Abstract
Introduction
Although Chlamydia trachomatis (CT) is the most common bacterial sexually transmitted infection worldwide, little is known about the natural course of the bacterial load during infection. We investigated the natural course of the bacterial load in the interval between screening and returning for treatment in genital and anorectal CT-infections.
Materials & Methods
CT-positive patients, visiting our STI-clinic in the Netherlands from June 2011–January 2014, provided a second urogenital and/or anorectal sample when returning for treatment (diagnostic sample = T1; treatment sample = T2). Patient-record provided data about the days between samples and the date of last unsafe sex. Included patients were ≥18 years old, HIV-negative and did not report antibiotic use in the study-interval. CT load was quantified using qPCR. CT load was log-transformed, and a CT load difference (Δ-CT load) of >1 log was deemed clinically relevant. Chi-square test compared load category distributions over time (decrease/equal/increase), between sample types.
Results
274 patients provided 296 paired samples. Majority of samples had a stable CT load in the interval T1-T2 (66.3%, 73.1% and 48.6% for vaginal swabs, urine and anorectal swabs resp. p = 0.07). Load decreased in 17–41% of patients, while ±10% of patients showed an increase in CT load. No association between Δ-CT load and the interval T1-T2 was observed. Large variations can be seen in CT load at T1 and over time.
Discussion
The majority (±90%) of patients have a stable or decreasing CT load in the time interval between screening and returning for treatment. The number of days between sampling was not associated with change in CT load. In the first month after the last unsafe sex, only stable CT loads were seen. Our data seems to indicate that when most patients visit an STI-clinic, recommended 2 weeks after infection, the infection has already been established or is in its downward phase.
Introduction
Although Chlamydia trachomatis (CT) is the most common bacterial sexually transmitted infection (STI) worldwide, with over 100 million people affected [1], little is known about the natural course of this infection. It is known that urogenital CT infections can have severe outcomes such as pelvic inflammatory disease and tubal scarring resulting in infertility and ectopic pregnancy in women [2]. However, spontaneous clearance of the bacteria has also been reported [3–7]. Too little is currently known about the natural course of a CT infection in humans to help predict the outcome, or even the duration of an infection in an individual patient. This may profoundly influence recommendations for control efforts such as STI screening frequency or time parameters for partner notification and treatment [3, 5].
Estimates of the duration of untreated CT infections, are highly variable by more than 40-fold, from 0.07 years to 2.99 years [8]. The number of patients that spontaneously clear their infection, ranges from 0–94% in studies [6, 9] depending on the time interval between tests. It is difficult to truly study the natural course of CT infections, as it is unethical to leave patients untreated after diagnosis. Moreover, nearly nothing is known about the natural course of the bacterial load during CT infections in humans.
The natural course of the bacterial load of Chlamydia muridarum in mouse models is more extensively studied. After CT administration, a sharp increase in CT load is seen, followed by a longer plateau phase, and eventually a decline in load until resolution, approximately 3–5 weeks after infection [10–12]. In humans, it is not unlikely that a similar load curve will be found, both in urogenital and anorectal samples [13]. However, all studies assessing CT load before treatment have determined load at a single time point during an infection [14–16].
We evaluated the bacterial load in two consecutive samples (one diagnostic sample and one sample before treatment) from CT-positive STI-clinic attendants to better understand the natural course of the urogenital and anorectal bacterial load over time.
Materials & Methods
Study population and procedures
From June 1st 2011 to January 2014 at the STI-clinic of Public Health Service South Limburg, the Netherlands, CT-positive patients of at least 18 years that attended one of five trained STI nurses partaking in the study, were asked to participate in this study by taking an extra self-collected vaginal swab for women and a first-void urine sample for men when returning for treatment. Some patients had been tested anorectally (i.e. all MSM and women based on their sexual history of receptive anorectal intercourse, and/or on reported anorectal symptoms) at the diagnostic visit and these participants also provided an extra self-collected anorectal swab when returning for treatment. For the purpose of this study, the first (diagnostic) sample that patients provided will from hereon be referred to as T1 and the second sample patients provided at the time of treatment as T2. Trained study nurses provided patients with a visual diagram and oral instructions about how to take separate self-collected vaginal and anorectal swabs. For the vaginal swab, the patient was instructed to insert the swab 2.5 cm into the vagina, rotate it for 5 to 10 seconds, and then place it in a capped tube to avoid potential contamination. This procedure was repeated in the anus for the anorectal swab. The rationale for using self-collected vaginal swabs for routine CT testing is that they have a similar or higher sensitivity compared to nurse-collected cervical swabs [17–19]. Specimens were screened for CT at the clinical microbiology laboratory at Maastricht University Medical Center (Maastricht, The Netherlands) using a commercial nucleic acid amplification test [polymerase chain reaction (PCR); Roche Cobas Amplicor until 2012 and later Roche Cobas 4800, Roche Diagnostics, Basel, Switzerland] as PCR has a higher sensitivity than culture based techniques [20].
