Abstract
Both acute stressful life events and ongoing strains are thought to confer vulnerability to emotional disorders. Unremitting stressful conditions may be particularly pathogenic, but prior research has struggled to delimit chronic versus transient stressful experiences. We aimed to isolate stable stressors—theorized to be indicators of a latent stress proneness trait—and to examine their effects on the temporal course of depression and panic disorder. We recruited 677 patients diagnosed with an emotional disorder and administered interviews for psychopathology and life stress three times over 12-month intervals. Trait-state-occasion modeling revealed that 74% of the variance in life stress was stable over the follow-up period. These stable stressors were associated with a more refractory course of depression and, to a much lesser extent, panic disorder over time. Additionally, neither gender nor participation in cognitive-behavioral therapy affected the persistence of environmental stress over the study timeframe. We discuss implications of these findings for explaining depression recurrence, improving psychological interventions for emotional disorders, and the measurement and evaluation of stress proneness.
Keywords: depression, panic, stress, trait-state-occasion modeling
Some stressful conditions are transient, whereas others endure and transform into ongoing strains. There is reason to believe that continuously stressful environments have a particularly strong influence on the temporal course of emotional disorders (Brown & Harris, 1978; Rutter & Sandberg, 1992). However, cross-sectional research has struggled to isolate the signal of enduring stressors amid the noise of transitory, and likely less pathogenic, life stress (Hammen, 2005). In a large clinical sample, the present study aimed to (a) estimate the degree of stress continuity over time, and (b) evaluate the effect of individual differences in chronic1 stress exposure on the longitudinal course of emotional disorders.
There are several possible mechanisms of stress continuity. First, many relationship, health, and occupational stressors are essentially continuous (e.g., chronic marital strain, obesity). Second, stress can beget stress (Paykel, 2003), in the sense that one stressful condition eventually can tax resources in other domains (e.g., divorce settlement leads to financial difficulty). Third, according to stress generation theory (Hammen, 1991), several traitlike psychological characteristics (e.g., excessive reassurance-seeking) confer vulnerability to stress exposure (Liu & Alloy, 2010). Consistent with these putative mechanisms of stress continuity, several lines of research have documented rank-order stability in stress exposure across both brief (e.g., weeks) and long (e.g., decades) intervals (e.g., Hazel, Hammen, Brennan, & Najman, 2008; Pearlin et al., 2005; Turner & Butler, 2003).
Although previous longitudinal data suggest that a stable aspect to major stress exposure almost certainly exists (e.g., Hazel et al., 2008), no research to date has attempted to quantify it directly. In other words, we do not know what proportion of life stress observed or reported at any given time is a reflection of persistent environmental conditions versus more transient challenges. This is an important omission in the literature, given that (a) stressor chronicity is theoretically and empirically related to pathogenicity (Brown & Rosellini, 2011; Hammen, 2005), and (b) examining the stability of stressful conditions in clinical samples can shed light on how effectively psychological interventions address environmental, in addition to psychological, vulnerabilities (cf. McMain, Guimond, Streiner, Cardish, & Links, 2012; Zanarini, Frankenburg, Reich, & Fitzmaurice, 2010).
The trait-state-occasion (TSO) modeling framework was formulated to parse stable versus unstable elements of psychological constructs (Cole, Martin, & Steiger, 2005). TSO is a form of structural equation modeling that partitions a condition at any given point in time (i.e., state) into time-invariant (i.e., trait) and time-variant (i.e., occasion) components. In the present study, the trait factor captures environmental stressors that are temporally stable (i.e., constant across all waves), whereas the occasion factor captures situational stressors that are not continuously present. Stress stability represented by the trait factor is theorized to reflect stress proneness; that is, personological characteristics or behavioral tendencies that promote stressful circumstances (e.g., impulsive decision-making style, affiliation with deviant peers). Those higher on a stress proneness trait would be expected to elicit, evoke, and maintain a variety of stressful circumstances that are due, at least in part, to their attitudes, behaviors, and personality styles (e.g., relationship conflict, poor work performance, health-risk behaviors). Consistent with the notion of a stress proneness trait, there is evidence from the behavioral genetics field that stressful life events are partly heritable (e.g., Kendler, Neale, Kessler, Heath, & Eaves, 1993). In contrast, the TSO occasion factors represent stressful conditions that are less stable (e.g., recovery from a life-threatening medical problem, year-long child custody battle).
Despite the power of TSO to illuminate the longitudinal structure of life stress, it has yet to be applied in studies of serious stressors. However, trait-state-error (TSE) modeling—an analogue of TSO applied when the construct of interest is indexed by only one manifest indicator at each time point (Kenny & Zautra, 1995)—has been used in two studies of the continuity of daily hassles. The original investigation found that approximately 27% of variation in hassles assessed monthly in a sample of older adults was completely stable over 10 months (Kenny & Zautra, 1995). A more recent study in a middle-aged community sample determined that 60% of hassles was attributable to stable factors (Hazel & Hankin, 2014). Although the literature is still in its infancy, investigators have also used TSO to examine the traitlike and statelike components of psychological constructs, such as anxiety (Olatunji & Cole, 2009), depression (Cole, 2006; Cole, Nolen-Hoeksema, Girgus, & Paul, 2006), and temperament (Naragon-Gainey, Gallagher, & Brown, 2013; Prenoveau et al., 2011). The present study provides the first investigation of stress stability from a TSO perspective.2
Although quantifying the continuity of life stress is useful in its own right, we also planned to extend prior TSO research in psychopathology by examining the impact of stable stress processes on external constructs theorized to be stress-dependent. Thus, we examined change over time in depression and panic disorder severity as a function of stable stressors. These two emotional disorder constructs were selected because both often wax and wane in severity, although the role of stress in the temporal course after onset has only been systematically studied in one (i.e., depression). That is, longitudinal studies have shown stress exposure to worsen the course of depressive symptoms over time (e.g., Brown & Rosellini, 2011). In contrast, the literature on life stress and panic is largely restricted to retrospective studies of the presence of acute stress at the time of panic disorder onset (e.g., Faravelli & Pallanti, 1989; Last, Barlow, & O’Brien, 1984), but very little research has addressed the role of stress as it relates to the maintenance of panic symptoms (cf. Wade, Monroe, & Michelson, 1993). Additionally, we explored differences in the stability of life stress across two groups: men versus women and treated versus untreated participants. Women are known to be at higher risk for emotional disorders as well as many forms of social stress (Hammen, 2005; Kendler & Gardner, 2014; Kessler et al., 2003). It has yet to be determined, however, whether women are prone to more stable, as compared to more frequent, exposure to stressful conditions. Along the same lines, most psychotherapies directly target intrapsychic processes, and the extent to which they interrupt ongoing stressors is unknown.
In the present study, we applied TSO modeling to annual interview-based assessments of major stress exposure over two years in a large clinical sample. Our first objective was to determine the degree of stability (versus transience) of stressful events. By isolating the perfectly stable component of life stress, we hypothesized that we would identify—and then evaluate the predictive validity of—a stress proneness trait that is responsible for evoking and sustaining chronically stressful circumstances. Although TSO modeling of life stressors represents an initial and novel approach to the explication and evaluation of stress proneness, it should be noted that there may be other viable methods for quantifying and validating this trait (e.g., development of manifest indicators of the stress proneness construct). We return to this issue later in the paper.
