Background
Patient participation in research is crucial for advancing knowledge and improving care. Barriers to successful recruitment can potentially hinder the feasibility of conducting psycho-oncology clinical trials [1]. Age has proven to be a consistent barrier to recruitment. Although older patients make up the largest proportion of those diagnosed with cancer; they remain under-represented in clinical trials [2]. Recruitment to psycho-oncology research may also be hampered by stigma surrounding mental health care [3], as well as the discussion of research concerning sensitive topics, such as sexual health. Despite this, there is a dearth of research regarding barriers to recruitment and alternative strategies in the domain of psycho-oncology.
The current report examines recruitment data from a clinical trial of a sexual health intervention for female anal and rectal cancer survivors. Sexual function represents a complex and multifactorial construct that has been noted to deteriorate after treatment for a number of cancers, including rectal, rectosigmoid and anal cancer [4]. Sexual dysfunction is also reported to be one of the most common and distressing consequences of cancer treatment [5], and is associated with impaired quality of life [4]. A four-session educational intervention was developed entitled: Cancer Survivorship Intervention-Sexual Health (CSI-SH), to address sexual dysfunction in female rectal, rectosigmoid and anal cancer survivors and piloted at a large urban cancer center. In this brief report, study recruitment will be examined and strategies for enhancing recruitment discussed in the context of this unique, challenging and important domain of psychosocial oncology.
Methods
Eligibility Criteria
Subject inclusion criteria for CSI-SH were: being post-treatment (radiation and/or surgery for stage I–III rectal adenocarcinoma or rectosigmoid cancer with an anastomosis ≤ 15cm, radiation and/or chemotherapy for anal cancer), without current evidence of disease, ≥ 21 years of age, and proficient in English. Also, participants had to have reported moderate or lower satisfaction with their overall sexual life. Exclusion criteria included significant cognitive or psychiatric disturbance.
Research Design of Pilot Study
The current study was a randomized clinical trial using a stratified block design to examine the feasibility, tolerability, acceptability (including adherence) and efficacy of an intervention designed to improve sexual functioning among rectal and anal cancer survivors. Participants were randomly assigned to either CSI-SH or usual care. The intervention group received four one-hour individual educational sessions facilitated by trained mental health professionals targeting topics such as use of dilators, lubricants, and sensate focus. Participants chose to complete the sessions in-person or via telephone. Participants also completed questionnaires by phone or mail at three time points: baseline and four and eight months following baseline.
Recruitment Strategy
Eligible patients (determined by medical chart review and clinician consultation) were approached either in clinic or by letter recruitment. Those receiving a letter were mailed a study brochure, introductory letter, a copy of the consent form, and contacted via telephone three times within two weeks of receiving the letter. In the clinic, women were approached either in a quiet section of the waiting room or while waiting for their physician in a private clinic room. They were provided a study overview and invited to participate by a research study assistant (RSA). If the patient expressed interest she was given a pre-screen one-item questionnaire regarding satisfaction with current sexual functioning. Females reporting low to moderate satisfaction were invited to participate. Those who declined participation were asked to provide a reason for declining.
Results
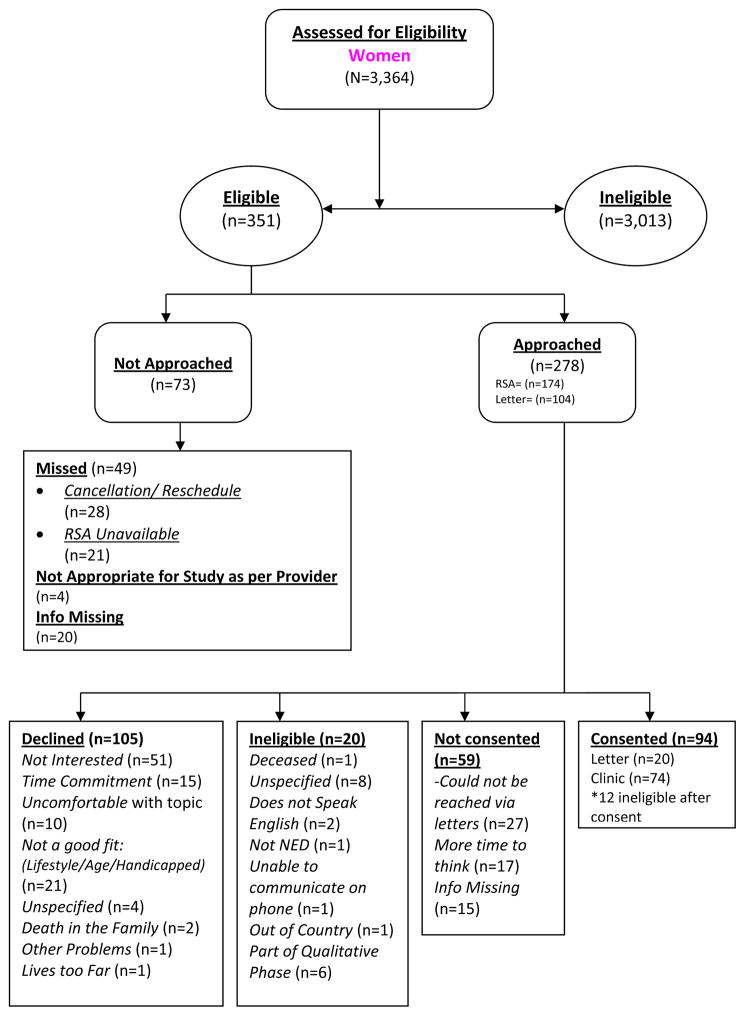
A total of 351 women were initially deemed eligible to participate across the four years of study enrolment. Of the 351 eligible participants, 73 were not approached because they were either missed in clinic or deemed inappropriate by their medical provider, thus 278 were approached either by letter recruitment (n=104, 37%) or in clinic (n=174, 63%).
