Abstract
Chlamydia trachomatis causes a predominantly asymptomatic, but generally inflammatory, genital infection that is associated with an increased risk for HIV acquisition. Endocervical epithelial cells provide the major niche for this obligate intracellular bacterium in women, and the endocervix is also a tissue in which HIV transmission can occur. The mechanism by which CT infection enhances HIV susceptibility at this site, however, is not well understood. Utilizing the A2EN immortalized endocervical epithelial cell line grown on cell culture inserts, we evaluated the direct role that CT-infected epithelial cells play in facilitating HIV transmission events. We determined that CT infection significantly enhanced the apical-to-basolateral migration of cell-associated, but not cell-free, HIVBaL, a CCR5-tropic strain of virus, across the endocervical epithelial barrier. We also established that basolateral supernatants from CT-infected A2EN cells significantly enhanced HIV replication in peripheral mononuclear cells and a CCR5+ T cell line. These results suggest that CT infection of endocervical epithelial cells could facilitate both HIV crossing the mucosal barrier and subsequent infection or replication in underlying target cells. Our studies provide a mechanism by which this common STI could potentially promote the establishment of founder virus populations and the maintenance of local HIV reservoirs in the endocervix. Development of an HIV/STI co-infection model also provides a tool to further explore the role of other sexually transmitted infections in enhancing HIV acquisition.
Introduction
Women aged 15–24 account for approximately 22% of new human immunodeficiency virus (HIV) infections [1], and heterosexual intercourse is the most common route of transmission in this group [2]. Young women < 25 years of age also have the highest prevalence of Chlamydia trachomatis (CT), a sexually transmitted bacterium that can cause adverse reproductive sequelae [3, 4] and is associated with an increased risk of HIV acquisition and increased viral shedding in the female reproductive tract (FRT) of HIV-infected women [5, 6]. CT serovars D-K are obligate intracellular pathogens that infect the columnar epithelial cells of the urogenital tract, and the endocervix is the primary site of infection in women [7]. The endocervix is also a permissive site for sexually transmitted HIV entry [8, 9], suggesting this is a major locale for interactions between the two pathogens. Understanding the mechanisms by which CT could enhance early events in HIV acquisition and replication in target cells at this site would facilitate the design of targeted prevention and intervention strategies to decrease the morbidity associated with both of these pathogens.
CT is the leading bacterial STI in the US and worldwide [4, 10–13], and it has been termed a ‘silent epidemic,’ as it is asymptomatic in >80% of women [14–18]. Asymptomatic women can still display clinical signs of inflammation with one third of patients exhibiting cervicitis upon examination [3, 7]. Chlamydiae can also ascend into the upper reproductive tract where chronic infection can lead to silent or symptomatic inflammation resulting in pelvic inflammatory disease (PID), tubal factor infertility, or ectopic pregnancy. CT undergoes a unique, biphasic developmental cycle that generally modulates between two morphological forms. Extracellular, infectious elementary bodies (EB) attach to epithelial cells, after which they are internalized into a membrane bound vesicle called an inclusion. EBs then differentiate into metabolically active, non-infectious, reticulate bodies (RBs) that undergo binary fission, followed by secondary differentiation into EBs, and are released upon host cell lysis or extrusion [19]. Alternatively, upon nutrient deprivation or stress stimuli, RBs may enter into viable, non-cultivable forms termed persistent bodies (PBs) that can reactivate after the stressor is removed [3, 20–23]. The ability to enter into a persistent state, and other well-documented evasion strategies utilized by the bacteria support natural history studies that indicate CT infections typically last for many months without treatment [3, 20, 24–26]. Further, the natural immunity that is generated in most young women is typically transient, and, therefore, re-infection is common [27, 28]. While routine screening and antibiotic treatment are relatively successful public health strategies that have led to decreased rates of PID in developed countries, many women of low socioeconomic means do not have access to appropriate care, reflecting the necessity for preventative approaches, such as microbicides or a vaccine. Taken together, the chronic, asymptomatic, yet inflammatory, characteristics of clinical chlamydial infections make it likely that CT-infected women would become infected with secondary sexually transmitted pathogens, such as HIV.
The mechanism by which CT infection could enhance HIV acquisition in the FRT has been relatively unexplored. We previously hypothesized that epithelial cells, the primary niche for CT and likely the first cells encountered by luminal HIV in the endocervix, may be central to viral transmission [29]. Potential mechanisms by which CT-infected epithelial cells and their secreted immune mediators could facilitate early HIV transmission events include, but are not limited to: i) disruption of the single columnar endocervical epithelial barrier, facilitating paracellular HIV migration and access to underlying susceptible target cells; ii) enhancement of transcellular HIV migration, also facilitating viral access to underlying susceptible leukocytes; iii) initiation or maintenance of the characteristic influx of activated, CCR5+CD4+ T lymphocytes, the major HIV target cells, observed in the endocervix of CT-infected patients [30, 31], and iv) enhancement of HIV replication in target cells at the site. To address some of these potential mechanisms in vitro, we utilized an endocervical epithelial cell line (A2EN) that is easily infected to greater than a 95% infection rate with CT when grown on cell culture inserts [32, 33]. We then used this model to determine whether cell-free or cell-associated HIV could migrate across the CT-infected epithelial barrier and whether CT-infected epithelial cells might play a role in facilitating HIV infection of CCR5+ CD4+ target cells that are present in the submucosa of the endocervix.
Materials and Methods
Cells
The A2EN human epithelial cell line was generated in our laboratory from primary endocervical epithelial cells and maintained in Keratinocyte Serum Free Medium (KSFM) supplemented with L-glutamine, calcium, bovine pituitary extract, and epidermal growth factor (Life Technologies, Carlsbad, CA) as previously described [33, 34]. The CCR5+ MT4-R5 T cell line was kindly provided by Dr. James Robinson (Tulane Medical School) and maintained in R10: RPMI1640 containing 10% fetal bovine serum (FBS) and L-glutamine supplemented with 1 μg/ml of puromycin (Invivogen, San Diego, CA) [35]. PM-1 cells [36] and J1.1 Jurkat cells chronically infected with HIVLAV [37] were obtained from the NIH AIDS Reagent Program (ARP) and cultured in R10. TZM-bl cells [38], from the ARP, were maintained in DMEM containing 10% FBS and L-glutamine. Peripheral blood mononuclear cells (PBMC) were isolated from whole heparinized blood (collected from normal donors using an IRB-approved protocol) by density gradient centrifugation on Lymphocyte Separation Medium (MP Biomedicals, Santa Ana, CA). Activated PBMC were generated by stimulating cells with 2.5μg/ml phytohemagglutinin (PHA; Sigma) for 2 d. Both resting and activated PBMC were cultured in RPMI1640 containing 20% FBS, HEPES, penicillin, streptomycin, and L-glutamine (referred to as R20) supplemented with 20 U/ml recombinant human IL-2 (Roche, Basel, Switzerland).
Virus
The HIVBaL strain [39, 40] was obtained from the ARP. Viral stocks were produced by passaging the virus in either PM-1 cells in R10 or in PHA-activated PBMC in R20 with IL-2. Virus-containing culture medium was harvested at 3 d intervals and clarified by centrifugation (250xg for 10 min) and 0.22μm filtration using a Steriflip apparatus (EMD Millipore, Billerica, MA). The virus was then aliquoted and stored at -80°C. For each stock, the 50% tissue culture infectious dose (TCID50) per ml was determined by endpoint titration using TZM-bl cells as described [41]. The HIVBaL passaged in PBMC was used in experiments testing cell-free virus migration as well as testing the effects of CT-infected A2EN cell culture supernatants on HIV infection of PBMC. The PM-1-derived HIVBaL stock was used in all other assays.
A2EN cell culture on membrane inserts and CT infection
A2EN cells were cultured on 0.4μm pore size polyester Corning Transwell® permeable membrane supports (Corning, NY) and used when their transepithelial electrical resistance (TEERs) exceeded 1000Ω/cm2 [33, 42, 43]. Additional wells of A2EN cells grown on cell culture inserts were always seeded in parallel to confirm that monolayers were also impermeable to small molecules using 3kD or 10kD Dextran-conjugated FITC (Sigma, St. Louis, MO) [44–46]. A2EN cells on cell culture inserts were infected with Chlamydia trachomatis serovar D (D/UW3/Cx) at an MOI of 3, which yielded a >95% infection rate that could be visualized using fluorescent microscopy, as previously described [32]. Briefly, CT diluted in sucrose-phosphate-glutamic acid buffer (SPG) was placed directly into the cell culture medium in the apical chamber, and cultures were centrifuged for 40 min at 1825xg at 35°C [32]. Infected cells were then incubated for 69 h at 37°C in cell culture medium (without cycloheximide) before the 3 h HIV migration assays were performed, so that experiments were completed at 72 h post chlamydial infection. Mock infections were performed by centrifuging cells in SPG buffer without CT.
Cell-free and cell-associated HIV migration assays
A2EN cells were infected with CT serovar D. Cell-free HIVBaL inocula of 10, 100, or 1000 TCID50 (equivalent to 0.2ng, 2ng, or 20ng p24 or 3 x 105, 3 x 106, or 3 x 107 RNA copies, respectively) was added to the apical chambers of mock or CT-infected A2EN cells for 1, 3, or 24 h at 37°C or 4°C. For 24 h HIV exposure experiments, virus was added to CT-infected A2EN cells at both 48 and 72 h post-CT infection for a total CT infection duration of 72 and 96 h. After the appropriate virus exposure time, the basolateral medium was collected and immediately assessed for infectious HIV using TZM-bl cells or was aliquoted and frozen at -80°C for later analysis of viral content by PCR or p24 ELISA. For cell-associated virus migration assays, HIV-infected cells were first generated by inoculating 2 x 107 MT4-R5 cells with HIVBaL (equivalent to 20ng p24) in puromycin-free R10. After 72 h, the HIV-infected cells were filtered through a 40μm cell strainer, washed twice with Dulbecco’s phosphate buffered saline (DPBS) and resuspended in puromycin-free R10. 1 x 106 HIV-infected MT4-R5 cells were then added to the apical chambers of mock or CT-infected A2EN cells. The basolateral medium was collected 3 h post virus exposure.
