Abstract
Purpose
Submucosal invasion depth (SID) in colorectal carcinoma (CRC) is an important factor in estimating risk of lymph node metastasis, but can be difficult to measure, leading to inadequate or over-extensive treatment. Here, we aimed to clarify the practical aspects of measuring SID in T1 CRC.
Methods
We investigated 568 T1 CRCs that were resected surgically at our hospital from April 2001 to December 2013, and relationships between SID and clinicopathological factors, including the means of measurement, lesion morphology, and lymph node metastasis.
Results
Of these 568 lesions, the SID was ≥1000 μm in 508 lesions. SIDs for lesions measured from the surface layer were all ≥1000 μm. Although lesions with SIDs ≥1000 μm were associated with significantly higher levels of unfavorable histologic types and lymphovascular infiltration than shallower lesions, a depth of ≥1000 μm was not a significant risk factor for lymph node metastasis (LNM) (6.7 vs. 9.8 %; P = 0.64), and no lesions for which the sole pathological factor was SID ≥1000 μm had lymph node metastasis. Protruded lesions showed deeper SIDs than other types.
Conclusions
Although we found several problems of measuring SID in this study, we also found, surprisingly, that SID is not a risk factor for lymph node metastasis, and its measurement is not needed to estimate the risk of lymph node metastasis.
Keywords: Risk factor, T1 colorectal carcinoma, Lymph node metastasis, Invasion depth
Introduction
In T1 colorectal cancer (CRC), deep submucosal invasion thought to signify malignant potential and submucosal invasion depth (SID) are considered important predictors of risk of lymph node metastasis (LNM) [1–9]. Haggitt’s classification criteria defined level 2 as a risk of LNM [10–12]. Kudo’s Classification of Degree of Submucosal Invasion defined sm1c, sm2, and sm3 as risk factors for LNM [13, 14]. Although the European Society for Medical Oncology (ESMO) guidelines recommend surgical resection after endoscopic resection if deeper infiltration into the submucosa is found [15], deeper infiltration into the submucosa is not well defined in these guidelines. Kitajima et al. established the method for measuring SID and reported no LNM were found in lesions with SID <1000 μm [5]. Therefore, SID has been thought to be an important factor in estimating LNM risk. The clinical guidelines of the Japanese Society for Cancer of the Colon and Rectum (JSCCR) describe the method of measuring an SID and advise additional surgical colectomy with lymph node dissection after endoscopic treatment for lesions with SID ≥1000 μm [16]. This “1000-μm rule” is also recommended as a criterion for additional colectomy in many previous papers [8, 17, 18] and is used as a gold-standard indicator for endoscopic diagnoses, such as magnifying endoscopy or image-enhanced endoscopy [19–23].
Overuse of surgery has been recently addressed as a major problem in T1 CRCs [24, 25]. As the percentage of T1 CRCs that lead to LNM is estimated as 6.3–17 % [1–7, 26, 27], many patients who undergo additional colectomies do not have LNM and might not need further resection. Moreover, several studies report that among patients with SID ≥1000 μm but no risk factors for LNMs (lymphovascular infiltration, unfavorable histological types, or tumor budding), few develop LNM [5, 27–29]. As endoscopic techniques progress, endoscopic treatment is becoming more widely acceptable for lesions with SID ≥1000 μm [17, 30, 31]. Problems in measuring SID are also reported in some studies, and both measuring methods and lesion morphology could affect measurement results [32, 33]. However, as these published cases and reports are few, we performed this larger-scale study to clarify the practical issues and significance of measuring SID in T1 CRCs.
Methods
Subjects
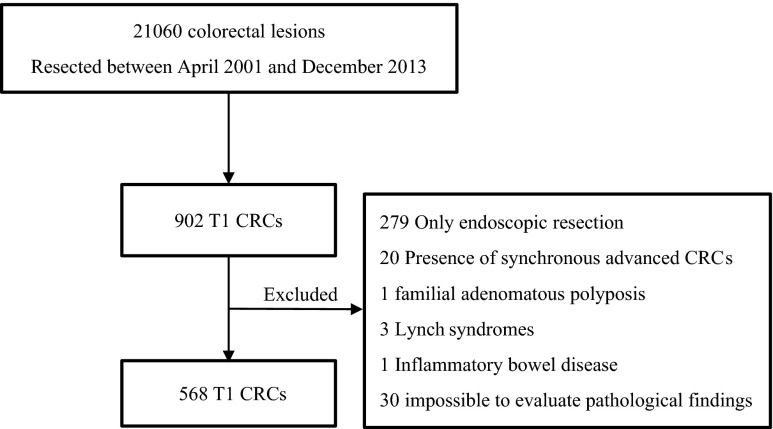
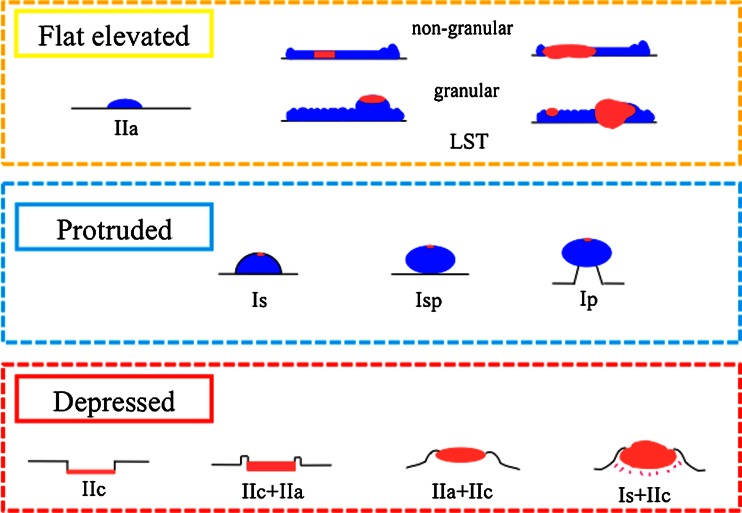
In the present study, we analyzed T1 CRCs that were resected at Showa University Northern Yokohama Hospital in Japan from April 2001 to December 2013. A total of 21,060 colorectal neoplasms, excluding advanced carcinomas, had been resected endoscopically or surgically. Of these, 902 were T1 CRCs. To evaluate precise pathological diagnoses and LNM outcomes, we excluded lesions from 334 patients, including 279 patients who underwent only endoscopic resection, 20 who had synchronous advanced CRCs, one with familial adenomatous polyposis, three with Lynch syndromes, one with inflammatory bowel disease, and 30 whose specimens were impossible to evaluate pathologically in detail because of damage or loss (Fig. 1). In total, 568 patients with T1 CRC were included in this study, of whom 295 underwent surgical resection and lymph node dissection as first-line treatment, and 273 underwent first-line endoscopic resection followed by additional surgery with lymph node dissection. None of the patients received preoperative radiotherapy or neoadjuvant chemotherapy. We found each patient’s age, sex, and tumor location from their hospital records. For the morphological classification, we divided the lesions into three types: flat elevated type (0–IIa or laterally spreading tumor [LST]) [13]; protruded type (0–Is, Isp, or Ip); and depressed type (0–IIc, IIc + IIa, IIa + IIc, Is + IIc, or Ip + IIc); Fig. 2 [34, 35].