After fitting the TSO model, we planned to map the trajectory of depression and panic disorder over two years as a function of chronic (i.e., time-invariant) stressors and to evaluate differences in the stability of life stress across gender and treatment status. Based on the accumulating evidence of stress continuity outlined above, we hypothesized that the majority of stressful experiences would be attributable to traitlike processes. Given prior findings linking chronic stress to poor prognosis for emotional disorders (e.g., Brown & Rosellini, 2011), we further hypothesized that this completely stable aspect of stress exposure would predict a more refractory course of depression and panic disorder symptoms over time. Regarding gender differences, a good deal of evidence suggests that post-pubertal women “generate” more stressors than men, particularly in younger age groups (see Hammen, 2005; Hankin & Abramson, 2001; Liu & Alloy, 2010). We therefore hypothesized women would exhibit heightened stability of stressful conditions. Finally, because stress generation theory posits that individual differences in stress proneness are evident even outside of an acute disorder episode (i.e., during premorbid and remitted periods), we predicted that psychological treatment—which is expected to remediate, at least to some extent, acute clinical symptoms—would not dramatically affect the stability of chronic stressors.
Method
Participants
Participants were 677 adults who presented for assessment and treatment at the Center for Anxiety and Related Disorders (CARD) at Boston University. Women constituted a larger portion of the sample (64.1%). The average age was 32.81 (SD = 12.29, range 18 to 74). The sample was predominantly Caucasian (89.7%; African-American = 4.1%; Asian = 5.8%; Other = 0.4%).
The rates of current clinical disorders that frequently occurred in the sample were as follows: panic disorder with or without agoraphobia (26.4%), social phobia (47.9%), generalized anxiety disorder (36.2%), obsessive-compulsive disorder (13.7%), posttraumatic stress disorder (4.4%), specific phobia (13.9%), anxiety disorder not otherwise specified (7.5%), major depressive disorder (24.1%), dysthymia (3.5%), and depressive disorder not otherwise specified (3.0%).
Procedures
Participants underwent a semistructured interview and completed a series of self-report questionnaires at the time of their initial assessment. Current and past diagnoses were established with the Anxiety Disorders Interview Schedule for DSM-IV-Lifetime version (ADIS-IV-L; Di Nardo, Brown, & Barlow, 1994). The ADIS-IV-L is a semistructured diagnostic interview designed to ascertain reliable diagnosis of the DSM-IV anxiety, mood, somatoform, and substance use disorders, and to screen for the presence of other conditions (e.g., psychotic disorders). The ADIS-IV-L has been shown to have good-to-excellent interrater agreement for current disorders (κs = .67 to .86) except dysthymia (κ = .31; Brown, Di Nardo, Lehman, & Campbell, 2001). Patients were reevaluated at 12 months (Time 2, T2) and 24 months (Time 3, T3) using the follow-up version of the ADIS-IV, which is identical to the ADIS-IV-L except that (a) sections for past diagnoses are omitted, and (b) a section is included to assess treatment follow-up (74% of participants received cognitive-behavioral therapy at CARD over the course of the study). Both ADIS-IV versions provide dimensional assessment of the key and associated features of disorders (0–8 ratings); such features are dimensionally rated regardless of whether a formal DSM-IV diagnosis is under consideration. For example, for major depressive disorder, ratings of each symptom that comprise the nine diagnostic features of a major depressive episode were rated dimensionally (0 = none to 8 = very severely disturbing/disabling) for the entire sample at each assessment point.
Measures
Multiple indicators (including self-report and interview measures) were selected for each construct, using marker variables similar or identical to those in Brown (2007). Each measure was completed at all three assessments, and the measure listed first was used as the marker indicator for a given construct in the latent variable analyses.
Depression
Indicators for a unipolar depression factor were: (a) Depression scale of the 21-item version of the Depression Anxiety Stress Scales (DASS-D; Lovibond & Lovibond, 1995; cf. Antony, Bieling, Cox, Enns, & Swinson, 1998; Brown, Chorpita, Korotitsch, & Barlow, 1997); (b) Beck Depression Inventory (BDI; Beck & Steer, 1987); and (c) the ADIS-IV dimensional ratings of the nine-symptom criteria of DSM-IV major depression, which ranged from 0 (none) to 8 (severe; interrater r = .74, Brown et al., 2001). In accordance with prior studies (e.g., Brown, 2007; Brown, Chorpita, & Barlow, 1998), the BDI was scored using the 10 items that load on a Cognitive/Affective factor (items 1–9, 13) because they are more specific to the unipolar mood disorders. Unlike the DASS-Depression indicator, the full BDI is comprised of items both specific and nonspecific to the construct of depression. Depression-specific items (as determined by factor analysis; see Brown, Chorpita, & Barlow, 1998) were used to better define and distinguish the DEP construct from general distress. The DASS-D was chosen as the marker indicator because it provided the most units of discrimination (the same logic applies to our choice of marker indicator for the panic disorder/agoraphobia factor below). The interrater correlation for the composite ADIS-IV dimensional rating of depression was .84, and the internal consistency estimates (Cronbach’s alpha) for the DASS-D and BDI were .91 and .86, respectively.
Panic Disorder/Agoraphobia
Indicators for panic disorder/agoraphobia (PD/A) were: (a) the sum composite of the ADIS-IV dimensional ratings of situational apprehension or avoidance of 22 agoraphobic situations; (b) the 0 to 8 clinical dimensional rating of DSM-IV PD/A criterion A (recurrent panic attacks); (c) the sum composite of dimensional ratings of the three symptoms of DSM-IV PD/A criterion B (worry/change in behavior); and (d) the Agoraphobia scale of the 27-item Albany Panic and Phobia Questionnaire (APPQ; Rapee, Craske, & Barlow, 1994–1995). Interrater rs for the ADIS-IV ratings of agoraphobia, recurrent panic attacks, and apprehension/behavioral change related to future panic attacks were .81, .71, and .76, respectively. Cronbach’s alpha for the APPQ was .87.
Life Stress
Chronic stressors were assessed at intake (Time 1, T1) and at both follow-up evaluations using the UCLA Life Stress Interview (LSI; Hammen et al., 1987). The LSI is a semistructured interview that assesses stress occurring in eight domains (social life, romantic relationships, family, work, school, finances, health of self, and health of others) over the past 6 months. The LSI defines chronic stressors as adverse situations with no discrete onset and offset date (cf. acute stressful life events), and LSI chronic stressors have been reliably linked to the onset and exacerbation of emotional disorders, especially unipolar depression (see Hammen, 2005). In the present study, interviewers rated each chronic stress domain on a 5-point scale ranging from 1 (exceptionally positive circumstances) to 5 (extremely adverse circumstances) in increments of 0.5 units using behaviorally specific anchors.
