Abstract
Objective
This study compared use of and associated expenditures for Medicaid-reimbursed school-based and out-of-school services for children with autism spectrum disorder (ASD) and those with other psychiatric disorders.
Methods
Philadelphia County Medicaid claims were used to identify children ages five to 17 who received behavioral health services through Medicaid any time between October 2008 and September 2009 (N=24,271). Children were categorized into four diagnostic groups: autism spectrum disorder (ASD), conduct disorder or oppositional defiant disorder (conduct-ODD), attention-deficit hyperactivity disorder (ADHD), and other psychiatric disorders. Logistic regression analysis compared use of in-school and out-of-school behavioral health services between children with ASD and children with other psychiatric disorders. Generalized linear models with gamma distribution were used to estimate differences in Medicaid expenditures for in-school and out-of-school services and total Medicaid expenditures for both service types by disorder, with adjustments for age, sex, and race-ethnicity.
Results
The most common diagnosis was ADHD (40%); 35% had other psychiatric disorders, 21% had conduct-ODD, and 4% had ASD. A significantly greater proportion of children with ASD (52%) received in-school behavioral health services (conduct-ODD, 5%; ADHD, 8%; and other psychiatric disorders, 1.7%) Per-child expenditures for both school-based and outof-school behavioral health services were significantly higher for children with ASD than for children in the other groups.
Conclusions
Medicaid represents an important source of in-school and out-of-school care for children with ASD and their families. States that expand Medicaid under the Affordable Care Act should give careful consideration to covering school-based mental health services for children with ASD.
Autism spectrum disorder (ASD) is characterized by impairments in social communication and interaction and by the presence of restricted interests and repetitive behaviors (1). The presentation of core and related symptoms, such as intellectual disability (2), aggressive and self-injurious behaviors, and sleep and eating problems, can vary widely among children with ASD and persist across the lifespan (3–7). As a result, children with ASD often receive intensive and costly long-term care, particularly in schools (8). Generally, school-based services address specific behaviors (for example, aggression, self-injury, attention, and impulse control) that significantly interfere with overall adaptation, learning, and functioning. Services may also include instructional and behavioral support from one-on-one aides (9). Given the amount of time that children with ASD spend in schools, access to these services is critically important (10).
The Centers for Disease Control and Prevention has estimated that one in 68 children in the United States has ASD (11). The growing number of children with ASD has raised concerns about the cost of care, which is generally higher than for children with other psychiatric disorders (12). Children with ASD receive educational services through the Individuals with Disabilities Education Act (IDEA), which provides services necessary for children to receive a “free and appropriate education” (8,13). IDEA prohibits use of federal education funds to pay for medical care, even though this care may be related to academic functioning (14). IDEA also is under-funded. The U.S. Department of Education's National Center for Education Statistics reports that in 2014 IDEA funds covered only 16% of the estimated cost of educating children with disabilities (15). Because IDEA does not cover medical services and because it is so underfunded, many states leverage Medicaid to pay for school-based services for children with special needs, including those with ASD (16–18). There is no published estimate, however, of the scale of Medicaid spending on school-based services for children with ASD.
This issue has assumed particular urgency because the number of children receiving Medicaid-reimbursed services is anticipated to increase by millions under the Affordable Care Act (ACA) (19). The ACA contains important provisions that may expand access to services for individuals with ASD. Under the ACA, most health insurance plans are no longer allowed to deny, limit, exclude, or charge more for coverage to anyone on the basis of a preexisting condition, including ASD; most private insurance plans must cover preventive services for children (including screening); individuals with ASD have expanded access to Medicaid and other affordable insurance options; and new health plans must cover “essential health benefits,” including hospitalization, preventive services, and prescription drugs, to help ensure that individuals have the coverage needed to stay healthy (20). With the ACA's implementation, there has been ample discussion about medical homes and community-based services; however, school-based services are not mentioned. Rigorous estimates of the number of children with ASD receiving Medicaid-reimbursed school-based services and the associated expenditures will guide policy makers and behavioral health care professionals as they make decisions about whether Medicaid expansion and the ACA should cover school-based mental health services.