Fig. 1.
Patient flow chart. CRC colorectal carcinoma
Fig. 2.
Kudo’s morphological/development classification
Histologic examination
All resected specimens were immediately fixed in 10 % buffered formalin solution, observed with a focus on pit pattern using a stereomicroscope, and dissected at the point where the deepest invasion area could be exposed on the cut end surface. The other histological specimens were subsequently dissected into parallel 2- to 3-mm-thick sections and stained with hematoxylin and eosin (H&E). An experienced pathologist (S.H.) examined all the specimens histologically. Histologic grade was diagnosed based on the World Health Organization Classification of Tumors [36] and the current JSCCR guidelines. Unfavorable histological types were poorly differentiated adenocarcinoma (Por) or mucinous carcinoma (Muc) at any part of the lesion; favorable histological types were well or moderately differentiated adenocarcinoma. Double staining with H&E and Victoria blue (Muto Pure Chemicals Co., Ltd., Tokyo, Japan) was used to diagnose vascular infiltration. Lymphatic infiltration and status of muscularis mucosae were evaluated using H&E staining and immunostaining with D2-40 antibody (Dako North America Inc., Carpinteria, CA, USA) and desmin antibody (Dako North America Inc.), respectively. Tumor budding was defined as a cancer cell nest consisting of 1 or ˂5 cells that had infiltrated the interstitium at the invasive margin of the cancer. After selecting the field where budding was the most intensive, buddings were counted in a 0.785-mm2 field as observed through an objective lens. Depending on the number of buddings, budding grade was scored as Grade 1: 0–4; Grade 2: 5–9; and Grade 3: ≥10 [8, 16, 37]. Grades 2–3 were defined as tumor budding positive.
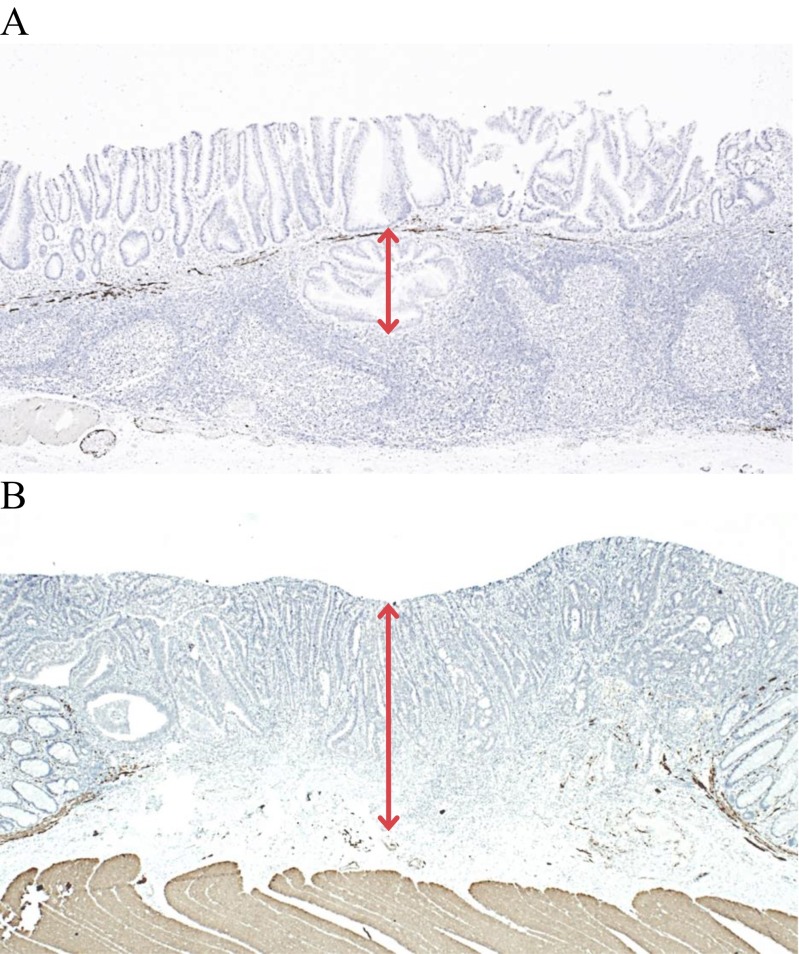
We measured SID according to the clinical guidelines of the JSCCR [5, 16]. SID can be measured in two ways (Fig. 3). When it was possible to identify or estimate the location of the muscularis mucosae, we measured the SID directly from the line of the muscularis mucosae (method A; Fig. 3a). When the line of the muscularis mucosae was not easily identified because of carcinoma invasion, we measured the SID from the surface layer of the lesion (method B; Fig. 3b).
Fig. 3.
Method used to measure submucosal invasion depth. a When identifying or estimating location of the muscularis mucosae, the submucosal invasion depth is measured directly from the line of the muscularis mucosae. b When the muscularis mucosae have not been identified, the submucosal invasion depth is measured from the lesion’s surface layer
The lesions were divided into two groups: those with SID <1000 μm and those with SID ≥1000 μm. Between the two groups, we compared incidences of clinicopathological factors: age, sex, tumor location, tumor morphology, tumor size, method of measurement, mean SID, histologic type, lymphatic infiltration, vascular infiltration, tumor budding, and LNM. Mean SID and the LNM rates were calculated for each morphological type. We also assessed correlations between histologic type, lymphatic infiltration, vascular infiltration, tumor budding, and LNM, and SID by depth (0–999 μm, 1000–1999 μm, 2000–2999 μm, 3000–3999 μm, 4000–4999 μm, 5000–5999 μm, 6000–6999 μm, 7000–7999 μm, and ≧8000 μm,). Finally, in lesions with SID ≥1000 μm, we examined correlations between LNM and histologic type, lymphatic infiltration, vascular infiltration, and tumor budding.
Statistical analysis
Data are presented as the mean ± standard deviation. Differences were analyzed using the χ2 test, Fisher’s exact test, Student’s t test, or Ryan multiple comparison as necessary. Statistical significance was defined as a P < 0.05. All statistical analyses were performed using R version 2.10.0. (http://www.r-project.org).
The ethics committee of our hospital approved the study protocol (approval number; 1408–01). Informed consent was obtained from all patients before endoscopy or surgery. This study was registered in the University Hospital Medical Network Clinical Trials Registry (UMIN R000017608). A summary of this study was presented at the United European Gastroenterology Week, Vienna, Austria on October 21, 2014 (oral presentation).
