Abstract
Zoonotic diseases can be occupational hazards to people who work in close contact with animals or their carcasses. In this cross-sectional study, 190 sera were collected from butchers and slaughterhouse workers in different regions of the Sistan va Baluchestan province, in Iran in 2011. A questionnaire was filled for each participant to document personal and behavioural information. The sera were tested for detection of specific IgG antibodies against brucellosis, leptospirosis, and Q fever (phase I and II) using commercial enzyme-linked immunosorbent assays (ELISA). The seroprevalence of brucellosis was 7.9%, leptospirosis 23.4%, and phase I and II of Q fever were 18.1% and 14.4%, respectively. The seroprevalence of Q fever and leptospirosis, but not brucellosis, varied among regions within the province (p = 0.01). Additionally, a significant relationship was found between seropositivity of Q fever and camel slaughtering (p = 0.04). Reduced seropositivity rate of brucellosis was associated with use of personal protective equipment (PPE) (p = 0.004). This study shows that brucellosis, leptospirosis and Q fever occur among butchers and slaughterhouse workers in this area.
Introduction
Many zoonotic diseases and human pathogens are occupational hazards faced by individuals who come into close contact with animals or their carcasses. The probability of contact with zoonotic pathogens while working depends upon various factors, such as the health status of the animals, the type of work performed, the frequency of contact with live animals, carcasses and tissues of slaughtered animals, the use of personal and environmental protective measures, and the attitudes and levels of knowledge of the people at risk [1]. Butchers and slaughterhouse workers are at high risk of contracting zoonotic diseases. In Iran, previous studies have identified zoonoses like brucellosis, leptospirosis and Q fever as potential occupational hazards for slaughterhouse workers [2–5].
Brucellosis is an important zoonosis worldwide affecting both livestock and humans; it is listed among the top ten pathogens at the wildlife-livestock interface [6,7]. It can be transmitted to humans through direct contact with infected tissues (especially genital organs and birth products), inhalation of aerosols, and ingestion of raw milk and dairy products from infected animals [8]. Brucellosis in humans is characterized mainly by intermittent fever, with manifestations such as gastrointestinal, cardiovascular, genitourinary, hematopoietic, nervous, skeletal, pulmonary, cutaneous, and ocular involvement [9].
Leptospirosis is a wide spread zoonotic disease that also affects both humans and animals [10]. The etiological agent, Leptospira spp., can be transmitted to humans through broken skin or mucous membranes during contact with tissues, body fluids, and organs from infected animals, or by consumption of food or water contaminated with the urine of infected animals [11]. In humans, leptospirosis cause a wide range of symptoms including fever, myalgia, conjunctivitis, jaundice, kidney failure, meningitis, myocarditis, meningoencephalitis and pulmonary haemorrhage with respiratory failure, which sometimes results in death[10]. The disease is an occupational hazard for farmers, sewer workers, miners, dairy and slaughterhouse workers, and fish industry workers [11].
Q fever is also a significant zoonotic disease caused by the rickettsia-like bacterium Coxiella burnetii [12]. This disease is considered to be an occupational hazard for livestock handlers, farmers, veterinarians, and butchers and slaughterhouse workers [13]. Livestock such as cattle, sheep and goats are among the main sources of human infection. In animals, Q fever is mostly asymptomatic or subclinical [12,14]. The disease is mainly transmitted to humans through inhalation of infectious agents, consumption of unpasteurized contaminated milk and dairy products, contact with infectious tissues, and, rarely, via tick bites [15]. About 60% of people infected with Q fever are asymptomatic. The symptoms of acute Q fever in humans may include severe headache, prolonged fever, pneumonia, hepatitis, myalgia, arthralgia, cough, cardiac failure and neurological disorders [12]. Patients with chronic Q fever have symptoms such as endocarditis, vascular infection, and fatigue and have a higher likelihood of abortion and stillbirth [15]. Phase I and II antibodies are detectable in patients with chronic Q fever, but antibodies against phase II are indicative of acute Q fever [12].
As butchers and slaughterhouse workers are in close contact with animals or their body fluids and tissues they are at high risk of contracting zoonotic diseases [16]. Imports of large numbers of livestock from eastern neighbouring countries, Afghanistan and Pakistan, to the Sistan va Baluchestan province in Iran [17], and a recent report of brucellosis and Q fever outbreak in Afghanistan [18] prompted us to evaluate the seroprevalence of brucellosis, leptospirosis and Q fever among butchers and slaughterhouse workers in this province. We also evaluated the risk factors related to these diseases among these individuals.
Materials and Methods
Study area
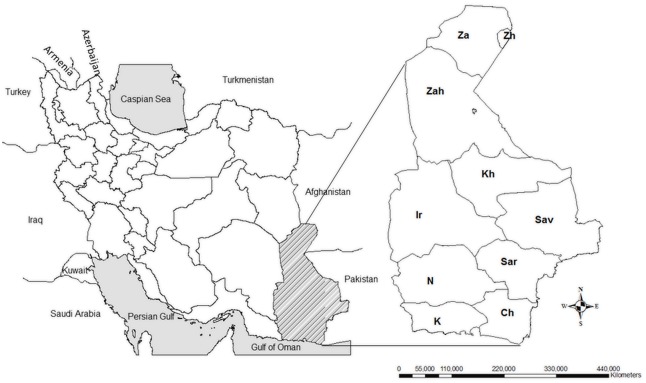
This study was carried out in the Sistan va Baluchestan province in south-eastern Iran in 2011. This province, the largest in the country, covers an area of 187,502 km2 and has a population of about 2.5 million people. Sistan va Baluchestan is bordered by the Oman Sea to the south, by Afghanistan and Pakistan in the east, by South Khorasan province to the north, and by the Kerman and Hormozgan provinces in the west (Fig 1). The climate of this province is semi-arid and experiences long, hot summers and short winters.