Chronic stress ratings reflect role functioning in different areas. For instance, all social domains (i.e., friendship, family, romantic relationship) are based on several relationship dimensions: closeness/mutual support, trust, stability, reciprocality, frequency of conflict, and management of conflict. For example, in the social life domain, a rating of 2 reflects having many friends, weekly socializing (e.g., in person or by telephone), diversity in activities, and good conflict resolution, whereas a rating of 4 reflects a limited number of friends, infrequent social contact, sporadic engagement in limited social activities (e.g., every few months), and poor conflict resolution. Similarly, low ratings in the romantic relationship domain in this study might correspond with an unstable relationship pattern (e.g., one or more breakups or time spent apart), mistrust, an inability of the respondent to confide in the significant other, and poor conflict resolution. The LSI has demonstrated high interrater reliability and strong criterion validity (Hammen, 2005). In the present study, the interrater r for the sum of all stress domain ratings was .70.
The indicators for chronic life stress were the LSI ratings for social life, romantic relationships, family, work/school, finances, and health of self. The LSI queries work and school chronic stress separately, but given that the large majority of participants were not simultaneously in school and working, we selected the higher (i.e., more stressful) rating among the two and omitted the lower. Additionally, a separate domain assessing health of significant others (e.g., spouse, family members) was queried but omitted after preliminary analyses revealed very low correlations with other domains (results available from first author upon request).
Statistical Analysis
The raw data were analyzed in Mplus (version 7.11; Muthén & Muthén, 1998–2014) using maximum likelihood (ML) minimization functions. Model goodness of fit was evaluated by the comparative fit index (CFI), the Tucker-Lewis index (TLI), the root mean square error of approximation (RMSEA), and the standardized root mean square residual (SRMR). Guidelines offered by Hu and Bentler (1999) were used to define acceptable model fit: RMSEA values close to 0.06 or below, CFI and TLI values close to .95 or above, and SRMR values close to .08 or below. Model fit was also judged on the basis of the presence/absence of localized area of strain and by the size and interpretability of parameter estimates. Missing data due to attrition were accommodated in all analyses using direct ML (see Allison, 2003). Those who did not participate at T2 (16% of baseline sample) did not differ from those who did with respect to baseline average chronic stress level (t[675] = 0.49, p = .96), any baseline psychopathology indicator (ts[675] < |1.20|, ps > .05), age (t[675] = 0.64, p = .83), or gender (χ2[1] = 0.35, p = .38). Likewise, T3 participants did not differ from attritors (43% of baseline sample) on any stress, psychopathology, or demographic index (ts[675] < |1.95|, ps > .05; χ2[1] = 0.33, p = .33).
Results
Longitudinal Measurement Models
As a preliminary step, we tested the measurement invariance of stress and disorder constructs across study waves. Each construct must demonstrate at least partial measurement invariance over time to be suitable for longitudinal latent variable modeling (e.g., TSO), otherwise true temporal change in the constructs could be conflated with measurement change over time. Each disorder latent variable must feature at least one invariant indicator beyond the marker indicator (Byrne, Shavelson, & Muthén, 1989). Because the TSO model did not involve mean structures, the chronic stress measurement model needed only to demonstrate invariant loadings over time. In contrast, the measurement models for disorder constructs were evaluated for factor loading and indicator intercept invariance because mean structures were estimated in these models.
A sequence of longitudinal confirmatory factor analyses was conducted for each construct. We first estimated a baseline model with no constraints, then a model in which each indicator’s factor loadings were constrained to equality across time, and finally (for depression and panic) a model in which factor loadings and indicator intercepts were equal across time. In all models, error terms of the same indicator at different time points (e.g., T1 BDI, T2 BDI) were permitted to correlate across waves to account for method effects. Statistically significant increases in the model chi-square value when constraints were imposed indicated that measurement invariance did not hold.
Confirmatory factor analysis results are presented in Table 1. The factor loadings of all indicators at all waves were large (range: .40–.97) and statistically significant, and model fit indices were consistently excellent. There were only four parameters that were not time-invariant: the BDI factor loading on the Depression factor, the ADIS-agoraphobia rating factor loading on the PD/A factor, and the indicator intercepts for ADIS clinical ratings for DSM-IV PD/A criteria A and B. Therefore, the data were appropriate for longitudinal factor analyses (i.e., the longitudinal measurement models were either fully or partially invariant).
Table 1.
Standardized Factor Loadings from Longitudinal Measurement Models
| Factor Loading |
||||
|---|---|---|---|---|
| Measure | Time 1 | Time 2 | Time 3 | Model Constraint |
| Depressiona | All held equal except BDI λ | |||
| DASS-D | .85 | .89 | .91 | |
| ADIS-D | .74 | .79 | .77 | |
| BDI | .90 | .89 | .90 | |
| Panicb | All held equal except ADIS-Ag λ and ADIS-A and ADIS-B τs |
|||
| APPQ | .64 | .58 | .60 | |
| ADIS-Ag | .86 | .81 | .80 | |
| ADIS-A | .80 | .81 | .91 | |
| ADIS-B | .83 | .92 | .97 | |
| Stressc | All λs held equal | |||
| Social Life | .55 | .57 | .57 | |
| Romantic | .44 | .48 | .46 | |
| Family | .47 | .51 | .49 | |
| Work/School | .60 | .63 | .68 | |
| Financial | .59 | .62 | .64 | |
| Health | .40 | .40 | .43 | |
Note. N = 677. Time 1 = intake; Time 2 = 12-month follow-up; Time 3 = 24-month follow-up; DASS-D = Depression scale of the Depression Anxiety Stress Scales; ADIS-D = Anxiety Disorders Interview Schedule for DSM-IV (ADIS-IV) ratings of major depression; BDI = Beck Depression Inventory; APPQ = Agoraphobia scale of Albany Panic and Phobia Questionnaire; ADIS-Ag = ADIS-IV ratings of agoraphobia; ADIS-A = ADIS-IV ratings of DSM-IV panic disorder/agoraphobia criterion A (recurrent panic attacks); ADIS-B = ADIS-IV ratings of DSM-IV panic disorder/agoraphobia criterion B (worry/change in behavior); λ = factor loading; τ = indicator intercept. All loadings are significant at p < .001. Model fit as shown below is for the final longitudinal invariance models.
Model fit: χ2(21) = 25.24, p = .24; CFI = 1.00; TLI = 1.00; RMSEA = 0.02; SRMR = .02.
Model fit: χ2(46) = 299.74, p < .001; CFI = .96; TLI = 0.95; RMSEA = 0.09; SRMR = .06.
Model fit: χ2(121) = 208.92, p < .001; CFI = .97; TLI = 0.96; RMSEA = 0.03; SRMR = .05.
Table 2 shows correlations between factors representing Stress, Depression, and PD/A at each study wave. Stress exhibited moderate-to-strong correlations with Depression at each timepoint (range = .56 to .73), whereas these values were considerably smaller for PD/A (range = .19 to .30). Additionally, each disorder construct demonstrated strong stability across assessment points.
Table 2.
