Abstract
Diffuse intrinsic pontine glioma (DIPG) is a brain cancer with a median survival of only 1 year. Lack of molecular characterization of this tumor impedes the development of novel therapies. Membrane protein B7-H3, aka CD276, involved in interactions with host defenses in certain cancers, has been shown to be over-expressed in the majority of malignant neuroectodermal tumors including adult high-grade glioma. Targeting B7-H3 with a monoclonal antibody has demonstrated safety and efficacy in the salvage treatment of stage IV childhood neuroblastoma, another neuroectodermal tumor. It thus stands to reason that B7-H3 might serve as a therapeutic target in DIPG. B7-H3 immunoreactivity was determined in DIPG and non-diffuse brainstem glioma specimens with immunohistochemistry. In addition, B7-H3 mRNA expression was evaluated with microarrays in another set of specimens. All of the nine (100 %) DIPG specimens were shown to be B7-H3 immunoreactive. In the non-diffuse brainstem glioma group, none of the eight WHO grade I specimens showed B7-H3 immunoreactivity and nine of the 24 WHO grade II specimens (37.5 %) showed B7-H3 immunoreactivity. The association between histological grade and B7-H3 immunoreactivity was statistically highly significant. B7-H3 mRNA expression was also significantly higher in DIPG samples than in normal brain and juvenile pilocytic astrocytoma (WHO grade I) specimens. In summary, B7-H3 is over-expressed in DIPG. Given the need for novel treatment in this disease, antibody-based immunotherapy against B7-H3 in DIPG warrants further investigation.
Keywords: Diffuse intrinsic pontine glioma, B7-H3, CD276, Immunotherapy
Introduction
Diffuse intrinsic pontine glioma (DIPG) is an extensively invasive malignancy of the brainstem. The median age of diagnosis is 7 years old. True incidence studies are lacking but it is estimated that there are 200–300 cases each year in the United States, representing 10–15 % of pediatric brain tumors. These tumors are lethal, with a median survival of only 10–12 months. The tumor’s location and diffusely infiltrative nature preclude surgical resection. Palliative external beam radiation therapy is the current standard of care.
Molecular profiling of brain tumors is important in understanding tumorigenesis, prognosis and therapeutic response and in developing effective therapies. Since the Children’s Cancer Group’s report in 1993 [1], the diagnosis of DIPG has been based on “typical” clinical and magnetic resonance imaging (MRI) findings and biopsy is rarely performed, resulting in the lack of tumor tissue. This limits the molecular characterization of DIPG, and in return hinders the screening of existing drugs and compounds as well as the development of new drugs. This shortcoming is even more significant given the dismal prognosis of this disease and the fact that no chemotherapy, biological therapy, new schedules of radiation therapy or combination therapies have shown any meaningful survival benefit [2].
B7-H3, also referred to as CD276, is a type I transmembrane glycoprotein that is part of the B7-CD28 family [3]. There is no consensus on its biological functions. It is the antigen recognized by monoclonal antibody 8H9 [4], which binds to the majority of tested neuroepithelial tumors but not normal neurons or glia [5]. This cell selectivity makes B7-H3 a therapeutic target in these tumors. Encouraged by the good safety and efficacy results in the salvage therapy of stage IV neuroblastoma using intrathecal 131I-8H9 in children [6], we studied B7-H3 expression at protein and mRNA levels in brainstem glioma specimens with the aim of determining its potential as a therapeutic target.
Materials and methods
Patients and specimens
The immunohistochemistry study was approved by the Ethics Committee of The Hospital for Sick Children (Toronto, ON, Canada). Specimens from two groups of patients were selected for analysis: DIPG group and non-diffuse brainstem glioma group. DIPG group included specimens obtained at autopsy from nine patients who presented to the hospital between 2000 and 2007 satisfying the following criteria: (1) At least two of the triad for clinical diagnosis of DIPG: ataxia, long tract signs and cranial nerve deficits; (2) Diffuse enlargement of the pons on MRI studies with involvement of no less than 50 % of the pons on T2-weighted images and no primary exophytic component; and (3) WHO II or higher grade glioma on histopathology. The non-diffuse brainstem glioma group consisted of specimens obtained at biopsy from 32 patients who presented to The Hospital for Sick Children between 1985 and 2001. The diagnoses of these focal, tectal, dorsal exophytic and crevicomedullary tumors were established by clinical presentations and computed tomography (CT) or MRI imaging. Only patients exhibiting glioma on histopathology were included in the analysis.
The expression microarray analysis was conducted with approval from the Institutional Review Board of University of Colorado College of Medicine (Denver, CO, USA). Specimens were obtained from patients who presented between 1997 and 2011 to Children’s Hospital Colorado (Aurora, CO, USA) or the University of Colorado Hospital (Denver, CO, USA). This part of the study consisted of five DIPG, nine juvenile pilocytic astrocytoma (JPA) and 14 normal brain specimens. DIPG samples were obtained through biopsy, JPA samples at the time of surgical resection and normal brain samples at autopsy. Samples were snap-frozen in liquid nitrogen at collection.
