Abstract
OBJECTIVE
Sleep duration is associated with obesity and cardiometabolic disease. It is unclear, though, how these relationship differs across age groups.
METHODS
Data from the 2007–2008 National Health and Nutrition Examination Survey (NHANES) were used, including respondents aged 16+ with complete data (N=5,607). Sleep duration and age were evaluated by self-report and body mass index (BMI) was assessed objectively. Sleep duration was evaluated continuously and categorically [very short (≤4h), short (5–6h), and long (≥9h) versus average (7–8h)]. Age was also evaluated continuously and categorically [adolescent (16–17yrs), young adult (18–29yrs), early middle age (30–49 yrs), late middle age (50–6 4yrs), and older adult (≥65 yrs)].
RESULTS
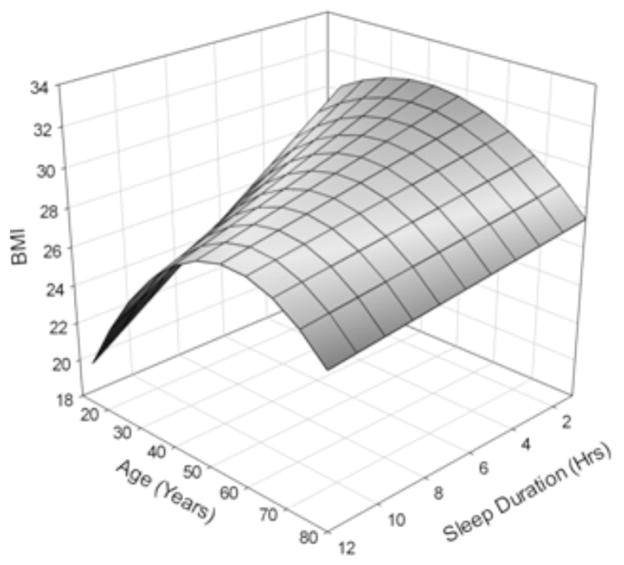
There was a significant interaction with age for both continuous (Pinteraction=0.014) and categorical (Pinteraction=0.035) sleep duration. A pseudo-linear relationship is seen among the youngest respondents, with the highest BMI associated with the shortest sleepers and the lowest BMI associated with the longest sleepers. This relationship becomes U-shaped in middle-age, and less of a relationship is seen among the oldest respondents.
CONCLUSIONS
These findings may provide insights for clinical recommendations and could help to guide mechanistic research regarding the sleep-obesity relationship.
Keywords: Sleep, Obesity, Age, Body Mass Index, Epidemiology, Sleep Duration
INTRODUCTION
Obesity is a major global health problem, and in the US the prevalence has increased at an alarming rate. Obesity is a major risk factor for cardiometabolic disease and other adverse health outcomes, many of which are linked to the leading causes of death in the population. Substantial research has clarified the role of behavioral factors in the etiology of obesity – particularly diet and exercise. However, it is recognized that other health behaviors are also important1. More recently, sleep has been identified as a health behavior that may play a role in obesity as well2.
Associations between sleep duration and obesity are well-characterized3. Empirical evidence suggests a strong association between habitual sleep duration and obesity. Proposed mechanisms for this relationship include insulin and glucose dysregulation4, an orexigenic pattern due to decreased leptin and/or increased ghrelin5, increased caloric consumption or other dietary changes6, increased systemic inflammation7, or decreased physical activity, perhaps due to increased daytime sleepiness8. These and other pathways may explain the mechanisms underlying why short sleep may cause increased body weight.
Despite the general agreement across studies that there is an association between sleep duration and obesity3, there is some notable inconsistency regarding the nature of this relationship. Some studies tend to show a relatively linear negative association between sleep duration and adiposity/obesity9, 10; however, others show a U-shaped association that implicates both short and long sleep duration11, similar in pattern to the frequently-observed relationship between sleep duration and mortality12. These inconsistencies across studies may be due to differences in measurement approaches for both sleep and obesity/adiposity, differences in adjustment for potential confounders, and differences in the characteristics of study populations, particularly among observational studies.
Since body mass, and associated chronic disease, generally reflects years of accumulated morbidity, it is possible that the relationship between sleep duration and body mass may differ across age groups. For example, obesity in young adulthood may reflect more proximal lifestyle and health factors, one of which may be short sleep duration. In addition, childhood obesity may reflect parenting behaviors and availability of calorific foods rather than lifestyle factors. Conversely, obesity in older age may reflect decades of accumulated risk factors, which, in aggregate, outweigh any effect of short sleep duration. For example, the comorbidities which tend to develop with aging may mitigate obesity effects on the causal pathways mentioned above. Thus, the effects of sleep duration on obesity may vary with aging, as has been shown for certain neurocognitive outcomes 13. Further, there is a possibility that hormonal influences (e.g., menopause in women and lower testosterone levels in men) may impact this relationship in the older age population.
The present study assesses whether the cross-sectional association between sleep duration and body mass index (BMI) differs as a function of age. Specifically, it is hypothesized that this sleep duration-BMI relationship will not be linear, but with differing patterns of association across age groups. To assess this possibility, the current analysis explores data from the 2007–2008 National Health and Nutrition Examination Survey, a cross-sectional, nationally-representative cohort that assessed self-reported sleep duration and objectively-determined BMI.
METHODS
Data source
Participants included respondents to the 2007–2008 National Health and Nutrition Examination Survey (NHANES), a national survey conducted by the Centers for Disease Control and Prevention to assess the health and nutritional characteristics of the US population14. The NHANES data, methodology, surveys, manuals, and procedures have been previously reported and are available online (http://www.cdc.gov/nchs/nhanes). Participants responded to questionnaires assessing demographic, socioeconomic, health, and other domains during face-to- face, in-home interviews. To supplement self-report data, physical examination data were gathered in mobile medical facilities. Blacks/African Americans, Hispanics/Latinos, and adults over 60 years were over-sampled to increase the power to detect differences in these groups. The NHANES is designed to ensure generalizability to the entire population across age groups. Given the complexity of the survey design, coupled with variable probabilities of selection, the data used in the following analyses were also weighted to control for representativeness, by following the procedures outlined in the current NHANES Analytic and Reporting Guidelines15. Presently, data on adults ages 16-80+ years with complete data on our variables of interest were analyzed. All respondents provided informed consent.