Correlations between Latent Variables Representing Stress, Depression, and Panic Severity across Three Study Waves
| Construct | STR1 | STR2 | STR3 | DEP1 | DEP2 | DEP3 | PD/A1 | PD/A2 |
|---|---|---|---|---|---|---|---|---|
| STR1 | — | |||||||
| STR2 | .63 | — | ||||||
| STR3 | .68 | .75 | — | |||||
| DEP1 | .56 | .53 | .53 | — | ||||
| DEP2 | .47 | .67 | .64 | .65 | — | |||
| DEP3 | .47 | .53 | .73 | .62 | .81 | — | ||
| PD/A1 | .19 | .15 | .16 | .16 | .13 | .12 | — | |
| PD/A2 | .17 | .20 | .26 | .13 | .26 | .21 | .81 | — |
| PD/A3 | .16 | .16 | .30 | .13 | .22 | .28 | .74 | .92 |
Note. N = 677. All correlations statistically significant at p < .001. STR = Stress; DEP = Depression; PD/A = Panic. Numbers following each construct label indicate assessment point. 1 = intake; 2 = 12-month follow-up; 3 = 24-month follow-up.
Trait-State-Occasion (TSO) Model of Chronic Stress
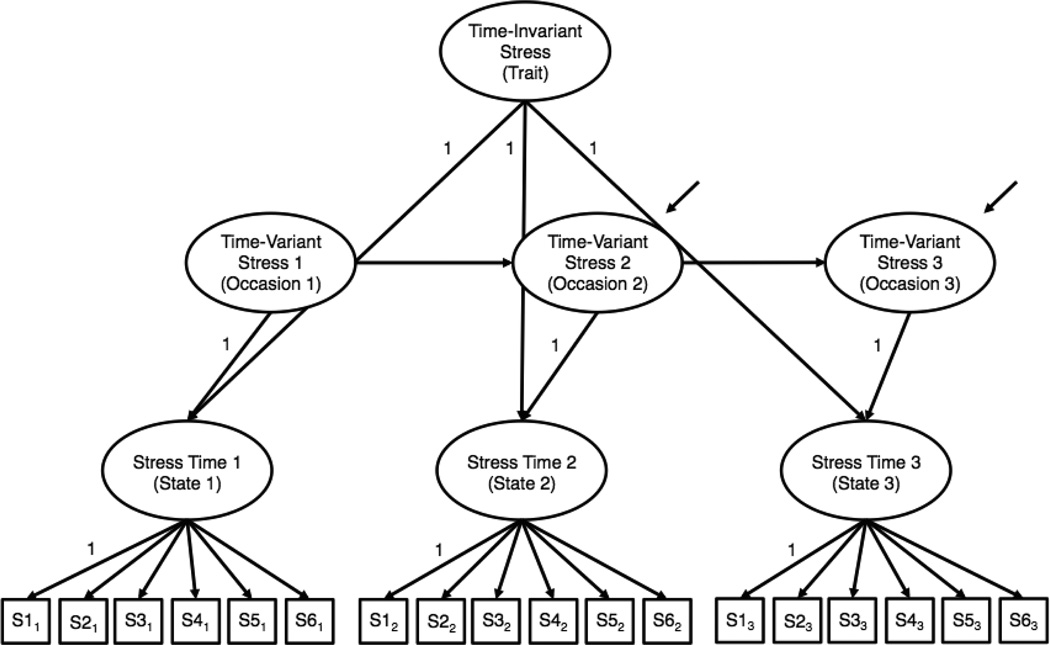
We applied the confirmatory factor analysis model depicted in Figure 1 to partition chronic stress variation into two qualitatively different sources: one time-invariant (i.e., trait) latent variable representing the aspect of stress exposure that is completely stable over time, and three time-varying (i.e., occasion) latent variables representing the aspect of stress exposure that is not perfectly stable over time (Cole et al., 2005). Thus, all latent stress variables were indicators of the fully stable trait factor, and each latent stress variable also loaded on a time-specific occasion factor (with all factor loadings fixed to unity). Additionally, autoregressive associations were specified among the occasion factors, allowing for the possibility that situational circumstances were somewhat persistent across study waves. State factor residual variances were constrained to zero so that stress variance was completely decomposed into the time-invariant and occasion factors.
Figure 1.
Trait-state-occasion model for life stress. S1 = social life, S2 = romantic, S3 = family, S4 = work/school, S5 = financial, S6 = health. For clarity of presentation, indicator residual variances and residual correlations are not shown. Subscripts refer to study wave: 1 = intake; 2 = 12-month follow-up; 3 = 24-month follow-up.
Following the recommendations of Cole et al. (2005), we (a) constrained factor loadings of chronic stress indicators on latent stress variables to equality over time, (b) constrained the residual terms of the latter two occasion factors to equality, (c) held the two (unstandardized) autoregressive parameters to equality, and (d) allowed correlations between the same chronic stress indicators over time to account for shared method variance (e.g., T1 romantic stress residual correlated with T2 romantic stress residual), thus providing a conservative estimate of stability.
Table 3 presents the model fit and parameter estimates for the TSO model. Overall, the model fit the data very well. Factor loadings were all statistically significant and moderate-to-large in magnitude. The unstandardized trait factor variance was 0.14, roughly double that of the average variance of the time-variant factors. This variance represented 61–74% of chronic stress total variance. The total variance changed across waves, accounting for the different estimates for trait variance at separate timepoints (e.g., trait variance represented the highest proportion of total variance at T1 because total variance was smallest at this time point). The trait factor variance and all three occasion factor variances were statistically significantly different from zero (all ps < .01). The stability of occasion factors was moderate and not statistically significant (b = 0.35, SE = 0.18, p = .06, Time 1-Time 2 β = .29, Time 2-Time 3 β = .39).
Table 3.
Estimates for a Trait-State-Occasion Model of Chronic Stress
| Chronic Stress Exposure |
|||
|---|---|---|---|
| Measure | Time 1 | Time 2 | Time 3 |
| Total variance (unstandardized) | 0.19*** | 0.21*** | 0.23*** |
| Time-invariant variance (unstandardized) | 0.14*** | 0.14*** | 0.14*** |
| Time-variant variance (unstandardized) | 0.05** | 0.07** | 0.09*** |
| Proportion of variance due to time-invariant component | .74 | .67 | .61 |
| Proportion of variance due to time-variant component | .26 | .33 | .39 |
| Stability coefficient (unstandardized/standardized) | — | .35/.29 | .35/.39 |
Note. N = 677. Time 1 = intake; Time 2 = 12-month follow-up; Time 3 = 24-month follow-up. Model fit: χ2(135) = 233.04, p < .001; CFI = .96; TLI = 0.96; RMSEA = 0.03; SRMR = .06.
p < .01;
p < .001.
Latent Growth Models (LGMs) of Depression and PD/A
We next tested unconditional LGMs for the disorder constructs over time to determine the trajectory of symptom change through the study period. The factor indicators and residual covariances were as described for the longitudinal measurement models in Table 1. Further, partial measurement invariance was allowed for Depression and PD/A as previously noted. In the LGMs, factor intercepts were set at zero, and factor residual variances were constrained to equality across waves. Based on prior studies using this same longitudinal design (in independent samples) showing that the large majority of symptom change occurs over the first follow up interval (e.g., Brown & Rosellini, 2011), loadings were specified as T1 = 0, T2 = freely estimated, and T3 = 1. Thus, the unstandardized mean of the slope factor reflected average symptom change over the entire study period in the metric of the marker indicators (Bollen & Curran, 2006).