Virus infectivity assays
TZM-bl luciferase reporter cells [38] were used to measure the infectious activity of HIV. For assays evaluating the effects of A2EN supernatants on infectious activity of virus, cell supernatants were incubated for 3 h with 10 TCID50 of HIVBaL, an amount of virus that produced relative light units (RLU) at least 10-fold above the background in TZM-bl cells. Dilutions of supernatants and virus were then added to TZM-bl cells in triplicate and cultured in black, clear bottom 96 well plates in complete DMEM supplemented with 75μg/mL DEAE-Dextran (Sigma). After 48 h, luminescence was measured as RLU using the Bright-Glo Luciferase Assay System (ProMega, Madison, WI) and a BioTek® Synergy MX plate reader and Gen5™ software. For assays evaluating the infectious activity of migrated HIV, 250μl of freshly collected A2EN basolateral supernatant was first incubated with 2 x 105 uninfected MT4-R5 cells to amplify virus. Infectious activity was then assessed 3 and 6 d later by adding 50μl of neat, 1:10, or 1:100 MT4-R5 culture medium to TZM-bl cells in triplicate and measuring RLU 48 h post virus exposure. Negative and positive controls for luciferase expression in TZM-bl cell assays were performed with medium alone or a known amount of HIVBaL, respectively.
Viral RNA quantification
Basolateral supernatants from A2EN cells that had been exposed to cell-free or cell-associated HIV were centrifuged at 20,000×g for 1 h at 4°C. The RNA was then purified using Ambion Trizol® Reagent (ThermoFisher, Waltham, MA) in accordance with the manufacturer's instructions. RNA templates were used as standards. The entire sample of RNA from each condition was reverse-transcribed, and polymerase chain reaction (PCR) amplification of the HIV-1 pol gene was performed on each sample, as previously described [47]. Two HIV-negative samples, one HIV-positive sample, and negative experimental controls were included in each assay. HIV levels are reported as copies per replicative sample.
HIV Infection of PBMC cultured with A2EN supernatants
Resting or PHA-activated PBMC in 100μl of R40 containing 40 U/ml IL-2 were added at 2 x 105 cells per well to a V-bottom 96-well tissue culture plate. An equal volume of epithelial cell medium or undiluted apical or basolateral supernatants from mock or CT-infected A2EN cells was then added. After 2 d at 37°C and 5% CO2, the activated PBMC were washed and resuspended in 100μl of medium alone or identical, but freshly thawed, A2EN supernatants. The activated PBMC were then infected with 200 TCID50 HIVBaL in 100μl of R40 with 40 U/ml IL-2. The resting PBMC were washed and infected with 200 TCID50 HIVBaL in 0.2ml of R20 with 20 U/ml IL-2 after 4 d. On d2 and d4 after infection, the culture medium was completely replaced with 200μl of R20 containing 20 U/ml IL-2. Culture medium harvested on day 6 was treated with Triton X-100 (0.5% v/v) and analyzed for viral content using a p24 ELISA.
p24 ELISA
Concentrations of p24 were measured using a p24 ELISA, as previously described [48]. Briefly, high protein binding microtiter plates (ThermoFisher) were coated overnight with an anti-p24 monoclonal antibody that had been purified from H12 hybridoma (ARP) culture medium using Protein G Sepharose (ThermoFisher). Plates were washed with PBS containing 0.05% Tween-20 (PBST) and blocked with PBST containing 5% nonfat dry milk and 1% FBS. Samples were serially diluted in 1% FBS/PBST and added to plates. A recombinant HIV p24 protein (ImmunoDiagnostics, Woburn, MA) previously calibrated using the PerkinElmer HIV p24 ELISA kit was used to generate a standard curve. Following an overnight reaction at 4°C, the plates were washed and treated for 1 h at 37°C with HIVIG (ARP) that had been biotinylated in the lab using EZ Link Sulfo NHS (ThermoFisher). The plates were then washed and consecutively treated for 30 min at room temperature with neutralite avidin-peroxidase and tetramethylbenzene (both SouthernBiotech, Birmingham, AL). After addition of H2SO4 stop solution, absorbance was recorded at 450nm. The concentration of p24 in samples was then interpolated from standard curves constructed with the SoftMax Pro computer program (Molecular Devices, Sunnyvale, CA).
Statistical Analyses
Statistical analyses were performed using Prism software (v4.0; GraphPad, San Diego, CA). One-way analysis of variance (ANOVA) with Tukey post-test was used to compare results in most experiments. One-tailed Mann-Whitney rank sum test was used to analyze cumulative p24 results from HIV-infected PBMCs cultured with apical or basolateral epithelial supernatants collected in 3 separate experiments. P-values <0.05 were considered significant.
Results
A2EN cells grown on cell culture inserts create a tight barrier against cell-free HIV
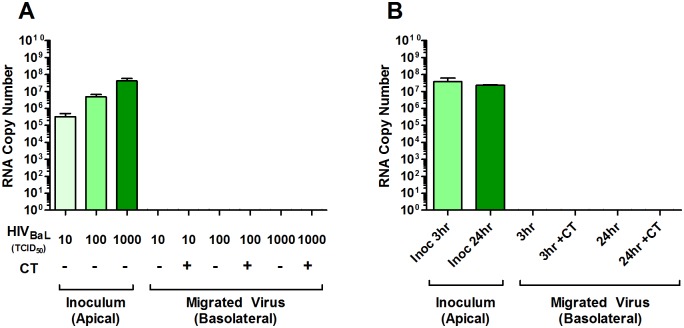
Both cell-free and cell-associated HIV have been detected in genital secretions [49, 50], and both are considered important modalities for sexual transmission of HIV [51–59]. We first determined whether cell-free virus could traverse from the apical surface of an A2EN monolayer into the basolateral compartment. The CCR5-tropic HIVBaL strain was selected for these studies, as sexually transmitted HIV isolates are predominantly CCR5-tropic [60–64]. Cell-free virus migration was investigated using varying inocula of virus, ranging from 10 TCID50, an amount at the high range of a physiological inoculum [65, 66], up to 1000 TCID50, an amount that others have reported is necessary for observing HIV transcytosis [54–56]. Cell-free virus was added to the apical chamber of A2EN cells for 1 h at either 37°C or 4°C in order to differentiate between transcellular and paracellular virus migration. Basolateral supernatants were collected and analyzed using a highly sensitive, quantitative PCR assay that can accurately detect as few as 10 copies of intact viral RNA per PCR reaction, as previously described [47]. We chose to use this assay to confidently measure HIV virions that cross the epithelial barrier rather than measuring HIV capsid protein, as p24 may be present on defective viral particles, cross the epithelium, and confound migration results. No viral RNA was detected in the basolateral chambers of either mock or CT-infected A2EN cells after 1 h at either 37°C (Fig 1A) or 4°C (data not shown) using any concentration of virus. We then used the highest inoculum (1000 TCID50), and increased the incubation times to 3 and 24 h, the latter of which is significantly longer than exposure times used in any other reports of cell-free transcytosis through an epithelial cell monolayer [54, 67–71]. For 24 h HIV exposure experiments, virus was added at both 48 and 72 h post-CT infection for a total CT infection time of 72 and 96 h (96h total duration time not shown), and no significant host cell lysis was observed, as previously described [32], making paracellular migration of virus in this assay an unlikely event. Even after 24 h, no viral RNA was observed in the basolateral chamber of either mock or CT-infected A2EN cells (Fig 1B), indicating that essentially no cell-free virus migrated through the epithelium.
Fig 1. Cell-free HIV does not migrate across mock or CT-infected A2EN cells.
(A) A2EN cells were infected with CT serovar D (> 95% infection rate) for 71 h as described in Materials and Methods. 10, 100, or 1000 TCID50 of cell-free HIVBaL was added to the apical chambers of mock and CT-infected A2EN cells for 1 h at either 4°C or 37°C so that the CT infection duration was 72 h total. (B) 1000 TCID50 of cell-free HIVBaL was added to the apical chambers of mock and CT-infected A2EN cells for 3 or 24 h at 37°C for a total CT infection duration of 72 h. Basolateral supernatants were then collected and analyzed for viral RNA using quantitative real-time PCR. Bars represent the mean values of RNA copies ± the standard deviation (SD). Data is representative of 4 independent experiments, each performed in quadruplicate. *p < 0.05.
It is possible, however, that virus migrated across the A2EN barrier at such a low rate that it was below the detection limit of our PCR assay. To investigate this, basolateral supernatants from A2EN cells exposed to 1000 TCID50 cell-free HIVBaL were incubated with uninfected CCR5+ MT4-R5 cells to amplify any viable virus that might have been in the basolateral supernatants. After 6 d, the MT4-R5 culture medium was tested for the presence of infectious HIV using TZM-bl cells. No virus was detected (data not shown). Overall, these results suggest that A2EN cells provide a tight, impenetrable barrier against cell-free HIV, similar to findings of others using different epithelial cells [55, 56, 67, 72, 73]. Furthermore, CT infection of A2EN cells did not modulate the integrity of the epithelial barrier to allow passage of cell-free HIV via either transcellular or paracellular mechanisms.
