Abstract
Background:
Recent attempts have been focused on employing chemical and natural supplemental agents for treatment of cyclic mastalgia. Among various agents, the potential effects of vitamins remain questionable. In the present study, we examined the efficacy of two types of these vitamin supplements (vitamin E and vitamin B6) in improving pain severity in cyclic mastalgia.
Materials and Methods:
In a randomized double-blinded clinical trial, 80 patients suffering from cyclic mastalgia were randomly assigned to receive 200 IU of vitamin E daily or 40 mg/day of vitamin B6 for 2 months. Written informed consent was obtained from all participants. Severity of breast pain was detected by the Cardiff breast pain score during one menstrual cycle before and two menstrual cycles after the intervention. Data were analyzed using t-test, Chi-squared test, analysis of variance (ANOVA), and regression with SPSS version 19 and P < 0.05 was considered significant.
Results:
There was no significant difference in the mean of severity of cyclic mastalgia during one menstrual cycle before the intervention between the vitamin E and B6 groups (9.1 ± 2.1 and 8.4 ± 3.1, respectively), but the difference was significant during the first cycle (5.1 ± 1.6 and 5.2 ± 2.5, respectively) and the second menstrual cycle (2.3 ± 1.0 and 2.6 ± 2.0, respectively) in the two groups after the intervention. The trend of changes in pain severity score showed significant downward trend of pain severity score within the study period in both the treatment groups (P < 0.001), while these trends were similar in both groups when examined by the repeated-measure ANOVA test. By multivariable linear regression analysis adjusted for baseline variables, we found that both the treatment regimens resulted in similar reduction in breast pain severity (P = 0.067).
Conclusions:
Both regimens containing vitamin E and vitamin B6 are similar in reducing breast pain severity in cyclic mastalgia.
Keywords: Breast pain, cyclic mastalgia, vitamin B6, vitamin E
INTRODUCTION
Some women's breasts are unusually tender and lumpy, with symptoms of pain and dull heaviness that vary with the menstrual cycle. This condition is called cyclic mastalgia and is often associated with premenstrual syndrome. Among women, the reported prevalence of mastalgia ranges from 41 to 79%, and the most common type is associated with menstruation. Cyclic mastalgia typically occurs monthly before the beginning of the menstrual period, is of mild severity, and is relieved within 7 days of the onset of menses. Spontaneous remission often occurs, but many women experience cyclic mastalgia for years, often with increasing severity until menopause. In some women, this pain interferes with activity, relationships, and quality of life. Cyclic mastalgia interferes with sexual activity (48%), Physical and social activities (21%), and employment or education (8%).[1]
Cyclical mastalgia may be associated with excessive use of mammograms with unnecessary, ineffective, or undesirable self-medication. When the lumps become significant enough to be called cysts, the condition is called fibrocystic breast disease. Besides discomfort, perhaps the worst problem of this condition is that it can mimic the appearance of breast cancer on mammograms, leading to false alarms. To make matters worse, fibrocystic changes can also hide true cancers, and some evidence hints that women with fibrocystic breast disease may also have a greater tendency toward breast cancer.[1,2]
The main etiologies of cyclic mastalgia remain unknown. However, various physiological conditions, inflammatory processes, and even underlying psychological disturbances have been postulated in affected patients.[1] Among pathophysiological aspects, increased water retention in breast and ductal ectasia have been suggested to be the causes in these patients.[2] Also, regarding the role of inflammatory mechanisms, increased level of some inflammatory biomarkers such as some interleukins (IL-6 and IL-1α) and tissue necrotizing factor (TNF-α) has been reported following the appearance of cyclic mastalgia.[3] Recently, perceived stress and anxiety has been found to be associated with cyclic mastalgia. Cyclic mastalgia is one of the major causes of breast pain for women visiting primary care clinics.[4] Due to the multifactorial features of this phenomenon, its management using single drug regimens seems not to be proper.
Recent attempts have been focused on employing chemical and natural supplemental agents for treatment of cyclic mastalgia. Among synthetic agents, the potential effects of some drugs such as Danazol as a gonadotrophin release inhibitor,[5,6] Bromocriptine as a dopamine agonist,[7,8,9] Tamoxifen as an anti-estrogen,[10,11] and Goserline as a, luteinizing Hormone-Releasing Hormone (LHRH) analog [12] have been examined and their benefits have been proved. However, the low response rate along with their serious side effects have limited their prescription and continued usage. In order to overcome these limitations, some approaches have started using agents of natural origin.
