The goals of the American College of Cardiology (ACC) and the American Heart Association (AHA) are to prevent cardiovascular (CV) diseases, improve the management of people who have these diseases through professional education and research, and develop guidelines, standards and policies that promote optimal patient care and CV health. Toward these objectives, the ACC and AHA have collaborated with the National Heart, Lung, and Blood Institute (NHLBI) and stakeholder and professional organizations, including those in the National Program to Reduce Cardiovascular Risk (NPRCR), to develop clinical practice guidelines for assessment of CV risk, lifestyle modifications to reduce CV risk, and management of blood cholesterol, overweight and obesity in adults.
In 2008, the NHLBI initiated these guidelines by sponsoring rigorous systematic evidence reviews for each topic by expert panels convened to develop critical questions (CQs), interpret the evidence and craft recommendations. In response to the 2011 report of the Institute of Medicine on the development of trustworthy clinical guidelines (1), the NHLBI Advisory Council (NHLBAC) recommended that the NHLBI focus specifically on reviewing the highest quality evidence and partner with other organizations to develop recommendations (2,3). Accordingly, in June 2013 the NHLBI initiated collaboration with the ACC and AHA to work with other organizations to complete and publish the 4 guidelines noted above and make them available to the widest possible constituency. Recognizing that the expert panels did not consider evidence beyond 2011 (except as specified in the methodology), the ACC, AHA, and collaborating societies plan to begin updating these guidelines starting in 2014.
The joint ACC/AHA Task Force on Practice Guidelines (Task Force) appointed a subcommittee to shepherd this transition, communicate the rationale and expectations to the writing panels and partnering organizations and expeditiously publish the documents. The ACC/AHA and partner organizations recruited a limited number of expert reviewers for fiduciary examination of content, recognizing that each document had undergone extensive peer review by representatives of the NHLBAC, key Federal agencies and scientific experts. Each writing panel responded to comments from these reviewers. Clarifications were incorporated where appropriate, but there were no substantive changes as the bulk of the content was undisputed.
Although the Task Force led the final development of these prevention guidelines, they differ from other ACC/AHA guidelines. First, as opposed to an extensive compendium of clinical information, these documents are significantly more limited in scope and focus on selected CQs in each topic, based on the highest quality evidence available. Recommendations were derived from randomized trials, meta-analyses, and observational studies evaluated for quality, and were not formulated when sufficient evidence was not available. Second, the text accompanying each recommendation is succinct, summarizing the evidence for each question. The Full Panel Reports include more detailed information about the evidence statements that serves as the basis for recommendations. Third, the format of the recommendations differs from other ACC/AHA guidelines. Each recommendation has been mapped from the NHLBI grading format to the ACC/AHA Class of Recommendation/Level of Evidence (COR/LOE) construct (Table 1) and is expressed in both formats. Because of the inherent differences in grading systems and the clinical questions driving the recommendations, alignment between the NHLBI and ACC/AHA formats is in some cases imperfect. Explanations of these variations are noted in the recommendation tables, where applicable.
Table 1.
Applying Classification of Recommendation and Level of Evidence
| SIZE OF TREATMENT EFFECT | |||||||
|---|---|---|---|---|---|---|---|
| ESTIMATE OF CERTAINT (PRECISION) OFTREATMENT EFFECT |
CLASS
I Benefit >>> Risk Procedure/Treatment SHOULD be performed/administered |
CLASS
IIa Benefit >> Risk Additional studies with focused objectives needed IT IS REASONABLE to perform procedure/administer treatment |
CLASS IIb Benefit ≥ Risk Additional studies with broad objectives needed; additional registry data would be helpful Procedure/Treatment MAY BE CONSIDERED |
CLASS IIINo
Benefit or CLASS IIIHarm |
|||
| Procedure/Test | Treatment | ||||||
| COR III: No benefit |
Not Helpful |
No Proven Benefit |
|||||
| COR III: Harm |
Excess Cost w/o Benefit or Harmful |
Harmful to Patients |
|||||
| LEVEL A Muktiple populations evaluated* Data derived from multiple randomized clinical rrials or meta-analyes |
▪ Recommendation that procedure or treatment is useful/effective ▪ Sufficient evidence from multiple randomized trials or meta-analyses |
▪ Recommendation in favor of treatment or procedure being useful/effective ▪ Some conflicting evidence from multiple randomized trials or meta-analyses |
▪
Recommendation’s usefulness/efficacy less well established ▪ Greater conflicting evidence from multiple randomized trials or meta-analyses |
▪ Recommendation that procedure or treatment is not useful/effective and may be harmful ▪ Sufficient evidence from multiple randomized trials ot meta-analyses |
|||
| LEVEL B Limited populations evaluated* Data derived from a single randomized trial or nonrandomized studies |
▪ Recommendation that procedure or treatment is useful/effective ▪ Evidence from single randomized trial or nonrandomized studies |
▪ Recommendation in favor of treatment or procedure being useful/effective ▪ Some conflicting evidence from single randomized trial or nonrandomized studies |
▪ Recommendations usefulness/efficacy less well established ▪ Greater conflicting evidence from single randomized trial or nonrandomized studies |
▪ Recommendation that procedure or treatment is not useful/effective and may be harmful ▪ Evidence from single randomized trial or nonrandomized studies |
|||
|
LEVEL C Very limited populations evaluated* Only consensus opinion of experts, case studies, oi standard of care |
▪ Recommendation that procedure or treatment is useful/effective ▪ Only expert opinion, case studies, or standard of care |
▪ Recommendation in favor of treatment or procedure being useful/effective ▪ Only diverging expert opinion, case studies, or standard of care |
▪
Recommendation’s usefulness/efficacy less well established ▪ Only diverging expert opinion, case studies, or standard of care |
▪ Recommendation that procedure or treatment is not useful/effective and may be harmful ▪ Only expert opinion, case studies, or standard of care |
|||
| Suggested phrases lor writing recommendations |
should is recommended is indicated is useful/effective/beneficial |
is reasonable can be useful/effective/beneficial is probably recommended or indicated |
may/might be considered may/might be reasonable usefulness/effectiveness is unknown/unclear/uncertain or not well established |
COR III: No Benefit |
COR III: Harm |
||
| is not recommended s not indicated should not be performed/administered/other is not useful/beneficial/effective |
potentially harmful causes harm associated with excess morbidity/mortality should not be performed/administered/other |
||||||
| Comparative effectiveness phrases† |
treatment/strategy A is recommended/indicated in preference to treatment B treatment A should be chosen over treatment B |
treatment/strategy A is
probably recommended/indicated in preference to treatment B it is reasonable to choose treatment A over treatment B |
|||||
A recommendation with Level of Evidence B or C does not imply that the recommendation is weak. Many important clinical questions addressed in the guidelines do not lend themselves to clinical trials. Even when randomized trials are unavailable, there may be a very clear clinical consensus that a particular test or therapy is useful or effective.
Data available from clinical trials or registries about the usefulness/efficacy in different subpopulations, such as sex, age, history of diabetes, history of prior myocardial infarction, history of heart failure, and prior aspirin use.
For comparative effectiveness recommendations (Class I and IIa; Level of Evidence A and B only), studies that support the use of comparator verbs should involve direct comparisons of the treatments or strategies being evaluated.
In consultation with NHLBI, the policies adopted by the writing panels to manage relationships of authors with industry and other entities (RWI) are outlined in the methods section of each panel report. These policies were in effect when this effort began in 2008 and throughout the writing process and voting on recommendations, until the process was transferred to ACC/AHA in 2013. In the interest of transparency, the ACC/AHA requested that panel authors resubmit RWI disclosures as of July 2013. Relationships relevant to this guideline are disclosed in Appendix 5. None of the ACC/AHA expert reviewers had relevant RWI (Appendix 6).
Appendix 5.
Author Relationships With Industry and Other Entities (Relevant)–2013 ACC/AHA Guideline on Assessment of Cardiovascular Risk
| Work Group Member |
Employment | Consultant | Speaker’s Bureau | Ownership/ Partnership/Principal |
Personal Research | Expert Witness |
|---|---|---|---|---|---|---|
| David C. Goff, Jr Co-Chair |
Colorado School of Public Health—Dean |
2008–2012: None |
2008–2012: None |
2008–2012: None |
2008–2012: • Merck |
2008–2012: None |
|
2013: None |
2013: None |
2013: None |
2008–2012: None |
2013: None |
||
| Donald
M. Lloyd-Jones Co-Chair |
Northwestern University Feinberg School of Medicine— Senior Associate Dean; Chair and Professor of Preventive Medicine; Professor of Medicine (Cardiology) |
2008–2012: None |
2008–2012: None |
2008–2012: None |
2008–2012: None |
2008–2012: None |
|
2013: None |
2013: None |
2013: None |
2013: None |
2013: None |
||
| Glen
Bennett Ex-Officio |
NHLBI—Coordinator |
2008–2012: None |
2008–2012: None |
2008–2012: None |
2008–2012: None |
2008–2012: None |
|
2013: None |
2013: None |
2013: None |
2013: None |
2013: None |
||
| Sean
Coady Ex-Officio |
NHLBI—Statistician |
2008–2012: None |
2008–2012: None |
2008–2012: None |
2008–2012: None |
2008–2012: None |
|
2013: None |
2013: None |
2013: None |
2013: None |
2013: None |
||
| Ralph B. D’Agostino |
Boston University—Professor of Mathematics and Statistics; Mathematics and Statistics Department—Chair |
2008–2012: None |
2008–2012: None |
2008–2012: None |
2008–2012: None |
2008–2012: None |
|
2013: None |
2013: None |
2013: None |
2013: None |
2013: None |
||
| Raymond Gibbons |
Nuclear Cardiology Laboratory Mayo Clinic—Professor of Medicine and Co-Director |
2008–2012: None |
2008–2012: None |
2008–2012: None |
2008–2012: None |
2008–2012: None |
|
2013: • AstraZeneca • Lantheus Medical Imaging |
2013: None |
2013: None |
2013: None |
2013: None |
||
| Philip Greenland | Northwestern University Feinberg School of Medicine— Senior Associate Dean for Clinical and Translational Research; Harry W. Dingman Professor of Medicine |
2008–2012: None |
2008–2012: None |
2008–2012: None |
2008–2012: None |
2008–2012: None |
|
2013: None |
2013: None |
2013: None |
2013: None |
2013: None |
||
| Daniel T. Lackland |
Medical University of
South Carolina—Professor of Epidemiology and Medicine |
2008–2012: None |
2008–2012: None |
2008–2012: None |
2008–2012: None |
2008–2012: None |
|
2013: None |
2013: None |
2013: None |
2013: None |
2013: None |
||
| Daniel
Levy Ex-Officio |
NHLBI—Framingham Heart Study, Director |
2008–2012: None |
2008–2012: None |
2008–2012: None |
2008–2012: • BG Medicine |
2008–2012: None |
|
2013: None |
2013: None |
2013: None |
2013: None |
2013: None |
||
| Christopher O’Donnell Ex-Officio |
NHLBI—Associate Director and Senior Investigator |
2008–2012: None |
2008–2012: None |
2008–2012: None |
2008–2012: None |
2008–2012: None |
|
2013: None |
2013: None |
2013: None |
2013: None |
2013: None |
||
| Jennifer Robinson |
University of Iowa—Professor of Epidemiology and Medicine; Director, Prevention Intervention Center |
2008–2012: None |
2008–2012: None |
2008–2012: None |
2008–2012: • Aegerion • Amarin* • Amgen* • AstraZeneca* • Daiichi-Sankyo* • Esperion • Genentech/Hoffman LaRoche* • GlaxoSmithKline* • Merck* • Sanofi- aventis/Regeneron* |
2008–2012: None |
|
2013: None |
2013: None |
2013: None |
2013: • Amarin* • Amgen* • AstraZeneca* • Daiichi-Sankyo* • Genentech/Hoffman LaRoche* • GlaxoSmithKline* • Merck* • Sanofi- aventis/Regeneron* |
2013: None |
||
| J. Sanford Schwartz |
University of
Pennsylvania— Leon Hess Professor of Internal Medicine, Health Management and Economics |
2008–2012: None |
2008–2012: None |
2008–2012: None |
2008–2012: None |
2008–2012: None |
|
2013: None |
2013: None |
2013: None |
2013: None |
2013: None |
||
| Susan T.
Shero Ex-Officio |
NHLBI—Public
Health Advisor |
2008–2012: None |
2008–2012: None |
2008–2012: None |
2008–2012: None |
2008–2012: None |
|
2013: None |
2013: None |
2013: None |
2013: None |
2013: None |
||
| Sidney C. Smith, Jr |
University of North
Carolina— Professor of Medicine; Center for Cardiovascular Science and Medicine—Director |
2008–2012: None |
2008–2012: None |
2008–2012: None |
2008–2012: None |
2008–2012: None |
|
2013: None |
2013: None |
2013: None |
2013: None |
2013: None |
||
| Paul
Sorlie Ex-Officio |
NHLBI—Chief of Division
of Epidemiology and Clinical Applications |
2008–2012: None |
2008–2012: None |
2008–2012: None |
2008–2012: None |
2008–2012: None |
|
2013: None |
2013: None |
2013: None |
2013: None |
2013: None |
||
| Neil J. Stone | Northwestern
Memorial Hospital—Bonow Professor of Medicine, Feinberg School of Medicine, Northwestern University |
2008–2012: None |
2008–2012: None |
2008–2012: None |
2008–2012: None |
2008–2012: None |
|
2013: None |
2013: None |
2013: None |
2013: None |
2013: None |
||
| Peter W.F. Wilson |
Emory Clinical Cardiovascular Research Institute—Professor of Medicine |
2008–2012: • Merck • XZK |
2008–2012: None |
2008–2012: None |
2008–2012: • Merck • LipoScience |
2008–2012: None |
|
2013: None |
2013: None |
2013: None |
2013: None |
2013: None |
This table reflects the relevant healthcare-related relationships of authors with industry and other entities (RWI) provided by the panels during the document development process (2008–2012). Both compensated and uncompensated relationships are reported. These relationships were reviewed and updated in conjunction with all meetings and/or conference calls of the Work Group during the document development process. Authors with relevant relationships during the document development process recused themselves from voting on recommendations relevant to their RWI. In the spirit of full transparency, the ACC and AHA asked Work Group members to provide updates and approve the final version of this table which includes current relevant relationships (2013).
To review the NHLBI and ACC/AHA’s current comprehensive policies for managing RWI, please refer to http://www.nhlbi.nih.gov/guidelines/cvd_adult/coi-rwi_policy.htm and http://www.cardiosource.org/Science-And-Quality/Practice-Guidelines-and-Quality-Standards/Relationships-With-Industry-Policy.aspx.
