Supplemental digital content is available in the text.
Key Words: aripiprazole, dopamine replacement therapy, gambling disorder, impulse control disorder, agonist, dopamine receptor
Background
In the last 10 years, dopamine replacement therapy (DRT) has become a well-known risk factor for developing an impulse control disorder, such as gambling disorder (GD). Another medication, aripiprazole (ARI), has been more recently identified as another risk factor. Dopamine replacement therapy and ARI share a dopamine agonist action. Our work aimed at comparing patients with PG according to their treatment with DRT or ARI.
Methods
Two methods were combined—a systematic review concentrated on case reports and the analysis of a French disordered gamblers cohort focused on patients using ARI or DRT at inclusion.
Results
We reported 48 cases of GD possibly due to DRT and 17 cases of GD possibly due to ARI. Because of their standardized assessment, only the EVALJEU patients could be compared. Two clinical patterns emerged. Patients in the ARI group were young, impulsive, and high novelty seekers and had a history of substance misuse. Their first gambling experience occurred during adolescence. Conversely, patients in the DRT group were old, and they began gambling late in life. They showed low levels of gambling-related cognition.
Conclusions
Patients in the ARI group seemed to be more severe pathological gamblers than patients in the DRT group. Aripiprazole is a partial D2 receptor agonist, whereas DRT includes full D2 receptor agonist. The trigger mechanism of PG development is complex and cannot only be attributed only to the pharmacodynamic effects of dopaminergic drugs. Indeed, individual vulnerability factors and environmental factors need to be considered.
Early detection of gambling disorder (GD) and specialized care or the problem/pathological gamblers has substantially progressed in the last 15 years. This development was made possible by better knowledge about the many predisposing, precipitating, and perpetuating risk factors that contribute to the disorder. Among them, the risk factor related to the use of dopamine receptor agonists was recently suggested.
Parkinson disease (PD), which is the most prevalent neurodegenerative disease after Alzheimer disease, maintains close and complex ties with impulse control disorders or behavioral addictions, especially GD. The prevalence of impulse control disorders in PD patients treated with dopamine replacement therapy (DRT) varied between 3.5% and 13.6%1 and that of GD between 2.3% and 8%,2 which is a significantly higher rate than that of the general population. According to many authors, GD is an adverse side effect of DRT,3 and the first cases of iatrogenic GD were reported in the early 2000s.4,5 Gambling disorder is considered to be iatrogenic based on chronological and pharmacological arguments: GD appeared after the onset of PD and DRT initiation and disappeared after discontinuing DRT; DRT acted on dopamine receptors in the nigrostriatal pathway and in the reward pathway, which plays a role in addiction. The most common medications under investigation are dopamine receptor agonists (pramipexole, ropinirole, pergolide, cabergoline, etc), but according to some authors, monotherapy with carbidopa or levodopa could also be considered.2,6–19 The risk of GD may increase if carbidopa/levodopa are associated with dopamine agonists because they cause broader stimulation of dopamine receptors.2,17,19
However, only a minority of individuals with PD develop this complication. According to the literature, it is uncertain whether this effect results from the treatment (chosen molecule, dosage used, patient [individual vulnerability factors], etc) or disease (particular clinical forms, etc). Some studies suggest that pramipexole is the dopamine receptor agonist that is most often to blame,8,10 whereas other studies state that there is no difference between the various dopamine receptor agonists.2,7,12,19 There are also contradictory results on the subject of causal associations between dosage and the occurrence of GD. A study reported a dose/effect relationship between agonists and the development of GD.20 Another study indicated that dopamine receptor agonists prescribed at the maximum authorized dose or above are at fault.2 Finally, other studies maintain that there is no association between the prescribed dose and the occurrence of GD, thus attributing the root cause to an underlying vulnerability.12,21 Some authors argue that DRT can trigger these nonmotor symptoms in PD if specific individual predisposing factors are present.22 All of these factors help illustrate the profile of PD patients who are more likely to develop this addictive disorder. Some specific characteristics have been observed, such as a young age and early onset of GD. On a personal level, they often have a higher level of sensation seeking, present greater difficulty in planning, and usually have a personal or family history of substance use disorder or impulse control disorder. On a clinical level, they often possess a history of iatrogenic (hypo)maniac episodes and are currently being treated with dopamine receptor agonists rather than dopa.1,2,14
In recent years, another medication (aripiprazole [ARI]) has received growing attention. Aripiprazole is an atypical antipsychotic drug with D2 partial agonist properties and high D2 receptor affinity. This partial agonist can reduce D2 hyperactivation in the mesolimbic pathway, thus alleviating positive symptoms of schizophrenia, but still providing enough D2 receptor stimulation in the mesocortical pathway and the nigrostriatal pathway to prevent both negative symptoms and extrapyramidal side effects.23 Little is known about the associations between ARI and impulse control disorders or behavioral addictions, and to the best of our knowledge, only a few case reports of GD that was possibly induced by ARI have been published.24–28 In the most recent case reports, other risk factors than ARI prescription were highlighted, such as regular gambling before the onset of an adverse drug reaction and a history of a mood, psychotic, or substance use disorder.28
Gambling disorder is a potential adverse drug reaction of drugs acting on dopamine receptors; however, it is a complex and multifactorial disorder. Concluding that medication is the only factor that can explain the onset of GD is simplistic and dangerous. Many other potential risk factors, including individual vulnerability factors as well as environmental factors, should be considered.29–31 Only exhaustive clinical assessment and follow-up of patients will better our understanding. Some teams specializing in addiction have developed efficient methods. In France, there is an innovative cohort of disordered gamblers seeking treatment (EVALJEU cohort), which can be used to assess the clinical and gambling characteristics of the patients in a standardized way to assist the clinician in defining the therapeutic strategy and to provide research data.