Evening primrose (Oenothera biennis) is a North American wild flower that has escaped cultivation and is a precursor of prostaglandin E1, which is one of the anti-inflammatory prostaglandins.[13,14] Because of the underlying abnormal metabolism of fatty acids in cyclic mastalgia and as this oil is rich in essential fatty acids, the use of this agent has been also considered as a first-line treatment for cyclic mastalgia.[15]
Recently, it has been recommended to add an antioxidant agent or co-factors in the proposed metabolic pathway for enhancing the therapeutic efficacy of other drugs.[16] In fact, these agents may be considered as safe alternatives to hormonal therapies or may be used in combination with hormonal drugs as they result in lesser drug-related side effects. Even these co-factor supplements may be employed for treatment of cyclic mastalgia. In the present study, we examined the efficacy of two types of vitamin supplements (vitamin E and vitamin B6) in improving pain severity in cyclic mastalgia.
MATERIALS AND METHODS
In this randomized, double-blinded clinical trial, Trial registration code of project was IRCT201106266888N1 80 patients of reproductive age who were suffering from cyclic mastalgia and referred to the medical and health centers in Hamadan city were included. They were randomly allocated into two groups. The main inclusion criteria were: Diagnosis of cyclic mastalgia, no previous history of breast malignancies, and not having consumed other vitamin supplements within 2 months of the study period. The main exclusion criteria included allergy to drug, pregnancy, and unwillingness to continue in the research.
Study design was approved by the ethics committee of Hamadan University of Medical Sciences and written informed consent was obtained from all participants. On admission to clinic, all relevant information was collected by interviewing, including demographic characteristics, marital state, occupation, educational level, characteristics related to cyclic mastalgia such as its time and duration, characteristics related to menstrual cycles, results of diagnostic interventions (breast sonography and mammography), and also, previous history of psychological disorders including depression or anxiety. Cyclical mastalgia was defined as a bilateral painful breast swelling lasting for >4 days and up to 3 weeks, premenstrually and always preceding menses, and subsiding progressively during menstruation.[17] After initial evaluation, patients with cyclic mastalgia were randomly assigned to receive 200 IU vitamin E daily or 40 mg/day vitamin B6 for 2 months. Severity of cyclic mastalgia was determined by the Cardiff breast pain score during one cycle before and two cycles after the intervention. Cardiff breast pain score was finally classified as one of the following levels: None, mild, moderate, or severe breast pain. Cyclical mastalgia characterized by a swelling and minor discomfort lasting 1–4 days premenstrually is considered mild and the symptoms lasting for 5–14 days or more every month is considered moderate to severe.[17,18]
The Cardiff breast pain chart has been utilized and it is a daily chart for monitoring breast pain, as shown in Figure 1.
Figure 1.
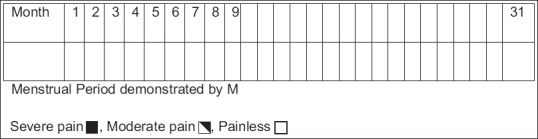
Cardiff breast pain chart (daily chart of breast pain)
Results were reported as mean and standard deviation (SD) for the quantitative variables and percentages for the categorical variables. The groups were compared using the Student's t-test or Mann–Whitney U test for the continuous variables and the Chi-square test (or Fisher's exact test if required) for the categorical variables. Trend of changes in pain severity score within the study period (during one menstrual cycle before and two menstrual cycles after the intervention) was examined by repeated-measure analysis of variance (ANOVA) test. The change in pain severity score was also examined by multivariate regression analysis to examine the treatment efficacy of the treatment protocols, with the baseline variables considered as probable potential confounders. P values of 0.05 or less were considered statistically significant. All the statistical analyses were performed using SPSS version 19.0.
