Abstract
Findings are presented from the first randomized clinical trial that compared changes in alcohol consumption and alcohol-related consequences among college student drinkers from baseline to follow-up across four conditions: (a) a new single component injunctive norms brief motivational intervention (IN-BMI) condition, (b) a single component descriptive norms brief motivational intervention (DN-BMI), (c) a Combined IN and DN brief motivational intervention (Combined-BMI), and (d) assessment-only control. DN-BMI focused on the juxtaposition of personal, perceived, and actual alcohol use by typical same-sex students at your university. INBMI focused on the juxtaposition of personal, perceived, and actual attitudes about alcohol related consequences by the typical same-sex student at your university. Exploratory analyses assessed the effect of IN-BMI and DN-BMI on matched (e.g., the effect of DN-BMI on perceived DN) and mismatched norms (e.g., the effect of DN-BMI on perceived IN). IN-BMI resulted in greater decreases in alcohol use and consequences when delivered alone and in conjunction with DN-BMI compared to the control condition. Further, the Combined-BMI condition reported greater reductions in alcohol use but not consequences compared to the DN condition. Receiving IN-BMI either alone or in combination with DN-BMI produced greater changes in IN perceptions than were produced in the control group. Grounded in norms theory, this study examined how college student problem drinking is affected by both IN-BMI and DN-BMI alone and in combination. We conclude that IN-BMI alone or in combination with DN-BMI is able to modify alcohol use and reduce alcohol related consequences.
Keywords: College Students, Alcohol, Injunctive Norms, Descriptive Norms, Randomized Clinical Trial
Alcohol use among college students remains a major public health concern. Nearly half of all college students endorse heavy episodic drinking in the past month (Hingson, Zha, and Weitzman, 2009). Heavy alcohol use among college students is associated with alcohol related consequences including physical injury, unprotected sex, and even death (Hingson et al., 2009). Further, Martinez, Sher, and Wood (2014) have shown that for a sizeable proportion of college students, alcohol related consequences accumulate throughout college, such that experiencing negative consequences predicts subsequent alcohol use rather than serving as a deterrent – a worrisome symptom of an alcohol use disorder (American Psychiatric Association, 2013). Longitudinal data from national surveys describe disquieting trends indicating that among college students, alcohol related deaths, heavy drinking, and reports of driving while intoxicated rose between 1998 and 2005 (Hingson et al., 2009). Accordingly, there is a need to improve the magnitude of effectiveness of available risk reduction interventions for college student drinkers.
Most college students overestimate the amount of alcohol that their peers consume (i.e., descriptive norms), as well as the permissiveness of the social environment with regard to risky drinking behaviors (i.e., injunctive norms; Borsari & Carey, 2003). These exaggerated perceptions are associated with heavier drinking (e.g., Lee, Geisner, Lewis, Neighbors, & Larimer, 2007). A number of individual empirical studies have demonstrated that correcting students’ perceptions of peer drinking using accurate descriptive norms (known as normative reeducation) promotes decreases in consumption (e.g., Reid & Carey, 2015). However, a large-scale integrated data meta-analysis highlighted the small effects associated with current forms of normative feedback interventions (cf. Huh et al., 2015). Thus, there is a need to improve upon descriptive normative re-education through the development of novel risk reduction strategies targeting college drinkers.
Cialdini, Reno, and Kallgren (1990) define social norms as consisting of two parts affecting human motivation, (a) the “is” (Descriptive Norm) defines what is normal behavior, and (b) the “ought” (Injunctive Norm) defines what is morally sanctioned behavior. The Focus Theory of Normative Conduct (Cialdini, Reno, & Kallgren, 1990) proposes that normative perceptions provide a shortcut that guides decision-making. For example, students may think that if their peers are engaging in a given behavior, then it must be an appropriate and reasonable behavior that they should be engaging in as well. Some students may even believe that the normative behavior is expected or sanctioned by one's peers, so engaging in that behavior will result in acceptance by the peer group.
Exaggerated perceptions of both descriptive norms (DN) and injunctive norms (IN) are prevalent (Perkins, Haines, & Rice, 2005), and both are independently associated with greater alcohol consumption (e.g., Larimer, Turner, Mallett, & Geisner, 2004; Lee, Geisner, Lewis, Neighbors, & Larimer, 2007; Neighbors, Lee, Lewis, Fossos, & Larimer, 2007; Park & Smith, 2007). However, the vast majority of social-norms based interventions focus on changing DN alone (Lewis & Neighbors, 2006; Miller, Leffingwell, Claborn, Meier, Walters, & Neighbors, 2013). Personalized feedback on DN has been shown to be effective in facilitating short-term reductions in alcohol consumption both using in-person (e.g., Borsari & Carey, 2000) and web-based (e.g., Neighbors, Larimer, & Lewis, 2004) intervention formats. Moreover, interventions that target DN feedback as a primary intervention component have been associated with larger effect sizes than those that do not (Carey, Scott-Sheldon, Carey, & DeMartini, 2007; Carey, Scott-Sheldon, Elliott, Garey, & Carey, 2012). Mediation analyses have shown that normative correction is an active ingredient explaining behavior change (e.g., Reid & Carey, 2015). Thus correcting exaggerated DN has been treated as an active ingredient of efficacious brief interventions. However, given that even efficacious interventions using DN feedback produce small-medium effects (Carey, Scott-Sheldon, Carey, & DeMartini, 2007; Huh et al., 2015) there is a strong case to be made for developing new and more efficacious interventions for college drinking.
Inspiration for enhancing the efficacy of feedback-based interventions comes from a well-studied theory that promotes the notion that DN and IN refer to separate sources of human motivation (Cialdini et al., 1990). Thus, the development of an IN feedback intervention for college drinkers is a natural next step. Only two alcohol prevention studies evaluated facilitatorled group interventions designed to change IN, reporting mixed results (Barnett, Far, Mauss, & Miller, 1996; Schroeder & Prentice, 1998). Barnett and colleagues (1996) demonstrated changes in both DN and IN immediately following a combined DN + IN feedback. Schroeder and Prentice (1998) found changes only for males in perceived norms following either a discussion about pluralistic ignorance (i.e., the assumption that one's privately held beliefs are more conservative than others’ beliefs despite engaging in similar behavior to others; Miller & McFarland, 1991) or an individualized discussion about responsible decision making at a 4- to 6-month follow-up. These interventions did not provide sufficient specificity in research design or intervention content to draw strong inferences about the effects of DN and IN feedback alone and/or in combination.
More recently, Prince and Carey (2010) demonstrated that perceptions about other students’ acceptability of excessive drinking (i.e., perceived IN) could be changed with brief feedback about others’ true attitudes about excessive drinking. This study also showed that in response to receiving feedback solely about injunctive norms, students also changed their perceived descriptive norms. The authors suggested a correspondence bias (Gilbert & Malone, 1995) that students may have been using when changing their perceptions. Specifically, participants generalized the information that students disapprove of excessive drinking (IN) to modify their estimates of students’ alcohol consumption (DN). This study provides a proof of the concept that perceived injunctive norms are amenable to change with brief feedback. However, this study did not link those changes in perception to changes in alcohol use or consequences.
Despite limited research examining injunctive norms feedback for college drinkers, interventions designed for health behaviors besides alcohol use have demonstrated that IN interventions result in behavior change (Mahler, Kulik, Butler, Gerrard & Gibbons, 2008; Schultz, Nolan, Cialdini, Goldstein, & Griskevicius, 2007, Reid & Aiken, 2013), and combined DN + IN interventions may be more effective than basic interventions (Mahler et al., 2008; Reid & Aiken, 2013).
