-monitor diet than the simplified paper self-monitoring checklist created for this study. Despite this, use of either type of self-monitoring was associated with greater weight loss and there were trends for increased likelihood of achieving a 5% weight loss. Providing options for modes and/or types of self-monitoring may be helpful in improving adherence to this recommended behavior.
Larger between group differences were observed on self-reported changes in physical activity than changes in diet in the current study. However, weight change and behavior change were more strongly associated within the intervention group than within the waitlist group. This suggests that the intervention group may have more accurately recalled their diet and physical activity behaviors or that the days reported were more representative of their usual behaviors than the recalls provided by waitlist participants. Given the challenge of accurately assessing diet and physical activity, it will be important to continue to explore how both aspects of energy balance contribute to the weight losses observed in lower-intensity weight loss programs.
This study contributes to the limited literature on men's weight loss programs however; there are limitations to consider. First, the relatively homogenous study sample is not representative of all men with overweight and obesity; thus, study results may not generalize to other groups. Secondly, this program was implemented and assessed by the same unblinded researcher (MMC). This may have influenced participants and increased their compliance to program recommendations and participation in follow up assessments. Finally, this study utilized a waitlist control group therefore there is no way to test which intervention components were effective.
This study evaluated the effect of a novel weight loss program designed to meet men's weight loss needs in a manner that was appealing to them in a randomized trial with high retention and program utilization rates. Future studies are needed to test the approach used in this program using a more generalizable sample of men in order to understand if the results can be replicated. Additionally, there is a need to test the effects of this approach over a longer time period. Because there was no evidence of weight regain after the weekly sessions ended, the weight loss approach encouraged in this program may be more sustainable than the calorie-counting approach used in more traditional programs.
What is already known about this subject
Men are underrepresented in trials of behavioral approaches to weight loss.
Currently available programs do not include features that would make programs appealing to men.
Few studies have been conducted that combine knowledge from successful behavioral interventions for weight loss with the program features that men seek from weight loss programs.
What this study adds
This study tests the efficacy of a weight loss intervention developed by combining men's preferences for weight loss with strategies believed to produce weight loss.
This intervention uses a multicomponent intervention for weight loss which focuses on reducing calories in multiple 100-calorie increments per day, increasing physical activity, increases personalization and autonomy through participant selected calorie-reduction strategy order, and is primarily Internet delivered.
Results indicate that the approach used in this intervention was successful in producing clinically significant weight loss.
Acknowledgments
The authors are grateful to the study participants and volunteer research assistants Marcus Layer and Lam Chau. The authors thank Kurt Ribisl for serving on MMC's dissertation committee.
Funding: This research was supported by funding provided to M. M. Crane through the Cancer Control Education Program (5R25-CA057726) at Lineberger Comprehensive Cancer Center at The University North Carolina at Chapel Hill and through the Dissertation Completion Fellowship provided by The Graduate School at the University of North Carolina at Chapel Hill.
Footnotes
Disclosure: The authors declare no conflict of interest. Dr. Deborah Tate receives personal fees as a scientific advisor for Weight Watchers International.
Author Contributions: MMC, LDL, DSW, JMB, and DFT contributed to the conception of the protocol and study design. MMC and DFT were involved with the intervention delivery and data collection and analysis. All authors were involved in writing the article and had final approval of the submitted manuscript.
Trial Registration: NCT01843595