Results
Clinicopathological characteristics
Initial or additional surgery with nodal dissection was performed for the 568 patients, who included 352 (62.0 %) men and 216 (38.0 %) women with a mean age of 65.0 ± 11.3 years (range 31–93 years). Mean tumor size was 20.6 ± 11.4 mm (range 4–100 mm). Tumors included 151 flat elevated type, 250 protruded type and 167 depressed type lesions, with 401 lesions located in colon and 167 in rectum, and 54 (9.4 %) lesions associated with LNM. Unfavorable histologic types were seen in 106 (18.7 %) lesions, lymphatic infiltration was positive in 237 (41.7 %) lesions, vascular infiltration was positive in 189 (33.5 %) lesions, and tumor budding was positive in 158 (27.8 %) lesions.
We found 60 lesions (10.6 %) with SID <1000 μm and 508 (89.4 %) with SID ≥1000 μm. SID was measured from the muscularis mucosa in 168 (32.2 %) lesions (method A) and from the surface in 385 (67.8 %) lesions (method B). Among the lesions measured using method A, 60 had SIDs <1000 μm and 123 had SIDs ≥1000 μm. All lesions measured using method B invaded deeper than 1000 μm.
SID and clinicopathological factors
The SID <1000 μm group had a lower rate of rectal T1 carcinomas than did the SID ≥1000 μm group (15.0 vs. 31.1 %; P = 0.010), depressed type lesions (13.3 vs. 31.3 %; P = 0.004), unfavorable histological types (8.3 vs. 19.9 %; P = 0.034), lymphatic infiltration (28.3 vs. 43.3 %; P = 0.027), and vascular infiltration (10.0 vs. 36.0 %; P < 0.001; Table 1). The two groups did not significantly differ by age, sex, or tumor size. The two groups also did not significantly differ by rate of LNM (6.7 vs. 9.8 %; P = 0.64) or tumor budding (20.0 vs. 28.7 %; P = 0.17).
Table 1.
Submucosal depth (<1000 or ≥1000 μm) and clinicopathological factors
| <1000 μm (n = 60) | ≥1000 μm (n = 508) | P value | |
|---|---|---|---|
| Age (years), mean (SD) | 65.5 ± 12.6 | 64.9 ± 11.2 | 0.7099 |
| Male sex | 42 (70.0) | 310 (61.0) | 0.2062 |
| Location (rectum) | 9 (15.0) | 158 (31.1) | 0.0103 |
| Morphology (depressed type) | 8 (13.3) | 159 (31.3) | 0.0040 |
| Tumor size (mm), mean (SD) | 19.5 ± 11.9 | 20.7 ± 11.3 | 0.4325 |
| Method of measurement (A) | 60 (100) | 123 (24.2) | <0.001 |
| SID (μm), mean (SD) | 406 ± 302 | 3680 ± 2233 | <0.001 |
| Histologic type (por or muc) | 5 (8.3) | 101 (19.9) | 0.0341 |
| Lymphatic infiltration (+) | 17 (28.3) | 220 (43.3) | 0.0271 |
| Vascular infiltration (+) | 6 (10.0) | 183 (36.0) | <0.001 |
| Budding (+) | 12 (20.0) | 146 (28.7) | 0.1722 |
| Lymph node metastasis (+) | 4 (6.7) | 50 (9.8) | 0.6401 |
Data are expressed as the number of patients (%) unless otherwise indicated
Por or muc poorly differentiated adenocarcinoma or mucinous carcinoma, SD standard deviation, SID submucosal invasion depth, Budding tumor budding
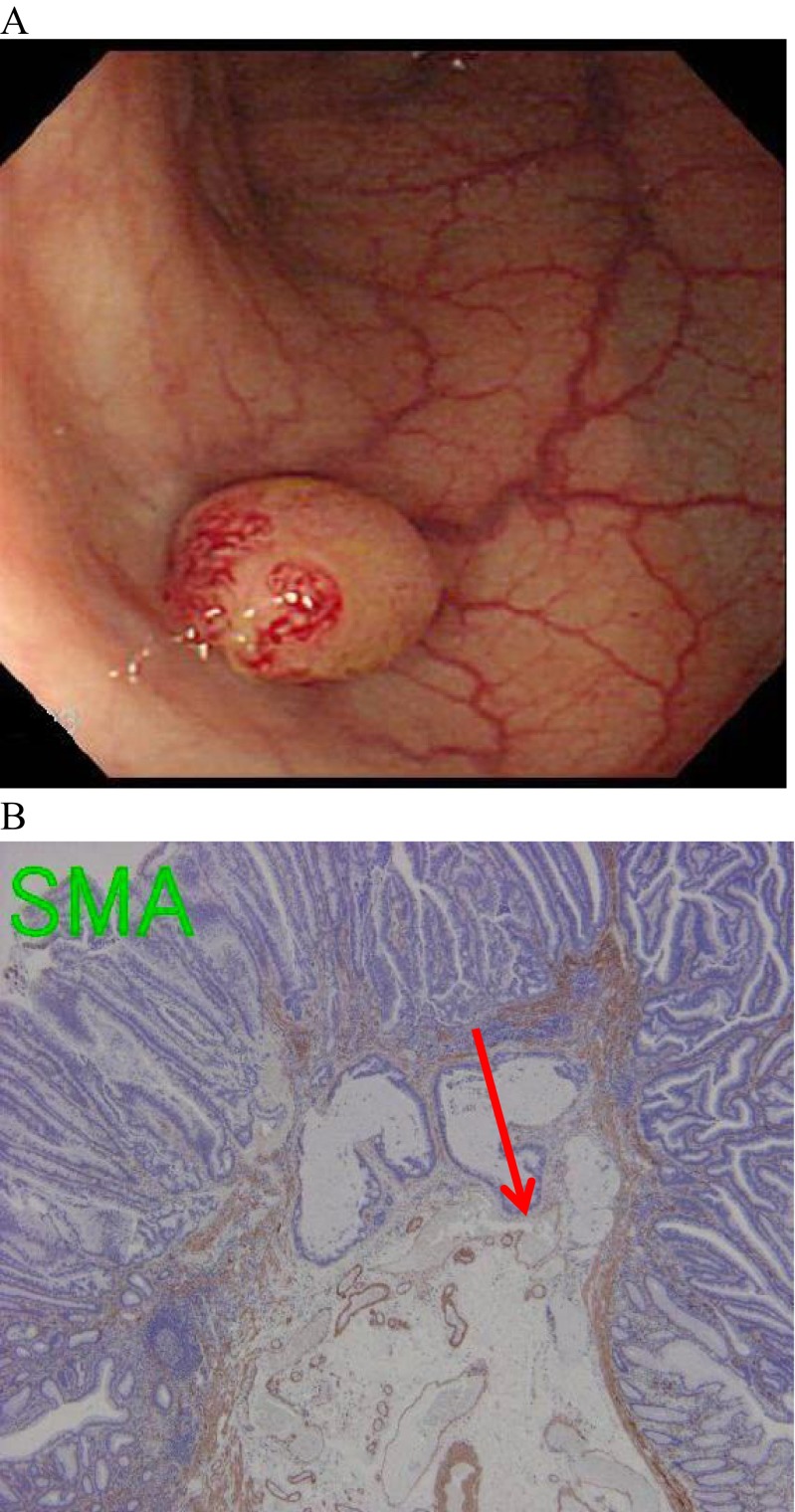
Figure 4 shows a lesion that metastasized to a lymph node even though its SID was <1000 μm. It was found in a 50-year-old male patient as a sessile lesion, 7 mm in diameter, in the sigmoid colon. Its SID was 800 μm, with positive lymphatic infiltration, and negative vascular infiltration and budding. This patient was treated with an additional surgical colectomy.