It follows then that a well-designed IN intervention for reducing college drinking has the potential to reduce college drinking when given alone or to increase the effectiveness of current DN interventions when added to existing protocols. Prince and Carey (2010) demonstrated that IN are malleable in college drinkers; however, at this point we can only extrapolate from other fields the potential effect that changing IN might have on excessive drinking behavior. Providing students with both DN + IN intervention strategies may have a positive additive effect, enhancing intervention efficacy for at risk college drinkers.
Normative feedback has been shown to be more effective under certain conditions. First, Walters, Vader, Harris, Field, and Jouriles (2009) demonstrated that personalized feedback is more powerful when delivered face-to-face compared to feedback presented online or mailed. Second, feedback is most effective when delivered using a Motivational Interviewing style (Murphy et al., 2004; Murphy, Dennhardt, Skidmore, Martens, & McDevitt-Murphy, 2010). Finally, research has shown that selection of a referent group is critical for facilitating behavior change in norms feedback interventions (cf., Neighbors et al., 2008). Larimer et al. (2009) recommend using a referent group that targets at least one level of specificity to the participant beyond the typical student (e.g., typical same-sex student).
The purpose of this study was to develop a personalized single component IN brief motivational intervention (IN-BMI) designed to re-educate students about the true attitudes of other students at the same university with regard to the acceptability of adverse alcohol consequences. We sought to optimize efficacy by delivering the intervention material in person, using a Motivational Interviewing style, and by testing the efficacy of IN-BMI and a single component DN brief motivational intervention (DN-BMI) alone and in combination compared to an assessment only control group.
This protocol is an improvement over existing intervention techniques because it addresses both primary sources of social norms information, namely perceptions about what other people do and what others approve (Cialdini, Reno, & Kallgren, 1990). Furthermore, we follow recommendations grounded in the Focus Theory of Normative Conduct that aligning IN and DN should enhance the normative correction effect (Reid, Cialdini, & Aiken, 2010). By adding the IN-BMI to the current DN based intervention protocol, students will not only gain more accurate knowledge about how much their peers are drinking, but also will become better informed about beliefs held by their peers with regard to adverse alcohol consequences.
Primary Hypotheses
Hypothesis 1
All active conditions will reduce alcohol use and consequences more than the control group.
Hypothesis 2
Combined descriptive and injunctive norms brief motivational intervention (Combined-BMI) will reduce alcohol use and consequences more than the DN-BMI alone.
Exploratory Hypotheses
Given the limited number of intervention studies including IN-BMI, we sought to test the extent to which DN-BMI and IN-BMI specifically changed matched norms (e.g., the effect of DN-BMI on DN perceptions). Based on studies suggesting that descriptive and injunctive norms are unique constructs (e.g., Lee et al., 2007; Merrill, Carey, Reid, & Carey, 2014), we hypothesized that DN-BMI would facilitate changes in perceived descriptive norms, that IN-BMI would facilitate changes in perceived injunctive norms, and that the Combined-BMI would facilitate changes in both perceived descriptive and injunctive norms. However, given the evidence presented by Prince and Carey (2010) for a correspondence bias following IN feedback, we were also interested in assessing for changes in mismatched norms (e.g., the effect of DNBMI on IN perceptions).
Exploratory hypothesis 1
DN-BMI and IN-BMI alone will change matched normative perceptions more than the control group.
Exploratory hypothesis 2
Combined-BMI feedback will change perceptions of both DN and IN more than the control group.
Exploratory hypothesis 3
DN-BMI and IN-BMI will change mismatched perceptions due to the correspondence bias.
Method
Design
The research design was a randomized factorial 2 (IN-BMI: yes or no) × 2 (DN-BMI: yes or no) × 2 (time: baseline and 4-6 weeks follow-up) design yielding four independent intervention conditions: a Combined-BMI, DN-BMI only, IN-BMI only, and an assessment-only control. Primary outcome variables were collected for the past 30-day interval and included level of intoxication on a typical night (tBAC; estimated typical blood alcohol concentration; cf. Agrawal, et al., 2009) and number of alcohol related consequences (ARC). ARC were assessed in addition to alcohol use because ARC are an indicator of functional impairment due to alcohol use. Secondary outcome measures were participants’ ratings of DN and IN that were used to assess specific intervention effects on matched and mismatched norms. The control group participated in assessments to control for research and assessment reactivity as well as history/maturation effects.
Participants
Participants were college students recruited from Introductory Psychology classes who were screened for current levels of alcohol use. Students were eligible to participate in the study if they reported at least one heavy drinking day (i.e., 5+ drinks for men/4+ drinks for women; Wechsler, Davenport, Dowdall, & Moeykens, 1994) in the past month and were 18 years of age or older. All provided informed consent prior to their participation. The initial baseline assessment to gather background information and the intervention occurred on the same day. A web-based follow-up assessment was conducted 4- to 6-weeks later. Similar follow-up intervals have been sensitive in detecting the effects of brief alcohol interventions (Carey et al., 2007). Participants were given course credit to complete the baseline assessment, the face-to-face intervention, and the post-intervention assessment, and they received a modest economic incentive (i.e., $15) for completing the follow-up assessment.
In the baseline assessment, students reported on their own alcohol use and attitudes about adverse alcohol consequences as well as their perceptions about the typical university student's use (i.e., DN) and attitudes about adverse alcohol consequences (i.e., IN). These data were used to create the personalized feedback form described below. The post-intervention assessment included manipulation check and satisfaction check items. In the follow-up assessment participants completed the same battery of measures as in the baseline survey to allow direct comparison.
Measures
Alcohol use
A multidimensional alcohol use assessment included questions regarding the number of typical drinks per drinking day and hours spent drinking to allow calculation of estimated typical BAC (Carey, Henson, Carey, & Maisto, 2009). Personal alcohol consumption in a typical and heavy week in the last month were also assessed using a 7-day grid (Baer, 1994) to allow for direct comparison to survey data presented in the DN-BMI.
Alcohol related consequences
The 24-item Brief Young Adult Alcohol Consequences Questionnaire (BYAACQ; Kahler, Strong, & Read, 2005) assessed the frequency of alcohol-related consequences in the last 30 days. Participants responded “yes” or “no” to 24 statements addressing possible consequences experienced during or following alcohol use (e.g., hangover, memory blackouts).
Descriptive norms
Perceived DN (for the “typical same-sex student at your university”) were assessed using a 7-day grid to assess perceptions of peer alcohol use (Baer, 1994).
Injunctive norms
The injunctive norms assessment consisted of a modified version of the BYAACQ where students were asked to rate the perceived acceptability of the 24 alcohol related consequences by a “typical same-sex student at your university” on a 6 point Likert scale (i.e., 1 = highly unacceptable, 2 = moderately unacceptable, 3 = fairly unacceptable, 4 = fairly acceptable, 5 = moderately acceptable, 6 = highly acceptable). Cronbach's alpha was .94 at baseline and .94 at follow-up.
Manipulation check
Students who received an intervention were asked five yes/no questions testing their ability to recognize information that either was or was not presented to them in the intervention. Two of the questions referred to content included in the interventions and three of the questions referred to content not included in the interventions. The question targeting whether participants were exposed to DN-BMI asked whether they were provided with information regarding how much other students drink. The question targeting whether participants were exposed to IN-BMI asked whether students discussed what other students think about excessive drinking. The remaining three questions asked about learning how to reduce BAC, what organs can be damaged by alcohol use, and how many calories are in alcoholic beverages.
