Abstract
Health information technology is an emerging area of focus in clinical medicine with the potential to improve injury and violence prevention practice. With injuries being the leading cause of death for Americans aged 1–44 years, greater implementation of evidence-based preventive services, referral to community resources, and real-time surveillance of emerging threats is needed. Through a review of the literature and capturing of current practice in the field, this paper showcases how health information technology applied to injury and violence prevention can lead to strengthened clinical preventive services, more rigorous measurement of clinical outcomes, and improved injury surveillance, potentially resulting in health improvement.
Introduction
In 2010, unintentional and violence-related injuries took more lives of people aged 1–44 years than cancer, heart disease, liver disease, HIV, stroke, diabetes, and birth defects combined.1 Injury and violence prevention is complex owing to variations in cause, intentionality, risk factors, and intervention points. Individual-, family-, school-, and community-based public approaches have demonstrated preventive effectiveness; however, clinical preventive services also have the potential for the primary and secondary prevention of injury, particularly in the areas of older adult falls, prescription drug overdose, and intimate partner violence.2-4 Clinical preventive services include clinical interventions to reduce the risk of an adverse health condition, screening to identify and treat a condition early to reduce severity and duration, and clinical interventions to reduce complications from a condition or recurrence of a condition.5 Although there have been few investigations of injury clinical preventive services with RCTs, assessment and referral for injury concerns are promising—particularly when based upon behavior change principles.6,7
Professional organizations and societies recommend clinical preventive services for injury and violence, with recent policy changes facilitating implementation. For example, the American Geriatrics Society and British Geriatrics Society developed a clinical practice guideline for prevention of falls in older persons,8 and the US Preventive Services Task Force (USPSTF) recommends exercise or physical therapy and vitamin D supplementation to prevent injuries from falls in community-dwelling adults aged 65 years or older.9 The USPSTF also recommends screening of women of childbearing age for intimate partner violence, including referral for women who screen positive to needed intervention services.10 Now, the Patient Protection and Affordable Care Act (PPACA)11 provides coverage for USPSTF-recommended preventive services, including the Annual Wellness Visit (AWV) for Medicare Part B beneficiaries that incorporates a Health Risk Assessment with questions on older adult fall risk.12
Organizations, societies, and states invest in the development of clinical practice guidelines to improve injury outcomes. For example, professional societies (e.g., American College of Emergency Physicians, American Pain Society/American Academy of Pain Medicine13,14) and states (e.g., Washington, Utah15,16) have promulgated guidelines on the prescription of opioids for treatment of non-cancer pain to reduce prescription drug overdoses.
Unfortunately, only 20% of adults visiting healthcare providers receive injury prevention counseling.17,18 The burgeoning of health information technology (IT) offers an opportunity to improve injury prevention services. Health IT is “the use of computer hardware and software to privately and securely store, retrieve, and share patient health and medical information.”19 Electronic health records (EHRs) are one form of health IT, within which other tools can be embedded, such as computerized clinical decision support (CDS).20 Other technologies, such as devices that assist in interviewing patients about their condition (e.g., computer-assisted self-interviews [CASIs]) can further assist in private sharing of health information. Well-designed and -implemented health IT can increase guideline adherence, improve disclosure rates for sensitive issues, enhance monitoring, and lead to health improvements.21
Now is the time to take advantage of evolving health IT to improve injury prevention. New advances in Health Information Exchange (HIE) are making it possible to enhance the utility of health IT tools, like EHRs. Widespread availability of secure electronic data transfer can allow: (1) providers to coordinate patient care by sharing information electronically between each other through interoperable health record systems; (2) patients to manage their own care by having access to electronic health information that can be reviewed and shared with new providers; (3) systems to improve the quality of care by rapidly deploying emerging clinical decision support within the EHR; and (4) health departments to conduct improved surveillance by accessing data from outpatient and inpatient settings through HIE data hubs.22,23
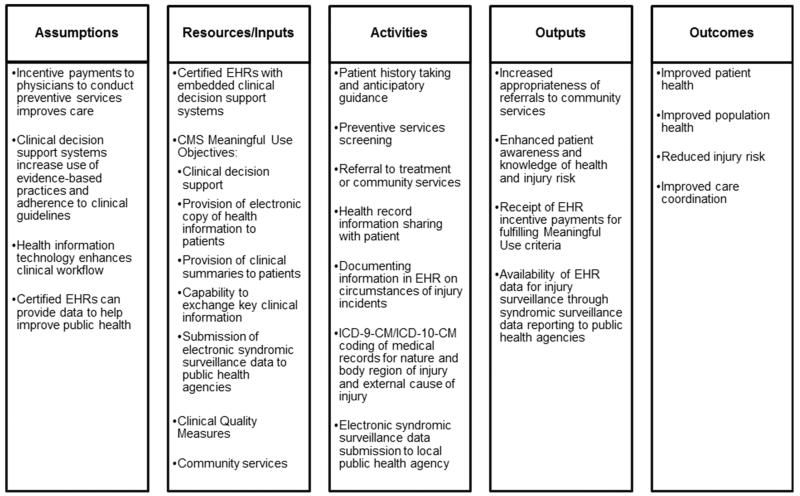
Through a review of the literature and current practice, this paper showcases how health IT applied to injury and violence prevention could lead to strengthened preventive services. A focus is placed on areas in which a return on investment is possible through the use of EHRs, CDS, and CASIs: older adult falls, prescription drug overdose, and intimate partner violence. Other innovative technology may contribute to reduced morbidity and mortality from injury, such as electronic wearable devices to enhance fall detection. However, reviewing such technology is beyond the current scope. Opportunities for sharing data between public health departments and primary care providers through health information exchanges are also highlighted. Advancements are possible through enhanced patient assessment and referral, rigorous service documentation and monitoring across time, and improved injury surveillance with use of external cause of injury codes (Figure 1).