Table 4 shows the results from the unconditional LGMs. Model fit was excellent in both cases. The slope mean estimates for Depression and PD/A, respectively, indicated a sizable reduction of symptoms over time (Cohen’s ds = 0.50 and 0.99, respectively). Additionally, the T2 unstandardized slope factor loadings (.96 and .84 for Depression and PD/A, respectively) demonstrated that the majority of the total change in symptoms occurred during the first follow-up interval (e.g., 96% of the change in depression severity over the course of the study occurred during the first interval). Further, initial levels of disorder severity (i.e., LGM intercepts) were inversely related to the degree of symptom reduction over time (i.e., LGM slopes) for depression (r = −.41, p < .001) and panic (r = −.65, p < .001), signaling that the most symptomatic participants at intake tended to experience the greatest improvement over time. Additionally, for both disorder constructs, the variances of the intercepts and slopes were statistically significant, indicating significant individual differences in initial symptom severity and symptom change over time.
Table 4.
Unstandardized Parameter Estimates from Unconditional Latent Growth Models of Depression and Panic
| Parameter | Depressiona | Panicb |
|---|---|---|
| Intercept variance | 17.50 (1.45) | 74.74 (7.42) |
| Mean slope | −2.82 (0.19) | −4.40 (0.34) |
| Slope variance | 8.89 (1.35) | 30.21 (3.90) |
| Slope-intercept r | −.41 (.05) | −.65 (.04) |
Note. N = 677. Standard errors appear in parentheses. All parameter estimates are significant at p < .001.
Model fit: χ2(23) = 40.25, p = .01; CFI = .99; TLI = 0.99; RMSEA = 0.03; SRMR = .03.
Model fit: χ2(47) = 266.58, p < .001; CFI = .97; TLI = 0.95; RMSEA = 0.08; SRMR = .06.
Longitudinal Stress-Disorder Associations
In our main analysis, we integrated the stress TSO and disorder LGMs to predict the trajectory of symptom change from the traitlike stress process. Specifically, we regressed the disorder slope factors on the time-invariant stress factor while holding baseline levels of disorder constant. In these models, the time-invariant stress factor was free to covary with the disorder intercepts, and time-variant stress factors could covary with corresponding disorder factors at a given time point (e.g., T1 time-invariant Stress with T1 Depression). For model identification and parsimony reasons, these latter covariances between concurrent Stress and disorder factors were constrained to equality across waves.
Model testing proceeded in two stages. First, we examined the effect of stress on the course of each disorder construct independently. Second, we examined the effect of stress on both outcomes in the same model to adjust for the overlap between the Depression and PD/A factors. In this second model, we freely estimated covariances between the disorder factors at the same wave (e.g., T1 Depression with T1 PD/A).
The initial model integrating stress TSO and depression LGM fit the data well, χ2(314) = 506.98, p < .001; CFI =.97; TLI = 0.97; RMSEA = 0.03; SRMR =.05. The correlation of the depression intercept and stress trait factor was large and statistically significant (r = .69, p < .001). Holding T1 depression constant, the stable stress factor had a moderate and statistically significant effect on change in depression over time (γ = 2.95, SE = 0.80, p < .001, standardized path = .43, f2 = .16). The direction of this effect indicated that higher levels of stable stress were associated with smaller reductions in depressive symptoms over time. Model fit for the conditional panic LGM also was good, χ2(391) = 842.64, p < .001; CFI = .95; TLI = 0.95; RMSEA = 0.04; SRMR = .07. Baseline PD/A was positively related to the stable stress factor (r = .20, p < .001). Holding T1 PD/A constant, the traitlike stress factor predicted a more refractory course (i.e., smaller reductions) of PD/A over the study period (γ = 1.39, SE = 0.72, p = .05, standardized path = .10, f2 = .02).
In the final model, which included LGMs of depression and panic simultaneously, the depression and PD/A intercepts were minimally correlated (r = .18, p < .001), and the depression and PD/A slopes exhibited a more moderate correlation (r = .39, p < .001). Holding the shared variance in the T1 disorder constructs constant, time-invariant stress continued to predict change in depression over time (γ = 3.04, SE = 0.74, p < .001, standardized path = .44, f2 = .17). However, in the final model, time-invariant stress was not associated with the rate of improvement in PD/A symptoms (γ = 0.84, SE = 0.66, p = .20, standardized path = .06, f2 = .00).3
Gender and Treatment Group Differences in Stress Stability
Prior to examining gender and treatment group differences in the degree of stress stability, invariance of factor loadings across groups on the life stress latent variable was evaluated. Omnibus chi-square difference tests indicated that factor loadings were fully invariant across treated versus untreated participants, χ2diff(15) = 23.43, p = .08, but not men versus women, χ2diff(15) = 32.72, p < .01. Follow-up tests indicated that only the finance and health indicator loadings were noninvariant across gender (i.e., partial measurement variance was evident); thus, all life stress factor loadings were freely estimated in both groups in the subsequent multiple-group analyses. We evaluated differences in trait variance across both treatment and gender groupings. Specifically, we used Wald tests of the equality of variance ratios (i.e., trait stress variance / total stress variance) to examine differential stability. For both gender, χ2(1) = 0.11, p = .74, and treatment status, χ2(1) = 0.25, p = .61, these tests indicated that the proportion of trait (i.e., stable) to total variance did not differ across groups. These proportions were 0.70 for women versus 0.76 for men, and 0.67 for untreated participants versus 0.77 for treated participants.
In addition to examining group differences in the proportion of trait stress variance, we conducted secondary analyses to examine gender and treatment status as moderators of stress-symptom associations. Chi-square difference tests revealed no statistically significant degradations in model fit as a result of constraining the paths from stress factors to slope factors to equality between gender or treatment status groups for either the depression or PD/A outcomes, both χ2diff(1) < 2, ps > .20.
Discussion
Our primary aims were to (a) determine the stability of adverse environmental conditions, (b) evaluate the impact of unremitting environmental stressors on the temporal course of emotional disorders, and (c) examine differences in the stability of life stress across gender and treatment status. We administered annual interviews and questionnaires to assess the presence of stressful conditions and the severity of depression and panic disorder over three time points in a large clinical sample. TSO modeling of the longitudinal structure of life stress revealed that the large majority of stress variability was time-invariant. Further, elevated chronic stress exposure predicted the trajectory of depression and, to a lesser extent, panic disorder symptoms across time. Chronic stress stability and pathogenicity was roughly equivalent across social versus non-social stress domains.
The majority of variance in life stress was stable across the two-year follow-up period. This observation aligns with prior sociological and clinical research documenting continuity in stressful environments across both brief and extended intervals (Hammen, Hazel, Brennan, & Najman, 2012; Hazel & Hankin, 2014; Pearlin, Schieman, Fazio, & Meersman, 2005). We went beyond previous work in using TSO to directly quantify the amount of stable life stress present at any given moment; that figure ranged from 61% to 74% over the three study waves (these percentages vary because, while the amount of stable trait variance is constant over time, the amount of total stress variance differed across waves).