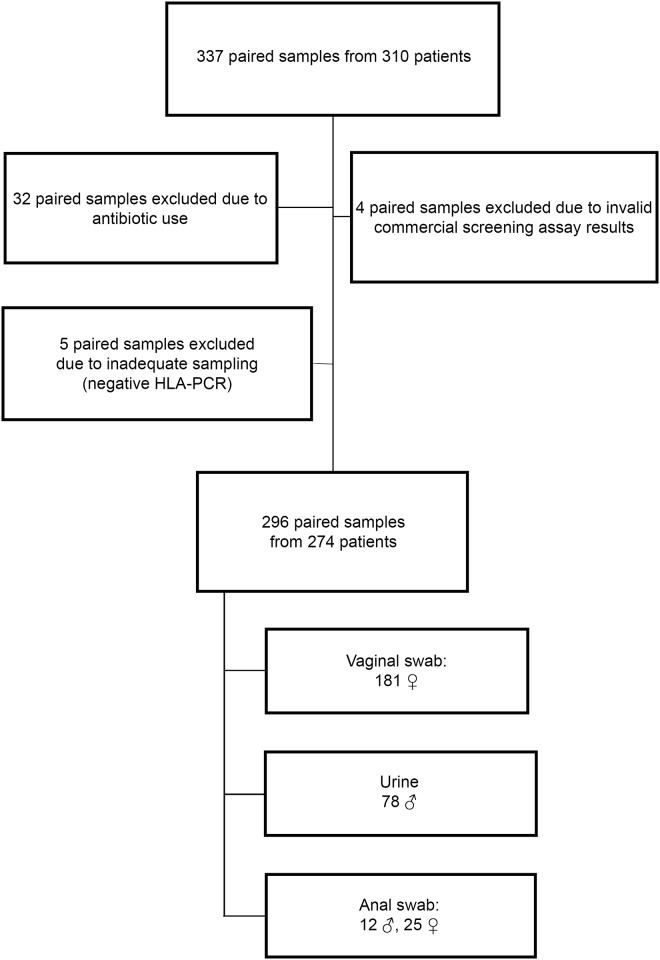
Patients empirically treated at the time of initial evaluation for CT-associated syndromes (e.g., urethritis or cervicitis) or other treatment indications (e.g., CT contact) were ineligible for inclusion in the study as the natural course of infection cannot be studied after treatment. Additional exclusion criteria for the current study were antibiotic use in the month before T1, or between T1 and T2, HIV-positivity and an invalid/inhibited CT-test result. This resulted in the exclusion of 41 paired samples from 36 patients (Fig 1).
Fig 1. Flow chart of patients who met inclusion/exclusion criteria for the study population.
310 patients participated in the study, providing 337 paired samples. Forty-one paired samples did not meet inclusion criteria due to antibiotic use (n = 32), an invalid/inhibited commercial screening assay result (n = 4) or due to inadequate sampling as demonstrated by a negative HLA-PCR (n = 5). In total, 274 patients with 296 paired samples were included in this study (181 vaginal swabs, 78 urines and 37 anorectal swabs).
A 30-day maximum time interval between T1 and T2 was allowed. Standard data registration at each consultation included sociodemographic information, antibiotic use, and for some patients also the date of the last unsafe sexual contact.
Ethics statement
Written informed consent was obtained from all patients prior to participation in the study. This study, including the consent procedure, was approved by the Medical Ethics Committee of the Maastricht University Medical Center (METC azM/UM nr. 10-4-66; 15-6-2011).
CT load quantification
When proven CT-positive at T1with the commercial screening assay, CT load quantification was performed for the T1 and T2 sample by an in-house qPCR as described by Dirks et al.[14]. In short, Taqman real-time PCR was used to quantify chlamydial OmpA-gene copies/ml and human leukocyte antigen (HLA)-gene copies/ml to ensure adequate sampling took place. Paired samples were excluded if no HLA could be detected in either sample (n = 5). Due to the lower sensitivity of the qPCR compared to the commercial screening assay, CT-positive samples with a CT load below the quantification limit were set to half the quantification limit[14].
Samples that were CT negative at T2 with the commercial screening assay, were included in this study as samples with 0 CT/ml. Every test is limited through a detection probability of samples with a low load, and we cannot rule out a very low CT load in these ‘CT-negative’ samples, despite duplicate testing.
Load analyses over time
Load values were log transformed for analyses. Logarithmic converted load at T1 was subtracted from T2 to create a new variable ‘Δ-load’. A Δ-load difference of less than 1 log load (-1 to +1) is considered the cut-off value for a stable CT load over time when test-technical variability is taken into account. In short, a positive Δ-load value of >1 log indicates an increase in CT load, a load between +1 and -1 an equal CT load, and a negative value <-1 log a decrease in CT load.