Our work aimed to provide an overview of possibly iatrogenic GD according to the patients' medication: ARI or DRT. This work was based both on a systematic review concentrated on case reports and on the analysis of a large French disordered gamblers cohort focused on patients using ARI or DRT at inclusion.
MATERIALS AND METHODS
Systematic Review
Methods
Systematic review methods were used in accordance with the PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) guidelines for conducting and reporting this systematic review.32
Search Resources
A search of 2 electronic databases was completed from inception to June 2015 (PubMed and Science Direct). The search terms were a combination of MESH terms and key words and included gambling disorder or pathological gambling or problem gambling or impulse control disorder and one of the following terms: aripiprazole, dopamine replacement therapy, cabergoline, pergolide, piribedil, pramipexole, ropinirole, levodopa, carbidopa in the title, abstract, or key words.
A manual search and screening of the bibliographies of the selected articles was performed in addition to the computerized screening. Duplicate searches were eliminated.
Eligibility Criteria
Articles had to fulfill the following criteria to be included:
The target problem was a GD (pathological gambling or problem gambling).
The medication was ARI or DRT used in PD.
The article was a case report.
Article Selection
First, all articles were screened based on their titles and abstracts. Second, the full text of all of the articles identified in this search process was read. The authors performed this work independently using the same bibliographic search. In the event of disagreement, the relevant articles were discussed.
Data Extraction
Extracted data included clinical and pharmacological considerations.
Analysis of the EVALJEU Cohort
Sample and Procedure
In 2009, our department, which specializes in GD management, constructed a cohort including any new patient starting a treatment for this particular reason with the aim of highlighting risk factors of GD initiation and persistence. The main criterion for inclusion in the EVALJEU Cohort was being a “problem gambler” (Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition [DSM-IV] criteria for pathological gambling ≥3) in the previous 12 months. The presence of at least 5 DSM-IV diagnostic criteria is required to confirm the diagnosis of pathological gambling, but the presence of 3 or 4 criteria is enough to suggest “at risk gambling” or “problem gambling.”33–35 Both pathological and problem gamblers require care, which explains the choice of the threshold of 3. The exclusion criteria included cognitive impairment and difficulties in reading and writing French. The local research ethics committee approved this study, and all subjects provided written informed consent. Based on the EVALJEU cohort, which included 166 patients, we extracted the data of patients using ARI or DRT at inclusion.
Assessment
All patients underwent a semistructured clinical interview and completed self-report questionnaires. Well-trained and experienced staff members performed this assessment. For the purpose of this specific study, we focused on gambling characteristics, comorbidities, and personality traits.
Mini International Neuropsychiatric Interview
The fifth version of this structured diagnosis interview allows for the main axis I psychiatric disorders of the DSM-IV to be explored in a quick and standardized way.36
Wender-Utah Rating Scale—Child
This self-report questionnaire is a tool that has been validated for retrospective evaluation in the adult of attention-deficit/hyperactivity disorder in childhood.37
UPPS Impulsive Behavior Scale
This is a 45-item self-questionnaire developed to measure 4 distinct pathways to impulsive behaviors: “urgency,” “(lack of) premeditation,” “(lack of) perseverance,” and “sensation seeking.”38
Temperament and Character Inventory-125
The shorter 125-item version of the Temperament and Character Inventory (TCI) is a self-report questionnaire that is used to briefly explore 4 temperament traits (novelty seeking, harm avoidance, reward dependence, and persistence) and 3 character traits (self-directedness, self-cooperation, and self-transcendence).39
Pathological Gambling Section in the DSM-IV
The inclusion in the EVALJEU cohort was achieved through an interview based on the DSM-IV 10 diagnostic criteria for pathological gambling. This categorical approach was completed using a dimensional approach by adding the number of positive DSM-IV criteria. The number of diagnostic criteria is correlated with the severity of the disorder.33
Gambling Attitudes and Beliefs Survey
The Gambling Attitudes and Beliefs Survey (GABS) is a self-rated questionnaire constructed to measure cognitive biases, irrational beliefs, positively valued attitudes toward gambling, subjective arousal, and gambling behaviors.40
Other Gambling Characteristics
In the structured interview, we were able to identify the favorite type of game for each subject. Lottery games, slot machines, scratch cards, and so on were classified under “pure chance games”; sports or horse-racing bets as well as black jack under “chance games with pseudo-skills”; and poker (including Texas hold'em poker) under “chance games with elements of skills” according to the classification proposed by Boutin.41 This interview also allowed us to define the medium that was usually used for gambling (on or off line). Finally, questions about gambling trajectory, gambling motives, perceived control over gambling, and craving were asked.
RESULTS
In regard to the patients treated with ARI, we identified 17 case reports in the literature. Among them, 8 cases were originally derived from the EVALJEU cohort28 and 9 had been published elsewhere.24–27 The clinical and pharmacological information are summarized in Supplementary Table 1, Supplemental Digital Content 1, http://links.lww.com/JCP/A349, which was previously published.28
In regard to the patients treated with DRT, we found 42 published case reports5,7,42–52 and 6 unpublished cases from the EVALJEU cohort. The 6 unpublished case reports are described in Supplementary Table 2, Supplemental Digital Content 2, http://links.lww.com/JCP/A350. The characteristics of all of these 48 cases are presented in Supplementary Table 3, Supplemental Digital Content 3, http://links.lww.com/JCP/A351.