Figure 1.
Health IT logic model for injury prevention
EHR = Electronic Health Record; ICD = International Classification of Diseases; CM = Clinical Modification; PH = CMS = Center for Medicare and Medicaid Services; IT = Information Technology
The Promise of Meaningful Use of Electronic Health Records
The advent of the meaningful use of EHRs and associated incentive programs established by the Centers for Medicare and Medicaid Services (CMS) in response to the Health IT for Economic and Clinical Health (HITECH) Act24 has provided an infrastructure to enhance the quality and consistency of preventive services. The CMS EHR Incentive Programs include a series of “core” and “menu” objectives that must be met for providers to receive Meaningful Use (MU) incentive payments; eligible professionals are required to report on core and “additional” Clinical Quality Measures (CQMs) through the EHR (more information is available at www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/). Objectives are evolving in stages of MU implementation from 2011 to 2016: Stage 1 (data capture and sharing), Stage 2 (advance clinical process), and Stage 3 (improved outcomes). CMS incentives have spurred the adoption of MU-certified EHRs: among family physicians, EHR adoption grew from 37% in 2006 to 68% in 2011 and was projected to exceed 80% in 2013.25
Three aspects of MU requirements have potential for improving injury preventive service quality and informing public health approaches to injury prevention at the population level: the core objective of implementing CDS, the CQM requirement, and the menu objective of submitting electronic syndromic surveillance data to public health agencies. Other ways in which the meaningful use requirements can assist injury and violence prevention activities are listed in Table 1.
Table 1.
Core and menu objectives for CMS EHR MU incentive payments– injury prevention potential
| Objectives | Examples of Injury Prevention Potential |
|---|---|
| CORE OBJECTIVES | |
| Computerized provider order entry |
Track type, quantity, and dose of drugs that increase risk for overdose (e.g., opioids) or falls (e.g., psychoactive drugs, drugs with anticholinergic side effects); Order assessments for injury preventive screening (e.g., tests for fall risk) |
| Drug-drug and drug-allergy checks |
Reduce co-prescribing of medications that increase overdose risk (e.g., opioids and benzodiazepines) or fall risk (e.g., psychoactive drugs, drugs with anticholinergic side effects) |
| Maintain an up-to-date problem list of current and active diagnoses |
Track injury-relevant diagnoses (e.g., poisoning, traumatic brain injury, self-injury) |
| E-Prescribing | Track type, quantity, and dose of drugs that increase risk for overdose (e.g., opioids) or falls (e.g., psychoactive drugs, drugs with anticholinergic side effects) |
| Maintain active medication list |
Reduce unnecessary polypharmacy to decrease risk for older adult falls, or misuse of controlled prescription drugs |
| Maintain active medication allergy list |
N/A |
| Record demographics | Enable alerts for fall risk screening for adults age 65 years or older, or injury prevention counseling for children at specific developmental milestones |
| Record and chart changes in vital signs |
N/A |
| Record smoking status for patients 13 years or older |
N/A |
| Report ambulatory clinical quality measures to CMS/states |
Monitor initiation and engagement of alcohol and other drug dependence treatment to reduce risk for overdose; Monitor screening for suicide risk among patients with depression, or fall risk among older adult patients |
| Implement clinical decision support |
Follow screening and treatment guidelines (e.g., opioid prescribing, fall risk assessment and referral, intimate partner violence screening) |
| Provide patients with an electronic copy of their health information, upon request |
Inform patients about their injury risk and recommendations for prevention/treatment |
| Provide clinical summaries for patients for each office visit |
Inform patients about their injury risk and recommendations for prevention/treatment |
| Capability to exchange key clinical information |
Exchange information about opioid use with other providers to reduce risk for overdose |
| Protect electronic health information |
N/A |
| MENU OBJECTIVES (Select 5, 1 from Public Health list) | |
| Submit electronic data to immunization registries (PH) |
N/A |
| Submit electronic syndromic surveillance data to public health agencies (PH) |
Conduct surveillance on nature, external cause, characteristics, and burden of injury; identify local injury epidemics |
| Drug formulary checks | Monitor type, quantity, and dose of drugs that increase risk for overdose (e.g., opioids) |
| Incorporate clinical lab-test results |
N/A |
| Generate lists of patients by specific conditions |
Understand the percentage of patients with specific forms of injury risk (e.g., fall, overdose, intimate partner violence, or suicide risk) to inform resource and referral needs |
| Send reminders to patients for preventive/follow-up care |
Provide referrals to community-based resources (e.g., community-based exercise programs for older adults at risk for falling, domestic violence resources) |
| Patient-specific education resources |
Provide specific recommendations tailored to each patient’s injury risk |
| Electronic access to health information for patients |
Allow patients to better track their medication use and identify injury risk (e.g., for falls or overdose) |
| Medication reconciliation | Monitor type, quantity, and dose of drugs that are prescribed by all providers to better identify injury risk (e.g., opioid overdose, falls) |
| Summary of care record for transitions of care |
Share information across care settings including the emergency department, primary care, and substance abuse treatment facilities for patients using prescription opioids inappropriately to implement a coordinated care plan |
CMS = Center for Medicare and Medicaid Services; EHR = Electronic Health Record; MU = Meaningful Use; PH = Public Health; N/A = Not Applicable to injury
Injury-Related Clinical Decision Support
A CDS system is “any electronic system designed to aid directly in clinical decision making, in which characteristics of individual patients are used to generate patient-specific assessments or recommendations that are then presented to clinicians for consideration.”26 These systems can be embedded within an EHR, and use alerts, reminders, and decision algorithms in real time to increase adherence to preventive service recommendations.27 EHR CDS for injury preventive services is in its infancy, with development in older adult fall assessment and opioid prescribing. Technologic innovations have also been made in intimate partner violence screening. Future innovations are promising in areas where reimbursement is available without patient cost sharing or CQMs are reportable.