The number of days between T1-T2 was used to construct a load curve in the short interval between T1 and T2. This natural load curve was then expanded by including the date of patients’ last unsafe sexual contact. The number of days since patients’ last (possible) exposure to CT was calculated by subtracting the date of patients’ last unsafe sexual contact from the consultation date (T1 and T2). This variable was then used to construct a natural load curve over time with two load measurements at distinct time points (T1 & T2), where T0 was the moment of the last sexual contact. Information about the date of the last unsafe sexual exposure was available for forty-six paired samples (15.5%), ranging from 3–565 days at T1 (median 80). As only 5 patients with anorectal swabs reported their last unsafe sexual contact, they were excluded from further analyses.
Statistical analysis
Statistical analyses were stratified by sample type due to different load distributions per specimen (data not shown). Descriptive analyses included median and CT load range, the median and range of the number of days between T1-T2 and the median and range of days since last unsafe sexual contact. For the association between the CT load and time between T1-T2, Chi-square test was used to compare the distribution of load categories (decrease/equal/increase) between sample types. Delta CT load (Δ-CT load), 95% confidence intervals (95%CI) and p-values are shown. The mean period between sampling-moments was compared over sample types using one way ANOVA. Results were considered statistically significant at p≤0.05. All statistical tests were performed using IBM SPSS Statistics for Windows, version 22.0 (IBM Corp. Armonk, NY, USA).
Results
Characteristics of the study population
274 patients provided 296 paired samples (T1-sample and T2-sample treated as one pair of samples). Fig 1 provides a flowchart of the 296 included paired samples. Patient age ranged from 18–63 years [median 22].
CT load distribution (in the time interval between T1-T2)
T1-samples had a CT load above the quantification limit of the qPCR in 85.8% (254/296), and T2-samples in 82.1% (243/296). At T2, 7.7% (n = 14) of vaginal swabs, 5.1% (n = 4) of urines and 10.8% (n = 4) of anorectal swabs were CT-negative according to the commercial screening assay (p = 0.36).
Table 1 shows the difference in CT load between samples, both absolute and in categories (increase/equal/decrease). Vaginal swabs had the largest range in CT load, varying from 0–2.2x108 CT/ml, followed by anorectal swabs with a range of 0–1.4x106 and the lowest range was detected in urines, from 0–1.3x105 CT/ml.
Table 1. CT load distribution in absolute values (CT/ml) and 3 categories (decrease/equal/increase).
| Sample type | N | Minimum | Maximum | T1 (median) | T2 (median) | Decrease % (n) | Equal % (n) | Increase % (n) |
|---|---|---|---|---|---|---|---|---|
| Vaginal swabs | 181 | 0 | 2.2x108 | 1.7x105 | 1.5x105 | 22.1% (40) | 66.3% (120) | 11.6% (21) |
| Urines | 78 | 0 | 1.3x105 | 2.5x102 | 2.8x102 | 16.7% (13) | 73.1% (57) | 10.3% (8) |
| Anorectal swabs | 37 | 0 | 1.4x106 | 3.9x103 | 1.2x103 | 40.5% (15) | 48.6% (18) | 10.8% (4) |
The majority of samples had a stable CT load in the interval between T1-T2 (66.3%, 73.1% and 48.6% for vaginal swabs, urine and anorectal swabs respectively; p = 0.78). Increases in CT load were observed in up to 11.6% of samples and this proportion did not vary significantly between sample types (11.6%, 10.3%, 10.8% for vaginal swabs, urine and anorectal swabs respectively, p = 0.78). The proportion of samples in which the load decreased was the largest in anorectal swabs (40.5%), compared to urine (16.7%, p = 0.02) and vaginal swabs (22.1%, p = 0.059).
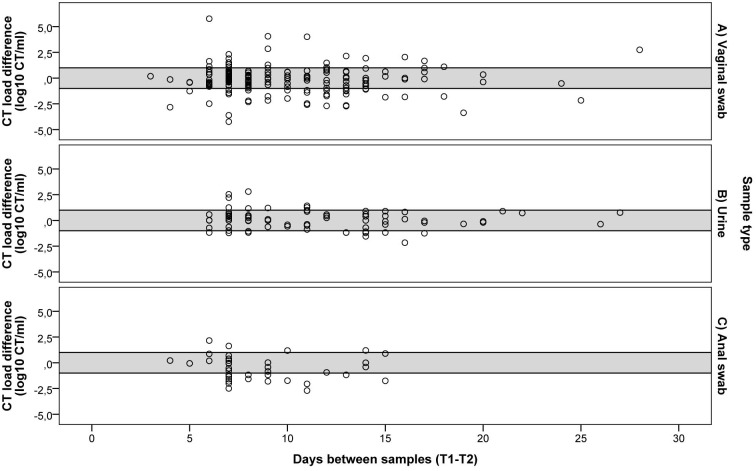
CT load change related to the duration of the time interval between T1-T2
The median period between sampling moments was 8 days (range3-28 days) for vaginal swabs, 10 days (range 6–27 days) for urines and 7 (range 4–15 days) for anorectal swabs (p = 0.70). When the Δ-CT load is plotted in relation to the time interval between T1-T2, as can be seen in Fig 2, it becomes apparent that the majority of patients have a stable CT load over time, as the Δ-CT load lies most frequently in the area between -1 log and +1 log. Furthermore, a larger number of days between samples does not appear to increase the Δ-CT load, as no clear funnelling of the results is apparent. Statistically, no association between Δ-CT load and time interval between T1-T2 was observed for vaginal swabs (Δ-CT load -0.08, 95% CI -0.60–0.43, p = 0.75), for urine (Δ-CT load 0.24, 95% CI -0.28–0.77, p = 0.36) and for anorectal swabs (Δ-CT load -0.17, 95% CI -1.45–1.12, p = 0.80).