To provide some insight into this issue, we identified use of in-school individual behavioral health services and out-of-school behavioral health services and average annual Medicaid expenditures for service use among children with ASD from 2008 to 2009 in a large, metropolitan county of Pennsylvania. To place these numbers in context, we compared service use and expenditures for children with ASD with those of other Medicaid-enrolled children with psychiatric disorders.
METHODS
Data Source and Study Sample
Philadelphia County Medicaid claims were used to identify a subset of children between the ages of five and 17 who received behavioral health services through Medicaid during October 2008 through September 2009 (N=24,271). The University of Pennsylvania's Institutional Review Board and the Institutional Review Board of the City of Philadelphia Department of Public Health approved the study protocol.
Variables
All variables, including age, sex, race-ethnicity, psychiatric diagnosis, behavioral health service use, and expenditures, were extracted from the Medicaid claims data. Annual mean Medicaid expenditures were calculated by summing the reimbursed dollar amount (2008–2009 dollars) per Medicaid claim by behavioral health service type and dividing the total amount by the number of service users. Children were categorized as having ASD, conduct disorder or oppositional defiant disorder (conduct-ODD), attention-deficit hyperactivity disorder (ADHD), or other psychiatric disorders. Children with two or more Medicaid claims associated with an ICD-9 primary diagnosis of 299.xx were identified as having ASD. Children with two or more Medicaid claims associated with an ICD-9 primary diagnosis of 312 or 313 were identified as having conduct-ODD. Children with two or more ICD-9 primary diagnoses of 314 were identified as having ADHD. Children with other ICD-9 primary diagnoses were categorized as having other psychiatric disorders. Children with comorbid diagnoses were classified according to the hierarchy of ASD, ADHD, conduct-ODD, and other psychiatric disorders. Of the 24,271 children in the sample, 4.4% (N=1,068) had two different psychiatric diagnoses and .02% (N=4) had three different psychiatric diagnoses in the Medicaid claims data.
Behavioral health services were categorized on the basis of the Level of Care codes from Medicaid claims data as in-school individual behavioral health services (one-on-one behavioral support) and out-of-school behavioral health services (outpatient treatment and out-of-school Behavioral Health Rehabilitation Services [BHRS]). In Pennsylvania, BHRS include wraparound services designed to provide therapeutic intervention to children ages three to 21 with serious emotional disturbance or social or behavioral problems (21). Demographic variables included age (recoded as 5–11, 12–14, and 15–17 years), sex (male and female), and race-ethnicity (African American, white, Hispanic, and other race).
Analysis
First, we examined the distribution of demographic characteristics and behavioral health service use by psychiatric disorder. Chi square tests were used to examine differences in distributions. Second, logistic regression analyses were used to model children's in-school and out-of-school behavioral health service use (dependent variable) by psychiatric disorder, adjusting for age, sex, and race-ethnicity. We also calculated annual mean Medicaid expenditures for service users by service type and total mean Medicaid expenditures for in-school and out-of-school service use for each psychiatric disorder. Generalized linear models with a gamma distribution and log link function were used to compare differences in expenditures for in-school and outof-school behavioral health service use and total mean expenditures for in-school and out-of-school service use by psychiatric disorder, adjusting for age, sex, and race-ethnicity.