Electronic Health Record Alerts and Reminders for Older Adult Fall Prevention
To enhance adherence to the American and British Geriatric Societies’ guideline for fall risk assessment, CDC developed the Stopping Elderly Accidents, Deaths, and Injuries (STEADI) toolkit.28 STEADI provides tools for healthcare providers who treat older adults at risk of falling, and supports clinicians in conducting fall risk assessment, treatment, and referrals. It assists clinicians in conducting fall risk assessment with standardized gait and balance assessment tests, case studies, and conversation starters, and educates patients about fall prevention with self-assessment brochures, including the Stay Independent brochure. The Oregon Health & Science University (OHSU) is now integrating STEADI into an EHR to enhance implementation in internal medicine and geriatric clinics. Results from the Stay Independent brochure, a vision screen, Timed Up and Go (TUG) test, orthostatic blood pressure measurements, and a medication review are entered into an Epic© EHR. The physician uses the Epic© STEADI order set to review medications and medical conditions and develop a fall reduction plan of care (e.g., adjusting high-risk medications, referral to exercise or physical therapy). The provider can provide electronically generated referrals in a discharge packet to A Matter of Balance (a program that reduces fear of falling and increases activity) and a community-based Tai Chi program (an exercise that has been shown to reduce the risk of falling).
Although findings from the STEADI evaluation are pending, U.S. Veterans Administration data illustrate the promise of integrating fall risk assessment into the EHR. In response to an EHR nurse screening reminder, a primary care physician follow-up reminder for gait, balance, and strength examination, and provision of educational materials and referrals, 75% of veterans aged 75 years or older were screened; further evaluation was needed for 49% of the patients who screened positive. Of those patients, 70% had a gait, balance, or strength problem, and 24% of those with problems were offered physical therapy or exercise.29 Another investigation in an integrated health system employed a randomized design to evaluate pharmacist and geriatrician review of patient medication records and EHR clinical practice guideline prompts. Compared to patients who received usual care, patients in the EHR intervention group were less likely to have fall-related diagnoses during the study period; however, no changes were seen in the overall number of prescribed medications. Physicians reported an increased awareness of falls and polypharmacy with 47% reporting having reviewed the guidelines and 42% reporting changing medical management because of the messages.30
Provision of Clinical Information and Guidelines for Prescription Drug Overdose Prevention
CDS has demonstrated improved care and outcomes in prescription monitoring and dosing31 that may have utility for opioid prescribing and prescription drug overdose prevention. State-based Prescription Drug Monitoring Programs (PDMPs) track opioid and other controlled prescription drug prescribing and dispensing. These programs store prescription information for controlled substances in a centralized database, identifying the drug, dose, and amount, as well as the prescriber, dispenser, and patient. PDMPs can provide data for EHR CDS to improve care for patients receiving opioid analgesics from multiple providers, engaging in possible drug diversion, or obtaining prescriptions for medications that may pose a problem if co-prescribed with an opioid. At the national level, a Stage 3 MU CQM is being considered to measure PDMP use in identifying potential narcotic misuse, abuse, and diversion.32 Further, the Office of the National Coordinator (ONC) led a joint initiative with the Substance Abuse and Mental Health Services Administration (SAMHSA), CDC, and the Office of National Drug Control Policy (ONDCP) to establish a standardized approach to make controlled prescription drug data from PDMPs available directly through EHRs and health information exchanges.33 Building on the success of this initial work, SAMHSA has now funded 16 states to further advance PDMP interoperability and EHR integration. CDC is conducting an evaluation of the impact of EHR integration in nine of these states; evaluation findings are pending.
Health systems also have integrated clinical prescribing and treatment guidelines into provider workflow in the EHR to reduce misuse and abuse and improve pain management. Group Health in Seattle34 and the U.S. Department of Veterans Affairs (VA) primary care clinics35 established care treatment plans in their EHRs to facilitate adherence to evidence-based guidelines through a stepwise algorithm. This includes encouraging non-narcotic alternatives for chronic non-cancer pain management such as nonsteroidal anti-inflammatory drugs, physical therapy, or complimentary/alternative medicine approaches.36
Computer-Based Screening for Intimate Partner Violence Prevention
Rates of screening for intimate partner violence are low,37 although numerous organizations recommend routine screening or assessment.10,38-41 To address identified barriers,42,43 save healthcare provider time, and reduce patient reluctance to disclose,44,45 CASIs have been developed. Four randomized and one non-randomized trial comparing a CASI to either usual care46-48 or prompted healthcare provider screening49,50 found equal or greater rates of disclosure. One of these RCTs also found that women were more likely to initiate discussions with providers after participating in a CASI.48 An RCT comparing healthcare provider screening and referral to an audio-CASI and a video of an actor portraying a doctor who provided interactive risk reduction messages also increased the likelihood of women discussing intimate partner violence with their provider.51 Finally, an RCT of an audio-CASI combined with a printout of resources available in response to women’s responses found that use of computers were more consistent in providing an adequate response to women who screened positive and generated almost equal rates of use of referral resources when compared to healthcare provider screening and referral.49 CASIs can allow women to maintain their autonomy in deciding when and to whom they disclose their experiences and how to independently access resources while still communicating that intimate partner violence is a serious health concern.52 Where face-to-face screening is preferred, computers can prompt physicians to screen, which increases the likelihood that healthcare providers have discussions about intimate partner violence with women.47,48,53
Injury-Related Clinical Quality Measures
Although CDS is used to enhance implementation of recommended practices, CQMs are used to track the quality of patient care, health outcomes, clinical processes, and population health. As part of the CMS EHR Incentive Program, eligible professionals are required to report on core and additional CQMs to fulfill MU requirements. Beginning with MU Stage 1, all professionals must report on three core CQMs, plus three additional that can be selected from a list of 38 measures. No quality measures in Stage 1 directly address injury prevention activities; however, one measure does include initiation of treatment for alcohol and other drug dependence (Table 2). In 2014, implementation of MU Stage 2 will require providers to choose nine CQMs above and beyond those required in Stage 1. Two of these CQMs are relevant to injury prevention, and focus on depression and older adult fall risk.54 Also as of 2014, CMS has aligned CQMs from the Medicare EHR Incentive Program with the Physician Quality Reporting System (PQRS) for EHR-based reporting.55 Two PQRS measures focus on fall risk.56 CQMs selected by CMS for the MU incentive program are likely to appear in EHRs as vendors seek to maximize provider and hospital federal Medicare and state Medicaid reimbursement.