Description of the ARI Group
Patients in the ARI group were young (mean age, 33.6 years), mostly men (88.2%) and most lived alone. Comorbid psychiatric and substance use disorders were common. Aripiprazole was prescribed in 5 of the 17 cases to treat mood disorders (major depression or bipolar disorder) and was prescribed to treat schizophrenic disorder (schizophrenia or schizoaffective disorder) in the 12 remaining cases. This psychiatric history may explain the sociodemographic characteristics. Most of the patients were regular gamblers (they gambled at least 1 time per year) before the first administration of ARI. Two patients were already problem gamblers before the first administration of ARI, but in such cases, their gambling problems became worse after the administration of ARI. The probability that PG is due to ARI is “possible” in 16 cases using the Naranjo algorithm.53
Description of the DRT Group
Patients receiving DRT were middle-aged (mean age, 55.2 years) and mostly men. For all patients, DRT was based on the association of a dopamine receptor agonist with levodopa/carbidopa. Substance use disorders were reported in a few cases. Psychiatric disorders (such as depressive symptoms) were current comorbidities in 30 of 48 cases. Some patients never gambled before PD. “Pure chance games” seemed to be the favorite type of game. The probability that GD is actually due to DRT is possible in 46 cases using the Naranjo algorithm.53
Comparison of the 2 Groups of Patients
Patients in the ARI group seemed to be younger and were more prone to have a history of psychiatric disorders and substance use disorders.
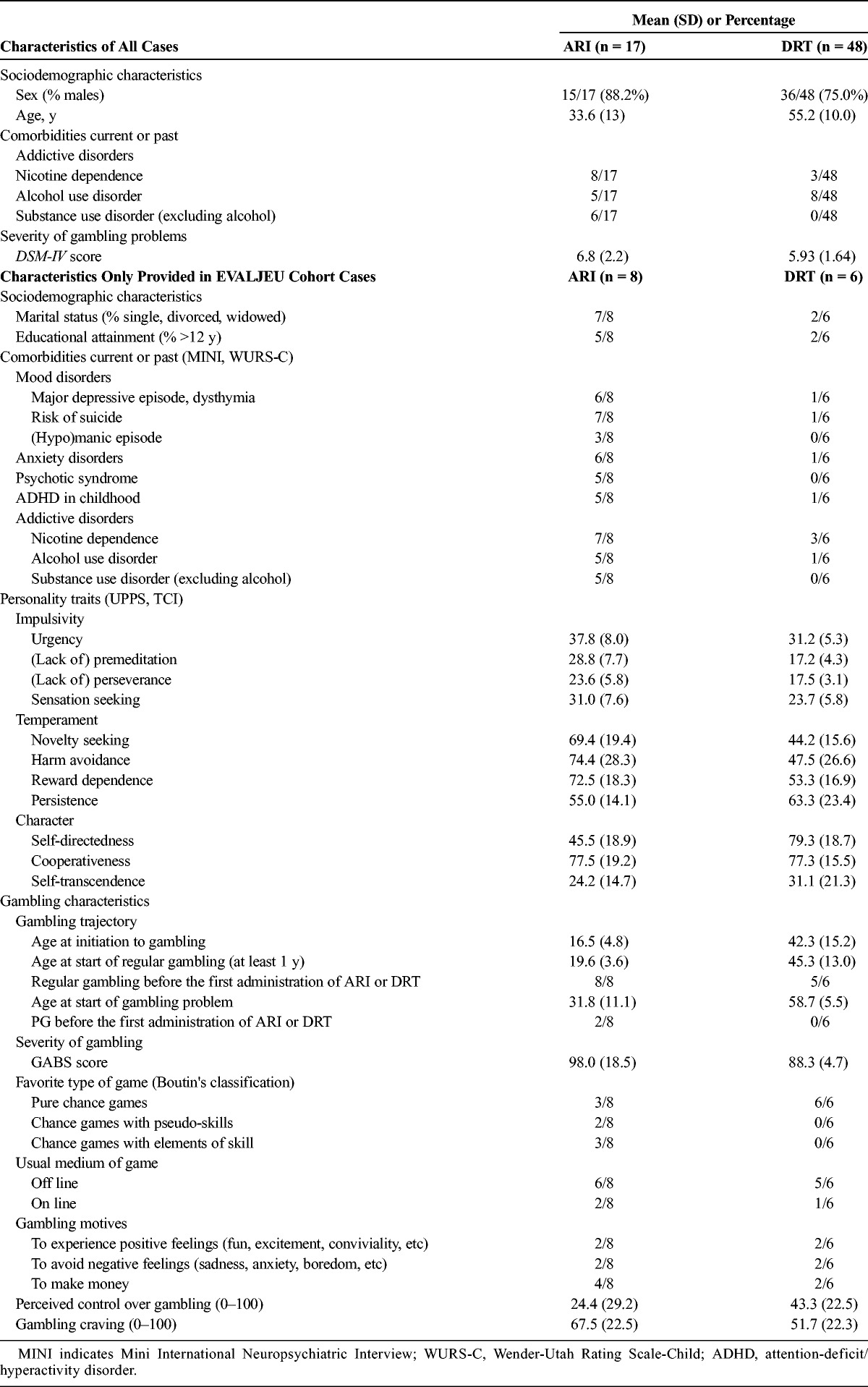
The standardized clinical evaluation of the patients from the EVALJEU cohort gave us more precise information about clinical and gambling characteristics (Table 1). Thus, patients in the ARI group also seemed to have more pronounced impulsive traits based on the results from the UPPS questionnaire. They particularly displayed significantly higher scores on the (lack of) perseverance, the (lack of) premeditation, and the sensations seeking facets of impulsivity. A similar pattern was observed concerning the TCI. Patients in the ARI group showed significantly higher scores on the novelty seeking and the “reward dependence” dimensions. Conversely, patients in the DRT group scored significantly higher on the “self-directedness” dimension. In regard to the gambling trajectory, differences were observed between the 2 groups. Particularly, patients in the ARI group were significantly younger when they started gambling, became regular gamblers, and became problem gamblers. All of the patients (except 1 in the DRT group) were regular gamblers before the first administration of the studied medication, regardless of type of medication (ARI or DRT). The time elapsing between the first use of the medication and the beginning of gambling problems ranged from a few days to several months. Only 2 patients were already problem gamblers before the first administration of the studied medication, namely, ARI. In such cases, their gambling problems became worse after the administration of ARI. Patients in the ARI group seemed to have more serious gambling problems. They displayed a higher score on the GABS. Pure chance games were the only favorite gambling games for all of the patients in the DRT group, whereas the patients in the ARI group gambled on pure chance games, chance games with pseudo-skills, and reported playing poker. Their gambling motives included gambling to experience positive feelings, gambling to avoid negative emotions, and gambling to make money, which were equally reported by the patients in the DRT group. Half of the patients in the ARI group said that they gambled to make money. Finally, patients in the ARI group had a particularly low perceived control over gambling, in addition to particularly high gambling cravings.