RESULTS
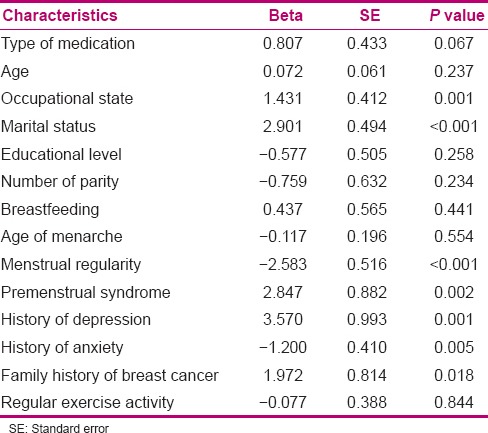
As shown in Table 1, the two groups treated with vitamin E and vitamin B6 were comparable in terms of baseline characteristics including age, age of marriage, socioeconomic level, body mass index, marital status, as well as the number of parity and menstrual regularity. Also, family history of breast cancer, exercise activity, and history of anxiety were similar between both groups. However, breastfeeding was reported to be more in the group treated with vitamin E and the mean age of menarche was also lower in this group compared with vitamin B6 group. Also, the prevalence of some underling comorbidities including premenstrual syndrome, pelvic pain, and history of depression was higher in the latter group. There was no significant difference in the mean of severity of cyclic mastalgia during one menstrual cycle before the intervention between the vitamin E and B6 groups (9.1 ± 2.1 and 8.4 ± 3.1, respectively), but the difference was significant in the two groups during the first cycle (5.1 ± 1.6 and 5.2 ± 2.5, respectively) and the second menstrual cycle (2.3 ± 1.0 and 2.6 ± 2.0, respectively) after the intervention. The trend of changes in pain severity score showed significant downward trend of pain severity score within the study period in both the treatment groups (P > 0.001) [Figure 1], while these trends were similar in both groups when examined by the repeated-measure ANOVA test [Table 2 and Figure 2]. By multivariable linear regression analysis adjusted for baseline variables [Table 3], it was found that both the treatment regimens resulted in similar reduction in breast pain severity. Vitamins E and B6 are the most effective and least toxic agents available for the treatment of breast pain [β = 0.807, standard error (SE) = 0.433, P = 0.067].
Table 1.
Baseline characteristics and clinical data of the study population
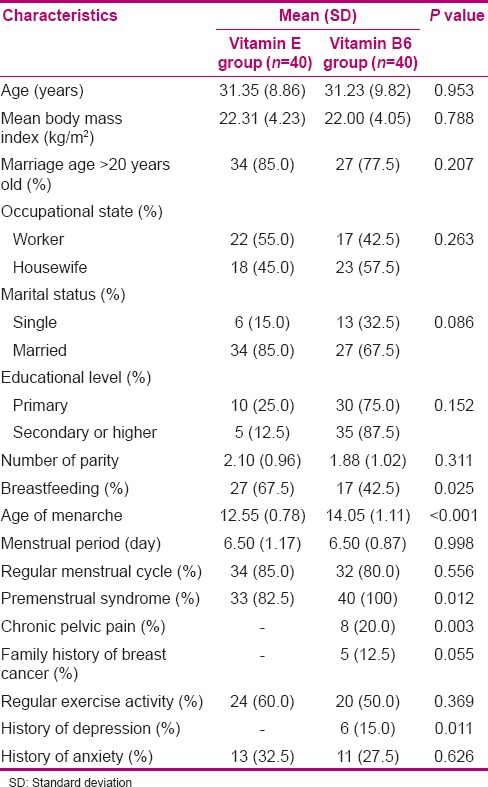
Table 2.
Level of pain severity in the two treatment groups
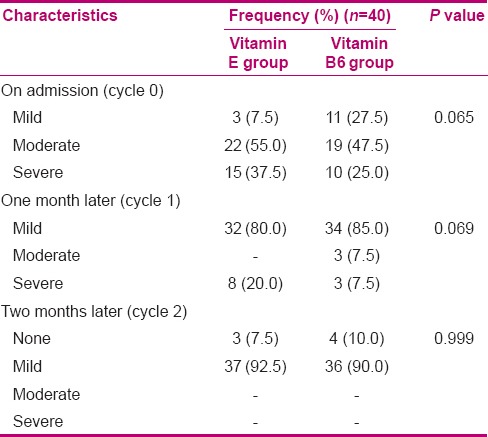
Figure 2.