Measures
Sleep duration
Sleep duration was assessed with the survey item, “How much sleep do you usually get at night on weekdays or workdays?” Thus, the data do not reflect weekend sleep. Responses were coded in whole numbers. This variable was used for the continuous measure of sleep duration. Sleep duration categories were also computed. Based on previous studies, responses were categorized as “very short” (≤4 hours), short (5–6 hours), average (7–8 hours) or long (≥9 hours). These categories were based on existing literature examining cardiovascular and metabolic consequences of habitual sleep duration and experimental sleep restriction16. Although the NHANES sleep duration item is a retrospective self-report (and not an objective or prospective measure of habitual sleep), it has demonstrated utility in many studies.
Body Mass Index
Body mass index (BMI) was computed using objectively-measured height and weight recorded during a physical exam. The details of this assessment are reported in the Anthropometry Procedures Manual 17.
Age
Age was assessed via self-report. In analyses, age was considered both continuously (to document linear relationships) and categorically (to document nonlinear relationships). Both approaches were chosen a priori. Categorical analyses of age examined late adolescents (16– 17yrs), young adults (18–29yrs), younger middle-aged adults (30–49yrs), older middle-aged adults (50–64 yrs), and older adults (≥65 yrs) separately.
Covariates
The present study adjusted for potential confounding factors by including the following covariates: Demographic variables included sex, race/ethnicity (Non-Hispanic White, Black/African-American, Mexican-American, Other Hispanic/Latino, or Asian/Other), and marital status (Married, Widowed, Divorced, Separated, Never Married, or Living with Partner), as these factors are known to affect sleep behaviors as well as health outcomes. Socioeconomic factors suspected to affect sleep and health outcomes were also entered as covariates, including education level (less than high school, high school, some college, college graduate) and income to poverty ratio (computed using household income, household size, and federal poverty level). Exercise (minutes of moderate and/or vigorous activity, assessed using standard NHANES methodology) was included as a covariate in all models due to the presence of exercise as a potential confounder, related to both sleep and BMI. Other health risk factors included smoking (number of smoking days in the past 30 days), alcohol (measured as average number of drinks per day over the past 12 months) and both total daily caloric intake and food variety (garnered from detailed dietary interviews18). Depression was included as a dichotomized variable comparing those that felt down, depressed, or hopeless in the past two-weeks to those that did not.
Statistical analyses
In analyses, age and sleep duration were considered as both continuous and categorical measures, in order to model both linear and nonlinear relationships. Relationships were first examined using categorical age groups (using both continuous and categorical sleep variables), and then relationships were examined using age as a continuous variable (using both continuous and categorical sleep variables).
Univariate comparisons across age groups for all variables were evaluated using ANOVA or X2 as appropriate. Then, linear regression analyses evaluated differences in BMI associated with sleep duration (as a continuous variable and as a categorical variable, using 7-8 hours as reference), stratified across categorical age groups. These analyses were performed in 3 stages: Model 1 was unadjusted, Model 2 adjusted for sex, race/ethnicity, marital status, income to poverty ratio, education, and exercise, and Model 3 included all Model 3 variables and total caloric intake, food variety, alcohol, and smoking. To examine the relationships with age as a continuous variable, linear regression analyses examined a sleep duration by age interaction on BMI using both continuous and categorical sleep duration variables. Significant interactions were plotted using 3-dimensional graphs for the continuous by continuous interaction and stratified line graphs for the categorical by continuous interaction. Since these relationships may differ for men and women, we performed secondary analyses separately for men and women, as well.
Since BMI among adolescents and younger adults may be better represented by BMI z-scores, we performed a secondary analysis, repeating all tests using BMI z-scores instead of BMI. BMI Z-scores for participants ≤20 years old were created based on Growth Charts from 2000 using the standardized method19. Z-scores for the rest of the sample were created by subtracting the with-in sample mean BMI from each participant’s value and dividing by the standard deviation.
Two-tailed P-values of <0.05 were used as the threshold for the determination of significance. All statistical calculations were performed using STATA/SE version 12 (STATA Corp, College Station TX).
RESULTS
Sample characteristics
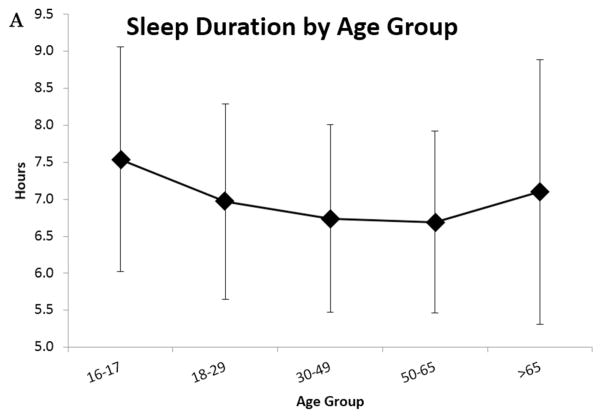
Characteristics of the sample are reported in Table 1. All cases were weighted, resulting in a sample that was nationally-representative. Sociodemographic, socioeconomic, and health variables were differentially distributed across age groups, justifying their inclusion as covariates. In addition, sleep duration (continuous and categorical) differed by age group, with the longest sleep duration in the youngest group (16–17 year olds) and the shortest sleep duration in the 50–64 year olds. Figure 1 depicts the distribution of sleep duration across age groups. Figure 1A depicts continuous sleep duration, and Figure 1B depicts sleep duration category.
Table 1.