Fig 2. CT load in correlation to the time interval between T1-T2.
CT load in A) vaginal swabs, B) urines and C) anorectal swabs. The grey area between lines (+1 to -1) indicates a stable Δ-CT load, the samples above the delineated area have an increase in CT load, and samples below the delineated area show a decrease in CT load in the time interval between T1-T2.
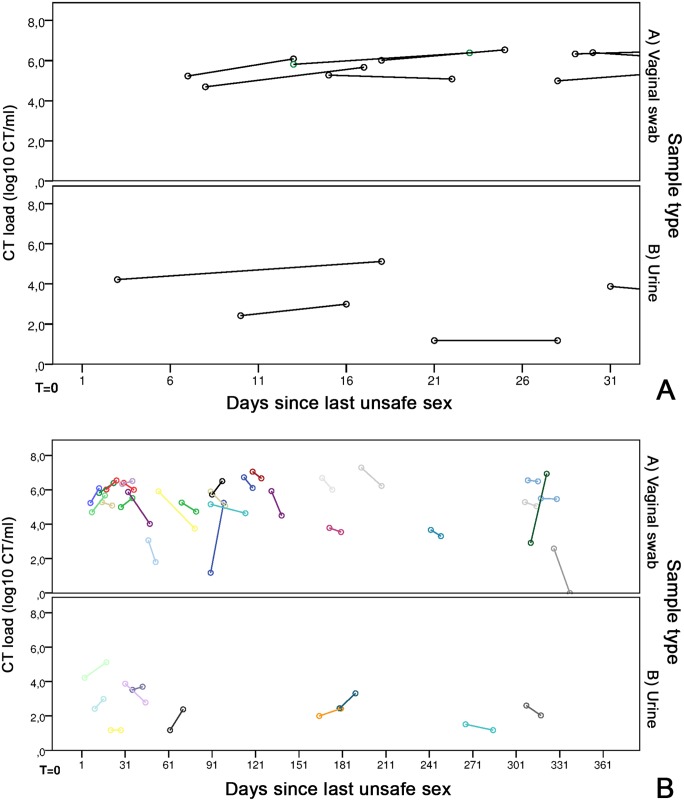
CT load in the time since patients’ last unsafe sexual exposure
The load curve was constructed for forty-one paired samples (13.9%), of whom the last unsafe sexual contact was 3–565 days ago at T1 [median 90 days]. The median number of days since the last unsafe sex was 90 days (range 7–565) for vaginal swabs and 62 days (range 3–380) for urines.
The CT load curve for the first 366 days since the last unsafe sexual exposure (Fig 3A), shows large variations in each patient, in both in the CT load at T1, as well as the Δ-CT load over time. However, a general downward trend can be seen, with most patients exhibiting a decrease in CT load between T1-T2. The first 30 days after unsafe sexual exposure, which is likely the moment that most patients get tested for their CT infection are more clearly shown in Fig 3B. Here, only stable loads can be seen. Furthermore, none of the patients visiting the STI clinic in the two weeks after their last unsafe sexual contact had a ‘low’ CT load, i.e. a positive CT test in the commercial assay, but below the limit of quantification of our in-house PCR.
Fig 3. CT load in correlation to the time of patients’ last unsafe sexual exposure.
(A) CT load in A) 29 vaginal swabs and B) 10 urines correlated to the last unsafe sexual contact of patients, for a maximum of 366 days. T = 0 is the moment of the last unsafe sex and each colour is a different patient. The first circle is the CT load at T1, and the second circle is the CT load at T2, where the length of the connecting line indicates the number of days between samples. (B) CT load in A) 8 vaginal swabs and B) 3 urines in the first month after the last unsafe sexual contact of patients. T = 0 is the moment of the last unsafe sex. The first circle is the CT load at T1, and the second circle is the CT load at T2, where the length of the connecting line indicates the number of days between samples.