Fig 1. Map of Sistan va Baluchestan province in southeast Iran.
Sampling from butchers and slaughterhouse workers was performed in the different counties of Sistan va Baluchestan province including: Zahak (Zh) and Zabol (Za) in the north, Zahedan (Zah), Iranshahr (Ir) and Khash (Kh) in the centre, and Saravan (Sav), Sarbaz (Sar), Nikshahr(N), Konarak (K) and Chabahar (Ch) in the south.
Ethical considerations
The ethical committee of the Pasteur Institute of Iran approved the consent procedure, the proposal and protocol of this study, covering all the samples taken (blood), questionnaire and verbal informed consent as most of the participants were either illiterate or had a primary education.
Samples collection
In this cross-sectional study, blood samples were obtained from butchers and slaughterhouse workers after obtaining their informed consent. All official slaughterhouses in this province were recruited and participants were selected randomly among the employees. Sampling was carried out in slaughterhouses in the north, centre, and south of the province. The inclusion criteria were being over 18 and working as a butcher or slaughterhouse worker for a minimum of 6 months. Information of each participant, including demographic characteristics (age and gender), work history, exposure to risks during work, use of personal protective equipment (PPE) (including mask, gloves, overalls and boots), and their knowledge, attitude, and practices about common zoonotic diseases was collected by means of a researcher-developed questionnaire (Table 1). A 10 mL blood sample was collected from each participant after obtaining informed consent. Sera were kept at -20°C and transferred to the Department of Epidemiology of the Pasteur Institute of Iran (Tehran).
Table 1. Analysis of risk factors associated with the seroprevalence of leptospirosis, brucellosis and Q fever among butchers and slaughterhouse workers in south-eastern Iran in 2011.
| Risk factor | Leptospirosis | Brucellosis | Q fever | ||||||
|---|---|---|---|---|---|---|---|---|---|
| No. Tested (% Seropositive) | OR (95% CI) | P- value | No. Tested (% Seropositive) | OR(95% CI) | P-value | No. Tested (% Seropositive) | OR (95% CI) | P-value | |
| Age (median = 33.5) | |||||||||
| ≤33.5 years | 91(21.98) | 1.20(0.61, 2.38) | 0.60 | 93(8.6) | 0.99(0.91,1.08) | 0.78 | 93(19.4) | 1.43(0.76,2.86) | 0.31 |
| >33.5 years | 91(25.27) | 93(7.5) | 94(25.5) | ||||||
| Work History (median = 8) | |||||||||
| ≤8 years | 82(21.95) | 1.22(0.61, 2.45) | 0.58 | 105(5.7) | 2.18(0.74,6.42) | 0.14 | 102(18.6) | 1.64(.081,3.32) | 0.17 |
| >8 years | 94(25.53) | 77(11.7) | 77(27.3) | ||||||
| Work Type | |||||||||
| Slaughtering | |||||||||
| No | 13(23.08) | 1.06(0.29,4.98) | 0.97 | 14(0.0) | 1.53(0.23,35.95) | 0.61 | 14(35.7) | 0.50(0.16,1.60) | 0.32 |
| Yes | 158(24.05) | 162(9.3) | 160(21.9) | ||||||
| Transportation of the remaining livestock | |||||||||
| No | 129(26.36) | 0.56(0.21, 1.34) | 0.21 | 133(7.5) | 1.62(0.52,5.03) | 0.53 | 131(23.7) | 0.85(0.37,1.97) | 0.71 |
| Yes | 42(16.67) | 43(11.6) | 43(20.9) | ||||||
| Splashing of Animal Secretions | |||||||||
| Face | |||||||||
| No | 46(23.91) | 0.96(0.44, 2.18) | 0.91 | 47(6.4) | 1.34(0.362,4.98) | 0.99 | 47(19.1) | 1.30(0.57,2.97) | 0.53 |
| Yes | 138(23.19) | 143(8.4) | 140(23.6) | ||||||
| Body | |||||||||
| No | 36(22.22) | 1.09(0.46, 2.76) | 0.86 | 37(8.1) | 0.97(0.26,3.64) | 0.99 | 36(25.0) | 0.85(0.36,1.98) | 0.70 |
| Yes | 147(31.25) | 152(7.9) | 150(22.0) | ||||||
| Occupational Injury | |||||||||
| Cutting hand or other organs | |||||||||
| ≤5 times | 130(23.08) | 1.20(0.55,2.55) | 0.63 | 136(8.8) | 0.44(0.09,2.04) | 0.36 | 134(19.4) | 2.07(0.97,4.341) | 0.06 |
| > 5 times | 49(26.53) | 49(4.1) | 48(33.3) | ||||||
| Bite from ectoparasite | |||||||||
| ≤5 times | 175(22.85) | 1.68(0.33,7.07) | 0.48 | 181(8.3) | 1.35(0.06,9.21) | 0.92 | 178(21.3) | 2.95(0.75,11.51) | 0.12 |
| > 5 time | 9(33.33) | 9(0.0) | 9(44.4) | ||||||
| Contact with Animals | |||||||||
| Cattle | |||||||||
| No | 45(31.11) | 0.54(0.25,1.19) | 0.12 | 45(8.9) | 0.77(0.23,2.59) | 0.75 | 45(26.7) | 0.72(0.33,1.56) | 0.40 |
| Yes | 137(19.71) | 143(7.0) | 140(20.7) | ||||||
| Sheep & Goat | |||||||||
| No | 26(15.8) | 1.71(0.58,6.11) | 0.36 | 27(3.7) | 2.30(0.27,18.21) | 0.70 | 26(11.5) | 2.40(0.69,8.46) | 0.16 |
| Yes | 156(28.05) | 161(8.1) | 159(23.9) | ||||||
| Camel | |||||||||
| No | 105(21.90) | 1.09(0.53,2.20) | 0.81 | 108(8.3) | 0.73(0.24,2.28) | 0.60 | 106(17) | 2.01 (0.99,4.09) | 0.049 |
| Yes | 77(23.38) | 80(6.2) | 79(29.1) | ||||||
| All 3 group of animals | |||||||||
| No | 112(20.53) | 1.33(0.65,2.72) | 0.42 | 115(8.7) | 0.61(0.18,2.02) | 0.41 | 112(17.9) | 1.86(0.92,3.74) | 0.08 |
| Yes | 70(25.71) | 73(5.5) | 73(28.8) | ||||||
| Attitude and Practice (Personal Protection) | |||||||||
| See themselves at risk for zoonotic diseases | |||||||||
| No | 35(20.00) | 1.28(0.53,3.41) | 0.60 | 38(7.9) | 0.99(.27,3.71) | 0.99 | 37(10.8) | 0.35(.012,1.07) | 0.06 |
| Yes | 148(24.32) | 151(7.9) | 149(25.5) | ||||||
| Personal Protection (median = 12)* | |||||||||
| ≤12 | 91(26.37) | 1.41(0.71,2.84) | 0.33 | 92(2.2) | 0.14(0.03,0.64) | 0.004 | 91(25.3) | 1.41(0.70,2.83) | 0.34 |
| >12 | 91(19.78) | 95(13.7) | 93(19.4) | ||||||
*Total scores earned by each participant in the use of PPE was considered as the performance of each participant. The median of the performance for all participants was 12.
