Abstract
Background
A diagnosis of personality disorder (PD) signals a negative prognosis for depressive and anxiety disorders, but the precise abnormal personality traits that regulate the temporal course of internalizing psychopathology are unknown. In the present study, we examined prospective associations between abnormal personality traits and the onset and recurrence of internalizing disorders.
Methods
A sample of 371 young adults at high risk for internalizing problems completed the Schedule for Nonadaptive and Adaptive Personality-Second Edition—a measure of 12 abnormal personality traits and three temperament dimensions (i.e., Negative Temperament, Positive Temperament, Disinhibition versus Control)—and underwent annual diagnostic interviews over four years of follow-up.
Results
In multivariate survival analyses, Negative Temperament was a robust predictor of both new onsets and recurrences of internalizing disorder. Further, the Dependency and Self-Harm abnormal personality dimensions emerged as independent predictors of new onsets and recurrences, respectively, of internalizing disorders after statistically adjusting for variation in temperament.
Conclusions
Our findings suggest that abnormal personality traits and temperament dimensions have complementary effects on the trajectory of internalizing pathology during young adulthood. In assessment and treatment settings, targeting the abnormal personality and temperament dimensions with the greatest prognostic value stands to improve the early detection of enduring internalizing psychopathology.
Keywords: anxiety, depression, internalizing disorders, naturalistic course, personality pathology, prognosis, temperament
Over the past few decades, researchers have made significant progress in delineating the characteristics of individuals and their environments that influence the temporal course of internalizing disorders. Female gender, family history of disorder, early age of onset, comorbidity, and chronicity of prior disorder episodes all have been implicated in risk for emergence or maintenance of these disorders.[1,2] In the present study, we examined the prognostic status of another factor thought to trigger and exacerbate internalizing problems: personality pathology.
Personality Pathology and Internalizing Disorder Prognosis
Since the release of the Third Edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III),[3] a sizable body of research has compared the clinical outcomes and naturalistic course of internalizing disorders in people with versus without PD.[4,5] Regarding clinical outcomes, the consensus in the literature is that coexisting PD interferes with pharmacological and psychological treatment. For instance, a meta-analytic review of the most recent data concluded that MDD with comorbid PD doubles the odds of poor outcome in depression treatment trials.[6]
PD also can change the naturalistic course (i.e., progression independent of treatment) of depressive and anxiety disorders. Epidemiological data indicate that avoidant, borderline, histrionic, paranoid, schizoid, and schizotypal PDs are related to more persistent MDD over three years of follow-up.[5] Similarly, investigations in large-scale clinical samples have found PD to predict longer time to remission, and quicker relapse after remission, from MDD over six years.[7,8] Additionally, a naturalistic study of 514 anxiety disorder patients reported that PD reduced the likelihood of remission from generalized anxiety disorder (GAD) and specific phobia over a five-year follow-up by 30% and 39%, respectively, although PD did not predict time to remission from panic disorder.[4] Other studies in anxiety disorder samples have corroborated these results for GAD and specific phobia,[9,10] albeit with some inconsistencies.[see 11]
Beyond the Categorical Personality Disorder Diagnoses
Two conceptual problems inherent to all PD research are diagnostic heterogeneity and comorbidity.[12,13] Heterogeneity within PD categories is a byproduct of a polythetic diagnostic algorithm, which allows two people in a given diagnostic category to exhibit very limited overlap in terms of etiology, phenomenology, and psychopathology of that disorder.[14] Comorbidity presents a challenge to researchers attempting to link clinical outcomes to one and only one PD. Due to extensive overlap among the PDs,[e.g., 15] researchers must be cautious in ascribing a causal role to any single PD in empirical studies, because a co-occurring PD may be responsible, to some degree, for the observed association. Together, the issues of heterogeneity and comorbidity complicate the interpretation of the research literature on PD and the naturalistic course of internalizing disorders. Specifically, they obscure the exact psychopathological elements, or core abnormal personality dimensions, of PD that mediate the relations between PD categories and a generally poorer prognosis for depressive and anxiety disorders.[16]
One approach to resolving this dilemma is to focus on the abnormal, or pathological, personality dimensions that serve as the scaffolding for the PD domain. Pathological traits, such as Dependency, Exhibitionism, and Impulsivity, are common to multiple DSM-defined PDs (i.e., problem of comorbidity); yet, two people diagnosed with the same PD do not necessarily exhibit similar levels of the trait (i.e., problem of heterogeneity). Research on more homogeneous trait dimensions can uncover the exact personality traits responsible for worse internalizing disorder prognosis in PD populations.[17]
Pathological traits, such as those measured by the Dimensional Assessment of Personality Pathology—Basic Questionnaire[18] or the Schedule for Nonadaptive and Adaptive Personality (SNAP),[19] reflect maladaptive personality processes that increase vulnerability to PD.[20] Emerging evidence suggests that, while pathological traits are conceptually separate from adaptive or normal-range personality constructs, these two sets of personality dimensions can be readily integrated into hierarchical models of personality anchored at the superordinate level by “big” traits such as neuroticism, conscientiousness, and agreeableness.[21,22] At the same time, recent research has demonstrated that abnormal personality traits show incremental validity relative to normal personality traits in predicting psychopathology and psychosocial dysfunction.[23–25]
Present Study
Our main objective was to investigate the prospective influence of abnormal personality constructs on the onset and recurrence of depressive and anxiety disorders over four years in a young adult sample enriched for elevated neuroticism/negative temperament. Participants completed the SNAP, which assessed variation on three temperament dimensions—Negative Temperament, Positive Temperament, and Disinhibition versus Constraint—and 12 abnormal personality traits within those temperament domains. As a result, we were able to statistically adjust for temperament dimensions while estimating the effects of more narrow bandwidth abnormal personality traits. Further, we simultaneously examined clinical features of prior internalizing psychopathology (i.e., severity, comorbidity, recurrence, and early onset) to distinguish the effects of personality versus existing internalizing vulnerabilities.
Based on prior community and clinical research,[20,24,26,27] we hypothesized that abnormal traits in the Negative Temperament and Positive Temperament domains—with stronger effect sizes for Negative Temperament traits—would predict new onset and recurrence rates. Following prior correlational research,[21,23] Disinhibition versus Control traits were not hypothesized to be related to internalizing risk. We expected that abnormal personality traits would continue to confer risk for disorder even after adjusting for temperament dimensions—all of which have been linked to internalizing disorder prognosis[28–31]—and clinical covariates (e.g., prior comorbidity, early onset).