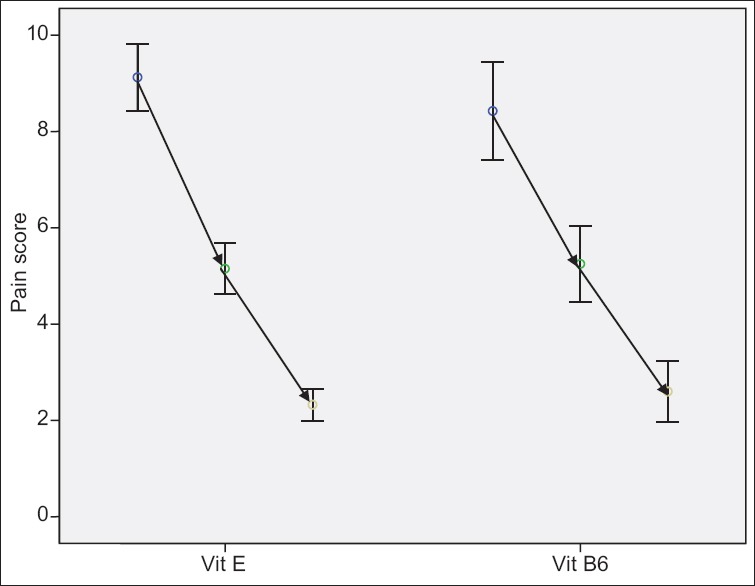
Trend of the changes in the pain severity score in the Vitamin E group and vitamin B6 group [although in both groups, this trend was gradually reducing (P < 0.001), the trend was similar across the two groups (P = 0.807)]
Table 3.
Multivariate linear regression model for comparing the effect of drugs on pain severity
DISCUSSION
Adding an antioxidant agent to first-line therapeutic regimes for treatment of cyclical mastalgia has been shown to be an effective schedule. Recently, direct attention has been paid toward using vitamins to facilitate pain relief in these patients. It has been suggested that use of adequate levels of vitamins as co-factors in the proposed metabolic pathways involving this complaint may be fully beneficial.[19] Although some controlled trials could demonstrate the effects of vitamins in relieving cyclical mastalgia pain, some others failed to support the efficacy. Thus, previous studies gave questionable results with conflicting evidence.[20,21,22] In a similar randomized trial of Iranian women suffering from mastalgia, administration of 200 mg twice daily could effectively reduce pain severity both 2 and 4 months after treatment, compared with the placebo group.[23] In another trial, daily doses of 1200 IU vitamin E alone or in combination with evening primrose oil taken for 6 months decreased the severity of cyclical mastalgia.[24] Also, a study similar to the present trial was conducted in the United Kingdom by Goyal and Mansel, who used a combination treatment arm of antioxidants and minerals which included beta-carotene, vitamin C, vitamin B6, zinc, niacin, and selenium in a coconut oil base and essential fatty acids. The investigators obtained equivocal results in the reduction of breast pain symptoms.[25] Three clinical trials have been performed, and all have shown vitamin E to be no better than placebo in the treatment of benign breast disease. In the first trial, 50 patients were asked whether their breast pain was better, worse, or unchanged after 2–3 months of therapy. In each group, 40% reported improvement.[26] The second trial did not assess breast pain, but found no reduction in nodularity.[27] The third trial found no reduction in nodularity or mammographic density, and although a larger proportion of women in the vitamin E group reported reduction in breast tenderness, this was statistically not significant.[28] Contrarily, some studies could not find beneficial effects of supplemental vitamins on mastalgia, probably because of small sample size or inappropriate nature of the study designs including ignoring adequate inclusion criteria or incorrect adjusting for confounders.[29,30,31] In uncontrolled studies, vitamin B6 has been used to treat cyclical mastalgia with mixed results. A small (n = 42), double-blinded, controlled study found that vitamin B6 did not significantly reduce cyclical mastalgia at a dose of 200 mg daily, as compared with a placebo.[31] Considering the key role of oxidation and inflammation processes in the appearance and expansion of cyclical mastalgia, it is believed that the use of vitamin supplements, especially of our studied vitamins, can successfully decrease the pain severity related to this phenomenon. However, it seems that the dosages of vitamins, duration of administration, as well as using them concurrently with other standard therapeutic regimens can all potentially influence the clinical results of these regimens, and thus, examining different regimens containing these vitamins in different doses and durations should be considered.
CONCLUSION
Both regimens containing vitamin E and vitamin B6 can similarly reduce breast pain severity in cyclic mastalgia. It seems that the dosages of vitamins, duration of administration, as well as using them concurrently with other standard therapeutic regimens can all potentially influence the clinical results of these regimens, and thus, examining different regimens containing these vitamins in different doses and durations should be considered.