Immunohistochemistry
A known B7-H3-positive glioblastoma multiforme (GBM) specimen was used as a positive control and a known B7-H3-negative normal muscle specimen as a negative control. Formalin-fixed paraffin-embedded specimens were deparaffinized and rehydrated in a standard xylene and ethanol solution sequence. Heat-induced epitope recovery was performed in 0.01 M citrate buffer (pH 6.0) for 22 min. The slides were blocked in 0.3 % H2O2 in methanol for 30 min, then with the Avidin/Biotin Blocking Kit (Vector Laboratories, Burlingame, CA, USA), and followed by 2 % horse serum (Jackson ImmunoResearch, West Grove, PA, USA) in phosphate buffered saline (PBS, pH 7.4) for 20 min. The sections were incubated overnight at 4 °C in a biotinylated anti-B7-H3 antibody (Cat # BAF1027, R&D Systems, Minneapolis, MN, USA) diluted at 1 μg/ml, and then processed with the Vectastain ABC Kit (Vector Laboratories). They were then incubated in DAB peroxidase substrate solution (Vector Laboratories) for 20 min and counterstained with Mayer’s hematoxylin (Sigma-Aldrich Canada, Oakville, ON, Canada) for 4 min. Finally, they were dehydrated in a standard ethanol solution series and cleared in xylene, and mounted with Permount (Fisher Scientific, Hanover Park, IL, USA). Slides were viewed individually by a neuropathologist (CH) and another investigator (GMI) without knowledge of the patients’ clinical diagnosis and outcome. Staining was graded as positive if both viewers confirmed any immunoreactivity was seen, with staining intensity, percentage of positively stained cells and distribution patterns of staining noted.
Gene expression microarray analysis
RNA was extracted from each snap-frozen sample using an RNeasy kit (QIAGEN, Germantown, MD, USA). Five micrograms of RNA from each sample was reverse transcribed using a T7-(dT) 24-oligomer and Superscript II reverse transcriptase (Invitrogen, Grand Island, NY, USA). The resulting cDNA was converted to cRNA, fragmented and biotin-labeled using the BioArray HighYield RNA transcript labeling kit (Enzo Life Sciences, Farmingdale, NY, USA) before being hybridized to Affymetrix Gene-Chip Human Genome U133 Plus 2.0 arrays (Affymetrix Inc., Santa Clara, CA, USA). Analysis of microarray data was performed using Bioconductor [7] in the R statistical computing environment [8]. Raw data were background adjusted, normalized and summarized using the GCRMA algorithm [9], resulting in expression data expressed in log2 values. The Affymetrix HGU133 Plus 2.0 microarray contains 54,675 probesets, with some genes represented by multiple probesets. The genes with multiple probesets were handled by generating a filtered list containing a single probeset for each gene that possessed the highest GCRMA expression levels across all samples.
Statistical analysis
The percentage of cells stained positive for B7-H3 was evaluated as a continuous variable and summarized as four categories (none, <10, 10–50 and >50 %). Staining intensity was evaluated as a categorical variable (none, moderate and strong). Comparison of B7-H3 positive staining rates/percentage of positive cells/staining intensity across pathological diagnosis groups was achieved by summarizing the immunohistochemistry specimens into three groups (WHO grade I, WHO grade II and high grade) followed by evaluating using Fisher’s exact test [10, 11]. Comparison between B7-H3 staining and overall survival was evaluated by fitting stratified Cox proportional hazards models. Comparison of B7-H3 mRNA expression levels across diagnosis groups was conducted using analysis of variance (ANOVA) and false discovery rate (FDR) [12] was calculated based on the number of probesets on the microarray chip. Analyses were performed in the R statistical computing environment [8]. P values <0.05 were considered statistically significant, and those <0.01 highly significant.
In the reading of the immunohistochemistry study, weighted kappa-statistic [13] was used to quantify agreement along the categorical scale between the two viewers. The two viewers agreed on the reactive versus non-reactive reading for all the DIPG and non-diffuse brainstem glioma samples. The weighted kappa value for the percentage of B7-H3-positive cells was 0.61, which was classified as “substantial inter-rater agreement;” and for B7-H3-staining intensity was 0.73, which was also classified as “substantial inter-rater agreement.”
Results
Immunohistochemistry evaluation
The nine patients in the DIPG group included six males and three females. Age at diagnosis ranged from 1.7 to 10.6 years old with a median of 6.5 years. None of the patients had known or suspected neurofibromatosis. All patients had received external beam radiation therapy. Histopathology showed seven WHO grade IV gliomas and two high-grade (WHO grade III/IV) gliomas. Overall survivals of seven patients were available and ranged from 0.55 to 4.92 years with a median of 1.00 year. The summary is shown in Table 1.
Table 1.
Summary of B7-H3 immunoreactivity in diffuse intrinsic pontine glioma
| Study no. | Gender | Age at diagnosis (year) | WHO grade | Overall survival (year) | Percentage of positive cellsa | Staining intensityb |
|---|---|---|---|---|---|---|
| DIPG03 | M | 4.63 | IV | 1.47 | ++ | ++ |
| DIPG04 | M | 10.64 | IV | 0.69 | + | ++ |
| DIPG05 | F | 8.90 | IV | 1.00 | + | ++ |
| DIPG06 | F | 8.93 | IV | 1.40 | ++ | ++ |
| DIPG07 | M | 4.98 | IV | 0.55 | + | + |
| DIPG08 | F | 5.83 | III/IV | 0.85 | ++ | ++ |
| DIPG09 | M | 6.52 | III/IV | 4.92 | +++ | ++ |
| DIPG10 | M | 7.60 | IV | ND | ++ | ++ |
| DIPG11 | M | 1.70 | IV | ND | ++ | ++ |
ND no data
+ <10 %, ++ 10–50 %, +++ >50 %
+ moderate, ++ strong
The non-diffuse brainstem glioma group consisted of specimens from 32 patients, including 19 males and 10 females, and the other three patients’ gender information was missing. Age at diagnosis was available for 23 patients ranging from 1.2 to 17.6 years old with a median of 12.0 years. This group included five ganglioglioma (WHO grade I), three pilocytic astrocytoma (WHO grade I), one gemistocytic astrocytoma (WHO grade II) and 23 fibrillary astrocytoma (WHO grade II).
All nine DIPG specimens showed B7-H3 immunoreactivity. Of these, three showed immunoreactivity in no more than 10 % of cells, five in 10–50 % of cells, and one in more than 50 % of cells. On staining intensity, only one showed moderate intensity; all the other specimens showed strong intensity. Patient-specific information is summarized in Table 1.