Another important contribution of the present study was the examination of the effect of chronic stress on the temporal course of two selected emotional disorders. Our analysis revealed that the trajectory of depressive symptoms varied as a function of chronic stress exposure. Specifically, higher chronic stress levels during follow-up were associated with minimal improvement in depressive symptoms. Prior clinical studies have provided mixed evidence regarding whether stressful conditions limit depressive symptom improvement in naturalistic and treatment contexts (Brown & Rosellini, 2011; Mazure, Bruce, Maciejewski, & Jacobs, 2000; Monroe, Kupfer, & Frank, 1992). Taken together, these findings suggest that accounting for the continuity of stress exposure, as opposed to “taking a snapshot” of stressful environments at any given time, may have a stronger prognostic value for depression.
The association between chronic stress levels and the temporal course of panic disorder symptoms was more tenuous. In an initial model that did not consider covariation between depressive and panic symptoms, chronic stress was strongly related to initial levels of panic disorder severity, but had only a marginally statistically significant effect on the course of panic disorder symptoms. This effect size was about 25% as large as that relating chronic stress to depression. In a model including both disorder constructs, the relation between chronic stress and the rate of change in panic disorder symptoms was smaller (i.e., standardized path = .06, compared to .10 in the initial model) and did not approach statistical significance. These results are consistent with notion that life stress is more germane to the onset of panic disorder than its maintenance (e.g., Faravelli & Pallanti, 1989). It is possible that a limited variety of life stressors—particularly those that relate to conditioned stimuli that signal risk for panic attacks (see Bouton, Mineka, & Barlow, 2001)—influence the progression of panic disorder, whereas diverse negative events can worsen the course of depression. While the reasons behind these differential associations await future study, the present data suggest that chronic life stress is not uniformly relevant to change in emotional disorder symptoms over time.
Clinical Implications
Approximately 75% of the sample participated in cognitive-behavioral therapy following the intake assessment wave. Thus, to a large degree, the LGM results reflect the course of emotional disorder symptoms in the context of treatment. Both depression and panic disorder evidenced substantial improvement over the study period (Cohen’s ds of approximately 0.50 and 1.00, respectively). Additionally, the TSO results shed light on the degree to which pathogenic environments remain stable—or are resolved—over the course of psychotherapy. In our study, nearly 75% of the environmental stress variance at T1 was stable across the entire study timeframe, regardless of whether the participant entered psychological treatment.
This observation is unsurprising insofar as most treatments address dysfunctional intrapsychic processes, such as distorted beliefs, emotion regulation deficits, or problematic attachment styles. Clearly, cognitive-behavioral treatments are generally effective (Tolin, 2010), and indeed, as mentioned above, there was marked symptom improvement in this sample. However, as reflected in the between-person variability in the present LGM slope estimates for depression and panic disorder, there is considerable heterogeneity in the naturalistic course and treatment response of emotional disorders (e.g., Arch & Craske, 2009). One possible source of this heterogeneity is individual differences in the extent to which environmental stressors are resolved as treatment progresses (cf. McMain et al., 2012; Zanarini et al., 2010). Life stress is known to operate as a maintenance factor for emotional disorders—especially depression—and the presence of continuing stress may trigger relapse after symptom improvement or simply impede symptom change (Hammen, 2005). Indeed, in the present study, chronic stress was inversely associated with the degree of depressive symptom reduction.
With these considerations in mind, we contend that it could be useful to conduct a thorough assessment of environmental conditions prior to depression treatment. It may be useful in other settings as well, given that stress had similar effects on the course of depression whether participants attended psychotherapy or not in this study (i.e., the effect of stress on depression was not moderated by treatment status), but here we focus on intervention in the context of psychological treatment. The stress assessment could inform decisions about optimal treatment intensity and duration, and also about whether some sort of treatment supplement may be indicated to directly address pathogenic environmental stressors. For instance, if the presenting problem involves depressed mood, anhedonia, and fatigue in the context of serious occupational stressors, then the lion’s share of intervention might aim to alleviate mood disturbance and promote behavioral activation, while a supplemental treatment module—one or several sessions in duration—might directly address occupational circumstances (e.g., effectively searching for jobs; proper conflict resolution with bosses and coworkers). Thus, treatment would target both the “diathesis” and “stress” components of diathesis-stress models of depression (e.g., Monroe & Simons, 1991). The additional assessment and treatment may not be efficient for other forms of disorder, given, for instance, the comparatively small effect of chronic stress on the trajectory of panic disorder severity in this sample.
Limitations
Several limitations to the present study are noteworthy. First, all participants were experiencing one or more emotional disorders at study outset, and we therefore did not evaluate the impact of ongoing strains on new cases of psychopathology. It is important to keep in mind that the effects documented here of stress on the trajectory of emotional disorders may not translate to the prediction of new onsets. Second, although we know the large majority of the sample underwent cognitive-behavioral therapy, we did not record the type (or length) of treatment. Some proportion underwent a transdiagnostic treatment for anxiety and depression developed by Barlow and colleagues (e.g., Ellard, Fairholme, Boisseau, Farchione, & Barlow, 2010). We do not know whether the principal diagnosis affected eligibility for this particular treatment, or indeed whether it guided any other treatment selection decisions. Future research is needed to determine whether different forms of intervention (e.g., interpersonal psychotherapy for depression versus exposure therapy for panic disorder) have varying effects not only on symptom improvement but also on the stability of adverse environmental conditions. Third, it is possible that some of the covariation between life stress and emotional disorder symptoms was attributable to mood-state distortion at the time of stress assessment (Brown, 2007). However, the LSI was designed specifically to collect information about the life stressors that is independent of subjective reactions to those stressors (Hammen et al., 1987). Of equal importance, we held constant initial levels of disorder symptoms when evaluating the influence of chronic stress on the course of depression and panic disorder over time. Fourth, the three assessment waves in the present study are the minimum required for TSO modeling, and number of timepoints is inversely associated with risk of improper solutions (e.g., Cole et al., 2005). Future studies involving more waves can better support TSO and provide a more detailed evaluation of the shape of growth trajectories.
It could be argued that a formative measurement model is appropriate for life stress, as opposed to the reflective model specified here (see Bollen & Lennox, 1991). A formative model of stress assumes that indicators cause individual differences on a latent “stress exposure” trait rather than vice versa (i.e., in path diagram terms, directional arrows from the indicators to the latent variables). A formative model is appropriate for fateful, or independent, life events (e.g., death of a loved one, crime victimization) that are not expected to reflect a personal trait because they are not evoked or influenced by the individual. On the other hand, many adverse circumstances are due, in large part, to a predisposition to elicit stressful experiences. For instance, regular conflict with one’s friend group, frequent romantic relationship breakups, ongoing arguments with family, and poor exercise and diet all depend on the individual. In contrast to, say, a death in the family, these ongoing strains either are largely initiated or maintained by one’s personality and behavior. The direction of causality, relative to the formative model, is reversed: changes in the latent construct—it could be labeled stress proneness—are expected to produce changes in the indicators. Thus, these categories of life stress are hypothesized to act as reflective indicators. We judged that the LSI chronic stress ratings were shaped predominantly by dependent stressors (see Methods for description of the LSI rating scheme). This conclusion is consistent with Hammen’s view of the chronic stress domains as analogous to functional impairment indices (e.g., Hammen, 2006). Therefore, we conceptualized the latent construct in the present study as stress proneness, as compared to stress exposure, and we contend that it is compatible with a reflective model. The moderate intercorrelations among chronic stress indicators—not expected under a formative model—in the present study were consistent with this perspective.