TABLE 1.
Comparison of the Characteristics of ARI and DRT Patients
DISCUSSION
This work aimed to characterize disordered gamblers whose GD could possibly result from an adverse drug reaction after the administration of a dopamine medication. Two types of dopamine medication were investigated involving 2 types of underlying diseases and thus 2 types of vulnerable patients. The probability that GD was actually due to a dopamine agonist was possible in 16 of 17 ARI cases and in 46 of 48 DRT cases. Gambling disorder appeared between a few days and a few months after dopaminergic medication was started—sometimes only after the dosage was increased—and it decreased between a few days and a few months after the treatment was stopped; in some cases, it stopped only after the dosage was decreased. The complex and varied temporal relationship between medication onset and GD onset has already been noted in a recent publication.54 Unfortunately, the published case reports were not presented in a standardized way, with important missing data in some cases (eg, history of a substance use disorder or GD severity). This lack of information is an important issue because GD etiology includes individual vulnerability factors, such as a premorbid psychiatric disorder, personality traits, maladaptive coping strategies, negative life events, and so on, as well as contextual factors, such as poor social support, a low educational or income level, many gambling opportunities, and so on. All of the factors could be confounders and should be considered.54 To alleviate this problem, the analysis of the EVALJEU cohort is invaluable. New clinical and gambling characteristics were highlighted, with differences between patients according to their medication. The greatest strength of our work was that it was based on a standardized assessment using validated tools. We obtained reliable data and proper diagnosis to compare the patients.
Two clinical patterns emerged. Patients in the ARI group were younger. Even if patients in the DRT group were older than the others, some were relatively young PD patients. Similar findings were reported in previous works that concluded that an early onset of PD was a predictive factor of DRT-induced GD or other impulsive control disorders.1,12 Previous works concluded that co-occurring psychiatric disorders, especially mood and anxiety disorders, were often associated with PD.55,56 Although some psychiatric disorders were observed as current comorbidities in patients in the DRT group, our results were not consistent with the literature, which may be explained by several hypotheses. First, patients in the DRT group were mostly men, and female sex is a risk factor of depression and anxiety in PD.55 Second, as noted by Grachev,57 the underlying pathophysiological mechanisms of the association between depression and PD are complex and not yet completely understood, including brain changes. Recently, Vriend et al58 speculated that depressive symptoms in PD might be specifically associated with the degeneration of dopaminergic projections and possibly with those specifically from the ventral tegmental area, resulting in dopamine loss in the caudate nucleus. We can assume that this localized degeneration manifests itself after a particular number of years after PD onset. Starting DRT or optimizing its dosage often allows for improvements in depressive symptoms. All of the patients in the DRT group had been undergoing treatment for several years. Third, depressive thoughts can be denied by patients if PD occurs, and gambling could represent a way to avoid confrontation with these negative effects. Most of the patients in the DRT group gambled to experience positive feelings and to avoid negative feelings. Therefore, a way of acting out, such as gambling, could be an intrapsychic defense mechanism. It is not surprising to find many psychiatric disorders in the patients in the ARI group because this medication is indicated to treat mood and schizophrenic disorders. Patients with mood disorders or schizophrenia have high rates of co-occurring substance use disorders.59 Dual diagnoses were indeed common in our sample.