CT infection of A2EN cells enhances cell-associated HIV migration
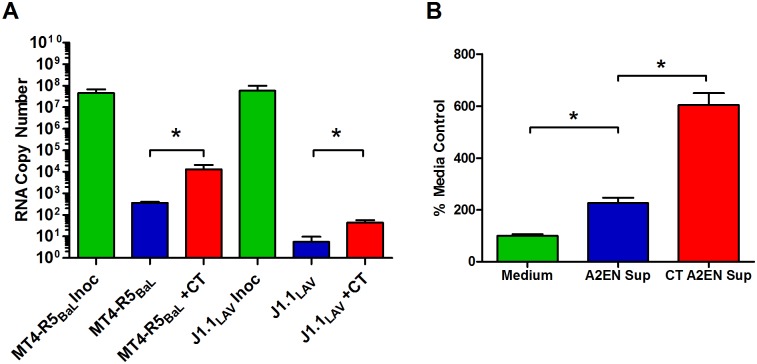
Next, we determined if cell-associated HIV could migrate across the A2EN monolayer. We first developed a standardized, reproducible protocol that generated a productive infection of MT4-R5 cells with HIVBaL, and consistently yielded RNA copies/ml similar to those in the 1000 TCID50 inoculum used above in experiments with cell-free HIV. 1 x 106 HIVBaL-infected MT4-R5 cells were added to mock and CT-infected A2EN cells for 3 h. Basolateral supernatants were collected and the viral RNA was quantified. Importantly, cell-associated HIV crossed the A2EN barrier at low levels (approximately 362 mean viral RNA copies per well), and these levels were significantly increased (approximately 13,264 mean viral RNA copies per well) when A2EN cells were infected with CT (p < 0.05; Fig 2A). These results were confirmed using a p24 ELISA (data not shown). To determine whether the migrated virus was infectious, basolateral supernatants were collected 3 h after virus exposure and incubated with uninfected MT4-R5 cells. Cultures were tested for infectious virus at 3 and 6 d (3 d time point shown in Fig 2B) using TZM-bl cells. Viable virus was detected at both time points, confirming that migrated virus was infectious. Migration assays were also performed with J1.1 Jurkat T cells chronically infected with the HIVLAV CXCR4-tropic virus. Similar findings were observed using J1.1 cells in mock and CT-infected A2EN cells (Fig 2A), suggesting that neither cell-associated HIV migration nor chlamydial enhancement of this migration was dependent upon viral tropism (CXCR4 vs CCR5). Taken together, these data suggest that HIV-infected T cells may facilitate low levels of virus migration across the endocervical epithelium, and that CT infection may enhance this process.
Fig 2. Cell-associated HIV crosses the A2EN epithelial barrier and is enhanced by CT infection.
A2EN cells were infected with CT serovar D (> 95% infection rate) for 72 h. 1 x 106 HIVBaL-infected MT4-R5 cells were added to the apical chambers of mock and CT-infected A2EN cells for 3 h at 37°C. (A) Viral RNA in basolateral supernatants from cell-associated HIV migration assays was quantitated using real-time PCR. Bars represent the mean RNA copies ± SD. (B) Basolateral supernatants collected in cell-associated HIV migration assays were incubated with uninfected MT4-R5 cells for 3 d. Supernatants from exposed MT4-R5 cells were then assayed for infectious virus using TZM-bl cells. Controls included TZM-bl cells incubated with an equivalent volume of epithelial cell medium. Data is expressed as a percentage of the mean RLU obtained for the medium alone controls. Bars represent the mean percentages ± SD. Results shown are representative of 4 separate experiments, each performed in quadruplicate. *p < 0.05.
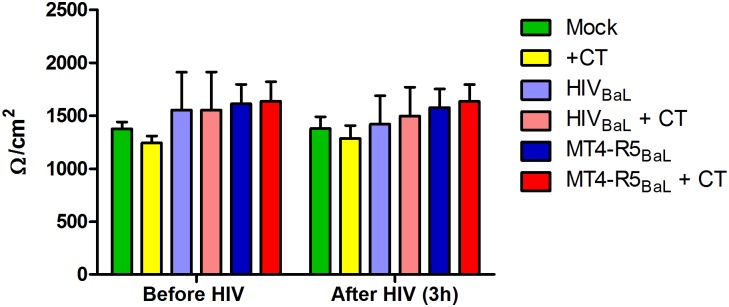
HIV-infected MT4-R5 cells do not significantly compromise the integrity of the A2EN epithelial barrier
One mechanism by which cell-associated HIV could cross an epithelial monolayer is by paracellular migration as a result of epithelial barrier disruption. Although we previously reported that chlamydial infection of A2EN cells grown on cell culture inserts did not decrease the epithelial barrier integrity [32], it is possible that the addition of HIV-infected T cells could disrupt the epithelium and allow virus to diffuse through the monolayer. To ascertain this, TEERs of both mock and CT-infected A2EN cells were recorded before and after the 3 h incubation with cell-free virus or infected MT4-R5 cells (Fig 3). There were no significant differences between TEERs, suggesting that neither cell-free nor cell-associated virus grossly disrupted junctional complexes or the tight barrier formed by A2EN epithelial cells. FITC-labeled dextran (3kD and 10kD) was also utilized to confirm that small molecules were incapable of penetrating A2EN cells after CT, HIV, or dual pathogen exposure (data not shown). These results suggest that the virus migration observed using HIV-infected MT4-R5 or J1.1 T cells was not due to disruption of the CT-infected A2EN epithelial barrier.
Fig 3. A2EN epithelial cell barrier integrity is not compromised by CT, cell-free HIV, or HIV-infected cells.
A2EN cells on cell culture inserts were infected with CT serovar D for 72 h. 1000 TCID50 of cell-free HIVBaL or 1 x 106 HIVBaL-infected MT4-R5 cells were then added to the apical surface of mock or CT-infected cells for 3 h. TEERs were measured before and after the addition of virus or infected cells. Bars represent the mean TEER values ± SD pooled from 3 separate experiments, each performed in triplicate.
HIV migration is likely dependent upon epithelial cell contact with HIV-infected T cells
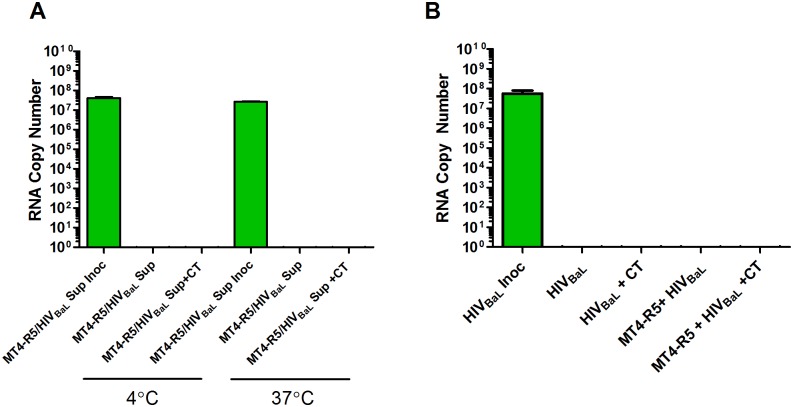
It is possible that cell-associated HIV crossed the A2EN barrier more efficiently than cell-free virus simply because the MT4-R5 cell line produced “fitter, more infectious virus” than PM-1 cells, the cell line in which the cell-free HIVBaL had been generated. Host adhesion molecules incorporated into the viral envelope might also differ for the HIVBaL produced in these cell lines [74, 75]. To confirm that MT4-R5-derived virus did not behave differently than PM-1-derived virus, 1000 TCID50 of cell-free HIVBaL freshly produced by HIVBaL-infected MT4-R5 cells was added to the apical chambers of mock and CT-infected A2EN cells. No viral RNA was observed in the basolateral chambers (Fig 4A), suggesting that virus produced by MT4-R5 cells does not cross the tight A2EN barrier more efficiently. A 1000 TCID50 dose of HIVBaL produced in PBMC also failed to cross the CT-infected A2EN epithelial barrier (data not shown).
Fig 4. Cell-associated HIVBaL migration is likely dependent upon epithelial cell contact with an HIV-infected T cell.
A2EN cells were infected with CT serovar D for 72 h. (A) 1000 TCID50 of cell-free HIVBaL freshly produced by MT4-R5 was added to apical chambers of mock and CT infected cells for 3 h at 4°C or 37°C. (B) 1000 TCID50 of PM-1-derived cell-free HIVBaL was added to mock and CT-infected A2EN cells in the presence or absence of 1 x 106 uninfected MT4-R5 cells. After a 3 h at 37°C, basolateral supernatants were collected and viral RNA was enumerated using PCR. Bars represent the mean RNA copies ± SD. Data is representative of 3 independent experiments, each performed in quadruplicate. *p < 0.05.
It is also possible that cell-associated virus migrated more efficiently because the T cells contacted the epithelial cells and stimulated specific cellular signaling events, making the epithelial cells more susceptible to virus entry [55, 58, 67, 76]. To determine if this might be the case, cell-free HIVBaL and uninfected MT4-R5 cells were simultaneously added to the apical chamber of mock and CT-infected A2EN cells. Consistently, we failed to observe any viral RNA in the basolateral chamber when uninfected T cells contacted the epithelial cells in the presence of cell-free virus (Fig 4B). These and the above results suggest that epithelial contact with an HIV-infected T cell is likely required for HIV migration across the A2EN epithelial cell barrier.