Finally, the trait of stress proneness was inferred, but not directly measured, by the TSO modeling of stressful life events. Thus, it could be questioned whether the trait factor in the TSO models was a pure and veridical representative of the stress proneness construct. For instance, it is possible that, to some extent, our indicators of life stress (e.g., romantic, health, financial stress) possessed variance due to fateful (i.e., uncontrollable) conditions that do not reflect stress proneness. Although our study provided an important initial step in the measurement and evaluation of stress proneness, this line of research could be extended by methodologies that incorporate more direct measures of this construct. For example, future studies of stress proneness should include a wider array of measures such as assessments of problematic interpersonal styles (e.g., romantic strain, friendship conflict), maladaptive health behaviors (e.g., risky sex, overeating), and a tendency to provoke daily hassles. These measures have the advantage of assessing only stressful events that are directly under a person’s control. If the assessment battery was expanded in this fashion, the convergent validity of the trait factor in the TSO model could be evaluated by associating it with these alternate putative manifestations of the stress proneness trait. Moreover, it would be very informative to conduct TSO modeling using these ostensibly more direct indices of stress proneness to determine whether such models outperform the current study’s TSO methodology (e.g., larger trait variance, stronger predictive validity).
Conclusion
In sum, the majority of variability in life stress observed in this clinical sample was stable over two years, and greater chronic stress exposure forecasted a poorer trajectory of emotional disorder symptoms over follow-up. This is the first study to quantify the stability of major stressors in a TSO framework. We speculate that these especially stable forms of environmental stress operate as maintenance factors for emotional disorders—particularly depression—and suggest that thorough assessment and intervention at the level of the environment may often be indicated. In addition to the directions previously noted (i.e., inclusion of a broader array of stress proneness measures), future research could extend this methodology to other stress-linked conditions (e.g., bipolar disorder) and integrate trait representations of stress proneness into diathesis-stress models of psychopathology (e.g., gene-environment interaction analyses).
General Scientific Summary.
Some life stressors are transient, with acute negative consequences, whereas others endure and take a toll over long periods of time. This study finds that mental health patients’ stressors can be highly stable and that these ongoing strains put them at risk for persistent anxiety and depression.
Acknowledgments
This research was supported by National Institute of Mental Health grant MH039096 awarded to the third author.
Footnotes
Except where otherwise noted, we use the term chronic in this article to refer to describe stressors that are perfectly stable over a given timeframe. In other articles, the term has been used to denote conditions that are more protracted than a discrete stressful life event, but do not necessarily span the entire time period of interest.
The main advantages of TSO, relative to TSE, are that it can be identified with three timepoints instead of four, and, more importantly, it is less susceptible to improper solutions (e.g, out-of-range parameter estimates) (Cole et al., 2005; Kenny & Zautra, 1995).
We repeated these analyses separating social and non-social stress given evidence that social stressors are more pathogenic (e.g., Hammen, 2005). For both types of stress, 67% of life stress variance at baseline was stable across the two years of follow up. The pattern and statistical significance of effects of time-invariant stress on the course of disorder constructs were equivalent for the two subsets of stressors and resembled those of the general stress latent variable. Full results are available from the first author upon request.
References
- Allison PD. Missing data techniques for structural equation modeling. Journal of Abnormal Psychology. 2003;112:545–557. doi: 10.1037/0021-843X.112.4.545. [DOI] [PubMed] [Google Scholar]
- Antony MM, Bieling PJ, Cox BJ, Enns MW, Swinson RP. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychological Assessment. 1998;10:176–181. [Google Scholar]
- Arch JJ, Craske MG. First-line treatment: A critical appraisal of cognitive behavioral therapy developments and alternatives. Psychiatric Clinics of North America. 2009;32:525–547. doi: 10.1016/j.psc.2009.05.001. [DOI] [PubMed] [Google Scholar]
- Bollen KA, Curran PJ. Latent curve models: A structural equation perspective. Hoboken, NJ: Wiley; 2006. [Google Scholar]
- Bollen K, Lennox R. Conventional wisdom on measurement: A structural equation perspective. Psychological Bulletin. 1991;110:305–314. [Google Scholar]
- Bouton ME, Mineka S, Barlow DH. A modern learning theory perspective on the etiology of panic disorder. Psychological Review. 2001;108:4–32. doi: 10.1037/0033-295x.108.1.4. [DOI] [PubMed] [Google Scholar]
- Brown GW, Harris T. Social origins of depression: A reply. Psychological Medicine. 1978;8:577–588. doi: 10.1017/s0033291700018791. [DOI] [PubMed] [Google Scholar]
- Brown TA. Temporal course and structural relationships among dimensions of temperament and DSM-IV anxiety and mood disorder constructs. Journal of Abnormal Psychology. 2007;116:313–328. doi: 10.1037/0021-843X.116.2.313. [DOI] [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, Barlow DH. Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology. 1998;107:179–192. doi: 10.1037//0021-843x.107.2.179. [DOI] [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, Korotitsch W, Barlow DH. Psychometric properties of the Depression Anxiety Stress Scales (DASS) in clinical samples. Behaviour Research and Therapy. 1997;35:79–89. doi: 10.1016/s0005-7967(96)00068-x. [DOI] [PubMed] [Google Scholar]
- Brown TA, Di Nardo PA, Lehman CL, Campbell LA. Reliability of DSM-IV anxiety and mood disorders: Implications for the classification of emotional disorders. Journal of Abnormal Psychology. 2001;110:49–58. doi: 10.1037//0021-843x.110.1.49. [DOI] [PubMed] [Google Scholar]
- Brown TA, Rosellini AJ. The direct and interactive effects of neuroticism and life stress on the severity and longitudinal course of depressive symptoms. Journal of Abnormal Psychology. 2011;120:844–856. doi: 10.1037/a0023035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrne BM, Shavelson RJ, Muthén B. Testing for the equivalence of factor covariance and mean structures: The issue of partial measurement invariance. Psychological Bulletin. 1989;105:456–466. [Google Scholar]
- Cole DA. Coping with longitudinal data in research on developmental psychopathology. International Journal of Behavioral Development. 2006;30:20–25. [Google Scholar]