A decrease in CT load was first seen after one month (30 days) since the last unsafe sexual exposure. No patients showed an (sharp) increase in CT load in the first 2 months after the last unsafe sexual exposure.
Within 30 days after sexual exposure, CT load showed a median Δ-CT load of 0.53 log CT/ml (range -0.40–0.97), while the CT load after one month had a median Δ-CT load of -0.35 log CT/ml (range -2.58–4.06). Split by sample type, vaginal swabs had a median Δ-CT load of 0.53 log CT/ml (range -0.40–0.97) within 31 days, and -0.45 log CT/ml (range -2.58–4.06) after this time. Urines had a median Δ-CT load of 0.57 log CT/ml (range 0–0.90) within one month, and -0.45 log CT/ml (range -1.09–1.21) after one month.
Discussion
We assessed the natural course of the CT load in the interval between screening and returning for treatment in patients visiting an STI-clinic patients. This is the first study to present quantitative data on the natural course of CT infections over time, in both urogenital infections and anorectal infections in men and women.
We demonstrated a stable CT load in the majority (47–73%) of patients in the time interval between screening and returning for treatment, which ranged in this study from 3–28 days. Depending on the sample type, load decreased in 17–41% of patients, while only ±10% of patients showed an increase in CT load. The number of days between T1-T2 did not correlate to the Δ-CT load, i.e. a longer time between sampling did not result in a larger difference in CT load. Furthermore, the time since last unsafe sexual exposure (to CT) was not clearly related to the course of CT load, with large variations over time.
Little is known about what determines CT load in humans [21], and even less is known about how it progresses during an infection. Prior studies (reviewed in [21]) have quantified load once during an infection, but never before were sequential time point analyses performed. It has become clear that the CT load can vary greatly, depending on the sample type, quantification methodology, age, immunological status, prior CT infections, and likely on the hormonal status of the patient [14, 22–24]. Furthermore, the moment of infection is always uncertain. To reconstruct the natural load-curve during CT infections, mice studies may be guiding. These studies showed a steady increase in bacterial load in the early hours after infection, after which the infection reaches a stable phase and after approximately a week a steady decline in the bacterial load sets in until resolution takes place [10, 11, 25, 26]. In our study, we demonstrated that the CT load is stable or decreasing in 90% of patients over time, both in urogenital and anorectal samples, consistent with the results found in animal studies. We correlated the number of days since patients’ last possible exposure to the CT load, but we could not demonstrate a similar sharp rise in the CT load in humans in the early moments after the last unsafe sexual exposure. We did see a minority of patients that experienced a sharp increase in CT load associated with the early stages of infection, congruent with murine studies, but we do not know their actual moment of infection. Unfortunately we did not have the data of last sexual exposure for all patients included in this study, while even this data would only provide a proxy of the actual moment of infection. Even after 3 days since their last unsafe sexual contact, patient load was sufficiently high to be detected through highly sensitive NAAT and in-house qPCR.
In this light, our results seem to indicate that the majority of patients visit the STI-clinic when the infection has already been established or is in its downward phase. This is surprising, as most current guidelines state that patients should get tested at least 2weeks after the last unsafe sexual practices based on CT’s incubation period of 1–3 weeks [27, 28]. Some recent guidelines incorporating current highly sensitive PCR-techniques are recommending immediate testing after CT exposure [4, 29], with the caution that a negative test must be repeated after 2 weeks. The data presented in this article provides new evidence that justifies the recent recommendations that the 2 week limit before tests might be let go.
Approximately 50% of CT-positives clear their urogenital infection within a year [3, 7]. In the interval between screening and treatment this number ranges from 9–44% in urogenital samples [3, 30, 31] and 18% (n = 11) in anorectal samples [13]. Contrastingly, we found few patients in whom spontaneous clearance occurred, only 8% (14/181) in vaginal swabs, 5% (4/78) in urines and 11% (4/37) in anorectal swabs, despite the use of tests with similar sensitivity and a similar test-interval [3, 32]. The low number of spontaneously cleared CT infections in our study can, most likely, be explained by the exclusion of patients who reported antibiotic use in the interval between T1 and T2 (9%). Anorectal load had a tendency to decrease more often than vaginal and urine load. A possible explanation is a more efficient immune response at the anorectal- than the urogenital site [33], but other factors may be at play.
A limitation of our study is the lack of data about prior CT infections in our patients, however, diagnosed prior infections are only a proxy of the total amount of previous CT infections and therefore may confound these analyses [31]. Another limitation of our study is the inability to perform serological analyses to provide insights into the natural course of CT infections (including possible persistent infections), as blood samples were only available for a minority of the patients included in this study.