Characteristics of the Analytic Sample, Overall and Stratified By Age
| Variable | Category | Overall Sample |
Stratification by Age Group
|
|||||
|---|---|---|---|---|---|---|---|---|
| 16–17 | 18–29 | 30–49 | 50–64 | ≥65 | P* | |||
| N | 100% | 3.82% | 21.12% | 36.86% | 23.48% | 14.71% | ||
|
| ||||||||
| Age | Years | 44.3 ± 17.5 | 16.4 ± 0.6 | 23.6 ± 3.2 | 40.1 ± 5.2 | 56.1 ± 4.3 | 73.4 ± 6.6 | <.0001 |
|
| ||||||||
| BMI | kg/m2 | 28.3 ± 6.7 | 24.1 ± 6.1 | 27.1 ± 6.7 | 28.7 ± 6.1 | 29.5 ± 6.5 | 28.3 ± 7.1 | <.0001 |
| z-score | −0.01 ± 1.02 | 0.56 ± 1.26 | −0.08 ± 1.04 | −0.05 ± 0.91 | 0.07 ± 0.98 | −0.12 ± 1.07 | <.0001 | |
|
| ||||||||
| Obese | Non-Obese | 67.54% | 83.44% | 74.40% | 66.42% | 59.97% | 68.45% | <.0001 |
| Obese | 32.46% | 16.56% | 25.60% | 33.58% | 40.03% | 31.55% | ||
|
| ||||||||
| Sleep Duration | Hours | 6.86 ± 1.38 | 7.54 ± 1.52 | 6.97 ± 1.32 | 6.74 ± 1.27 | 6.69 ± 1.23 | 7.10 ± 1.79 | <.0001 |
|
| ||||||||
| Sleep Duration Groups | ≤4 Hours | 4.96% | 0.63% | 4.73% | 5.86% | 4.95% | 4.17% | <.0001 |
| 5–6 Hours | 32.16% | 19.38% | 31.02% | 33.61% | 35.41% | 28.31% | ||
| 7–8 Hours | 55.68% | 62.47% | 54.44% | 55.49% | 56.04% | 55.58% | ||
| ≥9 Hours | 7.20% | 17.52% | 9.81% | 5.03% | 3.61% | 11.94% | ||
|
| ||||||||
| Gender | Female | 51.61% | 53.13% | 48.58% | 51.80% | 50.92% | 56.19% | 0.0954 |
| Male | 48.39% | 46.87% | 51.42% | 48.20% | 49.08% | 43.81% | ||
|
| ||||||||
| Race | White | 70.00% | 66.58% | 63.49% | 66.59% | 73.85% | 82.65% | <.0001 |
| Hispanic | 12.94% | 15.57% | 17.83% | 15.35% | 8.60% | 6.14% | ||
| Black | 11.25% | 14.44% | 12.86% | 12.09% | 9.99% | 7.99% | ||
| Other | 5.81% | 3.41% | 5.82% | 5.97% | 7.56% | 3.22% | ||
|
| ||||||||
| Marital Status | Married | 54.90% | 0.00% | 26.17% | 64.49% | 69.15% | 57.13% | <.0001 |
| Widowed | 5.23% | 0.00% | 0.00% | 0.69% | 3.40% | 27.18% | ||
| Divorced | 9.81% | 0.00% | 2.14% | 11.28% | 14.33% | 10.73% | ||
| Separated | 2.36% | 0.00% | 1.71% | 3.05% | 2.95% | 1.08% | ||
| Never Married | 20.86% | 100.00% | 53.51% | 12.76% | 7.26% | 2.79% | ||
| Living with Partner | 6.85% | 0.00% | 16.48% | 7.73% | 2.91% | 1.09% | ||
|
| ||||||||
| Exercise | Minutes | 166 ± 220 | 186 ± 211 | 217 ± 217 | 186 ± 224 | 139 ± 187 | 84 ± 182 | <.0001 |
|
| ||||||||
| Income to Poverty | Ratio | 3.01 ± 1.65 | 2.77 ± 1.86 | 2.51 ± 1.52 | 3.09 ± 1.52 | 3.59 ± 1.58 | 2.64 ± 1.80 | <.0001 |
|
| ||||||||
| Education | Less than High School | 23.08% | 94.08% | 19.98% | 19.42% | 16.91% | 28.37% | <.0001 |
| High School Graduate | 23.57% | 1.75% | 23.06% | 22.51% | 25.29% | 29.82% | ||
| Some College | 29.32% | 4.17% | 39.24% | 29.19% | 29.47% | 21.63% | ||
| College Graduate | 24.03% | 0.00% | 17.72% | 28.88% | 28.33% | 20.18% | ||
|
| ||||||||
| Energy Intake | kcal | 2,180 ± 1,040 | 2,180 ± 1,071 | 2,399 ± 1,131 | 2,292 ± 954 | 2,116 ± 975 | 1,695 ± 787 | <.0001 |
|
| ||||||||
| Alcohol | Drinks/day past 12 months | 1.92 ± 2.65 | N/A | 3.303 ± 2.941 | 2.226 ± 2.633 | 1.469 ± 1.933 | 0.760 ± 1.316 | <.0001 |
|
| ||||||||
| Smoke | Days smoked past 30 Days | 5.88 ± 11.62 | N/A | 7.599 ± 11.261 | 7.072 ± 11.494 | 5.637 ± 11.460 | 2.561 ± 10.361 | <.0001 |
|
| ||||||||
| Number of Foods | # | 16.8 ± 6.3 | 13.0 ± 5.6 | 15.1 ± 5.6 | 16.8 ± 5.7 | 18.1 ± 6.2 | 18.2 ± 7.5 | <.0001 |
|
| ||||||||
| Depression | Yes | 23.82% | N/A | 22.74% | 26.79% | 21.64% | 21.50% | |
Values presented as Mean ± Standard Deviation or Percent. Alcohol, Smoking, and Depression was not measured in the youngest age group.
P value from ANOVA or Chi-Square, as appropriate
Figure 1.
A. Sleep duration assessed as a continuous variable across age groups. B. Proportion of the sample in each sleep duration category in each age group.
A. Habitual sleep duration by age group. B. Distribution of sleep duration categories by age group.
The sample was not evenly distributed across age groups. For the 16–17 group, there were N=272 individuals (4.85% of the sample, adjusted to 3.82% after weighting). For the 18–29 group, there were N=1,016 individuals (18.12% of the sample, adjusted to 21.12% after weighting). For the 30–49 group there were N=1,748 individuals (31.18%, adjusted to 36.86% after weighting). For the 50–64 group, there were N=1,293 individuals (23.05%, adjusted to 23.48% after weighting). Finally for those 65 and older, there were N=1,278 individuals (22.79% of the sample, adjusted to 14.71% after weighting).