Materials and Methods
Participants
Participants were recruited as part of the Youth Emotion Project (YEP), a longitudinal study of the antecedents, course, and consequences of depressive and anxiety disorders among young people. Three successive groups of high school juniors at a school in suburban Los Angeles and another in suburban Chicago were given written invitations to participate in a screening stage for YEP. Students who provided assent and had parental consent (n = 1,976) were screened with the Neuroticism scale of revised Eysenck Personality Questionnaire (EPQ-R-N)[32] and were classified into low (n = 634), medium (n = 666), and high (n = 676) Neuroticism tertiles based on their responses. A subsample of 1,269 students overselected for high EPQ-R-N scores was invited to participate, and the percentages of participants in the low, medium, and high tertiles agreeing to participate in baseline assessments (n = 627) were 18.4%, 23.0%, and 58.6%, respectively. There were 283 (44.6%), 321 (48.3%), and 654 (96.5%) students invited to participate in the low-, medium-, and high-risk groups, respectively. Of the 283 low-risk students invited, 122 (43.1%) consented to participate; the corresponding frequencies for medium- and high-risk groups were 150/321 (46.7%) and 382/654 (58.4%), respectively. Independent samples t-tests indicated that providing consent was not statistically significantly associated with EPQ-R-N variation in low- (t[281] = 0.01, p = .99), medium- (t[319] = 1.96, p = .05), or high-risk (t[651] = 0.65, p = .51) tertiles. However, in the full sample, those who provided consent reported more Neuroticism than those who declined to participate in the baseline assessment (t[1,267] = 4.64, p < .001). The baseline sample was 68.7% female, owing to higher rates of female participation in EPQ-R screening, higher female EPQ-R-N scores, and females being more likely to participate in YEP baseline assessments if invited. Additional details regarding the study’s screening and selection procedures are available elsewhere.[33]
Of the 627 original YEP participants, 411 completed the SNAP. Attrition analyses showed that, of the 627 baseline participants, those who did versus did not complete the SNAP did not differ significantly on gender (χ2(1, 627) = 0.26, p = .61), ethnicity (χ2(1, 627) = 2.26, p = .13), or lifetime history of psychopathology (χ2(1, 627) = 3.65, p = .06) prior to SNAP administration. The mean length of time between study entry and SNAP administration was 5.62 years (SD = 0.92; range = 3.24 to 8.91 years). All participants contacted at Time 6 were invited to complete the SNAP. Ten participants were removed from analyses due to extensive missing SNAP data (missing responses to 20 or more SNAP items), 12 were dropped due to extreme scores on the SNAP Invalidity Index (described below), and an additional 18 did not participate in any follow-up diagnostic interviews after SNAP administration. After removing those cases, the final sample of 371 included 253 females (68.19%), and participants self-identified as Caucasian (51.75%), Hispanic/Latino (12.67%), African American (12.13%), Asian/Pacific Islander (4.85%), other race/ethnicity (5.66%), and multiracial (12.94%). Participants had a mean age of 16.9 (SD = 0.37) at the baseline interview and 22.4 (SD = 1.85) at the time of the SNAP personality assessment. Participants who completed SNAP and at least one follow-up wave did not differ from those who completed SNAP but not any follow-up on gender, ethnicity, or lifetime psychopathology rates (χ2s(1, 411) < 1.00, ps > .50).
Measures
SNAP[19]
The SNAP is a self-report personality inventory comprising 390 true-false items that assess three temperament dimensions (Negative Temperament, Positive Temperament, Disinhibition versus Control) and a number of abnormal trait dimensions within those temperament domains. The abnormal Negative Temperament traits are Mistrust, Manipulativeness, Aggression, Self-Harm, Eccentric Perceptions, and Dependency; abnormal Positive Temperament traits are Exhibitionism, Entitlement, and Detachment; and abnormal Disinhibition versus Control traits are Impulsivity, Propriety, and Workaholism. Independent item sets are used to define each scale; there is no item overlap across abnormal scales or between abnormal and temperament scales. The SNAP was constructed by dismantling DSM PD syndromes into their constituent traits and symptomatic behaviors, which, in combination with a factor analytic approach, resulted in more homogeneous and narrow constructs.[19,22] Prior studies have reported good internal consistency and test-retest reliabilities of the SNAP scales, and both the temperament and abnormal personality dimensions show appropriate convergent correlations with other personality inventories.[34,35] Additionally, cross-sectional research has shown the SNAP dimensions to be concurrently associated with internalizing diagnoses in patient populations.[24] In the present study, internal consistency estimates were adequate for all SNAP scales (median Cronbach’s alpha: .80; range: .75–.86). As noted above, the SNAP Invalidity Index was used to detect invalid scores due to random, inconsistent, or socially desirable response patterns.[19] This strategy eliminated 12 participants who scored greater than 2.5 standard deviations away from the mean of the Invalidity Index.
Structured Clinical Interview for DSM-IV, non-patient edition[36]
The Structured Clinical Interview for DSM-IV, non-patient edition (SCID) assesses DSM-IV diagnoses. The SCID was administered at YEP baseline (i.e., Time 1) to assess current and lifetime diagnoses and each subsequent year for nine years (i.e., Time 2-Time 10) to assess changes in diagnostic status since the prior assessment point. Thus, the SCID was modified to assess past diagnoses in each disorder category to identify disorder episodes that may have onset and remitted between study waves. This study focused on the diagnoses at years six through ten (i.e., Time 6-Time 10; see below), representing the period following SNAP administration, to establish the prospective effects of personality on the trajectory of internalizing disorders. SCID interviews were conducted by bachelor-level and above interviewers who had undergone extensive training, including didactics, tests, and live observation.[see 33 for more details] Each completed SCID was presented to a doctoral-level rating team that assigned diagnoses. To qualify for a diagnosis, respondents needed to satisfy DSM criteria for a particular disorder and also be assigned a clinical severity rating (CSR)[37] of four or higher. The CSR reflects the degree of symptomatology, distress, and impairment caused by a disorder, and ranges from zero (no notable symptoms, distress, or interference) to eight (extreme distress or interference). Ratings from one to three indicate subclinical severity, and ratings of four and higher indicate clinical significance. The CSR was substituted for the traditional yes/no judgment of clinically significant distress/impairment so that a dimensional, as opposed to binary, index of disorder severity could be used for research purposes. Inter-rater reliability for both CSRs (Pearson rs > .70) and DSM-IV diagnoses (kappas > .65) were in the acceptable to good range.
Procedures
Participants were recontacted 10 months after each assessment point to schedule the subsequent SCID interview, which took place 10 to 18 months after the prior assessment. The mean interval between follow-up waves was 0.94 year (SD = 0.12; range = 0.76 to 1.96). If a participant was not reachable or available to complete a given time point, he or she was later contacted to schedule the following interview, which queried new onsets and recurrences experienced since the last completed interview. The SNAP was administered through a secure website approximately two months following the sixth SCID assessment (i.e., Time 6). Our primary analyses examined the prospective effects of SNAP traits on incidence of disorder after Time 6, and hereafter we use the term “follow-up” to denote the interval from Time 6 (not inclusive) to Time 10. Of the 371 participants completing at least one follow-up assessment, 46 (12.4%) completed only one, 88 (23.7%) completed two, 132 (35.6%) completed three, and 105 (28.3%) completed all four. Participants were mailed a check after completion of each assessment. All study procedures were approved by Institutional Review Boards at Northwestern University and UCLA.