It is very difficult to speculate on implications of these results on reinfection rates, progression of disease and associated pathology. Much is still unknown about the clinical implications of the bacterial load, and its correlation to pathology. A low CT load has been associated with subsequent clearance in pharyngeal positive patients [34]. In this study too (results not shown), patients with a low CT load cleared their infection most easily. Furthermore, it has been demonstrated that the CT load is lower in repeat infections [15, 16], and that naturally cleared infections protect from reinfection [31]. Furthermore, Russel et al. [35] demonstrated that seropositive patients had a lower cervical CT load than seronegative patients. However, it has also been shown that repeat CT infections increase the risk of CT-complications like tubal factor infertility [36]. Russel et al. [35] demonstrated that the CT load in the lower genital tract appears unrelated to the endometrial CT load, which is likely most important in developing CT sequelae. The patients with a high CT load are likely at high risk of infecting their sexual partner. It has been shown for other STI’s that a high infectious dose is more easily transmitted than a low dose [37–40]. Furthermore, these patients are more likely to have a continued immune stimulation beyond that of patients with a low CT load, and it may be that this increases their risk of complications. Although many hypotheses exist regarding the CT load and its effect on negative sequelae and re-infection rates of CT, too much is currently unknown to fully elucidate the processes at play.
In short, CT load is stable or decreasing in the vast majority of STI-clinic patients in the time interval between diagnosis and treatment. The time-interval between samples is unrelated to the change in load over time, requiring further research to clarify other factors at play. We found only stable CT loads within the first month after the las unsafe sex, which might reinforce recent guidelines that propose instant CT-testing after unsafe sexual practises.
Acknowledgments
The authors thank the staff of the STI Clinic South Limburg for their valuable contribution to the sample collection. Furthermore, we would like to thank M. Franssen for her help in performing the experiments.
Data Availability
All relevant data are within the paper.
Funding Statement
This work was supported by the Public Health Service South Limburg and the Department of Medical Microbiology, Maastricht University Medical Center+.
References
- 1. World Health Organisation. Prevalence and incidence of selected sexually transmitted infections, Chlamydia trachomatis, Neisseria gonorrhoeae, syphilis and Trichomonas vaginalis: methods and results used by WHO to generate 2005 estimates. 2011. [Google Scholar]
- 2. Ljubin-Sternak S, Mestrovic T. Chlamydia trachomatis and Genital Mycoplasmas: Pathogens with an Impact on Human Reproductive Health. Journal of pathogens. 2014;2014:183167 Epub 2015/01/24. 10.1155/2014/183167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Geisler WM. Duration of untreated, uncomplicated Chlamydia trachomatis genital infection and factors associated with chlamydia resolution: a review of human studies. The Journal of infectious diseases. 2010;201 Suppl 2:S104–13. Epub 2010/05/28. 10.1086/652402 . [DOI] [PubMed] [Google Scholar]
- 4.Brocail M. How Soon Can I Get Tested for STDs After Unprotected Sex? 2015 [updated March 4, 2015; cited 2015 March 20]. Available from: www.stdcheck.com/blog/how-soon-get-tested-for-stds-unprotected-sex/.
- 5. Golden MR, Schillinger JA, Markowitz L, St Louis ME. Duration of untreated genital infections with chlamydia trachomatis: a review of the literature. Sexually transmitted diseases. 2000;27(6):329–37. [DOI] [PubMed] [Google Scholar]
- 6. Molano M, Meijer CJ, Weiderpass E, Arslan A, Posso H, Franceschi S, et al. The natural course of Chlamydia trachomatis infection in asymptomatic Colombian women: a 5-year follow-up study. The Journal of infectious diseases. 2005;191(6):907–16. 10.1086/428287 . [DOI] [PubMed] [Google Scholar]
- 7. Morre SA, van den Brule AJ, Rozendaal L, Boeke AJ, Voorhorst FJ, de Blok S, et al. The natural course of asymptomatic Chlamydia trachomatis infections: 45% clearance and no development of clinical PID after one-year follow-up. International journal of STD & AIDS. 2002;13 Suppl 2:12–8. 10.1258/095646202762226092 . [DOI] [PubMed] [Google Scholar]
- 8. Price MJ, Ades AE, Angelis DD, Welton NJ, Macleod J, Soldan K, et al. Mixture-of-exponentials models to explain heterogeneity in studies of the duration of Chlamydia trachomatis infection. Statistics in medicine. 2013;32(9):1547–60. 10.1002/sim.5603 . [DOI] [PubMed] [Google Scholar]
- 9. Handsfield HH, Alexander ER, Pin Wang S, Pedersen AH, Holmes KK. Differences in the therapeutic response of chlamydia-positive and chlamydia-negative forms of nongonococcal urethritis. Journal of the American Venereal Disease Association. 1976;2(3):5–9. Epub 1976/03/01. . [PubMed] [Google Scholar]