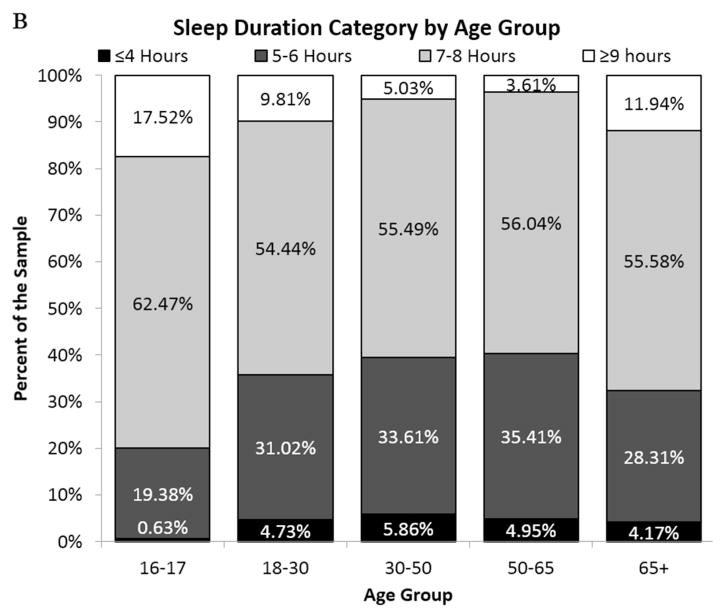
Linear relationships with continuous sleep duration
Results from linear regression analyses can be found in Table 2. In unadjusted analyses, shorter sleep duration was associated with higher BMI, but only among those in the 18–29 and 30–49 yrs age groups. No significant linear relationship was detected among other age groups. This pattern was maintained in adjusted analyses (which include sociodemographics) and fully-adjusted analyses (which include sociodemographics and health risk factors). A linear relationship between sleep duration and BMI was also observed for 16–17 year olds in the adjusted analysis only. These findings are displayed graphically in Figure 2, where filled markers indicate a relationship with P<0.05.
Table 2.
Linear Regression Results of Relationships Between Sleep Duration and Body Mass Index (BMI), Stratified by Age Group.
| Model | 16–17 | 18–29 | 30–49 | 50–64 | ≥65 |
|---|---|---|---|---|---|
| β (95% CI) | β (95% CI) | β (95% CI) | β (95% CI) | β (95% CI) | |
|
| |||||
| Unadjusted | −0.47 (−1.07, 0.14) | ***−0.75 (−1.12 – −0.38) | **−0.36 (−0.64 – −0.09) | −0.27 (−0.63 – 0.10) | −0.25 (−0.52 – 0.03) |
|
| |||||
| Adjusteda | *−0.57 (−1.13, −0.01) | ***−0.82 (−1.25 – −0.39) | *−0.35 (−0.63 – −0.06) | −0.26 (−0.65 – 0.13) | −0.26 (−0.55 – 0.02) |
|
| |||||
| Fully-Adjustedb | −0.54 (−1.10, 0.01) | ***−0.75 (−1.20, −0.31) | *−0.31 (−0.62, −0.00) | −0.34 (−0.73, 0.05) | −0.17 (−0.47, 0.13) |
β values reflect difference in BMI for each increased hour of sleep
P<0.05,
P<0.01,
P<0.001
Adjusted analyses include sex, race/ethnicity, marital status, exercise, income to poverty ratio, and education
Adjusted for sex, race/ethnicity, marital status, exercise, income to poverty ratio, education, total caloric intake, alcohol, smoking, number of foods in diet, and depression.
Figure 2.
Graphical depiction of regression results showing the relationship between continuous body mass index per hour of sleep, stratified by age group.
Difference in BMI per hour of sleep for each age group, predicted using regression. Filled symbols represent statistically significant findings.
Linear relationships with categorical sleep duration
Results from linear regression analyses with sleep duration categories can be found in Table 3. Among 18–29 year olds, in unadjusted analyses, elevated BMI was seen in very short (≤4 hours) and short (5–6 hours) sleepers, and lower BMI was seen in long (9+ hours) sleepers. In adjusted and fully-adjusted analyses, the relationships for short and very short sleep were maintained, though slightly attenuated. The finding for long sleep was no longer significant in these models (P<0.10). Among 30-49 year olds, short sleep duration (5–6 hours) was associated with elevated BMI in all models. No other significant relationships were found.
Table 3.
Relationships between Sleep Duration Category and BMI, stratified by Age Group.
| Model | Sleep Category | 16–17 | 18–29 | 30–49 | 50–64 | ≥65 |
|---|---|---|---|---|---|---|
| β (95% CI) | β (95% CI) | β (95% CI) | β (95% CI) | β (95% CI) | ||
|
| ||||||
| Unadjusted | ≤4 Hours | 5.22 (−2.82, 13.27) | ***4.32 (1.86, 6.78) | 1.23 (−0.00, 2.46) | 1.98 (−0.58, 4.54) | 1.24 (−0.54, 3.01) |
| 5–6 Hours | 1.48 (−0.61, 3.58) | *1.58 (0.35, 2.80) | **1.24 (0.42, 2.06) | 0.46 (−0.54, 1.46) | 0.76 (−0.23, 1.75) | |
| 7–8 Hours | Reference | Reference | Reference | Reference | Reference | |
| 9+ Hours | 0.30 (−2.18, 2.77) | *−1.43 (−2.78, −0.07) | 0.31 (−1.64, 2.26) | 0.13 (−1.79, 2.05) | −0.32 (−1.27, 0.63) | |
|
| ||||||
| Adjusteda | ≤4 Hours | 5.08 (−1.91, 12.07) | **3.49 (0.89, 6.09) | 0.77 (−0.48, 2.02) | 1.71 (−1.05, 4.46) | 1.38 (−0.34, 3.11) |
| 5–6 Hours | 0.97 (−0.93, 2.87) | **2.13 (0.77, 3.48) | **1.16 (0.32, 2.00) | 0.51 (−0.47, 1.49) | 0.78 (−0.21, 1.77) | |
| 7–8 Hours | Reference | Reference | Reference | Reference | Reference | |
| 9+ Hours | −0.14 (−2.61, 2.34) | −1.61 (−3.38, 0.15) | −0.02 (−1.95, 1.91) | 0.16 (−1.71, 2.02) | −0.35 (−1.34, 0.63) | |
|
| ||||||
| Fully-Adjustedb | ≤4 Hours | 4.91 (−2.03, 11.85) | 2.35 (−0.32, 5.01) | 0.44 (−0.92, 1.81) | 2.12 (−0.71, 4.94) | 1.30 (−0.48, 3.07) |
| 5–6 Hours | 1.49 (−0.48, 3.47) | *1.87 (0.44, 3.30) | **1.22 (0.32, 2.11) | 0.57 (−0.44, 1.59) | 0.50 (−0.54, 1.54) | |
| 7–8 Hours | Reference | Reference | Reference | Reference | Reference | |
| 9+ Hours | 0.46 (−1.93, 2.86) | −1.84 (−3.72, 0.04) | 0.01 (−2.06, 2.07) | 0.33 (−1.54, 2.20) | −0.17 (−1.22, 0.89) | |
β values reflect difference in BMI for each sleep duration group, relative to 7–8 hours.