Serological tests
Detection of brucellosis antibody (IgG)
The commercial enzyme-linked immunosorbent assay (ELISA) kit (IBL, Hamburg, Germany), was used for brucellosis antibody (IgG) detection. Briefly, 1 μL of the sera was diluted 1:100, and after washing with buffer-washing, 100 μL of horseradish peroxidase-conjugated anti-human IgG was added. The mixture was incubated for 30 minutes at room temperature and then treated with tetra methyl benzidine (TMB) for 20 minutes. A Brucella antibody-antigen reaction was indicated by a blue coloration. Subsequently, a TMB stop solution was added, and the optical density (OD) of the well was measured at 450 nm by a micro plate reader (ELx808, BioTek Instruments Inc., Winooski, VT, USA). Antibody activities were calculated using a standard curve according to the manufacturer's guidelines.
The positive and borderline sera detected using the ELISA method were confirmed with the standard tube agglutination (STA) test as a gold standard test for brucellosis diagnosis. We used a locally prepared antigen and a STA test produced by the Pasteur Institute of Iran. Sera were serially diluted from 1:20 to 1:1280, mixed with the standard tube agglutination antigen and then incubated at 37°C for approximately 24 hours. Each batch of the test included a positive control and a negative control. Serum titers ≥ 1:80 were considered positive [19,20].
Detection of leptospirosis antibody (IgG)
Anti-Leptospira IgG antibodies were detected using a commercial ELISA kit (Serion/Verion Co, Germany, Kit number: ESR 125 G) according to the manufacturer's instructions. The plates were read at 405 nm using a micro plate reader (ELx808, BioTek Instruments Inc., Winooski, VT, USA). The cut-off value was calculated on the basis of the standard curve corrected by the mean of the extinction of the standard serum in accordance with the manufacturer's instructions. Quantitative analysis was evaluated for IgG antibodies. A result >30 U/mL was regarded as positive.
Detection of Coxiella burnetii antibodies (IgG I and II)
IgG antibodies against C. burnetii were detected using a commercial ELISA kit (Serion/Verion Co., Germany, Kit number ESR 1312 G) according to the manufacturer’s instructions. Phase I and II antibodies were identified in separate assays. The plates were read at 405 nm using a microplate reader (ELx808, BioTek Instruments Inc., Winooski, VT, USA). For phase I antibodies, the sample was considered positive when the serum OD was >10% above the OD cut-off value. For phase II, antibody activities in IU/mL were calculated using a standard curve which was incorporated in the kit following the manufacturer's guidelines.
Statistical analysis
The data were analysed using SPSS software (Version 16, SPSS Inc, Chicago, Ill). Chi-square, Fisher's exact and logistic regression tests were used to compare the variables during analysis. All results were considered statistically significant if the p-value was equal to or less than 0.05, and marginally significant if the p-value was between 0.05 and 0.1.
Results
In this study, 190 blood samples was taken from butchers and slaughterhouse workers residing in 11 counties of the Sistan va Baluchistan province, including Zahak and Zabol in the north, Iranshahr, Zahedan and Khash in the centre and Chabahar, Sarbaz, Saravan and Konarak in the south of the province. The median (maximum, minimum) age and work experience of participants in this study were 33.5 (18, 86) and 8 (1, 44) years, respectively. All participants were male and 96.8% of them claimed to be satisfied with their occupation. Detailed information about the all participants is shown in S1 Dataset.
In total, 162 (85.3%) participants were directly involved in animal slaughtering, 43 (22.6%) in transportation and handling of animal residues, and 2 (1.1%) only inspected the carcases. A total of 161 (84.7%) participants were in contact with sheep and goats, 143 (75.3%) with cattle including calves, and 80 (42.1%) with camels during their daily activities. Moreover 75.3% of the workers reported a history of being splashed with animal fluids and viscera more than once onto their face and 80.0% on other parts of their bodies. In addition 25.8% of all individuals had a history of cutting their hands or other parts of their bodies at least once during their work, and 17.4% recalled ectoparasite bites within the last year. The obtained data showed that 39.7% of participants did not use any PPE (masks, gloves, overalls and boots), while 22.8% always used it. Also 83.6% of participants had never applied chemical disinfectants to their knives and hands, while 79.9% knew they were at risk of zoonotic infections.