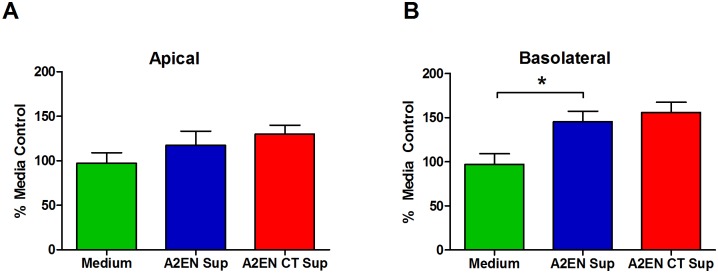
A2EN cell supernatants do not decrease infectious activity of HIV
It is possible that cell-free HIV migration was not observed because anti-microbial molecules in A2EN supernatants neutralized cell-free HIV at the apical surface and prevented viral migration [77–81]. CT infection has been shown to increase anti-microbial peptide expression in the reproductive tract and endocervical epithelial cells ([82]; unpublished observations), which might further decrease the probability that viable cell-free virus could cross the epithelium. To investigate this, apical or basolateral supernatants collected from mock or CT-infected A2EN cells were cultured with HIVBaL for 3 h. The infectious activity of the virus was then assessed using TZM-bl cells. There were no significant decreases in viral infectivity after culture with apical supernatants (Fig 5). Interestingly, basolateral supernatants from both mock and CT-infected A2EN cells increased viral infectivity above the medium control (p<0.05; Fig 5B). These results suggest that neither apical or basolateral A2EN supernatants, nor CT-infected A2EN supernatants, decrease HIV viability. Thus, a reduction in virus viability in the apical compartment does not explain why cell-free virus did not cross either the mock or CT-infected A2EN epithelial barrier. Furthermore, A2EN may produce molecules that enhance HIV infectivity of susceptible cell types.
Fig 5. A2EN supernatants do not decrease cell-free HIV viability.
A2EN cells were infected with CT serovar D, and supernatants were collected 72 h post-infection. Medium alone, (A) apical, or (B) basolateral supernatants were incubated with 1000 TCID50 of cell-free HIVBaL for 3 h. The infectious activity of the virus was then measured by transferring to TZM-bl cells and measuring luciferase activity 48 h later. Data shown is expressed as a percentage of the mean RLU recorded for medium alone controls. Bars represent the mean percentages ± SD. Data is representative of 3 independent experiments, each performed in quadruplicate. *p < 0.05.
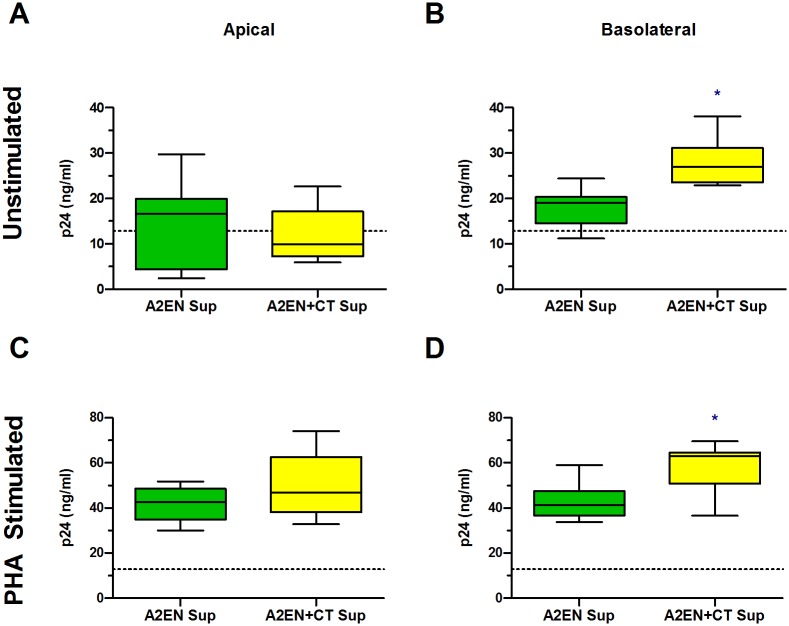
CT infection of A2EN cells results in an enhancement of HIV infection of target cells
We previously established that CT infection of A2EN cells significantly upregulates IL1α, a pro-inflammatory cytokine that can activate NFκB and could increase virus replication in target cells [32]. Concomitantly, CT infection abrogates the secretion of the CCR5 agonist RANTES, which would increase the chance that HIV could bind to its co-receptor on target cells [32]. Based on this and the above results showing enhanced HIV infection of TZM-bl cells in the presence of basolateral cell supernatants (Fig 5), we hypothesized that secretions from CT-infected endocervical epithelial cells may enhance HIV entry and/or replication in CCR5+ HIV target cells. To investigate this, PHA-activated PBMC were incubated with epithelial cell medium alone or apical or basolateral supernatants from mock or CT-infected A2EN cells for 2 days prior and 2 days after infection with HIVBaL. Viral production by PBMC was measured 6 d after HIV infection using a p24 ELISA that can accurately distinguish smaller fold changes in HIV compared to our qPCR assay (Fig 6). We also chose to test resting PBMC because we wanted to investigate the possibility that supernatants from CT-infected A2EN cells could partially activate resting T cells, making them more susceptible to HIV infection. For these assays, resting PBMC were pre-cultured with KSFM medium or A2EN supernatants for 4 d prior to infection with HIVBaL. Basolateral secretions from mock-infected A2EN cells were found to increase viral production over medium alone controls by approximately 2-fold in both resting and activated PBMC (p < 0.05, p24 levels of medium alone controls of resting and PHA stimulated PBMCs were 7.02 and 26.85pg/mL, respectively). However, exposure of resting or activated PBMC to basolateral supernatants from CT-infected A2EN cells increased viral production to a greater extent (Fig 6B).
Fig 6. Basolateral supernatants from CT-infected A2EN cells enhance HIV infection of PBMC.
A2EN cells grown on cell culture inserts were infected with CT serovar D for 72 h. (A, C) Apical and (B, D) basolateral supernatants collected from mock or CT-infected A2EN cells were incubated with (A, B) resting PBMC for 4 d or (C, D) PHA-activated PBMC for 2 d. The PBMC were then infected with 200 TCID50 of HIVBAL. Activated PBMC were additionally cultured with A2EN supernatants for another 2 d after infection. Every 2 d after infection, the culture medium was completely replaced. The viral content in culture medium collected 6 d after infection was determined using a p24 ELISA. Presented are the cumulative p24 results from 3 separate experiments, each performed in triplicate. Bars represent the mean ± SD. *p < 0.05.
Similar results were obtained when TZM-bl or MT4-R5 cells were cultured with A2EN supernatants for 4 d, then infected with PM-1-derived HIVBaL (S1 Fig). Taken together, these observations suggest endocervical epithelial cells may create a milieu at the basolateral surface that may activate resting T cells and facilitate HIV entry and/or replication in activated target cells. Should HIV gain access to the submucosa via trauma or a migration mechanism, CT-infected endocervical epithelial cells may produce factors that enhance HIV infection of target cells, potentially aiding in the establishment of early founder virus populations.
Discussion
HIV transmission studies using high dose, vaginal, cell-free SIV in non-human primate models, report that virus can cross the endocervical epithelium leading to recruitment of target cells and formation of small foci of infected T lymphocytes in the cervical stroma [8, 9, 83]. Clinical, diagnostic, and basic scientific studies, together, also demonstrate that endocervical epithelial cells are the major niche for CT, they produce proinflammatory cytokines in response to the organism, and infection is commonly accompanied by an influx of leukocytes, including activated, memory and CCR5+ T cells [30, 31]. Considering that these leukocyte subsets are the major targets for sexually transmitted strains of HIV [7, 30, 31], collectively, these observations suggest that an existing endocervical chlamydial infection could increase the likelihood of HIV transmission at this site and indicate a central role for infected epithelial cells as facilitators in this process. We therefore developed an endocervical epithelial cell model, A2EN, to investigate the direct contribution of CT infected epithelial cells in enhancing HIV migration and replication in target cell populations found in the submucosa of the CT infected endocervix.
We were able to demonstrate that CT infection of A2EN cells enhanced cell-associated, but not cell-free, virus migration across the epithelial barrier. These data support earlier studies which reported that cell-associated HIV is present in the in semen of infected men and may gain access to subepithelial target cells in the FRT of women [49, 51–53, 84], and it suggests that CT infection may further enhance this process. We also observed enhanced HIV infection in PBMC and CD4+, CCR5+ cell lines exposed to basolateral supernatants from CT-infected epithelial cells. These latter results suggest that, should virus cross the endocervical epithelial barrier, CT infection may facilitate viral infection in the local microenvironment, enhancing the probability of establishing a productive HIV infection.
Previous studies, using a variety of modeling conditions, have been conflicted as to whether cell-free HIV could traverse across an intact epithelium [49, 51, 52, 54–59, 69, 70, 72, 84–91]. Here, we focused on how HIV migrates across a mucus-producing, single cell, endocervical epithelial cell layer that recapitulates many primary properties of the endocervix [33, 34]. We were unable to observe any cell-free HIV migration across A2EN cells, suggesting that the epithelial barrier was not significantly compromised upon exposure to either CT or HIV. Furthermore, we were unable to observe any differences in epithelial barrier function between TEERs or dextran permeability in CT-infected, HIV-exposed A2EN cells, making disruption of tight junctions and subsequent paracellular migration of cell-free HIV an unlikely mechanism in this model. We also verified that the lack of cell-free HIV migration was not due to neutralization of virus by apically secreted anti-microbial molecules, a finding in contrast to others [77–81]. We utilized a high concentration of virus to ascertain viral migration and infectivity, which may account for the differences in our study compared to others [54, 67, 69–71]. It cannot be ruled out, however, that antimicrobial molecules may have been concentrated in the mucus on the apical surface of A2EN cells [92–94] and not sufficiently solubilized in the cell culture supernatants, which may have influenced HIV binding, viability, and/or entry. Another possible reason why paracellular cell-free HIV migration did not occur may be because A2EN cells infected with CT or exposed to HIV did not secrete TNFα at sufficient levels to disrupt tight junctions [32], which has been shown to occur in endometrial epithelial cell models [95]. The differences between our results and those of Nazli et al. [95] may highlight tissue-specific differences in the innate immune responses to HIV and subsequent virus diffusion across the epithelial barrier. Experiments using endocervical and endometrial epithelial cells derived from the same donor should ideally be performed to specifically evaluate these different sites and their roles in the immune response, their barrier functions and permissiveness for HIV migration, as all of these could influence the efficacy of preventative microbicides or vaccines against CT and HIV in the FRT. Moreover, the role of leukocyte-epithelial interactions should also be investigated within these model systems, as the dynamics of these interactions may also significantly and differentially influence parameters affecting early HIV transmission events.