Per ACC/AHA policy:
A person is deemed to have a significant interest in a business if the interest represents ownership of ≥5% of the voting stock or share of the business entity, or ownership of ≥$10,000 of the fair market value of the business entity; or if funds received by the person from the business entity exceed 5% of the person’s gross income for the previous year. Relationships that exist with no financial benefit are also included for the purpose of transparency. Relationships in this table are modest unless otherwise noted.
Significant relationship.
NHLBI indicates National Heart, Lung, and Blood Institute.
Systematic evidence reports and accompanying summary tables were developed by the expert panels and NHLBI. The guideline was reviewed by the ACC/AHA Task Force and approved by the ACC Board of Trustees, the AHA Science Advisory and Coordinating Committee, and the governing bodies of partnering organizations. In addition, ACC/AHA sought endorsement by other stakeholders, including professional organizations and members of the NPRCR. It is the hope of the writing panels, stakeholders, professional organizations, NHLBI, and the Task Force that the guidelines will garner the widest possible readership for the benefit of patients, providers and the public health.
Guidelines attempt to define practices that meet the needs of patients in most circumstances and are not a replacement for clinical judgment. The ultimate decision about care of a particular patient must be made by the healthcare provider and patient in light of the circumstances presented by that patient. As a result, situations might arise in which deviations from these guidelines may be appropriate. These considerations notwithstanding, in caring for most patients, clinicians can employ the recommendations confidently to reduce the risks of atherosclerotic cardiovascular disease (ASCVD) events.
See Tables 2 and 3 for an explanation of the NHLBI recommendation grading methodology.
Table 2.
NHLBI Grading the Strength of Recommendations
| Grade | Strength of Recommendation* |
|---|---|
| A | Strong recommendation There is high certainty based on evidence that the net benefit† is substantial. |
| B | Moderate recommendation There is moderate certainty based on evidence that the net benefit is moderate to substantial, or there is high certainty that the net benefit is moderate. |
| C | Weak recommendation There is at least moderate certainty based on evidence that there is a small net benefit. |
| D | Recommendation against There is at least moderate certainty based on evidence that it has no net benefit or that risks/harms outweigh benefits. |
| E | Expert opinion (“There is insufficient evidence
or evidence is unclear or conflicting, but this is what the Work Group recommends.”) Net benefit is unclear. Balance of benefits and harms cannot be determined because of no evidence, insufficient evidence, unclear evidence, or conflicting evidence, but the Work Group thought it was important to provide clinical guidance and make a recommendation. Further research is recommended in this area. |
| N | No recommendation for or against (“There is
insufficient evidence or evidence is unclear
or conflicting.”) Net benefit is unclear. Balance of benefits and harms cannot be determined because of no evidence, insufficient evidence, unclear evidence, or conflicting evidence, and the Work Group thought no recommendation should be made. Further research is recommended in this area. |
In most cases, the strength of the recommendation should be closely aligned with the quality of the evidence; however, under some circumstances, there may be valid reasons for making recommendations that are not closely aligned with the quality of the evidence (e.g., strong recommendation when the evidence quality is moderate, like smoking cessation to reduce CVD risk or ordering an ECG as part of the initial diagnostic work-up for a patient presenting with possible MI). Those situations should be limited and the rationale explained clearly by the Work Group.
Net benefit is defined as benefits minus risks/harms of the service/intervention.
CVD indicates cardiovascular risk; ECG, electrocardiography; MI, myocardial infarction; and NHLBI, National Heart, Lung, and Blood Institute.
Table 3.
Quality Rating the Strength of Evidence
| Type of Evidence | Quality Rating* |
|---|---|
|
High |
| Moderately certain about the estimate of effect. Further research may have an impact on our confidence in the estimate of effect and may change the estimate. | Moderate |
|
Low |
In some cases, other evidence, such as large all-or-none case series (e.g., jumping from airplanes or tall structures), can represent high or moderate quality evidence. In such cases, the rationale for the evidence rating exception should be explained by the Work Group and clearly justified.
Well-designed, well-executed refers to studies that directly address the question, use adequate randomization, blinding, allocation concealment, are adequately powered, use ITT analyses, and have high follow-up rates.
Limitations include concerns with the design and execution of a study that result in decreased confidence in the true estimate of the effect. Examples of such limitations include, but are not limited to: inadequate randomization, lack of blinding of study participants or outcome assessors, inadequate power, outcomes of interest are not prespecified or the primary outcomes, low follow-up rates, or findings based on subgroup analyses. Whether the limitations are considered minor or major is based on the number and severity of flaws in design or execution. Rules for determining whether the limitations are considered minor or major and how they will affect rating of the individual studies will be developed collaboratively with the methodology team.
Nonrandomized controlled studies refer to intervention studies where assignment to intervention and comparison groups is not random (e.g., quasi-experimental study design)
Observational studies include prospective and retrospective cohort, case-control, and cross sectional studies.
ITT indicates intention-to-treat; MA, meta-analysis; and RCT, randomized controlled trial.
1. Introduction
1.1. Organization of the Work Group
The Risk Assessment Work Group (Work Group) was composed of 11 members and 5 ex-officio members, including internists, cardiologists, endocrinologists, and experts in CV epidemiology, biostatistics, healthcare management and economics, and guideline development.
1.2. Document Review and Approval
A formal peer review process, which included 12 expert reviewers and representatives of Federal agencies, was initially completed under the auspices of the NHLBI. This document was also reviewed by 3 expert reviewers nominated by the ACC and the AHA when the management of the guideline transitioned to the ACC/AHA. The ACC and AHA Reviewers’ RWI information is published in this document (6).
This document was approved for publication by the governing bodies of the ACC and AHA and endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation, American Society for Preventive Cardiology, American Society of Hypertension, Association of Black Cardiologists, National Lipid Association, Preventive Cardiovascular Nurses Association, and Women Heart: The National Coalition for Women with Heart Disease.
1.3. Charge to the Work Group
The Work Group was 1 of 3 work groups appointed by the NHLBI to develop its own recommendations and provide cross-cutting input to 3 Expert Panels for updating guidelines on blood cholesterol, blood pressure (BP), and overweight/obesity.
The Work Group was asked to examine the scientific evidence on risk assessment for initial ASCVD events, and to develop an approach for risk assessment that could be used in practice and used or adapted by the risk factor panels (cholesterol, hypertension, and obesity) in their guidelines and algorithms. Specifically, the Work Group was charged with 2 tasks:
To develop or recommend an approach to quantitative risk assessment that could be used to guide care; and
To pose and address a small number of questions judged to be critical to refining and adopting risk assessment in clinical practice using systematic review methodology.
1.4. Methodology and Evidence Review
This guideline is based on the Full Work Group Report which is provided as a supplement to the guideline (http://jaccjacc.cardiosource.com/acc_documents/2013_FPR_S5_Risk_Assessment.pdf). The Full Work Group Report contains background and additional material related to content, methodology, evidence synthesis, rationale, and references and is supported by the NHLBI Systematic Evidence Review which can be found at (http://www.nhlbi.nih.gov/guidelines/cvd_adult/risk_assessment/). These documents also describe the process for the development of novel, comprehensive multivariable risk equations for the prediction of 10-year risk for development of ASCVD in nonHispanic African-American and nonHispanic White men and women from 40 to 79 years of age. These equations were developed from several long-standing population-based cohort studies funded by the NHLBI. Ten-year risk was defined as the risk of developing a first ASCVD event, defined as nonfatal myocardial infarction or coronary heart disease (CHD) death, or fatal or nonfatal stroke, over a 10-year period among people free from ASCVD at the beginning of the period.
In addition, through evaluation of evidence developed through systematic reviews of the literature, the Work Group addressed the following 2 CQs:
CQ1: “What is the evidence regarding reclassification or contribution to risk assessment when high-sensitivity C-reactive protein (hs-CRP), apolipoprotein B (ApoB), glomerular filtration rate (GFR), microalbuminuria, family history, cardiorespiratory fitness, ankle-brachial index (ABI), carotid intima-media thickness (CIMT), or coronary artery calcium (CAC) score are considered in addition to the variables that are in the traditional risk scores?”
CQ2: “Are models constructed to assess the long-term (≥15 years or lifetime) risk for a first cardiovascular disease (CVD) event in adults effective in assessing variation in long-term risk among adults at low and/or intermediate short-term risk, whether analyzed separately or combined?”
The evidence and recommendations in the guideline focus on the large proportion of the adult population without clinical signs or symptoms of ASCVD, who merit evaluation for the primary prevention of ASCVD. They do not apply to those with clinically-manifest ASCVD, who require secondary prevention approaches, or to highly-selected patient subgroups, such as those with symptoms suggestive of CVD who require diagnostic strategies rather than risk assessment. Furthermore, these recommendations were not developed for use in specific subgroups of asymptomatic individuals at unusually high risk, such as those with genetically determined extreme values of traditional risk factors (e.g., patients with familial hypercholesterolemia).
2. Risk Assessment: Recommendations
3. Approach to Risk Assessment
In addressing its charge, the Work Group recognized the need for a risk assessment approach that was based on the types of data that primary care providers could easily collect and that could be implemented in routine clinical practice. After deliberation, the Work Group endorsed the existing and widely employed paradigm of matching the intensity of preventive efforts with the individual’s absolute risk (24,25). The Work Group acknowledges that none of the risk assessment tools or novel risk markers examined in the present document have been formally evaluated in randomized controlled trials of screening strategies with clinical events as outcomes. Nevertheless, this approach balances an understanding of an individual’s absolute risk for CVD and potential treatment benefits against the potential absolute risks for harm from therapy. Using this framework, treatment can be targeted to those most likely to benefit without undue risk for harm, in the context of a “risk discussion.” A risk discussion could include the assessment of the patient’s risk for ASCVD, and potential benefits, negative aspects, risks, and patient preferences regarding initiation of relevant preventive therapies.
By its nature, such an approach requires a platform for reliable quantitative estimation of absolute risk based upon data from representative population samples. It is important to note that risk estimation is based on group averages that are then applied to individual patients in practice. This process is admittedly imperfect; no one has 10% or 20% of a heart attack during a 10-year period. Individuals with the same estimated risk will either have or not have the event of interest, and only those patients who are destined to have an event can have their event prevented by therapy. The criticism of the risk estimation approach to treatment-decision making also applies to the alternative, and much less efficient approach, of checking the patient’s characteristics against numerous and complex inclusion and exclusion criteria for a potentially large number of pertinent trials. Only a small fraction of trial participants have events, and only a fraction of these events are prevented by therapy. Using either approach, the clinician must apply the average results obtained from groups of patients to the individual patient in practice.
Given the modification and adoption of the Framingham 10-year risk score for CHD risk assessment by the “Third Report of the National Cholesterol Education Program Expert Panel on Diagnosis, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III)” (25), and the uptake of this algorithm by practice sites across the United States, the Work Group began by discussing the value of retaining this algorithm. In collaboration with other NHLBI panels, the Work Group decided not to use this algorithm in its 2013 recommendations, because of its derivation in an exclusively White sample population and the limited scope of the outcome (in determining CHD alone). Rather, the Work Group derived risk equations from community-based cohorts that are broadly representative of the U.S. population of Whites and African Americans, and focused on estimation of first hard ASCVD events (defined as first occurrence of nonfatal myocardial infarction or CHD death, or fatal or nonfatal stroke) as the outcome of interest because it was deemed to be of greater relevance to both patients and providers. The focus on hard ASCVD, rather than CHD alone, is also consistent with evidence reviewed in a statement from the AHA/American Stroke Association calling for the inclusion of ischemic stroke in the outcome of interest for CVD risk assessment (26).
Numerous multivariable risk scores/equations have been derived and published (Appendix 3, and for more details, the Full Work Group Report Supplement (http://jaccjacc.cardiosource.com/acc_documents/2013_FPR_S5_Risk_Assessment.pdf)). As part of its deliberations, the Work Group considered previously published risk scores with validation in NHLBI cohort data as 1 possible approach. However, a number of persistent concerns with existing risk equations were identified including nonrepresentative or historically dated populations, limited ethnic diversity, narrowly defined endpoints, endpoints influenced by provider preferences (e.g., revascularizations), and endpoints with poor reliability (e.g., angina and heart failure [HF]). Given the inherent limitations of existing scores, the Work Group judged that a new risk score was needed to address some of the deficiencies of existing scores, such as utilizing a population sample that approaches, to the degree possible, the ideal sample for algorithm development and closely represents the U.S. population.
Appendix 3.
Characteristics of Previously Published Risk Scores and Current Pooled Cohort Equations (Including Data Sources, Covariates, and Outcomes)
| Risk Score | Risk Factors/Covariates Included | Cardiovascular Disease Events | |||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hard CVD including cardiac failure | |||||||||||||||||||||||||||
| Hard ASCVD | |||||||||||||||||||||||||||
| Hard CHD | |||||||||||||||||||||||||||
| Total CHD | |||||||||||||||||||||||||||
| Total CHD including revascularization | |||||||||||||||||||||||||||
| Study Group |
Study and Region |
Data Source |
Pub- lication Year |
Age | Sex | Total Chol |
LDL- Chol |
HDL- Chol |
CRP | Systolic BP |
BP Rx |
Dia- betes |
HbA1c* | Smok- ing |
Family Hx CVD† |
Body Mass Index |
Social | Region | Coron- ary Revasc |
Angina Pectoris |
Unsta- ble Angina |
Myo- cardial Infarct |
CHD Death |
Stroke | Stroke Death |
Car- diac Failure |
TIA |
| Framing -ham CHD (56) |
Framing- ham MA, USA |
EAF, EAM |
1998 | x | x | x | x | X | x | x | x | x | x | X | x | ||||||||||||
| ATP III (25) |
Framing- ham MA, USA |
EAF, EAM |
2001 | x | x | x | X | x | x | x | X | x | |||||||||||||||
| Framing- ham Global (57) |
Framing- ham MA, USA |
EAF, EAM |
2008 | x | x | x | X | x | x | x | x | X | x | x | x | x | |||||||||||
| PRO- CAM (58) |
Muen- ster, Germany |
EM | 2002 | x | x | X | x | x | x | x | X | x | |||||||||||||||
| QRISK (59) |
QRESE ARCH, United Kingdom |
EF, EM | 2007 | x | x | x | X | x | x | x | x | x | X‡ | x | x | x | x | X | x | x | x | x | |||||
| Reyn- olds Men (60) |
Phys Health Study USA |
EAF | 2008 | x | x | X | x | x | x | x | x | X | x | x | x | ||||||||||||
| Reyn- olds Women (61) |
Wo- men’s Health Study USA |
EAM | 2007 | x | x | X | x | x | x | x | x | x | X | x | x | x | |||||||||||
| EURO- SCORE (62) |
12 cohorts Europe |
EF, EM | 2003 | x | x | x | X | x | x | x | x | x | |||||||||||||||
| Pooled Cohort (current) |
CARDIA, Framing- ham, ARIC, CHS,US A |
EAF, EAM AAF, AAM |
x | x | x | X | x | x | x | x | X | x | x | x | |||||||||||||
Risk calculators noted above include hyperlinks to the respective webpage.