- 10. Carey AJ, Cunningham KA, Hafner LM, Timms P, Beagley KW. Effects of inoculating dose on the kinetics of Chlamydia muridarum genital infection in female mice. Immunology and cell biology. 2009;87(4):337–43. 10.1038/icb.2009.3 . [DOI] [PubMed] [Google Scholar]
- 11. Maxion HK, Liu W, Chang MH, Kelly KA. The infecting dose of Chlamydia muridarum modulates the innate immune response and ascending infection. Infection and immunity. 2004;72(11):6330–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Su H, Messer R, Whitmire W, Hughes S, Caldwell HD. Subclinical chlamydial infection of the female mouse genital tract generates a potent protective immune response: implications for development of live attenuated chlamydial vaccine strains. Infection and immunity. 2000;68(1):192–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Apewokin SK, Geisler WM, Bachmann LH. Spontaneous resolution of extragenital chlamydial and gonococcal infections prior to therapy. Sexually transmitted diseases. 2010;37(5):343–4. 10.1097/OLQ.0b013e3181d73639 . [DOI] [PubMed] [Google Scholar]
- 14. Dirks JA, Wolffs PF, Dukers-Muijrers NH, Brink AA, Speksnijder AG, Hoebe CJ. Chlamydia trachomatis load in population-based screening and STI-clinics: implications for screening policy. PLoS One. 2015;10(3):e0121433 Epub 2015/04/01. 10.1371/journal.pone.0121433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gomes JP, Borrego MJ, Atik B, Santo I, Azevedo J, Brito de Sa A, et al. Correlating Chlamydia trachomatis infectious load with urogenital ecological success and disease pathogenesis. Microbes and infection / Institut Pasteur. 2006;8(1):16–26. Epub 2005/11/18. 10.1016/j.micinf.2005.05.014 . [DOI] [PubMed] [Google Scholar]
- 16. Walker J, Tabrizi SN, Fairley CK, Chen MY, Bradshaw CS, Twin J, et al. Chlamydia trachomatis incidence and re-infection among young women—behavioural and microbiological characteristics. PLoS One. 2012;7(5):e37778 Epub 2012/06/05. 10.1371/journal.pone.0037778 ; PubMed Central PMCID: PMCPmc3360595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hobbs MM, van der Pol B, Totten P, Gaydos CA, Wald A, Warren T, et al. From the NIH: proceedings of a workshop on the importance of self-obtained vaginal specimens for detection of sexually transmitted infections. Sex Transm Dis. 2008;35(1):8–13. Epub 2007/12/25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cook RL, Hutchison SL, Ostergaard L, Braithwaite RS, Ness RB. Systematic review: noninvasive testing for Chlamydia trachomatis and Neisseria gonorrhoeae. Ann Intern Med. 2005;142(11):914–25. Epub 2005/06/09. . [DOI] [PubMed] [Google Scholar]
- 19. Van Der Pol B, Taylor SN, Liesenfeld O, Williams JA, Hook EW 3rd. Vaginal swabs are the optimal specimen for detection of genital Chlamydia trachomatis or Neisseria gonorrhoeae using the Cobas 4800 CT/NG test. Sex Transm Dis. 2013;40(3):247–50. Epub 2013/02/15. 10.1097/OLQ.0b013e3182717833 . [DOI] [PubMed] [Google Scholar]
- 20. Schachter J. DFA, EIA, PCR, LCR and other technologies: what tests should be used for diagnosis of chlamydia infections? Immunol Invest. 1997;26(1–2):157–61. Epub 1997/01/01. . [DOI] [PubMed] [Google Scholar]
- 21. Vodstrcil LA, McIver R, Huston WM, Tabrizi SN, Timms P, Hocking JS. The epidemiology of organism load in genital Chlamydia trachomatis infection—a systematic review. The Journal of infectious diseases. 2014. Epub 2014/12/11. [DOI] [PubMed] [Google Scholar]
- 22. Agrawal T, Bhengraj AR, Vats V, Mittal A. Chlamydia trachomatis: TLR4-mediated recognition by human dendritic cells is impaired following oestradiol treatment. British journal of biomedical science. 2013;70(2):51–7. Epub 2013/07/31. . [DOI] [PubMed] [Google Scholar]
- 23. Hafner LM, Cunningham K, Beagley KW. Ovarian steroid hormones: effects on immune responses and Chlamydia trachomatis infections of the female genital tract. Mucosal immunology. 2013. 10.1038/mi.2013.46 . [DOI] [PubMed] [Google Scholar]
- 24. Wan C, Latter JL, Amirshahi A, Symonds I, Finnie J, Bowden N, et al. Progesterone activates multiple innate immune pathways in Chlamydia trachomatis-infected endocervical cells. American journal of reproductive immunology. 2014;71(2):165–77. 10.1111/aji.12168 . [DOI] [PubMed] [Google Scholar]
- 25. Gupta R, Wali S, Yu JJ, Chambers JP, Zhong G, Murthy AK, et al. In Vivo Whole Animal Body Imaging Reveals Colonization of Chlamydia muridarum to the Lower Genital Tract at Early Stages of Infection. Molecular imaging and biology: MIB: the official publication of the Academy of Molecular Imaging. 2014. 10.1007/s11307-014-0732-5 . [DOI] [PubMed] [Google Scholar]
- 26. He Q, Ananaba GA, Patrickson J, Pitts S, Yi Y, Yan F, et al. Chlamydial infection in vitamin D receptor knockout mice is more intense and prolonged than in wild-type mice. The Journal of steroid biochemistry and molecular biology. 2013;135:7–14. 10.1016/j.jsbmb.2012.11.002 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Marrazzo J. Clinical manifestations and diagnosis of Chlamydia trachomatis infections.2014 August 11, 2014.