Data Analytic Plan
Discrete-time survival analyses were used to examine the prospective effect of personality variation on risk for disorder over the follow-up period. Separate analyses were performed for new onsets and recurrences. New onsets were defined as the occurrence of any disorder during follow-up that had not been diagnosed at, or prior to, Time 6. Thus, for a participant who had been diagnosed with only panic disorder up to Time 6, a diagnosis of MDD during follow-up qualified as a new onset. All participants were included in new onset analyses given that no student was diagnosed with every internalizing disorder at baseline. Recurrence was defined as the presence of a given disorder during the follow-up period for any participant who had experienced that disorder prior to Time 6 but did not have a current diagnosis of the disorder at Time 6. Stated differently, participants were included in recurrence analyses (N = 163) if (a) they participated in follow-up waves and (b) there was at least one disorder for which they had a past, but not current, diagnosis at baseline (i.e., Time 6). Participants who experienced a new onset or recurrence at any point between Time 7-Time 9 were censored from analyses at subsequent time points.[38] We decided to collapse across internalizing disorders—as opposed to examining the personological predictors of each disorder category (e.g., MDD, GAD) separately—for survival analyses for conceptual and practical reasons. On a conceptual level, research has established that the general (i.e., nonspecific) personality risk markers for internalizing disorders outnumber the distinctive (i.e., specific) ones,[29] although there are some notable specific relations (e.g., extraversion/positive temperament with social phobia and depressive disorders).[26,39] On a practical level, the modest number of new onsets and recurrences, relative to what would be expected in a clinical sample, led to relatively few cases in any given diagnostic category (e.g., 12 new onsets of social phobia over follow-up). Both the new onset and recurrence analyses proceeded in two stages. First, the bivariate associations between all 20 (three temperament scales, 12 abnormal personality traits, four clinical features, and gender) of the predictors and survival outcome were estimated to determine the effect size of each predictor in isolation. Second, all statistically significant—meeting a liberal alpha threshold of .10—predictors (including temperaments, abnormal traits, and covariates) were submitted to a multivariate survival analysis (alpha = .05) to evaluate the effect of each predictor while adjusting for the presence of the others. The liberal alpha value for the first stage of analyses was selected to minimize Type II error; supplementary analyses indicated that the pattern of personality trait effects in multivariate analyses did not differ if the conventional .05 alpha value was used to select predictors for the multivariate analysis. Power analyses were performed in G*Power using a logistic regression model due to its compatibility with the discrete-time survival analysis framework. Analyses based on effect sizes reported in previous studies of normal-range neuroticism predicting new onset or relapse of anxiety or depression over time in large community samples (average odds ratio = 2.10),[40,41] along with one previous study examining cross-sectional associations between SNAP traits and internalizing disorders,[24] indicated that sample sizes of 102 and 67 were required to achieve .80 power in new onset and recurrence analyses (in which “event” rates were approximately 13% and 28%; see below), respectively, involving the broad Negative Temperament trait. The corresponding sample sizes needed for new onset and recurrence analyses involving abnormal Negative Temperament traits were 195 and 121. There are comparably little prior data on the longitudinal effects of normal- or abnormal-range Positive Temperament traits, although generally their relations with internalizing disorders are smaller,[29] so larger samples would be needed to achieve equivalent power.
The clinical features analyzed here were selected on the basis of previous evidence of association with the longitudinal course of internalizing problems. They included (a) the highest CSR rating assigned to an internalizing diagnosis at any SCID interview from baseline (i.e., Time 1) to Time 6, representing the severity of internalizing psychopathology prior to SNAP administration;[39] (b) recurrence of any internalizing disorder prior to Time 6;[42] (c) lifetime comorbidity of any two (or more) internalizing disorders prior to Time 6;[43] and (d) early onset (occurring prior to Time 1) of any internalizing disorder.[44] Female gender, which is a major risk factor for depression and anxiety,[45,46] and has been linked in some studies with a more refractory course of internalizing psychopathology,[47] was also covaried. The pattern of personality trait results was unaltered if covariates were excluded from the model (i.e., no odds ratio changed by more than 0.10). These results are available upon request. All analyses were performed in Stata 13.[48]
Results
Table 1 shows the Pearson correlations among the SNAP dimensions and clinical features. The temperament scales showed moderate to strong correlations with abnormal personality traits within the same temperament domain (e.g., Positive Temperament with Entitlement, Exhibitionism, and Detachment). Additionally, temperament scales and abnormal personality dimensions within the Negative Temperament and Positive Temperament domains—and especially Negative Temperament, Mistrust, Self-Harm, and Dependency—were moderately correlated with the clinical characteristics of prior internalizing disorders.
Table 1.