P<0.05,
P<0.01,
P<0.001
Adjusted analyses include sex, race/ethnicity, marital status, exercise, income to poverty ratio, and education
Adjusted for sex, race/ethnicity, marital status, exercise, income to poverty ratio, education, total caloric intake, alcohol, smoking, number of foods in diet, and depression.
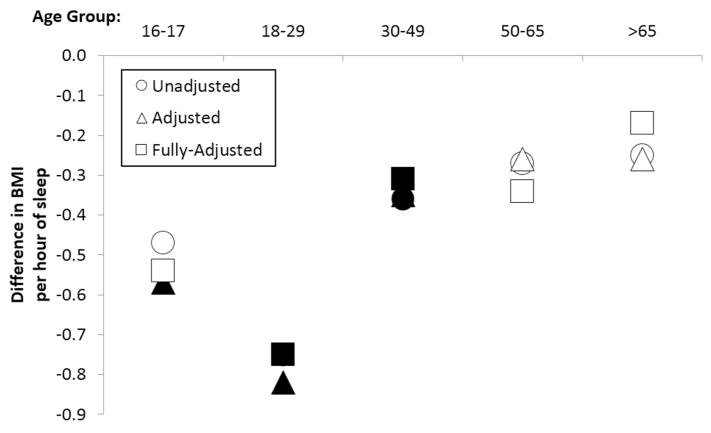
Interactions between sleep duration and age
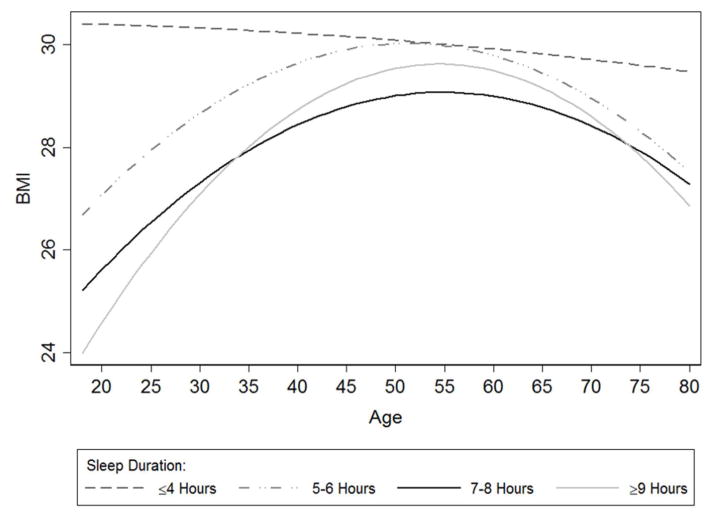
Sleep duration by age interaction terms in the fully-adjusted model were significant for both sleep duration variables. Thus, the relationship between sleep duration and BMI depended on age for both continuous (Pinteraction=0.014) and categorical (Pinteraction=0.035) sleep duration. The relationship between continuous sleep duration and BMI relative to age is depicted in Figure 3. As seen in this figure, a pseudo-linear relationship is seen among the youngest respondents, with the highest BMI associated with the shortest sleepers and the lowest BMI associated with the longest sleepers. This relationship flattens out and becomes slightly concave in middle age, with elevated BMI in both shorter and longer sleepers, and less of a relationship is seen among the oldest respondents.
Figure 3.
Three-dimensional plot of the relationship of sleep duration (continuous) and body mass index (continuous), as it depends on age (continuous).
Three-dimensional plot of regression results for the relationship between sleep duration and BMI, and how this varies by age, with all factors expressed as continuous variables.
An alternate pattern is seen in Figure 4, which depicts this relationship using sleep duration categories. In this Figure, the pseudo-linear relationship can be seen here as well, with the highest BMI in the shortest sleepers and the lowest BMI in the long sleepers. This finding progresses into a slightly U-shaped relationship in middle age respondents. Among the oldest respondents, there is little difference in BMI among sleep duration categories, except that the very short sleepers have nominally higher BMIs as compared to all of the other groups.
Figure 4.
Graphical representation of the relationship between categorical sleep duration and body mass index as it relates to age. Age is on the X axis and body mass index is on the Y axis, with separate lines for different sleep duration categories.
Plot of relationships between continuous age and continuous BMI stratified by sleep duration category.
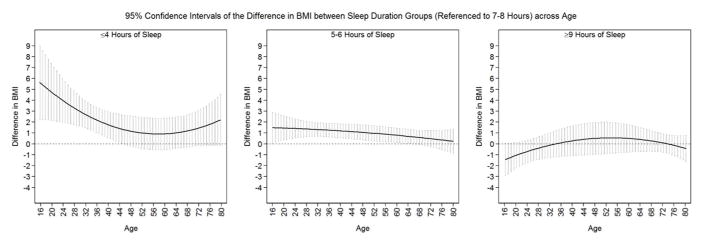
To test statistically these patterns, a post-hoc exploratory analysis was conducted (Figure 5). BMI values and 95% confidence intervals were plotted against values from 7–8 hour sleepers for each age. When the confidence interval does not cross the marker for 7–8 hours (the “0” line), that age group could be described as having a higher or lower BMI than the 7–8 hour sleepers. This figure demonstrates that although the very short sleepers (panel A) had consistently higher BMI values than the 7–8 hour sleepers, groups only differed among the younger respondents (perhaps due to power limitations). For the short sleepers (panel B), smaller, but more consistent differences were seen across age groups). The long sleepers (panel C) did demonstrate lower BMI values for younger respondents and higher BMI values for middle-aged respondents, but these differences were not statistically significant.