Table 2.
Injury-related clinical quality measures
| Source | Clinical Quality Measure |
|---|---|
| Meaningful Use Stage 1 | NQF0004: Percentage of adolescent and adult patients with a new episode of alcohol and other drug (AOD) dependence who initiate treatment through an inpatient AOD admission, outpatient visit, intensive outpatient encounter or partial hospitalization within 14 days of the diagnosis and who initiated treatment and who had two or more additional services with an AOD diagnosis within 20 days of the initiation visit. |
| Meaningful Use Stage 2 | NQF0104: Percentage of patients ≥ 18 years of age with a new diagnosis of recurrent episode of major depressive disorder who had a suicide risk assessment completed at each visit during the measurement period. |
| NQF0101: Percentage of patients ≥ 65 years of age who were screened for future fall risk during the measurement period. |
|
| Physician Quality Reporting System |
PQRS154: Risk Assessment: Percentage of patients aged 65 years and older with a history of falls who had a risk assessment completed within 12 months |
| PQRS155: Plan of Care: Percentage of patients aged 65 years and older with a history of falls who had plan of care for falls documented within 12 months |
NQF = National Quality Forum; PQRS = Physician Quality Reporting System; AOD = Alcohol and Other Drug dependence
EHRs can potentially improve the quality and usefulness of documentation of patient and healthcare information obtained in clinical settings used for injury-related CQMs, such as by improving the completeness and specificity of ICD-9-CM and ICD-10-CM external-cause-of-injury codes (and the who, what, when, where, how, of the incident).57 Timely capture of brief narratives on injury circumstances in the EHR with subsequent ICD diagnosis and external cause coding by health information specialists for all injury-related patients could better provide essential information for decision making.
Injury Monitoring Through Syndromic Surveillance
EHRs facilitate effective coordination and sharing of data between public health departments and primary care providers. MU requires the exchange of syndromic surveillance data between hospitals and public health agencies. Although ongoing transmission of electronic syndromic surveillance data from hospitals to public health agencies is being developed to provide timely public health information to detect and respond to outbreaks, natural disasters, and other health events, it also provides useful injury-related information for public health surveillance and assessment of utilization and quality of care.58 Public Health Information Network (PHIN) guidelines for syndromic surveillance59 include a standard set of core data elements and functional and technical requirements for public health information exchange using the certified EHR technology. One of the PHIN core data elements captures ICD-9-CM/ICD-10-CMa diagnosis and external-cause-of-injury codes. For injured patients, these codes provide useful information on the mechanism (e.g., motor vehicle crash, firearm) and intent of injury (unintentional, assault, intentional self-harm), place of occurrence, and activity at the time of injury. The usefulness of external cause–coded data for injury epidemiology and healthcare utilization in a local healthcare setting has been demonstrated.60 These data can help characterize injured patients who are treated and released from the emergency department or urgent care setting, or who are admitted to the hospital to assess clinical care, length of stay, charges, costs of clinical/other healthcare services, and health outcomes by external cause and injury-related diagnoses. Even more comprehensive, with patient medical records from inpatient and outpatient settings, HIEs could share data with public health agencies, thus providing longitudinal records on prevention actions and outcomes. No current requirement exists to share HIE data with public health agencies for CMS MU reimbursement.
Benefits of Health Information Technology for Injury Prevention and Healthcare Providers
Enhancing Quality of Care
The use of health IT can improve injury prevention practice by prompting physicians to complete recommended screenings, adhere to clinical guidelines, and fulfill the CQM reporting requirements. Reviews of EHR data can measure injury morbidity, identify areas where patients need counseling on lifestyle modification, illustrate guideline adherence, and identify where improvements are needed in group practice.61 Health IT also allows for the distribution of tailored health education materials to patients and assists in improved bidirectional communication between patients and providers. IT systems can also facilitate referral of patients to community-based agencies that provide injury prevention services. Many injury prevention activities occur outside the health system; health IT can assist in providing linkages to public health programs sponsored within other systems, such as nonprofit community-based organizations or schools. EHRs could automatically generate referral lists to coordinated care centers or community service providers. For example, providers using the STEADI toolkit within EHRs provide patients autogenerated discharge packets that contain referrals to local community exercise programs with contact information, making it easier for patients to comply with provider recommendations independently. As yet, a limitation of EHRs is the inability to make automated direct referrals to community groups, given concerns about protected health information. Thus, the debate has moved from whether EHRs could be used to improve injury prevention to how research can further ways they can be used efficiently, while protecting individuals’ health information.