Descriptive Statistics for Predictor Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Mean (SD)/N (%) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Negative Temperament | — | 11.07 (7.31) | ||||||||||
| 2. Positive Temperament | −.08 | — | 17.61 (6.10) | |||||||||
| 3. Disinhibition | .13 | .08 | — | 4.40 (2.79) | ||||||||
| 4. Mistrust | .52 | −.01 | .20 | — | 5.65 (4.51) | |||||||
| 5. Manipulativeness | .30 | −.07 | .55 | .35 | — | 5.20 (3.57) | ||||||
| 6. Aggression | .41 | −.10 | .30 | .43 | .41 | — | 4.11 (3.44) | |||||
| 7. Self-Harm | .49 | −.41 | .24 | .38 | .30 | .30 | — | 1.41 (2.07) | ||||
| 8. Eccentric Perceptions | .35 | .11 | .33 | .49 | .44 | .32 | .33 | — | 3.12 (3.09) | |||
| 9. Dependency | .42 | −.11 | .08 | .16 | .19 | −.05 | .29 | .12 | — | 5.34 (3.65) | ||
| 10. Entitlement | −.01 | .36 | .13 | .25 | .17 | .08 | −.24 | .26 | −.17 | — | 8.07 (3.72) | |
| 11. Exhibitionism | −.03 | .41 | .27 | −.06 | .21 | .06 | −.20 | .09 | −.02 | .41 | — | 7.71 (3.67) |
| 12. Detachment | .26 | −.44 | −.08 | .33 | .15 | .14 | .41 | .17 | .01 | −.10 | −.42 | 5.22 (3.46) |
| 13. Impulsivity | .09 | −.02 | .63 | .09 | .43 | .24 | .27 | .26 | .13 | −.12 | .20 | 5.53 (3.73) |
| 14. Propriety | .23 | .20 | −.13 | .30 | −.04 | .06 | .01 | .10 | .09 | .28 | .06 | 10.61 (4.40) |
| 15. Workaholism | .31 | .39 | −.12 | .38 | .07 | .18 | .08 | .35 | −.05 | .29 | .05 | 7.08 (3.81) |
| 16. Prior Disorder Severity | .41 | −.14 | −.03 | .26 | .12 | .10 | .31 | .10 | .22 | −.02 | −.07 | 2.97 (1.78) |
| 17. Prior Comorbidity | .38 | −.16 | .03 | .30 | .18 | .11 | .38 | .14 | .25 | −.08 | −.10 | 89 (22.9%) |
| 18. Prior Recurrence | .24 | −.15 | .02 | .07 | .07 | .06 | .26 | .05 | .23 | −.19 | −.08 | 78 (20.5%) |
| 19. Early Onset | .18 | −.08 | −.04 | .06 | .01 | .06 | .14 | −.02 | .11 | −.07 | −.03 | 81 (20.9%) |
| 20. Gender | .07 | .07 | −.22 | −.04 | −.23 | −.13 | −.11 | −.21 | .10 | .03 | −.01 | 264 (68.0%) |
| 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | |
|---|---|---|---|---|---|---|---|---|
| 12. Detachment | — | |||||||
| 13. Impulsivity | −.04 | — | ||||||
| 14. Propriety | .00 | −.30 | — | |||||
| 15. Workaholism | .15 | −.10 | .38 | — | ||||
| 16. Prior Disorder Severity | .16 | −.02 | .12 | .14 | — | |||
| 17. Prior Comorbidity | .21 | .08 | .08 | .07 | .54 | — | ||
| 18. Prior Recurrence | .06 | .08 | −.01 | −.02 | .43 | .46 | — | |
| 19. Early Onset | .04 | .06 | .04 | .04 | .41 | .30 | .46 | — |
| 20. Gender | −.09 | −.17 | −.05 | −.05 | .13 | .05 | .05 | .08 |
All correlations greater than |.09|, |.11|, and |.15| are statistically significant at the .05, .01, and .001 alpha levels, respectively. For gender, female = 1, male = 0. N = frequency of a binary predictor.
Table 2 presents rates of new onsets and recurrences of internalizing diagnoses at each assessment point. Over the four years of follow-up, 49 participants experienced a new onset and 45 experienced a recurrence. Of the new onsets, 32 were diagnosed among people with a history of some internalizing disorder other than the new diagnosis and 17 were diagnosed among people previously free from all internalizing psychopathology.
Table 2.
Rates of New Onset and Recurrence over Follow-up
| Time 6 (n = 345)
|
Time 7 (n = 353)
|
Time 8 (n = 326)
|
Time 9 (n = 238)
|
Time 10 (n = 121)
|
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No History | Prior History | New | Rec | New | Rec | New | Rec | New | Rec | |
| Major Depression | 238 | 120 | 6 | 17 | 11 | 9 | 1 | 7 | 1 | 2 |
| Dysthymia | 358 | 9 | 3 | 0 | 1 | 2 | 1 | 0 | 1 | 0 |
| Panic Disorder | 362 | 8 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 |
| Generalized Anxiety Disorder | 353 | 12 | 6 | 2 | 5 | 0 | 1 | 0 | 0 | 0 |
| Social Phobia | 316 | 41 | 4 | 2 | 7 | 3 | 0 | 1 | 1 | 0 |
| Specific Phobia | 343 | 21 | 3 | 1 | 5 | 1 | 1 | 1 | 0 | 0 |
| Post-Traumatic Stress Disorder | 361 | 9 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 |
| Obsessive-Compulsive Disorder | 353 | 15 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 0 |
| Any Internalizing Disorder | 201 | 130 | 21 | 20 | 22 | 14 | 4 | 9 | 2 | 2 |
Total sample size = 371. The ns at each timepoint refer to the number of participants interviewed at a given wave. The Time 6 Prior History column refers to the number of people with a history, but no current manifestation, of a particular internalizing disorder at Time 6, whereas the No History column refers to the number of people with no past or current diagnosis of that disorder at Time 6. The difference between the sum of the No History and Prior History columns and the total sample size represents the number of participants with a current manifestation of a given diagnosis at Time 6 (e.g., there was one current diagnosis of PTSD [371 – (361 + 9)]). For the 26 participants absent at Time 6 but recontacted at Times 7–10, history of disorders up to Time 6 was determined by responses to diagnostic interviews at previous timepoints (i.e., Times 1–5). Rec = number of recurrences; New = number of new onsets.
Prospective Associations of Personality Traits with New Onsets
Table 3 presents bivariate and multivariate models of new onsets of internalizing syndromes. In the preliminary bivariate models, all abnormal personality traits in the Negative Temperament domain predicted new onset rates, with a median odds ratio (OR) of 1.42 (range: 1.30–1.89). Impulsivity was the only other abnormal personality dimension to show a statistically significant effect on new onsets (OR = 1.41). Regarding temperament scales, Positive Temperament had virtually no impact on new onsets, whereas Negative Temperament and Disinhibition versus Control levels were both positively related to risk for new onsets over follow-up. Prior internalizing disorder severity also had a statistically significant effect on the probability of new onsets. Specifically, each one-point increment in maximum (across all internalizing disorders) CSR rating prior to Time 6 increased the chances of a new disorder onset by 23%.
Table 3.