Of these 278 women, 59 were not consented for various reasons (e.g. could not be reached through letter recruitment (27) or needed more time to think (32)), 20 were found ineligible, (e.g. did not speak English, resided outside of the United States, or still had evidence of disease), of which six were excluded due to prior participation in study focus groups, and105 women declined participation. The remaining 94 women (34% of the total approached) were consented (letter recruitment =20, clinic recruitment= 74) (Figure 1). Consenting women were significantly younger than those who declined (56 years (11.2) vs. 69 years (12.7), t(185) = 7.4, p<0.001)
Figure 1.
Individuals who declined participation (53% of eligible) were queried about reasons for refusal. Of the 105 women (letter recruitment =39, clinic recruitment =66), 51 (49%) were not interested in the topic, 21 (20%) felt they would not be a good fit due to lifestyle and/or age, 15 (14%) stated that they could not make the time commitment, 10 (10%) stated that they were uncomfortable with the topic, and 8 (7%) did not specify or had other reasons for not participating (e.g., death in the family).
Discussion
The current study examined recruitment data in the context of a pilot study focusing on sexual health in female rectal, rectosigmoid and anal cancer survivors. Previous research has suggested that many cancer survivors, including those with rectal, rectosigmoid and anal cancer, will experience post-treatment sexual dysfunction and may benefit from a focused intervention [6]. Despite targeted recruitment of women who reported low to moderate degree of their sexual satisfaction, 53% of the eligible individuals approached declined to participate. This rate is congruent with the findings reported by Andrykowski and Manne in a review of the effectiveness and acceptably of psychology interventions for cancer patients. They noted accrual rates of psycho-oncology studies to range between 50% – 60% or lower [7].
Also consistent with previous findings [2], age was a significant factor in recruitment, with those who chose to participate being significantly younger than those who declined (56 years vs. 69 years). The American Cancer Society notes that the risk for colorectal cancer increases with age, with 90% of individuals diagnosed over the age of 50 in 2010. [8]. Thus, alternative recruitment strategies and intervention s may need to be considered to ensure this population receives appropriate support across the cancer care continuum. Older patients may be less familiar with clinical research methodology and trial recruitment, as well as less comfortable discussing issues around sexual health. Allotting greater time to provide information and build rapport could potentially increase willingness to participate and thus increase representation of this group in clinical research.
Sexual functioning is not often discussed by heath care providers [9] and may not be raised by patients given its sensitive nature. We found that the main reason for refusal in the current study was lack of interest in research concerning sexual health. Research team members noted that when medical staff briefly mentioned the study to patients prior to being approached, or were approached in the privacy of a clinic room, they were more willing to consider participation. It is possible that these individuals were more likely perceived the discussion of their sexual health as part of their routine medical care and thus the stigma and discomfort surrounding sexual functioning and mental health were lessened. Efforts by oncology health professionals to discuss sexual health during routine visits may increase patients’ willingness to consider engaging in research to develop and test sexual health interventions in cancer.