Fig. 4.
A case of lymph node metastasis with the submucosal invasion depth <1000 μm. a A 7-mm sessile lesion was detected in the sigmoid colon. b The submucosal invasion depth was 800 μm (the arrow)
SID and morphology
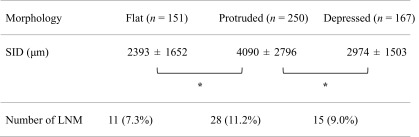
Mean SIDs of flat elevated type lesions, protruded type lesions, and depressed type lesions were 2393 ± 1652 μm, 4089 ± 2796 μm, and 2974 ± 1503 μm, respectively (Table 2). The mean SID of protruded lesions was greater than that of other types (P < 0.01). Rates of LNM for flat elevated (7.3 %), protruded (11.2 %), and depressed (9.0 %) lesions did not significantly differ (P = 0.42).
Table 2.
Mean depth of invasion and incidences of lymph node metastasis by morphology of the lesion
LNM lymph node metastasis, SID submucosal invasion depth
*P < 0.05
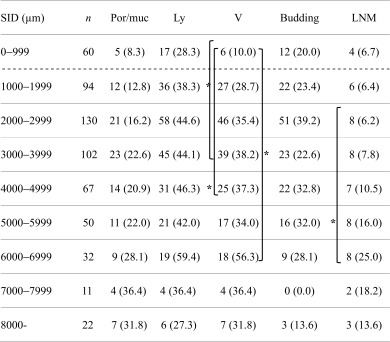
Actual measured SID value and pathological factors
Data on rates of unfavorable histologic type, lymphatic infiltration, vascular infiltration, tumor budding, and LNM according to SID are shown in Table 3. Rates of unfavorable histologic type, lymphatic infiltration, or budding did not significantly differ by SID. The rate of vascular infiltration was significantly less in lesions with a SID 0–999 μm than in lesions with a SID of 3000–3999 (P = 0.0002), 4000–4999 (P = 0.0008), and 6000–6999 μm (P < 0.0001). The rate of LNM was higher in lesions with a SID of 6000–6999 μm than in lesions with a SID of 2000–2999 (P = 0.0011).
Table 3.
Actual measured depth of submucosal invasion and pathological factors SX
Data are expressed as the number of patients (%)
SID submucosal invasion depth, n number of lesions, Por/muc poorly differentiated adenocarcinoma or mucinous carcinoma, Ly lymphatic infiltration, V vascular infiltration, Budding tumor budding, LNM lymph node metastasis
*P < 0.05
Pathological factors and LNM in the SID ≥1000 μm group
Table 4 shows correlations between LNM and histologic type, lymphatic infiltration, vascular infiltration, and tumor budding in the SID ≥1000 μm group. No patients in this group developed LNM except those who had a pathological factor associated with LNM (i.e., other than LNM). Among patients in this group who had LNM-associated pathological factors, the rate of LNM was 14.5 % (50/345).
Table 4.
Correlation between lymph node metastasis and pathological factors in lesions with submucosal depth of ≥1000 μm
| Lymph node metastasis | ||
|---|---|---|
| + | − | |
| Other pathological factorsa | 50 | 295 |
| None | 0 | 163 |
aOther pathological factors include lymphovascular permeation, unfavorable histologic types (poorly differentiated adenocarcinoma, signet-ring cell carcinoma, or mucinous carcinoma), or Grade 2–3 budding at the site of deepest invasion
Discussion
In the present study, we addressed some practical aspects of measuring SID and clarified the significance of SID as a risk factor for LNM.
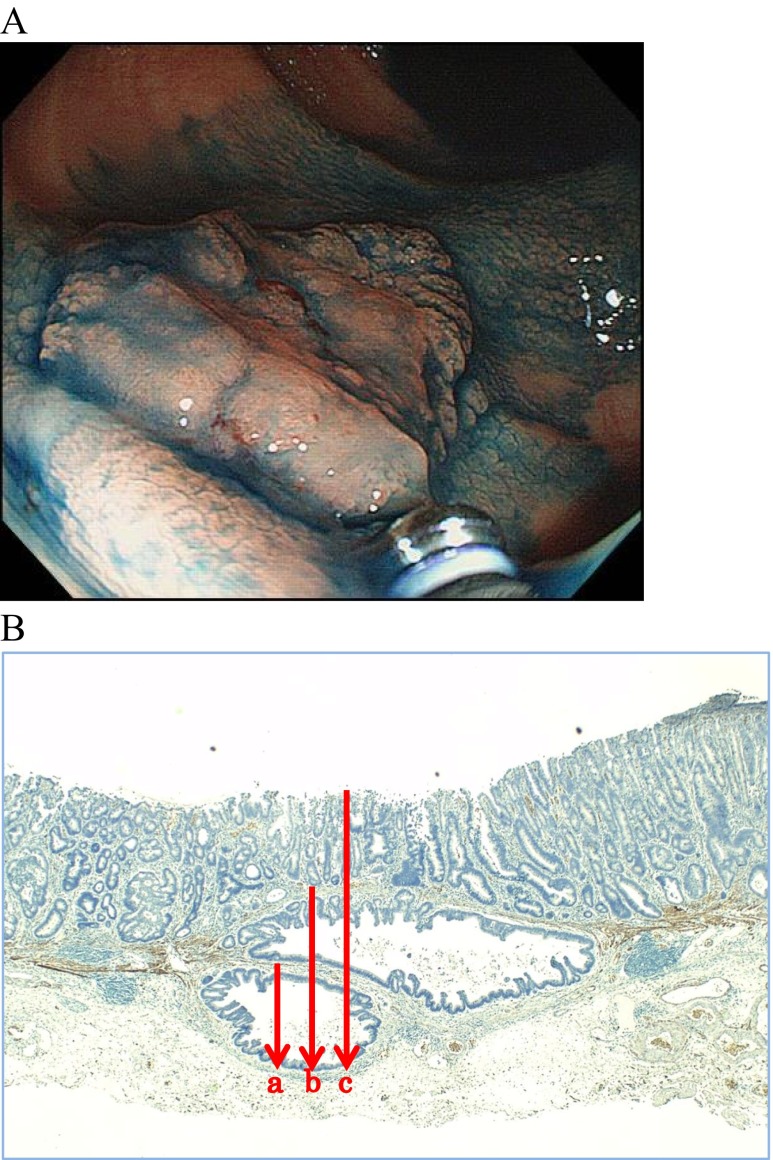
First, the method of measuring SID affects the results. In the present study, when measuring a SID from the surface layer (method B), the depth was always ≥1000 μm. Therefore, if a pathologist found that the muscularis mucosa of the lesion could not be easily identified, the 1000 μm rule implies that a colectomy with lymph node dissection should be considered without measuring the SID. Yoshida et al. also reported that SIDs measured from the surface layer were deeper than 1000 μm for all lesions [33]. Second, determining the baseline is difficult in some lesions. The muscularis mucosae sometimes show separations, and several baselines can be estimated in some cases. Figure 5, for example, shows a 23-mm non-granular LST located in the ascending colon. As the muscularis mucosae had split up, it was unclear which line we should measure from. The SID was 630 μm when measured from the lower line (Fig. 5a), 1325 μm when measured from the upper line (Fig. 5b), and 2150 μm when measured from the surface of the lesion (Fig. 5c). Whether additional surgical resection is necessary depends on which baseline the SID is measured from—in other words, the assessment of the pathologist who diagnoses the lesion [38].