Only among those with diabetes
Definitions of a positive family history vary
Measure of social deprivation
AAF indicates African-American females; AAM, African-American males; ASCVD, atherosclerotic cardiovascular disease; BP, blood pressure; Chol, cholesterol; CHD, coronary heart disease; CRP, C-reactive protein; CVD, cardiovascular disease; EF, European females; EM, European males; EAF, European American females; EAM, European American males; HbA1c, hemoglobin A1c; Hx, history; Revasc, revascularization; and TIA, transient ischemic attack.
Data are sparse regarding usage and impact of absolute risk scores in clinical practice in primary prevention settings (27). Two systematic reviews, based on few studies, support the conclusion that risk assessment, combined with counseling, is associated with favorable but modest changes in patient knowledge and intention to change, and with provider prescribing behavior and risk factor control (28,29). No data are available on hard event outcomes. The Work Group specifically calls for research in this area (Section 8).
The Work Group notes that the “2009 ACCF/AHA Performance Measures for the Primary Prevention of CVD” specifically recommended use of global CVD risk estimation in clinical practice (30). Likewise, the U.S. Preventive Services Task Force recommendations for aspirin (31), NHLBI Adult Treatment Panel III recommendations (25), and European (32) and Canadian (33,34) guidelines for primary prevention of CVD, among others, have all recommended the use of absolute risk assessment for decision making about the intensity of lifestyle and pharmacological preventive interventions. Risk scores have been implemented in practice through paper scoring sheets, and increasingly through websites and downloadable applications. The electronic medical record can be adapted to estimate absolute risks automatically using patient data and published equations, and it is anticipated that risk estimation using this technology will become a mainstream application of the current and future risk algorithms.
4. Development of New Pooled Cohort ASCVD Risk Equations
Having made the decision to develop new equations to estimate the 10-year risk for developing a first ASCVD event, the Work Group used the best available data from community-based cohorts of adults, with adjudicated endpoints for CHD death, nonfatal myocardial infarction, and fatal or nonfatal stroke. Cohorts that included African-American or White participants with at least 12 years of follow-up were included. Data from other race/ethnic groups were insufficient, precluding their inclusion in the final analyses. The final pooled cohorts included participants from several large, racially and geographically diverse, modern NHLBI-sponsored cohort studies, including the ARIC (Atherosclerosis Risk in Communities) study (8), Cardiovascular Health Study (5), and the CARDIA (Coronary Artery Risk Development in Young Adults) study (7), combined with applicable data from the Framingham Original and Offspring Study cohorts (4,6).
The Work Group used state-of-the-art statistical methods to derive and internally validate the Pooled Cohort Equations, which provide sex-and race-specific estimates of the 10-year risk for ASCVD for African-American and White men and women 40 to 79 years of age. The variables that statistically merit inclusion in the risk assessment equations are age, total and HDL-cholesterol, systolic BP (including treated or untreated status), diabetes, and current smoking status.
An expanded description of the derivation and validation of the Pooled Cohort Equations, as well as the means for implementing them in clinical practice, are provided in Appendix 4. Additional details are provided in the Full Report of the Work Group (http://jaccjacc.cardiosource.com/acc_documents/2013_FPR_S5_Risk_Assessment.pdf). A specific clinical vignette is also provided as an example in Appendix 4. In the clinical vignette, the 10-year risk is calculated for a patient 55 years of age who is a nonsmoker without diabetes, and with total cholesterol 213 mg/dL, HDL–cholesterol 50 mg/dL, and untreated systolic BP 120 mm Hg. Using these values in the Pooled Cohort Equations, the predicted 10-year ASCVD risks are 2.1% for White women, 3.0% for African-American women, 5.3% for White men, and 6.1% for African-American men.
Numerous other potential risk markers were considered for inclusion in the Pooled Cohort Equations, but for many there was no additional utility demonstrated upon their inclusion; for others, data were insufficient at the present time to determine their additional value. The equations were also assessed in external validation studies using data from other available cohorts. Other than the Framingham CHD risk score (and its derivative ATP-III risk assessment profile) and the European SCORE (System for Cardiac Operative Risk Evaluation) algorithm for CVD death, these equations have been subjected to more rigorous validation than other currently available equations, and they are the only risk assessment equations that include significant numbers of African Americans and focus on estimation of 10-year risk for the clinically relevant endpoint of ASCVD. The Work Group specifically calls for further research to develop similar equations applicable to other ethnic groups, to validate the utility of the Pooled Cohort Equations in diverse primary prevention settings, and to assess the potential benefit of novel risk markers when added to these equations, so that the equations may be modified or expanded over time as new data become available.
4.1. Recommendations for Assessment of 10-Year Risk for a First Hard ASCVD Event
Recommendation 1
The race- and sex-specific Pooled Cohort Equations to predict 10-year risk for a first hard ASCVD* event should be used in nonHispanic African Americans and nonHispanic Whites, 40 to 79 years of age.
(Grade B, Moderate); ACC/AHA COR I, LOE B
Recommendation 2
Use of the sex-specific Pooled Cohort Equations for nonHispanic Whites may be considered when estimating risk in patients from populations other than African Americans and nonHispanic Whites.
(Grade E, Expert Opinion); ACC/AHA COR IIb, LOE C
A downloadable spreadsheet enabling estimation of 10-year and lifetime risk for ASCVD and a web-based calculator are available at http://my.americanheart.org/cvriskcalculator and http://www.cardiosource.org/science-and-quality/practice-guidelines-and-quality-standards/2013-prevention-guideline-tools.aspx.
*Ten-year risk was defined as the risk of developing a first ASCVD event, defined as nonfatal myocardial infarction or CHD death, or fatal or nonfatal stroke, over a 10-year period among people free from ASCVD at the beginning of the period.
5. Implications for Risk Assessment
A range of estimated 10-year risk for a first hard ASCVD event is illustrated in the Full Work Group Report Supplement (Tables 8–11), across a broad range of risk factor burdens for selected combinations of the risk factors in sex-race groups (African-American and White women and men) (http://jaccjacc.cardiosource.com/acc_documents/2013_FPR_S5_Risk_Assessment.pdf). The estimated risks are specific to defined combinations of the risk factors, and demonstrate how they vary over a broad spectrum of potential profiles. Risk factor levels that are more adverse than those shown in these tables should always be associated with a higher estimated risk. For example, if a given risk factor combination indicates an estimated 10-year risk for hard ASCVD of 8%, but a patient has a higher level of systolic BP or total cholesterol, or a lower level of high-density lipoprotein cholesterol, than shown for that cell, then the estimated risk would be ≥8%. Because the estimated probabilities can become unstable when approaching the limits of the sample data, the risk probabilities are truncated at 1% and 30%. The proportion of the U.S. adult population, 40 to 79 years of age, in selected strata of estimated 10-year risk for hard ASCVD events, are shown overall and by sex and race in Table 5. When compared with nonHispanic Whites, estimated 10-year risk for ASCVD is generally lower in Hispanic-American and Asian-American populations and higher in American-Indian populations (35,36); hence, the lack of ethnic-specific risk algorithms are an important gap in our efforts to understand and prevent ASCVD in these populations. While the development of algorithms specific to these race/ethnic groups is encouraged, in the interim, providers may consider using the equations for nonHispanic Whites for these patients. When doing so, it is important to remember that the estimated risks may be over-estimates, especially for Hispanic- and Asian-Americans.
Table 5.
Distribution of Estimated 10-Year Risk for a First Hard ASCVD Event in the CVD-Free, Nonpregnant U.S. Population 40 to 79 Years of Age, by Sex, and Race*
| Predicted 10-Year Risk for Hard ASCVD Event | ||||||||
|---|---|---|---|---|---|---|---|---|
| <2.5% | 2.5%–4.9% | 5.0%–7.4% | 7.5%–9.9% | 10.0%–14.9% | 15.0%–19.9% | ≥20.0% | ||
| Total | % (95%
CI) n |
33.4 (31.2–35.5) 33,534,000 |
21.0 (19.4–22.7) 21,151,000 |
12.7 (11.4–14.0) 12,766,000 |
7.4 (6.5–8.3) 7,470,000 |
8.9 (8.1–9.6) 8,940,000 |
6.3 (5.6–7.1) 6,380,000 |
10.2 (9.5–11.0) 10,300,000 |
| Sex | ||||||||
| Men | % (95%
CI) n |
17.4 (15.2–19.7) 8,386,000 |
22.7 (20.3–25.1) 10,950,000 |
15.6 (13.8–17.4) 7,511,000 |
10.1 (8.5–11.6) 4,847,000 |
12.1 (10.7–13.5) 5,849,000 |
8.8 (7.4–10.2) 4,248,000 |
13.3 (12.1–14.4) 6,388,000 |
| Women | % (95%
CI) n |
48.0 (44.8–51.3) 25,148,000 |
19.5 (17.3–21.6) 10,200,000 |
10.0 (8.3–11.8) 5,256,000 |
5.0 (3.8–6.2) 2,622,000 |
5.9 (5.1–6.7) 3,091,000 |
4.1 (3.4–4.7) 2,131,000 |
7.5 (6.5–8.4) 3,912,000 |
| Race | ||||||||
| White | ||||||||
| Men | % (95%
CI) n |
18.0 (15.0–21.1) 6,467,000 |
22.4 (19.4–25.3) 8,016,000 |
15.7 (13.3–18.1) 5,616,000 |
10.0 (8.2–11.8) 3,584,000 |
11.7 (9.9–13.5) 4,189,000 |
8.7 (7.0–10.4) 3,112,000 |
13.6 (12.3–14.9) 4,870,000 |
| Women | % (95%
CI) n |
47.1 (43.0–51.1) 18,175,000 |
20.4 (17.7–23.0) 7,863,000 |
10.7 (8.6–12.8) 4,136,000 |
5.1 (3.6–6.7) 1,984,000 |
5.5 (4.6–6.5) 2,132,000 |
4.1 (3.4–4.9) 1,596,000 |
7.1 (5.9–8.2) 2,725,000 |
|
African American | ||||||||
| Men | % (95%
CI) n |
1.4 (0.3–2.6) 60,000 |
23.9 (19.9–28.0) 1,008,000 |
20.6 (17.0–24.2) 866,000 |
11.8 (8.8–14.8) 495,000 |
17.4 (14.3–20.5) 731,000 |
11.1 (8.2–13.9) 466,000 |
13.8 (11.0–16.7) 583,000 |
| Women | % (95%
CI) n |
36.5 (32.4–40.6) 1,921,000 |
18.7 (15.6–21.8) 985,000 |
10.9 (8.6–13.2) 572,000 |
6.5 (5.0–7.9) 339,000 |
9.4 (7.2–11.7) 496,000 |
5.7 (4.2–7.2) 300,000 |
12.3 (9.5–15.0) 645,000 |
| Hispanic | ||||||||
| Men | % (95%
CI) n |
24.0 (19.8–28.1) 1,303,000 |
22.1 (17.9–26.2) 1,200,000 |
13.2 (10.8–15.6) 718,000 |
10.6 (8.1–13.0) 574,000 |
11.4 (9.9–12.9) 619,000 |
6.2 (4.6–7.9) 339,000 |
12.6 (9.4–15.7) 683,000 |
| Women | % (95%
CI) n |
59.4 (54.3–64.4) 3,293,000 |
14.5 (11.5–17.5) 803,000 |
7.5 (5.4–9.6) 418,000 |
4.5 (2.6–6.4) 248,000 |
4.9 (3.4–6.5) 273,000 |
3.0 (2.0–3.9) 164,000 |
6.3 (4.7–7.9) 347,000 |
| Others | ||||||||
| Men | % (95%
CI) n |
20.8 (10.8–30.7) 555,000 |
27.1 (18.0–36.3) 726,000 |
11.6 (4.9–18.2) 310,000 |
7.2 (0.6–13.8) 193,000 |
11.5 (4.5–18.6) 309,000 |
12.3 (5.9–18.8) 330,000 |
9.4 (3.0–15.8) 251,000 |
| Women | % (95%
CI) n |
59.8 (50.2–69.3) 1,757,000 |
18.6 (10.8–26.5) 548,000 |
4.4 (0–8.7) 128,000 |
1.7 (0–3.5) 49,000 |
6.4 (2.1–10.7) 188,000 |
2.4 (0.4–4.5) 71,000 |
6.7 (2.3–11.0) 195,000 |
Data derived by applying the Pooled Cohort Equations to the National Health and Nutrition Examinations Surveys, 2007–2010 (N=5,367, weighted to 100,542,000 U.S. population)
ASCVD indicates atherosclerotic cardiovascular disease; CVD, cardiovascular disease; and U.S., United States.
6. CQs and Systematic Evidence Review
6.1. Critical Question 1
“What is the evidence regarding reclassification or contribution to risk assessment when hs-CRP, ApoB, GFR, microalbuminuria, family history, cardiorespiratory fitness, ABI, CAC, or CIMT are considered in addition to the variables that are in the traditional risk scores?”
The concept of matching the intensity of risk factor management to the estimated risk for CVD has been well established since the 27th Bethesda Conference in 1996 (24). As a consequence, widespread attention has focused on the accuracy and reliability of risk assessment. Claims that a minority of the risk for CVD can be explained by the major traditional risk factors, or that most patients presenting with CHD have no elevated traditional risk factors, have been disproven (37,38). Nonetheless, the desire to improve existing quantitative risk estimation tools has helped to stimulate and maintain interest in the search for new risk markers for CVD which might further enhance risk assessment.
CQ1 was developed to address whether newer risk markers have been identified that actually improve risk assessment enough to warrant routine measurement in clinical practice. This question applies to risk assessment in the general population, that is, the typical asymptomatic adult in routine clinical practice. This question does not address other highly selected patient subgroups, such as those with symptoms suggestive of CVD.