RESULTS
A total of 170,202 children ages five to 17 were enrolled in Medicaid in Philadelphia during the 2008–2009 school year; 24,271 received Medicaid-reimbursed behavioral health services. Table 1 presents demographic characteristics by psychiatric disorder. The most common psychiatric diagnosis was ADHD (39.8%); 35.2% had other psychiatric disorders, 21.1% had conduct-ODD, and 3.9% had ASD. Most of the children (63.1%) were male, and the average age was 11.3±3.6. Most of the children with ASD (69.7%) and with ADHD (66.6%) were between the ages of five and 11, whereas children with conduct-ODD and children with other psychiatric disorders had more evenly distributed ages. Psychiatric disorder groups differed by sex and race-ethnicity. Whereas only 15.6% of children with ASD were females, 33.4% children with conduct-ODD, 28.0% of children with ADHD, and 51.5% of children with other psychiatric disorders were females. Less than 50% of children with ASD or ADHD were African Americans, whereas 74.8% of children with conduct-ODD and 59.7% of children with other psychiatric disorders were African Americans. The ADHD group had the highest proportion of children of Hispanic origin (38.7%), followed by other psychiatric disorders (24.7%), conduct-ODD (16.2%), and ASD (13.6%).
TABLE 1.
Demographic characteristics of 24,271 children who received Medicaid-reimbursed behavioral health services, by psychiatric disordera
| ASD (N=941) |
Conduct-ODD (N=5,118) |
ADHD (N=9,669) |
Other psychiatric disorders (N=8,543) |
Total (N=24,271) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | N | % | N | % | N | % | N | % | N | % |
| Ageb | ||||||||||
| 5–11 | 656 | 69.7 | 1,920 | 37.5 | 6,439 | 66.6 | 3,046 | 35.7 | 12,061 | 49.7 |
| 12–14 | 166 | 17.6 | 1,745 | 34.1 | 2,181 | 22.6 | 2,339 | 27.4 | 6,431 | 26.5 |
| 15–17 | 119 | 12.7 | 1,453 | 28.4 | 1,049 | 10.9 | 3,158 | 37.0 | 5,779 | 23.8 |
| Race-ethnicityc | ||||||||||
| African American | 434 | 46.1 | 3,826 | 74.8 | 4,748 | 49.1 | 5,100 | 59.7 | 14,108 | 58.1 |
| White | 282 | 30.0 | 371 | 7.3 | 922 | 9.5 | 1,104 | 12.9 | 2,679 | 11.0 |
| Hispanic | 128 | 13.6 | 831 | 16.2 | 3,742 | 38.7 | 2,113 | 24.7 | 6,814 | 28.1 |
| Other | 97 | 10.3 | 90 | 1.8 | 257 | 2.7 | 226 | 2.7 | 670 | 2.8 |
| Sexc | ||||||||||
| Male | 794 | 84.4 | 3,409 | 66.6 | 6,961 | 72.0 | 4,144 | 48.5 | 15,308 | 63.1 |
| Female | 147 | 15.6 | 1,709 | 33.4 | 2,708 | 28.0 | 4,399 | 51.5 | 8,963 | 36.9 |
ASD, autism spectrum disorder;conduct-ODD, conduct disorder or oppositional defiant disorder;ADHD, attention-deficit hyperactivity disorder
Significant difference by psychiatric disorder category (p<.01)
Significant difference by psychiatric disorder category (p<.001)
Table 2 presents data for in-school and out-of-school behavioral health service use and annual mean Medicaid expenditures by psychiatric disorder. Behavioral health service use differed by psychiatric disorder in the unadjusted models. Among children with ASD, 51.9% used in-school individual behavioral health services, compared with 5.1% of children with conduct-ODD, 8.2% of children with ADHD, and 1.7% of children with other psychiatric disorders (p<.001). Although most children used out-of-school behavioral health services, the percentages of users ranged from 89.7% for children with conduct-ODD to 97.7% of children with ADHD (p<.001).
TABLE 2.