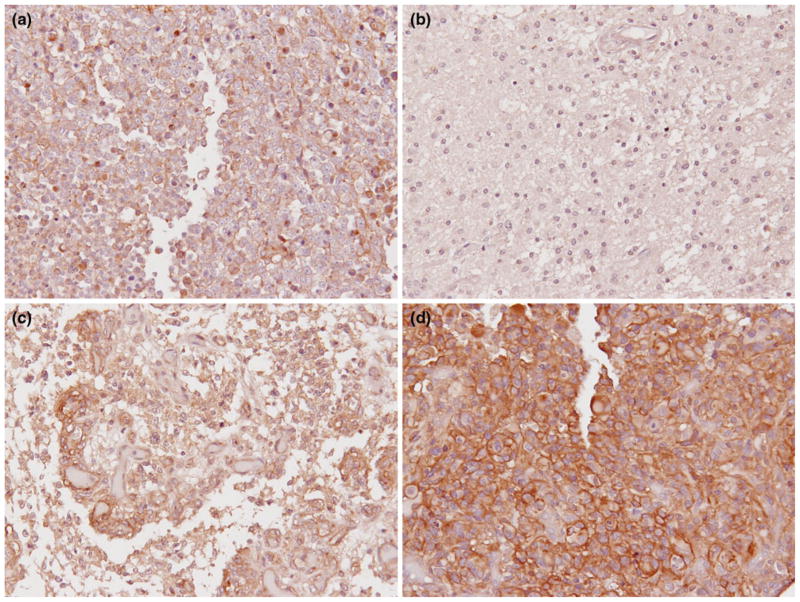
In the majority of the cases, staining was in a diffuse membranous pattern and positive cells were about evenly distributed throughout the sections. However, in two cases, staining was stronger in the vascular structures than in glioma cells while the staining of the vascular structures was punctate (Fig. 1c). One of these two had 10–50 % and the other over 50 % tumor cells showing B7-H3 immunoreactivity. Both had more than 50 % of the vascular structures stained positive. In both specimens, staining intensity for both tumor cells and vascular structures was classified as strong. Tumor cells stained positive in these two cases were also evenly distributed throughout the slides.
Fig. 1.
Representative B7-H3 immunohistochemistry of brainstem gliomas. a A DIPG sample shows positive immunoreactivity to an anti-B7-H3 antibody. The staining pattern is diffuse membrane-bound with more than 50 % of cells stained positive. b A pilocytic astrocytoma sample does not show immunoreactivity to the anti-B7-H3 antibody. c A B7-H3-positive DIPG specimen shows stronger staining on vascular structures than on tumor cells. Staining of tumor cells is diffuse membrane-bound while staining of vascular structures is punctate. Over 50 % of both tumor cells and vascular structures show B7-H3 immunoreactivity. d An adult GBM sample, which serves as the positive control, shows intensive immunoreactivity to the anti-B7-H3 antibody. The staining pattern is diffuse membrane-bound. All images were captured with ×20 objective magnification (×200 total magnification)
Of the 32 non-diffuse brainstem glioma specimens, nine (28 %) were stained positive for B7-H3. None of the eight grade I gliomas was stained positive and all of the positive staining occurred in the 24 grade II gliomas. The positive rate of grade II non-diffuse brainstem gliomas was 37.5 %. The staining intensity of all the 9 positive specimens was moderate. The percentage of cells stained positive was <10 % in 8 of the 9 positive specimens. In the other specimen, staining was predominately on the vascular structures similar to but weaker than in the two DIPG specimens with stronger vascular staining, with <10 % tumor cells positive and 10–50 % of the vascular structures positive. Tumor cells stained positive in this group were evenly distributed throughout the slides, as in the case of the DIPG group. The summary is shown in Table 2.
Table 2.
Summary of B7-H3 immunoreactivity in non-diffuse brainstem gliomas
| Pathology | Number of patients | Positive |
|---|---|---|
| Ganglioglioma (WHO I) | 5 | 0 |
| Pilocytic astrocytoma (WHO I) | 3 | 0 |
| Gemistocytic astrocytoma (WHO II) | 1 | 1 |
| Fibrillary astrocytoma (WHO II) | 23 | 8 |
| Total | 32 | 9 |
The associations between B7-H3 positive rates/percentage of positively stained cells/staining intensity and histological grades are all statistically highly significant (p = 1.59E–05, 2.64E–06 and 3.09E–08, respectively). In the DIPG group, neither the percentage of positive cells nor the intensity of B7-H3 immunoreactivity correlated with the patient’s overall survival (p > 0.05 for both).
Expression microarray evaluation
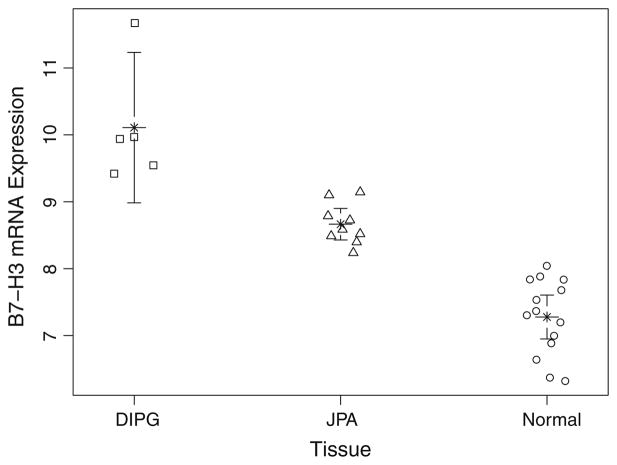
A group of DIPG samples (n = 5) were available for expression microarray analysis at Children’s Hospital Colorado and the University of Colorado Hospital. Age of patients in this group at diagnosis ranged from 3.5 to 9.0 years old. All samples had high-grade pathology (WHO grades III and IV). Comparison was made to RNA expression levels in normal brain (n = 14, ages 4.0–14.0 years) and JPA (n = 9, ages 3.0–12.0 years) samples from pediatric patients. The expression values of B7-H3 mRNA in each of these three groups have a narrow range. B7-H3 mRNA expression in DIPGs is considerably higher than in normal brain tissue and JPA. The difference in B7-H3 mRNA expression levels across diagnosis groups is statistically highly significant (p = 2.39E–09, FDR = 1.31E–04) (Fig. 2).