Intervention satisfaction
Students were asked three questions regarding their satisfaction with the intervention (i.e., how satisfied, how likely to share information, how interesting), using a 1 (highly satisfied) to 6 (highly dissatisfied) scale.
Normative feedback intervention
Each of the individual interventions took approximately 15 minutes to complete, and the Combined-BMI took approximately 30 minutes to complete; all were audio recorded for supervision purposes. Interventionists were three clinical psychology Ph.D. students who completed training in Motivational Interviewing, (Miller & Rollnick, 2012) including directed readings, MI training DVDs, and supervised role-plays. Interventionists participated in additional specialized training covering the intervention manual for the current protocol. Interventionists were supervised throughout the study by the second author, a licensed clinical psychologist, and the first author to ensure consistent intervention delivery. In total, training time for interventionists ranged from 4-5 hours of didactic training. The training protocol was a shortened version of the training that interventionists received for a previous multi-component intervention conducted by the fourth author and the second author (see Carey, Carey, Maisto, & Henson, 2006). Participants were randomly assigned to one of the three interventionists to complete the intervention, and all interventionists delivered all three intervention conditions. Interventions were manualized, and feedback elements were modeled after previously tested face-to-face motivational interviewing based norms interventions (e.g., Brief Alcohol Screening and Intervention for College Students (BASICS); Dimeff, Baer, Kivlahan, & Marlatt, 1999).
Referent group for normative feedback
Neighbors and colleagues (2008) assessed a variety of referent groups for both descriptive and injunctive norms and recommended typical same sex student as a preferred referent group for both types of normative feedback. However, they noted that injunctive norms may be more complex than descriptive norms, with fluctuations seen in the relationship between injunctive norms and drinking varying with the proximity of the referent group. Moreover, Larimer and colleagues (2009) recommended that at least one level of specificity to the participant (e.g., typical students at your school) be used for normative feedback interventions. Following these recommendations, we used “Same Sex Students at your university” as the referent group, providing students with two levels of specificity, which has been shown to enhance personalization and relevance (Larimer et al., 2009). This referent group has two primary advantages: (a) it controls for gender differences in alcohol consumption (Larimer et al., 2009), and (b) university-specific data are available at this level of specificity to compare to students’ perceptions about the consumption and attitudes of this group in the interventions.
Intervention content
Both the DN-BMI and IN-BMI followed the same general format but differed in the specific content of the personalized feedback and normative comparisons. First, the common structure will be described, followed by the specific content. Data from the baseline survey were used to create a personalized normative feedback form, which the interventionist used to guide the intervention discussion. As noted earlier, previous studies have shown that students tend to overestimate both their peers’ actual alcohol use as well as their peers’ acceptability of excessive drinking. The interventions were designed to create discrepancy through identifying self-other differences in two ways. The interventionist used available survey data on student drinking behaviors and attitudes to create normative data for the typical same sex student at the university and then compared the student's personal use and personal attitudes to the actual use and actual attitudes of typical university students (personal norms vs. actual norms). The DN-BMI referent sample (N = 1868) consisted of a composite of participants recruited to studies at the university, with an overall mean of 6.45 drinks per week. This composite sample included 8 subsamples collected over 8 years (i.e., 2001-2009) from the university's subject pool. The IN-BMI referent sample (N = 324) was similarly collected from the university's subject pool. The average acceptability of alcohol related consequences in the referent group sample was 2.01, which was equivalent to a rating of “moderately unacceptable” (1 = highly unacceptable, 2 = moderately unacceptable, 3 = fairly unacceptable, 4 = fairly acceptable, 5 = moderately acceptable, 6 = highly acceptable). In addition, the interventionist used the survey data to compare participants’ perceptions of the typical same sex student's use/attitudes to the actual behavior and attitudes of the typical same sex student (perceived norms vs. actual norms). The interventionist used a motivational interviewing style to guide students through personalized feedback and normative comparisons, giving them an opportunity to discuss their reactions to the information presented.
The specific goal of the DN-BMI was to revise behavioral norms downward, challenging students’ exaggerated perceptions about their peers’ drinking behaviors. This was achieved by presenting participants with accurate information about students’ drinking on campus. Often participants would learn that most students drink a smaller amount of alcohol than expected. The specific content of the DN-BMI involved a review of the participant's reported current personal alcohol use (i.e., number of drinking days, average number of drinks per week, maximum drinks in a single day, number of drinks during the heaviest week of drinking, and number of heavy drinking episodes) juxtaposed with his or her rank (percentile) among same-sex students at your university regarding typical drinks per week (e.g., You told me you drank 25 drinks per week, that means that you drank more than 85% of all male students at your university) and number of heavy drinking days (e.g., You reported 5 heavy drinking days, that means you had more heavy drinking days than 85% of all male students at your university). Next students were presented with a bar graph which included the student's current personal drinks in a typical week, the student's perception of how many drinks the typical student at your university drank in a typical week and the actual number of drinks per week that were consumed by the typical student at your university (e.g., “You reported drinking 15 drinks per week, you told us that you thought that the typical male student drank 25 drinks per week, and in reality the typical male student at your university actually only drinks 9 drinks per week”). After reviewing the graph students were told the difference between the number of drinks they thought the typical same sex student at your university was drinking and the actual number of drinks the typical same sex student at your university drinks (e.g., “You overestimated the drinking of male students at your university by 16 drinks per week”). Following the personalized DN-BMI, the student was prompted to consider the potential etiology of his or her exaggerated perceptions (or his/her ability to accurately judge) about peer drinking behaviors, as well as the implications of overestimation. In total, students in the DN-BMI condition received 10 points of feedback.
The specific goal of the IN-BMI was to revise perceptions of peer approval of alcohol consequences downward by challenging perceptions that peers find adverse alcohol consequences acceptable. This was achieved by presenting students with information that most of their peers find adverse alcohol consequences unacceptable. Specifically, the IN-BMI began by presenting students with their current personal attitudes regarding which consequences they considered to be the most acceptable (i.e., the two consequences they rated as most acceptable) and most unacceptable (i.e., the two consequences they rated as most unacceptable). Students were then presented with the typical student's actual attitudes regarding those specific consequences (i.e., the modal response by the typical student from the referent group dataset). In the case of a tie (i.e., when a participant rated multiple items with the same level of acceptability), the interventionists were instructed to select the two consequences with the greatest discrepancy from the typical student approval ratings. The consequences included most often as most acceptable included “having a hangover” (61%), “feeling embarrassed” (34.21%), and “unplanned drinking” (30%). The consequences included most often as unacceptable included “missing class/work” (29%), “work quality suffering” (26%), and “spending too much time drinking” (18%). Next, students were presented with their personal average acceptability of alcohol related consequences juxtaposed with their perception of others average acceptability of alcohol related consequences, and with other actual average acceptability of alcohol related consequences. Finally, students were presented with three histograms showing the percent endorsing each acceptability level for “blacking out”, “passing out”, and “sexual regret”, which also included arrows indicating their personal attitudes regarding each of these consequences and the actual attitudes of the typical same sex student regarding these consequences. For example, in this final section, a participant may have heard, “You personally rated passing out as a result of drinking alcohol as highly unacceptable, 95% of students at your university agree with you that passing out as a result of drinking alcohol is highly unacceptable.” Following the personalized IN-BMI, the students were prompted to consider the potential etiology of their exaggerated perceptions about (or their ability to accurately judge) peer attitudes about adverse alcohol consequences, as well as the possible implications of overestimation. In total, students in the IN-BMI condition received 10 points of feedback.