Fig. 5.
A case in which determining the submucosal invasion depth measurement baseline was difficult. a A 23-mm non-granular LST located in the ascending colon. b The pathological finding of desmin antibody staining. The submucosal invasion depth was 630 μm when measured from the lower line (Fig. 5b, a), 1325 μm when measured from the upper line (Fig. 5b, b), and 2150 μm when measured from the surface of the lesion (Fig. 5b, c)
Third, SID is affected by lesion morphology [39]. SIDs are greater for protruded lesions than for the other two types. Reportedly, flat elevated type lesions, especially LSTs, grow laterally, protruded types often grow upward, and depressed type lesions tend to invade downwards [40]. These growing patterns can affect SID measurements. Therefore, setting the cutoff value at 1000 μm should consider morphology.
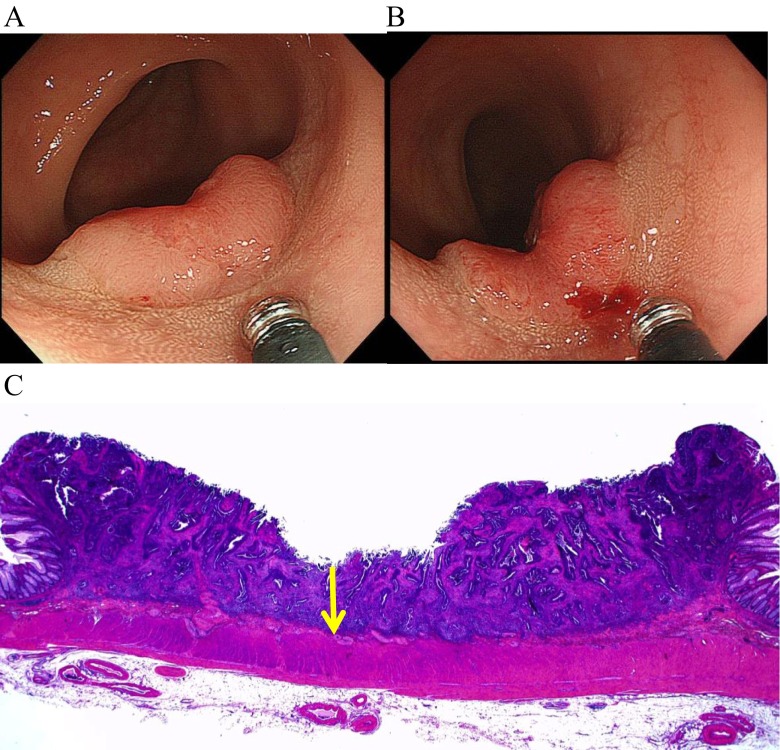
Fourth, some lesions develop depressed areas, and SID can decrease during the lesion’s progression. Generally, lesions with depressions or ulcerations are more advanced or aggressive [41–46]. Figure 6 shows a lesion in which the center area dimpled over a month’s time and the depth could have become shallower (Fig. 6a, b). Although the SID was only 1400 μm in the center of the lesion, the patient had an LNM. Increased SID does not reflect the lesion’s malignancy or progression or likelihood of LNM. Although the 1000-μm rule quantifies SID as a comprehensible value and provides a clear-cut criterion, its measurement can be difficult to perform and interpret.
Fig. 6.
A typical case in which the submucosal invasion depth might become shorter during the carcinoma’s progression. a A 19-mm IIa + IIc lesion was detected in the rectosigmoid. b The observation of the same lesion 1 month later. c The pathological finding with hematoxylin and eosin staining of the lesion. The submucosal invasion depth was 1400 μm in the center of the lesion (the arrow)
SID does provide useful information. The presence of unfavorable histological types or lymphovascular infiltration in lesions with SID <1000 μm was significantly lower than in those with SID ≥1000 μm. Thus, the SID <1000 μm threshold can help estimate the risk of unfavorable histological types or lymphovascular infiltration. However, it is not a significant risk factor for LNM. In the present study, four patients with SID <1000 μm had LNM, two of whom had other LNM-associated factors, such as unfavorable histologic type, lymphovascular infiltration, or tumor budding. This concords with other studies that report patients with SID <1000 μm developing LNM [8, 24, 28, 47, 48]. Several studies have reported deep SID as a risk factor for LNM in patients with T1 CRC [1, 2, 4–9], and others did not evaluate LNM+ cases with SID <1000 μm [5, 7, 9, 26], but most of these studies, except for a meta-analysis, had fewer T1 CRC cases than in the present study, even though our study was a single-center study. In the Western World, the discrimination of the submucosal layer into sm1, sm2 (<1000 μm), and sm3 (≥1000 μm) is established to estimate the potential risk of lymph node metastasis [49, 50]. But there also exists the redundancy in the classification same as the “1000-μm rule.”
Moreover, of the cases with SID ≥1000 μm but no LNM-associated pathological factors—unfavorable histological type, lymphovascular infiltration, or tumor budding—none had LNM. In contrast, among cases with SID ≥1000 μm and any of these pathological factors, the rate of LNM was 14.5 %. If the SID is omitted from the risk factors of LNM, we could reduce the number of additional surgeries that are performed according to the 1000-μm rule. Other studies have also reported extremely low incidence of LNM regardless of SID among lesions with no LNM-associated pathological factors [5, 24, 27–29]. Such lesions might be treated only with endoscopic resections. Currently, other factors such as histological type, lymphovascular infiltration, and tumor budding are considered more important than a SID ≥1000 μm. In this study, we addressed several practical problems in measuring SID; therefore, more detailed prospective investigations of LNM risk factors will be needed besides SID. Hereafter, without causing incomplete endoscopic resections, more accurate criteria to recommend additional surgery should be established.