Fig. 2.
Microarray analysis of B7-H3 mRNA expression in brainstem gliomas. B7-H3 mRNA expression is significantly higher in DIPG compared with those in JPA and normal brain tissues. Center star indicates the group mean and error bars the 95 % confidence interval
Discussion
The pathology of DIPG is not well understood partly because of its low incidence and low biopsy and autopsy rates. From the available surgical specimens obtained prior to radiation therapy, about 70–90 % of DIPG are anaplastic astrocytoma (WHO grade III) and GBM (WHO grade IV). More grade III tumors were reported than grade IV in the HIT-GBM protocols [14, 15] while earlier reports from other groups had more grade IV than grade III [16, 17]. At late stage of the disease or autopsy, the vast majority of DIPG is high grade and have dissemination within the neuraxis [18].
DIPG is a disease entity distinct from both adult and pediatric supratentorial high-grade gliomas (HGG) and is in desperate need of novel therapeutic approaches. The median survival is about 1 year despite numerous investigations of new schedules of radiation, chemotherapy and their combinations [2]. Cancer genetics provides valuable guidance to the development of novel therapies. However, the low incidence and low biopsy and autopsy rates have lead to a lack of available specimens and a resultant underdeveloped molecular characterization of DIPG.
Despite the paucity of tumor specimens, efforts have been made to characterize DIPG molecularly. Limited but recent genetic evidence supports that DIPG is genetically complex and distinct from both adult and pediatric supra-tentorial HGG. Recent evidence points to platelet-derived growth factor and its receptors as among the major driving forces of tumorigenesis in the majority of cases [19–23]. Another growth factor receptor, epidermal growth factor receptor, shows strong immunohistochemistry staining in about 27 % of cases [20], and amplification of the gene at a rate of 7–9 % [20, 22]. Unlike the case in pediatric supratentorial HGG, CDKN2A deletion is non-existent in DIPG [22, 24]. Amplification of CDK4 and CDK6 in DIPG occurs at a rate of 7 and 11.6 %, respectively [22]. Approximately 50 % of DIPG have p53 mutation [25, 26], and loss of a region of 17p containing the p53 gene was reported in 30–65 % of cases [20, 24, 27]. In approximately 50 % of DIPG patients, allelic loss of a region of 10q where the PTEN gene is located was observed [27–28].
B7-H3 is a membrane glycoprotein discovered in 2001 [3]. The predominantly expressed isoform in human is 4Ig-B7-H3 [29, 30] containing tandem duplicate of immunoglobulin-like IgV-IgC domains. The other isoform expressed in human is 2Ig-B7-H3 [29, 30], without duplication of the extracellular IgV-IgC domains. The biological functions of B7-H3 in cancer are not well understood. The largest clinical relevance study so far showed that B7-H3 exhibits complex and predominately inhibitory interactions with host T cells in prostate cancer patients, and is thought to potentially play a role in promoting tumor invasion and/or metastasis [31]. In this prostate cancer study, 93 % of tumors were stained positive and the median percentage of positively stained cells was 80 %, and aberrant expression correlated with tumor recurrence and death [31]. Similar immunohistochemistry findings and clinical relevance have been reported in colon [32], pancreatic [33], renal cell cancers [34], ovarian carcinomas [35] and urothelial cell carcinoma of the bladder [36]. In contrast to these studies, in our limited cohort of DIPG specimens, the majority had fewer than 50 % of cells stained positive, and no correlation can be made between overall survival and percentage of positively stained cells or staining intensity, which may be a result of the small size of the study. Previous investigations demonstrated that HGG, including glioblastoma, are more frequently immunoreactive to 8H9, the monoclonal antibody that recognizes B7-H3 [4], than low-grade gliomas [5]. In the current study, the correlation between positive staining rate and grade of malignancy remains.
A predominantly vascular staining pattern, as seen in a small number in this series, has also been described in clear cell renal cell cancer [34] and ovarian carcinoma [35], and was associated with poor prognosis in both studies. This invites the question what role B7-H3 plays in tumor angiogenesis. It is noteworthy that a correlation at the mRNA level between B7-H3 and such signals as vascular endothelial growth factor (VEGF), matrix metalloproteinases and prostaglandin-endoperoxide synthases, has been reported in colorectal tumors [37]. These signals have been shown to play vital roles in tumor angiogenesis [38–41], suggesting that B7-H3 may also be involved in the process. Further supporting this notion is that the absence of intratumoral T cells has been associated with poor outcome and increased levels of VEGF in ovarian carcinoma [42], considering that B7-H3 exerts predominately inhibitory effects on T cells in cancer [31]. However, it is unclear what the causal links are between B7-H3 and the known proangiogenesis signals.
In the current series of brainstem gliomas for immunohistochemistry studies, all of the DIPG specimens were acquired by autopsy, whereas non-diffuse brainstem glioma specimens by biopsy. One might argue that the small size of biopsy specimens lowers the probability of B7-H3 detection. However, positive cells were about evenly distributed throughout the sections, suggesting that even small samples of these tumors may be sufficient to identify B7-H3 immunoreactivity. Another important difference between the two groups is that unlike non-diffuse biopsy specimens, DIPG autopsy specimens were from tumors that were previously irradiated and at a much later stage. Irradiation is unlikely the cause of the differential expression of B7-H3 antigen between DIPG and non-diffuse brainstem gliomas since significant elevation of B7-H3 was also observed at the mRNA level from biopsy specimens in the microarray study. In other tumor types, the expression of B7-H3 has not been linked to radiation exposure either [5, 31, 33].