The data extracted from the EVALJEU cohort provided us more details. Indeed, differences between patients appeared when personality traits were considered. Pathological gamblers are significantly more likely to demonstrate impulsivity, sensation seeking, and novelty seeking than controls.38,60,61 Patients in the ARI group are characterized by their impulsive profile, with high novelty seeking. These are well-known features in substance misuse and behavioral addiction38,62 and are particularly pronounced in schizophrenic patients with a dual diagnosis.63 Parkinson disease patients are often described as low novelty seekers,64 whereas novelty seeking is robustly associated with GD in PD.14 Therefore, this temperamental dimension allows for a distinction to be made between patients. Parkinson disease patients were more perseverant and seemed to be more persistent.65 Several hypotheses could be proposed to explain the differences between the patients: (1) sensation seeking tends to decrease with age66; (2) sensation seeking scores vary with the favorite type of game67; and (3) PD leads to prefrontal dysfunction in which perseveration is an early sign.65 A specific impairment of shifting behaviors after negative outcomes due to a disconnection between the anterior cingulate cortex and the striatum only affects PD patients with GD and not those without GD.68
Patients using ARI or DRT also differed according to their gambling trajectory. Patients using ARI exhibit a classical young adult trajectory,69 and patients using DRT exhibit a mid-life trajectory, regardless of their medication. Mood disorders and schizophrenic disorders occur early in life and are risk factors of GD.70–72 In the last 2 decades, the increasing opportunities for gambling constitute an evident risk factor of GD in the general population and could explain why the patients in the DRT group (older patients) began gambling later in mid-life, approximately 20 years ago.73 All of these patients (except one) were regular gamblers before the first administration of ARI or DRT. Obviously, regular gambling is a risk factor of developing gambling problems.74 Patients in the ARI group seemed to experience more severe gambling problems, with a higher level of gambling-related cognition. Previous works concluded that GD severity and the gambling-related cognition level are positively correlated.75,76 The underlying bipolar or schizophrenic disorder may explain that patients exhibit more cognitive distortions, such as optimistic bias and superstitions.77 This view is supported by the main gambling motive reported in the ARI group: patients hoped to make money. Conversely, PD patients were seeking enhancement and coping, in addition to having a financial motive. Gambling motives both in the ARI group and in the DRT group could account for their favorite games: strategic games (which promote cognitive distortions, such as the illusion of control) in the ARI group and nonstrategic games (to avoid thinking and allow escapism) in the DRT group. Persistence, perseverance, and perseveration, which are dimensions displayed by the PD patient, could explain why they preferred gambling using slot machines or scratch cards.
CONCLUSIONS
The hypothesis that both ARI and DRT could be involved in the development of impulse control disorders or behavioral addictions, especially GD, is supported by our results. In our study, patients in the ARI group seemed to be more severe problem gamblers than patients in the DRT group, leading to an apparent pharmacological paradox. Indeed, ARI is a partial D2 receptor agonist, whereas DRT includes full D2 receptor agonist. These observations may be related to the initial disorders for which the treatment is indicated, various effects of the environment, or life habits. The trigger mechanism of developing GD is complex and cannot be attributed only to the dopaminergic drugs' pharmacodynamic effects. Indeed, the characteristics of the various diseases for which treatment is indicated and the environment need to be considered to understand the type of gambling behavior the patient may develop. Vigilance regarding the prescription of dopaminergic therapy is still required. However, given the limitations of our work (small number of case reports, heterogeneous assessment methods, etc), further studies are needed to attribute a causal relationship between medication and GD. A cohort study is a promising way to obtain further evidence.
Supplementary Material
AUTHOR DISCLOSURE INFORMATION
M.G.B., A.S., J.L., and G.B. declare that the Addictology and Psychiatry Department has received funding directly from the University Hospital of Nantes and French state gambling operators (FDJ and PMU). Scientific independence toward gambling industry operators is warranted. There were no constraints on publishing. The work under consideration for publication is part of the EVALJEU cohort, for which the Addictology and Psychiatry Department has received grants from the French Health Ministry and the French interdepartmental agency for the fight against drugs and drug addiction. P.D. received research support from the Michael J. Fox Foundation for Parkinson's disease and the France Parkinson association and a speech honorarium from Novartis. F.P., F.E., L.G., P.J., and C.V.V. declare that they have no conflicts of interest.