The Combined-BMI included all of the elements of both the DN-BMI and IN-BMI described above. In total students in the Combined-BMI condition received 20 points of feedback.
Fidelity check
A checklist of the intervention material was created, to assess whether interventionists covered the appropriate intervention material in each intervention. The first author reviewed 25% of the completed intervention audio recordings (i.e., 33 recordings in total) that were randomly selected using a random number generator. In general, the fidelity checklist was composed of the 10 points specific to the DN-BMI, and 10 points specific to the IN-BMI, as well as a check that the interventionist discussed the risks of overestimating the amount one's peers drink (DN-BMI) or the risk of overestimating the acceptability by one's peers of alcohol related consequences (IN-BMI). The Combined-BMI conditions needed to include all 22 points.
Analyses
Following normality tests and appropriate transformations when necessary, the two dependent variables (i.e., ARC and tBAC) were computed. Dependent variables were change scores (sometimes called gain scores) that were calculated by subtracting the baseline value from the follow-up value for each participant. Change scores were chosen because the analysis of group differences of change scores is identical to the analysis of covariance with baseline values as the covariate and follow-up values as the dependent variable; however, by not estimating the slope parameter an extra degree of freedom is gained, which adds statistical power for small samples (Maxwell & Delaney, 2004).
The analysis strategy varied for primary and exploratory hypotheses. Primary hypothesis 1 compared each active intervention condition (i.e., DN-BMI, IN-BMI, and Combined-BMI) to the control group, and was thus tested with two one-way analyses of variance (ANOVAs) with intervention condition as the independent variable. Dunnett's procedure was used to control for alpha inflation when conducting the pair-wise comparisons. This procedure is the preferred method for testing intervention conditions against a control group and balances statistical power with experiment-wise alpha control (Ruxton & Beauchamp, 2008; Maxwell & Delaney, 2004). Primary hypothesis 2 (comparisons between the Combined-BMI group and the DN-BMI group) were tested using a priori independent samples t-tests with change scores as the dependent variables. Because unique hypotheses were tested with a set of planned comparisons, we evaluated a priori pairwise contrasts regardless of the outcome of the omnibus test of the ANOVAs (Ruxton & Beauchamp, 2008).
The exploratory hypotheses were also tested with independent-samples t-tests, except that a Bonferroni correction was applied to control for alpha inflation (α = .05/3 = .017). In addition, we presented Cohen's d effect sizes for all pairwise comparisons of group differences in changes in ARC and tBAC separately from the planned comparisons. Effect size estimates provide information about the magnitude and direction of group differences without adding additional significance tests (Tabachnick & Fidell, 2007).
Results
Participants and Randomization check
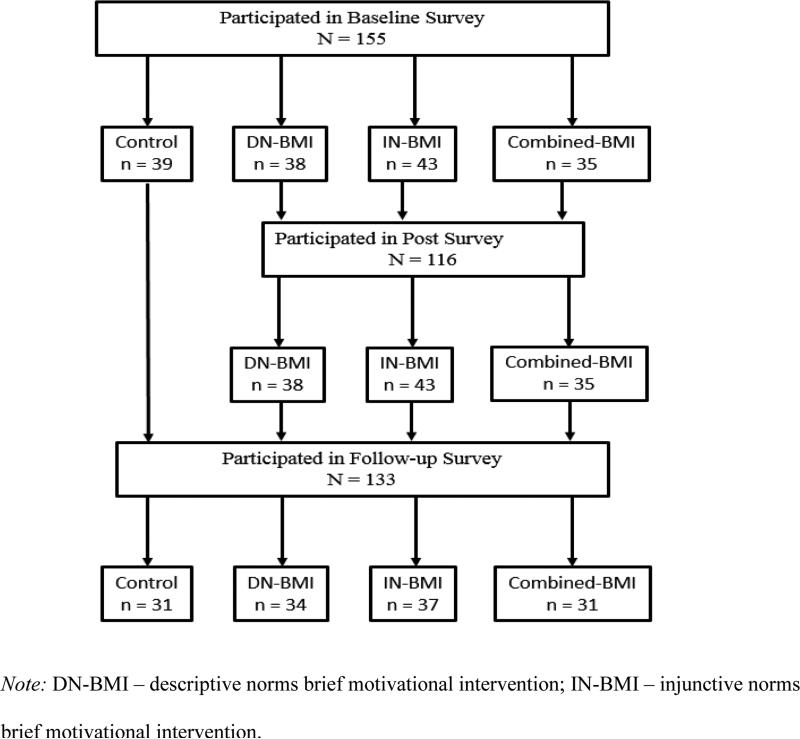
The current sample was 48% female, and predominately Caucasian (77%) and non-Hispanic (88%). Table 1 presents baseline and follow-up alcohol use and consequences and DN and IN ratings by condition and for the complete sample. Table 1 also presents within group Cohen's d effect sizes for each group and the overall sample demonstrating the magnitude of the change in each variable from baseline to follow-up. There were no differences among the conditions on alcohol use or consequences variables at baseline, on any of the demographic variables (e.g., gender, ethnicity), or on either of the norms measures (i.e., descriptive norms at baseline, injunctive norms at baseline), ps > .05 for t-tests, one-way ANOVAs or chi-square tests, as appropriate. The baseline sample included 155 college students of which 133 completed the follow-up survey. A Consolidated Standards of Reporting Trials (CONSORT) diagram is presented in Figure 1. Further, there were no differences in attrition across groups, and missingness was not associated with alcohol use, ARC, or DN or IN perceptions at follow-up, ps > .05. Finally, although the follow-up assessment was scheduled for 4-6 weeks following the intervention, post-treatment data collection continued beyond that period resulting in lengthy follow-up times for some participants (M = 7.99 weeks, SD = 4.01, Median = 6.71 weeks, range: 4-23 weeks). However, time-to-follow-up was not associated with tBAC, ARC, DN or IN at follow-up nor with any of the change scores, ps > .05.
Table 1.
Baseline and follow-up drinking, consequences and norms ratings by condition.
| Control | IN-BMI | DN-BMI | Combined-BMI | Total | |
|---|---|---|---|---|---|
| n | n | n | n | N | |
| Baseline | 39 | 43 | 38 | 35 | 155 |
| Follow-up | 31 | 37 | 34 | 31 | 133 |
| M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | |
| tBAC | |||||
| Baseline | .09 (.13) | .12 (.14) | .09 (.06) | .10 (.08) | .10 (.11) |
| Follow-up | .07 (.07) | .07 (.07) | .09 (.13) | .07 (.10) | .07 (.09) |
| Cohen's dw | 0.10 | 0.78 | 0.19 | 0.88 | 0.83 |
| ARC | |||||
| Baseline | 6.16 (4.19) | 7.05 (4.27) | 6.18 (4.07) | 6.94 (4.30) | 6.59 (4.19) |
| Follow-up | 5.87 (4.19) | 4.86 (3.99) | 4.61 (3.56) | 4.90 (3.42) | 5.05 (3.79) |
| Cohen's dw | 0.05 | 0.60 | 0.39 | 0.62 | 0.42 |
| DN-rating | |||||
| Baseline | 30.29 (21.27) | 23.70 (13.92) | 22.66 (9.95) | 24.57 (14.67) | 24.27 (15.59) |
| Follow-up | 26.13 (14.19) | 15.95 (6.55) | 14.09 (5.05) | 15.09 (6.70) | 17.67 (9.84) |
| Cohen's dw | 0.21 | 1.55 | 0.88 | 1.89 | 1.01 |
| IN-rating | |||||
| Baseline | 3.16 (.83) | 3.03 (.78) | 3.01 (.77) | 3.14 (.86) | 3.08 (.80) |
| Follow-up | 3.11 (.80) | 1.85 (.66) | 2.22 (.84) | 1.69 (.70) | 2.20 (.92) |
| Cohen's dw | 0.30 | 0.58 | 1.02 | 0.92 | 0.58 |
Note: IN-BMI = injunctive norms brief motivational intervention condition; DN-BMI = descriptive norms brief motivational intervention condition; IN-rating = perceived injunctive norms ratings; DN-rating = perceived descriptive norms ratings; tBAC= estimated typical blood alcohol content; ARC = alcohol related consequences; Cohen's dw = within group change effect size.