Our study is limited by being a single-center retrospective study, which could reflect some selection bias. However, the pathological specimens were examined in the same manner [48], and with a larger sample size, than any other single-institutional reports published so far. Second, patients treated only by endoscopic resection were excluded from this analysis, as such endoscopically removed lesions occasionally disguise a metachronous recurrence in consideration of skip lymphovascular invasion or discontinuous foci of tumor cells [51]. Risk factors for metachronous recurrence or prognosis are the subject of future investigations. Finally, all patients examined in this study were Japanese. Some biological differences might be seen between Japan and the Western World. Further multicenter trials in the Eastern and Western World would be necessary before the “1000 μm border“ is excluded for risk stratification.
In conclusion, the present study showed several problems of measuring SID and demonstrated that SID is not an important risk factor for LNM. If the surface layer was used as the baseline, all cases would be ≥1000 μm. SID is associated with lesion morphology, and it can sometimes become shorter in progression of the lesions. Some lesions with SID <1000 μm had LNM, whereas SID ≥1000 μm was not a significant risk factor for LNM. Moreover, among lesions with SID ≥1000 μm but no pathological factors associated with LNM, none had LNM. SID should be reconsidered as a risk factor for LNM, or an indicator for additional surgery. We need to devise more accurate methods to assess lesions at high risk for LNM without measuring SID.
Acknowledgments
The authors thank all members of the Digestive Disease Center and the Department of Pathology, Showa University Northern Yokohama Hospital for their excellent assistance.
Compliance with ethical standards
Financial disclosures
No funding was received for this study.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Beaton C, Twine CP, Williams GL, Radcliffe AG. Systematic review and meta-analysis of histopathological factors influencing the risk of lymph node metastasis in early colorectal cancer. Color Dis Off J Assoc Coloproctol G B Irel. 2013;15(7):788–797. doi: 10.1111/codi.12129. [DOI] [PubMed] [Google Scholar]
- 2.Bosch SL, Teerenstra S, de Wilt JH, Cunningham C, Nagtegaal ID. Predicting lymph node metastasis in pT1 colorectal cancer: a systematic review of risk factors providing rationale for therapy decisions. Endoscopy. 2013;45(10):827–834. doi: 10.1055/s-0033-1344238. [DOI] [PubMed] [Google Scholar]
- 3.Choi PW, Yu CS, Jang SJ, Jung SH, Kim HC, Kim JC. Risk factors for lymph node metastasis in submucosal invasive colorectal cancer. World J Surg. 2008;32(9):2089–2094. doi: 10.1007/s00268-008-9628-3. [DOI] [PubMed] [Google Scholar]
- 4.Egashira Y, Yoshida T, Hirata I, Hamamoto N, Akutagawa H, Takeshita A, Noda N, Kurisu Y, Shibayama Y. Analysis of pathological risk factors for lymph node metastasis of submucosal invasive colon cancer. Mod Pathol Off J US Can Acad Pathol Inc. 2004;17(5):503–511. doi: 10.1038/modpathol.3800030. [DOI] [PubMed] [Google Scholar]
- 5.Kitajima K, Fujimori T, Fujii S, Takeda J, Ohkura Y, Kawamata H, Kumamoto T, Ishiguro S, Kato Y, Shimoda T, Iwashita A, Ajioka Y, Watanabe H, Watanabe T, Muto T, Nagasako K. Correlations between lymph node metastasis and depth of submucosal invasion in submucosal invasive colorectal carcinoma: a Japanese collaborative study. J Gastroenterol. 2004;39(6):534–543. doi: 10.1007/s00535-004-1339-4. [DOI] [PubMed] [Google Scholar]
- 6.Okabe S, Arai T, Maruyama S, Murase N, Tsubaki M, Endo M. A clinicopathological investigation on superficial early invasive carcinomas of the colon and rectum. Surg Today. 1998;26:687–695. doi: 10.1007/BF02484613. [DOI] [PubMed] [Google Scholar]
- 7.Tominaga K, Nakanishi Y, Nimura S, Yoshimura K, Sakai Y, Shimoda T. Predictive histopathologic factors for lymph node metastasis in patients with nonpedunculated submucosal invasive colorectal carcinoma. Dis Colon Rectum. 2005;48(1):92–100. doi: 10.1007/s10350-004-0751-4. [DOI] [PubMed] [Google Scholar]
- 8.Ueno H, Mochizuki H, Hashiguchi Y, Shimazaki H, Aida S, Hase K, Matsukuma S, Kanai T, Kurihara H, Ozawa K, Yoshimura K, Bekku S. Risk factors for an adverse outcome in early invasive colorectal carcinoma. Gastroenterology. 2004;127(2):385–394. doi: 10.1053/j.gastro.2004.04.022. [DOI] [PubMed] [Google Scholar]
- 9.Yasuda K, Inomata M, Shiromizu A, Shiraishi N, Higashi H, Kitano S. Risk factors for occult lymph node metastasis of colorectal cancer invading the submucosa and indications for endoscopic mucosal resection. Dis Colon Rectum. 2007;50(9):1370–1376. doi: 10.1007/s10350-007-0263-0. [DOI] [PubMed] [Google Scholar]
- 10.Haggitt RC, Glotzbach RE, Soffer EE, Wruble LD. Prognostic factors in colorectal carcinomas arising in adenomas: implications for lesions removed by endoscopic polypectomy. Gastroenterology. 1985;89(2):328–336. doi: 10.1016/0016-5085(85)90333-6. [DOI] [PubMed] [Google Scholar]
- 11.Pollard CW, Nivatvongs S, Rojanasakul A, Reiman HM, Dozois RR. The fate of patients following polypectomy alone for polyps containing invasive carcinoma. Dis Colon Rectum. 1992;35(10):933–937. doi: 10.1007/BF02253494. [DOI] [PubMed] [Google Scholar]
- 12.Nivatvongs S, Rojanasakul A, Reiman HM, Dozois RR, Wolff BG, Pemberton JH, Beart RW, Jr, Jacques LF. The risk of lymph node metastasis in colorectal polyps with invasive adenocarcinoma. Dis Colon Rectum. 1991;34(4):323–328. doi: 10.1007/BF02050592. [DOI] [PubMed] [Google Scholar]
- 13.Kudo S. Endoscopic mucosal resection of flat and depressed types of early colorectal cancer. Endoscopy. 1993;25(7):455–461. doi: 10.1055/s-2007-1010367. [DOI] [PubMed] [Google Scholar]