Discrete-Time Survival Models for New Onset and Recurrence
| New Onseta
|
Recurrenceb
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bivariate Model
|
Multivariate Model
|
Bivariate Model
|
Multivariate Model
|
|||||||||
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | |
| Personality Trait Scales | ||||||||||||
| Temperament | ||||||||||||
| Negative Temperament | 1.96 | 1.49,2.61 | .0000 | 1.50 | 1.01,2.25 | .0404 | 2.00 | 1.39,2.86 | .0001 | 1.63 | 1.07,2.48 | .0198 |
| Positive Temperament | 0.91 | 0.68,1.20 | .4752 | 0.68 | 0.50,0.90 | .0076 | 0.87 | 0.63,1.23 | .4443 | |||
| Disinhibition | 1.38 | 1.06,1.79 | .0139 | 1.04 | 0.70,1.55 | .8415 | 1.02 | 0.73,1.43 | .9904 | |||
| Abnormal Personality | ||||||||||||
| Mistrust | 1.44 | 1.08,1.90 | .0102 | 1.07 | 0.70,1.62 | .7718 | 1.34 | 1.01,1.77 | .0385 | 0.88 | 0.63,1.23 | .4437 |
| Manipulativeness | 1.71 | 1.30,2.27 | .0001 | 1.31 | 0.88,1.95 | .1770 | 0.96 | 0.71,1.30 | .7895 | |||
| Aggression | 1.30 | 1.01,1.70 | .0455 | 1.00 | 0.73,1.38 | .9999 | 1.24 | 0.91,1.67 | .1615 | |||
| Self-Harm | 1.38 | 1.08,1.75 | .0076 | 0.89 | 0.66,1.20 | .4237 | 1.65 | 1.32,2.05 | .0000 | 1.41 | 1.05,1.92 | .0198 |
| Eccentric Perceptions | 1.40 | 1.11,1.79 | .0047 | .99 | 0.73,1.34 | .9466 | 1.03 | 0.75,1.42 | .8513 | |||
| Dependency | 1.89 | 1.46,2.46 | .0000 | 1.64 | 1.19,2.25 | .0022 | 1.19 | 0.90,1.58 | .1971 | |||
| Entitlement | 1.00 | 0.73,1.38 | .9999 | 0.76 | 0.55,1.04 | .0801 | ||||||
| Exhibitionism | 1.04 | 0.79,1.38 | .7718 | 0.80 | 0.58,1.09 | .1499 | ||||||
| Detachment | 1.11 | 0.84,1.46 | .4752 | 1.19 | 0.91,1.54 | .1902 | ||||||
| Impulsivity | 1.41 | 1.06,1.62 | .0151 | 1.20 | 0.80,1.79 | .3681 | 1.10 | 0.79,1.51 | .5738 | |||
| Propriety | 1.12 | 0.84,1.48 | .4319 | 0.99 | 0.72,1.36 | .9502 | ||||||
| Workaholism | 1.00 | 0.74,1.35 | .9999 | 1.09 | 0.77,1.52 | .6380 | ||||||
| Clinical Covariates | ||||||||||||
| Prior Disorder Severity | 1.23 | 1.05,1.45 | .0085 | 1.11 | 0.88,1.42 | .3576 | 1.56 | 1.03,1.93 | .0324 | 1.22 | 0.73,2.10 | .4413 |
| Prior Disorder Comorbidity | 1.70 | 0.90,3.22 | .0969 | 0.59 | 0.24,1.42 | .2301 | 1.99 | 1.05,3.78 | .0308 | 0.97 | 0.33,2.20 | .9417 |
| Prior Recurrence | 1.90 | 0.98,3.67 | .0524 | 1.13 | 0.51,2.51 | .7642 | 1.96 | 1.04,3.74 | .0332 | 1.37 | 0.67,2.83 | .3735 |
| Early Onset of Disorder | 1.10 | 0.53,2.25 | .8026 | 1.36 | 0.73,2.53 | .3173 | ||||||
| Gender | 1.07 | 0.71,2.03 | .8259 | 2.20 | 1.01,4.90 | .0483 | 2.43 | 1.05,5.64 | .0340 | |||
OR = odds ratio; CI = confidence interval.
N = 371;
N = 163.
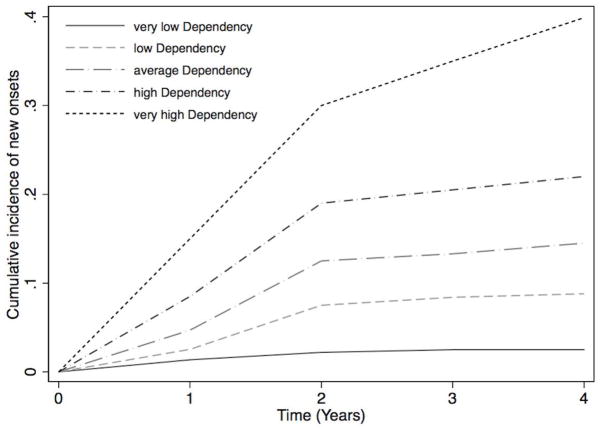
Effect sizes were generally attenuated in the multivariate model, and Dependency (OR = 1.64) and Negative Temperament (OR = 1.50) were the only predictors to have statistically significant independent effects on risk for new internalizing disorders. Figure 1 depicts the nature of the association between Dependency and risk for new internalizing disorders over time.
Figure 1.
Cumulative incidence function for the new onset of any internalizing disorder as a function of Dependency. “Very low” and “very high” refer to two standard deviations from the mean of Dependency, and “low” and “high” refer to one standard deviation from the mean.
Prospective Associations of Personality Traits with Recurrences
Table 3 summarizes the associations of personality traits with risk for recurrence. Only four personality traits—two abnormal personality dimensions (Self-Harm, Mistrust) and two temperament scales (Negative Temperament, Positive Temperament)—exhibited statistically significant bivariate relations with recurrence. Of the clinical covariates, all but early onset predicted higher rates of recurrence over follow-up. In the multivariate analysis, Self-Harm (OR = 1.41), Negative Temperament (OR = 1.63), and female gender (OR = 2.43) retained significant associations with recurrence. Figure 2 illustrates the nature of the association between Self-Harm variation and risk for recurrence over follow-up.
Figure 2.
Cumulative incidence function for the recurrence of any internalizing disorder as a function of Self-Harm. “Very low” and “very high” refer to two standard deviations from the mean of Self-Harm, and “low” and “high” refer to one standard deviation from the mean.
Discussion
A PD diagnosis often signals poor prognosis for depression and anxiety, but the core pathological personality processes mediating this effect are unknown. We went beyond prior research based on DSM-defined PDs by examining the prognostic status of precise abnormal personality traits and temperament dimensions that form the scaffolding for the PD domain. We also incorporated clinical risk factors—including prior internalizing disorder severity, recurrence, and comorbidity—into our predictive models to evaluate the effect sizes of abnormal personality constructs while adjusting for the effects of established risk factors. There were two main findings: (1) multiple abnormal personality traits—particularly those related to Negative Temperament—were related to the trajectory of internalizing problems over four years of follow-up; and (2) abnormal trait effect sizes were attenuated when adjusting for temperament and clinical risk factors, such that only Dependency (new onset) and Self-Harm (recurrence) retained significant associations with the course of internalizing disorders.
Prior research has connected numerous PDs with the development and exacerbation of internalizing disorders.[5] Results from our bivariate models were consistent with these findings in that multiple abnormal personality trait dimensions—especially Negative Temperament traits—portended a negative course of internalizing disorder. However, in multivariate analyses designed to isolate the independent effects of each abnormal personality trait, only two dimensions emerged as influential predictors. Dependency, or the predisposition toward an external locus of control and limited self-reliance, increased the odds of developing a new internalizing disorder. Self-Harm, reflecting low self-esteem and self-destructive tendencies, was the only abnormal personality dimension that demonstrated an independent effect on the probability of recurrence. To that extent that Dependency and Self-Harm are central features of borderline PD (cf. DSM-5 diagnostic criteria related to abandonment and suicidality), these results are in line with prior studies showing that the deleterious effects of borderline PD on concurrent internalizing pathology exceed those of other PDs.[e.g., 5,49] It is notable that Dependency was only weakly related to recurrence and Self-Harm had little effect on new onsets of disorder. This disjunction suggests that different forms of personality pathology may be relevant to separate elements of the trajectory of internalizing problems.