CQ1 was addressed using 2 independent approaches. First, in the process of developing the Pooled Cohort Equations, the additional risk markers listed in CQ1 were tested for inclusion in the model if they were available in the databases and could be evaluated on the basis of at least 10 years of follow up. A review of meta-analyses and systematic reviews published before September 19, 2013 was conducted in 2 stages. In the first stage, meta-analyses and systematic reviews published before April 2011 were identified and reviewed. In a second stage, conducted to update the evidence base before publication, additional meta-analyses and systematic reviews published before September 19, 2013 were identified and reviewed using the same criteria applied in the first stage. The reliance on published meta-analyses to evaluate novel biomarkers is a conservative approach that helps avoid the influence of positive publication bias that can occur early in the evaluation of a novel association and assures that we relied on a mature body of evidence (39).
Members of the Work Group proposed an initial list of novel risk markers for inclusion in CQ1 which was then prioritized during several rounds of discussion. In selecting the final list, the Work Group gave priority to factors that have engendered substantial discussion in the scientific community and that could be reasonably considered as potentially feasible for widespread population use by primary care providers in routine clinical settings in the United States. These deliberations considered availability, cost, assay reliability, and risks of the test or downstream testing. The final list of new risk markers to be evaluated included several blood and urine biomarkers (hs-CRP, ApoB, creatinine [or estimated GFR], and microalbuminuria), several measures of subclinical CV disease (CAC, CIMT, and ABI), family history, and cardiorespiratory fitness. Other novel potential screening tools may be the subject of future guideline updates. When considering the utility of incorporating these new risk factors into routine risk assessment, guidance published by Hlatky et al (40) was considered. Special attention was given to the additional value these markers contributed to risk assessment in terms of discrimination, calibration, reclassification, and cost-effectiveness, in the context of any potential harm.
6.1.1. Summary of Systematic Reviews and Meta-Analyses for CQ1
Thirteen systematic review articles or meta-analyses met the inclusion/exclusion criteria (9–18,41–43). Publication dates ranged from 2008 to 2013. The Work Group reviewed the 13 systematic reviews and meta-analyses and created a table to list their key findings (Appendix 1). None of these markers has been evaluated as a screening test in randomized controlled trials with clinical events as outcomes. On the basis of current evidence, it is the opinion of the Work Group that assessments of family history of premature CVD, and measurement of hs-CRP, CAC, and ABI show some promise for clinical utility among the novel risk markers, based on limited data. Table 6 provides expert opinion regarding thresholds of these measures that may be considered for clinical decision making.
Table 6.
Expert Opinion Thresholds for use of Optional Screening Tests When Risk-Based Decisions Regarding Initiation of Pharmacological Therapy are Uncertain Following Quantitative Risk Assessment
| Measure | Support Revising Risk Assessment Upward |
Do Not Support Revising Risk Assessment |
|---|---|---|
| Family history of premature CVD |
Male <55 years of age Female <65 years of age (1st degree relative) |
Occurrences at older ages only (if any) |
| hs-CRP | ≥2 mg/L | <2 mg/L |
| CAC score | ≥300 Agatston units or ≥75th
percentile for age, sex, and ethnicity* |
<300 Agatston units and <75 percentile
for age, sex, and ethnicity* |
| ABI | <0.9 | ≥0.9 |
For additional information, see http://www.mesa-nhlbi.org/CACReference.aspx.
ABI indicates ankle-brachial index; CAC, coronary artery calcium; CVD, cardiovascular disease; and hs-CRP, high-sensitivity C-reactive protein.
The Work Group notes that the review by Peters et al. (16) provides evidence to support the contention that assessing CAC is likely to be the most useful of the current approaches to improving risk assessment among individuals found to be at intermediate risk after formal risk assessment. Furthermore, the Work Group recognizes that the “2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults” made recommendations regarding CAC testing (44). However, the Work Group notes that the outcomes in the studies reviewed by Peters et al. (16) and by Greenland et al. (44) were CHD outcomes, not hard ASCVD events that included stroke; hence, uncertainty remains regarding the contribution of assessing CAC to estimating 10-year risk of first hard ASCVD events after formal risk assessment using the new Pooled Cohort Equations. Furthermore, issues of cost and radiation exposure related to measuring CAC were discussed resulting in some uncertainty regarding potential risks of more widespread screening, which resulted in a decision in the current guideline to make assessment of CAC a Class IIb recommendation among individuals for whom a risk-based treatment decision is uncertain after formal risk estimation. The Work Group notes that this Class IIb recommendation is consistent with the recommendations in the 2010 ACCF/AHA guideline (44) for patients with a 10-year CHD risk of <10%, as well as for many other patients, because of the lower risk threshold (7.5% 10-year risk for a first hard ASCVD event) adopted by the “2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults” for recommending initiation of statin therapy for ASCVD risk reduction.
Furthermore, it was noted that measuring ApoB, albuminuria, GFR, or cardiorespiratory fitness is of uncertain value. Finally, the Work Group judged that the evidence provided by Den Ruijter et al (18) in combination with the concerns about measurement quality provided sufficient rationale to recommend against measuring CIMT in routine clinical practice for risk assessment for a first ASCVD event. If any of the 9 markers considered in this report is assessed in selected patients, the use of the information to guide treatment decisions will require sound clinician judgment and should be based on shared decision making.
6.1.2. Recommendations for CQ1: Use of Newer Risk Markers After Quantitative Risk Assessment
Recommendation 1
If, after quantitative risk assessment, a risk-based treatment decision is uncertain, assessment of 1 or more of the following—family history, hs-CRP, CAC score, or ABI—may be considered to inform treatment decision making.
(Grade E, Expert Opinion); ACC/AHA COR IIb, LOE B
Recommendation 2
CIMT is not recommended for routine measurement in clinical practice for risk assessment for a first ASCVD event.
(Grade N, No Recommendation For or Against); ACC/AHA Class III: No Benefit, LOE B
Based on new evidence reviewed during ACC/AHA update of the evidence.
Recommendation 3
The contribution to risk assessment for a first ASCVD event using ApoB, chronic kidney disease, albuminuria, or cardiorespiratory fitness is uncertain at present.
(Grade N, No Recommendation For or Against)
6.2. Critical Question 2
“Are models constructed to assess the long-term (≥15 years or lifetime) risk for a first CVD event in adults effective in assessing variation in long-term risk among adults at low and/or intermediate short-term risk, whether analyzed separately or combined?”
A number of studies have noted that younger men (typically <50 years of age) and most women have low (e.g., <5% or <10%) predicted 10-year risks for CHD, and more broad CVD outcomes, despite the presence of significant risk factor burden (45,46). However, extensive epidemiological, pathological, and basic science data indicate that the development of atherosclerosis, the precursor of ASCVD, occurs over decades and is related to long-term and cumulative exposure to causal, modifiable risk factors. Thus, a life course perspective to risk assessment and prevention must be considered, especially among younger individuals. The primary value of risk factor measurement and quantitative long-term risk estimation in younger adults is 2-fold: first, to identify risk in individuals with extreme values of risk factors (e.g., familial hypercholesterolemia); second, to provide risk information and context regarding the potential benefits of lifestyle modification. When posing CQ2, the Work Group did not anticipate that long-term or lifetime risk would replace 10-year risk assessment as the foundation for absolute risk assessment and clinical decision-making. Rather, longer term risk estimates, if found to be useful, could provide adjunctive information for risk communication.
CQ2 was developed to assess the utility of long-term and lifetime risk assessment as an adjunct to short-term (10-year) risk assessment. It was recognized that there is little “disconnect” regarding approaches to prevention when the 10-year risk estimate is high (e.g., >10% predicted 10-year risk): such patients merit intensive prevention efforts and should be considered for drug therapy to reduce or modify adverse levels of causal risk factors. CQ2 was selected for evaluation to determine whether quantitative or semi-quantitative long-term risk assessment would provide differential information that could be useful in risk communication, specifically to patients estimated to be at lower short-term risk. However, it is unclear what the long-term predicted and observed risks for CHD and CVD are among individuals who are at low predicted 10-year risk. CQ2 was designed to identify studies that assessed both short- and long-term risk, particularly focusing on those studies that provide long-term outcomes data for groups predicted to be at low 10-year risk. If a sufficiently large proportion of the population is at high long-term risk despite being at low short-term risk, then incorporating long-term risk assessment into routine clinical practice might have value for informing risk conversations with patients and guiding therapeutic lifestyle counseling and other aspects of care.
6.2.1. Summary of Evidence for CQ2
Ten studies that met inclusion/exclusion criteria were identified by the systematic review performed in April, 2011, and were examined (19–22,47–52). Publication dates ranged from 1999 to 2009. All of the studies were observational. On the basis of these studies, 7 evidence statements were adopted (Appendix 2).
Multiple sources provided consistent evidence regarding the associations of traditional risk factors with events occurring during both short-term and long-term follow up. The important associations are best represented and understood in the context of multivariable risk equations that reliably predict absolute risk for ASCVD events. In addition, most of these risk factors are both causal and modifiable, indicating their central clinical importance for ASCVD prevention efforts. Given the additional evidence suggesting improved risk prediction using updated clinical covariates, the Work Group makes the following recommendations.
6.2.2. Recommendations for CQ2: Long-Term Risk Assessment
Recommendation 1
It is reasonable to assess traditional ASCVD risk factors every 4 to 6 years in adults 20 to 79 year of age who are free from ASCVD and estimate 10-year ASCVD risk every 4 to 6 years in adults 40 to 79 years of age who are free from ASCVD.
(Grade B, Moderate); ACC/AHA COR IIa, LOE B
Recommendation 2
Assessing 30-year or lifetime ASCVD risk based on traditional risk factors† may be considered in adults 20 to 59 years of age who are free from ASCVD and who are not at high short-term risk.
(Grade C, Weak); ACC/AHA COR IIb, LOE C
A downloadable spreadsheet enabling estimation of 10-year and lifetime risk for ASCVD and a web-based calculator are available at http://my.americanheart.org/cvriskcalculator and http://www.cardiosource.org/science-and-quality/practice-guidelines-and-quality-standards/2013-prevention-guideline-tools.aspx.
†Age, sex, total and HDL–cholesterol, systolic BP, use of antihypertensive therapy, diabetes, and current smoking.
Evidence was not found regarding the utility of lifetime risk assessment for guiding pharmacologic therapy decisions, and the Work Group judged that long-term and lifetime risk information may be used more appropriately at this time to motivate therapeutic lifestyle change in younger individuals. This perspective influenced the choice of age 20 as the starting point for long-term risk assessment, despite a threshold of age 40 for short-term 10-year ASCVD risk assessment.
Long-term and lifetime risk estimation may be less valuable for individuals who are found to be at high short-term (10-year) risk based on multivariable equations in whom decisions regarding prevention efforts may be clear. However, an understanding of long-term risk may provide a means for encouraging adherence to lifestyle or pharmacological therapies, especially for patients who might have difficulty understanding the importance of their short-term risk. Likewise, for older individuals, or those with limited life expectancy, clinical considerations should dictate the intensity of risk assessment and prevention efforts.
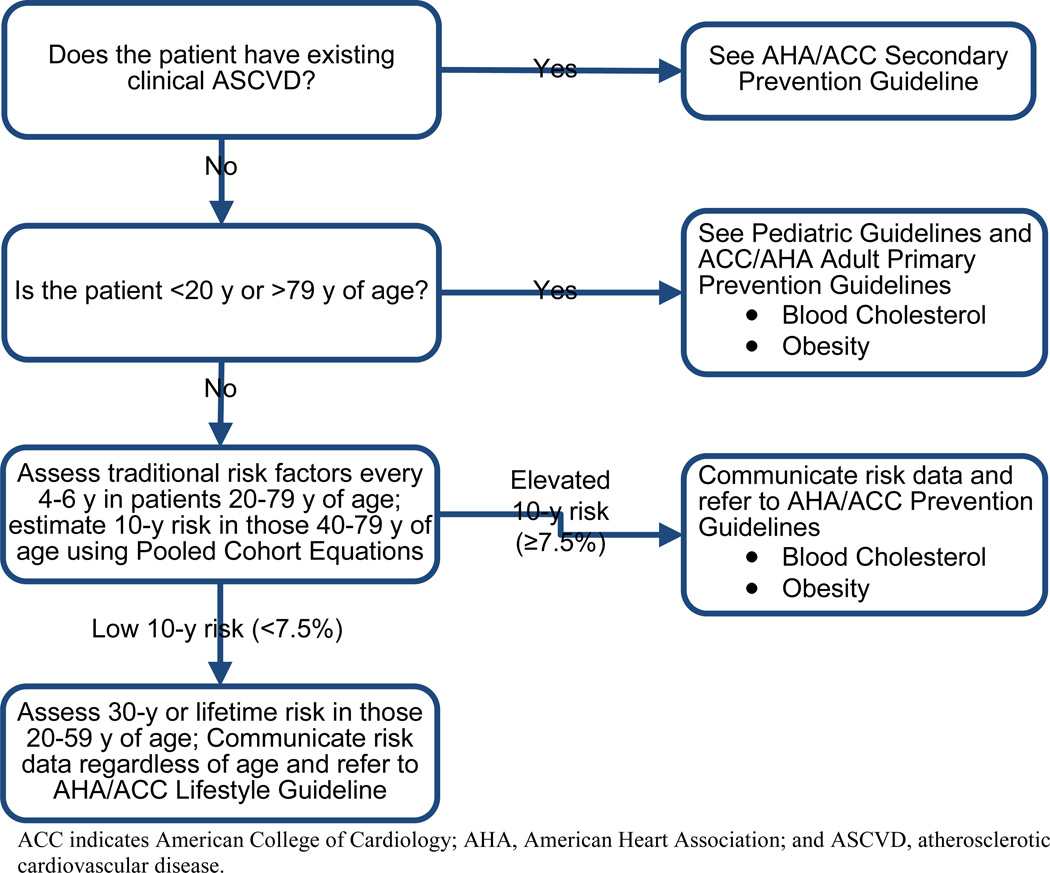
7. Implementation Considerations for Risk Assessment
A suggested approach for incorporating these recommendations into clinical practice is shown in Figure 1. For patients 20 to 79 years of age who are free from clinical ASCVD, the first step is to assess ASCVD risk factors. Whereas it is reasonable to assess ASCVD risk factors in younger and older individuals, limitations in available data prevented the development of robust risk assessment algorithms in these populations. Hence, for patients outside this age range, providers should refer to applicable clinical practice guidelines (i.e., pediatric (53) and adult primary prevention guidelines (54,55)). Risk assessment should be repeated every 4 to 6 years in persons who are found to be at low 10-year risk (<7.5%). Beginning at age 40, formal estimation of the absolute 10-year risk for ASCVD is recommended. Long-term or lifetime risk estimation is recommended for all persons who are between 20 to 39 years of age and for those between 40 to 59 years of age who are determined to be at low 10-year risk (<7.5%). As shown in Figure 1, all patients should receive applicable risk information and appropriate lifestyle counseling. The 10-year risk estimates provided by the new Pooled Cohort Equations differ from those generated by the Adult Treatment Panel III algorithm in several respects (25) as discussed in detail in the Full Work Group Report (http://jaccjacc.cardiosource.com/acc_documents/2013_FPR_S5_Risk_Assessment.pdf). To summarize, based on the risk estimation algorithm recommended by Adult Treatment Panel III, approximately 31.9% of the ASCVD-free, nonpregnant U.S. population between 40 and 79 years of age have a 10-year risk of a first hard CHD event of at least 10% or have diabetes. Based on the new Pooled Cohort Equations described here, approximately 32.9% have a 10-year risk of a first hard ASCVD of at least 7.5%. The outcomes and thresholds of these 2 approaches are different, but the overlap of these 2 means for defining high-risk groups is substantial, at roughly 75%. Nonetheless, these important differences make simple linear conversions imprecise. We recommend that healthcare organizations convert to these new Pooled Cohort Equations as soon as practical (Appendix 4). A downloadable spreadsheet enabling estimation of 10-year and lifetime risk for ASCVD and a web-based calculator are available at http://my.americanheart.org/cvriskcalculator and http://www.cardiosource.org/science-and-quality/practice-guidelines-and-quality-standards/2013-prevention-guideline-tools.aspx.