ELISA results revealed that 8.4% of participants were positive and 4.2% at borderline for anti-Brucella IgG; the seroprevalence of brucellosis among the participants was 7.9% using the standard tube agglutination test (STAT).
Furthermore, 23.4% and 15.8% of participants were positive and borderline, respectively, for anti-Leptospira IgG using ELISA.
Seroprevalence of Q fever antibodies, of phases I and II (IgG) were 18.1% and 14.4%, respectively, and 13.9% and 8.4% of participants had a borderline titre for phase I and phase II antibodies, respectively. The overall seroprevalence of Q fever (participants having antibodies of phase I and/or phase II) was 22.5%.
The highest brucellosis seroprevalence was observed in Chabahar (20.0%) and Nikshahr (20.0%), and the highest Q fever seroprevalence was in Zahak (40.0%) and Iranshahr (42.9%). Leptospirosis seroprevalence was highest in Khash (58.3%) and Zahak (40.0%). The participants from Saravan County in the south of the province had no antibodies to any of the three pathogens (Table 1).
Participants from central and northern regions were 7.26 (OR: 7.26, 95%CI: 1.64, 32.18) (p = 0.01) and 10.38 (OR: 10.38, 95%CI: 2.19, 49.13) (p = 0.003) times more likely to be seropositive, respectively, for Q fever than those from southern regions. A significant difference in leptospirosis seropositivity was seen between southern (11.4%) and central (32%) regions (OR: 3.66, 95%CI: 1.32, 10.2, p = 0.01), but no significant difference was found between southern and northern regions (OR: 2.07, 95%CI: 0.63, 6.76, p = 0.23). Brucellosis seroprevalence did not differ significantly among regions (Table 2).
Table 2. Seroprevalence of Q fever, brucellosis and leptospirosis among butchers and slaughter workers in Sistan va Baluchestan province according to region and city.
| Leptospirosis | Brucellosis | Q fever | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Region/ County | No tested (% infected) | OR (95% CI) | P value | No. Tested (% infected) | OR (95% CI) | P value | No. Tested (% infected) | OR (95% CI) | P value |
| North | 43(20.9) | 2.07(0.63, 6.76) | 0.23 | 44(0.0) | ND* | 0.999 | 43(32.6) | 10.38(2.19, 49.13) | 0.003 |
| Zahak | 5(40.0) | 5(0.0) | 5(40.0) | ||||||
| Zabol | 38(18.4) | 39(0.0) | 38(31.6) | ||||||
| Centre | 97(32.0) | 3.66(1.32, 10.20) | 0.01 | 100(11.0) | 1.3(0.39, 4.32) | 0.67 | 99(25.3) | 7.26 (1.64, 32.18) | 0.01 |
| Iranshahr | 13(23.1) | 14(7.1) | 14(42.9) | ||||||
| Zahedan | 72(28.2) | 74(12.2) | 73(23.3) | ||||||
| Khash | 12(58.3) | 12(8.3) | 12(25.0) | ||||||
| South | 44(11.4) | Reference group | 46(8.7) | Reference group | 45(6.7) | Reference group | |||
| Chabahar | 10(0.0) | 10(20.0) | 10(0.0) | ||||||
| Sarbaz | 6(16.7) | 6(0.0) | 5(0.0) | ||||||
| Konarak | 10(10.0) | 10(0.0) | 10(10.0) | ||||||
| Saravan | 10(0.0) | 10(0.0) | 10(0.0) | ||||||
| Nikshahr | 8(12.5) | 10(20.0) | 10(20.0) | ||||||
| Total | 184(23.4) | 190(7.9) | 187(22.5) | ||||||
* ND: Not Defined
There were no associations between the age of the investigated persons and the seroprevalence rates of leptospirosis, Q fever or brucellosis. There was, however, a significant association between seroprevalence of Q fever and camels slaughtering (p = 0.05, OR: 2.01, 95%CI: 0.99, 4.09). The use of PPE was negatively associated with the seroprevalence of brucellosis (p = 0.004, OR: 0.14, 95% CI: 0.03, 0.64). A marginally significant positive correlation was found between seroprevalence of Q fever and having a history of cutting hands (p = 0.06, OR: 2.07, 95% CI: 0.97, 4.34) and the attitude of the workers (considering themselves at risk of zoonotic disease, because of their job: p = 0.06, OR: 0.35, 95% CI: 0.12, 1.07; Table 1).
Variables such as work history, work type, splashing of animal secretions on face or body and occupational injury were not significantly associated with seroprevalence rates of leptospirosis, brucellosis or Q fever.
Discussion
In this study we obtained the seroprevalence of antibodies to three zoonotic bacterial diseases among slaughterhouse workers and butchers in the Sistan va Baluchestan province in south-eastern Iran.
Brucellosis is an endemic disease in Iran and has been reported from different parts of the country [21]. In our study, the seroprevalence of brucellosis among butchers and slaughterhouse workers was 7.9%. Different similar studies were conducted among slaughterhouse workers and general population [2, 4, 22–27]. This rate was lower than those obtained from similar studies conducted on butchers and slaughterhouse workers from Khorasan Razavi province in the northeast of Iran (48%) [25], Kerman city in the south of Iran (58.6%) [4], Saudi Arabia (35%) [27], India (25.5%) [28], Pakistan (22%) and (21.7%) [29, 30], and Tanzania (19.5%) [6] and was higher than what was reported from Brazil (4.2%) [31], and South Korea (0.8%) [32] (Table 3). Collectively, these studies indicate that butchers and slaughterhouse workers might face different levels of risk to zoonotic infectious diseases in different areas, possibly due to variation in infection rates among animals, differences in human lifestyle and use of PPE. Taken together, working in a slaughterhouse in Iran seems to be a risk factor for contracting brucellosis, which is further supported by a previous screening among blood donors in the general population in the Bushehr province, southern Iran, that estimated brucellosis seroprevalence to 0.057% [26].