- 14.Kashida H, Kudo SE. Early colorectal cancer: concept, diagnosis, and management. Int J Clin Oncol. 2006;11(1):1–8. doi: 10.1007/s10147-005-0550-5. [DOI] [PubMed] [Google Scholar]
- 15.Schmoll HJ, Van Cutsem E, Stein A, Valentini V, Glimelius B, Haustermans K, Nordlinger B, van de Velde CJ, Balmana J, Regula J, Nagtegaal ID, Beets-Tan RG, Arnold D, Ciardiello F, Hoff P, Kerr D, Kohne CH, Labianca R, Price T, Scheithauer W, Sobrero A, Tabernero J, Aderka D, Barroso S, Bodoky G, Douillard JY, El Ghazaly H, Gallardo J, Garin A, Glynne-Jones R, Jordan K, Meshcheryakov A, Papamichail D, Pfeiffer P, Souglakos I, Turhal S, Cervantes A. ESMO Consensus Guidelines for management of patients with colon and rectal cancer. A personalized approach to clinical decision making. Ann Oncol. 2012;23(10):2479–2516. doi: 10.1093/annonc/mds236. [DOI] [PubMed] [Google Scholar]
- 16.Watanabe T, Itabashi M, Shimada Y, Tanaka S, Ito Y, Ajioka Y, Hamaguchi T, Hyodo I, Igarashi M, Ishida H, Ishiguro M, Kanemitsu Y, Kokudo N, Muro K, Ochiai A, Oguchi M, Ohkura Y, Saito Y, Sakai Y, Ueno H, Yoshino T, Fujimori T, Koinuma N, Morita T, Nishimura G, Sakata Y, Takahashi K, Takiuchi H, Tsuruta O, Yamaguchi T, Yoshida M, Yamaguchi N, Kotake K, Sugihara K, Japanese Society for Cancer of the C, Rectum Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2010 for the treatment of colorectal cancer. Int J Clin Oncol. 2012;17(1):1–29. doi: 10.1007/s10147-011-0315-2. [DOI] [PubMed] [Google Scholar]
- 17.Tanaka S, Asayama N, Shigita K, Hayashi N, Oka S, Chayama K. Towards safer and appropriate application of endoscopic submucosal dissection for T1 colorectal carcinoma as total excisional biopsy: future perspectives. Dig Endosc Off J Japan Gastroenterol Endosc Soc. 2015;27(2):216–222. doi: 10.1111/den.12326. [DOI] [PubMed] [Google Scholar]
- 18.Kawachi H, Eishi Y, Ueno H, Nemoto T, Fujimori T, Iwashita A, Ajioka Y, Ochiai A, Ishiguro S, Shimoda T, Mochizuki H, Kato Y, Watanabe H, Koike M, Sugihara K. A three-tier classification system based on the depth of submucosal invasion and budding/sprouting can improve the treatment strategy for T1 colorectal cancer: a retrospective multicenter study. Mod Pathol Off J US Can Acad Pathol Inc. 2015 doi: 10.1038/modpathol.2015.36. [DOI] [PubMed] [Google Scholar]
- 19.Kanao H, Tanaka S, Oka S, Kaneko I, Yoshida S, Arihiro K, Yoshihara M, Chayama K. Clinical significance of type V(I) pit pattern subclassification in determining the depth of invasion of colorectal neoplasms. World J Gastroenterol. 2008;14(2):211–217. doi: 10.3748/wjg.14.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tobaru T, Mitsuyama K, Tsuruta O, Kawano H, Sata M. Sub-classification of type VI pit patterns in colorectal tumors: relation to the depth of tumor invasion. Int J Oncol. 2008;33(3):503–508. [PubMed] [Google Scholar]
- 21.Sakamoto T, Saito Y, Nakajima T, Matsuda T. Comparison of magnifying chromoendoscopy and narrow-band imaging in estimation of early colorectal cancer invasion depth: a pilot study. Dig Endosc Off J Japan Gastroenterol Endosc Soc. 2011;23(2):118–123. doi: 10.1111/j.1443-1661.2010.01049.x. [DOI] [PubMed] [Google Scholar]
- 22.Sakamoto T, Matsuda T, Nakajima T, Saito Y, Fujii T. Impact of clinical experience on type V pit pattern analysis using magnifying chromoendoscopy in early colorectal cancer: a cross-sectional interpretation test. BMC Gastroenterol. 2014;14:100. doi: 10.1186/1471-230X-14-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wada Y, Kudo SE, Kashida H, Ikehara N, Inoue H, Yamamura F, Ohtsuka K, Hamatani S. Diagnosis of colorectal lesions with the magnifying narrow-band imaging system. Gastrointest Endosc. 2009;70(3):522–531. doi: 10.1016/j.gie.2009.01.040. [DOI] [PubMed] [Google Scholar]
- 24.Nakadoi K, Tanaka S, Kanao H, Terasaki M, Takata S, Oka S, Yoshida S, Arihiro K, Chayama K. Management of T1 colorectal carcinoma with special reference to criteria for curative endoscopic resection. J Gastroenterol Hepatol. 2012;27(6):1057–1062. doi: 10.1111/j.1440-1746.2011.07041.x. [DOI] [PubMed] [Google Scholar]
- 25.Benizri EI, Bereder JM, Rahili A, Bernard JL, Vanbiervliet G, Filippi J, Hebuterne X, Benchimol D. Additional colectomy after colonoscopic polypectomy for T1 colon cancer: a fine balance between oncologic benefit and operative risk. Int J Color Dis. 2012;27(11):1473–1478. doi: 10.1007/s00384-012-1464-0. [DOI] [PubMed] [Google Scholar]
- 26.Shimomura T, Ishiguro S, Konishi H, Wakabayashi N, Mitsufuji S, Kasugai T, Manou M, Kodama T. New indication for endoscopic treatment of colorectal carcinoma with submucosal invasion. J Gastroenterol Hepatol. 2004;19(1):48–55. doi: 10.1111/j.1440-1746.2004.03261.x. [DOI] [PubMed] [Google Scholar]
- 27.Sohn DK, Chang HJ, Park JW, Choi DH, Han KS, Hong CW, Jung KH, Kim DY, Lim SB, Choi HS, Jeong SY. Histopathological risk factors for lymph node metastasis in submucosal invasive colorectal carcinoma of pedunculated or semipedunculated type. J Clin Pathol. 2007;60(8):912–915. doi: 10.1136/jcp.2006.043539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oka S, Tanaka S, Nakadoi K, Kanao H, Chayama K. Risk analysis of submucosal invasive rectal carcinomas for lymph node metastasis to expand indication criteria for endoscopic resection. Dig Endosc Off J Japan Gastroenterol Endosc Soc. 2013;25(Suppl 2):21–25. doi: 10.1111/den.12089. [DOI] [PubMed] [Google Scholar]
- 29.Ueno H, Hashiguchi Y, Kajiwara Y, Shinto E, Shimazaki H, Kurihara H, Mochizuki H, Hase K. Proposed objective criteria for "grade 3" in early invasive colorectal cancer. Am J Clin Pathol. 2010;134(2):312–322. doi: 10.1309/AJCPMQ7I5ZTTZSOM. [DOI] [PubMed] [Google Scholar]