Figure 1.
Implementation of Risk Assessment Work Group Recommendations
ACC indicates American College of Cardiology; AHA, American Heart Association; and ASCVD, atherosclerotic cardiovascular disease.
8. Evidence Gaps and Future Research Needs
The Work Group strongly recommends continued research to fill gaps in knowledge regarding short- and long-term ASCVD risk assessment and outcomes in all race/ethnic groups, across the age spectrum, and in women and men. Future research should include analyses of short- and long-term risk in diverse groups; optimal communication of ASCVD risk information; utility of short-and long-term risk assessment for motivating behavioral change and adherence to therapy; utility of short-and long-term risk assessment for influencing risk factor levels and clinical outcomes; utility of differential information conveyed by short- and long-term risk assessment; and utility of novel risk markers in short- and long-term risk assessment.
9. Conclusions
The Work Group’s approach to risk assessment represents a step forward in ASCVD prevention that is large enough to justify the challenges inherent in implementing a new approach, rather than staying with the CHD risk assessment approach recommended previously. The final recommendations are summarized in Table 4 and Figure 1. Two major advantages of this approach are the ability to estimate risk for a broader based ASCVD outcome that is more relevant to additional segments of the population, including women and African Americans, and the ability to provide risk estimates specific to African Americans. Promoting lifetime risk estimation may represent an additional step forward in supporting lifestyle behavior change counseling efforts. Periodic updating of the guidelines should address numerous issues related to risk assessment.
Table 4.
Summary of Recommendations for Risk Assessment
| Recommendations | NHLBI Grade | NHLBI Evidence Statements |
ACC/AHA COR |
ACC/AHA LOE |
|---|---|---|---|---|
| 1. The race- and sex-specific Pooled
Cohort Equations* to predict 10-year risk for a first hard ASCVD event should be used in nonHispanic African Americans and nonHispanic Whites, 40 to 79 years of age. |
B (Moderate) | N/A | I | B (4–8) |
| 2. Use of the sex-specific Pooled
Cohort Equations for nonHispanic Whites may be considered when estimating risk in patients from populations other than African Americans and nonHispanic Whites. |
E (Expert Opinion) |
Appendix
2 CQ2/ES1 |
IIb | C |
| 3. If, after quantitative risk assessment, a risk-based
treatment decision is uncertain, assessment of 1 or more of the following—family history, hs-CRP, CAC score, or ABI—may be considered to inform treatment decision making. |
E (Expert Opinion) | Appendix 1 | IIb† | B (9–17) |
| 4. The contribution to risk assessment for
a first ASCVD event using ApoB, CKD, albuminuria, or cardiorespiratory fitness is uncertain at present. |
N (No Recommendation For or Against) | Appendix 1 | N/A | N/A |
| 5. CIMT is not recommended for
routine measurement in clinical practice for risk assessment for a first ASCVD event. |
N (No Recommendation For or Against) | Appendix 1 | III: No Benefit† |
B (12,16,18) |
| 6. It is reasonable to assess traditional
ASCVD risk factors‡ every 4 to 6 years in adults 20 to 79 years of age who are free from ASCVD and to estimate 10-year ASCVD risk every 4 to 6 years in adults 40 to 79 years of age without ASCVD. |
B (Moderate) |
Appendix
2 CQ2/ES7 |
IIa | B (19,20) |
| 7. Assessing 30-year or lifetime ASCVD
risk based on traditional risk factors‡ may be considered in adults 20 to 59 years of age without ASCVD and who are not at high short-term risk. |
C (Weak) |
Appendix
2 CQ2/ES2, CQ2/ES3, CQ2/ES4, CQ2/ES5, CQ2/ES6 |
IIb | C (20–22) |
A downloadable spreadsheet enabling estimation of 10-year and lifetime risk for ASCVD and a web-based calculator are available at http://my.americanheart.org/cvriskcalculator and http://www.cardiosource.org/science-and-quality/practice-guidelines-and-quality-standards/2013-prevention-guideline-tools.aspx.
Derived from the ARIC study (8), CHS (5), CARDIA study (23), Framingham original and offspring cohorts (4,6).
Based on new evidence reviewed during ACC/AHA update of evidence.
Age, sex, total and HDL–cholesterol, systolic BP, use of antihypertensive therapy, diabetes, and current smoking.
ABI indicates ankle-brachial index; ACC, American College of Cardiology; AHA, American Heart Association; ApoB, Apolipoprotein B; ASCVD, atherosclerotic cardiovascular disease; BP, blood pressure; CAC, coronary artery calcium;; CKD, chronic kidney disease; CIMT, carotid intima-media thickness; COR, Class of Recommendation; CQ, critical question, ES, evidence statement; HDL–C, high-density lipoprotein cholesterol; hs-CRP, high-sensitivity C-reactive protein; LOE, Level of Evidence; and NHLBI, National Heart, Lung, and Blood Institute.
Acknowledgment
The Work Group would like to acknowledge the significant contributions of Dr. Hongyan Ning, Biostatistician at Northwestern University Feinberg School of Medicine, in providing statistical analyses for this document.
Presidents and Staff
American College of Cardiology Foundation
John Gordon Harold, MD, MACC, President, Shalom Jacobovitz, Chief Executive Officer, William J. Oetgen, MD, MBA, FACC, Executive Vice President, Science, Education & Quality, Charlene May, Senior Director, Science and Clinical Policy
American College of Cardiology Foundation/American Heart Association
Lisa Bradfield, CAE, Director, Science and Clinical Policy
American Heart Association
Mariell Jessup, MD, FACC, FAHA, President, Nancy Brown, Chief Executive Officer, Rose Marie Robertson, MD, FAHA, Chief Science Officer, Gayle R. Whitman, PhD, RN, FAHA, FAAN, Senior Vice President, Office of Science Operations, Marco Di Buono, PhD, Vice President of Science and Research, Jody Hundley, Production Manager, Scientific Publications, Office of Science Operations
National Heart, Lung, and Blood Institute
Denise Simons-Morton, MD, PhD
RTI International
Harmon Jordan, ScD
Science Applications International Corporation
Lev Nevo, MD
National Program to Reduce Cardiovascular Risk Coordinating Committee — Organizational Representatives:
Academy of Nutrition and Dietetics, Penny Kris-Etherton, PhD, RD, American Academy of Family Physicians, Paul A. James, MD, American Academy of Pediatrics, Geoffrey L. Rosenthal, MD, PhD, American Academy of Physician Assistants, Cynthia Booth Lord, MHS, PA-C, American Association of Nurse Practitioners, Penny Kaye Jensen, DNP, APRN, FNP-C, FAANP, American College of Cardiology, Roger S. Blumenthal, MD, FACC, FAHA, American College of Physicians, Vera A. Bittner, MD, FACP, American Diabetes Association, Robert E. Ratner, MD, FACP, FACE, American College of Sports Medicine, William E. Kraus, MD, American Medical Association, Omar Hasan, MBBS, MPH, MS, FACP, American Pharmacists Association, CoraLynn B. Trewet, MS, PharmD, BCPS, CDE, American Public Health Association, Linda Rae Murray, MD, MPH, American Society of Hypertension, John D. Bisognano, MD, PhD, Association of Black Cardiologists, Inc., Karol E. Watson, MD, PhD, FACC, National Committee for Quality Assurance, Mary Barton, MD, National Initiative for Children’s Healthcare Quality, Shikha Anand, MD, MPH, National Medical Association, Leonard Weather Jr, RPh, MD, National Stroke Association, James Baranski, Preventive Cardiovascular Nurses Association, Jerilyn K. Allen, RN, ScD, FAAN, The National Lipid Association, Terry A. Jacobson, MD, The Obesity Society, Harvey Grill, PhD, Agency for Healthcare Research and Quality, David Meyers, MD, Centers for Disease Control and Prevention, Peter Briss, MD, MPH, Centers for Medicare & Medicaid Services, Joseph Chin, MD, Health Resources and Services Administration, Sarah R. Linde, MD, Indian Health Service, Susan V. Karol, MD, National Institutes of Health, Barry Portnoy, PhD, U.S. Department of Agriculture (USDA), Rajen S. Anand, PhD, U.S. Department of Defense, Warren Lockette, MD, U.S. Department of Veterans Affairs, Salim S. Virani, MD, PhD, U.S. Food and Drug Administration, Robert Temple, MD
Appendix 1
Evidence Statements for CQ1
| ES Number |
Author/Group | Factor | Evidence Statement/Conclusion |
|---|---|---|---|
| 1 | USPSTF (9) | hs-CRP | “Strong evidence indicates that CRP is
associated with CHD events. Moderate, consistent evidence suggests that adding CRP to risk prediction models among initially intermediate-risk persons improves risk stratification.” “Few studies directly assessed the effect of CRP on risk reclassification in intermediate-risk persons.” hs-CRP was associated with risk and results in some reclassification in intermediate-risk persons, but it was not clear whether this reclassification led to a net improvement in prediction. Values of receiver operating curve C-statistics, measures of discrimination, are mentioned but not reported; hence, no evidence on discrimination, calibration, net reclassification index or cost-effectiveness was provided. Reports some impact on reclassification, probably modest (pp. 488–491). |
| 2 | Helfand et al., 2009 (12) |
hs-CRP, CAC, CIMT, ABI |
With respect to risk assessment for major CHD, the
authors concluded that, “The current evidence does not support the routine use of any of the 9 risk factors for further risk stratification of intermediate-risk persons.” The nine risk factors examined were: hs-CRP, CAC score as measured by electron-beam computed tomography, lipoprotein (a) level, homocysteine level, leukocyte count, fasting blood glucose, periodontal disease, ABI, and CIMT. hs-CRP was associated with CHD and led to some reclassification. The authors cite the JUPITER results to support the conclusion that hs-CRP testing may be useful in intermediate-risk patients to drive statin therapy. The Work Group recognizes that more recent individual study results have been published. Updated systematic reviews addressing discrimination, calibration, reclassification, and cost issues in the context of the newer ASCVD risk assessment model proposed in this document are needed. CAC was associated with CHD and with some reclassification, but it is uncertain how much and how valuable this reclassification is. The document provides little evidence regarding discrimination, calibration, and cost-effectiveness. The Work Group also is concerned about radiation and incidental findings. The Work Group recognizes that more recent individual study results have been published. Updated systematic reviews addressing discrimination, calibration, reclassification, cost, and safety issues in the context of the newer ASCVD risk assessment model proposed in this document are needed. CIMT was associated with CHD, but the document provides little evidence regarding reclassification, discrimination, calibration, and cost-effectiveness. The Work Group also has concerns about measurement issues. Standardization of CIMT measurement is a major challenge. The Work Group recognizes that more recent individual study results have been published. Updated systematic reviews addressing discrimination, calibration, reclassification, cost, and measurement (standardization) issues in the context of the newer ASCVD risk assessment model proposed in this document are needed. ABI was associated with CHD and some reclassification, but it is uncertain how much and how valuable this reclassification is. Evidence suggests some improvement in discrimination, but the document provides little evidence regarding calibration and cost-effectiveness. The Work Group members are uncertain whether more recent individual study results have been published relevant to ABI. Updated systematic reviews addressing discrimination, calibration, reclassification, and cost issues in the context of the newer ASCVD risk assessment model proposed in this document are needed. |
| 3 | Emerging Risk Factors Collaboration (13) |
hs-CRP | “CRP concentration has continuous associations
with the risk for coronary heart disease, ischaemic stroke, vascular mortality, and death from several cancers and lung disease that are each of broadly similar size. The relevance of CRP to such a range of disorders is unclear. Associations with ischaemic vascular disease depend considerably on conventional risk factors and other markers of inflammation.” hs-CRP is associated with risk for CVD. This analysis did not directly assess value in risk prediction. No additional evidence was provided regarding discrimination, calibration, reclassification, or cost-effectiveness. |
| 4 | Schnell-Inderst et al., 2010 (17) |
hs-CRP | For MI and cardiovascular mortality, “Adding
hs-CRP to traditional risk factors improves risk prediction, but the clinical relevance and cost-effectiveness of this improvement remain unclear.” Absolute differences in C-statistics between models including and not including hs-CRP ranged from 0.00 to 0.027. Some evidence was provided to support the cost-effectiveness of hs-CRP testing in some modeling scenarios, characterized by intermediate- and higher-risk populations and lower cost (generics) statins of at least moderate efficacy. |
| 5 | Emerging Risk Factors Collaboration (41) |
ApoB | This paper provided evidence of rough equivalence of
associations of CVD with non-HDL–C and ApoB after multivariable adjustment (including HDL–C). See Figure 1 for CHD and the text for stroke. By inference, this finding means there would be rough equivalence between ApoB and total cholesterol with similar adjustment. |
| 6 | Sniderman et al., 2011 (43) |
ApoB | ApoB was more strongly related to risk for ASCVD than
either non-HDL–C or LDL–C in a substitution model that also included HDL–C. No evidence was presented pertinent to an addition model in which ApoB might be added to a model that included total cholesterol, LDL–C or non-HDL–C. Additional models are the type of model of interest to this question. By inference, these results may mean that ApoB is more strongly related to risk than is total cholesterol. This paper did not address directly the value of adding ApoB to a model with traditional risk factors. No information was presented regarding discrimination, calibration, reclassification, or cost. The relative risks evaluated in the meta-analysis were adjusted for various sets of covariates in the various primary reports, and the adjustments were judged to be incomplete. Furthermore, studies of varying designs and quality were included, leaving the Work Group members concerned regarding the validity of the evidence |
| 7 | Kodama et al., 2009 (42) |
Cardiorespiratory fitness |
Better cardiorespiratory fitness was associated with
lower risk for all-cause mortality and CHD/CVD. Based on the sensitivity analyses in table 2, evidence of association was weaker for CHD/CVD, but still significant, when based on studies with more complete adjustment for other risk factors. The utility of assessing cardiorespiratory fitness in risk prediction was not assessed (discrimination, calibration, reclassification and cost). |