Table 3. The comparison of the seroprevalence surveys of brucellosis, leptospirosis and Q fever carried out in different areas among butchers and slaughter workers.
| Studies Disease | Region | Number of tested | Seropositivity (%) | P-value | OR (%95 CI) | Ref. |
|---|---|---|---|---|---|---|
| Brucellosis | This study | 190 | 7.9 | Ref. | ||
| Iran: Gilan | 186 | 9.8 | 0.54 | 0.8 (0.38, 1.65) | [22] | |
| Iran: Shiraz | 250 | 11.7 | 0.20 | 0.65 (0.33, 1.25) | [23] | |
| Iran: Kurdistan | 50 | 12 | 0.37 | 0.63 (0.23, 1.86) | [2] | |
| Iran: Urmia | 154 | 13 | 0.13 | 0.57 (0.28, 1.17) | [24] | |
| Iran: Khorasan Razavi | 250 | 48 | <0.001 | 0.9 (0.05, 0.16) | [25] | |
| Iran: Kerman | 75 | 58.6 | <0.001 | 0.06 (0.03, 0.12) | [4] | |
| South-Korea | 1482 | 0.8 | <0.001 | 10.47 (4.79, 23.29) | [32] | |
| Brazil | 551 | 4.2 | 0.06 | 1.97 (0.98, 3.85) | [31] | |
| Tanzania | 41 | 19.5 | 0.04 | 0.36 (0.14, 0.95) | [6] | |
| Pakistan | 260 | 21.7 | <0.001 | 0.31 (0.17, 0.55) | [30] | |
| Pakistan | 251 | 22 | <0.001 | 0.31 (0.16, 0.55) | [29] | |
| India | 165 | 25.5 | <0.001 | 0.3 (0.15, 0.56) | [28] | |
| Saudi Arabia | 269 | 35 | <0.001 | 0.16 (0.19, 0.28) | [27] | |
| Leptospirosis | This study | 184 | 23.4 | Ref. | ||
| Iran: Khoy | 30 | 13 | 0.22 | 1.98 (0.69, 6.96) | [36] | |
| Iran: Zanjan | 98 | 34.7 | 0.02 | 0.57 (0.33, 0.98) | [5] | |
| Iran: Tehran | 120 | 58 | <0.001 | 0.23 (0.14, 0.37) | [37] | |
| Brazil | 150 | 4 | <0.001 | 7.28 (3.15, 19.38) | [38] | |
| Mexico | 292 | 8.2 | <0.001 | 3.97 (1.99, 3.90) | [39] | |
| New Zealand | 567 | 11 | <0.001 | 2.48 (1.60, 3.82) | [40] | |
| India | 20 | 30 | 0.25 | 0.71 (0.26, 2.13) | [41] | |
| Q Fever | This study | 187 | 22.5 | Ref. | ||
| Iran: Kurdistan | 50 | 38 | 0.03 | 0.47 (0.24, 0.93) | [2] | |
| Iran: Kerman | 75 | 68 | <0.001 | 0.14 (0.07, 0.25) | [3] | |
| Brazil | 144 | 29 | 0.17 | 0.70 (0.43, 1.16) | [51] | |
| Turkey | 118 | 50.9 | <0.001 | 0.28 (0.17, 0.46) | [52] |
In the present study, 22.8% of participants always used PPE (masks, gloves, overalls and boots) and use of PPE was found to be a protective factor against brucellosis, similar to other studies [6,32]. The accidental splashing of blood and other fluids of infected animals in the vicinity of the mouth and/or injured parts of the body increases the exposure of slaughterhouse workers and butchers to Brucella [32]. Previously identified risk factors for the acquisition of brucellosis in Iran include the consumption of fresh cheese, contact with animal skins and consuming undercooked meat or raw milk [33]. Brucellosis is also an occupational hazard for certain professions in health settings, such as veterinary and laboratory personnel’s [33].
The environment and the socioeconomic conditions along the Caspian Sea littoral zone in the north of Iran are more favourable for the survival and transmission of Leptospira spp. spirochetes than in other areas of Iran [34,35]. The dry and desert climates in the Sistan va Baluchestan are believed to be less suitable for environmental survival of Leptospira spp. spirochetes. This disease can be transmitted to people coming into close contact with animals. Different studies were conducted among slaughterhouse workers and butchers in Iran [5, 36–38]. In our study, the seroprevalence of leptospirosis was 23.4% among butchers and slaughterhouse workers in the province. In other studies carried out on butchers and slaughterhouse workers in Iran, the seroprevalence of leptospirosis was higher in Zanjan province (northwest of Iran)) 34.7% ([5] and in Tehran province (northern Iran)) 58% ([37]. However, in similar studies in other countries, the seroprevalence of leptospirosis was lower than this study: Brazil (4%) [38], Mexico (8.2%) [39] and New Zealand (11%) [40] (Table 3). The comparatively high seropositivity rate in this study is interesting, as no human leptospirosis case has been reported from Sistan va Baluchestan and that none of the seropositive individuals in this study had clinical symptoms registered in their medical history. However, this disease has been reported from South Khorasan and Afghanistan which share borders with Sistan va Baluchestan [42,43]. A study in Pakistan in 2010–2011 revealed a 44% seropositivity rate among veterinarians, pet-owners and livestock holders [44].