The prospective influence of these abnormal traits on the trajectory of internalizing problems withstood statistical adjustment for temperament variation. The importance of that adjustment was evident from moderate to large bivariate effect sizes for temperament dimensions, conforming with some, but not all, prior research on the role of broadband personality constructs in risk for internalizing psychopathology.[see 26] For instance, a standard unit increment in Negative Temperament roughly doubled the odds of both new onsets and recurrences in bivariate models. Our results suggest that the deleterious effects of PD on the trajectory of internalizing problems is attributable in part to abnormal personality variation, and not only extreme standing on core temperament dimensions such as Negative Temperament. These prospective associations provide some support for a pathoplasty model of personality-internalizing relations.[29] The pathoplasty model holds that personality influences the expression of disorder after its onset. Thus, Negative Temperament and Self-Harm demonstrated pathoplastic effects on internalizing disorders over time insofar as they predicted the temporal course (i.e., recurrence) of disorder.
In addition to temperament dimensions, relevant clinical and demographic features were included in our survival analyses to account for other possible explanations for the effect of PD on internalizing risk. The severity, comorbidity, age of onset, and recurrence of prior internalizing pathology have all been linked in previous research to the course of depression and anxiety.[1,2,39,50] Indeed, in bivariate analyses, histories of comorbidity and recurrence were responsible for large increases in risk for future internalizing disorder episodes (OR range: 1.70–1.99). However, when covariation among risk factors was partialled out, these effects were no longer statistically significant, likely reflecting the considerable overlap of these clinical features with each other and with personality traits in the Negative Temperament domain (see Table 1). Finally, after adjusting for the presence of all other risk factors, female gender was linked with more than double the odds of disorder recurrence, consistent with several prior investigations on the relation between gender and MDD recurrence.[e.g.,51] Possibly due to the high-risk nature of the sample, gender was not related to first onsets of internalizing disorders, as would be expected in the general population.[45,52]
Several limitations of the present study should be noted. First, the sample available for survival analyses was a subset of participants completing YEP baseline procedures (i.e., 371 of 627). Additionally, the baseline sample was a subset of the 1,269 students originally invited to participate in the study. Although attrition analyses suggested that our final sample did not diverge considerably from the original sample with respect to several demographic features, baseline participants endorsed more neuroticism/negative temperament than those who declined to participate. Additionally, the considerable dropout over the 10 years of follow-up diminishes, to some extent, the generalizability of findings. Also relevant to generalizability, our study addressed the personality underpinnings of internalizing disorders in a specific developmental epoch (i.e., young adulthood). Many internalizing disorders tend to onset prior in childhood or early adolescence (i.e., prior to our study baseline phase); therefore, effect sizes might vary in younger samples.
Second, we collapsed across all internalizing diagnostic categories in the present study due to the relatively low frequency of individual disorders. However, evidence from cross-sectional research supports some specificity in personality-disorder relations, in particular the linkage of extraversion/positive temperament with social phobia and the depressive disorders.[21,26] Future work in large clinical samples is needed to determine whether certain abnormal personality traits (e.g., SNAP Positive Temperament traits) show specific links with individual internalizing syndromes. Third, the SNAP was administered at only one time point, precluding investigation into the dynamic interrelations between personality and psychopathology constructs. Research involving repeated assessments of personality pathology and clinical disorders has the potential to adjudicate between different explanatory models of personality-psychopathology relations (e.g., common cause model, scar model).[29] Additionally, because the SNAP was administered two months after Time 6, it is possible that some (but probably very few) disorder onsets recorded at Time 7 actually occurred before the SNAP was completed. Therefore, it must be noted that the present design is not fully prospective. Fourth, the present sample was enriched for elevated neuroticism/negative temperament, and comparisons with unselected samples therefore must be made with caution. Fifth, the sample size for multivariate analyses was modest. Multivariate results should be considered alongside results from the simpler bivariate analyses when evaluating personality trait effect sizes. Along these same lines, the multiple significance tests needed to evaluate the full set of SNAP dimensions and competing clinical covariates raised the probability of Type I error. Thus, we recommend some caution in interpreting the results—especially those hovering around the threshold of statistical significance—until large-scale replication studies are available, and we suggest that interpretations focus on effect sizes rather than significance tests. Sixth, there were some non-standard aspects to SCID administration (i.e., advanced student interviewers versus those with terminal degrees; administration in adolescence). Thus, although reliability proved acceptable in this study, the validity of this specific application of the SCID remains to be systematically examined. Finally, the content of some abnormal personality traits overlapped with the psychopathology of internalizing disorders (e.g., Self-Harm and depressive disorders), raising the possibility of artificially inflated effect sizes due to criterion contamination. However, we expect any such inflation was minimized by statistical adjustment for prior severity of internalizing problems.
Conclusion
In sum, we adopted a new approach to investigating the effects of PD on coexisting internalizing problems by dismantling PD into its constituent abnormal personality and temperament dimensions. The Dependency and Self-Harm abnormal dimensions prospectively influenced the trajectory of internalizing disorders, but in different ways: Dependency predicted new onsets, whereas Self-Harm predicted recurrences. These effects withstood statistical adjustments for variation on core temperament dimensions. Our findings inform explanatory models of internalizing psychopathology and highlight the abnormal personality traits that may provide the best prognostic information in assessment and treatment settings.
Acknowledgments
This research was supported by a two-site grant from the National Institute of Mental Health (NIMH) to MGC (R01-MH065651) and to SM and REZ (R01-MH065652). The content is the responsibility of the authors and does not necessarily represent the official views of the NIMH.
Footnotes
Conflict of Interest Disclosure: Drs. Craske, Mineka, and Zinbarg report grant funding from the National Institute of Mental Health during the conduct of the study.