Footnotes
Supplemental digital contents are available for this article. Direct URL citation appears in the printed text and is provided in the HTML and PDF versions of this article on the journal's Web site (www.psychopharmacology.com).
REFERENCES
- 1. Ambermoon P, Carter A, Hall WD, et al. Impulse control disorders in patients with Parkinson's disease receiving dopamine replacement therapy: evidence and implications for the addictions field. Addiction. 2011; 106: 283– 293. [DOI] [PubMed] [Google Scholar]
- 2. Gallagher DA, O'Sullivan SS, Evans AH, et al. Pathological gambling in Parkinson's disease: risk factors and differences from dopamine dysregulation. An analysis of published case series. Mov Disord. 2007; 22: 1757– 1763. [DOI] [PubMed] [Google Scholar]
- 3. Voon V, Fernagut PO, Wickens J, et al. Chronic dopaminergic stimulation in Parkinson's disease: from dyskinesias to impulse control disorders. Lancet Neurol. 2009; 8: 1140– 1149. [DOI] [PubMed] [Google Scholar]
- 4. Seedat S, Kesler S, Niehaus DJ, et al. Pathological gambling behaviour: emergence secondary to treatment of Parkinson's disease with dopaminergic agents. Depress Anxiety. 2000; 11: 185– 186. [DOI] [PubMed] [Google Scholar]
- 5. Molina JA, Sainz-Artiga MJ, Fraile A, et al. Pathologic gambling in Parkinson's disease: a behavioral manifestation of pharmacologic treatment? Mov Disord. 2000; 15: 869– 872. [DOI] [PubMed] [Google Scholar]
- 6. Driver-Dunckley E, Samanta J, Stacy M. Pathological gambling associated with dopamine agonist therapy in Parkinson's disease. Neurology. 2003; 61: 422– 423. [DOI] [PubMed] [Google Scholar]
- 7. Avanzi M, Uber E, Bonfa F. Pathological gambling in two patients on dopamine replacement therapy for Parkinson's disease. Neurol Sci. 2004; 25: 98– 101. [DOI] [PubMed] [Google Scholar]
- 8. Dodd ML, Klos KJ, Bower JH, et al. Pathological gambling caused by drugs used to treat Parkinson disease. Arch Neurol. 2005; 62: 1377– 1381. [DOI] [PubMed] [Google Scholar]
- 9. Lu C, Bharmal A, Suchowersky O. Gambling and Parkinson disease. Arch Neurol. 2006; 63: 298. [DOI] [PubMed] [Google Scholar]
- 10. Szarfman A, Doraiswamy PM, Tonning JM, et al. Association between pathologic gambling and parkinsonian therapy as detected in the Food and Drug Administration Adverse Event database. Arch Neurol. 2006; 63: 299– 300. [DOI] [PubMed] [Google Scholar]
- 11. Weintraub D, Siderowf AD, Potenza MN, et al. Association of dopamine agonist use with impulse control disorders in Parkinson disease. Arch Neurol. 2006; 63: 969– 973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Voon V, Hassan K, Zurowski M, et al. Prospective prevalence of pathologic gambling and medication association in Parkinson disease. Neurology. 2006; 66: 1750– 1752. [DOI] [PubMed] [Google Scholar]
- 13. Grosset KA, Macphee G, Pal G, et al. Problematic gambling on dopamine agonists: not such a rarity. Mov Disord. 2006; 21: 2206– 2208. [DOI] [PubMed] [Google Scholar]
- 14. Voon V, Thomsen T, Miyasaki JM, et al. Factors associated with dopaminergic drug-related pathological gambling in Parkinson disease. Arch Neurol. 2007; 64: 212– 216. [DOI] [PubMed] [Google Scholar]
- 15. Singh A, Kandimala G, Dewey RB, Jr, et al. Risk factors for pathologic gambling and other compulsions among Parkinson's disease patients taking dopamine agonists. J Clin Neurosci. 2007; 14: 1178– 1181. [DOI] [PubMed] [Google Scholar]
- 16. Drapier D, Drapier S, Sauleau P, et al. Pathological gambling secondary to dopaminergic therapy in Parkinson's disease. Psychiatry Res. 2006; 144: 241– 244. [DOI] [PubMed] [Google Scholar]
- 17. Imamura A, Uitti RJ, Wszolek ZK. Dopamine agonist therapy for Parkinson disease and pathological gambling. Parkinsonism Relat Disord. 2006; 12: 506– 508. [DOI] [PubMed] [Google Scholar]
- 18. O'Sullivan SS, Lees AJ. Pathological gambling in Parkinson's disease. Lancet Neurol. 2007; 6: 384– 386. [DOI] [PubMed] [Google Scholar]
- 19. Crockford D, Quickfall J, Currie S, et al. Prevalence of problem and pathological gambling in Parkinson's disease. J Gambl Stud. 2008; 24: 411– 422. [DOI] [PubMed] [Google Scholar]
- 20. Lee JY, Kim JM, Kim JW, et al. Association between the dose of dopaminergic medication and the behavioral disturbances in Parkinson disease. Parkinsonism Relat Disord. 2010; 16: 202– 207. [DOI] [PubMed] [Google Scholar]
- 21. Santangelo G, Vitale C, Trojano L, et al. Cognitive dysfunctions and pathological gambling in patients with Parkinson's disease. Mov Disord. 2009; 24: 899– 905. [DOI] [PubMed] [Google Scholar]
- 22. Santangelo G, Barone P, Trojano L, et al. Pathological gambling in Parkinson's disease. A comprehensive review. Parkinsonism Relat Disord. 2013; 19: 645– 653. [DOI] [PubMed] [Google Scholar]
- 23. Rang HP, Dale MM, Ritter JM, et al. Rang & Dale's Pharmacology. 7th ed London, United Kingdom: Elsevier Churchill Livingstone; 2012: 792. [Google Scholar]
- 24. Gavaudan G, Magalon D, Cohen J, et al. Partial agonist therapy in schizophrenia: relevance to diminished criminal responsibility. J Forensic Sci. 2010; 55: 1659– 1662. [DOI] [PubMed] [Google Scholar]