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wadden TA, Webb VL, Moran CH, Bailer BA. Lifestyle Modification for Obesity: New developments in diet, physical activity, and behavior therapy. Circulation. 2012;125:1157–1170. doi: 10.1161/CIRCULATIONAHA.111.039453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pagoto SL, Schneider KL, Oleski JL, Luciani JM, Bodenlos JS, Whited MC. Male inclusion in randomized controlled trials of lifestyle weight loss interventions. Obesity. 2011;20:1234–1239. doi: 10.1038/oby.2011.140. [DOI] [PubMed] [Google Scholar]
- 4.Wieland LS, Falzon L, Sciamanna CN, T KJ, Brodney S, Schwartz JE, Davidson KW. Interactive computer-based interventions for weight loss or weight loss maintenance in overweight or obese people. Cochrane Database of Systematic Reviews. 2012;15:CD007675. doi: 10.1002/14651858.CD007675.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Franz MJ, VanWormer JJ, Crain AL, Boucher JL, Histon T, Caplan W, Bowman JD, Pronk NP. Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc. 2007;107:1755–1767. doi: 10.1016/j.jada.2007.07.017. [DOI] [PubMed] [Google Scholar]
- 6.Robertson C, Archibald D, Avenell A, Douglas F, Hoddinott P, van Teijlingen E, Boyers D, Stewart F, Boachie C, Fioratou E, et al. Systematic reviews of and integrated report on the quantitative, qualitative and economic evidence base for the management of obesity in men. Health Technol Assess. 2014;18 doi: 10.3310/hta18350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Williams RL, Wood LG, Collins CE, Callister R. Effectiveness of weight loss interventions- is there a difference between men and women: A systematic review. Obes Rev. 2015;16:171–186. doi: 10.1111/obr.12241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gough B, Conner MT. Barriers to healthy eating amongst men: A qualitative analysis. Soc Sci Med. 2006;62:387–395. doi: 10.1016/j.socscimed.2005.05.032. [DOI] [PubMed] [Google Scholar]
- 9.Sabinsky MS, Toft U, Raben A, Holm L. Overweight men's motivations and perceived barriers towards weight loss. Eur J Clin Nutr. 2007;61:526–531. doi: 10.1038/sj.ejcn.1602537. [DOI] [PubMed] [Google Scholar]
- 10.de Souza P, Ciclitira KE. Men and dieting: A qualitative analysis. Journal of Health Psychology. 2005;10:793–804. doi: 10.1177/1359105305057314. [DOI] [PubMed] [Google Scholar]
- 11.Wolfe BL, Smith JE. Different strokes for different folks: Why overweight men do not seek weight loss treatment. Eating Disorders. 2002;10:115–124. doi: 10.1080/10640260290081687. [DOI] [PubMed] [Google Scholar]
- 12.Egger G, Mowbray G. A qualitative analysis of obesity and at-risk overweight in working men. Australian Journal of Nutrition and Dietetics. 1993;50:10–14. [Google Scholar]
- 13.Morgan PJ, Warren JM, Lubans DR, Collins CE, Callister R. Engaging men in weight loss: Experiences of men who participated in the male only SHED-IT pilot study. Obesity Research & Clinical Practice. 2011;5:e239–c248. doi: 10.1016/j.orcp.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 14.Morgan PJ, Callister R, Collins CE, Plotnikoff RC, Young MD, Berry N, McElduff P, Burrows T, Aguia E, Saunders KL. The SHED-IT community trial: A randomized controlled trial of internet- and paper-based weight loss programs tailored for overweight and obese men. Ann Behav Med. 2013;45:138–152. doi: 10.1007/s12160-012-9424-z. [DOI] [PubMed] [Google Scholar]
- 15.Morgan PJ, Collins CE, Plotnikoff RC, Cook AT, Berthon B, Mitchell S, Callister R. Efficacy of a workplace-based weight loss program for overweight male shift workers: The Workplace POWER (Preventing Obesity Without Eating Like a Rabbit) randomized controlled trial. Prev Med. 2011;52:317–325. doi: 10.1016/j.ypmed.2011.01.031. [DOI] [PubMed] [Google Scholar]
- 16.Morgan PJ, Lubans DR, Collins CE, Warren JM, Callister R. The SHED-IT randomized controlled trial: evaluation of an Internet-based weight-loss program for men. Obesity. 2009;17:2025–2032. doi: 10.1038/oby.2009.85. [DOI] [PubMed] [Google Scholar]
- 17.Morgan PJ, Lubans DR, Collins CE, Warren JM, Callister R. 12-Month outcomes and process evaluation of the SHED-IT RCT: An internet-based weight loss program targeting men. Obesity. 2011;19:142–151. doi: 10.1038/oby.2010.119. [DOI] [PubMed] [Google Scholar]
- 18.Patrick K, Calfas KJ, Norman GJ, Rosenberg D, Zabinski MF, Sallis JF, Rock CL, Dillon LW. Outcomes of a 12-month web-based intervention for overweight and obese men. Annals Behavioral Medicine. 2011;42:391–401. doi: 10.1007/s12160-011-9296-7. [DOI] [PubMed] [Google Scholar]
- 19.Azar KMJ, Aurora M, Wang EJ, Muzaffar A, Pressman A, Palaniappan LP. Vitual small groups for weight managment: An innovative delivery machanism for evidenced-based lifestyle interventions among obese men. Translational Behavioral Medicine. 2015;5:37–44. doi: 10.1007/s13142-014-0296-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thomas S, Reading J, Shephard R. Revision of the Physical Activity Readiness Questionnaire (PAR-Q) Can J Sport Sci. 1992;17:338–345. [PubMed] [Google Scholar]