With less than one third of clinical trials achieving their original recruitment target [10], recruitment is obviously challenging. It may be possible to enhance recruitment through a priori consideration of enrollment strategies, reasons for potential decline, the way in which sensitive topics are presented by research staff, and by including medical staff in the recruitment process. As noted, the way in which patients are approached may be important in psycho-oncology and sexual health research and deserving of consideration in study design. It is valuable to note that a significantly higher rate of women consented via clinic approach rather than letter recruitment. Letter recruitment enables passive decline of participation, in contrast to in-person recruitment strategies. Approaching patients in a clinical setting provides the opportunity to build rapport and also address potential concerns that may have served as a barrier to engagement. Thus, explicit efforts to approach patients in person and in a private environment, as well as presenting sexual health as part of comprehensive medical care, may be necessary to reduce barriers to recruitment in studies that may be stigmatized (e.g., mental health) or sensitive in nature (e.g., sexual functioning).
Recruitment to psycho-oncology trials can be challenging and may be influenced by participant and study characteristic, yet there exists a paucity of published literature regarding recruitment strategies in the context of sensitive or stigmatized research studies. Greater knowledge of participant interest and recruitment strategies could improve the feasibility of psycho-oncology clinical trials. Consistent reporting of recruitment strategies and barriers encountered could provide impetus for greater consideration of recruitment in study and protocol development, promote information sharing amongst research groups, and ultimately enhance care in this important domain of psycho-oncology.
Key Points.
Multiple barriers exist in the recruitment of participants to psychosocial research in the context of cancer, including advanced age, disease status and sensitive research topics.
Despite targeted recruitment of females expressing low to moderate satisfaction with sexual functioning, more than half (53%) of eligible individuals approached declined participation in a pilot sexual health psychosocial intervention.
Patients who refused were significantly older than those who agreed to participate. The main reason reported by women for declining study participation was lack of interest in the topic of sexual health.
Specific strategies may assist in recruiting women to psychosocial studies, particularly to those that present multiple barriers to participation (e.g. research focusing on a sensitive topic).
Greater consideration and reporting of recruitment strategies in psychosocial cancer research, particularly in fields such as sexual health, may assist in the development of more effective and targeted patient recruitment and ultimately enhance research and clinical efforts.
Acknowledgments
Support for this research was provided by a grant from the National Cancer Institute (R21 CA129195-01).
References
- 1.Barnett J, et al. Recruiting and retaining low-income, multi-ethnic women into randomized controlled trials: successful strategies and staffing. Contemp Clin Trials. 2012;33(5):925–32. doi: 10.1016/j.cct.2012.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Townsley CA, Selby R, Siu LL. Systematic review of barriers to the recruitment of older patients with cancer onto clinical trials. J Clin Oncol. 2005;23(13):3112–24. doi: 10.1200/JCO.2005.00.141. [DOI] [PubMed] [Google Scholar]
- 3.Schain Barriers to Clinical Trials: Part II: Knowledge and Attitudes of Potential Participants. Cancer. 1994;74(S9):6. doi: 10.1002/1097-0142(19941101)74:9+<2666::aid-cncr2820741814>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 4.Philip EJ, et al. Psychological Correlates of Sexual Dysfunction in Female Rectal and Anal Cancer Survivors: Analysis of Baseline Intervention Data. J Sex Med. 2013 doi: 10.1111/jsm.12152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bober SL, V, Varela S. Sexuality in adult cancer survivors: challenges and intervention. J Clin Oncol. 2012;30(30):3712–9. doi: 10.1200/JCO.2012.41.7915. [DOI] [PubMed] [Google Scholar]
- 6.Hendren SK, et al. Prevalence of Male and Female Sexual Dysfunction Is High Following Surgery for Rectal Cancer. Annals of Surgery. 2005;242(2):212–223. doi: 10.1097/01.sla.0000171299.43954.ce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Michael A, Andrykowski SLM. Are Psychological Interventions Effective and Accepted by Cancer Patients? I. Standards and Levels of Evidence. the Society of Behavioral Medicine. 2006;32(2):93–97. doi: 10.1207/s15324796abm3202_3. [DOI] [PubMed] [Google Scholar]
- 8.American Cancer Society. Cancer Facts & Figures 2014. Atlanta: American Cancer Society; 2014. Retrieved from: http://www.cancer.org/acs/groups/content/@research/documents/document/acspc-041770.pdf. [Google Scholar]
- 9.Esposito K, et al. Obesity and sexual dysfunction, male and female. Int J Impot Res. 2008;20(4):358–65. doi: 10.1038/ijir.2008.9. [DOI] [PubMed] [Google Scholar]
- 10.McDonald AM, et al. What influences recruitment to randomised controlled trials? A review of trials funded by two UK funding agencies. Trials. 2006;7:9. doi: 10.1186/1745-6215-7-9. [DOI] [PMC free article] [PubMed] [Google Scholar]