While we were unable to detect cell-free HIV migration, cell-associated virus crossed the endocervical epithelial barrier with low efficiency, and this significantly increased in the presence of chlamydial infection. These results support other laboratories’ work demonstrating an important role for cell-associated virus in HIV acquisition in the FRT [51–53, 55, 84, 96]. The low efficiency rate observed by us and others may aid in explaining why heterosexual transmission rates are low, as the epithelium, mucus, and secreted antimicrobial molecules in the FRT clearly can create an effective barrier to prevent high numbers of virions from gaining access to the submucosa. Despite the fact that many have observed that cell-associated virus can migrate across epithelial barriers [55, 58, 67, 76, 85, 97], the mechanism of how this occurs is still unknown. The cell-associated viral migration observed in our study was not simply due to ‘fitter’ virus or T cell contact, suggesting that there may be a “synapse” that occurs between HIV infected lymphocytes and epithelial cells that facilitates the uptake and/or migration process, a mechanism that has been proposed by others [67, 87]. CT infection of A2EN cells may enhance this “synaptic” process, allowing more virions to gain access to the basolateral compartment. Since neither TEERs nor dextran permeability significantly changed upon the addition of HIV-infected T cells to A2EN cells, it is likely that cell-associated virus migration occurred via a trans-cellular mechanism, such as the endocytic recycling pathway [88], as others have reported. It is also possible that cell-associated virus may cross via a paracellular mechanism if HIV-infected T lymphocytes extend pseudopodia between the epithelial cells without significantly disrupting the tight junctions, which can occur with HIV-infected dendritic cells and intestinal epithelial cells [98]. Virus may also cross the epithelial cell barrier by a sequestration process whereby virions are taken up at the apical surface and released at the basolateral membrane non-specifically [89, 90, 96, 99, 100]. Distinguishing sequestration from an active transcytosis mechanism is challenging as it is not yet known what host cellular machinery is utilized by HIV to facilitate either process. Overall, HIV and CT may modulate multiple factors in the endocervical epithelial cells that could facilitate cell-associated virus migration. Further, in depth, experimentation might be warranted to elucidate the exact mechanisms involved in order to design specific therapies to inhibit these initial HIV infection events.
We previously reported that CT infection of A2EN cells significantly upregulated the proinflammatory cytokine, IL1α, but abrogated the expression of the CCR5 ligand RANTES [32]. Taken together, we hypothesized that supernatants from CT-infected A2EN may enhance HIV replication in target cells, as IL1α can stimulate the NFκB pathway in target cells, leading to increased HIV replication [101, 102]. Concomitantly, a decrease in RANTES could allow more virions to bind to the CCR5 co-receptors present on target cells [103–105]. When basolateral supernatants from non-infected A2EN cells were incubated with PBMC or MT4-R5 cells and inoculated with virus, we observed an increase in HIV production. Furthermore, CT-infected A2EN basolateral supernatants further enhanced HIV production, but apical supernatants did not, despite the finding that apical IL1α increases after chlamydial infection [32]. These results may be explained by the fact that A2EN cells secrete IL1 receptor antagonist (IL1ra) at the apical surface, but not at the basolateral surface [32], which would inhibit IL1α from functioning in the apical environment. Our results suggest that the functional IL1α, or an unidentified factor, or a combination of factors present in the basolateral supernatants from CT-infected A2EN cells, may be acting upon target cells to facilitate HIV entry and/or replication. Should HIV gain access to the endocervical submucosa via migration or trauma, virus may be more likely to infect and replicate in an underlying susceptible target cell. Considering these results and our previous observations that CT infection of the endocervix leads to an increase in CD4+ and CCR5+ lymphocytes at this site [30, 31], the microenvironment created by CT-infected epithelial cells may contribute to the establishment of HIV founder virus populations in target cells present within the cervical submucosa.
In conclusion, our endocervical model is one of the first to allow the in vitro study of interactions between the two sexually transmitted pathogens, CT and HIV. It could also serve as a tool for similar co-infection models, microbicide testing, screening of specific neutralizing antibodies, or for building more complex models that incorporate various defined leukocyte subpopulations. Further, the tractability and primary cell-like properties of the model could enable the investigation of endogenous and exogenous cofactors such as semen, mucus, and hormones and their influence on cell-free and cell-associated HIV transmission. The studies presented here suggest CT infection of endocervical epithelial cells increases cell-associated HIV migration across the epithelial barrier and can enhance viral replication in target cells via basolaterally-secreted factors. These results suggest CT infection of endocervical epithelial cells could facilitate HIV access to underlying susceptible cell types, the establishment of a founder virus population, and ultimately, HIV transmission. The ability of CT to infect the FRT for extended periods of time in the absence of symptoms likely increases the probability of introducing a secondary pathogen, such as HIV, into a CT-infected FRT. Collectively, these observations reiterate the importance of finding alternative preventative strategies for CT infection, as this and other highly prevalent sexually transmitted pathogens contribute to HIV acquisition in women worldwide.
Supporting Information
A2EN cells on cell culture inserts were infected with CT serovar D. Supernatants from mock or CT-infected A2EN cells were collected after 72 h and incubated with either TZM-bl cells or MT4-R5 cells for 24 h. 10 TCID50 was then added to each well of TZM-bl cells or to 2 x 105 MT4-R5 cells. (A, B) Virus exposed TZM-bl cells were assayed for luciferase expression 48 h after virus addition. (C, D) Virus exposed MT4-R5 T cells were incubated for 6 d. The culture medium was then tested for infectious HIV after transfer to TZM-bl cells. Controls included TZM-bl cells incubated with a known amount of virus or an equivalent volume of KFSM medium alone. Data shown is expressed as percentage of the mean RLU obtained with KFSM controls. Bars represent the mean percentages ± SD. Data is representative of 3 independent experiments, each performed in quadruplicate. *p < 0.05.
(TIF)
Acknowledgments
This work was supported by the Louisiana Vaccine Center and the Louisiana Board of Regents. The following reagents were obtained from the NIH AIDS Reagent Program: HIVLAI-infected J1.1 cells (contributed by Dr. Thomas Folks), HIVBaL (Drs. Suzanne Gartner, Mikulas Popovic and Robert Gallo), PM-1 cells (Drs. Paulo Lusso and Robert Gallo), TZM-bl cells (Drs. John Kappes and Xiaoyin Wu and Tranzyme Inc).
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by National Institute of Health, National Institute of Allergy and Infectious Diseases grants AI110373 and AI087899 (AJQ, AMA, and DJS), and the Louisiana Vaccine Center funded by the Louisiana Board of Regents (AJQ).
References
- 1.UNAIDS. Women, girls, gender equality and HIV. Geneva, Switzerland: UNAIDS; 2010. [Google Scholar]
- 2.Hladik F, McElrath MJ. Setting the stage: host invasion by HIV. Nature reviews Immunology. 2008;8(6):447–57. Epub 2008/05/13. 10.1038/nri2302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brunham RC, Rey-Ladino J. Immunology of Chlamydia infection: implications for a Chlamydia trachomatis vaccine. Nat Rev Immunol. 2005;5(2):149–61. Epub 2005/02/03. [DOI] [PubMed] [Google Scholar]
- 4.CDC. Sexually Transmitted Disease Surveillance 2014. Altanta, GA: US Department of Health and Human Services; 2015; Available: http://www.cdc.gov/std/stats14/std-trends-508.pdf. [Google Scholar]
- 5.Peterman TA, Newman DR, Maddox L, Schmitt K, Shiver S. Risk for HIV following a diagnosis of syphilis, gonorrhoea or chlamydia: 328,456 women in Florida, 2000–2011. International journal of STD & AIDS. 2015;26(2):113–9. Epub 2014/04/10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Venkatesh KK, van der Straten A, Cheng H, Montgomery ET, Lurie MN, Chipato T, et al. The relative contribution of viral and bacterial sexually transmitted infections on HIV acquisition in southern African women in the Methods for Improving Reproductive Health in Africa study. International journal of STD & AIDS. 2011;22(4):218–24. Epub 2011/04/26. [DOI] [PubMed] [Google Scholar]
- 7.Brunham RC, Paavonen J, Stevens CE, Kiviat N, Kuo CC, Critchlow CW, et al. Mucopurulent cervicitis—the ignored counterpart in women of urethritis in men. The New England journal of medicine. 1984;311(1):1–6. Epub 1984/07/05. [DOI] [PubMed] [Google Scholar]