Enhancing Data Sharing and Identifying the Epidemiology of Injury
Sharing of injury data through EHRs can improve the usefulness of data from emergency departments and inpatient facilities to identify patterns and characteristics of injuries by diagnosis and external cause of injury in the patient population at the local level. Analysis of local data can improve understanding of injury epidemiology of the patient population served by specific hospitals, their patterns of care, and their impact on healthcare resources, and can be used in hospital and citywide decision making concerning allocation of resources and treatment/prevention strategies.60
EHR and HIE data sharing can improve the timeliness of data used at the state and national levels to identify patterns and characteristics of injury-related emergency department visits and hospitalizations and track trends in nonfatal injuries and injury rates by diagnosis and external cause of injury using population-based morbidity data. Currently, emergency department and hospitalization data are transmitted to state health departments or other state entities (e.g., state hospital associations) and are aggregated into statewide emergency department and hospital discharge databases. These data are not only used for administrative purposes and billing, but also for injury surveillance and prevention program planning and evaluation. Data from most of these statewide administrative data systems also are transmitted to the U.S. Agency for Healthcare Research and Quality and made available for analysis through the Healthcare Cost and Utilization Project (HCUP).62 HCUP includes state data sets and nationally representative data sets used for health services and epidemiologic research. For example, injury-related HCUP data have been used to examine the prevalence and characteristics of injury patients by diagnosis and external cause of injury (e.g., traumatic brain injury, fall-related injuries among older adults), as well as estimating the medical care costs of injury.1,63-65
Sharing of injury data through EHRs can improve timeliness of the availability of statewide hospital discharge and emergency department data for use in injury surveillance and prevention program planning and evaluation at the state and national levels. To examine current trends and the effectiveness of injury prevention programs, more timely, de-identified data are needed on injury morbidity outcomes associated with external causes of injury. Currently, there is a 2-year lag in the availability of statewide emergency department and hospital discharge data for population-based analysis. Efforts to improve timeliness in the availability of state and national death data through state-based electronic death registration systems are under way.66 These parallel efforts should help to provide more timely injury mortality and morbidity data for use in injury surveillance, epidemiologic research, and assessment of injury prevention activities.
Implementation Challenges of Health Information Technology for Injury Prevention
Expectations for clinical preventive service delivery are rapidly growing. One estimate is that it would take more than 7 hours per day for a primary care physician to fully satisfy the clinical recommendations of the USPSTF.67 Adding multiple practice guidelines within EHR CDS to assist in implementation could result in prompt and alert fatigue. Further, providers must already report on multiple CQMs through MU requirements; adding new injury prevention CQMs could be seen as increasing burden on providers and systems, and would likely result in low adoption. It is important to assist providers (and EHR vendors) in prioritizing which preventive service algorithms are coded within EHRs, and which CQMs are reported on. Prioritizing clinical preventive services, and in turn associated CDS and CQMs, based on clinically preventable burden and cost effectiveness68 could assist in reducing concerns about provider fatigue and compliance. Unfortunately, lack of strong evidence of effective injury preventive services based on RCTs with economic evaluation and few injury preventive services recommended by the USPSTF make it difficult to provide a strong case for EHR vendors to build in related CDS. Also, organizational bodies, such as the ONC, face challenges in selecting CQMs associated with such services and encouraging reimbursement. Further research is needed to develop the evidence base for injury preventive services using rigorous research designs that examine both health outcomes and costs. Following new evidence-based research findings, quality measures can then be introduced to the National Quality Forum for wide endorsement, a repository used by CMS to select MU CQMs.
Another challenge could be getting patients comfortable using technology and ensuring technology access to share information with their providers about their condition, receive information about risk and treatment options, and manage their own care. Technology in the medical setting has been found to be acceptable to patients under some conditions. In the area of partner violence, for example, patients may actually prefer self-administered questionnaires (including CASIs) over face-to-face interviews for answering questions.46,48-50,69 However, some patients may have concerns about privacy and technology interfering with the emotional connection formed between the patient and provider.46,70
Finally, data sharing between hospitals and public health agencies through syndromic surveillance is just beginning. Data use agreements for sharing of data between organizations are in their infancy, and state health department capacity is limited for receipt of clinical data. A standard algorithm for pulling injury data information from syndromic surveillance systems to make such data useful has not yet been developed. Thus, critical innovations are still needed as the stages of MU unfold and HIE mechanisms are established so that injury data can be exchanged and used to inform epidemiology and practice.
Conclusions
Health IT is an emerging area in clinical medicine with the potential to improve practice across the health system. It can also serve as a critical link between evidence-based clinical medicine and improved public health. There is much promise for reducing practice variability, engaging broad healthcare teams, facilitating patient-centered care, improving injury epidemiology, and supporting evaluation of prevention practice. Although the primary examples provided here focus on older adult falls, prescription drug overdose, and intimate partner violence, other areas of injury prevention could benefit greatly from the application of health IT—in particular, the recognition and management of mild traumatic brain injury and concussions, as clinical guidelines are becoming more sophisticated, enabling electronic CDS algorithms and coordinated care. As health IT integrates injury prevention into systems alongside chronic and infectious conditions, greater advancements in reducing the burden of injury at a population level are possible.
Acknowledgments
We wish to thank Seth Foldy, Judy Stevens, Christopher M. Jones, and Heidi Ehrenreich for their thoughtful reviews, comments, and suggestions.
The conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
The authors of this manuscript are employees of the Centers for Disease Control and Prevention. No funding was provided for this work beyond salary support.
Footnotes
Note: ICD-10-CM will be implemented in the U.S. for morbidity data coding on October 1, 2014. ICD-10-CM will provide much more detailed information than ICD-9-CM on the body part affected, nature of injury, and external cause of injury.