Figure 5.
Separate plots of the relationship between sleep duration category (relative to 7-8 hour sleepers) and body mass index, across age groups, with 95% confidence intervals for each age. This shows how there are significant relationships, but only in certain age ranges.
Regression results and 95% Confidence intervals of relationships between age and BMI for each sleep duration category, relative to 7–8 hours.
Stratification by Sex
Prior to stratification, interaction terms were computed for continuous and categorical sleep duration and are reported in Supplementary Table 1. Although none of the interactions were significant (thus mathematically not justifying stratification), we performed exploratory stratified analyses. Although not statistically significant, a trend towards a stronger relationship between sleep and BMI was observed in women compared to the men when stratifying by sex, as can be seen in Supplementary Tables 2 and 3. Since interaction terms were not significant, these results should be interpreted with appropriate caution, though.
Analysis of BMI Z-Scores
Analyses of BMI z-scores for the complete sample are reported in Supplementary Tables 4 and 5. Supplementary Table 4 shows that continuous sleep duration was associated with BMI zscores among 18–29 and 30–49 age groups. Supplementary Table 5 shows that sleep duration of ≤4 hours was associated with significantly higher BMI Z-scores among those age 16–17 and 18– 29, and sleep duration of 5–6 hours was associated with higher BMI z-scores among those age 18–29 and 30–49.
Sex-stratified results for analysis of BMI z-scores are reported in Supplementary Tables 6, 7, and 8. Supplementary Table 6 shows that there were no significant interactions, so interpretation of stratified analyses were performed with caution. Stratified analyses suggested a trend towards, as with BMI, relationships with BMI z-scores were generally stronger among women. As above, sex-stratified results (reported in Supplementary Tables 7 and 8) should be interpreted with appropriate caution.
DISCUSSION
This study examined data from the 2007–2008 NHANES to determine whether the relationship between sleep duration and BMI varies based on age. Sleep duration was assessed both continuously and categorically. In both cases, significant interactions were observed. Post-hoc analyses of these interactions identified a pattern such that younger adults demonstrate a relatively linear negative association between sleep duration and BMI, middle-aged adults show a more U-shaped relationship, and older adults show a more attenuated relationship, with a possible association only for very short sleep duration.
Sleep duration and BMI patterns associated with age
The present study examined age as both a continuous and categorical variable. This approach was taken because many previous studies of sleep across the lifespan have used age as a continuous variable, to chart differences in sleep by year. However, many previous studies have also shown that the relationship between sleep and age is nonlinear, and there may be important relationships that differ between adolescents, young adults, middle-aged adults, and older adults. For example, sleep need is greater among adolescents, subjective sleep disturbances peak in young adults, some sleep problems peak in middle age, women experience severe sleep problems due to menopause, and objective sleep disturbances are well-documented in the elderly. Given that 18–29 year olds tend to sleep more than older adults, the relationship between sleep and BMI could be most pronounced in this age group since short sleep compared to a longer sleep duration would be proportionally more sleep restriction than when total sleep time tends to be lower (as in middle/older adults). Also, exposure to different types of stress at different ages may play a role in both short sleep and higher BMI among various age groups20.
It is notable that the relationship in middle adulthood reflects a U-shaped association, such that long sleep is also associated with higher BMI. This age range may be associated with hormonal changes in both men and women, though this relationship may be more pronounced in women21. The present study attempted to account for variables known to affect sleep and health outcomes, but it is plausible that unknown covariates (i.e. residual confounding) were not accounted for in the analysis.
It is plausible that the reason for attenuated results among older adults reflects accumulated morbidity, such that effects of sleep on body weight have already manifest or other accumulated effects on BMI have overshadowed effects of current sleep. Also, adults who survive to old age tend to be healthier than those who have succumbed (i.e., survivor effects). Perhaps individuals with a lifetime of suboptimal sleep, especially in those for whom sleep would play a major impact in these factors, did not survive to older age. This notion is consistent with findings related to sleep apnea in the elderly where a protective effect of apnea has been postulated 22. Although untreated sleep apnea is associated with elevated cardiometabolic mortality risk, this risk is significantly attenuated in the elderly 23.
Previous studies of sleep duration and BMI
Previous studies have found inconsistent results when examining sleep duration and BMI. After examining the ages of participants in the conflicting studies, varying age ranges and average ages of the participants may explain the varying results24. Marshall, Glozier and Grunstein24 examined inconsistent findings by age group and found similar age-related patterns. For instance, several studies had large age ranges such as: 17–65 (N=64,110)25, 20–80 (N=1,042)26, 20–92 (n=1,203)27, 30–81 (N=316)28, 30–102 (N=1,116,936)29 and 17–83 (N=4,793)30. Although a large age range may improve generalizability of the sample, the inclusion of age as a linear covariate may be obscuring the relationship between BMI and sleep duration. This notion may especially be the case for studies which included multiple age ranges, reflecting different patterns of association.
Studies that included greater numbers of younger participants tended to find a linear relationship25, 31, 32, 33. Studies with middle-aged participants more frequently found U-shaped associations between sleep duration and BMI/obesity29, 34, 35 or at least found part of this U-shape relationship with long sleepers having higher BMI36. Nagai and colleagues37 found that long sleep duration increased the risk of a participant’s gaining weight, but only if they were already obese. Hasler and colleagues suggest that part of the relationship between short and/or long sleep and obesity may depend on age-related patterns of psychopathology38. Previous research has shown that the relationship between sleep and weight decreased with age39, which is also what was found in the current study.
Limitations
There are several limitations with the current study. One is that this is a cross-sectional analysis, therefore we cannot make inferences with regards to causality. Future research should include a greater emphasis on longitudinal studies to examine how sleep and BMI vary by age within an individual over time. Multiple longitudinal cohorts with different ages of participants would help to corroborate and extend our findings. Mechanistic research is also critical to draw rigorous conclusions.