B7-H3 was identified as a therapeutic target for neuroectodermal tumors as a result of the pre-clinical and clinical studies in various central nervous system (CNS) tumors of 8H9, a monoclonal antibody that targets this protein [4] and binds to the majority of tested neuroepithelial tumors but not normal neurons or glia [5]. B7-H3 can be targeted with therapeutic antibodies, e.g., 8H9. Binding of antibodies to membrane proteins induces antibody-induced cytotoxicity, through multiple mechanisms including antibody-dependent cellular cytotoxicity [43, 44] and complement-dependent cytotoxicity [45]. Such antibodies can also be used as the targeting moiety in recombinant toxin design. Such therapeutic molecules as monoclonal antibodies and recombinant toxins would be best delivered into the tumor using a local delivery method, such as convection-enhanced delivery (CED), due to their inability to cross the blood–brain barrier. Where only a subset of tumor cells express B7-H3 such as the case in DIPG in this study, B7-H3 can also serve as an anchor to target nearby tumor cells not expressing this antigen in addition to B7-H3-expressing cells by such ways as conjugating the antibody with a radioisotope. The labeled antibody will bind to those cells that express the antigen. Radiation from the conjugated radioisotope will reach a short distance (e.g., positrons from iodine-124 has an average range of 1.15 mm in soft tissues [46]). Cancer cells, with higher proliferative activity, will theoretically be killed preferentially over normal cells by the radiation released from the radioisotope. An anti-B7-H3 monoclonal antibody, MJ18, produced good results in a pancreatic cancer model [33]. Neutralization of 4Ig-B7-H3 by monoclonal antibody 5B14 enhanced lysis of neuroblastoma cells by natural killer cells [47]. 8H9 and 8H9(Fv)-PE38, a chimeric toxin utilizing 8H9 as the targeting moiety, can be safely delivered into normal brains and glioma xenografts in rats via CED [48, 49]. 8H9(Fv)-PE38 prolonged the survival of tumor-bearing animals [49]. 8H9(Fv)-PE38 has also shown good efficacy in breast cancer, osteosarcoma and neuroblastoma models [50]. Clinically, intrathecal 131I-8H9 has shown good safety and efficacy results in the salvage therapy in patients with CNS-metastatic neuroblastoma [6]. Fifteen of the 18 patients receiving 131I-8H9 salvage therapy were alive 7–74 months (median 28 months) since CNS relapse, with all 15 remaining free of CNS neuroblastoma. Two of the other three patients died from non-CNS events. Only one progressed in the CNS 14 months and died 35 months after the initial CNS event. This is a considerable improvement over results from the same institution where CNS-metastatic neuroblastoma patients had a median time to death of 6.6 months before this clinical trial.
The current report, along with the encouraging results of pre-clinical and clinical studies targeting B7-H3, supports the use of B7-H3-directed therapies in DIPG. Obviously, the biggest limitation of this study is the small number of DIPG samples. It would be desirable and ideal to have a larger study in the future, where expression levels of B7-H3 are studied at both the mRNA and protein levels in the same samples, potentially with a component to determine whether the gene is amplified and mutated, which could be able to give better insights to the regulation and clinical relevance of B7-H3 expression in brainstem gliomas.
Conclusion
Our study shows that B7-H3 is over-expressed in DIPG and the rates of B7-H3 expression are associated with malignancy grade in brainstem gliomas. B7-H3 can be utilized as a therapeutic target in DIPG given its tumor selectivity and the availability of a therapeutic monoclonal antibody, i.e., 8H9.
Acknowledgments
This study was supported in part by grants from the Beez Foundation (to ZZ and MMS), the Cristian Rivera Foundation (to MMS), the Matthew Larson Foundation (to ZZ) and the St. Baldrick’s Foundation (to MMS).
Contributor Information
Zhiping Zhou, Email: zhz2004@med.cornell.edu, Department of Neurological Surgery, Weill Medical College of Cornell University, 1300 York Ave, Box 99, New York, NY 10065, USA.
Neal Luther, Department of Neurological Surgery, Weill Medical College of Cornell University, 1300 York Ave, Box 99, New York, NY 10065, USA.
George M. Ibrahim, Department of Neurosurgery, The Hospital for Sick Children, Toronto, ON, Canada
Cynthia Hawkins, Department of Pathology, The Hospital for Sick Children, Toronto, ON, Canada.
Rajeev Vibhakar, Department of Pediatrics, University of Colorado School of Medicine, Denver, CO, USA. Department of Pediatrics, Children’s Hospital Colorado, Aurora, CO, USA.