The last human case of Q fever in Iran was reported in 1973 [45]. Recently, this infection was reported in livestock in different regions of the country [46–48], and anti-C. burnetii antibodies were detected in febrile patients in the Kerman province, west of Sistan va Baluchestan [49]. It is known that antibodies against antigens of phase I and II persist for months or years after primary infection. Since the clinical diagnosis is difficult, in most cases, diagnosis of Q fever depends on serological tests [50]. In our study, the seroprevalence rate of phase I and II antibodies in butchers and slaughterhouse workers of Sistan va Baluchestan were 18.1% and 14.4%, respectively.
In other studies carried out on butchers and slaughterhouse workers, the seroprevalence of phase I and II IgG antibodies for Q fever was higher in Kurdistan province, western Iran (38%) [2], Kerman province, south-eastern Iran (68%) [3], Brazil (29%) [51] and Turkey (50.9%) [52] (Table 3). In the present study, the seropositivity of Q fever among butchers and slaughterhouse workers in the central and northern regions of Sistan va Baluchestan was significantly higher than the southern regions of the province, which may be related to the recent human outbreak of Q fever in Afghanistan (Bamyan province in 2011) [18], and/or to larger livestock population in this region and high number of animals imported from Afghanistan. In this study, we observed an association between Q fever seropositivity and camel slaughtering, a finding which is in agreement with other studies reporting Q fever infection in camels in south-eastern Iran [14,53]. Also, in a study in Chad, Africa, camel breeding was a significantly associated with Q fever seropositivity [54].
Apart from occupation, other factors like access to safe water supplies and basic sanitation can contribute to infection risk. The risk of these three bacterial zoonotic diseases to butchers and slaughterhouse workers could have been evaluated more precisely if we had included the general population sera as a control group, which unfortunately was not feasible at the time of the study. Another, drawback was lack of access to the gold standard tests for confirmation of leptospirosis and Q fever.
The current study provided some valuable information on health status of butchers and slaughterhouse workers from south-eastern Iran, which can be useful for health policy makers in their future planning.
Supporting Information
(XLSX)
Acknowledgments
We like to express our gratitude to Dr Behzad Esfandiari, from Pasteur institute of Iran, and the staff of Zahedan and Zabol University of Medical Sciences for their help in sampling and Ms Manijeh Yousefi Behzadi, who assisted us in data entry.
Data Availability
All relevant data are within the paper and its Supporting Information file.
Funding Statement
The authors appreciate the financial support of the Centre for Disease Control and Prevention of the Iranian Ministry of Health; this work was approved by the Pasteur Institute of Iran (Session No.508). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Battelli G. Zoonoses as occupational diseases. Veterinaria Italiana. 2008; 44: 601–609. [PubMed] [Google Scholar]
- 2.Esmaeili S, Pourhossein B, Gouya MM, Amiri FB, Mostafavi E. Seroepidemiological Survey of Q Fever and Brucellosis in Kurdistan province, Western Iran. 2014; Vector-Borne and Zoonotic Diseases 14: 41–44. 10.1089/vbz.2013.1379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khalili M, Mosavi M, Diali HG, Mirza HN. Serologic survey for Coxiella burnetii phase II antibodies among slaughterhouse workers in Kerman, southeast of Iran. Asian Pacific Journal of Tropical Biomedicine. 2014; 4: S209–S212. 10.12980/APJTB.4.2014C1268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khalili M, Sami M, Aflatoonian MR, Shahabi-Nejad N. Seroprevalence of brucellosis in slaughterhouse workers in Kerman city, Iran. Asian Pacific Journal of Tropical Disease. 2012; 2: 448–450. [Google Scholar]
- 5.Majd NS, Darian EK, Khaki P, Bidhendi SM, Yahaghi E, Mirnejad R. Epidemiological patterns of Leptospira spp. among slaughterhouse workers in Zanjan–Iran. Asian Pacific Journal of Tropical Disease. 2012; 2: 550–552. [Google Scholar]
- 6.Swai E, Schoonman L. Human brucellosis: seroprevalence and risk factors related to high risk occupational groups in Tanga Municipality, Tanzania. Zoonoses and Public Health. 2009; 56: 183–187. 10.1111/j.1863-2378.2008.01175.x [DOI] [PubMed] [Google Scholar]
- 7.Wiethoelter AK, Beltrán-Alcrudo D, Kock R, Mor SM. Global trends in infectious diseases at the wildlife–livestock interface. Proceedings of the National Academy of Sciences. 2015; 112: 9662–9667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Franco MP, Mulder M, Gilman RH, Smits HL. Human brucellosis. The Lancet Infectious Diseases. 2007; 7: 775–786. [DOI] [PubMed] [Google Scholar]
- 9.Aygen B, Doğanay M, Sümerkan B, Yildiz O, Kayabaş Ü. Clinical manifestations, complications and treatment of brucellosis: a retrospective evaluation of 480 patients. Medecine et Maladies Infectieuses. 2002; 32: 485–493. [Google Scholar]
- 10.Bharti AR, Nally JE, Ricaldi JN, Matthias MA, Diaz MM, Lovett MA, et al. Leptospirosis: a zoonotic disease of global importance. The Lancet Infectious Diseases 2003; 3: 757–771. [DOI] [PubMed] [Google Scholar]
- 11.Adler B, De La Pena Moctezuma A. Leptospira and leptospirosis. Veterinary Microbiology. 2010; 140: 287–296. 10.1016/j.vetmic.2009.03.012 [DOI] [PubMed] [Google Scholar]
- 12.Angelakis E, Raoult D. Q fever. Veterinary Microbiology. 2010; 140: 297–309. 10.1016/j.vetmic.2009.07.016 [DOI] [PubMed] [Google Scholar]