- 25. Roxanas MG. Pathological gambling and compulsive eating associated with aripiprazole. Aust N Z J Psychiatry. 2010; 44: 291. [DOI] [PubMed] [Google Scholar]
- 26. Cohen J, Magalon D, Boyer L, et al. Aripiprazole-induced pathological gambling: a report of 3 cases. Curr Drug Saf. 2011; 6: 51– 53. [DOI] [PubMed] [Google Scholar]
- 27. Smith N, Kitchenham N, Bowden-Jones H. Pathological gambling and the treatment of psychosis with aripiprazole: case reports. Br J Psychiatry. 2011; 199: 158– 159. [DOI] [PubMed] [Google Scholar]
- 28. Gaboriau L, Victorri-Vigneau C, Gerardin M, et al. Aripiprazole: a new risk factor for pathological gambling? A report of 8 case reports. Addict Behav. 2014; 39: 562– 565. [DOI] [PubMed] [Google Scholar]
- 29. Sharpe L. A reformulated cognitive-behavioral model of problem gambling. A biopsychosocial perspective. Clin Psychol Rev. 2002; 22: 1– 25. [DOI] [PubMed] [Google Scholar]
- 30. Iancu I, Lowengrub K, Dembinsky Y, et al. Pathological gambling: an update on neuropathophysiology and pharmacotherapy. CNS Drugs. 2008; 22: 123– 138. [DOI] [PubMed] [Google Scholar]
- 31. Blaszczynski A, Nower L. A pathways model of problem and pathological gambling. Addiction. 2002; 97: 487– 499. [DOI] [PubMed] [Google Scholar]
- 32. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009; 62: 1006– 1012. [DOI] [PubMed] [Google Scholar]
- 33. Toce-Gerstein M, Gerstein DR, Volberg RA. A hierarchy of gambling disorders in the community. Addiction. 2003; 98: 1661– 1672. [DOI] [PubMed] [Google Scholar]
- 34. Potenza MN, Maciejewski PK, Mazure CM. A gender-based examination of past-year recreational gamblers. J Gambl Stud. 2006; 22: 41– 64. [DOI] [PubMed] [Google Scholar]
- 35. Toneatto T, Millar G. Assessing and treating problem gambling: empirical status and promising trends. Can J Psychiatry. 2004; 49: 517– 525. [DOI] [PubMed] [Google Scholar]
- 36. Lecrubier Y, Sheehan D, Weiller E, et al. The Mini International Neuropsychiatric Interview (MINI), a short diagnostic structured interview: reliability and validity according to the CIDI. Eur Psychiatry. 1997; 12: 224– 231. [Google Scholar]
- 37. Ward MF, Wender PH, Reimherr FW. The Wender Utah Rating Scale: an aid in the retrospective diagnosis of childhood attention deficit hyperactivity disorder. Am J Psychiatry. 1993; 150: 885– 890. [DOI] [PubMed] [Google Scholar]
- 38. Whiteside SP, Lynam DR, Miller JD, et al. Validation of the UPPS Impulsive Behaviour Scale: a four model of impulsivity. Eur J Pers. 2005; 19: 559– 574. [Google Scholar]
- 39. Cloninger CR. The Temperament and Character Inventory-125 (TCI-125; version 1). St Louis, MO: Washington University Center for Psychobiology of Personality; 1992. [Google Scholar]
- 40. Breen RB, Zuckerman M. ‘Chasing’ in gambling behavior: personality and cognitive determinants. Pers Individividual Diffferences. 1999; 27: 1097– 1111. [Google Scholar]
- 41. Boutin C. Le jeu: chance ou stratégie? Choisir librement la place du jeu dans votre vie. Montréal, Canada: Les Editions de l'Homme; 2010: 272. [Google Scholar]
- 42. Bandini F, Primavera A, Pizzorno M, et al. Using STN DBS and medication reduction as a strategy to treat pathological gambling in Parkinson's disease. Parkinsonism Relat Disord. 2007; 13: 369– 371. [DOI] [PubMed] [Google Scholar]
- 43. Bosco D, Plastino M, Colica C, et al. Opioid antagonist naltrexone for the treatment of pathological gambling in Parkinson disease. Clin Neuropharmacol. 2012; 35: 118– 120. [DOI] [PubMed] [Google Scholar]
- 44. Bostwick JM, Hecksel KA, Stevens SR, et al. Frequency of new-onset pathologic compulsive gambling or hypersexuality after drug treatment of idiopathic Parkinson disease. Mayo Clin Proc. 2009; 84: 310– 316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Garcia RF, Ordacgi L, Mendlowicz MV, et al. Treatment of juvenile Parkinson disease and the recurrent emergence of pathologic gambling. Cogn Behav Neurol. 2007; 20: 11– 14. [DOI] [PubMed] [Google Scholar]
- 46. Pignatti R, Brioschi A, Mauro A, et al. Selective IGT decision-making impairment in a patient with juvenile Parkinson's disease and pathological gambling: a role for dopaminergic therapy? Neurocase. 2012; 18: 503– 513. [DOI] [PubMed] [Google Scholar]
- 47. Tschopp L, Salazar Z, Gomez Botello MT, et al. Impulse control disorder and piribedil: report of 5 cases. Clin Neuropharmacol. 2010; 33: 11– 13. [DOI] [PubMed] [Google Scholar]
- 48. Wilson L, Sheehan J, Thorpe M. Three cases of impulse control disorder in Parkinson's disease patients receiving dopamine replacement therapy. Ir Med J. 2013; 106: 24– 25. [PubMed] [Google Scholar]
- 49. Montastruc JL, Schmitt L, Bagheri H. Pathological gambling behavior in a patient with Parkinson's disease treated with levodopa and bromocriptine [in French]. Rev Neurol (Paris). 2003; 159: 441– 443. [PubMed] [Google Scholar]
- 50. Kurlan R. Disabling repetitive behaviors in Parkinson's disease. Mov Disord. 2004; 19: 433– 437. [DOI] [PubMed] [Google Scholar]
- 51. Larner AJ. Medical hazards of the internet: gambling in Parkinson's disease. Mov Disord. 2006; 21: 1789. [DOI] [PubMed] [Google Scholar]
- 52. Wong SH, Cowen Z, Allen EA, et al. Internet gambling and other pathological gambling in Parkinson's disease: a case series. Mov Disord. 2007; 22: 591– 593. [DOI] [PubMed] [Google Scholar]