- 30.Saito Y, Yamada M, So E, Abe S, Sakamoto T, Nakajima T, Otake Y, Ono A, Matsuda T. Colorectal endoscopic submucosal dissection: technical advantages compared to endoscopic mucosal resection and minimally invasive surgery. Dig Endosc Off J Japan Gastroenterol Endosc Soc. 2014;26(Suppl 1):52–61. doi: 10.1111/den.12196. [DOI] [PubMed] [Google Scholar]
- 31.Asayama N, Oka S, Tanaka S, Hayashi N, Arihiro K, Chayama K. Endoscopic submucosal dissection as total excisional biopsy for clinical T1 colorectal carcinoma. Digestion. 2015;91(1):64–69. doi: 10.1159/000368866. [DOI] [PubMed] [Google Scholar]
- 32.Hamatani S, Kudo S, Miyachi HA. Pathological problem associated with permeation distance of 1000μm in relation to colorectal SM invasive cancer. Intestine. 2012;16(2):137–141. [Google Scholar]
- 33.Yoshida N, Yanagisawa A, Sakai K, et al. Necessity of measurement of depth of submucosal invasion in cancers invading the submucosa. Gastroenterol Endosc. 2010;52(6):1522–1527. [Google Scholar]
- 34.Kudo S, Lambert R, Allen JI, Fujii H, Fujii T, Kashida H, Matsuda T, Mori M, Saito H, Shimoda T, Tanaka S, Watanabe H, Sung JJ, Feld AD, Inadomi JM, O'Brien MJ, Lieberman DA, Ransohoff DF, Soetikno RM, Triadafilopoulos G, Zauber A, Teixeira CR, Rey JF, Jaramillo E, Rubio CA, Van Gossum A, Jung M, Vieth M, Jass JR, Hurlstone PD. Nonpolypoid neoplastic lesions of the colorectal mucosa. Gastrointest Endosc. 2008;68(4 Suppl):S3–S47. doi: 10.1016/j.gie.2008.07.052. [DOI] [PubMed] [Google Scholar]
- 35.Kudo S, Tamura S, Nakajima T, Yamano H, Kusaka H, Watanabe H. Diagnosis of colorectal tumorous lesions by magnifying endoscopy. Gastrointest Endosc. 1996;44(1):8–14. doi: 10.1016/S0016-5107(96)70222-5. [DOI] [PubMed] [Google Scholar]
- 36.Bosman FTCH, Hruban RH, Theise ND. WHO classification of tumours of the digestive system. Lyon: IARC Press; 2010. [Google Scholar]
- 37.Ueno H, Murphy J, Jass JR, Mochizuki H, Talbot IC. Tumour ‘budding’ as an index to estimate the potential of aggressiveness in rectal cancer. Histopathology. 2002;40:127–132. doi: 10.1046/j.1365-2559.2002.01324.x. [DOI] [PubMed] [Google Scholar]
- 38.Ajioka Y, Kawachi H, Tanaka S. Pathologic problems for expansion of concept of the curative condition in cases with submucosal invasive carcinoma resected endoscopically ─with special reference to the method for measuring depth of SM invasion. Stomach Intest. 2011;46(10):1453–1458. [Google Scholar]
- 39.Bujanda L, Cosme A, Gil I, Arenas-Mirave JI. Malignant colorectal polyps. World J Gastroenterol. 2010;16(25):3103–3111. doi: 10.3748/wjg.v16.i25.3103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kudo SE, Takemura O, Ohtsuka K. Flat and depressed types of early colorectal cancers: from east to west. Gastrointest Endosc Clin N Am. 2008;18(3):581–593. doi: 10.1016/j.giec.2008.05.013. [DOI] [PubMed] [Google Scholar]
- 41.Rembacken BJ, Fujii T, Cairns A, Dixon MF, Yoshida S, Chalmers DM, Axon AT. Flat and depressed colonic neoplasms: a prospective study of 1000 colonoscopies in the UK. Lancet. 2000;355(9211):1211–1214. doi: 10.1016/S0140-6736(00)02086-9. [DOI] [PubMed] [Google Scholar]
- 42.Jaramillo E, Watanabe M, Slezak P, Rubio C. Flat neoplastic lesions of the colon and rectum detected by high-resolution video endoscopy and chromoscopy. Gastrointest Endosc. 1995;42(2):114–122. doi: 10.1016/S0016-5107(95)70066-8. [DOI] [PubMed] [Google Scholar]
- 43.Fujii T, Rembacken BJ, Dixon MF, Yoshida S, Axon AT. Flat adenomas in the United Kingdom: are treatable cancers being missed? Endoscopy. 1998;30(5):437–443. doi: 10.1055/s-2007-1001304. [DOI] [PubMed] [Google Scholar]
- 44.Chiu HM, Lin JT, Chen CC, Lee YC, Liao WC, Liang JT, Shun CT, Wang HP, Wu MS. Prevalence and characteristics of nonpolypoid colorectal neoplasm in an asymptomatic and average-risk Chinese population. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc. 2009;7(4):463–470. doi: 10.1016/j.cgh.2008.11.026. [DOI] [PubMed] [Google Scholar]
- 45.Tsuda S, Veress B, Toth E, Fork FT. Flat and depressed colorectal tumours in a southern Swedish population: a prospective chromoendoscopic and histopathological study. Gut. 2002;51(4):550–555. doi: 10.1136/gut.51.4.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shimoda T, Ikegami M, Fujisaki J, Matsui T, Aizawa S, Ishikawa E. Early colorectal carcinoma with special reference to its development de novo. Cancer. 1989;64(5):1138–1146. doi: 10.1002/1097-0142(19890901)64:5<1138::AID-CNCR2820640529>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- 47.Nakadoi K, Oka S, Tanaka S, Hayashi N, Terasaki M, Arihiro K, Shimamoto F, Chayama K. Condition of muscularis mucosae is a risk factor for lymph node metastasis in T1 colorectal carcinoma. Surg Endosc. 2014;28(4):1269–1276. doi: 10.1007/s00464-013-3321-9. [DOI] [PubMed] [Google Scholar]
- 48.Tateishi Y, Nakanishi Y, Taniguchi H, Shimoda T, Umemura S. Pathological prognostic factors predicting lymph node metastasis in submucosal invasive (T1) colorectal carcinoma. Mod Pathol Off J US Can Acad Pathol Inc. 2010;23(8):1068–1072. doi: 10.1038/modpathol.2010.88. [DOI] [PubMed] [Google Scholar]
- 49.Quirke P, Risio M, Lambert R, von Karsa L, Vieth M. Quality assurance in pathology in colorectal cancer screening and diagnosis-European recommendations. Virchows Arch Int J Pathol. 2011;458(1):1–19. doi: 10.1007/s00428-010-0977-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kikuchi R, Takano M, Takagi K, Fujimoto N, Nozaki R, Fujiyoshi T, Uchida Y. Management of early invasive colorectal cancer. Risk of recurrence and clinical guidelines. Dis Colon Rectum. 1995;38(12):1286–1295. doi: 10.1007/BF02049154. [DOI] [PubMed] [Google Scholar]
- 51.Okamoto Y, Mitomi H, Ichikawa K, Tomita S, Fujimori T, Igarashi Y. Effect of skip lymphovascular invasion on hepatic metastasis in colorectal carcinomas. Int J Clin Oncol. 2014 doi: 10.1007/s10147-014-0778-z. [DOI] [PubMed] [Google Scholar]