- 13.Van den Brom R, Vellema P. Q fever outbreaks in small ruminants and people in the Netherlands. Small Ruminant Research. 2009; 86: 74–79. [Google Scholar]
- 14.Doosti A, Arshi A, Sadeghi M. Investigation of Coxiella burnetii in Iranian camels. Comparative Clinical Pathology. 2014; 23(1): 43–46. [Google Scholar]
- 15.Angelakis E, Raoult D. Emergence of Q fever. Iranian Journal of Public Health. 2011; 40: 1–18. [PMC free article] [PubMed] [Google Scholar]
- 16.Omokhodion FO, Adebayo A. Occupational hazards and self-reported health problems of butchers in Ibadan, southwest Nigeria. Journal of Public Health. 2013; 21(2): 131–134. [Google Scholar]
- 17.Alavi-Naini R, Moghtaderi A, Koohpayeh HR, Sharifi-Mood B, Naderi M, Metanat M, et al. Crimean-Congo hemorrhagic fever in Southeast of Iran. Journal of Infection. 2006; 52: 378–382. [DOI] [PubMed] [Google Scholar]
- 18.Saeed K, Ansari J, Asghar R, Ahadi J. Concurrent brucellosis and Q fever infection: A case control study in Bamyan province, Afghanistan in 2011. International Journal of Infectious Diseases. 2012; 16(1): e37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Amini B, Baghchesaraie H, Jelodar DT. Seroprevalence of Brucella antibody titer in rural population of Abhar, Iran. Archives of Clinical Infectious Diseases 2010; 5: 152–155. [Google Scholar]
- 20.Roushan MRH, Amiri MJS, Laly A, Mostafazadeh A, Bijani A. Follow-up standard agglutination and 2-mercaptoethanol tests in 175 clinically cured cases of human brucellosis. International Journal of Infectious Diseases. 2010; 14: e250–e253. [DOI] [PubMed] [Google Scholar]
- 21.Mostafavi E, Asmand M. Trends of brucellosis (malta fever) in Iran during the period 1991–2008. Journal of Epidemiology and Community Health. 2011; 65: A136–A137. [Google Scholar]
- 22.Nikokar I, Hosseinpour M, Asmar M. Seroprevalence of Brucellosis among high risk individuals in Guilan, Iran. Journal of Research in Medical Sciences: The Official Journal of Isfahan University of Medical Sciences. 2011; 16: 1366–1371. [PMC free article] [PubMed] [Google Scholar]
- 23.Karimi A, Alborzi A, Rasooli M, Kadivar M, Nateghian A. Prevalence of antibody to Brucella species in butchers, slaughterers and others. East Mediterr Health Journal. 2003; 9: 178–184. [PubMed] [Google Scholar]
- 24.Taravati M, Salari S, Khalili F, Kheiri A. Seroepidemiogical study of brucellosis among slaughter house, veterinary staff in Urmia. Urmia Medical Journal. 2007; 18: 459–450 [Google Scholar]
- 25.Parizadeh SMJ, Seyednozadi M, Erfanian MR, Nezhad MA. A Survey on Antibody Levels among Individuals at Risk of Brucellosis in Khorasan Razavi province, Iran. Pakistan Journal of Nutrition. 2009; 8: 139–144. [Google Scholar]
- 26.Rabbani Khorasgani M, Esmaeili H, Pourkarim M, Mankhian A, Zahraei Salehi T. Anti-Brucella antibodies in blood donors in Boushehr, Iran. Comparative Clinical Pathology 2008; 17: 267–269. [Google Scholar]
- 27.Al-Sekait MA. Seroepidemiological survey of brucellosis antibodies in Saudi Arabia. Annals of Saudi Medicine. 1999; 19: 219–222. [DOI] [PubMed] [Google Scholar]
- 28.Barbuddhe S, Kumar P, Malika S, Singh D, Gupta L. Seropositivity for intracellular bacterial infections among abattoir associated personnels. The Journal of Communicable Diseases. 2000; 32: 295–299. [PubMed] [Google Scholar]
- 29.Mukhtar F. Brucellosis in a high risk occupational group: seroprevalence and analysis of risk factors. JPMA-Journal of the Pakistan Medical Association. 2010; 60: 1031–1034. [PubMed] [Google Scholar]
- 30.Mukhtar F, Kokab F. Brucella serology in abattoir workers. Journal of Ayub Medical College Abbottabad. 2008; 20: 57–61. [PubMed] [Google Scholar]
- 31.Ramos TRR, Pinheiro JW Junior, Moura Sobrinho PA, Santana VLA, Guerra NR, Melo LEH, et al. Epidemiological aspects of an infection by Brucella abortus in risk occupational groups in the microregion of Araguaína, Tocantins. Brazilian Journal of Infectious Diseases. 2008; 12: 133–138. [DOI] [PubMed] [Google Scholar]
- 32.Yoo SJ, Choi YS, Lim HS, Lee K, Park MY, Chu C, et al. Seroprevalence and risk factors of brucellosis among slaughterhouse workers in Korea. Journal of Preventive Medicine and Public Health. 2009; 42: 237–242. 10.3961/jpmph.2009.42.4.237 [DOI] [PubMed] [Google Scholar]
- 33.Alavi SM, Motlagh ME. A review of epidemiology, diagnosis and management of brucellosis for general physicians working in the Iranian health network. Jundishapur Journal of Microbiology. 2012; 5(2): 384–387. [Google Scholar]
- 34.Honarmand H, Eshraghi S, Khorramizadeh M, Hartskeerl R, Ghanaei F, Abdolahpour GR, et al. Distribution of Human Leptospirosis in Guilan province, Northern Iran. Iranian Journal of Public Health. 2007; 36(1): 68–72. [Google Scholar]
- 35.Zakeri S, Sepahian N, Afsharpad M, Esfandiari B, Ziapour P, Dinparast-jadid N. Molecular epidemiology of leptospirosis in northern Iran by nested polymerase chain reaction/restriction fragment length polymorphism and sequencing methods. The American journal of Tropical Medicine and Hygiene. 2010; 82: 899–903. 10.4269/ajtmh.2010.09-0721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Imandar M, Hassanpour A, Asgarlou S, Abdollahpour G, Sadeghi Z, Khakpoor M. Seroprevalence of leptospirosis in industrial livestock slaughterhouse workers in Khoy City. Scientific Journal of Kurdistan University of Medical Sciences. 2011; 16: 77–85. [Google Scholar]
- 37.Vande-yousefi J, Moradi BidHendi S, Aarabi A, Adeli M, Charkhkar S. Serological study of Leptospirosis in humans and livestock. Third National congress of diseases transmitted between humans and animals. 1997: 59–60.