- 53. Naranjo CA, Busto U, Sellers EM, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981; 30: 239– 245. [DOI] [PubMed] [Google Scholar]
- 54. Olley J, Blaszczynski A, Lewis S. Dopaminergic medication in Parkinson's disease and problem gambling. J Gambl Stud. 2015; 31: 1085– 1106. [DOI] [PubMed] [Google Scholar]
- 55. de Rezende Costa FH, Zuma Rosso AL, Maultasch H, et al. Depression in Parkinson's disease: diagnosis and treatment. Arq Neuropsichiatr. 2012; 70: 617– 620. [DOI] [PubMed] [Google Scholar]
- 56. Stefanova E, Ziropadja L, Petrovic M, et al. Screening for anxiety symptoms in Parkinson disease: a cross-sectional study. J Geriatr Psychiatry Neurol. 2013; 26: 34– 40. [DOI] [PubMed] [Google Scholar]
- 57. Grachev ID. Dopamine transporter imaging with [123I]FP-CIT (DaTSCAN) in Parkinson's disease with depressive symptoms: a biological marker for causal relationships? J Neurol Neurosurg Psychiatry. 2014; 85: 130– 131. [DOI] [PubMed] [Google Scholar]
- 58. Vriend C, Raijmakers P, Veltman DJ, et al. Depressive symptoms in Parkinson's disease are related to reduced [123I]FP-CIT binding in the caudate nucleus. J Neurol Neurosurg Psychiatry. 2014; 85: 159– 164. [DOI] [PubMed] [Google Scholar]
- 59. Mueser KT, Gingerich S. Treatment of co-occurring psychotic and substance use disorders. Soc Work Public Health. 2013; 28: 424– 439. [DOI] [PubMed] [Google Scholar]
- 60. Cloninger CR, Svrakic DM, Przybeck TR. A psychobiological model of temperament and character. Arch Gen Psychiatry. 1993; 50: 975– 990. [DOI] [PubMed] [Google Scholar]
- 61. Vitaro F, Arseneault L, Tremblay RE. Impulsivity predicts problem gambling in low SES adolescent males. Addiction. 1999; 94: 565– 575. [DOI] [PubMed] [Google Scholar]
- 62. Milivojevic D, Milovanovic SD, Jovanovic M, et al. Temperament and character modify risk of drug addiction and influence choice of drugs. Am J Addict. 2012; 21: 462– 467. [DOI] [PubMed] [Google Scholar]
- 63. Zhornitsky S, Rizkallah E, Pampoulova T, et al. Sensation-seeking, social anhedonia, and impulsivity in substance use disorder patients with and without schizophrenia and in non-abusing schizophrenia patients. Psychiatry Res. 2012; 200: 237– 241. [DOI] [PubMed] [Google Scholar]
- 64. McNamara P, Durso R, Harris E. Alterations of the sense of self and personality in Parkinson's disease. Int J Geriatr Psychiatry. 2008; 23: 79– 84. [DOI] [PubMed] [Google Scholar]
- 65. Stoffers D, Berendse HW, Deijen JB, et al. Motor perseveration is an early sign of Parkinson's disease. Neurology. 2001; 57: 2111– 2113. [DOI] [PubMed] [Google Scholar]
- 66. Gonzales N, Mora M, Gutierrez-Maldonado J, et al. Pathological gambling and age: differences in personality, psychopathology and response to treatment variables. Addict Behav. 2005; 30: 380– 388. [DOI] [PubMed] [Google Scholar]
- 67. Bonnaire C, Varescon I, Bungener C. Sensation seeking in a French population of horse betting gamblers: comparison between pathological and regular [in French]. Encéphale. 2007; 33: 798– 804. [DOI] [PubMed] [Google Scholar]
- 68. Cilia R, Cho SS, van Eimeren T, et al. Pathological gambling in patients with Parkinson's disease is associated with fronto-striatal disconnection: a path modeling analysis. Mov Disord. 2011; 26: 225– 233. [DOI] [PubMed] [Google Scholar]
- 69. Nelson SE, Laplante DA, Labrie RA, et al. The proxy effect: gender and gambling problem trajectories of Iowa gambling treatment program participants. J Gambl Stud. 2006; 22: 221– 240. [DOI] [PubMed] [Google Scholar]
- 70. Kessler RC, Hwang I, LaBrie R, et al. DSM-IV pathological gambling in the National Comorbidity Survey Replication. Psychol Med. 2008; 38: 1351– 1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Kim SW, Grant JE, Eckert ED, et al. Pathological gambling and mood disorders: clinical associations and treatment implications. J Affect Disord. 2006; 92: 109– 116. [DOI] [PubMed] [Google Scholar]
- 72. Aragay N, Roca A, Garcia B, et al. Pathological gambling in a psychiatric sample. Compr Psychiatry. 2012; 53: 9– 14. [DOI] [PubMed] [Google Scholar]
- 73. Pearce J, Mason K, Hiscock R, et al. A national study of neighbourhood access to gambling opportunities and individual gambling behaviour. J Epidemiol Community Health. 2008; 62: 862– 868. [DOI] [PubMed] [Google Scholar]
- 74. Currie SR, Hodgins DC, Wang J, et al. Risk of harm among gamblers in the general population as a function of level of participation in gambling activities. Addiction. 2006; 101: 570– 580. [DOI] [PubMed] [Google Scholar]
- 75. Emond MS, Marmurek HH. Gambling related cognitions mediate the association between thinking style and problem gambling severity. J Gambl Stud. 2010; 26: 257– 267. [DOI] [PubMed] [Google Scholar]
- 76. Xian H, Shah KR, Phillips SM, et al. Association of cognitive distortions with problem and pathological gambling in adult male twins. Psychiatry Res. 2008; 160: 300– 307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Prentice KJ, Gold JM, Carpenter WT., Jr Optimistic bias in the perception of personal risk: patterns in schizophrenia. Am J Psychiatry. 2005; 162: 507– 512. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