Use of Medicaid-reimbursed behavioral health services by 24,271 children, by type of service and psychiatric disordera
| ASD |
Conduct-ODD |
ADHD |
Other psychiatric disorders |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Service | N | % | OR | N | % | OR | 95% CI | p | N | % | OR | 95% CI | p | N | % | OR | 95% CI | p |
| In-school individual servicesb | 488 | 51.9 | 1.00 | 259 | 5.1 | .06 | .05-.07 | <.001 | 794 | 8.2 | .09 | .07-10 | <.001 | 142 | 1.7 | .02 | .02-.03 | <.001 |
| Out-of-school servicesc | 913 | 97.0 | 1.00 | 4,590 | 89.7 | .29 | .70-10 | <.001 | 9,444 | 97.7 | 1.13 | .75-1.69 | <.001 | 8,304 | 97.2 | .96 | .64-1.45 | <.001 |
ASD, autism spectrum disorder; conduct-ODD, conduct disorder or oppositional defiant disorder; ADHD, attention-deficit hyperactivity disorder. Each row presents a separate model (yes, 1; no, 0) comparing children with all other psychiatric disorders with children with ASD.
Model statistics: χ2=2,026.00, df=9, p<.001
Model statistics: χ2=680.44, df=9, p<.001
Table 2 presents adjusted ORs and 95% confidence intervals for behavioral health service use by psychiatric disorder. Compared with children with ASD, children with conduct-ODD were less likely to use in-school services (OR=.06) and also less likely to use out-of-school services (OR=.29) (p<.001 for both). Compared with children with ASD, those with ADHD were less likely to use in-school services (OR=.09) and more likely to use out-of-school services (OR=1.13) (p<.001 for both). Compared with children with ASD, those with other psychiatric disorders were less likely to use in-school services (OR=.02) and to use out-of-school services (OR=.96) (p<.001 for both).
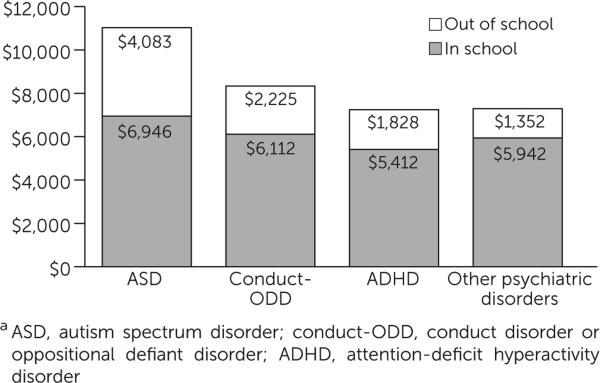
Figure 1 shows annual unadjusted mean Medicaid expenditures for in-school individual behavioral health services and out-of-school behavioral health services, by disorder. Mean±SD expenditures for both in-school and out-of-school services were highest for children with ASD ($6,946±$3,609 and $4,083±$5,375, respectively). Children with ASD had higher mean expenditures for in-school services than did children with conduct-ODD ($6,112±$3,560), ADHD ($5,412±$3,589), and other psychiatric disorders ($5,942±3,949). Children with ASD also had higher mean expenditures for outof-school services than children with conduct-ODD ($2,225±$4,027), ADHD ($1,828±$3,368), and other psychiatric disorders ($1,352±$2,946).
FIGURE 1.
Annual mean Medicaid expenditures for in-school and out-of-school behavioral health service use by 24,271 childrena
The generalized linear model analysis with gamma distribution indicated significant differences in adjusted Medicaid expenditures for both types of behavioral health service use by psychiatric disorder (Table 3). Compared with expenditures for in-school individual behavioral health services for children with ASD, expenditures were lower for children with conduct-ODD (OR=.89, p<.05)) and children with ADHD (OR=.80, p<.001). Compared with expenditures for out-of-school services for children with ASD, expenditures for children with conduct-ODD, children with ADHD, and children with other psychiatric disorders were lower (OR=.50, OR=.47, and OR=.32, respectively, p<.001 for all). Adjusted and unadjusted total expenditures for in-school and out-of-school services also differed significantly by psychiatric disorder (p<.001 for all). Compared with the total mean expenditures for children with ASD, expenditures for children with conduct-ODD, children with ADHD, and children with other psychiatric disorders were lower in the adjusted model (OR=.33, OR=.31, and OR=.20, respectively, p<.001 for all).
TABLE 3.