Figure 1.
CONSORT diagram.
Fidelity check
There were no instances of interventionists covering information in one intervention that belonged in another intervention (i.e., no evidence of cross-contamination), and the treatment fidelity rate (i.e., average percentage covered across the 22 items) was 99%.
Manipulation check
For questions targeting whether participants received DN-BMI, overall 89% of students responded “yes”, with 84% in the IN-BMI condition incorrectly responding with “yes”, 97% of students in the Combined-BMI condition correctly responding with “yes”, and 94% of students in the DN-BMI condition correctly responding with “yes”. In response to the question targeting whether participants received IN-BMI, nearly all students in the IN-BMI and Combined-BMI conditions responded correctly, but over half of those in the DN-BMI condition responded incorrectly (percent responding “yes”: Overall: 83%, IN: 97%, Combined-BMI: 100%, DN: 57%). In response to three questions targeting content not included in either form of feedback, nearly all students correctly answered that they had not received the corresponding information.
Intervention satisfaction
The majority of students reported being “highly satisfied” with the content of the intervention discussion (62%), with a higher percentage endorsing “highly satisfied” in the IN-BMI condition than in other conditions, IN-BMI: 74%; Combined-BMI: 66%; DN-BMI: 47%, χ2 (12) = 25.64, p < .01. The majority of students reported that they were either “moderately or very likely” to share the intervention material with their peers (66%), with the highest likelihood of sharing being reported by the Combined-BMI group, IN-BMI: 69%; Combined-BMI: 71%, DN-BMI: 58%, χ2 (18) = 44.31, p < .01. The most common response for the question regarding how interesting the intervention content was perceived was “Very Interesting” (49%), with the highest percentage of students reporting “Very Interesting” in the IN-BMI condition, IN: 60%, Combined-BMI: 46%, DN-BMI: 42%, χ2 (12) = 58.24, p < .01.
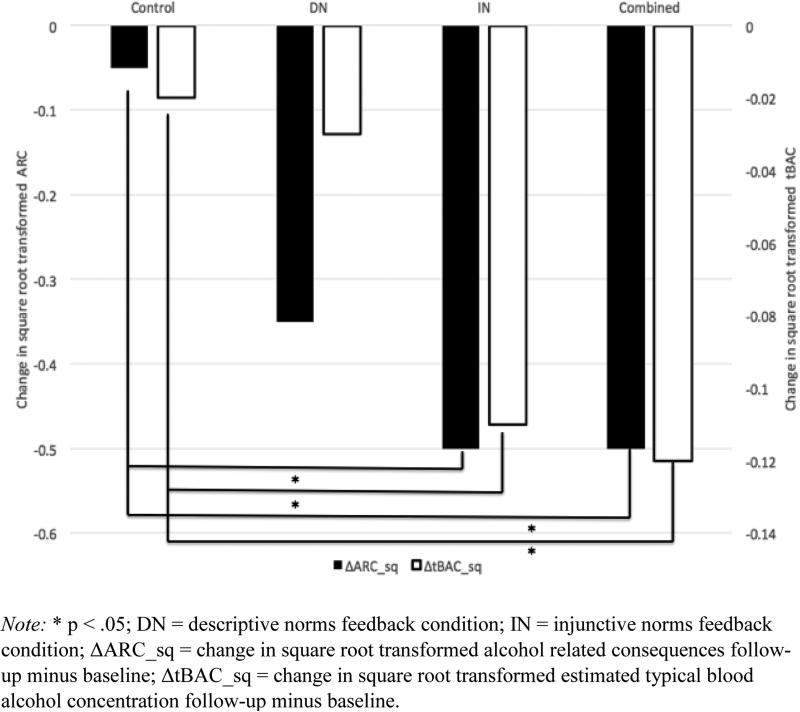
Primary Study Hypotheses
Both ARC and tBAC were positively skewed. Square root transformations were conducted to normalize the distributions. Change scores were calculated using the square root transformed variables. The final transformed distribution of the change scores exhibited skew within acceptable limits (change in square root transformed alcohol related consequences (ΔARCsq) skew = −.65 (SE = .21); change in square root transformed estimated typical blood alcohol concentration (ΔtBACsq) skew = −.26, (SE = .21); Tabachnick & Fidell, 2007). Untransformed means and standard deviations are presented in Table 1 for baseline and follow-up alcohol use and consequences ratings for ease of interpretation; Table 1 also contains within-group effect sizes, showing some degree of improvement in all groups. Figure 2 presents changes in square root transformed ARC and tBAC by group to aid in interpretation of the primary hypotheses described below.
Figure 2.
Primary outcomes: Changes in square root transformed ARC and tBAC by feedback condition.
Primary Hypothesis 1
Dunnett's method to control for alpha inflation was used to compare each group to the control group on change scores for ARC and tBAC. The IN-BMI group reported greater reductions in ARC than the control group, Mdiff = −.45 (SEdiff = .21), p = .047. The DN-BMI group and the control group showed no difference in ARC change, Mdiff = −.31 (SEdiff = .22), p = .179. The Combined-BMI group reported trend level greater reductions in ARC compared to the control group, Mdiff = −.45 (SEdiff = .22), p = .057. Similarly, the IN-BMI group reported greater reductions in tBAC than the control group, Mdiff = −.09 (SEdiff = .04), p = .029. The DN-BMI group and the control groups showed no difference in tBAC change, Mdiff = −.01 (SEdiff = .04), p = .625. The Combined-BMI group showed greater reductions in tBAC than the control group, Mdiff = −.10 (SEdiff = .04), p = .027.
Primary Hypothesis 2
Planned contrast independent samples t-tests comparing DNBMI to the Combined-BMI groups on changes in ARC and tBAC revealed that the Combined-BMI group reported greater changes in tBAC than the DN-BMI condition, Mdiff = −.09 (SEdiff = .04), p = .037, but that there were no differences between groups on changes in ARC, Mdiff = −.14 (SEdiff = .22), p = .517.
Description of effect size table
All pairwise Cohen's d effect sizes are presented in Table 2. We did not have a priori hypotheses about IN-BMI vs. DN-BMI and IN-BMI vs. Combined-BMI, but they may be of interest to some readers. Regarding the comparison of the IN-BMI and DN-BMI groups, there is a medium sized effect in favor of the IN-BMI group reporting greater changes in tBAC than the DN-BMI group but no effect for differences in changes in ARC. Regarding the IN-BMI and Combined-BMI groups comparison, the effect sizes suggest no difference in either tBAC or ARC between these two groups.