- 38.Gonçalves DD, Teles PS, Reis CRd, Lopes FMR, Freire RL, Navarro IT, et al. Seroepidemiology and occupational and environmental variables for leptospirosis, brucellosis and toxoplasmosis in slaughterhouse workers in the Paraná State, Brazil. Revista do Instituto de Medicina Tropical de São Paulo. 2006; 48: 135–140. [DOI] [PubMed] [Google Scholar]
- 39.Rodríguez-Parra ME, Bocanegra-Alonso A, Casar-Solares A, Acosta-González RI, Cruz-Hernández N, Flores-Gutiérrez GH, et al. Epidemiological patterns of Leptospira interrogans among slaughterhouse workers from the Eastern United States-Mexico border region. African Journal of Microbiology Research. 2012; 6: 1584–1590. [Google Scholar]
- 40.Dreyfus A, Benschop J, Collins-Emerson J, Wilson P, Baker MG, Heuer C. Sero-prevalence and risk factors for leptospirosis in abattoir workers in New Zealand. International journal of Environmental Research and Public Health. 2014; 11: 1756–1775. 10.3390/ijerph110201756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sharma S, Vijaiachari P, Sugunan AP, Natrajaseenivasan K, Sehgal SC. Seroprevalence of leptospirosis among high-risk population of Andaman Islands, India. The American Journal of Tropical Medicine and Hygiene. 2006;74: 278–283. [PubMed] [Google Scholar]
- 42.Sakhaee E. Detection of Leptospiral antibodies by microscopic agglutination test in north–east of Iran. Asian Pacific Journal of Tropical Biomedicine 2011; 1: 227–229. 10.1016/S2221-1691(11)60032-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wallace MR, Hale BR, Utz GC, Olson PE, Earhart KC, Thornton SA, et al. Endemic infectious diseases of Afghanistan. Clinical Infectious Diseases. 2002; 34: S171–S207. [DOI] [PubMed] [Google Scholar]
- 44.Saleem MH, Khan MS, Durrani AZ, Hassan A, Ijaz M, Ali MM, et al. Leptospirosis: An Emerging Zoonosis in Pakistan. Pakistan Journal of Zoology. 2013; 45(4): 909–912. [Google Scholar]
- 45.Mostafavi E, Rastad H, Khalili M. Q Fever: An Emerging Public Health Concern in Iran. Asian Journal of Epidemiology. 2012; 45(3): 66–74. [Google Scholar]
- 46.Khalili M, Sakhaee E. An update on a serologic survey of Q fever in domestic animals in Iran. The American journal of tropical medicine and hygiene 2009; 80: 1031–1032. [PubMed] [Google Scholar]
- 47.Esmaeili S, Mostafavi E, Shahdordizadeh M, Mahmoudi H. A seroepidemiological survey of Q fever among sheep in Mazandaran province, northern Iran. Annals of Agricultural and Environmental Medicine. 2013; 20: 708–710. [PubMed] [Google Scholar]
- 48.Esmaeili S, Bagheri Amiri F, Mostafavi E. Seroprevalence Survey of Q Fever among Sheep in Northwestern Iran. Vector-Borne and Zoonotic Diseases. 2014; 14: 189–192. 10.1089/vbz.2013.1382 [DOI] [PubMed] [Google Scholar]
- 49.Khalili M, Shahabi-Nejad N, Golchin M. Q fever serology in febrile patients in southeast Iran. Transactions of the Royal Society of Tropical Medicine and Hygiene. 2010; 104: 623–624. 10.1016/j.trstmh.2010.04.002 [DOI] [PubMed] [Google Scholar]
- 50.Missailidis S, Godoy D, Mares-Guia M, Favacho A, Lemos E (2014) Current and Future Trends in the Clinical Diagnosis of Rickettsioses Sensu Lato. International Journal of Tropical DiseaseIS & Health 4: 147–181. [Google Scholar]
- 51.RiemannI HP, Brant PC, Behyber DE, Franti CE. Toxoplasma gondii and Coxiella burneti antibodies among Brazilian slaughterhouse employees. American Journal of Epidemiology. 1975; 102: 386–393. [DOI] [PubMed] [Google Scholar]
- 52.Berktas M, Ceylan E, Yaman G, Çiftci H. Seroprevalence of Coxiella burnetii Antibodies in High Risk Groups in Eastern Turkey. Turkiye Klinikleri Journal of Medical Sciences 2011; 31: 45–50. [Google Scholar]
- 53.Rahimi E, Ameri M, Karim G, Doosti A. Prevalence of Coxiella burnetii in Bulk Milk Samples from Dairy Bovine, Ovine, Caprine, and Camel Herds in Iran as Determined by Polymerase Chain Reaction. Foodborne Pathogens and Disease. 2011; 8: 307–310. 10.1089/fpd.2010.0684 [DOI] [PubMed] [Google Scholar]
- 54.Schelling E, Diguimbaye C, Daoud S, Nicolet J, Boerlin P, et al. Brucellosis and Q-fever seroprevalences of nomadic pastoralists and their livestock in Chad. Preventive Veterinary Medicine. 2003; 61: 279–293. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information file.