Mean annual Medicaid expenditures (2008-2009 dollars) for behavioral health services used by 24,271 children, by type of service and psychiatric disordera
| Conduct-ODD |
ADHD |
Other psychiatric disorders |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ASD |
Mean estimateb |
Mean estimateb |
Mean estimateb |
|||||||||||
| Service | Median | Mean estimateb | Median | Exp (b) | 95% CI | p | Median | Exp (b) | 95% CI | p | Median | Exp (b) | 95% CI | p |
| In-school individual services | $6,663 | 1.00 | $5,860 | .89 | .79-1.00 | .041 | $5,000 | .80 | .73-.87 | <.001 | $5,634 | .88 | .76-1.00 | .059 |
| Out-of-school services | $2,637 | 1.00 | $973 | .50 | .46-55 | <.001 | $637 | .47 | .43-51 | <.001 | $564 | .32 | 30-.35 | <.001 |
| Total services | $6,182 | 1.00 | $842 | .33 | 30-.36 | <.001 | $625 | .31 | 29-.34 | <.001 | $550 | .20 | .18-.22 | <.001 |
ASD, autism spectrum disorder; conduct-ODD, conduct disorder or oppositional defiant disorder; ADHD, attention-deficit hyperactivity disorder
Mean estimates (exponentiated beta coefficients) compare expenditures for each group with the reference group (ASD).
DISCUSSION AND CONCLUSIONS
Our findings suggest the importance of Medicaid-funded behavioral health services for children with ASD. Children with ASD were significantly more likely than children with all other psychiatric disorders to use in-school behavioral health services. Children with ASD were also significantly more likely than children with conduct-ODD and with other psychiatric disorders (except those with ADHD) to use outof-school behavioral health services. Medicaid-reimbursed expenditures for in-school services for children with ASD were significantly higher than for children with conduct-ODD or ADHD. Medicaid expenditures for out-of-school services for children with ASD were significantly higher than for children with any other psychiatric disorder. Although children with ASD constituted the smallest group of those receiving Medicaid-funded behavioral health services, total expenditures for in-school and out-of school service use were significantly higher than for children with all other psychiatric disorders. The behavioral health system spends more on services for children with ASD than for children with any other disorder, despite the relatively small number of children with ASD.
Some study limitations should be mentioned. First, the analysis was limited to Philadelphia Medicaid claims, which limits the geographic generalizability of the findings and does not take into account the potential role of spending through the education system, through private insurance, or out-of-pocket costs. Philadelphia is an important study site in its own right, in that it serves one-third of Pennsylvania's Medicaid population, is more urban, and has a higher number of children from racial-ethnic minority groups than other counties. Large, urban school districts, such as Philadelphia, serve a disproportionately large number of children in the United States (22) and therefore represent important areas for study.
A second limitation is that our analysis was based on one year of cross-sectional data. The results should be interpreted with caution because the content of services and the reimbursement structure may change over time and service use and expenditures change accordingly. Finally, diagnoses were not validated, although recent studies suggest the accuracy of the autism diagnosis in Medicaid claims (23).
Despite these limitations, the findings have important implications. Medicaid is a particularly important resource for children with ASD in providing school-based behavioral health services. However, it is unclear how behavioral health services will be financed and delivered in schools under the ACA. States that participate in the Medicaid expansion must offer benefits similar to those provided by private insurance companies in that state (24). These services generally include inpatient and outpatient hospital services, X-ray and lab services, physician services, mental health services, well-child care, and prescription drugs (24). School-based services are notably absent from this list.