Table 2.
Cohen's d effects sizes for pairwise comparisons of differences in change in tBAC and ARC among conditions.
| Comparison | ΔtBAC | ΔARC |
|---|---|---|
| Control vs. IN-BMI | .58 | .51 |
| Control vs. DN-BMI | .07 | .35 |
| Control vs. Combined-BMI | .58 | .53 |
| IN-BMI vs. DN-BMI | −.51 | −.16 |
| IN-BMI vs. Combined-BMI | .04 | −.001 |
| DN-BMI vs. Combined-BMI | .51 | .16 |
Note: Cohen's d cutoffs: .2 = small, .5 = medium, .8 = large. tBAC = estimated typical blood alcohol content; ARC = alcohol related consequences; IN-BMI = injunctive norms brief motivational intervention condition; DN = descriptive norms brief motivational intervention condition; Positive value means that the second group had the larger change and negative value means the first group had the larger change (e.g., IN had greater change than control in the medium to large range).
Exploratory analyses
Exploratory analyses were conducted to describe specificity of DN-BMI and IN-BMI to differentially change normative perceptions. To provide an overall frame of reference for within group norms changes, as expected, paired t-tests revealed changes in both IN and DN perceptions from baseline to follow-up in all three active conditions (ps ≤ .01), and no significant changes in either IN or DN perceptions in the control group (ps > .05).
Exploratory hypothesis 1
Changes in matched norms were tested with independent samples t-tests. Results indicated that the IN-BMI group changed IN perceptions more than the control group, Mdiff = .94, SEdiff = .18, p < .001, but the DN-BMI group's change in DN perceptions did not differ from that of the control group, Mdiff = 2.76, SEdiff = 3.71, p = .460. Notably, the control group reported small reductions in both DN and IN perceptions from baseline to follow-up (Reduction in DN: d = 0.21; Reduction in IN: d = 0.30).
Exploratory hypothesis 2
Comparisons between the Combined-BMI and control groups in changes in DN and IN perceptions were tested with independent samples t-tests. These tests revealed that the Combined-BMI group reported greater changes in IN than the control group, Mdiff = 1.30, SEdiff = .20, p < .001, but no difference in change of DN perceptions, Mdiff = 5.07, SEdiff = 4.34, p = .247.
Exploratory hypothesis 3
One sample t-tests were conducted comparing change in mismatched norms to 0 in the IN and DN groups. The IN-BMI group did not report changes in DN perceptions greater than 0, Mdiff = .71, SEdiff = 3.93, p = .86; however, the DN-BMI group did report changes in IN perceptions greater than 0, Mdiff = .53, SEdiff = .19, p = .009.
Discussion
The current study developed and evaluated a brief, face-to-face personalized IN-BMI. This randomized controlled trial indicated that receiving personalized IN-BMI resulted in greater decreases in alcohol use and consequences when delivered alone and when delivered in conjunction with DN-BMI compared to an assessment only control group. Further, the Combined-BMI group reported greater reductions in alcohol use but not consequences compared to the DN-BMI group. Given evidence that the efficacy of DN-BMI is modest in general student samples such as this one (see also Huh et al., 2015), we propose that IN-BMI should be considered as an alternative intervention for college drinkers that can reduce alcohol use and alcohol related consequences. Interestingly, effect size estimates comparing the IN-BMI group to the Combined-BMI group do not suggest an advantage for combining IN-BMI and DN-BMI over providing IN-BMI alone. Moreover, students in the IN-BMI group reported the most interest and satisfaction with the feedback they received.
One primary difference between DN-BMI and IN-BMI is the typical pattern of information students received. In the DN group, students typically learned that they drank more than the typical student who in turn actually drinks less than they thought. In contrast, in the INBMI group, students typically learned that the typical student actually holds more conservative attitudes than they expected and that are more in line with their personally held attitudes about adverse alcohol consequences. One potential explanation for the stronger effect for the IN-BMI group is that they were given permission to act in a way that aligns with their values rather than modifying behavior to match the norm due to a feeling of cognitive dissonance that may be triggered by receiving DN-BMI (McNally, Palfai, & Kahler, 2005). Thus, IN-BMI may have been more acceptable and less threatening than DN-BMI. By extension, it is possible that the higher satisfaction ratings in the IN-BMI group may have resulted from having their personal values affirmed through learning that their peers held similarly conservative views regarding the acceptability of alcohol related consequences.
In addition to examining changes in alcohol use and consequences, this study explored the specificity of DN-BMI and IN-BMI to change matched norms. Overall, all three active conditions modified both DN and IN perceptions and the control group did not. However, an interesting pattern emerged when comparing changes in perceived norms among conditions. Receiving IN-BMI either alone or in combination with DN-BMI produced changes in IN perceptions more than the control group, but the same pattern did not hold for DN-BMI. DNBMI changed DN perceptions equal to the control group when given alone or in combination with IN-BMI. Further, as described above, DN-BMI produced small but non-significant changes in alcohol use and consequences. Examining the effect of DN-BMI on DN perceptions and the effect of DN-BMI on outcomes leads us to the conclusion that the changes in DN perceptions that resulted from receiving DN-BMI (i.e., the a path in a mediation model) may not have been sufficient to result in changes in outcomes (i.e., the b path in mediation models). Lack of support for the b path with a significant a path is rare, but not unprecedented (see Reid & Carey, 2015 for a review). One potential explanation for the lack of differences between DN-BMI and the control group is that the control group reported decreases in IN and DN in the small effect size range. Though these effects did not reach significance they set a higher threshold for the pairwise comparisons with the active conditions.
When we examined changes in mismatched norms, we found that while the IN group did not report changes in DN perceptions, the DN group did report differences in IN perceptions. Taken together, these findings suggest a correspondence bias (Gilbert & Malone, 1995) in which DN-BMI influenced perceptions of IN – novel information not available in the Prince and Carey (2010) study. Additional evidence of a correspondence bias was seen in our manipulation check, on which substantial numbers of participants in both IN-BMI and DN-BMI conditions reported learning something about mismatched content. Students assumed both that they learned about others’ attitudes when they actually learned about others behaviors and when they learned about others’ behavior they assumed they also learned about others’ attitudes. This implies that the conditions were not subjectively distinct with regard to normative messages. However, on items unrelated to norms (e.g., how to reduce BAC, how to reduce calories, and which organs are affected by alcohol) the vast majority of students responded correctly that they had not discussed those topics regardless of condition.
Despite evidence for the correspondence bias, our fidelity check and manipulation check support strong internal validity. Specifically, our fidelity check showed that interventions were delivered as intended and our manipulation check revealed that nearly 100% of participants correctly endorsed receiving the information they did in fact receive. We can suggest two potential explanations for incorrect endorsement of receiving information that was not presented. First, participants were college students currently enrolled in an introductory psychology course. As such, they were in a learning environment that rewards drawing inferences from newly learned information – particularly when such inferences are related to psychological concepts. Thus, upon learning about their peers’ true attitudes or behavior they may have quickly transferred the information about one to the other. Second, much attention has been paid to the concept of attitude-behavior consistency (cf. Gross & Niman, 1975) - the general tendency for people to assume that attitudes are precursors of behavior (Cohen, 1964). It is reasonable to surmise that students used the attitude-behavior consistency heuristic when inferring attitudinal or behavioral information from the behavioral or attitudinal information they were presented, respectively.