ACKNOWLEDGMENTS
The authors would like to thank the staff of Hamadan University of Medical Sciences, Hamadan, Iran, for their valuable support and participation. This article is the result of a research project that was approved by the Research Deputy of Hamadan University of Medical Sciences. The project has been funded by the Research Deputy of Hamadan University of Medical Sciences.
Footnotes
Source of Support: The project has been funded by the Research Center for Child and Maternity Care, School of Nursing and Midwifery, Hamadan University of Medical Sciences, Hamadan, Iran
Conflict of Interest: The authors declare that they have no conflicts of interest in this article.
REFERENCES
- 1.Srivastava A, Mansel RE, Arvind N, Prasad K, Dhar A, Chabra A. Evidence-based management of Mastalgia: A meta-analysis of randomised trials. Breast. 2007;16:503–12. doi: 10.1016/j.breast.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 2.Olawaiye A, Withiam-Leitch M, Danakas G, Kahn K. Mastalgia: A review of management. J Reprod Med. 2005;50:933–9. [PubMed] [Google Scholar]
- 3.Smith RL, Pruthi S, Fitzpatrick LA. Evaluation and management of breast pain. Mayo Clin Proc. 2004;79:353–72. doi: 10.4065/79.3.353. [DOI] [PubMed] [Google Scholar]
- 4.Padden DL. Mastalgia: Evaluation and management. Nurse Pract Forum. 2000;11:213–8. [PubMed] [Google Scholar]
- 5.Tejwani PL, Srivastava A, Nerkar H, Dhar A, Hari S, Thulkar S, et al. Centchroman regresses mastalgia: A randomized comparison with danazol. Indian J Surg. 2011;73:199–205. doi: 10.1007/s12262-010-0216-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O’Brien PM, Abukhalil IE. Randomized controlled trial of the management of premenstrual syndrome and premenstrual mastalgia using luteal phase-only danazol. Am J Obstet Gynecol. 1999;180:18–23. doi: 10.1016/s0002-9378(99)70142-0. [DOI] [PubMed] [Google Scholar]
- 7.Mansel RE, Preece PE, Hughes LE. A double blind trial of the prolactin inhibitor bromocriptine in painful benign breast disease. Br J Surg. 1978;65:724–7. doi: 10.1002/bjs.1800651015. [DOI] [PubMed] [Google Scholar]
- 8.Aydin Y, Atis A, Kaleli S, Uludağ S, Goker N. Cabergoline versus bromocriptine for symptomatic treatment of premenstrual mastalgia: A randomised, open-label study. Eur J Obstet Gynecol Reprod Biol. 2010;150:203–6. doi: 10.1016/j.ejogrb.2010.02.024. [DOI] [PubMed] [Google Scholar]
- 9.Saied GM, Kamel RM, Dessouki N. Low intensity laser therapy is comparable to bromocriptine-evening primrose oil for the treatment of cyclical mastalgia in Egyptian females. Tanzan Health Res Bull. 2007;9:196–201. [PubMed] [Google Scholar]
- 10.Tehranian N, Fatemeh Shobeiri F, Hafezi Pour F, Hagizadeh E. Risk factors for breast cancer in Iranian women aged less than 40 years. Asian Pacific J Cancer Prev. 2010;11:1723–5. [PubMed] [Google Scholar]
- 11.Fentiman IS, Caleffi M, Brame K, Chaudary MA, Hayward JL. Double-blind controlled trial of tamoxifen therapy for mastalgia. Lancet. 1986;1:287–8. doi: 10.1016/s0140-6736(86)90825-1. [DOI] [PubMed] [Google Scholar]
- 12.Mansel RE, Goyal A, Preece P, Leinster S, Maddox PR, Gateley C, et al. European randomized, multicenter study of goserelin (Zoladex) in the management of mastalgia. Am J Obstet Gynecol. 2004;191:1942–9. doi: 10.1016/j.ajog.2004.06.100. [DOI] [PubMed] [Google Scholar]
- 13.Sharma N, Gupta A, Jha PK, Rajput P. Mastalgia cured! Randomized trial comparing centchroman to evening primrose oil. Breast J. 2012;18:509–10. doi: 10.1111/j.1524-4741.2012.01288.x. [DOI] [PubMed] [Google Scholar]