| 8 | Ankle Brachial Index Collaboration (11) |
ABI | ABI is associated with total CHD risk and leads to
significant reclassification, and the pattern of reclassification is different by sex. Among men, the effect is to down-classify high-risk men. Among women the effect is to up-classify low-risk women. Overall, the FRS, as applied by the investigators, showed relatively poor discrimination in this meta-analysis, with C-statistics of 0.646 (95% CI: 0.643–0.657) in men and 0.605 (0.590–0.619) in women. There was an improvement in C-statistic in both men, 0.655 (0.643–0.666) and women 0.658 (0.644–0.672) when ABI was added to a model with FRS. The improvement in the C-statistic was greater and significant in women but was not significant in men. No evidence on calibration, net reclassification index, or cost-effectiveness was provided. |
| 9 | Empana, et al, 2011 (10) |
Family history of CHD |
“In separate models adjusted for age, gender,
and study cohort, a family history of CHD, BMI, and waist circumference were all predictors of CHD. When traditional risk factors were controlled for, family history of CHD (p<0.001) and BMI (p=0.03) but not waist circumference (p=0.42) remained associated with CHD. However, the addition of family history of CHD or BMI to the traditional risk factors model did not improve the discrimination of the model (not shown).” This paper developed a CHD risk prediction algorithm based on 4 French population studies, and evaluated, among other factors, the contribution of family history to traditional risk factors. Family history of CHD was defined as the self-report of a myocardial infarction (MI) in first degree relatives (parents and siblings) in the D.E.S.I.R. and SU.VI.MAX studies, as a history of MI before 55 years in men and before 65 years in women in parents, siblings, and grandparents in the PRIME study, and as a death due to MI in first degree relatives in the Three City study. No evidence on calibration, net reclassification index, or cost-effectiveness was provided. |
| 10 | Moyer et al. 2013 (15) |
ABI | This paper is an updated review of the utility of
assessing ABI for the USPSTF. “The USPSTF concludes that the current evidence is insufficient to assess the balance of benefits and harms of screening for PAD and CVD risk assessment with the ABI in adults. (I statement)” “The USPSTF found no evidence that screening for and treatment of PAD in asymptomatic patients leads to clinically important benefits. It also reviewed the potential benefits of adding the ABI to the FRS and found evidence that this results in some patient risk reclassification; however, how often the reclassification is appropriate or whether it results in improved clinical outcomes is not known.” The Work Group notes that this review provides some evidence that assessing ABI may improve risk assessment; however, no evidence was found by the USPSTF reviewers pertinent to the question of whether measuring ABI leads to better patient outcomes. |
| 11. | Peters et al. 2012 (16) |
CIMT, CAC | This paper is a systematic review of the literature
regarding the contribution to risk assessment of imaging for subclinical atherosclerosis. “Published evidence on the added value of atherosclerosis imaging varies across the different markers, with limited evidence for FMD and considerable evidence for CIMT, carotid plaque and CAC. The added predictive value of additional screening may be primarily found in asymptomatic individuals at intermediate cardiovascular risk. Additional research in asymptomatic individuals is needed to quantify the cost effectiveness and impact of imaging for subclinical atherosclerosis on cardiovascular risk factor management and patient outcomes.” Regarding CIMT: “The c-statistic of the prediction models without CIMT increased from 0.00 to 0.03 when CIMT was added. In the Atherosclerosis Risk In Communities (ARIC) study, addition of CIMT to the prediction model resulted in an NRI overall of 7.1% (95% CI 2.2% to 10.6%) and an IDI of 0.007 (95% CI 0.004 to 0.010). The NRI intermediate was 16.7% (95% CI 9.3% to 22.4%). In contrast, 10 year results from the Carotid Atherosclerosis Progression Study showed that addition of CIMT to the prediction model resulted in an IDI of 0.04% and NRI overall of −1.41%. Analysis of 1574 participants from the Firefighters and Their Endothelium study showed an NRI overall of 11.6% (p=0.044) and an NRI intermediate of 18.0% (p=0.034).” The Work Group notes that this paper provides some evidence to consider assessing CIMT; however, this conclusion was not supported by the Den Ruijter article described below. Regarding CAC: “The c-statistic increased from 0.04 to 0.13 when CAC was added to the model. Four recently published studies also reported results on the NRI and/or the IDI. One of these studies comprised a subgroup analysis of an earlier publication in the total population in individuals without indications for statin therapy. Analyses of the MESA study showed that addition of CAC to the conventional prediction model resulted in an NRI overall of 25% (95% CI 16% to 34%) and an NRI intermediate of 55% (95% CI 41% to 69%). The IDI in the MESA study was 0.026. Results were similar in the Rotterdam study. Addition of CAC to the prediction model led to an NRI overall of 14% (p<0.01) which was mainly driven by correctly reclassifying those at intermediate risk according to the traditional prediction model. Results from the Heinz Nixdorf Recall study also showed large NRIs when CAC was added to the Framingham Risk Score. Using different thresholds to define the intermediate risk category (10–20% or 6–20%), the NRI overall was 22% and 20%, respectively. The NRI intermediate was 22% for intermediate risk thresholds of 10–20% and 31% for intermediate risk thresholds of 6–20%. In addition, the IDI was 0.0152 when the prediction models with and without CAC were compared. The NRI overall was 25.1% and the IDI was 0.0167 in individuals from the Heinz Nixdorf Recall study without indications for statin therapy.” The Work Group notes that this paper provides evidence to support the conclusion that assessing CAC is likely to be the most useful approach to improving risk assessment among individuals found to be at intermediate risk after formal risk assessment. Furthermore, we note that the outcomes in the studies reviewed above were CHD, not ASCVD. The Work Group discussed concerns about cost, radiation exposure and the uncertainty of the contribution of assessing CAC to estimating 10-year risk of hard ASCVD after formal risk assessment. |
| 12. | Kashani et al, 2013 (14) |
Family history | This paper is an integrative literature review on the
contribution of assessing family history to
risk appraisal. “The evidence demonstrates that family history is an independent contributor to risk appraisal and unequivocally supports its incorporation to improve accuracy in global CVD risk estimation.” The Work Group notes that a variety of endpoints, clinical and subclinical, were included in the reviewed papers. No evidence on discrimination, calibration, net reclassification index, or cost-effectiveness was provided. |
| 13. | Den Ruijter et al, 2012 (18) |
CIMT | This paper is an individual level meta-analysis of
“14 population-based cohorts contributing data for 45 828 individuals. During a median follow-up of 11 years, 4007 first-time myocardial infarctions or strokes occurred.” “We first refitted the risk factors of the FRS and then extended the model with common CIMT measurements to estimate the absolute 10-year risks to develop a first-time myocardial infarction or stroke in both models. The C statistic of both models was similar (0.757; 95% CI, 0.749–0.764; and 0.759; 95% CI, 0.752–0.766). The net reclassification improvement with the addition of common CIMT was small (0.8%; 95% CI, 0.1%–1.6%). In those at intermediate risk, the net reclassification improvement was 3.6% in all individuals (95% CI, 2.7%–4.6%) and no differences between men and women.” “The addition of common CIMT measurements to the FRS was associated with small improvement in 10-year risk prediction of first-time myocardial infarction or stroke, but this improvement is unlikely to be of clinical importance.” The Work Group judged this paper to provide the strongest evidence available regarding the potential value of CIMT to risk assessment. The Work Group also has concerns about measurement issues. Standardization of CIMT measurement is a major challenge. |
ABI indicates ankle-brachial index; ApoB, apolipoprotein B; BMI, body mass index; ASCVD, atherosclerotic cardiovascular disease; CVD, cardiovascular disease; CAC, coronary artery calcium; CHD, coronary heart disease; CIMT, carotid intima-media thickness; ES, evidence statement; FRS, Framingham Risk Score; HDL–C, high-density lipoprotein cholesterol; hs-CRP, high-sensitivity C-reactive protein; JUPITER, Justification for the Use of Statins in Primary Prevention: An Intervention Trial Evaluating Rosuvastatin; LDL–C, low-density lipoprotein cholesterol; MI, myocardial infarction; and USPSTF, United States Preventive Services Task Force.
Appendix 2
Evidence Statements for CQ2
| Evidence Statement | References |
|---|---|
| 1. We found no evidence assessing variations in
long-term or lifetime risk for CVD outcomes among persons at low or
intermediate short-term risk in race/ethnic groups other than nonHispanic Whites in the United States and Europe. Strength of Evidence: None |
-- |
| 2. ASCVD risk factors measured in young and
middle-aged adults, considered singly or jointly, generally are associated with
short-term (≤10 years), long-term (≥15 years), and lifetime risk
for ASCVD. Strength of Evidence: Low (for diabetes and metabolic syndrome) to Moderate (for BMI, cholesterol, systolic BP, and smoking). |
(20,21,47,48,51,52) |
| 3. Multivariable short-term (10-year) CHD risk
prediction models underestimate absolute lifetime risk for CHD, but may
stratify relative lifetime risk for CHD in women and older men.* Strength of Evidence: Low *CHD is defined as all manifestations of CHD, or as CHD death/nonfatal MI. |
(22) |
| 4. Long-term (30-year) risk equations based on
traditional ASCVD risk factors* provide more accurate prediction of
long-term ASCVD† risk than do extrapolations of short-term (10-year) risk equations among individuals 20 to 59 years of age free from ASCVD. Strength of Evidence: Low *Age, sex, total and HDL–C, systolic BP, use of antihypertensive therapy, diabetes, current smoking †CHD death, nonfatal MI, or fatal/nonfatal stroke; or all ASCVD |
(20) |
| 5. The presence and severity of selected
traditional ASCVD risk factors* stratify absolute levels of lifetime risk for
ASCVD† among nonHispanic White adults 45 to 50 years of age who are free of ASCVD and not at high short-term risk. Strength of Evidence: Low *Risk factors were considered in 5 mutually exclusive strata encompassing the full spectrum of risk levels, as follows: 1) ≥2 major risk factors (defined as total cholesterol ≥240 mg/dL or treated, systolic BP ≥160 or diastolic BP ≥100 mm Hg or treated, or diabetes, or current smoking), lifetime risk for ASCVD >50%; 2) 1 major risk factor only, lifetime risk for ASCVD 39% to 50%; 3) ≥1 elevated risk factors (defined as untreated total cholesterol 200 to 239 mg/dL, or untreated systolic BP 140 to 159 mm Hg or diastolic BP 90 to 99 mm Hg, and no diabetes and no current smoking), lifetime risk for ASCVD 39% to 46%; 4) 1 or more risk factors at nonoptimal levels (untreated total cholesterol 180 to 199 mg/dL, or untreated systolic BP 120 to 139 mm Hg or diastolic BP 80 to 89 mm Hg, and no diabetes and no current smoking), lifetime risk for ASCVD 27% to 36%; and 5) all optimal levels of risk factors (defined as untreated total cholesterol <180 mg/dL, and untreated BP <120/<80 mm Hg, and no diabetes, and no current smoking), lifetimes risk for ASCVD <10%. †CHD death, MI, coronary insufficiency, angina, fatal/nonfatal atherothrombotic stroke, claudication, other CVD death |
(21) |
| 6. Long-term (≥15 years) risk prediction
models based on selected traditional ASCVD risk factors* predict CHD death with
good discrimination and calibration, and better in women than men, in U.S. nonHispanic White populations. Strength of Evidence: Low *Age, sex, total cholesterol, systolic BP, diabetes, smoking |
(50) |
| 7. Measuring and updating ASCVD risk factors every
4 to 6 years improves short- and long-term risk
prediction. Strength of Evidence: Moderate |
(19,20) |
ASCVD indicates atherosclerotic cardiovascular disease; BMI, body mass index; BP, blood pressure; CHD, coronary heart disease; CVD, cardiovascular disease; CQ, critical question; HDL–C, high-density lipoprotein cholesterol; IDI, improvement index; MI, myocardial infarction; NRI, net reclassification index; PAD, peripheral artery disease; and --, none.
Appendix 4
Development and Steps for Implementation of the ASCVD Pooled Cohort Risk Equations
Prior experience with the development of the Framingham Heart Study 10-year CHD risk prediction equations (25,56), and the more recent Framingham 10-year general CVD risk prediction equations (63), were used as a basis for developing the new Pooled Cohort Risk Equations. To expand the utility and generalizability of the new equations, extensive data were used from several large, racially and geographically diverse, modern NHLBI-sponsored cohort studies, including the ARIC (Atherosclerosis Risk in Communities) study (8), Cardiovascular Health Study (5), and the CARDIA (Coronary Artery Risk Development in Young Adults) study (7), combined with applicable data from the Framingham Original and Offspring Study cohorts (4,6).
A total of 11,240 White women (who experienced 902 hard ASCVD events), 9,098 White men (1,259 hard ASCVD events), 2,641 African-American women (290 hard ASCVD events), and 1,647 African-American men (238 hard ASCVD events) who met the following criteria were included: 40 to 79 years of age, apparently healthy, and free of a previous history of nonfatal myocardial infarction (recognized or unrecognized), stroke, HF, percutaneous coronary intervention, coronary artery bypass surgery, or atrial fibrillation. Data from the included participants were used to develop sex- and race-specific equations to predict 10-year risk for a first hard ASCVD event. Due to the growing health burden of HF, the Work Group examined the possibility of including HF as an outcome. However, study-by-study ascertainment and adjudication of HF varied considerably, and therefore HF could not be included as an outcome. Due to known substantial geographic variation in use, (Dartmouth Atlas of Healthcare, http://www.dartmouthatlas.org/) self-selection, and physician recommendation biases (64), coronary revascularization was also not included as an endpoint.