No financial disclosures were reported by the authors of this paper.
References
- 1.Centers for Disease Control and Prevention Web-based Injury Statistics Query and Reporting System (WISQARS) 2013 www.cdc.gov/ncipc/wisqars.
- 2.Stevens J, Noonan R, Rubenstein L. Older adult fall prevention: Perceptions, beliefs, and behaviors. Am J Lifestyle Med. 2010;4(1):16–20. [Google Scholar]
- 3.Dasgupta N, Sanford C, Albert S, Brason F., II Opioid drug overdoses: A prescription for harm and potential for prevention. Am J Lifestyle Med. 2010;10(1):32–7. [Google Scholar]
- 4.Black M. Intimate partner violence and adverse health consequences: implications for clinicians. Am J Lifestyle Med. 2011;5(5):428–39. [Google Scholar]
- 5.Frieden TR, CDC Use of selected clinical preventive services among adults — United States, 2007–2010. MMWR Morb Mortal Wkly Rep. 2012;61(Supplement):1–2. [PubMed] [Google Scholar]
- 6.Ballesteros M, Gielen A. Patient counseling for unintentional injury prevention. Am J Lifestyle Med. 2010;4(1):38–41. [Google Scholar]
- 7.Gielen A, Sleet D. Application of behavior change theories and methods to injury prevention. Epidemiol Rev. 2003;25(1):65–76. doi: 10.1093/epirev/mxg004. [DOI] [PubMed] [Google Scholar]
- 8.Panel on Prevention of Falls in Older Persons. American Geriatrics Society. British Geriatrics Society Summary of the updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011;59(1):148–57. doi: 10.1111/j.1532-5415.2010.03234.x. [DOI] [PubMed] [Google Scholar]
- 9.Moyer V, US Preventive Services Task Force Prevention of falls in community-dwelling older adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;157(3):197–204. doi: 10.7326/0003-4819-157-3-201208070-00462. [DOI] [PubMed] [Google Scholar]
- 10.Moyer V, US Preventive Services Task Force Screening for intimate partner violence and abuse of elderly and vulnerable adults: U.S. preventive services task force recommendation statement. Ann Intern Med. 2013;158(6):478–86. doi: 10.7326/0003-4819-158-6-201303190-00588. [DOI] [PubMed] [Google Scholar]
- 11.The Patient Protection and Affordable Care Act of 2010. Pub. L No.. 111-148, 124 Stat. 119, as amended by the Health Care and Education Reconciliation Act of 2010, Pub. L. No. 111-152, 124 Stat. 1029, together referred to as the Affordable Care Act. [Google Scholar]
- 12.DHHS. Centers for Medicare and Medicaid Services. Medicare Learning Network Quick Reference Information: The ABCs of Providing the Annual Wellness Visit. 2014 http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/AWV_Chart_ICN905706.pdf.
- 13.Cantrill SV, Brown MD, Carlisle RJ, et al. Clinical policy: Critical issues in the prescribing of opioids for adult patients in the emergency department. Ann Emerg Med. 2012;60(4):499–525. doi: 10.1016/j.annemergmed.2012.06.013. [DOI] [PubMed] [Google Scholar]
- 14.Chou R, Fanciullo G, Fine P, et al. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009;10(2):113–30. doi: 10.1016/j.jpain.2008.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Washington Agency Medical Directors’ Group . Interagency guideline on opioid dosing for chronic non-cancer pain: An educational aid to improve care and safety with opioid therapy. Washington Agency Medical Directors’ Group; Washington State: 2010. [Google Scholar]
- 16.Sundwaall DN, Rolfs RT, Johnson E, Utah Department of Health . Utah clinical guidelines on prescribing opioids for treatment of pain. Utah Department of Health; Salt Lake City, Utah: 2009. health.utah.gov/prescription/pdf/guidelines/final.04.09opioidGuidlines.pdf. [DOI] [PubMed] [Google Scholar]
- 17.Dellinger A, Chen J, Vance A, Breiding M, Simon T, Ballesteros M. Injury prevention counseling for adults: Have we made progress? Fam Community Health. 2009;32(2):115–22. doi: 10.1097/FCH.0b013e31819946e7. [DOI] [PubMed] [Google Scholar]
- 18.Chen J, Kresnow M, Simon T, Dellinger A. Injury-prevention counseling and behavior among US children: results from the second Injury Control and Risk Survey. Pediatrics. 2007;119(4):e958–65. doi: 10.1542/peds.2006-1605. [DOI] [PubMed] [Google Scholar]
- 19.White House. US Department of Health and Human Services HealthIT.gov. http://www.healthit.gov/
- 20.Goldschmidt P. HIT and MIS: Implications of health information technology and medical information systems. Commun ACM. 2005;48(10):69–74. [Google Scholar]
- 21.Chaudhry B, Wang J, Wu S, et al. Systematic review: Impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006;144(10):742–52. doi: 10.7326/0003-4819-144-10-200605160-00125. [DOI] [PubMed] [Google Scholar]
- 22.Dixon B, Grannis S, Revere D. Measuring the impact of a health information exchange intervention on provider-based notifiable disease reporting using mixed methods: A study protocol. BMC Med Inform Decis Mak. 2013;13:121. doi: 10.1186/1472-6947-13-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.White House. US Department of Health and Human Services. Health Information Exchange http://www.healthit.gov/HIE.