- 8.Zhang Z, Schuler T, Zupancic M, Wietgrefe S, Staskus KA, Reimann KA, et al. Sexual transmission and propagation of SIV and HIV in resting and activated CD4+ T cells. Science. 1999;286(5443):1353–7. Epub 1999/11/13. [DOI] [PubMed] [Google Scholar]
- 9.Li Q, Estes JD, Schlievert PM, Duan L, Brosnahan AJ, Southern PJ, et al. Glycerol monolaurate prevents mucosal SIV transmission. Nature. 2009;458(7241):1034–8. Epub 2009/03/06. 10.1038/nature07831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Research DoRHa. Global incidence and prevalence of selected curable sexually transmitted infections-2008. In: Organization WH, editor. 2012. [Google Scholar]
- 11.Giuliano AR, Botha MH, Zeier M, Abrahamsen ME, Glashoff RH, van der Laan LE, et al. High HIV, HPV, and STI prevalence among young Western Cape, South African women: EVRI HIV prevention preparedness trial. J Acquir Immune Defic Syndr. 2015;68(2):227–35. Epub 2014/11/22. 10.1097/QAI.0000000000000425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Newman L, Rowley J, Vander Hoorn S, Saman Wijesooriya N, Unemo M, Low N, et al. Global Estimates of the Prevalence and Incidence of Four Curable Sexually Transmitted Infections in 2012 Based on Systematic Review and Global Reporting. PLOS ONE. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yirenya-Tawiah D, Annang TN, Apea-Kubi KA, Lomo G, Mensah D, Akyeh L, et al. Chlamydia Trachomatis and Neisseria Gonorrhoeae prevalence among women of reproductive age living in urogenital schistosomiasis endemic area in Ghana. BMC research notes. 2014;7:349 Epub 2014/06/12. 10.1186/1756-0500-7-349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peipert JF. Clinical practice. Genital chlamydial infections. The New England journal of medicine. 2003;349(25):2424–30. Epub 2003/12/19. [DOI] [PubMed] [Google Scholar]
- 15.Harrison HR, Costin M, Meder JB, Bownds LM, Sim DA, Lewis M, et al. Cervical Chlamydia trachomatis infection in university women: relationship to history, contraception, ectopy, and cervicitis. American journal of obstetrics and gynecology. 1985;153(3):244–51. Epub 1985/10/01. [DOI] [PubMed] [Google Scholar]
- 16.Paavonen J, Stevens CE, Wolner-Hanssen P, Critchlow CW, Derouen T, Kiviat N, et al. Colposcopic manifestations of cervical and vaginal infections. Obstetrical & gynecological survey. 1988;43(7):373–81. Epub 1988/07/01. [DOI] [PubMed] [Google Scholar]
- 17.Darville T. Recognition and treatment of chlamydial infections from birth to adolescence. Advances in experimental medicine and biology. 2013;764:109–22. Epub 2013/05/10. [DOI] [PubMed] [Google Scholar]
- 18.Walsh C, Anderson LA, Irwin K. The silent epidemic of Chlamydia trachomatis: the urgent need for detection and treatment in women. Journal of women's health & gender-based medicine. 2000;9(4):339–43. Epub 2000/06/27. [DOI] [PubMed] [Google Scholar]
- 19.Abdelrahman YM, Belland RJ. The chlamydial developmental cycle. FEMS microbiology reviews. 2005;29(5):949–59. Epub 2005/07/27. [DOI] [PubMed] [Google Scholar]
- 20.Hogan RJ, Mathews SA, Mukhopadhyay S, Summersgill JT, Timms P. Chlamydial persistence: beyond the biphasic paradigm. Infect Immun. 2004;72(4):1843–55. Epub 2004/03/25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beatty WL, Morrison RP, Byrne GI. Persistent chlamydiae: from cell culture to a paradigm for chlamydial pathogenesis. Microbiol Rev. 1994;58(4):686–99. Epub 1994/12/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Belland RJ, Nelson DE, Virok D, Crane DD, Hogan D, Sturdevant D, et al. Transcriptome analysis of chlamydial growth during IFN-gamma-mediated persistence and reactivation. Proc Natl Acad Sci U S A. 2003;100(26):15971–6. Epub 2003/12/16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lewis ME, Belland RJ, AbdelRahman YM, Beatty WL, Aiyar AA, Zea AH, et al. Morphologic and molecular evaluation of Chlamydia trachomatis growth in human endocervix reveals distinct growth patterns. Frontiers in cellular and infection microbiology. 2014;4:71 Epub 2014/06/25. 10.3389/fcimb.2014.00071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gottlieb SL, Martin DH, Xu F, Byrne GI, Brunham RC. Summary: The natural history and immunobiology of Chlamydia trachomatis genital infection and implications for Chlamydia control. J Infect Dis. 2010;201 Suppl 2:S190–204. Epub 2010/06/05. [DOI] [PubMed] [Google Scholar]
- 25.Molano M, Meijer CJ, Weiderpass E, Arslan A, Posso H, Franceschi S, et al. The natural course of Chlamydia trachomatis infection in asymptomatic Colombian women: a 5-year follow-up study. J Infect Dis. 2005;191(6):907–16. Epub 2005/02/18. [DOI] [PubMed] [Google Scholar]
- 26.Morre SA, van den Brule AJ, Rozendaal L, Boeke AJ, Voorhorst FJ, de Blok S, et al. The natural course of asymptomatic Chlamydia trachomatis infections: 45% clearance and no development of clinical PID after one-year follow-up. Int J STD AIDS. 2002;13 Suppl 2:12–8. Epub 2003/01/23. [DOI] [PubMed] [Google Scholar]
- 27.Geisler WM, Wang C, Morrison SG, Black CM, Bandea CI, Hook EW 3rd. The natural history of untreated Chlamydia trachomatis infection in the interval between screening and returning for treatment. Sexually transmitted diseases. 2008;35(2):119–23. Epub 2007/09/28. [DOI] [PubMed] [Google Scholar]
- 28.Rank RG, Batteiger BE, Soderberg LS. Susceptibility to reinfection after a primary chlamydial genital infection. Infection and immunity. 1988;56(9):2243–9. Epub 1988/09/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schust DJ, Ibana JA, Buckner LR, Ficarra M, Sugimoto J, Amedee AM, et al. Potential mechanisms for increased HIV-1 transmission across the endocervical epithelium during C. trachomatis infection. Current HIV research. 2012;10(3):218–27. Epub 2012/03/06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ficarra M, Ibana JS, Poretta C, Ma L, Myers L, Taylor SN, et al. A distinct cellular profile is seen in the human endocervix during Chlamydia trachomatis infection. Am J Reprod Immunol. 2008;60(5):415–25. Epub 2008/09/19. 10.1111/j.1600-0897.2008.00639.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ibana JA, Myers L, Porretta C, Lewis M, Taylor SN, Martin DH, et al. The major CD8 T cell effector memory subset in the normal and Chlamydia trachomatis-infected human endocervix is low in perforin. BMC Immunol. 2012;13:66 Epub 2012/12/12. 10.1186/1471-2172-13-66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Buckner LR, Lewis ME, Greene SJ, Foster TP, Quayle AJ. Chlamydia trachomatis infection results in a modest pro-inflammatory cytokine response and a decrease in T cell chemokine secretion in human polarized endocervical epithelial cells. Cytokine. 2013;63(2):151–65. Epub 2013/05/16. 10.1016/j.cyto.2013.04.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Buckner LR, Schust DJ, Ding J, Nagamatsu T, Beatty W, Chang TL, et al. Innate immune mediator profiles and their regulation in a novel polarized immortalized epithelial cell model derived from human endocervix. J Reprod Immunol. 2011;92(1–2):8–20. Epub 2011/09/29. 10.1016/j.jri.2011.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Herbst-Kralovetz MM, Quayle AJ, Ficarra M, Greene S, Rose WA 2nd, Chesson R, et al. Quantification and comparison of toll-like receptor expression and responsiveness in primary and immortalized human female lower genital tract epithelia. Am J Reprod Immunol. 2008;59(3):212–24. Epub 2008/01/19. 10.1111/j.1600-0897.2007.00566.x [DOI] [PubMed] [Google Scholar]
- 35.Krowicka H, Robinson JE, Clark R, Hager S, Broyles S, Pincus SH. Use of tissue culture cell lines to evaluate HIV antiviral resistance. AIDS Res Hum Retroviruses. 2008;24(7):957–67. Epub 2008/08/02. 10.1089/aid.2007.0242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lusso P, Cocchi F, Balotta C, Markham PD, Louie A, Farci P, et al. Growth of macrophage-tropic and primary human immunodeficiency virus type 1 (HIV-1) isolates in a unique CD4+ T-cell clone (PM1): failure to downregulate CD4 and to interfere with cell-line-tropic HIV-1. J Virol. 1995;69(6):3712–20. Epub 1995/06/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Perez VL, Rowe T, Justement JS, Butera ST, June CH, Folks TM. An HIV-1-infected T cell clone defective in IL-2 production and Ca2+ mobilization after CD3 stimulation. J Immunol. 1991;147(9):3145–8. Epub 1991/11/01. [PubMed] [Google Scholar]
- 38.Montefiori DC. Measuring HIV neutralization in a luciferase reporter gene assay. Methods Mol Biol. 2009;485:395–405. Epub 2008/11/21. 10.1007/978-1-59745-170-3_26 [DOI] [PubMed] [Google Scholar]
- 39.Gartner S, Markovits P, Markovitz DM, Kaplan MH, Gallo RC, Popovic M. The role of mononuclear phagocytes in HTLV-III/LAV infection. Science. 1986;233(4760):215–9. Epub 1986/07/11. [DOI] [PubMed] [Google Scholar]
- 40.Popovic M, Gartner S., Read-Connole E., Beaver B., Reitz M. Cell tropism and expression of HIV-1 isolates in natural targets In: Ga Valette, editor. Retroviruses of Human AIDS and Related Animal Diseases. Paris, Marnes-La-Coquette: Colloque Des Cent Gardes; 1989. p. 21–7. [Google Scholar]