By juxtaposing our current sample with results from Prince and Carey (2010) we can get a broader view of the current evidence for the presence of a correspondence bias that may result from personalized normative BMI. While Prince and Carey (2010) found that IN-BMI changed DN perceptions after written feedback, the current sample more often reported changes in IN perceptions following DN-BMI delivered in person. Further, those who received IN-BMI in the current sample changed DN perceptions on manipulation check items but not in tests conducted as exploratory analyses. Taken together, it appears that context may be important in determining whether personalized normative feedback generalizes. Examining this question further could help to design a parsimonious intervention that contains sufficient feedback to change both norms.
This clinical trial has several notable strengths. First, we used norms theory to expand our knowledge and understanding of how college student drinking is affected by both IN-BMI and DN-BMI alone and in combination. Second, we developed a manualized IN-BMI that can be used as a model for future studies seeking to improve upon the current findings. Third, we demonstrated that IN-BMI alone or in combination with DN-BMI provides an alternative to DNBMI alone that is effective in reducing alcohol use and consequences among college drinkers. Fourth, we provide preliminary data that raises interesting questions about the specificity of effects of DN-BMI and IN-BMI. Results of exploratory analyses suggest that changes in perceived norms may not be specific to matched normative perceptions. Rather, they may change together under some circumstances in response to personalized normative feedback.
This trial's novel findings should be interpreted in the context of its limitations. First, this study would have benefited from analyses of order effects within the Combined-BMI condition. Every participant in the Combined-BMI condition received DN-BMI then IN-BMI, so we cannot determine whether the pattern of findings would be different if IN-BMI were presented first. Second, the current sample consisted of heavier than average drinkers, which potentially limits generalizability to heavy drinkers. For comparison, the current sample reported drinking on average 12.82 drinks per week and the average drinks per week in the DN-BMI referent group sample of over 1800 students collected at the same university was 6.45. Third, in the IN-BMI condition we gave feedback on personally approved/disapproved of consequences and prompted reflection as well as provided personalized information about self/other/attitudes toward consequences. We were unable to disentangle which component of the IN-BMI was the active ingredient with the current study design. Fourth, the Combined-BMI condition, while still brief, was double the length of either of the single component conditions (i.e., Combined-BMI: 30 minutes vs. Single-component: 15 minutes). Although the IN-BMI and Combined-BMI conditions generally did not differ, we acknowledge that length of intervention is a dimension worthy of further study. Finally, we operationalized IN-BMI as the acceptability of consequences, while we recognize that IN-BMI could address other targets such as acceptability of consumption or acceptability of use of protective behavioral strategies.
In summary, this study presents initial promising results on the effectiveness of a brief personalized face-to-face IN-BMI for college drinkers. Specifically, the IN-BMI resulted in the greatest reductions in drinking and consequences and was considered to be the most satisfying and interesting among the intervention conditions. We recommend replication to further enhance our understanding of the unique and combined effects of DN-BMI and IN-BMI on normative perceptions as well as the effect on college student drinking and ARC. Finally, more work needs to be conducted to assess the role of correspondence bias in normative feedback interventions, especially when either type of feedback is presented alone.
Acknowledgments
Drs. Prince and Rice are supported by a training grant (T32-AA007583) from the National Institute on Alcohol Abuse and Alcoholism (NIAAA). This work was performed in partial fulfillment of the requirements for the Ph.D. degree of the first author under the supervision of the second author at Syracuse University. This work was supported in part by Dr. Maisto's 2K05 AA16928 from the NIAAA.
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 5th ed. Author; Washington, DC: 2013. [Google Scholar]
- Agrawal A, Grant JD, Littlefield A, Waldron M, Pergadia ML, Lynskey MT, Madden PAF, Todorov A, Trull T, Bucholz KK, Todd RD, Sher K, Heath AC. Developing a quantitative measure of alcohol consumption for genomic studies on prospective cohorts. Journal of Studies on Alcohol and Drugs. 2009;70:157–168. doi: 10.15288/jsad.2009.70.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baer JS. Effects of college residence on perceived norms for alcohol consumption: An examination of the first year in college. Psychology of Addictive Behaviors. 1994;8:43–50. [Google Scholar]
- Barnett LA, Far JM, Mauss AL, Miller JA. Changing perceptions of peer norms as a drinking reduction program for college students. Journal of Alcohol and Drug Education. 1996;41:39–62. [Google Scholar]
- Borsari B, Carey KB. Effects of a brief motivational intervention with college student drinkers. Journal of Consulting and Clinical Psychology. 2000;68:428–433. [PubMed] [Google Scholar]
- Borsari B, Carey KB. Descriptive and injunctive norms in college drinking: A meta-analytic integration. Journal of Studies on Alcohol. 2003;64:331–341. doi: 10.15288/jsa.2003.64.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Henson JM, Carey MP, Maisto SA. Perceived norms mediate effects of a brief motivational intervention for sanctioned college drinkers. Clinical Psychology: Science and Practice. 2010;17:58–71. doi: 10.1111/j.1468-2850.2009.01194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Carey MP, Maisto SA, Henson JM. Brief motivational interventions for heavy college drinkers: A randomized controlled trial. Journal Of Consulting And Clinical Psychology. 2006;74:943–954. doi: 10.1037/0022-006X.74.5.943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Henson JM, Carey MP, Maisto SA. Computer versus in-person intervention for students violating campus alcohol policy. Journal of Consulting and Clinical Psychology. 2009;77:74–87. doi: 10.1037/a0014281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LAJ, Carey MP, DeMartini KS. Individual-level interventions to reduce college student drinking: A meta-analytic review. Addictive Behaviors. 2007;32:2469–2494. doi: 10.1016/j.addbeh.2007.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LA, Elliott JC, Garey L, Carey MP. Face-to-face versus computer-delivered alcohol interventions for college drinkers: a meta-analytic review, 1998 to 2010. Clinical psychology review. 2012;32:690–703. doi: 10.1016/j.cpr.2012.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cialdini RL, Reno RR, Kallgren CA. A focus theory of normative conduct: Recycling the concept of norms to reduce littering in public places. Journal of Personality and Social Psychology. 1990;58:1015–1026. [Google Scholar]
- Cohen AR. Attitude Change and Social Influence. Basic Books; New York, NY: 1964. [Google Scholar]
- Dimeff LA, Baer JS, Kivlahan DR, Marlatt GA. Brief alcohol screening and intervention for college students: A harm reduction approach. Guilford Press; New York, NY: 1999. [Google Scholar]
- Gilbert DT, Malone JG. The correspondence bias. Psychological Bulletin. 1995;177:21–38. doi: 10.1037/0033-2909.117.1.21. [DOI] [PubMed] [Google Scholar]
- Gross JS, Niman CM. Attitude-Behavior Consistency: A Review. The Public Opinion Quarterly. 1975;39:358–368. [Google Scholar]