- 24.Health Information Technology for Economic and Clinical Health (HITECH) Act . Title XIII of Division A and Title IV of Division B of the American Recovery and Reinvestment Act of 2009 (ARRA) Feb. 2009. Pub. L. No. 111-5, 123 Stat. 226. [Google Scholar]
- 25.Xierali I, Hsiao C, Puffer J, et al. The rise of electronic health record adoption among family physicians. Ann Fam Med. 2013;11(1):14–9. doi: 10.1370/afm.1461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kawamoto K, Houlihan C, Balas E, Lobach D. Improving clinical practice using clinical decision support systems: A systematic review of trials to identify features critical to success. BMJ. 2005;330(7494):765–772. doi: 10.1136/bmj.38398.500764.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bright T, Wong A, Dhurjati R, et al. Effect of clinical decision-support systems: a systematic review. Ann Intern Med. 2012;157(1):29–43. doi: 10.7326/0003-4819-157-1-201207030-00450. [DOI] [PubMed] [Google Scholar]
- 28.Stevens J, Phelan E. Development of STEADI: A fall prevention resource for health care providers. Health Promot Pract. 2013;14(5):706–14. doi: 10.1177/1524839912463576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Spears G, Roth C, Miake-Lye I, Sliba D, Shekelle P, Ganz D. Redesign of an electronic clinical reminder to prevent falls in older adults. Med Care. 2013;51(3 Suppl 1):S37–43. doi: 10.1097/MLR.0b013e31827807f8. [DOI] [PubMed] [Google Scholar]
- 30.Weber V, White A, Mcllvried R. An electronic medical record (EMR)-based intervention to reduce polypharmacy and falls in an ambulatory rural elderly population. J Gen Intern Med. 2008;23(4):399–404. doi: 10.1007/s11606-007-0482-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nieuwlaat R, Connolly S, Mackay J, et al. Computerized clinical decision support systems for therapeutic drug monitoring and dosing: A decision-maker-researcher partnership systematic review. Implement Sci. 2011;6(1):90. doi: 10.1186/1748-5908-6-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hirsch MD. Meaningful Use Stage 3 may tackle prescription drug abuse. Fierce EMR; 2012. http://www.fierceemr.com/story/meaningful-use-stage-3-may-tackle-prescription-drug-abuse/2012-10-30. [Google Scholar]
- 33.Standards and Interoperability Framework PDMP and Health Integration Home Page. wiki.siframework.org/PDMP+%26+Health+IT+Integration+Homepage.
- 34.Trescott C, Beck R, Seelig M, Von Korff M. Group Health’s initiative to avert opioid misuse and overdose among patients with chronic noncancer pain. Health Aff (Milwood) 2011;30(8):1420–4. doi: 10.1377/hlthaff.2011.0759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dobscha S, Corson K, Perrin N, et al. Collaborative care for chronic pain in primary care: a cluster randomized trial. JAMA. 2009;301(12):1242–52. doi: 10.1001/jama.2009.377. [DOI] [PubMed] [Google Scholar]
- 36.Rubinstein S, van Middlekoop M, Kuijpers T, et al. A systematic review on the effectiveness of complementary and alternative medicine for chronic non-specific low-back pain. Eur Spine J. 2010;19(8):1213–28. doi: 10.1007/s00586-010-1356-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.D’Avolio D. System issues: challenges to intimate partner violence screening and intervention. Clin Nurs Res. 2011;20(1):64–80. doi: 10.1177/1054773810387923. [DOI] [PubMed] [Google Scholar]
- 38.American Medical Association Family and intimate partner violence. http://www.ama-assn.org/ama/pub/about-ama/our-people/house-delegates/policyfinder.page.
- 39.American College of Obstetricians and Gynecologists ACOG Committee Opinion No. 518: Intimate partner violence. Obstet Gynecol. 2012;119(2 Pt1):412–7. doi: 10.1097/AOG.0b013e318249ff74. [DOI] [PubMed] [Google Scholar]
- 40.Thackeray J, Hibbard R, Dowd M, Committee on Child Abuse and Neglect. Committee on Injury Violence and Poison Prevention Intimate partner violence: The role of the pediatrician. Pediatrics. 2010;125(5):1094–100. doi: 10.1542/peds.2010-0451. [DOI] [PubMed] [Google Scholar]
- 41.IOM . Clinical Preventive Services for Women: Closing the Gaps. National Academies Press; Washington, DC: 2011. [Google Scholar]
- 42.Sprague S, Madden K, Simunovic N, et al. Barriers to screening for intimate partner violence. Women Health. 2012;52(6):587–605. doi: 10.1080/03630242.2012.690840. [DOI] [PubMed] [Google Scholar]
- 43.Hathaway J, Willis G, Zimmer B. Listening to survivors’ voices: addressing partner abuse in the health care setting. Violence Against Women. 2002;8(6):687–716. [Google Scholar]
- 44.McNutt L, Waltermauer E, McCauley J, Campbell J, Ford D. Rationale for and development of the computerized intimate partner violence screen for primary care. Fam Viol Prev Health Pract. 2005;3:1–14. [Google Scholar]
- 45.Renker P. Breaking the barriers: the promise of computer-assisted screening for intimate partner violence. J Midwifery Womens Health. 2008;53(6):496–503. doi: 10.1016/j.jmwh.2008.07.017. [DOI] [PubMed] [Google Scholar]
- 46.Ahmad F, Hogg-Johnson S, Stewart D, Skinner H, Glazier R, Levinson W. Computer-assisted screening for intimate partner violence and control: a randomized trial. Ann Intern Med. 2009;151(2):93–102. doi: 10.7326/0003-4819-151-2-200907210-00124. [DOI] [PubMed] [Google Scholar]