- 14.Bayles B, Usatine R. Evening primrose oil. Am Fam Physician. 2009;80:1405–8. [PubMed] [Google Scholar]
- 15.Stonemetz D. A review of the clinical efficacy of evening primrose. Holist Nurs Pract. 2008;22:171–4. doi: 10.1097/01.HNP.0000318026.45527.07. [DOI] [PubMed] [Google Scholar]
- 16.Rosolowich V, Saettler E, Szuck B, Lea RH, Levesque P, Weisberg F, et al. Society of Obstetricians and Gynecologists of Canada (SOGC). Mastalgia. J Obstet Gynaecol Can. 2006;28:49–71. doi: 10.1016/S1701-2163(16)32027-8. quiz 58-60, 72-4. [DOI] [PubMed] [Google Scholar]
- 17.Plu-Bureau G, Lê MG, Sitruk-Ware R, Thalabard JC. Cyclical mastalgia and breast cancer risk: Results of a French cohort study. Cancer Epidemiol Biomarkers Prev. 2006;15:1229–31. doi: 10.1158/1055-9965.EPI-05-0745. [DOI] [PubMed] [Google Scholar]
- 18.Gateley CA, Miers M, Mansel RE, Hughes LE. Drug treatment for mastalgia: 17 years experience in the Cardiff Mastalgia Clinic. J R Soc Med. 1992;85:12–5. doi: 10.1177/014107689208500105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mansel RE, Fenn NJ, Davies EL. Benign breast disease and its management. In: Taylor I, Johnson CD, editors. Recent Advance in Surgery No. 21. Edinburgh: Churchill Livingstone; 1988. pp. 71–83. [Google Scholar]
- 20.Millet AV, Dirbas FM. Clinical management of breast pain: A review. Obstet Gynecol Surv. 2002;57:451–61. doi: 10.1097/00006254-200207000-00022. [DOI] [PubMed] [Google Scholar]
- 21.Pye JK, Mansel RE, Hughes LE. Clinical experience of drug treatments for mastalgia. Lancet. 1985;2:373–7. doi: 10.1016/s0140-6736(85)92506-1. [DOI] [PubMed] [Google Scholar]
- 22.Faiz O, Fentiman IS. Management of breast pain. Int J Clin Prac. 2000;54:228–32. [PubMed] [Google Scholar]
- 23.Parsay S, Olfati F, Nahidi S. Therapeutic effects of vitamin E on cyclic mastalgia. Breast J. 2009;15:510–4. doi: 10.1111/j.1524-4741.2009.00768.x. [DOI] [PubMed] [Google Scholar]
- 24.Pruthi S, Wahner-Roedler DL, Torkelson CJ, Cha SS, Thicke LS, Hazelton JH, et al. Vitamin E and evening primrose oil for management of cyclical mastalgia: A randomized pilot study. Altern Med Rev. 2010;15:59–67. [PubMed] [Google Scholar]
- 25.Goyal A, Mansel RE. Efamast Study Group. A randomized multicenter study of gamolenic acid (Efamast) with and without antioxidant vitamins and minerals in the management of mastalgia. Breast J. 2005;11:41–7. doi: 10.1111/j.1075-122X.2005.21492.x. [DOI] [PubMed] [Google Scholar]
- 26.Gumm R, Cunnick GH, Mokbel K. Evidence for the management of mastalgia. Curr Med Res Opin. 2004;20:681–4. doi: 10.1185/030079904125003377. [DOI] [PubMed] [Google Scholar]
- 27.Shrestha S, Sen T. Analysis of mastalgia cases presented at Manipal Teaching Hospital, Pokhara, Nepal. Nepal Med Coll J. 2004;6:129–32. [PubMed] [Google Scholar]
- 28.Meyer EC, Sommers DK, Reitz CJ, Mentis H. Vitamin E and benign breast disease. Surgery. 1990;107:549–51. [PubMed] [Google Scholar]
- 29.McFayden IJ, Forrest AP, Chetty U, Raab G. Cyclical breast pain-some observations and the difficulties in treatment. Br J Clin Pract. 1992;46:161–4. [PubMed] [Google Scholar]
- 30.Wetzig NR. Mastalgia: A 3 year Australian study. Aust N Z J Surg. 1994;64:329–31. doi: 10.1111/j.1445-2197.1994.tb02221.x. [DOI] [PubMed] [Google Scholar]
- 31.Pain JA, Cahill CJ. Management of cyclical mastalgia. Br J Clin Pract. 1990;44:454–6. [PubMed] [Google Scholar]