- 41.Koup RA, Ho DD, Poli G, Fauci AS. Isolation and quantitation of HIV in peripheral blood. Current protocols in immunology / edited by John E Coligan [et al. ]. 2001;Chapter 12:Unit 12.2. Epub 2008/04/25. [DOI] [PubMed] [Google Scholar]
- 42.Halldorsson S, Asgrimsson V, Axelsson I, Gudmundsson GH, Steinarsdottir M, Baldursson O, et al. Differentiation potential of a basal epithelial cell line established from human bronchial explant. In Vitro Cell Dev Biol Anim. 2007;43(8–9):283–9. Epub 2007/09/19. [DOI] [PubMed] [Google Scholar]
- 43.Fahey JV, Schaefer TM, Channon JY, Wira CR. Secretion of cytokines and chemokines by polarized human epithelial cells from the female reproductive tract. Hum Reprod. 2005;20(6):1439–46. Epub 2005/03/01. [DOI] [PubMed] [Google Scholar]
- 44.Gorodeski GI. Vaginal-cervical epithelial permeability decreases after menopause. Fertil Steril. 2001;76(4):753–61. Epub 2001/10/10. [DOI] [PubMed] [Google Scholar]
- 45.Strengert M, Knaus UG. Analysis of epithelial barrier integrity in polarized lung epithelial cells. Methods Mol Biol. 2011;763:195–206. Epub 2011/08/30. 10.1007/978-1-61779-191-8_13 [DOI] [PubMed] [Google Scholar]
- 46.Yuan SY, Rigor RR. Methods for measuring permeability Regulation of Endothelial Barrier Function. San Rafael (CA)2010. [PubMed] [Google Scholar]
- 47.Henning TR, Lacour N, Amedee AM. Efficient methodologies for sensitive HIV-1 RNA quantitation from plasma and vaginal secretions. J Clin Virol. 2009;46(4):309–13. Epub 2009/09/29. 10.1016/j.jcv.2009.08.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wehrly K, Chesebro B. p24 antigen capture assay for quantification of human immunodeficiency virus using readily available inexpensive reagents. Methods. 1997;12(4):288–93. Epub 1997/08/01. [DOI] [PubMed] [Google Scholar]
- 49.Quayle AJ, Xu C, Mayer KH, Anderson DJ. T lymphocytes and macrophages, but not motile spermatozoa, are a significant source of human immunodeficiency virus in semen. J Infect Dis. 1997;176(4):960–8. Epub 1997/10/23. [DOI] [PubMed] [Google Scholar]
- 50.Mayer KH, Boswell S, Goldstein R, Lo W, Xu C, Tucker L, et al. Persistence of human immunodeficiency virus in semen after adding indinavir to combination antiretroviral therapy. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 1999;28(6):1252–9. Epub 1999/08/18. [DOI] [PubMed] [Google Scholar]
- 51.Anderson DJ. Modeling mucosal cell-associated HIV type 1 transmission in vitro. J Infect Dis. 2014;210 Suppl 3:S648–53. Epub 2014/11/22. 10.1093/infdis/jiu537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Anderson DJ, Le Grand R. Cell-associated HIV mucosal transmission: the neglected pathway. J Infect Dis. 2014;210 Suppl 3:S606–8. Epub 2014/11/22. 10.1093/infdis/jiu538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Barreto-de-Souza V, Arakelyan A, Margolis L, Vanpouille C. HIV-1 vaginal transmission: cell-free or cell-associated virus? Am J Reprod Immunol. 2014;71(6):589–99. Epub 2014/04/16. 10.1111/aji.12240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bobardt MD, Chatterji U, Selvarajah S, Van der Schueren B, David G, Kahn B, et al. Cell-free human immunodeficiency virus type 1 transcytosis through primary genital epithelial cells. J Virol. 2007;81(1):395–405. Epub 2006/10/20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bomsel M. Transcytosis of infectious human immunodeficiency virus across a tight human epithelial cell line barrier. Nat Med. 1997;3(1):42–7. Epub 1997/01/01. [DOI] [PubMed] [Google Scholar]
- 56.Bouschbacher M, Bomsel M, Verronese E, Gofflo S, Ganor Y, Dezutter-Dambuyant C, et al. Early events in HIV transmission through a human reconstructed vaginal mucosa. AIDS. 2008;22(11):1257–66. Epub 2008/06/27. 10.1097/QAD.0b013e3282f736f4 [DOI] [PubMed] [Google Scholar]
- 57.Coombs RW, Reichelderfer PS, Landay AL. Recent observations on HIV type-1 infection in the genital tract of men and women. AIDS. 2003;17(4):455–80. Epub 2003/02/25. [DOI] [PubMed] [Google Scholar]
- 58.Phillips DM. The role of cell-to-cell transmission in HIV infection. AIDS. 1994;8(6):719–31. Epub 1994/06/01. [DOI] [PubMed] [Google Scholar]
- 59.Phillips DM, Zacharopoulos VR, Tan X, Pearce-Pratt R. Mechanisms of sexual transmission of HIV: does HIV infect intact epithelia? Trends Microbiol. 1994;2(11):454–8. Epub 1994/11/01. [DOI] [PubMed] [Google Scholar]
- 60.Margolis L, Shattock R. Selective transmission of CCR5-utilizing HIV-1: the 'gatekeeper' problem resolved? Nature reviews Microbiology. 2006;4(4):312–7. Epub 2006/03/17. [DOI] [PubMed] [Google Scholar]
- 61.McNearney T, Hornickova Z, Markham R, Birdwell A, Arens M, Saah A, et al. Relationship of human immunodeficiency virus type 1 sequence heterogeneity to stage of disease. Proc Natl Acad Sci U S A. 1992;89(21):10247–51. Epub 1992/11/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.van't Wout AB, Kootstra NA, Mulder-Kampinga GA, Albrecht-van Lent N, Scherpbier HJ, Veenstra J, et al. Macrophage-tropic variants initiate human immunodeficiency virus type 1 infection after sexual, parenteral, and vertical transmission. The Journal of clinical investigation. 1994;94(5):2060–7. Epub 1994/11/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wolinsky SM, Wike CM, Korber BT, Hutto C, Parks WP, Rosenblum LL, et al. Selective transmission of human immunodeficiency virus type-1 variants from mothers to infants. Science. 1992;255(5048):1134–7. Epub 1992/02/28. [DOI] [PubMed] [Google Scholar]
- 64.Zhu T, Mo H, Wang N, Nam DS, Cao Y, Koup RA, et al. Genotypic and phenotypic characterization of HIV-1 patients with primary infection. Science. 1993;261(5125):1179–81. Epub 1993/08/27. [DOI] [PubMed] [Google Scholar]
- 65.Celum CL, Buchbinder SP, Donnell D, Douglas JM Jr., Mayer K, Koblin B, et al. Early human immunodeficiency virus (HIV) infection in the HIV Network for Prevention Trials Vaccine Preparedness Cohort: risk behaviors, symptoms, and early plasma and genital tract virus load. J Infect Dis. 2001;183(1):23–35. Epub 2000/12/07. [DOI] [PubMed] [Google Scholar]
- 66.Pilcher CD, Joaki G, Hoffman IF, Martinson FE, Mapanje C, Stewart PW, et al. Amplified transmission of HIV-1: comparison of HIV-1 concentrations in semen and blood during acute and chronic infection. AIDS. 2007;21(13):1723–30. Epub 2007/08/11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Alfsen A, Yu H, Magerus-Chatinet A, Schmitt A, Bomsel M. HIV-1-infected blood mononuclear cells form an integrin- and agrin-dependent viral synapse to induce efficient HIV-1 transcytosis across epithelial cell monolayer. Molecular biology of the cell. 2005;16(9):4267–79. Epub 2005/06/25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Drannik AG, Nag K, Yao XD, Henrick BM, Ball TB, Plummer FA, et al. Anti-HIV-1 activity of elafin depends on its nuclear localization and altered innate immune activation in female genital epithelial cells. PLoS One. 2012;7(12):e52738 Epub 2013/01/10. 10.1371/journal.pone.0052738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hocini H, Becquart P, Bouhlal H, Chomont N, Ancuta P, Kazatchkine MD, et al. Active and selective transcytosis of cell-free human immunodeficiency virus through a tight polarized monolayer of human endometrial cells. J Virol. 2001;75(11):5370–4. Epub 2001/05/03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hocini H, Bomsel M. Infectious human immunodeficiency virus can rapidly penetrate a tight human epithelial barrier by transcytosis in a process impaired by mucosal immunoglobulins. J Infect Dis. 1999;179 Suppl 3:S448–53. Epub 1999/04/01. [DOI] [PubMed] [Google Scholar]
- 71.Stoddard E, Ni H, Cannon G, Zhou C, Kallenbach N, Malamud D, et al. gp340 promotes transcytosis of human immunodeficiency virus type 1 in genital tract-derived cell lines and primary endocervical tissue. J Virol. 2009;83(17):8596–603. Epub 2009/06/26. 10.1128/JVI.00744-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Greenhead P, Hayes P, Watts PS, Laing KG, Griffin GE, Shattock RJ. Parameters of human immunodeficiency virus infection of human cervical tissue and inhibition by vaginal virucides. J Virol. 2000;74(12):5577–86. Epub 2000/05/24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Van Herrewege Y, Michiels J, Waeytens A, De Boeck G, Salden E, Heyndrickx L, et al. A dual chamber model of female cervical mucosa for the study of HIV transmission and for the evaluation of candidate HIV microbicides. Antiviral research. 2007;74(2):111–24. Epub 2006/11/14. [DOI] [PubMed] [Google Scholar]
- 74.Mondor I, Ugolini S, Sattentau QJ. Human immunodeficiency virus type 1 attachment to HeLa CD4 cells is CD4 independent and gp120 dependent and requires cell surface heparans. J Virol. 1998;72(5):3623–34. Epub 1998/04/29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ugolini S, Mondor I, Parren PW, Burton DR, Tilley SA, Klasse PJ, et al. Inhibition of virus attachment to CD4+ target cells is a major mechanism of T cell line-adapted HIV-1 neutralization. The Journal of experimental medicine. 1997;186(8):1287–98. Epub 1997/10/23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ganor Y, Zhou Z, Tudor D, Schmitt A, Vacher-Lavenu MC, Gibault L, et al. Within 1 h, HIV-1 uses viral synapses to enter efficiently the inner, but not outer, foreskin mucosa and engages Langerhans-T cell conjugates. Mucosal immunology. 2010;3(5):506–22. Epub 2010/06/24. 10.1038/mi.2010.32 [DOI] [PubMed] [Google Scholar]