The Pooled Cohort Equations for estimating ASCVD were developed from sex- and race-specific proportional hazards models that included the covariates of age, treated or untreated systolic BP level, total cholesterol and high-density lipoprotein cholesterol levels, current smoking status (Y/N), and history of diabetes (Y/N). A variable representing lipid treatment was considered, but not retained in the final model because lipid therapy was relatively uncommon in the cohorts and statistical significance was lacking. Baseline characteristics of the participants included in the equation derivation model are shown in the Full Panel Report Data Supplement, as are details of the methods used to derive, evaluate, and validate (internally and externally) the resulting risk equations and their potential limitations. In summary, discrimination and calibration of the models were very good. C statistics ranged from a low of 0.713 (African-American men) to a high of 0.818 (African-American women). Calibration chi-square statistics ranged from a low of 4.86 (nonHispanic White men) to a high of 7.25 (African-American women). The coefficients for the equations for calculating an estimate of an individual’s 10-year risk for a first hard ASCVD event are provided in Table A, along with examples based on a specific risk profile for each race-sex group. The step-by-step process for estimating the risk in the specific examples of Table A is provided in Table B. These 2 tables are intended to enable programmers to integrate these equations into electronic health records.
Table A.
Equation Parameters of the Pooled Cohort Equations for Estimation of 10-Year Risk for Hard ASCVD* and Specific Examples for Each Race and Sex Group
| White | African American | |||||
|---|---|---|---|---|---|---|
| Coefficient | Individual Example Value |
Coefficient × Value† | Coefficient | Individual Example Value |
Coefficient × Value† | |
| Women (Example: 55 years of age with total cholesterol 213 mg/dL, HDL–C 50 mg/dL, untreated systolic BP 120 mm Hg, nonsmoker, and without diabetes) | ||||||
| Ln Age (y) | –29.799 | 4.01 | –119.41 | 17.114 | 4.01 | 68.58 |
| Ln Age, Squared |
4.884 | 16.06 | 78.44 | N/A | N/A | N/A |
| Ln Total Cholesterol (mg/dL) |
13.540 | 5.36 | 72.59 | 0.940 | 5.36 | 5.04 |
| Ln
Age×Ln Total Cholesterol |
–3.114 | 21.48 | –66.91 | N/A | N/A | N/A |
| Ln HDL–C (mg/dL) |
–13.578 | 3.91 | –53.12 | –18.920 | 3.91 | –74.01 |
| Ln Age×Ln HDL–C |
3.149 | 15.68 | 49.37 | 4.475 | 15.68 | 70.15 |
| Log Treated Systolic BP (mm Hg) |
2.019 | – | – | 29.291 | – | – |
| Log Age×Log Treated Systolic BP |
N/A | N/A | N/A | –6.432 | – | – |
| Log Untreated Systolic BP (mm Hg) |
1.957 | 4.79 | 9.37 | 27.820 | 4.79 | 133.19 |
| Log
Age×Log Untreated Systolic BP |
N/A | N/A | N/A | –6.087 | 19.19 | –116.79 |
| Current Smoker (1=Yes, 0=No) |
7.574 | 0 | 0 | 0.691 | 0 | 0 |
| Log Age × Current Smoker |
–1.665 | 0 | 0 | N/A | N/A | N/A |
| Diabetes (1=Yes, 0=No) |
0.661 | 0 | 0 | 0.874 | 0 | 0 |
| Individual Sum | –29.67 | 86.16 | ||||
| Mean (Coefficient×Value) |
N/A | N/A | –29.18 | N/A | N/A | 86.61 |
| Baseline Survival |
N/A | N/A | 0.9665 | N/A | N/A | 0.9533 |
| Estimated 10-Y Risk for hard ASCVD |
N/A | N/A | 2.1% | N/A | N/A | 3.0% |
| Men (Example: 55 years of age with total cholesterol 213 mg/dL, HDL–C 50 mg/dL, untreated systolic BP 120 mm Hg, nonsmoker, and without diabetes) | ||||||
| Log Age (y) | 12.344 | 4.01 | 49.47 | 2.469 | 4.01 | 9.89 |
| Log Total Cholesterol (mg/dL) |
11.853 | 5.36 | 63.55 | 0.302 | 5.36 | 1.62 |
| Log
Age×Log Total Cholesterol |
–2.664 | 21.48 | –57.24 | N/A | N/A | N/A |
| Log HDL–C (mg/dL) |
–7.990 | 3.91 | –31.26 | –0.307 | 3.91 | –1.20 |
| Log Age×Log HDL–C |
1.769 | 15.68 | 27.73 | N/A | N/A | N/A |
| Log Treated Systolic BP (mm Hg) |
1.797 | – | – | 1.916 | – | – |
| Log Untreated Systolic BP (mm Hg) |
1.764 | 4.79 | 8.45 | 1.809 | 4.79 | 8.66 |
| Current Smoker (1=Yes, 0=No) |
7.837 | 0 | 0 | 0.549 | 0 | 0 |
| Log Age × Current Smoker |
–1.795 | 0 | 0 | N/A | N/A | N/A |
| Diabetes (1=Yes, 0=No) |
0.658 | 0 | 0 | 0.645 | 0 | 0 |
| Individual Sum | 60.69 | 18.97 | ||||
| Mean (Coefficient×Value) |
N/A | N/A | 61.18 | N/A | N/A | 19.54 |
| Baseline Survival |
N/A | N/A | 0.9144 | N/A | N/A | 0.8954 |
| Estimated 10-Y Risk for hard ASCVD |
N/A | N/A | 5.3% | N/A | N/A | 6.1% |
Defined as first occurrence of nonfatal MI or CHD death, or fatal or nonfatal stroke.
Coefficient×Value: For age, lipids, and BP, defined as the natural log of the value multiplied by the parameter estimate. When an age interaction is present with lipids or BP, the natural log of age is multiplied by the natural log of the lipid or BP, and the result is multiplied by the parameter estimate. “N/A” indicates that that specific covariate was not included in the model for that sex-race group; “–” indicates that this value was not included in the example (e.g., this example used untreated systolic BP, not treated systolic BP).
ASCVD indicates atherosclerotic cardiovascular disease; BP indicates blood pressure; CHD, congestive heart disease; HDL–C, high-density lipoprotein cholesterol; MI, myocardial infarction; and N/A, not included.
Table B.
Estimating an Individual’s 10-Year Risk for Incident Hard ASCVD
| The hypothetical profile provided in Table 5 (the “Individual Example
Value” column) is identical for each race and sex group and is based on the overall sample mean. The profile assumes an individual 55 years of age (for which the Ln[Age]=4.01), with a total cholesterol of 213 mg/dL, HDL–C of 50 mg/dL, and an untreated systolic BP of 120 mm Hg. This individual is not a current smoker and does not have diabetes. For the equations, the values for age, lipids, and systolic BP are log transformed. Interactions between age and lipids or age and systolic BP use the natural log of each variable (e.g., Ln[Age]×Ln[Total Cholesterol]). | |
| Calculation of the 10-year risk estimate for hard
ASCVD can best be described as a series of steps. The natural log of age, total cholesterol, HDL–C, and systolic BP are first calculated with systolic BP being either a treated or untreated value. Any appropriate interaction terms are then calculated. These values are then multiplied by the coefficients from the equation (“Coefficient” column of Table A) for the specific race-sex group of the individual. The “Coefficient×Value” column in the table provides the results of the multiplication for the risk profile described above. | |
| The sum of the
“Coefficient×Value” column is then calculated for the
individual. For the profile shown in Table
A, this value is shown as “Individual Sum” for each race and sex group. | |
| The estimated 10-year risk of a first hard ASCVD
event is formally calculated as 1 minus the survival rate at 10 years (“Baseline Survival” in Table A), raised to the power of the exponent of the “Coefficient×Value” sum minus the race and sex specific overall mean “Coefficient×Value” sum; or, in equation form: | |
| Using White men as an example: equates to a 5.3% probability of a first hard ASCVD event within 10 years. |
ASCVD indicates atherosclerotic cardiovascular disease; BP, blood pressure; and HDL–C, high-density lipoprotein cholesterol.
The Work Group also considered the inclusion of additional and novel risk markers in the risk equations. Based on the availability of data across cohorts at applicable examination cycles, additional risk markers were evaluated for potential inclusion if they improved model performance using the framework of Hlatky et al (40). The additional risk markers that were evaluated included diastolic BP; family history of ASCVD; moderate or severe chronic kidney disease (defined as an estimated GFR of <60 mL/min per 1.73 m2) (65); and body mass index (continuous or categorical). None of these variables significantly improved discrimination for 10-year hard ASCVD risk prediction when added to the final base models. Other risk markers (hs-CRP, ApoB, microalbuminuria, cardiorespiratory fitness, CAC score, CIMT, and ABI) could not be evaluated in creating this new model due to absence of data or lack of inclusion in the appropriate examination cycle of 1 or more of the studies. Therefore, these and the other risk markers were addressed in CQ1 as potential adjuncts to quantitative risk estimation.
Further research using state-of-the art statistical techniques (including net reclassification improvement and integrative discrimination index (66)) are needed to examine the utility of novel biomarkers when added to these new Pooled Cohort Equations in different populations and patient subgroups. Randomized clinical trials demonstrating the utility of screening with novel risk markers would represent the best evidence for their inclusion in future risk assessment algorithms. In the absence of evidence from trials, methodologically rigorous observational studies should be conducted to evaluate utility.
Appendix 6
ACC/AHA Expert Reviewer Relationships With Industry and Other Entities
| Reviewer | Employment | Representing | Consultant | Speaker’s Bureau |
Ownership/ Partnership/ Principal |
Personal Research |
Expert Witness |
|---|---|---|---|---|---|---|---|
| Ezra A. Amsterdam |
University of California (Davis) Medical Center, Division of Cardiology— Professor |
ACC/AHA | None | None | None | None | None |
| Ralph G. Brindis |
University of California, San Francisco— Department of Medicine & the Phillip R. Lee Institute for Health Policy Studies—Clinical Professor of Medicine |
ACC/AHA Task Force on Practice Guidelines |
None | None | None | None | None |
| Frederick A. Masoudi |
University of Colorado, Anschutz Medical Campus—Professor of Medicine (Cardiology) |
ACC/AHA | None | None | None | None | None |
ACC indicates American College of Cardiology and AHA American Heart Association.
Appendix 7
Abbreviations
- ABI
ankle-brachial index
- ACC
American College of Cardiology
- AHA
American Heart Association
- ApoB
apolipoprotein B
- ASCVD
atherosclerotic cardiovascular disease
- BP
blood pressure
- CAC
coronary artery calcium
- CHD
coronary heart disease
- CIMT
carotid intima-media thickness
- COR
class of recommendation
- CQ
critical question
- CV
cardiovascular
- CVD
cardiovascular disease
- GFR
glomerular filtration rate
- HF
heart failure
- hs-CRP
high-sensitivity C-reactive protein
- LOE
level of evidence
- NHLBI
National Heart, Lung, and Blood Institute
- NHLBAC
NHLBI Advisory Council
- NPRCR
National Program to Reduce Cardiovascular Risk
- RWI
relationships of authors with industry and other entities
- Task Force
ACC/AHA Task Force on Practice Guidelines
- U.S.
United States
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
This document was approved by the American College of Cardiology Board of Trustees and the American Heart Association Science Advisory and Coordinating Committee in November 2013.