References
- 1.Lewinsohn PM, Rohde P, Seeley JR, Klein DN, Gotlib IH. Natural course of adolescent major depressive disorder in a community sample: predictors of recurrence in young adults. Am J Psychiatry. 2000;157:1584–1591. doi: 10.1176/appi.ajp.157.10.1584. [DOI] [PubMed] [Google Scholar]
- 2.Tyrer P, Seivewright H, Johnson T. The Nottingham Study of Neurotic Disorder: Predictors of 12-year outcome of dysthymic, panic and generalized anxiety disorder. Psychol Med. 2004;34:1385–1394. doi: 10.1017/s0033291704002569. [DOI] [PubMed] [Google Scholar]
- 3.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3. Washington, DC: American Psychiatric Association; 1980. [Google Scholar]
- 4.Massion AO, Dyck IR, Shea MT, Phillips KA, Warshaw MG, Keller MB. Personality disorders and time to remission in generalized anxiety disorder, social phobia, and panic disorder. Arch Gen Psychiatry. 2002;59:434–440. doi: 10.1001/archpsyc.59.5.434. [DOI] [PubMed] [Google Scholar]
- 5.Skodol AE, Grilo CM, Keyes K, Geier T, Grant BF, Hasin DS. Relationship of personality disorders to the course of major depressive disorder in a nationally representative sample. Am J Psychiatry. 2011;168:257–264. doi: 10.1176/appi.ajp.2010.10050695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Newton-Howes G, Tyrer P, Johnson T, Mulder R, Kool S, Dekker J, Schoevers R. Influence of personality on the outcome of treatment in depression: Systematic review and meta-analysis. J Pers Disord. 2013;27:1–17. doi: 10.1521/pedi_2013_27_070. [DOI] [PubMed] [Google Scholar]
- 7.Grilo CM, Sanislow CA, Shea MT, Skodol AE, Stout RL, Gunderson JG, McGlashan TH. Two-year prospective naturalistic study of remission from major depressive disorder as a function of personality disorder comorbidity. J Consult Clin Psychol. 2005;73:78–85. doi: 10.1037/0022-006X.73.1.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grilo CM, Stout RL, Markowitz JC, Sanislow CA, Ansell EB, Skodol AE, McGlashan TH. Personality disorders predict relapse after remission from an episode of major depressive disorder: A 6-year prospective study. J Clin Psychiatry. 2010;71:1629–1635. doi: 10.4088/JCP.08m04200gre. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Noyes R, Jr, Reich J, Christiansen J, Suelzer M, Pfohl B, Coryell WA. Outcome of panic disorder: relationship to diagnostic subtypes and comorbidity. Arch Gen Psychiatry. 1990;47:809–818. doi: 10.1001/archpsyc.1990.01810210017003. [DOI] [PubMed] [Google Scholar]
- 10.Yonkers KA, Dyck IR, Warshaw M, Keller MB. Factors predicting the clinical course of generalised anxiety disorder. Br J Psychiatry. 2000;176:544–549. doi: 10.1192/bjp.176.6.544. [DOI] [PubMed] [Google Scholar]
- 11.Mennin DS, Heimberg RG. The impact of comorbid mood and personality disorders in the cognitive-behavioral treatment of panic disorder. Clin Psychol Rev. 2000;20:339–357. doi: 10.1016/s0272-7358(98)00095-6. [DOI] [PubMed] [Google Scholar]
- 12.Clark LA. Assessment and diagnosis of personality disorder: Perennial issues and an emerging reconceptualization. Annu Rev Psychol. 2007;58:227–257. doi: 10.1146/annurev.psych.57.102904.190200. [DOI] [PubMed] [Google Scholar]
- 13.Widiger TA, Trull TJ. Plate tectonics in the classification of personality disorder: Shifting to a dimensional model. Am Psychol. 2007;62:71–83. doi: 10.1037/0003-066X.62.2.71. [DOI] [PubMed] [Google Scholar]
- 14.Kupfer DJ, First MB, Regier DA, editors. A Research agenda for DSM-V. Washington, DC: American Psychiatric Association; 2008. [Google Scholar]
- 15.Grant BF, Hasin DS, Stinson FS, Dawson DA, Chou SP, Ruan WJ, Pickering RP. Prevalence, correlates, and disability of personality disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry. 2004;65:948–958. doi: 10.4088/jcp.v65n0711. [DOI] [PubMed] [Google Scholar]
- 16.Siever LJ, Davis KL. A psychobiological perspective on the personality disorders. Am J Psychiatry. 1991;148:1647–1658. doi: 10.1176/ajp.148.12.1647. [DOI] [PubMed] [Google Scholar]
- 17.Widiger TA, Clark LA. Toward DSM-V and the classification of psychopathology. Psych Bull. 2000;126:946–963. doi: 10.1037/0033-2909.126.6.946. [DOI] [PubMed] [Google Scholar]
- 18.Livesley WJ, Jackson D. Manual for the Dimensional Assessment of Personality Pathology—Basic Questionnaire. Port Huron, MI: Sigma; 2009. [Google Scholar]
- 19.Clark LA, Simms LJ, Wu KD, Casillas A. Manual for the Schedule for Nonadaptive and Adaptive Personality–2nd Edition (SNAP) Minneapolis: University of Minnesota; in press. [Google Scholar]
- 20.Reynolds SK, Clark LA. Predicting dimensions of personality disorder from domains and facets of the five-factor model. J Pers. 2001;69:199–222. doi: 10.1111/1467-6494.00142. [DOI] [PubMed] [Google Scholar]
- 21.Watson D, Stasik SM, Ro E, Clark LA. Integrating normal and pathological personality relating the DSM-5 trait-dimensional model to general traits of personality. Assessment. 2013;20:312–326. doi: 10.1177/1073191113485810. [DOI] [PubMed] [Google Scholar]
- 22.Widiger TA, Livesley WJ, Clark LA. An integrative dimensional classification of personality disorder. Psychol Assess. 2009;21:243–255. doi: 10.1037/a0016606. [DOI] [PubMed] [Google Scholar]
- 23.Clark LA, Vittengl J, Kraft D, Jarrett RB. Separate personality traits from states to predict depression. J Pers Disord. 2003;17:152–172. doi: 10.1521/pedi.17.2.152.23990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gamez W, Watson D, Doebbeling BN. Abnormal personality and the mood and anxiety disorders: Implications for structural models of anxiety and depression. J Anxiety Disord. 2007;21:526–539. doi: 10.1016/j.janxdis.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 25.Ro E, Clark LA. Interrelations between psychosocial functioning and adaptive- and maladaptive-range personality traits. J Abnorm Psychol. 122:822–835. doi: 10.1037/a0033620. [DOI] [PubMed] [Google Scholar]
- 26.Kotov R, Gamez W, Schmidt F, Watson D. Linking “big” personality traits to anxiety, depressive, and substance use disorders: A meta-analysis. Psych Bull. 2010;136:768–821. doi: 10.1037/a0020327. [DOI] [PubMed] [Google Scholar]