Michael H. Handler, Department of Neurological Surgery, University of Colorado School of Medicine, Denver, CO, USA. Department of Neurosurgery, Children’s Hospital Colorado, Aurora, CO, USA
Mark M. Souweidane, Department of Neurological Surgery, Weill Medical College of Cornell University, 1300 York Ave, Box 99, New York, NY 10065, USA. Department of Pediatrics, Weill Medical College of Cornell University, New York, NY, USA. Department of Neurosurgery, Memorial Sloan-Kettering Cancer Center, New York, NY, USA
References
- 1.Albright AL, Packer RJ, Zimmerman R, Rorke LB, Boyett J, Hammond GD. Magnetic resonance scans should replace biopsies for the diagnosis of diffuse brain stem gliomas: a report from the Children’s Cancer Group. Neurosurgery. 1993;33:1026–1029. doi: 10.1227/00006123-199312000-00010. discussion 1029–1030. [DOI] [PubMed] [Google Scholar]
- 2.Hargrave D, Bartels U, Bouffet E. Diffuse brainstem glioma in children: critical review of clinical trials. Lancet Oncol. 2006;7:241–248. doi: 10.1016/S1470-2045(06)70615-5. [DOI] [PubMed] [Google Scholar]
- 3.Chapoval AI, Ni J, Lau JS, Wilcox RA, Flies DB, Liu D, Dong H, Sica GL, Zhu G, Tamada K, Chen L. B7–H3: a costimulatory molecule for T cell activation and IFN-gamma production. Nat Immunol. 2001;2:269–274. doi: 10.1038/85339. [DOI] [PubMed] [Google Scholar]
- 4.Xu H, Cheung IY, Guo HF, Cheung NK. MicroRNA miR-29 modulates expression of immunoinhibitory molecule B7-H3: potential implications for immune based therapy of human solid tumors. Cancer Res. 2009;69:6275–6281. doi: 10.1158/0008-5472.CAN-08-4517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Modak S, Kramer K, Gultekin SH, Guo HF, Cheung NK. Monoclonal antibody 8H9 targets a novel cell surface antigen expressed by a wide spectrum of human solid tumors. Cancer Res. 2001;61:4048–4054. [PubMed] [Google Scholar]
- 6.Kramer K, Kushner BH, Modak S, Pandit-Taskar N, Smith-Jones P, Zanzonico P, Humm JL, Xu H, Wolden SL, Souweidane MM, Larson SM, Cheung NK. Compartmental intrathecal radioimmunotherapy: results for treatment for metastatic CNS neuroblastoma. J Neurooncol. 2010;97:409–418. doi: 10.1007/s11060-009-0038-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gentleman RC, Carey VJ, Bates DM, Bolstad B, Dettling M, Dudoit S, Ellis B, Gautier L, Ge Y, Gentry J, Hornik K, Hothorn T, Huber W, Iacus S, Irizarry R, Leisch F, Li C, Maechler M, Rossini AJ, Sawitzki G, Smith C, Smyth G, Tierney L, Yang JY, Zhang J. Bioconductor: open software development for computational biology and bioinformatics. Genome Biol. 2004;5:R80. doi: 10.1186/gb-2004-5-10-r80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ihaka R, Gentleman R. R: a language for data analysis and graphics. J Comput Graph Stat. 1996;5:299–314. [Google Scholar]
- 9.Wu Z, Irizarry RA, Gentleman R, Martinez-Murillo F, Spencer F. A model-based background adjustment for oligonucleotide expression arrays. J Am Stat Assoc. 2004;99:909–917. [Google Scholar]
- 10.Mehta CR, Patel NR. ALGORITHM 643: FEXACT: a FORTRAN subroutine for Fisher’s exact test on unordered r × c contingency tables. ACM Trans Math Softw. 1986;12:154–161. [Google Scholar]
- 11.Clarkson DB, Fan Y-a, Joe H. A remark on algorithm 643: FEXACT: an algorithm for performing Fisher’s exact test in r × c contingency tables. ACM Trans Math Softw. 1993;19:484–488. [Google Scholar]
- 12.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc. 1995;57:289–300. [Google Scholar]
- 13.Cohen J. Weighted kappa: nominal scale agreement with provision for scaled disagreement or partial credit. Psychol Bull. 1968;70:213–220. doi: 10.1037/h0026256. [DOI] [PubMed] [Google Scholar]
- 14.Wolff JE, Classen CF, Wagner S, Kortmann RD, Palla SL, Pietsch T, Kuhl J, Gnekow A, Kramm CM. Subpopulations of malignant gliomas in pediatric patients: analysis of the HIT-GBM database. J Neurooncol. 2008;87:155–164. doi: 10.1007/s11060-007-9495-z. [DOI] [PubMed] [Google Scholar]
- 15.Wolff JE, Driever PH, Erdlenbruch B, Kortmann RD, Rutkowski S, Pietsch T, Parker C, Metz MW, Gnekow A, Kramm CM. Intensive chemotherapy improves survival in pediatric high-grade glioma after gross total resection: results of the HIT-GBM-C protocol. Cancer. 2010;116:705–712. doi: 10.1002/cncr.24730. [DOI] [PubMed] [Google Scholar]
- 16.Cartmill M, Punt J. Diffuse brain stem glioma. A review of stereotactic biopsies. Childs Nerv Syst. 1999;15:235–237. doi: 10.1007/s003810050379. discussion 238. [DOI] [PubMed] [Google Scholar]
- 17.Fisher PG, Breiter SN, Carson BS, Wharam MD, Williams JA, Weingart JD, Foer DR, Goldthwaite PT, Tihan T, Burger PC. A clinicopathologic reappraisal of brain stem tumor classification. Identification of pilocystic astrocytoma and fibrillary astrocytoma as distinct entities. Cancer. 2000;89:1569–1576. doi: 10.1002/1097-0142(20001001)89:7<1569::aid-cncr22>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 18.Sethi R, Allen J, Donahue B, Karajannis M, Gardner S, Wisoff J, Kunnakkat S, Mathew J, Zagzag D, Newman K, Narayana A. Prospective neuraxis MRI surveillance reveals a high risk of leptomeningeal dissemination in diffuse intrinsic pontine glioma. J Neurooncol. 2011;102:121–127. doi: 10.1007/s11060-010-0301-y. [DOI] [PubMed] [Google Scholar]