- 47.Trautman D, McCarthy M, Miller N, Campbell J, Kelen G. Intimate partner violence and emergency department screening: computerized screening versus usual care. Ann Emer Med. 2007;49(4):526–34. doi: 10.1016/j.annemergmed.2006.11.022. [DOI] [PubMed] [Google Scholar]
- 48.Rhodes K, Drum M, Anliker E, Frankel R, Howes D, Levinson W. Lowering the threshold for discussions of domestic violence: a randomized controlled trial of computer screening. Arch Intern Med. 2006;166(10):1107–14. doi: 10.1001/archinte.166.10.1107. [DOI] [PubMed] [Google Scholar]
- 49.Klevens J, Sadowski L, Kee R, Trick W, Garcia D. Comparison of screening and referral strategies for exposure to partner violence. Womens Health Issues. 2012;22(1):e45–52. doi: 10.1016/j.whi.2011.06.008. [DOI] [PubMed] [Google Scholar]
- 50.MacMillan H, Wathen C, Jamieson E, et al. Approaches to screening for intimate partner violence in health care settings. JAMA. 2006;296(5):530–6. doi: 10.1001/jama.296.5.530. [DOI] [PubMed] [Google Scholar]
- 51.Humphreys J, Tsoh J, Kohn M, Gerbert B. Increasing discussions of intimate partner violence in prenatal care using video doctor plus cueing: a randomized, controlled trial. Womens Health Issues. 2011;21(2):136–44. doi: 10.1016/j.whi.2010.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Renker P. Perinatal violence assessment: Teenagers’ rationale for denying violence when asked. J Obstet Gynecol Neonatal Nurs. 2006;35(1):56–67. doi: 10.1111/j.1552-6909.2006.00018.x. [DOI] [PubMed] [Google Scholar]
- 53.Rhodes K. The promise and problems with using information technology to achieve routine screening for intimate partner violence. Fam Viol Prev Health Pract. 2005;3:1–14. [Google Scholar]
- 54.Centers for Medicare and Medicaid Services 2011-2012 Eligible Professional Clinical Quality Measures (CQMs) 2011 www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Downloads/CQM_EPs_2012_02_02.pdf.
- 55.Centers for Medicare and Medicaid Services 2014 Physican Quality Reporting System (PQRS): Implementation Guide. 2013 http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/PQRS/MeasuresCodes.html.
- 56.Centers for Medicare and Medicaid Services 2014 Physican Quality Reporting System (PQRS) Measures List. 2013 www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/PQRS/How_To_Get_Started.html.
- 57.Adams W, Mann A, Bauchner H. Use of an electronic medical record improves the quality of urban pediatric primary care. Pediatrics. 2003;111(3):626–32. doi: 10.1542/peds.111.3.626. [DOI] [PubMed] [Google Scholar]
- 58.Henning K. What is syndromic surveillance? Syndromic surveillance: Reports from a national conference. MMWR Morb Mortal Wkly Rep. 2004;53(S1):7–11. [Google Scholar]
- 59.CDC . PHIN Messaging Guide for Syndromic Surveillance: Emergency Department, Urgent Care, and Inpatient Settings. DHHS, CDC; Atlanta, GA: 2013. Release 1.9. [Google Scholar]
- 60.Odero W, Tierney W, Einterz R, Mungai S. Using an electronic medical record system to describe injury epidemiology and health care utilization at an inner-city hospital in Indiana. Inj Control Saf Promot. 2004;11(4):269–79. doi: 10.1080/156609704/233/289616. [DOI] [PubMed] [Google Scholar]
- 61.Brimmer K. Five ways hospitals can use data analytics. Healthcare IT News; Feb 28, 2013. www.healthcareitnews.com/news/5-ways-hospitals-can-use-data-analytics. [Google Scholar]
- 62.Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project (HCUP) www.hcup-us.ahrq.gov/ [PubMed]
- 63.Parks S, Sugerman D, Xu L, Coronado V. Characteristics of non-fatal abusive head trauma among children in the USA, 2003–2008: Application of the CDC operational case definition to national hospital inpatient data. Inj Prev. 2012;18(6):392–8. doi: 10.1136/injuryprev-2011-040234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Stevens J, Corso P, Finkelstein E, Miller T. The costs of fatal and non-fatal falls among older adults. Inj Prev. 2006;12(5):290–5. doi: 10.1136/ip.2005.011015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Corso P, Mercy J, Simon T, Finkelstein E, Miller T. Medical costs and productivity losses due to interpersonal and self-directed violence in the United States. Am J Prev Med. 2007;32(6):474–82. doi: 10.1016/j.amepre.2007.02.010. [DOI] [PubMed] [Google Scholar]
- 66.National Association of Public Health Statistics and Information Systems Electronic death registration systems project. naphsis-web.sharepoint.com/Pages/ElectronicDeathRegistrationSystemsProject.aspx.
- 67.Yarnall K, Pollak K, Ostbye T, Krause K, Michener J. Primary care: Is there enough time for prevention? Am J Public Health. 2003;93(4):635–41. doi: 10.2105/ajph.93.4.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Maciosek M, Coffield A, Edwards N, Flottemesch T, Goodman M, Solberg L. Priorities among effective clinical preventive services: results of a systematic review and analysis. Am J Prev Med. 2006;31(1):52–61. doi: 10.1016/j.amepre.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 69.Furbee P, Sikora R, Williams J, Derk S. Comparison of domestic violence screening methods: a pilot study. Ann of Emer Med. 1998;31(4):495–501. doi: 10.1016/s0196-0644(98)70260-4. [DOI] [PubMed] [Google Scholar]
- 70.Chang J, Dado D, Schussler S, et al. In person versus computer screening for intimate partner violence among pregnant patients. Patient Educ Couns. 2012;88(3):443–8. doi: 10.1016/j.pec.2012.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]