The number of families seeking Medicaid-funded ASD services may decrease as more states enact mandates that require private insurance companies to cover autism services (23). However, autism insurance mandates notably do not cover ASD-related services in schools (12). It is imperative that as the number of mandates increases, coverage of school-based services is not lost. Although a large amount of money is spent on in-school individual behavioral health services, a growing body of research suggests that the quality and outcomes of these services are relatively poor. Thus further investigation to identify high-quality, evidence-based interventions for effective and efficient school-based care in the real-world setting is important. The ACA explicitly emphasizes the importance of using evidence-based practices, but there is no discussion in the legislation of how these practices should be chosen, implemented, or measured. On the basis of our findings, protecting Medicaid-reimbursed school-based care for children with ASD is of the utmost importance. Schools should be considered an important site for service delivery for children with ASD and other psychiatric disorders, regardless of the funding mechanism.
Acknowledgments
This study was partially funded by the Department of Behavioral Health and Intellectual Disability Services, City of Philadelphia. Preparation of this article was supported in part by grant K01MH100199 from the National Institute of Mental Health, grant 13-ECA-01L from the Autism Science Foundation, and a FARFund Early Career Award to Dr. Locke. The Medicaid claims data were shared through a memorandum of understanding between the City of Philadelphia Department of Behavioral Health and Intellectual Disability Services and the University of Pennsylvania. The authors thank the City of Philadelphia Department of Behavioral Health and Intellectual Disability Services for sharing data and providing feedback on the study findings.
Footnotes
Dr. Marcus reports receiving consulting fees from Alkermes, Forest, Johnson & Johnson, Shire, and Sunovion. The other authors report no financial relationships with commercial interests.
Contributor Information
Dr. Christina D. Kang-Yi, Department of Psychiatry, Perleman School of Medicine, University of Pennsylvania, Philadelphia
Dr. Jill Locke, Department of Psychiatry, Perleman School of Medicine, University of Pennsylvania, Philadelphia
Dr. Steven C. Marcus, School of Social Policy and Practice, University of Pennsylvania, Philadelphia
Dr. Trevor R. Hadley, Department of Psychiatry, Perleman School of Medicine, University of Pennsylvania, Philadelphia
Dr. David S. Mandell, Department of Psychiatry, Perleman School of Medicine, University of Pennsylvania, Philadelphia
REFERENCES
- 1.Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; Arlington, Va: 2013. [Google Scholar]
- 2.Gillberg C, Billstedt E. Autism and Asperger syndrome: co-existence with other clinical disorders. Acta Psychiatrica Scandinavica. 2000;102:321–330. doi: 10.1034/j.1600-0447.2000.102005321.x. [DOI] [PubMed] [Google Scholar]
- 3.Hoffman C, Sweeney D, Gilliam J, et al. Sleep problems and symptomology in children with autism. Focus on Autism and Other Developmental Disabilities. 2005;20:194–200. [Google Scholar]
- 4.Horvath K, Perman JA. Autistic disorder and gastrointestinal disease. Current Opinion in Pediatrics. 2002;14:583–587. doi: 10.1097/00008480-200210000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Richdale AL. Sleep problems in autism: prevalence, cause, and intervention. Developmental Medicine and Child Neurology. 1999;41:60–66. doi: 10.1017/s0012162299000122. [DOI] [PubMed] [Google Scholar]
- 6.Wing L. The autistic spectrum. Lancet. 1997;350:1761–1766. doi: 10.1016/S0140-6736(97)09218-0. [DOI] [PubMed] [Google Scholar]
- 7.Volkmar FR, Pauls D. Autism. Lancet. 2003;362:1133–1141. doi: 10.1016/S0140-6736(03)14471-6. [DOI] [PubMed] [Google Scholar]
- 8.Mandell DS, Cao J, Ittenbach R, et al. Medicaid expenditures for children with autistic spectrum disorders: 1994 to 1999. Journal of Autism and Developmental Disorders. 2006;36:475–485. doi: 10.1007/s10803-006-0088-z. [DOI] [PubMed] [Google Scholar]