- 21.Reinert DF, Allen JP. The alcohol use disorders identification test (AUDIT): a review of recent research. Alcoholism: Clinical and Experimental Research. 2002;26:272–279. [PubMed] [Google Scholar]
- 22.Bandura A. Social cognitive theory of self-regulation. Organ Behav Hum Decis Process. 1991;50:248–287. [Google Scholar]
- 23.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55:68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- 24.Diabetes Prevention Program Research Group. The Diabetes Prevention Program (DPP): Description of lifestyle intervention. Diabetes Care. 2002;25:2165–2171. doi: 10.2337/diacare.25.12.2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.The Look AHEAD Research Group. The Look AHEAD Study: A description of the lifestyle intervention and the evidence supporting it. Obesity. 2006;14:737–752. doi: 10.1038/oby.2006.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tate DF, Turner-McGrievy GM, Lyons E, Stevens J, Erickson K, Polzien K, Diamond M, Wang X, Popkin BM. Replacing caloric beverages with water or diet beverages for weight loss in adults: Main results of the Choose Healthy Options Consciously Everyday (CHOICE) randomized clinical trial. Am J Clin Nutr. 2012;95:555–563. doi: 10.3945/ajcn.111.026278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wyatt HR, Grunwald GK, Mosca CL, Klem ML, Wing RR, Hill JO. Long-term weight loss and breakfast in subjects in the National Weight Control Registry. Obesity. 2002;10:78–82. doi: 10.1038/oby.2002.13. [DOI] [PubMed] [Google Scholar]
- 28.Collins CE, Morgan PJ, Warren JM, Lubans DR, Callister R. Men participating in a weight-loss intervention are able to implement key dietary messages, but not those relating to vegetables or alcohol: the Self-Help, Exercise and Diet using Internet Technology (SHED-IT) study. Public Health Nutrition. 2011;14:168–175. doi: 10.1017/S1368980010001916. [DOI] [PubMed] [Google Scholar]
- 29.Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith BK. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2009;41:459–471. doi: 10.1249/MSS.0b013e3181949333. [DOI] [PubMed] [Google Scholar]
- 30.Steinberg DM, Tate DF, Bennett GG, Ennett S, Samuel-Hodge C, Ward DS. The efficacy of a daily self-weighing weight loss intervention using smart scales and email. Obesity. 2013;21:1789–1797. doi: 10.1002/oby.20396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wing RR, Tate DF, Gorin AA, Raynor HA, Fava JL. A self-regulation program for maintenance of weight loss. N Engl J Med. 2006;355:1563–1571. doi: 10.1056/NEJMoa061883. [DOI] [PubMed] [Google Scholar]
- 32.Wing RR, Tate D, Espeland M, Gorin A, Gokee LaRose J, Robichaud EF, Erickson K, Perdue L, Bahnson J, Lewis CE. Weight gain prevention in young adults: Design of the Study of Novel Approachs to Weight Gain Prevention (SNAP) randomized controlled trial. BMC Public Health. 2013;13 doi: 10.1186/1471-2458-13-300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nelson KM, Weinsier RL, Long CL, Schutz Y. Prediction of resting energy expenditure from fat-free mass and fat mass. Am J Clin Nutr. 1992;56:848–856. doi: 10.1093/ajcn/56.5.848. [DOI] [PubMed] [Google Scholar]
- 34.Paffenbarger R, Hyde R, Wing A, Hsieh C. Physical activity, all-cause mortality, and longevity of college alumni. The New England Journal of Medicine. 1986;314:605–613. doi: 10.1056/NEJM198603063141003. [DOI] [PubMed] [Google Scholar]
- 35.The Compendium of Physical ActivitiesTracking Guide. https://sites.google.com/site/compendiumofphysicalactivities/
- 36.Linde JA, Jeffery RW, French SA, Pronk NP, Boyle RG. Self-weighing in weight gain prevention and weight loss trials. nn Behav Med. 2005;30:210–216. doi: 10.1207/s15324796abm3003_5. [DOI] [PubMed] [Google Scholar]
- 37.VanWormer JJ, Martinez AM, Cosentino D, Pronk NP. Satisfaction with a weight loss program: what matters? Am J Health Promot. 2010;24:238–245. doi: 10.4278/ajhp.080613-QUAN-92. [DOI] [PubMed] [Google Scholar]
- 38.Lutes LD, Winett R, Barger S, Wojcik J, Herbert W, Nickols-Richardson S, Anderson E. Small changes in nutrition and physical activity promote weight loss and maintenance: 3-month evidence from the ASPIRE randomized trial. Ann Behav Med. 2008;35:351–357. doi: 10.1007/s12160-008-9033-z. [DOI] [PubMed] [Google Scholar]
- 39.Lutes LD, Daiss SR, Barger SD, Read M, Steinbaugh E, Winett RA. Small changes approach promotes initial and continued weight loss with a phone-based follow-up: Nine-month outcomes from ASPIRES II. Am J Health Promot. 2012;26:235–238. doi: 10.4278/ajhp.090706-QUAN-216. [DOI] [PubMed] [Google Scholar]
- 40.Damschroder LJ, Lutes LD, Kirsh S, Kim HM, Gallon L, Holleman RG, Goodrich DE, Lowery JC, Richardson CR. Small-changes obesity treatment among veterans. Am J Prev Med. 2014;47:541–553. doi: 10.1016/j.amepre.2014.06.016. [DOI] [PubMed] [Google Scholar]