- 28.Radcliffe K. Testing for chlamydia the "window period" 2008 [updated March 20, 2008; cited 2015 April 4]. Available from: www.bashh.org/documents/1686.pdf.
- 29.Family Planning Association. Chlamydia—Looking after your sexual health: Department of Health; 2014 [updated June 2014; cited 2015 March 26]. Available from: www.fpa.org.uk/sites/default/files/chlamydia-information-and-advice.pdf.
- 30. Geisler WM, Black CM, Bandea CI, Morrison SG. Chlamydia trachomatis OmpA genotyping as a tool for studying the natural history of genital chlamydial infection. Sexually transmitted infections. 2008;84(7):541–4; discussion 4–5. 10.1136/sti.2008.030825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Geisler WM, Lensing SY, Press CG, Hook EW 3rd. Spontaneous resolution of genital Chlamydia trachomatis infection in women and protection from reinfection. The Journal of infectious diseases. 2013;207(12):1850–6. Epub 2013/03/09. 10.1093/infdis/jit094 ; PubMed Central PMCID: PMCPmc3654745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Geisler WM, Wang C, Morrison SG, Black CM, Bandea CI, Hook EW 3rd. The natural history of untreated Chlamydia trachomatis infection in the interval between screening and returning for treatment. Sexually transmitted diseases. 2008;35(2):119–23. . [DOI] [PubMed] [Google Scholar]
- 33. Iwasaki A. Antiviral immune responses in the genital tract: clues for vaccines. Nature reviews Immunology. 2010;10(10):699–711. 10.1038/nri2836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. van Rooijen MS, van der Loeff MF, Morre SA, van Dam AP, Speksnijder AG, de Vries HJ. Spontaneous pharyngeal Chlamydia trachomatis RNA clearance. A cross-sectional study followed by a cohort study of untreated STI clinic patients in Amsterdam, The Netherlands. Sexually transmitted infections. 2015;91(3):157–64. Epub 2014/09/23. 10.1136/sextrans-2014-051633 . [DOI] [PubMed] [Google Scholar]
- 35. Russell AN, Zheng X, O'Connell CM, Taylor BD, Wiesenfeld HC, Hillier SL, et al. Analysis of Factors Driving Incident and Ascending Infection and the Role of Serum Antibody in Chlamydia trachomatis Genital Tract Infection. The Journal of infectious diseases. 2015. Epub 2015/09/09. 10.1093/infdis/jiv438 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Haggerty CL, Gottlieb SL, Taylor BD, Low N, Xu F, Ness RB. Risk of Sequelae after Chlamydia trachomatis Genital Infection in Women. Journal of Infectious Diseases. 2010;201(Supplement 2):S134–S55. 10.1086/652395 [DOI] [PubMed] [Google Scholar]
- 37. Anglemyer A, Rutherford GW, Horvath T, Baggaley RC, Egger M, Siegfried N. Antiretroviral therapy for prevention of HIV transmission in HIV-discordant couples. The Cochrane database of systematic reviews. 2013;4:Cd009153 Epub 2013/05/02. 10.1002/14651858.CD009153.pub3 ; PubMed Central PMCID: PMCPmc4026368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Chappell CA, Cohn SE. Prevention of perinatal transmission of human immunodeficiency virus. Infectious disease clinics of North America. 2014;28(4):529–47. Epub 2014/12/03. 10.1016/j.idc.2014.08.002 . [DOI] [PubMed] [Google Scholar]
- 39. Dionne-Odom J, Tita AT, Silverman NS. #38: Hepatitis B in pregnancy screening, treatment, and prevention of vertical transmission. American journal of obstetrics and gynecology. 2015. Epub 2015/10/11. 10.1016/j.ajog.2015.09.100 . [DOI] [PubMed] [Google Scholar]
- 40. Garcia-Tejedor A, Maiques-Montesinos V, Diago-Almela VJ, Pereda-Perez A, Alberola-Cunat V, Lopez-Hontangas JL, et al. Risk factors for vertical transmission of hepatitis C virus: a single center experience with 710 HCV-infected mothers. European journal of obstetrics, gynecology, and reproductive biology. 2015;194:173–7. Epub 2015/09/27. 10.1016/j.ejogrb.2015.09.009 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.