- Cole DA, Jacquez FM, Truss AE, Pineda AQ, Weitlauf AS, Tilghman-Osborne CE, Maxwell MA. Gender differences in the longitudinal structure of cognitive diatheses for depression in children and adolescents. Journal of Clinical Psychology. 2009;65:1312–1326. doi: 10.1002/jclp.20631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole DA, Martin NC, Steiger JH. Empirical and Conceptual Problems With Longitudinal Trait-State Models: Introducing a Trait-State-Occasion Model. Psychological Methods. 2005;10:3–20. doi: 10.1037/1082-989X.10.1.3. [DOI] [PubMed] [Google Scholar]
- Cole DA, Nolen-Hoeksema S, Girgus J, Paul G. Stress exposure and stress generation in child and adolescent depression: A latent trait-state-error approach to longitudinal analyses. Journal of Abnormal Psychology. 2006;115:40–51. doi: 10.1037/0021-843X.115.1.40. [DOI] [PubMed] [Google Scholar]
- Faravelli C, Pallanti S. Recent life events and panic disorder. American Journal of Psychiatry. 1989;146:622–626. doi: 10.1176/ajp.146.5.622. [DOI] [PubMed] [Google Scholar]
- Hammen C. Generation of stress in the course of unipolar depression. Journal of Abnormal Psychology. 1991;100:555–561. doi: 10.1037//0021-843x.100.4.555. [DOI] [PubMed] [Google Scholar]
- Hammen C. Stress and depression. Annual Review of Clinical Psychology. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- Hammen C, Hazel NA, Brennan PA, Najman J. Intergenerational transmission and continuity of stress and depression: Depressed women and their offspring in 20 years of follow-up. Psychological Medicine. 2012;42:931–942. doi: 10.1017/S0033291711001978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazel NA, Hammen C, Brennan PA, Najman J. Early childhood adversity and adolescent depression: The mediating role of continued stress. Psychological Medicine. 2008;38:581–589. doi: 10.1017/S0033291708002857. [DOI] [PubMed] [Google Scholar]
- Hazel NA, Hankin BL. A trait-state-error model of adult hassles over two years: Magnitude, sources, and predictors of stress continuity. Journal of Social and Clinical Psychology. 2014;33:103–123. doi: 10.1521/jscp.2014.33.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Kendler KS, Gardner CO. Sex differences in the pathways to major depression: A study of opposite-sex twin pairs. American Journal of Psychiatry. 2014;171:426–435. doi: 10.1176/appi.ajp.2013.13101375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ. A longitudinal twin study of personality and major depression in women. Archives of General Psychiatry. 1993;50:853–862. doi: 10.1001/archpsyc.1993.01820230023002. [DOI] [PubMed] [Google Scholar]
- Kenny DA, Zautra A. The trait-state-error model for multiwave data. Journal of Consulting and Clinical Psychology. 1995;63:52–59. doi: 10.1037//0022-006x.63.1.52. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Wang PS. The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS-R) JAMA: Journal of the American Medical Association. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Last CG, Barlow DH, O’Brien GT. Precipitants of agoraphobia: role of stressful life events. Psychological Reports. 1984;54:567–570. doi: 10.2466/pr0.1984.54.2.567. [DOI] [PubMed] [Google Scholar]
- Liu RT, Alloy LB. Stress generation in depression: A systematic review of the empirical literature and recommendations for future study. Clinical Psychology Review. 2010;30:582–593. doi: 10.1016/j.cpr.2010.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond PF, Lovibond SH. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy. 1995;33:335–343. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- Mazure CM. Life stressors as risk factors in depression. Clinical Psychology: Science and Practice. 1998;5:291–313. [Google Scholar]
- Mazure CM, Bruce ML, Maciejewski PK, Jacobs SC. Adverse life events and cognitive-personality characterstics in the prediction of major depression and antidepressant response. American Journal of Psychiatry. 2000;157:896–903. doi: 10.1176/appi.ajp.157.6.896. [DOI] [PubMed] [Google Scholar]
- McMain SF, Guimond T, Streiner DL, Cardish RJ, Links PS. Dialectical behavior therapy compared with general psychiatric management for borderline personality disorder: Clinical outcomes and functioning over a 2-year follow-up. American Journal of Psychiatry. 2012;169:650–661. doi: 10.1176/appi.ajp.2012.11091416. [DOI] [PubMed] [Google Scholar]
- Monroe SM, Kupfer DJ, Frank EF. Life stress and treatment course of recurrent depression: I. Response during index episode. Journal of Consulting and Clinical Psychology. 1992;60:718–724. doi: 10.1037//0022-006x.60.5.718. [DOI] [PubMed] [Google Scholar]
- Monroe SM, Simons AD. Diathesis-stress theories in the context of life stress research: Implications for the depressive disorders. Psychological Bulletin. 1991;110:406–425. doi: 10.1037/0033-2909.110.3.406. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus version 7. Los Angeles, CA: Muthén & Muthén; 1998–2014. [Google Scholar]
- Naragon-Gainey K, Gallagher MW, Brown TA. Stable “trait” variance of temperament as a predictor of the temporal course of depression and social phobia. Journal of Abnormal Psychology. 2013;122:611–623. doi: 10.1037/a0032997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olatunji BO, Cole DA. The longitudinal structure of general and specific anxiety dimensions in children: Testing a latent trait-state-occasion model. Psychological Assessment. 2009;21:412–424. doi: 10.1037/a0016206. [DOI] [PubMed] [Google Scholar]
- Paykel ES. Life events and affective disorders. Acta Psychiatrica Scandinavica. 2003;108:61–66. doi: 10.1034/j.1600-0447.108.s418.13.x. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Schieman S, Fazio EM, Meersman SC. Stress, Health, and the Life Course: Some Conceptual Perspectives. Journal of Health and Social Behavior. 2005;46:205–219. doi: 10.1177/002214650504600206. [DOI] [PubMed] [Google Scholar]
- Prenoveau JM, Craske MG, Zinbarg RE, Mineka S, Rose RD, Griffith JW. Are anxiety and depression just as stable as personality during late adolescence? Results from a three-year longitudinal latent variable study. Journal of Abnormal Psychology. 2011;120:832–843. doi: 10.1037/a0023939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter M, Sandberg S. Psychosocial stressors: Concepts, causes and effects. European Child and Adolescent Psychiatry. 1992;1:3–13. doi: 10.1007/BF02084429. [DOI] [PubMed] [Google Scholar]
- Tolin DF. Is cognitive-behavioral therapy more effective than other therapies? A meta-analytic review. Clinical Psychology Review. 2010;30:710–720. doi: 10.1016/j.cpr.2010.05.003. [DOI] [PubMed] [Google Scholar]
- Turner HA, Butler MJ. Direct and indirect effects of childhood adversity on depressive symptoms in young adults. Journal of Youth and Adolescence. 2003;32:89–103. [Google Scholar]
- Wade SL, Monroe SM, Michelson LK. Chronic life stress and treatment outcome in agoraphobia with panic attacks. American Journal of Psychiatry. 1993;150:1491–1495. doi: 10.1176/ajp.150.10.1491. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Reich DB, Fitzmaurice G. The 10-year course of psychosocial functioning among patients with borderline personality disorder and Axis II comparison subjects. Acta Psychiatrica Scandinavica. 2010;122:103–109. doi: 10.1111/j.1600-0447.2010.01543.x. [DOI] [PMC free article] [PubMed] [Google Scholar]