In addition, sleep duration was measured by a single self-report item. More reliable results could be achieved through objective means (e.g., actigraphy) or other prospective self-reports (e.g., sleep diaries). Also, asking for an overall sleep duration may be less accurate than using validated questionnaires that include measures of sleep duration, or getting multiple subjective sleep durations over several days or weeks (including weekends), or computing sleep duration based on sleep timing24, 40. Nonetheless, we view a single self-reported sleep duration as a crucial variable clinically, since clinicians will typically intervene based on this information rather than more objectively obtained longitudinal data.
A third limitation is that there were relatively small sample sizes for both extreme sleep durations as well as extreme age groups. These power limitations resulted in unstable parameter estimates. Also, there could be additional factors affecting some of these smaller groups. As mentioned above, there might be something systematically different about middle-aged adults who are able to sleep nine or more hours a day, especially given that people in this age cohort tend to work, raise families, and otherwise maintain schedules where excessive sleep duration is unfeasible. Further research should seek underlying mechanisms and to acquire larger samples of participants from extreme sleep durations and age groups so as to maximize statistical predictions.
Conclusions
This current study attempts to explain why there have been inconsistent results when examining sleep duration and BMI. The relationship between these two variables likely depends on age. In young adults, this relationship between sleep and BMI is linear, where more sleep is associated with lower BMI. However, this relationship changes for the middle-aged where 7–8 hours of sleep is associated with the lowest BMI, and both short and long sleepers tend to have a higher BMI. In older adults, the association between sleep duration and BMI weakens. Due to the changing relationship among age, sleep and BMI, these data suggest that simply including age as a linear covariate may not most accurately account for this relationship. Researchers may need to consider stratification for different age groups.
Supplementary Material
What is already known?
Habitual short sleep duration is associated with obesity.
Sleep need, sleep-related behaviors, and obesity risk all vary by age.
Some studies show obesity risks associated with long sleep duration as well.
What does this study add?
The relationship between sleep duration and BMI is not consistent in all age groups.
There is more of a linear relationship in youth, a U-shaped relationship in middle age and an unclear relationship in older age
These findings explain some of the inconsistencies in the epidemiologic literature and may inform future mechanistic research
Acknowledgments
This work was supported by 12SDG9180007 (AHA), K23HL110216 (NHLBI), R21ES022931 (NIEHS), and the University of Pennsylvania CTSA (UL1RR024134). Also, we wish to thank the Centers for Disease Control and Prevention for collecting these data and making them available, as well as the NHANES participants.
Footnotes
DISCLOSURE STATEMENT
The authors report no conflicts of interest.
References
- 1.Hubacek JA. Eat less and exercise more - is it really enough to knock down the obesity pandemia? Physiol Res. 2009;58(Suppl 1):S1–6. doi: 10.33549/physiolres.931855. [DOI] [PubMed] [Google Scholar]
- 2.Knutson KL. Does inadequate sleep play a role in vulnerability to obesity? Am J Hum Biol. 2012;24(3):361–371. doi: 10.1002/ajhb.22219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patel SR. Reduced sleep as an obesity risk factor. Obes Rev. 2009;10(Suppl 2):61–68. doi: 10.1111/j.1467-789X.2009.00664.x. [DOI] [PubMed] [Google Scholar]
- 4.Knutson KL, Van Cauter E. Associations between sleep loss and increased risk of obesity and diabetes. Ann N Y Acad Sci. 2008;1129:287–304. doi: 10.1196/annals.1417.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spiegel K, Tasali E, Penev P, Van Cauter E. Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004;141(11):846–850. doi: 10.7326/0003-4819-141-11-200412070-00008. [DOI] [PubMed] [Google Scholar]
- 6.St-Onge MP, Roberts AL, Chen J, Kelleman M, O'Keeffe M, Roy Choudhury A, et al. Short sleep duration increases energy intakes but does not change energy expenditure in normal-weight individuals. Am J Clin Nutr. 2011;94(2):410–416. doi: 10.3945/ajcn.111.013904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grandner MA, Sands-Lincoln MR, Pak VM, Garland SN. Sleep duration, cardiovascular disease, and proinflammatory biomarkers. Nat Sci Sleep. 2013;5:93–107. doi: 10.2147/NSS.S31063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grandner MA, Kripke DF. Self-reported sleep complaints with long and short sleep: a nationally representative sample. Psychosom Med. 2004;66(2):239–241. doi: 10.1097/01.psy.0000107881.53228.4d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grandner MA, Chakravorty S, Perlis ML, Oliver L, Gurubhagavatula I. Habitual sleep duration associated with self-reported and objectively determined cardiometabolic risk factors. Sleep Med. 2014;15(1):42–50. doi: 10.1016/j.sleep.2013.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Altman NG, Izci-Balserak B, Schopfer E, Jackson N, Rattanaumpawan P, Gehrman PR, et al. Sleep duration versus sleep insufficiency as predictors of cardiometabolic health outcomes. Sleep Med. 2012;13(10):1261–1270. doi: 10.1016/j.sleep.2012.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1(3):e62. doi: 10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grandner MA, Patel NP, Hale L, Moore M. Mortality associated with sleep duration: The evidence, the possible mechanisms, and the future. Sleep Med Rev. 2010;14:191–203. doi: 10.1016/j.smrv.2009.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Duffy JF, Willson HJ, Wang W, Czeisler CA. Healthy older adults better tolerate sleep deprivation than young adults. J Am Geriatr Soc. 2009;57(7):1245–1251. doi: 10.1111/j.1532-5415.2009.02303.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention; U.S. Department of Health and Human Services, editor. National Health and Nutrition Examination Survey Data. Hyattsville, MD: National Center for Health Statistics; 2008. [Google Scholar]