- 19.Becher OJ, Hambardzumyan D, Walker TR, Helmy K, Nazarian J, Albrecht S, Hiner RL, Gall S, Huse JT, Jabado N, MacDonald TJ, Holland EC. Preclinical evaluation of radiation and perifosine in a genetically and histologically accurate model of brainstem glioma. Cancer Res. 2010;70:2548–2557. doi: 10.1158/0008-5472.CAN-09-2503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zarghooni M, Bartels U, Lee E, Buczkowicz P, Morrison A, Huang A, Bouffet E, Hawkins C. Whole-genome profiling of pediatric diffuse intrinsic pontine gliomas highlights platelet-derived growth factor receptor alpha and poly (ADP-ribose) polymerase as potential therapeutic targets. J Clin Oncol. 2010;28:1337–1344. doi: 10.1200/JCO.2009.25.5463. [DOI] [PubMed] [Google Scholar]
- 21.Puget S, Philippe C, Bax DA, Job B, Varlet P, Junier MP, Andreiuolo F, Carvalho D, Reis R, Guerrini-Rousseau L, Roujeau T, Dessen P, Richon C, Lazar V, Le Teuff G, Sainte-Rose C, Geoerger B, Vassal G, Jones C, Grill J. Mesenchymal transition and PDGFRA amplification/mutation are key distinct oncogenic events in pediatric diffuse intrinsic pontine gliomas. PLoS ONE. 2012;7:e30313. doi: 10.1371/journal.pone.0030313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Paugh BS, Broniscer A, Qu C, Miller CP, Zhang J, Tatevossian RG, Olson JM, Geyer JR, Chi SN, da Silva NS, Onar-Thomas A, Baker JN, Gajjar A, Ellison DW, Baker SJ. Genome-wide analyses identify recurrent amplifications of receptor tyrosine kinases and cell-cycle regulatory genes in diffuse intrinsic pontine glioma. J Clin Oncol. 2011;29:3999–4006. doi: 10.1200/JCO.2011.35.5677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Paugh BS, Qu C, Jones C, Liu Z, Adamowicz-Brice M, Zhang J, Bax DA, Coyle B, Barrow J, Hargrave D, Lowe J, Gajjar A, Zhao W, Broniscer A, Ellison DW, Grundy RG, Baker SJ. Integrated molecular genetic profiling of pediatric high-grade gliomas reveals key differences with the adult disease. J Clin Oncol. 2010;28:3061–3068. doi: 10.1200/JCO.2009.26.7252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barrow J, Adamowicz-Brice M, Cartmill M, MacArthur D, Lowe J, Robson K, Brundler MA, Walker DA, Coyle B, Grundy R. Homozygous loss of ADAM3A revealed by genome-wide analysis of pediatric high-grade glioma and diffuse intrinsic pontine gliomas. Neuro Oncol. 2011;13:212–222. doi: 10.1093/neuonc/noq158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Badhe PB, Chauhan PP, Mehta NK. Brainstem gliomas–a clinicopathological study of 45 cases with p53 immunohistochemistry. Indian J Cancer. 2004;41:170–174. [PubMed] [Google Scholar]
- 26.Zhang S, Feng X, Koga H, Ichikawa T, Abe S, Kumanishi T. p53 gene mutations in pontine gliomas of juvenile onset. Biochem Biophys Res Commun. 1993;196:851–857. doi: 10.1006/bbrc.1993.2327. [DOI] [PubMed] [Google Scholar]
- 27.Louis DN, Rubio MP, Correa KM, Gusella JF, von Deimling A. Molecular genetics of pediatric brain stem gliomas. Application of PCR techniques to small and archival brain tumor specimens. J Neuropathol Exp Neurol. 1993;52:507–515. doi: 10.1097/00005072-199309000-00009. [DOI] [PubMed] [Google Scholar]
- 28.Cheng Y, Ng HK, Zhang SF, Ding M, Pang JC, Zheng J, Poon WS. Genetic alterations in pediatric high-grade astrocytomas. Hum Pathol. 1999;30:1284–1290. doi: 10.1016/s0046-8177(99)90057-6. [DOI] [PubMed] [Google Scholar]
- 29.Ling V, Wu PW, Spaulding V, Kieleczawa J, Luxenberg D, Carreno BM, Collins M. Duplication of primate and rodent B7–H3 immunoglobulin V- and C-like domains: divergent history of functional redundancy and exon loss. Genomics. 2003;82:365–377. doi: 10.1016/s0888-7543(03)00126-5. [DOI] [PubMed] [Google Scholar]
- 30.Sun M, Richards S, Prasad DV, Mai XM, Rudensky A, Dong C. Characterization of mouse and human B7–H3 genes. J Immunol. 2002;168:6294–6297. doi: 10.4049/jimmunol.168.12.6294. [DOI] [PubMed] [Google Scholar]
- 31.Zang X, Thompson RH, Al-Ahmadie HA, Serio AM, Reuter VE, Eastham JA, Scardino PT, Sharma P, Allison JP. B7–H3 and B7x are highly expressed in human prostate cancer and associated with disease spread and poor outcome. Proc Natl Acad Sci USA. 2007;104:19458–19463. doi: 10.1073/pnas.0709802104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee H, Kim JH, Yang SY, Kong J, Oh M, Jeong DH, Chung JI, Bae KB, Shin JY, Hong KH, Choi I. Peripheral blood gene expression of B7 and CD28 family members associated with tumor progression and microscopic lymphovascular invasion in colon cancer patients. J Cancer Res Clin Oncol. 2010;136:1445–1452. doi: 10.1007/s00432-010-0800-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yamato I, Sho M, Nomi T, Akahori T, Shimada K, Hotta K, Kanehiro H, Konishi N, Yagita H, Nakajima Y. Clinical importance of B7–H3 expression in human pancreatic cancer. Br J Cancer. 