- 77.Anderson BL, Ghosh M, Raker C, Fahey J, Song Y, Rouse DJ, et al. In vitro anti-HIV-1 activity in cervicovaginal secretions from pregnant and nonpregnant women. American journal of obstetrics and gynecology. 2012;207(1):65.e1–10. Epub 2012/06/26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ghosh M, Fahey JV, Shen Z, Lahey T, Cu-Uvin S, Wu Z, et al. Anti-HIV activity in cervical-vaginal secretions from HIV-positive and -negative women correlate with innate antimicrobial levels and IgG antibodies. PLoS One. 2010;5(6):e11366 Epub 2010/07/09. 10.1371/journal.pone.0011366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Schaefer TM, Fahey JV, Wright JA, Wira CR. Innate immunity in the human female reproductive tract: antiviral response of uterine epithelial cells to the TLR3 agonist poly(I:C). J Immunol. 2005;174(2):992–1002. Epub 2005/01/07. [DOI] [PubMed] [Google Scholar]
- 80.Wira CR, Ghosh M, Smith JM, Shen L, Connor RI, Sundstrom P, et al. Epithelial cell secretions from the human female reproductive tract inhibit sexually transmitted pathogens and Candida albicans but not Lactobacillus. Mucosal immunology. 2011;4(3):335–42. Epub 2010/11/05. 10.1038/mi.2010.72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wira CR, Patel MV, Ghosh M, Mukura L, Fahey JV. Innate immunity in the human female reproductive tract: endocrine regulation of endogenous antimicrobial protection against HIV and other sexually transmitted infections. Am J Reprod Immunol. 2011;65(3):196–211. Epub 2011/02/08. 10.1111/j.1600-0897.2011.00970.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Porter E, Yang H, Yavagal S, Preza GC, Murillo O, Lima H, et al. Distinct defensin profiles in Neisseria gonorrhoeae and Chlamydia trachomatis urethritis reveal novel epithelial cell-neutrophil interactions. Infect Immun. 2005;73(8):4823–33. Epub 2005/07/26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Haase AT. Targeting early infection to prevent HIV-1 mucosal transmission. Nature. 2010;464(7286):217–23. Epub 2010/03/12. 10.1038/nature08757 [DOI] [PubMed] [Google Scholar]
- 84.Politch JA, Marathe J, Anderson DJ. Characteristics and quantities of HIV host cells in human genital tract secretions. J Infect Dis. 2014;210 Suppl 3:S609–15. Epub 2014/11/22. 10.1093/infdis/jiu390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Belec L, Ghys PD, Hocini H, Nkengasong JN, Tranchot-Diallo J, Diallo MO, et al. Cervicovaginal secretory antibodies to human immunodeficiency virus type 1 (HIV-1) that block viral transcytosis through tight epithelial barriers in highly exposed HIV-1-seronegative African women. J Infect Dis. 2001;184(11):1412–22. Epub 2001/12/26. [DOI] [PubMed] [Google Scholar]
- 86.Carreno MP, Krieff C, Irinopoulou T, Kazatchkine MD, Belec L. Enhanced transcytosis of R5-tropic human immunodeficiency virus across tight monolayer of polarized human endometrial cells under pro-inflammatory conditions. Cytokine. 2002;20(6):289–94. Epub 2003/03/14. [DOI] [PubMed] [Google Scholar]
- 87.Costiniuk CT, Jenabian MA. Cell-to-cell transfer of HIV infection: implications for HIV viral persistence. The Journal of general virology. 2014;95(Pt 11):2346–55. Epub 2014/08/26. 10.1099/vir.0.069641-0 [DOI] [PubMed] [Google Scholar]
- 88.Kinlock BL, Wang Y, Turner TM, Wang C, Liu B. Transcytosis of HIV-1 through vaginal epithelial cells is dependent on trafficking to the endocytic recycling pathway. PLoS One. 2014;9(5):e96760 Epub 2014/05/17. 10.1371/journal.pone.0096760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Saidi H, Magri G, Carbonneil C, Bouhlal H, Hocini H, Belec L. Apical interactions of HIV type 1 with polarized HEC-1 cell monolayer modulate R5-HIV type 1 spread by submucosal macrophages. AIDS Res Hum Retroviruses. 2009;25(5):497–509. Epub 2009/04/29. 10.1089/aid.2008.0156 [DOI] [PubMed] [Google Scholar]
- 90.Saidi H, Magri G, Nasreddine N, Requena M, Belec L. R5- and X4-HIV-1 use differentially the endometrial epithelial cells HEC-1A to ensure their own spread: implication for mechanisms of sexual transmission. Virology. 2007;358(1):55–68. Epub 2006/08/29. [DOI] [PubMed] [Google Scholar]
- 91.Wu Z, Chen Z, Phillips DM. Human genital epithelial cells capture cell-free human immunodeficiency virus type 1 and transmit the virus to CD4+ Cells: implications for mechanisms of sexual transmission. J Infect Dis. 2003;188(10):1473–82. Epub 2003/11/19. [DOI] [PubMed] [Google Scholar]
- 92.Hein M, Valore EV, Helmig RB, Uldbjerg N, Ganz T. Antimicrobial factors in the cervical mucus plug. Am J Obstet Gynecol. 2002;187(1):137–44. Epub 2002/07/13. [DOI] [PubMed] [Google Scholar]
- 93.Ming L, Xiaoling P, Yan L, Lili W, Qi W, Xiyong Y, et al. Purification of antimicrobial factors from human cervical mucus. Hum Reprod. 2007;22(7):1810–5. Epub 2007/05/22. [DOI] [PubMed] [Google Scholar]
- 94.Schumacher GF, Kim MH, Hosseinian AH, Dupon C. Immunoglobulins, proteinase inhibitors, albumin, and lysozyme in human cervical mucus. I. Communication: hormonal profiles and cervical mucus changes—methods and results. American journal of obstetrics and gynecology. 1977;129(6):629–36. Epub 1977/11/15. [DOI] [PubMed] [Google Scholar]
- 95.Nazli A, Chan O, Dobson-Belaire WN, Ouellet M, Tremblay MJ, Gray-Owen SD, et al. Exposure to HIV-1 directly impairs mucosal epithelial barrier integrity allowing microbial translocation. PLoS Pathog. 2010;6(4):e1000852 Epub 2010/04/14. 10.1371/journal.ppat.1000852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kohli A, Islam A, Moyes DL, Murciano C, Shen C, Challacombe SJ, et al. Oral and vaginal epithelial cell lines bind and transfer cell-free infectious HIV-1 to permissive cells but are not productively infected. PLoS One. 2014;9(5):e98077 Epub 2014/05/27. 10.1371/journal.pone.0098077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Chomont N, Hocini H, Gody JC, Bouhlal H, Becquart P, Krief-Bouillet C, et al. Neutralizing monoclonal antibodies to human immunodeficiency virus type 1 do not inhibit viral transcytosis through mucosal epithelial cells. Virology. 2008;370(2):246–54. Epub 2007/10/09. [DOI] [PubMed] [Google Scholar]
- 98.Cavarelli M, Foglieni C, Rescigno M, Scarlatti G. R5 HIV-1 envelope attracts dendritic cells to cross the human intestinal epithelium and sample luminal virions via engagement of the CCR5. EMBO molecular medicine. 2013;5(5):776–94. Epub 2013/04/23. 10.1002/emmm.201202232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Dezzutti CS, Guenthner PC, Cummins JE Jr., Cabrera T, Marshall JH, Dillberger A, et al. Cervical and prostate primary epithelial cells are not productively infected but sequester human immunodeficiency virus type 1. J Infect Dis. 2001;183(8):1204–13. Epub 2001/03/23. [DOI] [PubMed] [Google Scholar]
- 100.Meng G, Wei X, Wu X, Sellers MT, Decker JM, Moldoveanu Z, et al. Primary intestinal epithelial cells selectively transfer R5 HIV-1 to CCR5+ cells. Nat Med. 2002;8(2):150–6. Epub 2002/02/01. [DOI] [PubMed] [Google Scholar]
- 101.Mingyan Y, Xinyong L, De Clercq E. NF-kappaB: the inducible factors of HIV-1 transcription and their inhibitors. Mini reviews in medicinal chemistry. 2009;9(1):60–9. Epub 2009/01/20. [DOI] [PubMed] [Google Scholar]
- 102.Pande V, Ramos MJ. Nuclear factor kappa B: a potential target for anti-HIV chemotherapy. Current medicinal chemistry. 2003;10(16):1603–15. Epub 2003/07/23. [DOI] [PubMed] [Google Scholar]
- 103.Eccleston A . Chemokine inhibitors for HIV. Nature biotechnology. 1997;15(8):709, 10. Epub 1997/08/01. [DOI] [PubMed] [Google Scholar]
- 104.Olson WC, Rabut GE, Nagashima KA, Tran DN, Anselma DJ, Monard SP, et al. Differential inhibition of human immunodeficiency virus type 1 fusion, gp120 binding, and CC-chemokine activity by monoclonal antibodies to CCR5. J Virol. 1999;73(5):4145–55. Epub 1999/04/10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Oravecz T, Pall M, Norcross MA. Beta-chemokine inhibition of monocytotropic HIV-1 infection. Interference with a postbinding fusion step. J Immunol. 1996;157(4):1329–32. Epub 1996/08/15. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A2EN cells on cell culture inserts were infected with CT serovar D. Supernatants from mock or CT-infected A2EN cells were collected after 72 h and incubated with either TZM-bl cells or MT4-R5 cells for 24 h. 10 TCID50 was then added to each well of TZM-bl cells or to 2 x 105 MT4-R5 cells. (A, B) Virus exposed TZM-bl cells were assayed for luciferase expression 48 h after virus addition. (C, D) Virus exposed MT4-R5 T cells were incubated for 6 d. The culture medium was then tested for infectious HIV after transfer to TZM-bl cells. Controls included TZM-bl cells incubated with a known amount of virus or an equivalent volume of KFSM medium alone. Data shown is expressed as percentage of the mean RLU obtained with KFSM controls. Bars represent the mean percentages ± SD. Data is representative of 3 independent experiments, each performed in quadruplicate. *p < 0.05.
(TIF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.