- 27.Vittengl JR, Clark LA, Thase ME, Jarrett RB. Nomothetic and idiographic symptom change trajectories in acute-phase cognitive therapy for recurrent depression. J Consult Clin Psychol. 2013;81:615–626. doi: 10.1037/a0032879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Duggan CF, Lee AS, Murray RM. Does personality predict long-term outcome in depression? Br J Psychiatry. 1990;157:19–24. doi: 10.1192/bjp.157.1.19. [DOI] [PubMed] [Google Scholar]
- 29.Klein DN, Kotov R, Bufferd SJ. Personality and depression: explanatory models and review of the evidence. Annu Rev Clin Psychol. 2011;7:269–295. doi: 10.1146/annurev-clinpsy-032210-104540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Morris BH, Bylsma LM, Rottenberg J. Does emotion predict the course of major depressive disorder? A review of prospective studies. Br J Clin Psychol. 2009;48:255–273. doi: 10.1348/014466508X396549. [DOI] [PubMed] [Google Scholar]
- 31.Quilty LC, De Fruyt F, Rolland JP, Kennedy SH, Rouillon PF, Bagby RM. Dimensional personality traits and treatment outcome in patients with major depressive disorder. J Affect Disord. 2008;108:241–250. doi: 10.1016/j.jad.2007.10.022. [DOI] [PubMed] [Google Scholar]
- 32.Eysenck HJ, Eysenck SBG. Manual of the Eysenck Personality Questionnaire. London: Hodder & Stoughton; 1975. [Google Scholar]
- 33.Zinbarg RE, Mineka S, Craske MG, Griffith JW, Sutton J, Rose RD, Waters AM. The Northwestern-UCLA youth emotion project: Associations of cognitive vulnerabilities, neuroticism and gender with past diagnoses of emotional disorders in adolescents. Behav Res Ther. 2010;48:347–358. doi: 10.1016/j.brat.2009.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Clark LA, Livesley WJ, Schroeder ML, Irish SL. The structure of maladaptive personality traits: Convergent validity between two systems. Psychol Assess. 1996;8:294–303. [Google Scholar]
- 35.Melley AH, Oltmanns TF, Turkheimer E. The Schedule for Nonadaptive and Adaptive Personality (SNAP): Temporal stability and predictive validity of the diagnostic scales. Assessment. 2002;9:181–187. doi: 10.1177/10791102009002009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV-TR Axis I disorders, research version, non-patient edition (SCID-I/NP) New York: New York State Psychiatric Institute; 2002. [Google Scholar]
- 37.Di Nardo PA, Barlow DH. Anxiety disorders interview schedule-revised (ADIS-R) Albany, NY: Phobia and Anxiety Disorders Clinic, State University of New York; 1988. [Google Scholar]
- 38.Hosmer DW, Lemeshow S, May S. Applied survival analysis: Regression modeling of time to event data. 2. Hoboken, NJ: John Wiley & Sons, Inc; 2008. [Google Scholar]
- 39.Watson D, Naragon-Gainey K. Personality, emotions, and the emotional disorders. Clin Psychol Sci. 2:422–442. doi: 10.1177/2167702614536162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Spijker J, de Graaf R, Bijl RV, Beekman AT, Ormel J, Nolen WA. Determinants of persistence of major depressive episodes in the general population. Results from the Netherlands Mental Health Survey and Incidence Study (NEMESIS) J Affect Disord. 2004;81:231–240. doi: 10.1016/j.jad.2003.08.005. [DOI] [PubMed] [Google Scholar]
- 40.de Graaf R, Bijl RV, Ravelli A, Smit F, Vollenbergh WAM. Predictors of first incidence of DSM-III-R psychiatric disorders in the general population: findings from the Netherlands Mental Health Survey and Incidence Study. Acta Psychiatr Scand. 2002;106:303–13. doi: 10.1034/j.1600-0447.2002.01397.x. [DOI] [PubMed] [Google Scholar]
- 41.Kendler KS, Gatz M, Gardner CO, Pederson NL. Personality and major depression. Arch Gen Psychiatry. 2006;63:1113–20. doi: 10.1001/archpsyc.63.10.1113. [DOI] [PubMed] [Google Scholar]
- 42.Kennedy N, Abbott R, Paykel ES. Remission and recurrence of depression in the maintenance era: long-term outcome in a Cambridge cohort. Psychol Med. 2003;33:827–838. doi: 10.1017/s003329170300744x. [DOI] [PubMed] [Google Scholar]
- 43.Klein D, Shankman S, Rose S. Ten-year prospective follow-up study of the naturalistic course of dysthymic disorder and double depression. Am J Psychiatry. 2006;163:872–880. doi: 10.1176/ajp.2006.163.5.872. [DOI] [PubMed] [Google Scholar]
- 44.Klein DN, Schatzberg AF, McCullough JP, Dowling F, Goodman D, Howland RH, Keller MB. Age of onset in chronic major depression: relation to demographic and clinical variables, family history, and treatment response. J Affect Disord. 1999;55:149–157. doi: 10.1016/s0165-0327(99)00020-8. [DOI] [PubMed] [Google Scholar]
- 45.Craske MG. Origins of phobias and anxiety disorders: Why more women than men? Amsterdam: Elsevier; 2003. [Google Scholar]
- 46.Nolen-Hoeksema S, Girgus JS. The emergence of gender differences in depression during adolescence. Psych Bull. 1994;115:424–443. doi: 10.1037/0033-2909.115.3.424. [DOI] [PubMed] [Google Scholar]
- 47.Kornstein SG, Schatzberg AF, Thase ME, Yonkers KA, McCullough JP, Keitner G, Keller MB. Gender differences in chronic major and double depression. J Affect Disord. 2000;60:1–11. doi: 10.1016/s0165-0327(99)00158-5. [DOI] [PubMed] [Google Scholar]
- 48.StataCorp. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP; 2013. [Google Scholar]
- 49.Gunderson JG, Stout RL, Sanislow CA, Shea MT, McGlashan TH, Zanarini MC, Skodol AE. New episodes and new onsets of major depression in borderline and other personality disorders. J Affect Disord. 2008;111:40–45. doi: 10.1016/j.jad.2008.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pine DS, Cohen P, Gurley D, Brook J, Ma Y. The risk for early-adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Arch Gen Psychiatry. 1998;55:56–64. doi: 10.1001/archpsyc.55.1.56. [DOI] [PubMed] [Google Scholar]
- 51.Kendler KS, Kuhn J, Prescott The interrelationship of neuroticism, sex, and stressful life events in the prediction of episodes of major depression. Am J Psychiatry. 2004;161:631–636. doi: 10.1176/appi.ajp.161.4.631. [DOI] [PubMed] [Google Scholar]
- 52.Rohde P, Lewinsohn PM, Klein DN, Seeley JR, Gau JM. Key characteristics of major depressive disorder occurring in childhood, adolescence, emerging adulthood, and adulthood. Clin Psychol Sci. 2013;1:41–53. doi: 10.1177/2167702612457599. [DOI] [PMC free article] [PubMed] [Google Scholar]