- 9.Kang-Yi CD, Mandell DS, Hadley T. School-based mental health program evaluation: children's school outcomes and acute mental health service use. Journal of School Health. 2013;83:463–472. doi: 10.1111/josh.12053. [DOI] [PubMed] [Google Scholar]
- 10.Locke J, Kratz H, Reisinger E, et al. Implementation of evidence-based practices for children with autism spectrum disorders in public schools. In: Beidas R, Kendall P, editors. Child and Adolescent Therapy: Dissemination and Implementation of Empirically Supported Treatments. Oxford University Press; New York: 2014. [Google Scholar]
- 11.CDC Estimates 1 in 68 Children Has Been Identified With Autism Spectrum Disorder. Centers for Disease Control and Prevention; Atlanta, Ga: Mar 27, 2014. [Oct 1, 2014]. Available at www.cdc.gov/media/releases/2014/p0327-autism-spectrum-disorder.html. [Google Scholar]
- 12.Wang L, Leslie DL. Health care expenditures for children with autism spectrum disorders in Medicaid. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:1165–1171. doi: 10.1016/j.jaac.2010.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.US Department of Education Assistance to states for the education of children with disabilities. Federal Register. 2013;78:10525–10538. [Google Scholar]
- 14.Mandell DS, Machefsky A, Rubin D, et al. Medicaid's role in financing health care for children with behavioral health care needs in the special education system: implications of the Deficit Reduction Act. Journal of School Health. 2008;78:532–538. doi: 10.1111/j.1746-1561.2008.00340.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Individuals With Disabilities Education Act . Funding Distribution 2014. US Department of Education National Center for Education Statistics; Washington, DC: Apr 25, 2014. [Oct 1, 2014]. Available at febp.newamerica.net/background-analysis/individuals-disabilities-education-act-funding-distribution. [Google Scholar]
- 16.Cidav Z, Lawer L, Marcus SC, et al. Age-related variation in health service use and associated expenditures among children with autism. Journal of Autism and Developmental Disorders. 2013;43:924–931. doi: 10.1007/s10803-012-1637-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Semansky RM, Xie M, Mandell DS. Medicaid's increasing role in treating youths with autism spectrum disorders. Psychiatric Services. 2011;62:588. doi: 10.1176/ps.62.6.pss6206_0588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang L, Mandell DS, Lawer L, et al. Healthcare service use and costs for autism spectrum disorder: a comparison between Medicaid and private insurance. Journal of Autism and Developmental Disorders. 2013;43:1057–1064. doi: 10.1007/s10803-012-1649-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.The Affordable Care Act and Adolescents. US Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation; Washington, DC: Aug, 2013. [Jan 19, 2014]. Available at www.aspe.hhs.gov/health/reports/2013/Adolescents/rb_adolescent.cfm. [Google Scholar]
- 20.The Affordable Care Act and Autism. Autism Speaks; Washington, DC: Jun, 2014. [Oct 1, 2014]. Available at www.autismspeaks.org/advocacy/insurance/affordable-care-act. [Google Scholar]
- 21.Utilizing Management Guide . Community Behavioral Health. City of Philadelphia Department of Behavioral Health and Intellectual Disability Services; Philadelphia: 2006. [Jan 2015]. Available at dbhids.us/assets/Forms-Documents/CBH/UMFULLrev0110.pdf. [Google Scholar]
- 22.Enrollment, Poverty, and Federal Funds for the 100 Largest School Districts, by Enrollment Size in 2010. National Center for Educational Statistics; Washington, DC: 2011. [March 2015]. Available at nces.ed.gov/programs/digest/d12/tables/dt12_104.asp. [Google Scholar]
- 23.Burke JP, Jain A, Yang W, et al. Does a claims diagnosis of autism mean a true case? Autism. 2014;18:321–330. doi: 10.1177/1362361312467709. [DOI] [PubMed] [Google Scholar]
- 24.Stein BD, Sorbero MJ, Goswami U, et al. Impact of a private health insurance mandate on public sector autism service use in Pennsylvania. Journal of the American Academy of Child and Adolescent Psychiatry. 2012;51:771–779. doi: 10.1016/j.jaac.2012.06.006. [DOI] [PubMed] [Google Scholar]