References
- 1.Committee on Standards for Developing Trustworthy Clinical Practice Guidelines, Institute of Medicine. Clinical Practice Guidelines We Can Trust: The National Academies Press. 2011 [Google Scholar]
- 2.Gibbons GH, Harold JG, Jessup M, Robertson RM, Oetgen WJ. The Next Steps in Developing Clinical Practice Guidelines for Prevention. Journal of the American College of Cardiology. 2013;62:1399–1400. doi: 10.1016/j.jacc.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 3.Gibbons GH, Shurin SB, Mensah GA, Lauer MS. Refocusing the Agenda on Cardiovascular Guidelines: An Announcement From the National Heart, Lung, and Blood Institute. Journal of the American College of Cardiology. 2013;62:1396–1398. doi: 10.1016/j.jacc.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 4.Dawber TR, Kannel WB, Lyell LP. An approach to longitudinal studies in a community: the Framingham study. Ann N Y Acad Sci. 1963;107:539–556. doi: 10.1111/j.1749-6632.1963.tb13299.x. [DOI] [PubMed] [Google Scholar]
- 5.Fried LP, Borhani NO, Enright P, et al. The Cardiovascular Health Study: design and rationale. Annals of epidemiology. 1991;1:263–76. doi: 10.1016/1047-2797(91)90005-w. [DOI] [PubMed] [Google Scholar]
- 6.Kannel WB, Feinleib M, McNamara PM, Garrison RJ, Castelli WP. An investigation of coronary heart disease in families. The Framingham offspring study. Am J Epidemiol. 1979;110:281–290. doi: 10.1093/oxfordjournals.aje.a112813. [DOI] [PubMed] [Google Scholar]
- 7.Friedman GD, Cutter GR, Donahue RP, et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41:1105–1116. doi: 10.1016/0895-4356(88)90080-7. [DOI] [PubMed] [Google Scholar]
- 8.Investigators TA. The Atherosclerosis risk in communities (ARIC) study: design and objectives. Am J Epidemiol. 1989;129:687–702. [PubMed] [Google Scholar]
- 9.Buckley DI, Fu R, Freeman M, Rogers K, Helfand M. C-reactive protein as a risk factor for coronary heart disease: a systematic review and meta-analyses for the U.S. Preventive Services Task Force. Annals of internal medicine. 2009;151:483–495. doi: 10.7326/0003-4819-151-7-200910060-00009. [DOI] [PubMed] [Google Scholar]
- 10.Empana JP, Tafflet M, Escolano S, et al. Predicting CHD risk in France: a pooled analysis of the D.E.S.I.R., Three City, PRIME, and SU.VI.MAX studies. European journal of cardiovascular prevention and rehabilitation : official journal of the European Society of Cardiology, Working Groups on Epidemiology & Prevention and Cardiac Rehabilitation and Exercise Physiology. 2011;18:175–185. doi: 10.1177/1741826710389354. [DOI] [PubMed] [Google Scholar]
- 11.Fowkes FGR, Murray GD, Butcher I, et al. Ankle brachial index combined with Framingham Risk Score to predict cardiovascular events and mortality: a meta-analysis. JAMA : the journal of the American Medical Association. 2008;300:197–208. doi: 10.1001/jama.300.2.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Helfand M, Buckley DI, Freeman M, et al. Emerging risk factors for coronary heart disease: a summary of systematic reviews conducted for the U.S. Preventive Services Task Force. Annals of internal medicine. 2009;151:496–507. doi: 10.7326/0003-4819-151-7-200910060-00010. [DOI] [PubMed] [Google Scholar]
- 13.Kaptoge S, Di Angelantonio E, Lowe G, et al. C-reactive protein concentration and risk of coronary heart disease, stroke, and mortality: an individual participant meta-analysis. Lancet. 2010;375:132–140. doi: 10.1016/S0140-6736(09)61717-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kashani M, Eliasson A, Vernalis M, Costa L, Terhaar M. Improving Assessment of Cardiovascular Disease Risk by Using Family History: An Integrative Literature Review. The Journal of cardiovascular nursing. 2013 doi: 10.1097/JCN.0b013e318294b206. [DOI] [PubMed] [Google Scholar]
- 15.Moyer VA. Screening for peripheral artery disease and cardiovascular disease risk assessment with the ankle-brachial index in adults: u.s. Preventive services task force recommendation statement. Annals of internal medicine. 2013;159:342–348. doi: 10.7326/0003-4819-159-5-201309030-00008. [DOI] [PubMed] [Google Scholar]
- 16.Peters SA, den Ruijter HM, Bots ML, Moons KG. Improvements in risk stratification for the occurrence of cardiovascular disease by imaging subclinical atherosclerosis: a systematic review. Heart. 2012;98:177–184. doi: 10.1136/heartjnl-2011-300747. [DOI] [PubMed] [Google Scholar]
- 17.Schnell-Inderst P, Schwarzer R, Göhler A, et al. Prognostic value, clinical effectiveness, and cost-effectiveness of high-sensitivity C-reactive protein as a marker for major cardiac events in asymptomatic individuals: a health technology assessment report. International journal of technology assessment in health care. 2010;26:30–39. doi: 10.1017/S0266462309990870. [DOI] [PubMed] [Google Scholar]
- 18.Den Ruijter HM, Peters SA, Anderson TJ, et al. Common carotid intima-media thickness measurements in cardiovascular risk prediction: a meta-analysis. JAMA : the journal of the American Medical Association. 2012;308:796–803. doi: 10.1001/jama.2012.9630. [DOI] [PubMed] [Google Scholar]
- 19.Karp I, Abrahamowicz M, Bartlett G, Pilote L. Updated risk factor values and the ability of the multivariable risk score to predict coronary heart disease. American journal of epidemiology. 2004;160:707–716. doi: 10.1093/aje/kwh258. [DOI] [PubMed] [Google Scholar]
- 20.Pencina MJ, D'Agostino RB, Larson MG, Massaro JM, Vasan RS. Predicting the 30-year risk of cardiovascular disease: the framingham heart study. Circulation. 2009;119:3078–3084. doi: 10.1161/CIRCULATIONAHA.108.816694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lloyd-Jones DM, Leip EP, Larson MG, et al. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation. 2006;113:791–798. doi: 10.1161/CIRCULATIONAHA.105.548206. [DOI] [PubMed] [Google Scholar]
- 22.Lloyd-Jones DM, Wilson PWF, Larson MG, et al. Framingham risk score and prediction of lifetime risk for coronary heart disease. The American journal of cardiology. 2004;94:20–24. doi: 10.1016/j.amjcard.2004.03.023. [DOI] [PubMed] [Google Scholar]
- 23.Friedman GD, Cutter GR, Donahue RP, et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41:1105–1116. doi: 10.1016/0895-4356(88)90080-7. [DOI] [PubMed] [Google Scholar]
- 24.27th Bethesda Conference. Matching the Intensity of Risk Factor Management with the Hazard for Coronary Disease Events. September 14–15, 1995. Journal of the American College of Cardiology. 1996;27:957–1047. [PubMed] [Google Scholar]
- 25.Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Final Report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 26.Lackland DT, Elkind MS, D'Agostino R, et al. Inclusion of Stroke in Cardiovascular Risk Prediction Instruments: A Statement for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2012;43:1998–2027. doi: 10.1161/STR.0b013e31825bcdac. [DOI] [PubMed] [Google Scholar]
- 27.Shillinglaw B, Viera AJ, Edwards T, Simpson R, Sheridan SL. Use of global coronary heart disease risk assessment in practice: a cross-sectional survey of a sample of U.S. physicians. BMC health services research. 2012;12:20. doi: 10.1186/1472-6963-12-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sheridan SL, Crespo E. Does the routine use of global coronary heart disease risk scores translate into clinical benefits or harms? A systematic review of the literature. BMC health services research. 2008;8:60. doi: 10.1186/1472-6963-8-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sheridan SL, Viera AJ, Krantz MJ, et al. The effect of giving global coronary risk information to adults: a systematic review. Archives of internal medicine. 2010;170:230–239. doi: 10.1001/archinternmed.2009.516. [DOI] [PubMed] [Google Scholar]
- 30.Redberg RF, Benjamin EJ, Bittner V, et al. AHA/ACCF 2009 performance measures for primary prevention of cardiovascular disease in adults: a report of the American College of Cardiology Foundation/American Heart Association task force on performance measures (writing committee to develop performance measures for primary prevention of cardiovascular disease): developed in collaboration with the American Academy of Family Physicians; American Association of Cardiovascular and Pulmonary Rehabilitation; and Preventive Cardiovascular Nurses Association: endorsed by the American College of Preventive Medicine, American College of Sports Medicine, and Society for Women's Health Research. Circulation. 2009;120:1296–1336. doi: 10.1161/CIRCULATIONAHA.109.192617. [DOI] [PubMed] [Google Scholar]
- 31.Aspirin for the prevention of cardiovascular disease: U.S. Preventive Services Task Force recommendation statement. Annals of internal medicine. 2009;150:396–404. doi: 10.7326/0003-4819-150-6-200903170-00008. [DOI] [PubMed] [Google Scholar]
- 32.Perk J, De Backer G, Gohlke H, et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012): The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts) * Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR) Eur Heart J. 2012;33:1635–1701. doi: 10.1093/eurheartj/ehs092. [DOI] [PubMed] [Google Scholar]
- 33.Anderson TJ, Grégoire J, Hegele RA, et al. 2012 Update of the Canadian Cardiovascular Society Guidelines for the Diagnosis and Treatment of Dyslipidemia for the Prevention of Cardiovascular Disease in the Adult. The Canadian journal of cardiology. 2013;29:151–167. doi: 10.1016/j.cjca.2012.11.032. [DOI] [PubMed] [Google Scholar]
- 34.Genest J, McPherson R, Frohlich J, et al. 2009 Canadian Cardiovascular Society/Canadian guidelines for the diagnosis and treatment of dyslipidemia and prevention of cardiovascular disease in the adult - 2009 recommendations. Can J Cardiol. 2009;25:567–579. doi: 10.1016/s0828-282x(09)70715-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Morbidity & Mortality: 2012 Chartbook on Cardiovascular, Lung, and Blood Diseases. Bethesda, MD: 2012. [Google Scholar]
- 36.Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics--2013 update: a report from the American Heart Association. Circulation. 2013;127:e6–e245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Greenland P, Knoll MD, Stamler J, et al. Major risk factors as antecedents of fatal and nonfatal coronary heart disease events. JAMA : the journal of the American Medical Association. 2003;290:891–897. doi: 10.1001/jama.290.7.891. [DOI] [PubMed] [Google Scholar]
- 38.Magnus P, Beaglehole R. The real contribution of the major risk factors to the coronary epidemics: time to end the “only-50%” myth. Archives of internal medicine. 2001;161:2657–2660. doi: 10.1001/archinte.161.22.2657. [DOI] [PubMed] [Google Scholar]
- 39.Ioannidis JP, Panagiotou OA. Comparison of effect sizes associated with biomarkers reported in highly cited individual articles and in subsequent meta-analyses. JAMA : the journal of the American Medical Association. 2011;305:2200–2210. doi: 10.1001/jama.2011.713. [DOI] [PubMed] [Google Scholar]
- 40.Hlatky MA, Greenland P, Arnett DK, et al. Criteria for evaluation of novel markers of cardiovascular risk: a scientific statement from the American Heart Association. Circulation. 2009;119:2408–2416. doi: 10.1161/CIRCULATIONAHA.109.192278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Di Angelantonio E, Sarwar N, Perry P, et al. Major lipids, apolipoproteins, and risk of vascular disease. JAMA : the journal of the American Medical Association. 2009;302:1993–2000. doi: 10.1001/jama.2009.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kodama S, Saito K, Tanaka S, et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA : the journal of the American Medical Association. 2009;301:2024–2035. doi: 10.1001/jama.2009.681. [DOI] [PubMed] [Google Scholar]
- 43.Sniderman AD, Williams K, Contois JH, et al. A meta-analysis of low-density lipoprotein cholesterol, non-high-density lipoprotein cholesterol, and apolipoprotein B as markers of cardiovascular risk. Circulation Cardiovascular quality and outcomes. 2011;4:337–345. doi: 10.1161/CIRCOUTCOMES.110.959247. [DOI] [PubMed] [Google Scholar]
- 44.Greenland P, Alpert JS, Beller GA, et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology. 2010;56:e50–e103. doi: 10.1016/j.jacc.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 45.Cavanaugh-Hussey MW, Berry JD, Lloyd-Jones DM. Who exceeds ATP-III risk thresholds? Systematic examination of the effect of varying age and risk factor levels in the ATP-III risk assessment tool. Preventive medicine. 2008;47:619–623. doi: 10.1016/j.ypmed.2008.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Marma AK, Lloyd-Jones DM. Systematic examination of the updated Framingham heart study general cardiovascular risk profile. Circulation. 2009;120:384–390. doi: 10.1161/CIRCULATIONAHA.108.835470. [DOI] [PubMed] [Google Scholar]
- 47.Berry JD, Dyer A, Carnethon M, Tian L, Greenland P, Lloyd-Jones DM. Association of traditional risk factors with cardiovascular death across 0 to 10, 10 to 20, and >20 years follow-up in men and women. The American journal of cardiology. 2008;101:89–94. doi: 10.1016/j.amjcard.2007.07.079. [DOI] [PubMed] [Google Scholar]
- 48.Håheim LL, Tonstad S, Hjermann I, Leren P, Holme I. Predictiveness of body mass index for fatal coronary heart disease in men according to length of follow-up: a 21-year prospective cohort study. Scandinavian journal of public health. 2007;35:4–10. doi: 10.1080/14034940510032293. [DOI] [PubMed] [Google Scholar]
- 49.Jousilahti P, Tuomilehto J, Rastenyte D, Vartiainen E. Headache and the risk of stroke: a prospective observational cohort study among 35,056 Finnish men and women. Archives of internal medicine. 2003;163:1058–1062. doi: 10.1001/archinte.163.9.1058. [DOI] [PubMed] [Google Scholar]
- 50.Liao Y, McGee DL, Cooper RS, Sutkowski MB. How generalizable are coronary risk prediction models? Comparison of Framingham and two national cohorts. American heart journal. 1999;137:837–845. doi: 10.1016/s0002-8703(99)70407-2. [DOI] [PubMed] [Google Scholar]
- 51.Menotti A, Lanti M. Coronary risk factors predicting early and late coronary deaths. Heart (British Cardiac Society) 2003;89:19–24. doi: 10.1136/heart.89.1.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wannamethee SG, Shaper AG, Lennon L, Morris RW. Metabolic syndrome vs Framingham Risk Score for prediction of coronary heart disease, stroke, and type 2 diabetes mellitus. Archives of internal medicine. 2005;165:2644–2650. doi: 10.1001/archinte.165.22.2644. [DOI] [PubMed] [Google Scholar]
- 53.HEALTH EPOIGFC, CHILDREN RRI, ADOLESCENTS. Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents: Summary Report. Pediatrics. 2011;128:S213–S256. doi: 10.1542/peds.2009-2107C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.MD J, DH R, CM A, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology /American Heart Association Task Force on Practice Guidelines, and The Obesity Society. Journal of the American College of Cardiology. 2013 doi: 10.1016/j.jacc.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 55.Stone N, Robinson J, AH L, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology /American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology. 2013 doi: 10.1016/j.jacc.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 56.Wilson PW, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 57.D'Agostino RB, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: The Framingham Heart Study. Circulation. 2008;117:743–753. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
- 58.Assmann G, Cullen P, Schulte H. Simple scoring scheme for calculating the risk of acute coronary events based on the 10-year follow-up of the prospective cardiovascular Münster (PROCAM) study. Circulation. 2002;105:310–315. doi: 10.1161/hc0302.102575. [DOI] [PubMed] [Google Scholar]
- 59.Hippisley-Cox J, Coupland C, Vinogradova Y, Robson J, May M, Brindle P. Derivation and validation of QRISK, a new cardiovascular disease risk score for the United Kingdom: prospective open cohort study. BMJ. 2007;335:136. doi: 10.1136/bmj.39261.471806.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ridker PM, Paynter NP, Rifai N, Gaziano JM, Cook NR. C-reactive protein and parental history improve global cardiovascular risk prediction: the Reynolds Risk Score for men. Circulation. 2008;118:2243–2251. doi: 10.1161/CIRCULATIONAHA.108.814251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ridker PM, Buring JE, Rifai N, Cook NR. Development and validation of improved algorithms for the assessment of global cardiovascular risk in women: the Reynolds Risk Score. JAMA : the journal of the American Medical Association. 2007;297:611–619. doi: 10.1001/jama.297.6.611. [DOI] [PubMed] [Google Scholar]
- 62.Conroy RM, Pyorala K, Fitzgerald AP, et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J. 2003;24:987–1003. doi: 10.1016/s0195-668x(03)00114-3. [DOI] [PubMed] [Google Scholar]
- 63.D'Agostino RB, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117:743–753. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
- 64.Patel MR, Dehmer GJ, Hirshfeld JW, Smith PK, Spertus JA. ACCF/SCAI/STS/AATS/AHA/ASNC 2009 Appropriateness Criteria for Coronary RevascularizationA Report by the American College of Cardiology Foundation Appropriateness Criteria Task Force, Society for Cardiovascular Angiography and Interventions, Society of Thoracic Surgeons, American Association for Thoracic Surgery, American Heart Association, and the American Society of Nuclear Cardiology Endorsed by the American Society of Echocardiography, the Heart Failure Society of America, and the Society of Cardiovascular Computed Tomography. Journal of the American College of Cardiology. 2009;53:530–553. doi: 10.1016/j.jacc.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 65.Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Annals of internal medicine. 2009;150:604–12. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Pencina MJ, D'Agostino RB, D'Agostino RB, Jr., Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27:157–172. doi: 10.1002/sim.2929. discussion 207–12. [DOI] [PubMed] [Google Scholar]