- 15.Centers for Disease Control and Prevention. Analytic and Reporting Guidelines: The National Health and Nutrition Examination Survey (NHANES) National Center for Health Statistics; Hyattsville, MD: 2006. [Google Scholar]
- 16.Grandner MA, Patel NP, Gehrman PR, Perlis ML, Pack AI. Problems associated with short sleep: Bridging the gap between laboratory and epidemiological studies. Sleep Med Rev. 2010;14:239–247. doi: 10.1016/j.smrv.2009.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention. Anthropometry Procedures Manual. National Center for Health Statistics; Hyattsville, MD: 2007. [Google Scholar]
- 18.Centers for Disease Control and Prevention. MEC In-Person Dietary Interviewers Procedures Manual. National Center for Health Statistics; Hyattsville, MD: 2008. [Google Scholar]
- 19.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320(7244):1240–1243. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Slopen N, Williams DR. Discrimination, other psychosocial stressors, and self-reported sleep duration and difficulties. Sleep. 2014;37(1):147–156. doi: 10.5665/sleep.3326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grandner MA, Martin JL, Patel NP, Jackson NJ, Gehrman PR, Pien G, et al. Age and sleep disturbances among american men and women: data from the u.s. Behavioral risk factor surveillance system. Sleep. 2012;35(3):395–406. doi: 10.5665/sleep.1704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lavie P, Lavie L. Unexpected survival advantage in elderly people with moderate sleep apnoea. J Sleep Res. 2009;18(4):397–403. doi: 10.1111/j.1365-2869.2009.00754.x. [DOI] [PubMed] [Google Scholar]
- 23.Ancoli-Israel S, DuHamel ER, Stepnowsky C, Engler R, Cohen-Zion M, Marler M. The relationship between congestive heart failure, sleep apnea, and mortality in older men. Chest. 2003;124(4):1400–1405. doi: 10.1378/chest.124.4.1400. [DOI] [PubMed] [Google Scholar]
- 24.Marshall NS, Glozier N, Grunstein RR. Is sleep duration related to obesity? A critical review of the epidemiological evidence. Sleep Med Rev. 2008;12(4):289–298. doi: 10.1016/j.smrv.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 25.Roenneberg T, Allebrandt KV, Merrow M, Vetter C. Social jetlag and obesity. Curr Biol. 2012;22(10):939–943. doi: 10.1016/j.cub.2012.03.038. [DOI] [PubMed] [Google Scholar]
- 26.Moraes W, Poyares D, Zalcman I, de Mello MT, Bittencourt LR, Santos-Silva R, et al. Association between body mass index and sleep duration assessed by objective methods in a representative sample of the adult population. Sleep Med. 2013;14(4):312–318. doi: 10.1016/j.sleep.2012.11.010. [DOI] [PubMed] [Google Scholar]
- 27.Stamatakis KA, Brownson RC. Sleep duration and obesity-related risk factors in the rural Midwest. Prev Med. 2008;46(5):439–444. doi: 10.1016/j.ypmed.2007.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O'Brien EM, Fava J, Subak LL, Stone K, Hart CN, Demos K, et al. Sleep duration and weight loss among overweight/obese women enrolled in a behavioral weight loss program. Nutrition & diabetes. 2012;2:e43. doi: 10.1038/nutd.2012.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59(2):131–136. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 30.Ko GT, Chan JC, Chan AW, Wong PT, Hui SS, Tong SD, et al. Association between sleeping hours, working hours and obesity in Hong Kong Chinese: the 'better health for better Hong Kong' health promotion campaign. Int J Obes (Lond) 2007;31(2):254–260. doi: 10.1038/sj.ijo.0803389. [DOI] [PubMed] [Google Scholar]
- 31.Meyer KA, Wall MM, Larson NI, Laska MN, Neumark-Sztainer D. Sleep duration and BMI in a sample of young adults. Obesity (Silver Spring) 2012;20(6):1279–1287. doi: 10.1038/oby.2011.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vioque J, Torres A, Quiles J. Time spent watching television, sleep duration and obesity in adults living in Valencia, Spain. Int J Obes Relat Metab Disord. 2000;24(12):1683–1688. doi: 10.1038/sj.ijo.0801434. [DOI] [PubMed] [Google Scholar]
- 33.Hasler G, Buysse DJ, Klaghofer R, Gamma A, Ajdacic V, Eich D, et al. The association between short sleep duration and obesity in young adults: a 13-year prospective study. Sleep. 2004;27(4):661–666. doi: 10.1093/sleep/27.4.661. [DOI] [PubMed] [Google Scholar]
- 34.Chaput JP, Despres JP, Bouchard C, Tremblay A. The association between sleep duration and weight gain in adults: a 6-year prospective study from the Quebec Family Study. Sleep. 2008;31(4):517–523. doi: 10.1093/sleep/31.4.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bjorvatn B, Sagen IM, Oyane N, Waage S, Fetveit A, Pallesen S, et al. The association between sleep duration, body mass index and metabolic measures in the Hordaland Health Study. J Sleep Res. 2007;16(1):66–76. doi: 10.1111/j.1365-2869.2007.00569.x. [DOI] [PubMed] [Google Scholar]
- 36.Tu X, Cai H, Gao YT, Wu X, Ji BT, Yang G, et al. Sleep duration and its correlates in middle-aged and elderly Chinese women: the Shanghai Women's Health Study. Sleep Med. 2012;13(9):1138–1145. doi: 10.1016/j.sleep.2012.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nagai M, Tomata Y, Watanabe T, Kakizaki M, Tsuji I. Association between sleep duration, weight gain, and obesity for long period. Sleep Med. 2013;14(2):206–210. doi: 10.1016/j.sleep.2012.09.024. [DOI] [PubMed] [Google Scholar]
- 38.Hasler G, Pine DS, Gamma A, Milos G, Ajdacic V, Eich D, et al. The associations between psychopathology and being overweight: a 20-year prospective study. Psychol Med. 2004;34(6):1047–1057. doi: 10.1017/s0033291703001697. [DOI] [PubMed] [Google Scholar]
- 39.Patel SR, Blackwell T, Redline S, Ancoli-Israel S, Cauley JA, Hillier TA, et al. The association between sleep duration and obesity in older adults. Int J Obes (Lond) 2008;32(12):1825–1834. doi: 10.1038/ijo.2008.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kurina LM, McClintock MK, Chen JH, Waite LJ, Thisted RA, Lauderdale DS. Sleep duration and allcause mortality: a critical review of measurement and associations. Ann Epidemiol. 2013;23(6):361–370. doi: 10.1016/j.annepidem.2013.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.