- Hingson RW, Zha W, Weitzman ER. Magnitude of and trends in alcohol-related mortality and morbidity among U.S. college students ages 18-24. Journal of Studies on Alcohol and Drugs. 2009;12:12–20. doi: 10.15288/jsads.2009.s16.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huh D, Mun EY, Larimer ME, White HR, Ray AE, Rhew IC, Atkins DC. Brief motivational interventions for college student drinking may not be as powerful as we think: An individual participant-level data meta-analysis. Alcoholism: Clinical and Experimental Research. 2015;39:919–931. doi: 10.1111/acer.12714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahler CW, Strong DR, Read JP. Toward efficient and comprehensive measurement of the alcohol problems continuum in college students: The Brief Young Adult Alcohol Consequences Questionnaire. Alcoholism: Clinical and Experimental Research. 2005;29:1180–1189. doi: 10.1097/01.alc.0000171940.95813.a5. [DOI] [PubMed] [Google Scholar]
- Larimer ME, Turner AP, Mallett KA, Geisner IM. Predicting drinking behavior and alcohol-related problems among fraternity and sorority members: Examining the role of descriptive and injunctive norms. Psychology of Addictive Behaviors. 2004;18:203–212. doi: 10.1037/0893-164X.18.3.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larimer ME, Kaysen DL, Lee CM, Kilmer JR, Lewis MA, Dillworth T, Montoya HD, Neighbors C. Evaluating level of specificity of normative referents in relation to personal drinking behavior. Journal of Studies on Alcohol and Drugs, Supplement Number. 2009;16:115–121. doi: 10.15288/jsads.2009.s16.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee ML, Geisner IM, Lewis MA, Neighbors C, Larimer ME. Social motives and the interaction between descriptive and injunctive norms in college student drinking. Journal of Studies on Alcohol and Drugs. 2007;68:714–721. doi: 10.15288/jsad.2007.68.714. [DOI] [PubMed] [Google Scholar]
- Lewis MA, Neighbors C. Social norms approaches using descriptive drinking norms education: A review of the research and personalized normative feedback. Journal of American College Health. 2006;54:213–218. doi: 10.3200/JACH.54.4.213-218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahler HI, Kulik JA, Butler HA, Gerrard M, Gibbons FX. Social norms information enhances the efficacy of an appearance-based sun protection intervention. Social Science & Medicine. 2008;67:321–329. doi: 10.1016/j.socscimed.2008.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez JA, Sher KJ, Wood PK. Drinking consequences and subsequent drinking in college students over 4 years. Psychology Of Addictive Behaviors. 2014;28(4):1240–1245. doi: 10.1037/a0038352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell SE, Delaney HD. Designing experiments and analyzing data: A model comparison perspective. 2nd ed. Lawrence Erlbaum Associates, Inc; Maywah, NJ: 2004. [Google Scholar]
- McNally AM, Palfai TP, Kahler CW. Motivational interventions for heavy drinking college students: Examining the role of discrepancy-related psychological processes. Psychology of Addictive Behaviors. 2005;19:79–87. doi: 10.1037/0893-164X.19.1.79. [DOI] [PubMed] [Google Scholar]
- Merrill JE, Carey KB, Reid AE, Carey MP. Drinking Reductions Following Alcohol-Related Sanctions Are Associated With Social Norms Among College Students. Psychology of Addictive Behaviors. 2014;28:553–558. doi: 10.1037/a0034743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller MB, Leffingwell T, Claborn K, Meier E, Walters S, Neighbors C. Personalized feedback interventions for college alcohol misuse: An update of Walters & Neighbors (2005). Psychology of addictive behaviors. 2013;27:909. doi: 10.1037/a0031174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller DK, McFarland C. When social comparison goes awry: The case of pluralistic ignorance. In: Suls J, Wills T, editors. Social comparison: Contemporary theory and research. Lawrence Erlbaum; Hillsdale, NJ: 1991. pp. 287–313. [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Helping people change. Guilford press; New York, NY: 2012. [Google Scholar]
- Murphy JG, Dennhardt AA, Skidmore JR, Martens MP, McDevitt-Murphy ME. Computerized versus motivational interviewing alcohol interventions: Impact on discrepancy, motivation, and drinking. Psychology of Addictive Behaviors. 2010;24:628–639. doi: 10.1037/a0021347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy JG, Benson TA, Vuchinich RE, Deskins MM, Eakin D, Flood AM, McDevitt-Murphy M, Torrealday O. A comparison of personalized feedback for college student drinkers delivered with and without motivational interview. Journal of Studies on Alcohol. 2004;65:200–203. doi: 10.15288/jsa.2004.65.200. [DOI] [PubMed] [Google Scholar]
- Neighbors C, Larimer ME, Lewis MA. Targeting misperceptions of descriptive drinking norms: Efficacy of a computer delivered personalized normative feedback intervention. Journal of Consulting and Clinical Psychology. 2004;72:434–447. doi: 10.1037/0022-006X.72.3.434. [DOI] [PubMed] [Google Scholar]
- Neighbors C, Lee CM, Lewis MA, Fossos N, Larimer ME. Are social norms the best predictor of outcomes among heavy-drinking college students?. Journal of Studies on Alcohol and Drugs. 2007;68:556–565. doi: 10.15288/jsad.2007.68.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neighbors C, O'Connor RM, Lewis MA, Chawla N, Lee CM, Fossos N. The relative impact of injunctive norms on college student drinking: The role of reference group. Psychology of Addictive Behaviors. 2008;22:576–581. doi: 10.1037/a0013043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park HS, Smith SW. Distinctiveness and influence of subjective norms, personal descriptive and injunctive norms, and societal descriptive and injunctive norms on behavioral intent: A case of two behaviors critical to organ donation. Human Communication Research. 2007;33:194–218. [Google Scholar]
- Perkins WH, Haines MP, Rice R. Misperceiving the college drinking norm and related problems: A nationwide study of exposure to prevention information, perceived norms and student alcohol misuse. Journal of Studies on Alcohol. 2005;66:470–478. doi: 10.15288/jsa.2005.66.470. [DOI] [PubMed] [Google Scholar]
- Prince MA, Carey KB. The malleability of injunctive norms among college students. Addictive Behaviors. 2010;35:940–947. doi: 10.1016/j.addbeh.2010.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid AE, Aiken LS. Correcting injunctive norm misperceptions motivates behavior change: A randomized controlled sun protection intervention. Health Psychology. 2013;32:551–560. doi: 10.1037/a0028140. [DOI] [PubMed] [Google Scholar]
- Reid AE, Carey KB. Interventions to reduce college student drinking: State of the evidence for mechanisms of behavior change. Clinical Psychology Review. 2015;40:213–224. doi: 10.1016/j.cpr.2015.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid AE, Cialdini RB, Aiken LS. Handbook of Behavioral Medicine. Springer; New York: 2010. Social norms and health behavior. pp. 263–274. [Google Scholar]
- Ruxton GD, Beauchamp G. Time for some a priori thinking about post hoc testing. Behavioral Ecology. 2008;19:690–693. [Google Scholar]
- Schroeder CM, Prentice DA. Exposing pluralistic ignorance to reduce alcohol use among college students. Journal of Applied Social Psychology. 1998;28:2150–2180. [Google Scholar]
- Schultz PW, Nolan JN, Cialdini RB, Goldstein NJ, Griskevicius V. The constructive, destructive, and reconstructive power of social norms. Psychological Science. 2007;18:429–486. doi: 10.1111/j.1467-9280.2007.01917.x. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using Multivariate Statistics. 5th ed. Allyn & Bacon/Pearson Education; Boston, MA: 2007. [Google Scholar]
- Walters ST, Vader AM, Harris TR, Field CA, Jouriles EN. Constructive motivational interviewing and feedback for college drinkers: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 2009;77:64–73. doi: 10.1037/a0014472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler H, Davenport A, Dowdall G, Moeykens B. Health and behavioral consequences of binge drinking in college: A national survey of students at 140 campuses. JAMA: Journal Of The American Medical Association. 1994;272:1672–1677. [PubMed] [Google Scholar]