2009;101:1709–1716. doi: 10.1038/sj.bjc.6605375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Crispen PL, Sheinin Y, Roth TJ, Lohse CM, Kuntz SM, Frigola X, Thompson RH, Boorjian SA, Dong H, Leibovich BC, Blute ML, Kwon ED. Tumor cell and tumor vasculature expression of B7–H3 predict survival in clear cell renal cell carcinoma. Clin Cancer Res. 2008;14:5150–5157. doi: 10.1158/1078-0432.CCR-08-0536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zang X, Sullivan PS, Soslow RA, Waitz R, Reuter VE, Wilton A, Thaler HT, Arul M, Slovin SF, Wei J, Spriggs DR, Dupont J, Allison JP. Tumor associated endothelial expression of B7–H3 predicts survival in ovarian carcinomas. Mod Pathol. 2010;23:1104–1112. doi: 10.1038/modpathol.2010.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Boorjian SA, Sheinin Y, Crispen PL, Farmer SA, Lohse CM, Kuntz SM, Leibovich BC, Kwon ED, Frank I. T-cell coregulatory molecule expression in urothelial cell carcinoma: clinicopathologic correlations and association with survival. Clin Cancer Res. 2008;14:4800–4808. doi: 10.1158/1078-0432.CCR-08-0731. [DOI] [PubMed] [Google Scholar]
- 37.Galon J, Costes A, Sanchez-Cabo F, Kirilovsky A, Mlecnik B, Lagorce-Pages C, Tosolini M, Camus M, Berger A, Wind P, Zinzindohoue F, Bruneval P, Cugnenc PH, Trajanoski Z, Fridman WH, Pages F. Type, density, and location of immune cells within human colorectal tumors predict clinical outcome. Science. 2006;313:1960–1964. doi: 10.1126/science.1129139. [DOI] [PubMed] [Google Scholar]
- 38.Handsley MM, Edwards DR. Metalloproteinases and their inhibitors in tumor angiogenesis. Int J Cancer. 2005;115:849–860. doi: 10.1002/ijc.20945. [DOI] [PubMed] [Google Scholar]
- 39.Ferrara N. VEGF and the quest for tumour angiogenesis factors. Nat Rev Cancer. 2002;2:795–803. doi: 10.1038/nrc909. [DOI] [PubMed] [Google Scholar]
- 40.Ruoslahti E, Rajotte D. An address system in the vasculature of normal tissues and tumors. Annu Rev Immunol. 2000;18:813–827. doi: 10.1146/annurev.immunol.18.1.813. [DOI] [PubMed] [Google Scholar]
- 41.Ruoslahti E. Specialization of tumour vasculature. Nat Rev Cancer. 2002;2:83–90. doi: 10.1038/nrc724. [DOI] [PubMed] [Google Scholar]
- 42.Zhang L, Conejo-Garcia JR, Katsaros D, Gimotty PA, Massobrio M, Regnani G, Makrigiannakis A, Gray H, Schlienger K, Liebman MN, Rubin SC, Coukos G. Intratumoral T cells, recurrence, and survival in epithelial ovarian cancer. N Engl J Med. 2003;348:203–213. doi: 10.1056/NEJMoa020177. [DOI] [PubMed] [Google Scholar]
- 43.Hellstrom I, Brankovan V, Hellstrom KE. Strong antitumor activities of IgG3 antibodies to a human melanoma-associated ganglioside. Proc Natl Acad Sci USA. 1985;82:1499–1502. doi: 10.1073/pnas.82.5.1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Steplewski Z, Lubeck MD, Koprowski H. Human macrophages armed with murine immunoglobulin G2a antibodies to tumors destroy human cancer cells. Science. 1983;221:865–867. doi: 10.1126/science.6879183. [DOI] [PubMed] [Google Scholar]
- 45.Mayer P, Handgretinger R, Bruchelt G, Schaber B, Rassner G, Fierlbeck G. Activation of cellular cytotoxicity and complement-mediated lysis of melanoma and neuroblastoma cells in vitro by murine antiganglioside antibodies MB 3.6 and 14.G2a. Melanoma Res. 1994;4:101–106. doi: 10.1097/00008390-199404000-00004. [DOI] [PubMed] [Google Scholar]
- 46.Pagani M, Stone-Elander S, Larsson SA. Alternative positron emission tomography with non-conventional positron emitters: effects of their physical properties on image quality and potential clinical applications. Eur J Nucl Med. 1997;24:1301–1327. doi: 10.1007/s002590050156. [DOI] [PubMed] [Google Scholar]
- 47.Castriconi R, Dondero A, Augugliaro R, Cantoni C, Carnemolla B, Sementa AR, Negri F, Conte R, Corrias MV, Moretta L, Moretta A, Bottino C. Identification of 4Ig-B7-H3 as a neuroblastoma-associated molecule that exerts a protective role from an NK cell-mediated lysis. Proc Natl Acad Sci USA. 2004;101:12640–12645. doi: 10.1073/pnas.0405025101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Luther N, Cheung NK, Dunkel IJ, Fraser JF, Edgar MA, Gutin PH, Souweidane MM. Intraparenchymal and intratumoral interstitial infusion of antiglioma monoclonal antibody 8H9. Neurosurgery. 2008;63:1166–1174. doi: 10.1227/01.NEU.0000334052.60634.84. discussion 1174. [DOI] [PubMed] [Google Scholar]
- 49.Luther N, Cheung NK, Souliopoulos EP, Karempelas I, Bassiri D, Edgar MA, Guo HF, Pastan I, Gutin PH, Souweidane MM. Interstitial infusion of glioma-targeted recombinant immunotoxin 8H9scFv-PE38. Mol Cancer Ther. 2010;9:1039–1046. doi: 10.1158/1535-7163.MCT-09-0996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Onda M, Wang QC, Guo HF, Cheung NK, Pastan I. In vitro and in vivo cytotoxic activities of recombinant immunotoxin 8H9(Fv)-PE38 against breast cancer, osteosarcoma, and neuroblastoma. Cancer Res. 2004;64:1419–1424. doi: 10.1158/0008-5472.can-03-0570. [DOI] [PubMed] [Google Scholar]